Abstract
Background:
Due to the recurrent nature of type 1 bipolar disorder, evaluating the disease symptoms and a long-term follow-up of the disease after discharge is very important.Objectives:
This study evaluated the six-month follow-up of the symptoms of patients with type 1 bipolar disorder after the implementation of the home nursing care program.Methods:
This study is part of a clinical trial designed and conducted in two phases. In the first phase, an intervention was conducted to assess the effect of home nursing care on the severity of symptoms of type 1 bipolar patients, and in the second phase, the patients were followed up over 6 months. Data were collected using a demographic questionnaire and young scale and were analyzed by SPSS 24 software with repeated-measures analysis of variance, Mann-Whitney U, and Fisher’s tests at the significance level of < 0.05.Results:
The severity of symptoms was significantly decreased in the experimental group after the intervention. Until the second month of follow-up, almost the same severity scores were reported, but from the third month, an increase was observed in the severity of symptoms (P < 0.001).Conclusions:
A continuous care program for a specific period can maintain the effect of the intervention on reducing the severity of symptoms in type 1 bipolar patients. A home nursing care program is effective in reducing the severity of symptoms until four months after the intervention. This care program should be repeated every four months to maintain the effectiveness of the intervention and reduce the severity of the symptoms of the disease.Keywords
1. Background
In the latest version of the DSM5 (Fifth Edition), bipolar disorder is considered an independent disorder (1, 2), which is influenced by family history and genetics as well as seasons (3). Bipolar disorder, as a chronic illness, is also known as periodic dementia with complications, such as poor economic status, unemployment, dismissal, marital disputes, lack of continuing education, and multiple hospitalizations in psychiatric centers (4).
Bipolar disorder type I is characterized by episodes of mania with or without depression (5), so sometimes patients develop depression or periods of mania (6). Although the exact cause of these disorders has not been determined yet, possible causative factors are hereditary, time of birth, and external factors such as infection (7). Structure neuroimaging techniques suggest that parts of the brain may be involved in patients with mania (8). In this disorder, the patient suffers from individual and social dysfunction. Thus, type 1 bipolar disorder can be classified as one of the chronic mental disorders that, in addition to functional decline, can also affect interpersonal interactions and quality of life (9). It has also been shown as the sixth most debilitating mental disorder worldwide (10), with a global prevalence of 2.4% (11) and 1% in Iran (12). Therefore, bipolar disorder type 1(BID) is a common, chronic, and recurrent disease. Only 7% of all patients are asymptomatic, while 45% of patients experience more than one recurrence, and 40% experience the chronic type of the disease (13).
Due to the destructive effects of this disease on individual and social relationships and the quality of life of patients, effective treatment has been a mental concern for many years (14). Despite the effectiveness of the treatment process, which is often carried out in a controlled and precise manner during hospital stays, the lack of patient cooperation in continuing the treatment after discharge can lead to the development of symptoms and recurrence of the disorder. This, in turn, may result in the patient being referred back to the hospital, creating a vicious cycle of rehospitalization (15). In this regard, post-discharge follow-up is considered an important issue that links the coherence of inpatient and post-hospital conditions. Following the course of the disease and paying attention to the patient’s condition after discharge can improve the medical system, prevent rehospitalization of patients, and impose additional costs on the government and family (16).
Researchers believe that providing a codified follow-up program is the best method to treat patients and emphasize that, in most cases, the patient does not fully understand the importance of post-discharge training and follow-up (17, 18). Therefore, in order to reduce the complications of the disease after discharge and prevent the recurrence of the disease, it is better to train and follow the patient after discharge (19). During follow-ups, potential and actual problems of the patient can be found by the treatment and care team, which provides an opportunity to use the right method to manage the disease. However, the care and training should be repeated periodically and consistently, and it should be specified how long it should be done again (20). These follow-up programs may be considered 3 to 6 months after discharge, and sometimes they are longer (21). To effectively plan post-discharge care, it is important to establish a time frame to assess the long-term impact of the home care plan and determine if any additional care is needed (22, 23). The results of a one-year follow-up study on 31 patients with consecutive bipolar disorder showed that the severity of the patient’s symptoms improved significantly only at the time of discharge and did not markedly change after discharge (24).
