Respuesta patológica completa de pacientes con cáncer de mama HER2 positivo tratadas con quimioterapia neoadyuvante en Colombia
Resumen
Introduction. Breast cancer is the most common type of cancer and the leading cause of death by cancer in women in Colombia. Approximately 15 to 20% of breast cancers overexpress HER2.
Objective. To analyze the relationship between multiple clinical and histological variables and pathological complete response in patients with HER2-positive breast cancer undergoing neoadjuvant therapy in a specialized cancer center in Colombia.
Materials and methods. We performed a retrospective analysis of non-metastatic HER2-positive breast cancer patients who received neoadjuvant therapy between 2007 and 2020 at the Instituto de Cancerología Las Americas Auna (Medellín, Colombia). Assessed parameters were tumor grade, proliferation index, estrogen receptor, progesterone receptor, HER2 status, type of neoadjuvant therapy, pathologic complete response rates, and overall survival.
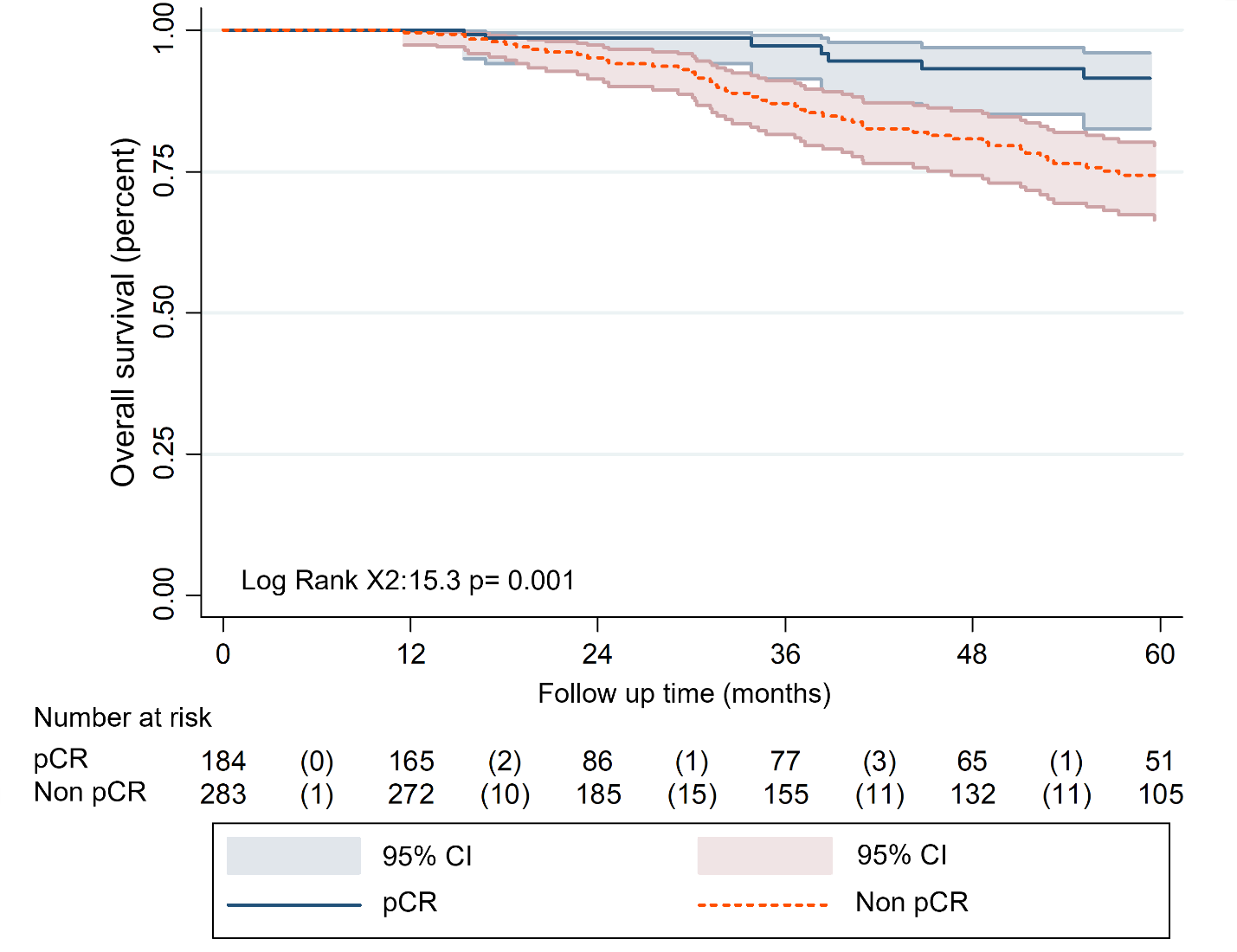
Results. Variables associated with low pathologic complete response rates were tumor grades 1-2 (OR = 0.55; 95% CI = 0.37-0.81; p = 0.03), estrogen receptor positivity (OR =0.65; 95%; CI = 0.43-0.97; p=0.04), and progesterone receptor positivity (OR = 0.44; 95% CI = 0.29-0.65; p = 0.0001). HER2 strong positivity (score 3+) was associated with high pathological complete response rates (OR = 3.3; 95% CI = 1.3-8.35; p=0.013). Five-year overall survival was 91.5% (95% CI = 82.6-95.9) in patients with pathological complete response and 73.6% (95% CI = 66.4-79.6) in patients who did not achieve pathological complete response (p = 0.001). Additionally, the pathological complete response rate was three times higher in patients receiving combined neoadjuvant chemotherapy with anti-HER2 therapy than in those with chemotherapy alone (48% versus 16%).
