Abstract
Background:
Endometriosis is a chronic disease in women of reproductive age accompanied by chronic pelvic pain and painful intercourse. It has a severe negative impact on these patients' psychosocial parameters. The noninvasive treatment of endometriosis remains challenging.Objectives:
This study aimed to investigate the effectiveness of hypnotherapy on the pain intensity of endometriosis patients treated with dienogest.Methods:
In this preliminary study (a pilot double-blind, randomized clinical trial), conducted from November 2021 to July 2022, 22 patients (18 to 45 years old) with endometriosis treated with dienogest in Shahid Akbar Abadi Hospital (Tehran, Iran) were enrolled. Via block randomization, they were divided into a control group and an intervention group (n = 11 each). The patients of both groups were given 2 mg of dienogest tablets daily as prescribed by the gynecologist. The main intervention involved hypnotherapy, which was administered only for the intervention group individually for 8 weekly sessions online (on WhatsApp) for 30 - 45 minutes. Dysmenorrhea, dyspareunia, and chronic pelvic pain were evaluated using the visual analog scale (VAS) at the beginning of the intervention, immediately after the intervention, and 4 weeks after the intervention in both groups. Mean, standard deviation, frequency, chi-square, Fisher's exact test, Mann-Whitney U, and Friedman test were used for data analysis.Results:
Dysmenorrhea severity score in the intervention group was 6.30 ± 1.25 before the intervention, 5.50 ± 1.08 after the intervention, and 4.60 ± 0.97 during the follow-up, and the changes were significant (P < 0.001, effect size = 0.93). Dyspareunia severity score was 3.14 ± 4.50 before the intervention, 2.91 ± 4.30 after the intervention, and 2.42 ± 3.50 during the follow-up. These changes were also significant (P = 0.015, effect size = 0.41). However, the pelvic pain score did not significantly change despite the average decrease of 0.2 during the follow-up (P = 0.135).Conclusions:
Hypnotherapy, along with drug treatment, was more effective in relieving endometriosis pain than drug treatment alone.Keywords
Endometriosis Hypnotherapy Pain Dienogest Dysmenorrhea Dyspareunia
1. Background
Endometriosis is a progressive, chronic, estrogen-dependent disorder in women in which the endometrial tissue grows outside the uterine cavity and leads to inflammation (1). The endometrial tissue responds to hormonal changes and bleeding during menstruation (2) and leads to cysts, adhesions, and fibrosis, which may cause chronic pelvic pain and infertility (3). Today, the incidence of endometriosis is increasing in different communities. It is estimated that this chronic disease affects between 10 and 15% of women of childbearing age (4). According to the latest statistics, endometriosis afflicts about 176 million women annually all over the world (5). Despite these statistics, the exact prevalence of this disease is not known because there are no accurate non-invasive tools for diagnosing it; moreover, it is asymptomatic in some cases (6).
The pelvis is the most common part of endometriosis. The most prevalent and annoying symptom of this disease is pain, which directs the patient to medical centers more than other signs and symptoms (7, 8). According to the definition of the International Association for the Study of Pain, pain is an unpleasant sensory or emotional experience that is associated with actual or potential injury and has sensory and emotional dimensions. The sensory dimension of pain refers to the intensity of pain, while the emotional dimension refers to the level of unhappiness experienced by the person (9). The location and intensity of pain in endometriosis patients are different, and the most common type is chronic pelvic pain (10). The other common pains include back pain (with disruption of daily activities) (11), dysmenorrhea (painful menstruation with heavy bleeding and possible absenteeism from school or work) (12), and dyspareunia (painful intercourse, with sexual dysfunction and complications negatively affecting couples' relationships) (13, 14). Constant pain has adverse effects on all aspects of life, such as familial and marital relations, social activities, sports, work, and education. Patients with chronic pain suffer from long-term psychological problems, impaired physical performance, excessive dependence on others, and an uncertain prognosis (15). Therefore, disease management should aim to improve the health-related quality of life of patients by alleviating the symptoms and preventing long-term complications (14, 15).