In a six-month study on 13 patients with the first episode of mania, it was found that 54% of patients continued their treatment and followed medication after three months, but this rate decreased to 38% in the sixth month (25). Also, during 17 months of follow-up in patients with mania diagnosed with type 1 bipolar disorder, 40.9% of patients recurred (26). It seems that these recurrences were due to the lack of continuing the patient care program after discharge (27).
Following home nursing care will strengthen family care as well as maintain patient independence (28). On the other hand, due to the nature of psychiatric diseases and the existence of recurrent periods in this type of disorder, home nursing care can be considered a suitable solution to maintain the quality of the treatment after home care (29). Home nursing care services in the first phase of this study immediately after the intervention caused a reduction in the severity of symptoms in type 1 bipolar patients (30), but its effect in the second phase of the study, which was a 6-month follow-up, was not known to the researchers. On the other hand, the studies were conducted mostly on psychotic patients diagnosed with schizophrenia, and in limited studies, post-discharge follow-up was also conducted for mood patients. Thus, this study investigated the symptoms of patients with BID after home care in a 6-month follow-up.
2. Objectives
The objective of this study was to examine the duration of the effect of nursing home care on patients with type 1 bipolar disorder during the follow-up period.
3. Methods
3.1. Design
This study is part of a clinical trial designed and conducted in two phases, and this article presents the result of the second phase.
3.2. Participants and Setting
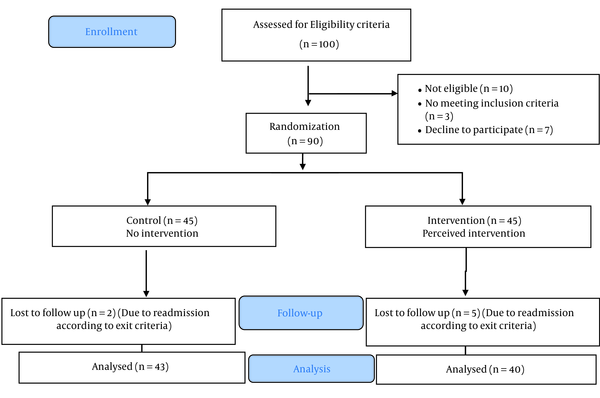
In the first phase, an intervention was conducted on 100 people who volunteered to participate in the research. However, based on the inclusion criteria, only 90 individuals were deemed eligible and were subsequently divided into two groups: The intervention group and the control group. Thus, 45 people were assigned to each group (Figure 1). After three months, the intervention, which involved receiving nursing care at home after discharge, was analyzed. The details of the intervention are described below. Following the analysis, the study entered its second phase, which involved a 6-month follow-up period to track the results of the intervention. The statistical population of this study consisted of type 1 bipolar patients at 22nd Bahman Hospital in Qazvin in 2019. The sample size was estimated at 37 people in each group, considering a similar study with an average effect size of 0.25, a type 1 error of 0.05, and a power of 0.80 (31). However, this was increased to 45 people in each group due to the possible attrition of 20%. Inclusion criteria consisted of patients with mania in a psychiatric hospital in Qazvin aged at least 18 years. Rehospitalization and participation in similar programs were considered exclusion criteria.
Consort diagram
3.3. Intervention
A total of 90 patients who were selected by the convenience sampling method were divided into two experimental and control groups by randomly assigning 15 blocks of six. In this study, in order to hide the random allocation process, the names of the groups were placed in envelopes, numbered from one to 90, and placed in a packet. For the intervention group, the package designed for nursing care was implemented at home, and for the control group, this nursing care was not performed, and the researchers did not intervene in other routine treatment programs of the hospital performed for both groups. The home nursing care program included family support and education, patient support and education, mental health assessment in patients, access to basic mental health care, and promotion of the mental health of patients. The ethical code was IR.QUMS.REC.1398.192, and the IRCT code was IRCT20190928044911N1. The participation was voluntary, and the participants could leave the study if desired. They were also assured of the confidentiality of information and the accuracy and confidentiality in recording information and data obtained at data collection.