Conclusion. In patients with HER2-positive breast cancer, tumor grade 3, estrogen receptor negativity, progesterone receptor negativity, strong HER2 positivity (score 3+), and the use of the neoadjuvant trastuzumab are associated with higher pathological complete response rates.
Descargas
Referencias bibliográficas
Ministerio de Salud y Protección Social. Boletín del aseguramiento en salud. Boletín No. 01 -Primer trimestre 2017. Accessed: February 10, 2022. Available in: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VP/DOA/boletin-aseguramiento-i-trimestre-2017.pdf.
Pardo C, de Vries E, Buitrago L, Gamboa O. Atlas de mortalidad por cáncer en Colombia. Cuarta edición. Bogotá, D. C.: Instituto Nacional de Cancerología; 2017. p. 124.
Bravo LE, Muñoz N. Epidemiology of cancer in Colombia. Colomb Med. 2018;49:9-12. https://doi.org/10.25100/cm.v49i1.3877
Brome-Bohórquez MR, Montoya-Restrepo DM, Amell L. Cancer incidence and mortality in Medellín-Colombia, 2010-2014. Colomb Med. 2018;49:81-8. https://doi.org/10.25100/cm.v49i1.3740
Registro Poblacional de Cáncer de Antioquia. Situación del cáncer, departamento de Antioquia. Año 2017. Accessed: February 10, 2022. Available in: https://www.dssa.gov.co/images/estadisticas/cancer/Perfil_Epidemiologio_Cancer_Version28_Mayo2019_Definitivo.pdf
Ossa CA, Gómez R, Ascuntar J, García H. Supervivencia global y libre de enfermedad según subtipo molecular intrínseco en una cohorte de 2.200 pacientes con cáncer de mama. Experiencia de un centro colombiano. Revista Médica Sanitas. 2015;18:122-32.