Nowadays, psychological interventions such as cognitive behavioral therapy (CBT) (16), yoga (17), and hypnotherapy (18) are administered simultaneously with drug treatments to obtain better results and reduce side effects in endometriosis patients (19). Hypnosis is a transitory state that arises from a change in a person's attention and includes phenomena such as changes in awareness and memory, increased sensitivity, suggestibility, and the occurrence of responses and ideas that are not present in the person's normal state) (18).
Due to the prevalence of endometriosis, the effect of psychological factors in this disease, and the dearth of studies on this topic, research seems necessary for planning appropriate nonpharmacological treatment strategies. In addition, due to the side effects of this disease, high economic costs of its treatment, drug interactions, and side effects which have caused many problems for these patients, the achievement of nonpharmacological treatment methods, in parallel with drug treatments, may reduce the duration of treatment and accelerate recovery.
2. Objectives
This study aimed to determine the effect of hypnotherapy on reducing the pain of patients with endometriosis treated with dinogest.
3. Methods
This was a pilot double-blind, randomized clinical trial (2021 - 2022) with ethical code IR.MAZUMS.REC.1400.398 and IRCT code IRCT20110827007422N4.
3.1. Participants
The participants were selected from patients with endometriosis who visited the Gynecology Clinic of Shahid Akbar Abadi Hospital (Tehran, Iran) from November 2021 to July 2022.
3.2. Inclusion Criteria
Women were included if they had endometriosis (confirmed by laparoscopy or laparotomy and histology), were treated with dienogest, were married, aged 18 - 45 years, complained of painful menstruation or painful intercourse, or had pelvic pain with a minimum score of 5 cm on the visual analog scale (VAS) at the beginning of the treatment (18), had a smartphone, and had access to the internet.
3.3. Exclusion Criteria
Women were excluded if they had a history of endometriosis treatment (laparotomy, laparoscopy, or hysterectomy), a history of major or minor psychiatric disorders in themselves or a first-degree relative (father, mother, sister, brother, or child), used other nonpharmacological methods to reduce pain (e.g., yoga, herbal medicine, acupressure, acupuncture, traditional medicine, and biofeedback), or were treated for anxiety, depression, or uncontrolled seizures.
3.4. Sample Size
The sample size was considered to be 10 people in each group according to the recommendations of Herzog et al. for pilot studies (20), based on the formula for calculating the sample size by the pilot method. With a 10% attrition rate in mind, the sample size of 22 (11 people in the intervention group and 11 people in the control group) was calculated, and the multiprotocol method was used to calculate the missing data.
3.5. Variables
The primary outcome was changes in pain scores between groups over time. The participants' satisfaction with the intervention was examined as the secondary outcome.
3.6. Randomization
The sampling method was convenient in the first stage to identify eligible women with endometriosis treated with dienogest, and block randomization was used in the next stage. The numbers were randomly generated with the RANDBETWEEN command in Microsoft Excel version 2016 in the range of 0 - 6. Blinding was performed at the outcome assessor level and evaluation at the analysis level.
3.7. Procedure
The eligible individuals provided written informed consent. Then, the demographic information form was completed by the patients of both groups who were treated with dienogest at the rate of a 2mg tablet per day based on the standard treatment of the international endometriosis protocols (3).
For the intervention group (11 people treated with dienogest), an experienced researcher who was trained in the Iranian Scientific Society of Clinical Hypnosis and had a valid certificate performed hypnotherapy. For each patient in the intervention group, 8 sessions of hypnotherapy were administered. The first session was face-to-face and individual and lasted for 40 minutes (21). The remaining 7 sessions of hypnotherapy were held weekly, individually, online (on WhatsApp), and for 30-45 minutes for the intervention group. At the end of each session, an audio recording of the session was made for each participant (Table 1). The intervention group was asked to perform hypnosis exercises at home at least twice a day (for 30 minutes) and to record the number of exercises in the form provided to them. No intervention was administered during the study for the control group (11 people treated with dienogest). Only after the research process was completed, to comply with research ethics, the control group was presented with the recorded files of the hypnotherapy sessions.