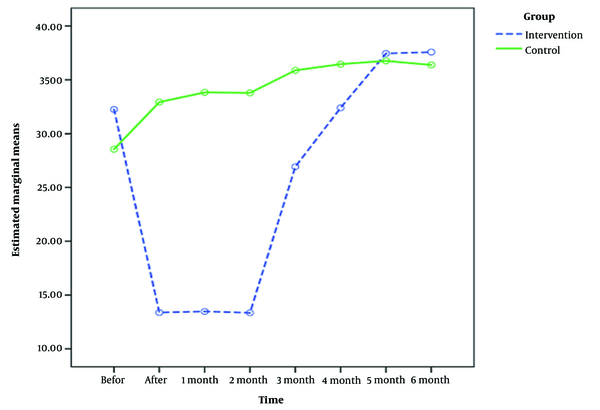
The research instruments included the Demographic Characteristics Questionnaire and the Young Mania Rating Scale (YMRS) (1978). The YMRS scores range from 0 - 60, and a score of above 20 indicates a manic phase (32). Young’s questionnaire was created by Young in 1978. It has a concurrent validity of 0.96, inter-rater reliability of 0.92, and Cronbach’s alpha of 0.72. The results showed a reliability of 0.72 for the patient group and 0.62 for the normal group, while the inter-rater reliability was 0.96. Also, the validity coefficient of total scores and group membership (focal correlation) was 0.92, and the results of the validity analysis of the questions indicated the high power of all questions in differentiating the normal group from the patient group (33). Subjects were asked to complete the questionnaires before the intervention and then after three months. The patients were subjected to the intervention (home nursing care) by making two telephone calls every 15 days and holding meetings (30 - 45 min) with the patient and his/her family. At the end of three months, the patients completed the YMRS to assess the severity of symptoms, and the control group that did not receive the intervention also completed the questionnaire (the first phase of the study). Follow-up was then performed for six months after the intervention (the second phase of the study), during which no intervention was performed. The questionnaires were completed by subjects every month, and then the result was compared with before the follow-up (Figure 2). SPSS 24 software was used to analyze the data.
The trend of disease severity in the experimental and control groups before and after the intervention
Sample size formula
F tests–ANOVA: Repeated measures between factors
Analysis: A priori: Compute required sample size
Input:Effect size f = 0.25
α err prob = 0.05
Power (1-β err prob) = 0.80
Number of groups = 2
Number of measurements = 8
Corr. among rep measures = 0.5
Output: Noncentrality parameter λ = 8.2222222
Critical F = 3.9738970
Numerator df = 1.0000000
Denominator df = 72.0000000
Total sample size = 74
Actual power = 0.807586
4. Results
The studied patients were examined for all quantitative and qualitative demographic variables, including age, sex, education, family history of mental illness, duration of illness, and the number of hospitalizations (Table 1). It was found that the two groups were homogenous regarding these factors (P < 0.05).
Homogeneity of Demographic Variables of Type 1 Bipolar Patients in Experimental and Control Groups a
| Variables and Levels | Experimental Group | Control Group | P-Value b |
|---|---|---|---|
| Gender | 0.362 | ||
| Female | 12 (30) | 17 (40) | |
| Male | 28 (70) | 25 (60) | |
| Education | 0.252 | ||
| Below diploma | 19 (47.5) | 27 (64.2) | |
| Diploma | 15 (37.5) | 9 (21.5) | |
| University | 6 (15) | 6 (14.3) | |
| Family history of mental illness | 0.176 | ||
| Yes | 15 (37.5) | 22 (52) | |
| No | 25 (62.5) | 20 (48) | |
| Quantitative variables | |||
| Age (y) | 38.75 ± 12. 91 | 41.53 ± 8.93 | 0.072 c |
| Duration of disease (mo) | 97.67 ± 99.71 | 130.62 ± 110.64 | 0.167 c |
| Number of hospitalizations | 3.22 ± 3.12 | 4.62 ± 5.62 | 0.275 c |
A comparison of the mean scores of the severity of symptoms is presented in Figure 2 and Table 2. Before the intervention, there was no difference between the two groups, but the difference was statistically significant after the intervention.