Egurrola-Pedraza JA, Gómez-Wolff LR, Ossa-Gómez CA, Sánchez-Jiménez V, Herazo-Maya F, García-García HI. Diferencias en supervivencia debidas al aseguramiento en salud en pacientes con cáncer de mama atendidas en un centro oncológico de referencia en Medellín, Colombia. Cad Saúde Publica. 2018;34:e00114117. https://doi.org/10.1590/0102-311X00114117
Narod SA, Iqbal J, Miller AB. Why have breast cancer mortality rates declined? J Cancer Policy. 2015;5:8-17. https://doi.org/10.1016/j.jcpo.2015.03.002
Azamjah N, Soltan-Zadeh Y, Zayeri F. Global trend of breast cancer mortality rate: A 25-year study. Asian Pacific J Cancer Prev. 2019;20:2015-20. https://doi.org/10.31557/APJCP.2019.20.7.2015
Sotiriou C, Neo SY, McShane LM, Korn EL, Long PM, Jazaeri A, et al. Breast cancer classification and prognosis based on gene expression profiles from a population-based study. Proc Natl Acad Sci USA. 2003;100:10393-8. https://doi.org/10.1073/pnas.1732912100
Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thürlimann B, et al. Personalizing the treatment of women with early breast cancer: Highlights of the St Gallen international expert consensus on the primary therapy of early breast cancer 2013. Ann Oncol. 2013;9:2206-23. https://doi.org/10.1093/annonc/mdt303
Wuerstlein R, Harbeck N. Neoadjuvant therapy for HER2-positive breast cancer. Rev Recent Clin Trials. 2017;12:81-92. https://doi.org/10.2174/1574887112666170202165049
Von Minckwitz G, Untch M, Blohmer JU, Costa SD, Eidtmann H, Fasching PA, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30:1796-804. https://doi.org/10.1200/JCO.2011.38.8595
von Minckwitz G, Huang CS, Mano MS, Loibl S, Mamounas EP, Untch M, et al. Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N Engl J Med. 2019;380:617-28. https://doi.org/10.1056/NEJMoa1814017
Mieog JSD, van der Hage JA, van de Velde CJH. Preoperative chemotherapy for women with operable breast cancer. Cochrane Database Syst Rev. 2007;2:CD005002. https://doi.org/10.1002/14651858.CD005002.pub2
Asselain B, Barlow W, Bartlett J, Bergh J, Bergsten-Nordström E, Bliss J, et al. Long-term outcomes for neoadjuvant versus adjuvant chemotherapy in early breast cancer: Metaanalysis of individual patient data from ten randomised trials. Lancet Oncol. 2018;19:27-39. https://doi.org/10.1016/S1470-2045(17)30777-5
Balic M, Thomssen C, Würstlein R, Gnant M, Harbeck N. St. Gallen/Vienna 2019: A brief summary of the consensus discussion on the optimal primary breast cancer treatment. Breast Care (Basel). 2019;14:103-10. https://doi.org/10.1159/000499931
Gianni L, Eiermann W, Semiglazov V, Lluch A, Tjulandin S, Zambetti M, et al. Neoadjuvant and adjuvant trastuzumab in patients with HER2-positive locally advanced breast cancer (NOAH): Follow-up of a randomised controlled superiority trial with a parallel HER2-negative cohort. Lancet Oncol. 2014;15:640-7. https://doi.org/10.1016/S1470-2045(14)70080-4
Cortázar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: The CTNeoBC pooled analysis. Lancet. 2014;384:164-72. https://doi.org/10.1016/S0140-6736(13)62422-8
Korde LA, Somerfield MR, Carey LA, Crews JR, Denduluri N, Hwang ES, et al. Neoadjuvant chemotherapy, endocrine therapy, and targeted therapy for breast cancer: ASCO guideline. J Clin Oncol. 2021;39:1485-505. https://doi.org/10.1200/JCO.20.03399
Leon-Ferre RA, Hieken TJ, Boughey JC. The Landmark series: Neoadjuvant chemotherapy for triple-negative and HER2-positive breast cancer. Ann Surg Oncol. 2021;28:2111-9. https://doi.org/10.1245/s10434-020-09480-9
Gianni L, Pienkowski T, Im YH, Tseng LM, Liu MC, Lluch A, et al. 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): A multicentre, open-label, phase 2 randomised trial. Lancet Oncol. 2016;17:791-800. https://doi.org/10.1016/S1470-2045(16)00163-7
Petrelli F, Borgonovo K, Cabiddu M, Ghilardi M, Barni S. Neoadjuvant chemotherapy and concomitant trastuzumab in breast cancer: A pooled analysis of two randomized trials. Anticancer Drugs. 2011;22:128-35. https://doi.org/10.1097/cad.0b013e32834120aa
Kuehn T, Bauerfeind I, Fehm T, Fleige B, Hausschild M, Helms G, et al. Sentinel-lymphnode biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): A prospective, multicentre cohort study. Lancet Oncol. 2013;14:609-18. https://doi.org/10.1016/S1470-2045(13)70166-9