The Content of the Hypnotherapy Sessions for Endometriosis
| Session | The Content of the Session |
|---|---|
| First | History taking, full explanation of how to do the work, and resolving misconceptions about hypnosis |
| Second | Advanced muscle relaxation (PMR) a technique |
| Third | Induction and deepening |
| Forth | Ego boost |
| Fifth | Conditioning |
| Sixth | Age regression |
| Seventh | Age progression |
| Eighth | Reviewing previous sessions and filling out the questionnaires |
For the intervention group, the number of times they did the hypnosis exercises, took painkillers, or used other nonpharmacological methods of pain control was asked twice a week during a telephone interview. The patients of both groups were given the visual analog scale on 3 occasions (at the beginning of the intervention, immediately after the intervention, and 4 weeks after the intervention). Both groups were taught to register in the special forms provided to them if they received any type of pain reliever during this period. The registration forms were collected at the end of each week. After the completion of the training and intervention sessions, for 4 weeks, the process of performing the hypnosis exercises by the patients was followed via telephone interviews once a week (22). Four weeks after the end of the intervention, the researcher checked the pain level of the participants again.
3.8. Questionnaires
3.8.1. Medical and Demographic Information Form
This form was designed after an extensive review of the relevant literature and input from the research team. It examined the following items: Age, the individual's adequacy of monthly income, socioeconomic status, level of satisfaction with the socioeconomic status, home ownership status, occupation, education level, and marital status.
3.8.2. Visual Analog Scale
The visual analog scale (VAS) (1) is the most widely used tool for measuring pain intensity. Besides its validity and reliability, the most important feature of this tool is its ease of use. The VAS for measuring pain intensity involves the use of a 10cm graduated line, where a score of 10 is considered for the most severe pain and a score of 0 for no pain. The intensity of pain is determined by the patient on the line. Scores of 1 - 3 indicate mild pain, 4 - 7 indicate moderate pain, and 8 - 10 indicate severe pain (23). The VAS is the most widely used scale in endometriosis studies, with a minimum clinically important difference after treatment (MCID) minimal clinically important difference (23). The validity and reliability of this tool have been confirmed in many studies. In the study of Hawker et al., the reliability of VAS was confirmed with a correlation of 0.99 between the vertical and horizontal directions (24). In Iran, the reliability of this scale was confirmed with a correlation coefficient of r = 0.88 (25, 26).
3.9. Ethical Considerations
This study was approved by the Ethics Committee of Mazandaran University of Medical Sciences (ethics code: IR.MAZUMS.REC.1400.398) and reported according to the CONSORT (Consolidated Standards of Reporting Trials) guidelines. All the participants signed the informed consent form. There was no financial compensation.
3.10. Data Analysis
Descriptive and inferential statistical methods were used to analyze the data. The data were entered into SPSS v. 25 (IBM Corp., Armonk, NY, USA). Descriptive statistical methods such as mean, median, standard deviation (SD), and frequency were used for demographic characteristics. Effect size was used to evaluate the strength of the intervention effect (27). The Shapiro-Wilk test was performed to check the normality of the variables' distribution. The chi-square test and Fisher's exact test were used to compare the qualitative data. The Mann-Whitney U test was used to compare the means of the groups, and the Friedman test was performed to compare the within-group means. The significance level was P < 0.05.
4. Results
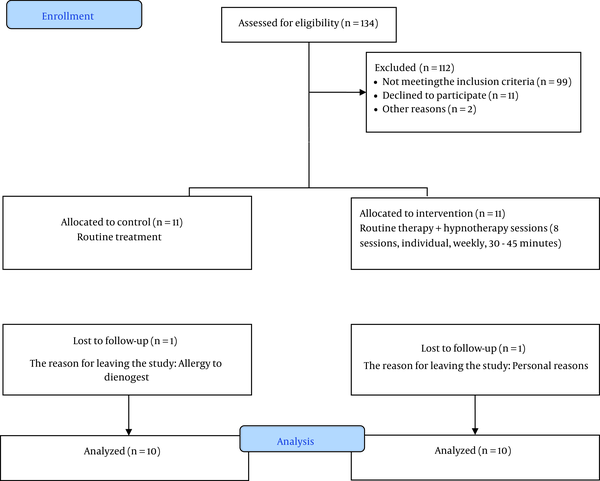
Figure 1 shows that 20 people (10 in the control group and 10 in the intervention group) completed the study. The two groups did not significantly differ from each other in terms of education, age, occupation, satisfaction with income, socioeconomic status, satisfaction with the socioeconomic status, home ownership, and the family history of endometriosis (Table 2).