Mean Scores of Symptom Severity in Type 1 Bipolar Patients Before and After the Intervention a
| Disease Severity | Experimental Group | Control Group | Significance Level (Independent t-Test) |
|---|---|---|---|
| Before intervention | 32. 25 ± 9.93 | 28. 54 ± 10.97 | 0.113 |
| After intervention | 13. 38 ± 5.16 | 32.9 ± 12.81 | < 0.001 |
| One month after the intervention | 13. 47 ± 4.92 | 33.83 ± 14.49 | < 0.001 |
| Two months after the intervention | 13. 35 ± 5.05 | 33.78 ± 14.48 | < 0.001 |
| Three months after the intervention | 26. 92 ± 9.92 | 35.88 ± 12.73 | 0.001 |
| Four months after the intervention | 32.4 ± 11.56 | 36.45 ± 12.59 | 0.134 |
| Five months after the intervention | 37.45 ± 10.65 | 36.76 ± 12.44 | 0.789 |
| Six months after the intervention | 37.57 ± 10.70 | 36.38 ± 12.58 | 0.646 |
| Result of repeated-measures ANOVA | F = 80.89, P < 0.001 | F = 12.43, P < 0.001 |
Also, one, two, and three months after the intervention, the mean score of symptom severity was 13.47 ± 4.92, 13.35 ± 5.05, and 26.92 ± 9.92 in the experimental group and 33.83 ± 14.49, 33.78 ± 14.48, and 35.88 ± 12.73 in the control group, respectively. The difference between the two groups was statistically significant. In all three follow-ups, the mean score of symptom severity was lower in the experimental group than in the control group (P < 0.05).
Also, 4 months after the intervention, the mean score of disease severity was 32.4 ± 11.56 in the experimental group and 36.45 ± 12.59 in the control group. The experimental group had a lower mean score, but this difference was not statistically significant between the two groups (P < 0.05). At five and six months of follow-up, the mean score of symptom severity was slightly higher in the experimental group than in the control group (P < 0.05).
Also, the results of repeated-measures ANOVA showed a significant decrease in the severity of symptoms after the intervention. Until the second month of follow-up, almost the same mean severity scores were reported, but after the third month of follow-up, an increase was observed in the severity of symptoms, which was statistically significant (P < 0.001). However, in the control group, in general, there was an increasing trend in the severity of symptoms, which was statistically significant (P < 0.001).
Tables 3 and 4 indicate the overall effect of time and group using repeated-measures ANOVA. The results showed that the effect of time, the interaction of time and group, and the effect of all three factors (time, interaction of time, and group) were found to be significant based on the significant value, test statistics, and partial eta squared. Therefore, the intervention had a significant effect (P < 0.001) on reducing the severity of symptoms. Also, the difference in the mean score of symptom severity in the follow-up showed a significant effect (Tables 3 and 4).