von Minckwitz G, Untch M, Nüesch E, Loibl S, Kaufmann M, Kümmel S, et al. Impact of treatment characteristics on response of different breast cancer phenotypes: Pooled analysis of the German neo-adjuvant chemotherapy trials. Breast Cancer Res Treat. 2011;125:145-56. https://doi.org/10.1007/s10549-010-1228-x
Schneeweiss A, Chia S, Hickish T, Harvey V, Eniu A, Waldron-Lynch M, et al. Long-term efficacy analysis of the randomised, phase II TRYPHAENA cardiac safety study: Evaluating pertuzumab and trastuzumab plus standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer. Eur J Cancer. 2018;89:27-35. https://doi.org/10.1016/j.ejca.2017.10.021
Chen S, Liang Y, Feng Z, Wang M. Efficacy and safety of HER2 inhibitors in combination with or without pertuzumab for HER2-positive breast cancer: A systematic review and metaanalysis. BMC Cancer. 2019;19:973. https://doi.org/10.1186/s12885-019-6132-0
Nakashoji A, Hayashida T, Yokoe T, Maeda H, Toyota T, Kikuchi M, et al. The updated network meta-analysis of neoadjuvant therapy for HER2-positive breast cancer. Cancer Treat Rev. 2018;62:9-17. https://doi.org/10.1016/j.ctrv.2017.10.009
Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30:1194-220. https://doi.org/10.1093/annonc/mdz173
Niikura N, Tomotaki A, Miyata H, Iwamoto T, Kawai M, Anan K, et al. Changes in tumor expression of HER2 and hormone receptors status after neoadjuvant chemotherapy in 21,755 patients from the Japanese breast cancer registry. Ann Oncol. 2016;27:480-7. https://doi.org/10.1093/annonc/mdv611
Algunos artículos similares:
- Guillermo Sánchez, Carlos Gustavo Niño, Carolina Estupiñán, Factores asociados con el tratamiento oportuno de mujeres con cáncer de mama apoyadas por una organización no gubernamental en Bogotá , Biomédica: Vol. 35 Núm. 4 (2015)
- Jefferson Antonio Buendía, Carlos Vallejos, Andrés Pichón-Rivière, Evaluación económica del trastuzumab como tratamiento adyuvante en cáncer de mama HER2- positivo en Colombia , Biomédica: Vol. 33 Núm. 3 (2013)
- Elizabeth Borrero, Gabriel Carrasquilla, Neal Alexander, Descentralización y reforma: ¿cuál es su impacto sobre la incidencia de malaria en los municipios colombianos? , Biomédica: Vol. 32 (2012): Suplemento 1, Malaria
- Óscar Gamboa, Sandra Díaz, Liliana Chicaíza, Mario García, Análisis de costo-efectividad en Colombia de anastrazol Vs. tamoxifeno como terapia inicial en mujeres con cáncer temprano de mama y receptor hormonal positivo , Biomédica: Vol. 30 Núm. 1 (2010)
- Sandra Lorena Girón, Julio César Mateus, Fabián Méndez, Impacto de un botadero a cielo abierto en el desarrollo de síntomas respiratorios y en costos familiares de atención en salud de niños entre 1 y 5 años en Cali, Colombia , Biomédica: Vol. 29 Núm. 3 (2009)
- José Joaquín Carvajal, Ligia Inés Moncada, Mauricio Humberto Rodríguez, Ligia del Pilar Pérez, Víctor Alberto Olano, Caracterización preliminar de los sitios de cría de Aedes (Stegomyia) albopictus (Skuse, 1894) (Diptera: Culicidae) en el municipio de Leticia, Amazonas, Colombia , Biomédica: Vol. 29 Núm. 3 (2009)
- Jaime E. Bernal, Martha Lucía Tamayo , Ignacio Briceño , Escilda Benavides , Tamizaje neonatal en Colombia: la experiencia de un programa privado en Bogotá , Biomédica: Vol. 44 Núm. 1 (2024)
- Patricia Escobar, Katherine Paola Luna, Indira Paola Hernández, César Mauricio Rueda, María Magdalena Zorro, Simon L. Croft, Susceptibilidad in vitro a hexadecilfosfocolina (miltefosina), nifurtimox y benznidazole de cepas de Trypanosoma cruzi aisladas en Santander, Colombia , Biomédica: Vol. 29 Núm. 3 (2009)
- Gustavo Pradilla, Julio César Mantilla, Reynaldo Badillo, Encefalitis rábica humana por mordedura de murciélago en un área urbana de Colombia , Biomédica: Vol. 29 Núm. 2 (2009)
- Rosa Magdalena Uscátegui, Adriana M. Correa, Jaime Carmona-Fonseca, Cambios en las concentraciones de retinol, hemoglobina y ferritina en niños palúdicos colombianos , Biomédica: Vol. 29 Núm. 2 (2009)
Derechos de autor 2023 Biomédica

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |

