Enrollment of the participants
Comparison of the Frequency of Demographic Variables in the Control and Intervention Groups at the Beginning of the Study
| Variables | Control Group, No. (%) | Intervention Group, No. (%) | P-Value |
|---|---|---|---|
| Education | |||
| Lower than a high school diploma | 3 (27.3) | 4 (36.4) | 1.000 a |
| University | 8 (72.7) | 7 (63.6) | |
| Age, y | |||
| 19 - 35 | 6 (54.5) | 7 (63.6) | 0.655 |
| >35 | 5 (45.5) | 4 (36.4) | |
| Occupation | |||
| Unemployed | 1 (9.1) | 3 (27.3) | 0.586 a |
| Employed | 10 (90.9) | 8 (72.7) | |
| Satisfaction with income | |||
| Not at all | 3 (27.3) | 3 (27.3) | 1.000 a |
| Almost or completely | 8 (72.7) | 8 (72.7) | |
| Socioeconomic status | |||
| Low | 1 (9.1) | 2 (18.2) | 1.000 a |
| Moderate or high | 10 (90.9) | 9 (81.8) | |
| Satisfaction with the socioeconomic status | |||
| Not at all | 4 (36.4) | 4 (36.4) | 1.000 a |
| Almost or completely | 7 (63.6) | 7 (63.6) | |
| Homeownership | |||
| Owner | 7 (63.6) | 5 (50.0) | 0.528 |
| Tenant | 4 (36.4) | 5 (50.0) | |
| Family history of endometriosis | |||
| No | 4 (36.4) | 6 (54.5) | 0.392 |
| Yes | 7 (63.6) | 5 (45.5) |
Using the Shapiro-Wilk test, we found that the data related to dysmenorrhea, dyspareunia, and pelvic pain did not have a normal distribution (P < 0.05). The results of the Friedman test showed that the dysmenorrhea score in the control and intervention groups had a significant decrease over time. In the intervention group, we saw an effect size of 0.93 versus the control group (0.70). Dyspareunia was significantly reduced in both intervention and control groups over time, and the effect sizes were approximately the same (0.44 versus 0.41, respectively). However, pelvic pain did not significantly decline over time in the control and intervention groups (Table 3). The results of the Mann-Whitney U test (Table 3) show that the effect of the group in the dysmenorrhea score was not significant before the intervention, but it was significant immediately after the intervention with a high effect (0.73), i.e., the pain score of the intervention group was lower than that of the control group. The effect of the group on the dysmenorrhea score, with a high effect of 0.79, was also significant 4 weeks after the intervention, i.e., the pain score of the intervention group was lower than that of the control group. The effect of the group on dyspareunia score was not significant pre-intervention (P = 0.949). It was also nonsignificant immediately after the intervention. Although the dyspareunia score was less in the intervention group than in the control group after 4 weeks, the effect size was not significant. The effect of the group on the score of pelvic pain before the intervention, immediately after the intervention, and 4 weeks later was not significant (Table 3).
Comparison of the Pain Score Over Time Between and Within the Two Groups
| Type of Pain and Groups | Before the Intervention | After the Intervention | Follow-up (4 Weeks After Intervention) | P-Value a | Effect Size |
|---|---|---|---|---|---|
| Dysmenorrhea | |||||
| Control | 4.70 ± 2.41 | 3.20 ± 1.40 | 1.90 ± 0.57 | 0.001 | 0.70 |
| Intervention | 6.30 ± 1.25 | 5.50 ± 1.08 | 4.60 ± 0.97 | <0.001 | 0.93 |
| P-value b | 0.076 | 0.001 | <0.001 | ||
| Effect size | 0.40 | 0.73 | 0.79 | ||
| Dyspareunia | |||||
| Control | 4.00 ± 3.37 | 2.40 ± 2.07 | 1.90 ± 2.02 | 0.013 | 0.44 |
| Intervention | 4.50 ± 3.14 | 4.30 ± 2.91 | 3.50 ± 2.42 | 0.015 | 0.41 |
| P-value b | 0.949 | 0.089 | 0.165 | ||
| Effect size | 0.01 | 0.26 | 0.24 | ||
| Pelvic pain | |||||
| Control | 2.10 ± 2.64 | 1.30 ± 1.42 | 1.10 ± 1.10 | 0.062 | 0.27 |
| Intervention | 1.80 ± 2.25 | 1.80 ± 2.25 | 1.60 ± 2.01 | 0.135 | 0.20 |
| P-value b | 0.797 | 0.853 | 0.853 | ||
| Effect size | 0.06 | 0.04 | 0.04 |
5. Discussion
The present study determined the effectiveness of hypnotherapy on the pain intensity of endometriosis patients treated with dienogest.
The findings indicated that hypnotherapy sessions, along with the use of dienogest, caused a significant reduction in dysmenorrhea compared to dienogest alone. In 2010, a retrospective study in Germany evaluated the effectiveness of combined treatment of traditional Chinese medicine and hypnotherapy (SART) as a new treatment for endometriosis-related symptoms. In this study, the effect of hypnosis on relieving pain related to endometriosis, such as dysmenorrhea and dyschezia, was investigated, but it was not reported to be significant (18). The results of the mentioned study were not completely aligned with the results of the present study. This difference can be because the 2010 study compared two interventions, but only one intervention was investigated in the current study.
In the present study, the severity of dysmenorrhea complaints in the intervention group was declining and significant. Another randomized clinical trial in 2014 examined the effectiveness of hypnosis on dysmenorrhea in female freshman nursing students at the University of Nursing and Midwifery in India. This study concluded that hypnosis can be effective on primary dysmenorrhea in young girls (28). The results of this study, like the current study, showed the effect of hypnosis on dysmenorrhea, but the participants of the cited study were teenage girls who had dysmenorrhea and did not report any other disease (such as endometriosis). Another quasi-experimental study was conducted in 2015 to compare the effectiveness of CBT and therapeutic hypnosis on pain self-efficacy and pain intensity in girls with primary dysmenorrhea in Ardabil (Iran) (29). The effect of hypnosis on dysmenorrhea was confirmed in this study, as in the present research. The important differences between the mentioned study and the current research are the participants and objectives. Psychological treatment in women with endometriosis is more difficult due to the presence of several pains. The research population in the cited study were girls suffering from dysmenorrhea, none of whom had endometriosis, and the aim of the study was to compare CBT and hypnotherapy (29).
The role of hypnotherapy in relieving chronic pelvic pain was the second variable investigated in the current study. Although the average pelvic pain score in the intervention group decreased after the intervention and during the follow-up, the difference was not significant compared to before the study. In 2011, a study provided a supportive intervention by several psychologists and gynecologists and reported a reduction in pelvic pain and migraines in women with endometriosis. This study, like the current research, observed the validity of the protocol and determined the correct sample size for the generalizability of the results, but it did not report significant results. Still, the average pain in the intervention group was reduced (30). In 2014, a study explored the effectiveness of group acceptance and commitment therapy on catastrophic and disabling pain in women with chronic pelvic pain. The intervention group underwent group acceptance and commitment therapy for 8 sessions of 90 minutes. The results revealed that group acceptance and commitment therapy was effective in women with chronic pelvic pain based on the Pain Catastrophizing Scale (31). The results of this study were not in line with those of the current study. Although the interventions in the two studies were both psychological, their type differed; in hypnosis, the presence of the instructor is needed more than in other psychological interventions for long-term treatment. In another study, Treatment based on acceptance and commitment to catastrophizing and disabling pain commitment-based therapy was administered in person for 8 sessions of 90 minutes (31). A meta-analysis study showed that all psychological treatments can reduce chronic pelvic pain, but their overall results were not significant (32). The studies reviewed in this meta-analysis demonstrated that face-to-face and psychological studies are more effective than non-face-to-face interventions (32).
The role of hypnotherapy in the relief of dyspareunia was another finding of this study. In the current study, even though the average score in the intervention group after the sessions and at the follow-up significantly decreased compared to before the intervention due to the reduction of dyspareunia in the control group, this change was not significant compared to the control group. A 2020 meta-analysis examined 10 studies on hypnosis and dyspareunia and stated the effects of hypnosis on pain reduction during sexual activity (OR = 3.55; 95% CI = 2.63 - 4.79; P = 0.001). In this meta-analysis, 6 studies did not declare the results of psychological interventions to be effective in reducing dyspareunia, and their significance level was >0.05. However, due to the high significance level of the other 4 studies, the general index was declared effective and significant (33). Another study in 2018 explored the effect of cognitive-behavioral hypnotherapy on the improvement of anxiety and sexual performance of women with vaginismus (34). The cited study found that group, individual, and self-hypnosis hypnotherapy can alleviate anxiety and improve vaginismus. One of the complaints of the women participating in this study was pain at the beginning of intercourse, which significantly changed with hypnosis (34). The main reason for the difference in the results is the difference in the type of intervention.
The limitations of the present study include the sample size and the impossibility of generalizing the results to the entire population. Besides, since the statistical population comprised married women with endometriosis aged 18 - 45 years who could use smartphones and had access to the internet, it is not possible to generalize the findings to the entire target population.
One of the strengths of this study is the consistent, weekly, and individual sessions for each patient. Moreover, during the week, home exercises were followed up, the necessity of performing hypnosis during the day was reminded, the questions were answered, and their problems were resolved over phone calls. In conducting this study, blinding was carried out at the evaluator and analyzer level, which contributed to the strength of the results. Another strength of this research was the follow-up 4 weeks after the end of the intervention.
5.1. Conclusions
This preliminary study revealed that the treatment of endometriosis with hypnotherapy and Dienogest can lead to a significant reduction of pain, especially dysmenorrhea, in patients with resistant endometriosis. Hypnotherapy is a valuable complementary treatment method as part of a multifaceted approach to endometriosis treatment. Although the effect of hypnotherapy in decreasing dyspareunia was clinically significant, the reduction in dyspareunia pain and chronic pelvic pain was not statistically significant; therefore, more studies should be conducted in this field with larger samples.
An important implication of this study is the progress and necessity of hypnotherapy science. In emergencies such as the COVID-19 pandemic, when quarantine must be observed, or when it is not possible to visit the patient in person to start or continue the treatment process for any reason, hypnotherapy can be administered throughout the treatment process online and remotely. The second implication is that this study was a prelude to larger experimental studies.
Acknowledgements
References
-
1.
Fuldeore MJ, Soliman AM. Prevalence and Symptomatic Burden of Diagnosed Endometriosis in the United States: National Estimates from a Cross-Sectional Survey of 59,411 Women. Gynecol Obstet Invest. 2017;82(5):453-61. [PubMed ID: 27820938]. https://doi.org/10.1159/000452660.
-
2.
Olsarova K, Mishra GD. Early life factors for endometriosis: a systematic review. Hum Reprod Update. 2020;26(3):412-22. [PubMed ID: 32141508]. https://doi.org/10.1093/humupd/dmaa002.
-
3.
Zakhari A, Edwards D, Ryu M, Matelski JJ, Bougie O, Murji A. Dienogest and the Risk of Endometriosis Recurrence Following Surgery: A Systematic Review and Meta-analysis. J Minim Invasive Gynecol. 2020;27(7):1503-10. [PubMed ID: 32428571]. https://doi.org/10.1016/j.jmig.2020.05.007.
-
4.
Mendes N, Figueiredo B. [Psychological approach to endometriosis: women's pain experience and quality of life improvement]. Psychol Health Dis. 2012;13(1):36-48. Portuguese. https://doi.org/10.15309/12psd130104.
-
5.
Keckstein J, Becker CM, Canis M, Feki A, Grimbizis GF; Working Group of ESGE, ESHRE and WES, et al. Recommendations for the surgical treatment of endometriosis Part 2: deep endometriosis daggerdouble dagger paragraph sign. Facts Views Vis Obgyn. 2020;11(4):269-97. [PubMed ID: 32322824]. [PubMed Central ID: PMC7162667].
-
6.
Ashrafi M, Sadatmahalleh SJ, Akhoond MR, Talebi M. Evaluation of Risk Factors Associated with Endometriosis in Infertile Women. Int J Fertil Steril. 2016;10(1):11-21. [PubMed ID: 27123195]. [PubMed Central ID: PMC4845520]. https://doi.org/10.22074/ijfs.2016.4763.
-
7.
Nnoaham KE, Hummelshoj L, Webster P, d'Hooghe T, de Cicco Nardone F, de Cicco Nardone C, et al. Reprint of: Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril. 2019;112(4 Suppl1):e137-52. [PubMed ID: 31623725]. https://doi.org/10.1016/j.fertnstert.2019.08.082.
-
8.
Ezzat L. Medical treatment of endometriosis: An update. Int J Reprod Contracept Obstet Gynecol. 2017;6(10):4187-92. https://doi.org/10.18203/2320-1770.ijrcog20174193.
-
9.
Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976-82. [PubMed ID: 32694387]. [PubMed Central ID: PMC7680716]. https://doi.org/10.1097/j.pain.0000000000001939.
-
10.
Fawole AO, Bello FA, Ogunbode O, Odukogbe AT, Nkwocha GC, Nnoaham KE, et al. Endometriosis and associated symptoms among Nigerian women. Int J Gynaecol Obstet. 2015;130(2):190-4. [PubMed ID: 25935474]. https://doi.org/10.1016/j.ijgo.2015.02.030.
-
11.
McPeak AE, Allaire C, Williams C, Albert A, Lisonkova S, Yong PJ. Pain Catastrophizing and Pain Health-Related Quality-of-Life in Endometriosis. Clin J Pain. 2018;34(4):349-56. [PubMed ID: 28731958]. https://doi.org/10.1097/AJP.0000000000000539.
-
12.
Evans SF, Brooks TA, Esterman AJ, Hull ML, Rolan PE. The comorbidities of dysmenorrhea: a clinical survey comparing symptom profile in women with and without endometriosis. J Pain Res. 2018;11:3181-94. [PubMed ID: 30588070]. [PubMed Central ID: PMC6300370]. https://doi.org/10.2147/JPR.S179409.
-
13.
Orr NL, Noga H, Williams C, Allaire C, Bedaiwy MA, Lisonkova S, et al. Deep Dyspareunia in Endometriosis: Role of the Bladder and Pelvic Floor. J Sex Med. 2018;15(8):1158-66. [PubMed ID: 30078464]. https://doi.org/10.1016/j.jsxm.2018.06.007.
-
14.
Kor E, Mostafavi SRS, Mazhin ZA, Dadkhah A, Kor A, Arvanagh SH, et al. Relationship between the severity of endometriosis symptoms (dyspareunia, dysmenorrhea and chronic pelvic pain) and the spread of the disease on ultrasound. BMC Res Notes. 2020;13(1):546. [PubMed ID: 33239095]. [PubMed Central ID: PMC7687799]. https://doi.org/10.1186/s13104-020-05388-5.
-
15.
Sieberg CB, Lunde CE, Borsook D. Endometriosis and pain in the adolescent- striking early to limit suffering: A narrative review. Neurosci Biobehav Rev. 2020;108:866-76. [PubMed ID: 31862211]. [PubMed Central ID: PMC7175958]. https://doi.org/10.1016/j.neubiorev.2019.12.004.
-
16.
Zarbo C, Brugnera A, Frigerio L, Malandrino C, Rabboni M, Bondi E, et al. Behavioral, cognitive, and emotional coping strategies of women with endometriosis: a critical narrative review. Arch Womens Ment Health. 2018;21(1):1-13. [PubMed ID: 28932912]. https://doi.org/10.1007/s00737-017-0779-9.
-
17.
Goncalves AV, Barros NF, Bahamondes L. The Practice of Hatha Yoga for the Treatment of Pain Associated with Endometriosis. J Altern Complement Med. 2017;23(1):45-52. [PubMed ID: 27869485]. https://doi.org/10.1089/acm.2015.0343.
-
18.
Meissner K, Bohling B, Schweizer-Arau A. Long-term effects of traditional Chinese medicine and hypnotherapy in patients with severe endometriosis: A retrospective evaluation. Forsch Komplementmed. 2010;17(6):314-20. [PubMed ID: 21196745]. https://doi.org/10.1159/000322890.
-
19.
Van Niekerk L, Weaver-Pirie B, Matthewson M. Psychological interventions for endometriosis-related symptoms: a systematic review with narrative data synthesis. Arch Womens Ment Health. 2019;22(6):723-35. [PubMed ID: 31081520]. https://doi.org/10.1007/s00737-019-00972-6.
-
20.
Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health. 2008;31(2):180-91. [PubMed ID: 18183564]. https://doi.org/10.1002/nur.20247.
-
21.
Flynn N. Effect of an Online Hypnosis Intervention in Reducing Migraine Symptoms: A Randomized Controlled Trial. Int J Clin Exp Hypn. 2019;67(3):313-35. [PubMed ID: 31251706]. https://doi.org/10.1080/00207144.2019.1612674.
-
22.
Johnson C. Measuring Pain. Visual Analog Scale Versus Numeric Pain Scale: What is the Difference? J Chiropr Med. 2005;4(1):43-4. [PubMed ID: 19674646]. [PubMed Central ID: PMC2647033]. https://doi.org/10.1016/S0899-3467(07)60112-8.
-
23.
Bourdel N, Alves J, Pickering G, Ramilo I, Roman H, Canis M. Systematic review of endometriosis pain assessment: how to choose a scale? Hum Reprod Update. 2015;21(1):136-52. [PubMed ID: 25180023]. https://doi.org/10.1093/humupd/dmu046.
-
24.
Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S240-52. [PubMed ID: 22588748]. https://doi.org/10.1002/acr.20543.
-
25.
Rezvani AM, Siratinayer M, Abadi A, Moradyan T. Correlation between visual analogue scale and short form of McGill questionnaire in patients with chronic low back pain. Qom Univ Med Sci J. 2012;6(1):31-4.
-
26.
Tan G, Rintala DH, Jensen MP, Fukui T, Smith D, Williams W. A randomized controlled trial of hypnosis compared with biofeedback for adults with chronic low back pain. Eur J Pain. 2015;19(2):271-80. [PubMed ID: 24934738]. https://doi.org/10.1002/ejp.545.
-
27.
Rice ME, Harris GT. Comparing effect sizes in follow-up studies: ROC Area, Cohen's d, and r. Law Hum Behav. 2005;29(5):615-20. [PubMed ID: 16254746]. https://doi.org/10.1007/s10979-005-6832-7.
-
28.
Shah M, Monga A, Patel S, Shah M, Bakshi H. The effect of hypnosis on dysmenorrhea. Int J Clin Exp Hypn. 2014;62(2):164-78. [PubMed ID: 24568323]. https://doi.org/10.1080/00207144.2014.869128.
-
29.
Farshbaf Manei Sefat F, Abolghasemi A, Barahmand U, Hajloo N. [Comparing the effectiveness of cognitive behavioral therapy and hypnosis therapy pain self-efficacy and pain severity in girls with primary dysmenorrhea]. Armaghane Danesh. 2017;22(1):87-103. Persian.
-
30.
Karp BI, Sinaii N, Nieman LK, Silberstein SD, Stratton P. Migraine in women with chronic pelvic pain with and without endometriosis. Fertil Steril. 2011;95(3):895-9. [PubMed ID: 21145540]. [PubMed Central ID: PMC3415219]. https://doi.org/10.1016/j.fertnstert.2010.11.037.
-
31.
Rezaian M, Ebrahimi A, Zargham M. [Treatment based on acceptance and commitment on catastrophizing and disabling pain in women with chronic pelvic pain]. Cogn Behav Sci Res. 2013;4(2):17-30. Persian.
-
32.
Cheong YC, Smotra G, Williams AC. Non-surgical interventions for the management of chronic pelvic pain. Cochrane Database Syst Rev. 2014;(3). CD008797. [PubMed ID: 24595586]. https://doi.org/10.1002/14651858.CD008797.pub2.
-
33.
Kumalasari RD, Tamtomo DG, Prasetya H. Hypnosis and Dyspareunia: A Meta Analysis. Indones J Med. 2020;5(4):291-8. https://doi.org/10.26911/theijmed.2020.05.04.04.
-
34.
Rajaei FA, Eshghi R. [The effect of cognitive-behavioral hypnotherapy on improving anxiety and sexual performance of patients with vaginismus]. Clini Psychol. 2016;9(4):55-69. Persian. https://doi.org/10.22075/jcp.2018.11810.1164.