Intragroup Effect (Time) of Type 1 Bipolar Patients Using Repeated-measures Analysis of Variance
| Source | Mean Square | F | P-Value | Partial Eta Squared | Observed Power |
|---|---|---|---|---|---|
| Time effect | 2919.64 | 70.50 | 0.00 | 0.46 | 0.99 |
| Group *time effect | 2202.55 | 53.18 | 0.00 | 0.39 | 0.99 |
Intergroup Effect (Group) of Type 1 Bipolar Patients Using Repeated-measures Analysis of Variance
| Source | Mean Square | F | P-Value | Partial Eta Squared | Observed Power |
|---|---|---|---|---|---|
| Intercept | 593425.31 | 840.39 | 0.00 | 0.91 | 0.99 |
| Group effect | 11762.47 | 16.65 | 0.00 | 0.17 | 0.98 |
5. Discussion
Bipolar disorder is a reversible disease, and most patients experience recurrences throughout their lives if they do not receive proper treatment and follow-up. Each recurrence, in addition to unpleasant effects on the mental state of the patient and those living with them, also has a negative effect on the course of the disease. Also, the acute phase of the disease and its relapse impose high costs directly and indirectly on the family and society (34).
Navidian et al., in their clinical trial on the effect of family education on the psychological burden of home caregivers of mentally ill patients, showed that the mean psychological burden of caregivers of schizophrenic patients who received group training intervention was significantly reduced compared with the control group. As a result, the quality of life of mentally ill caregivers increased significantly (35). Hubbard et al. conducted a study in which short-term psychological interventions were considered for caregivers of patients with bipolar disorder. According to their results, the training group, compared with the control group, showed a reduction in the psychological burden of caregivers and an increase in their knowledge about bipolar disorder and caregiver self-efficacy. These changes persisted at follow-up and after one month and then increased (36).
In a study to investigate the impact of critical time intervention on reducing psychiatric rehospitalization following hospital discharge, Tomita and Herman showed that at the end of the follow-up period, psychiatric rehospitalization was significantly lower in the group assigned to critical time intervention compared with the usual services group (37). Lee et al. showed that rehospitalization in patients was decreased (38). Pan et al., in their study on the effect of the frequency of three-year follow-up after discharge on treatment costs in discharged patients with bipolar disorder, showed that patients subjected to 13 - 17 postoperative visits paid the lowest costs for mental health services and health care (39). Roos et al. assessed the use of mental health services in patients with severe mental disorders in the first 12 months after discharge from a psychiatric hospital and showed that post-discharge mental health services reduced patients’ total use of medical services and costs without an increase in hospitalization rate (40).
Li et al. examined the recurrence and improvement of social functioning in discharged psychiatric patients with bipolar disorder. They found a significant difference in the recurrence of the disease after a follow-up in the first year after discharge and the first two years after discharge (41). Khaleghparast et al. showed that the discharge program can be effective in improving knowledge and reducing rehospitalization of patients with schizophrenia (42). The results of the mentioned studies are all consistent with the present study, indicating that follow-up after discharge in psychiatric patients reduces the recurrence of the disease and reduces the number of hospitalizations and costs.
In contrast, Amini et al. conducted a study assessing a follow-up of patients with mania. They showed that the severity of symptoms in patients with bipolar disorder decreased significantly during hospitalization; however, it did not change significantly during one year of follow-up (43). To explain this finding, it can be said that a follow-up of the patient after discharge can significantly reduce the number of hospitalizations. Sometimes, the patient does not understand the importance of post-discharge education. Thus, to reduce the complications of the disease in the post-discharge period, it is better to follow and train the patient seriously after discharge. During follow-up, the patient’s health problems can be detected by the care team, providing an opportunity to apply the correct method of patient management.
5.1. Limitation
The limitations of the study included the non-cooperation of patients and their families, possibly due to the nature of psychiatric disorders. In this regard, the possible benefits of the research, including the reduction of rehospitalization and, as a result, the reduction of costs, were explained to them.
5.2. Conclusions
The results of this study showed that a post-discharge care program for up to four months reduces the severity of symptoms in type 1 bipolar patients. Also, due to the special conditions of bipolar type 1 patients and the recurrent nature of the disease, repeating the home nursing care program at an appropriate time can help reduce the severity of symptoms in these patients, which cannot be achieved without repetition as well as follow-up. The periodic repetition of this care program at intervals of four months will maintain the improvements and reduce the severity of symptoms in these patients. Accordingly, the patient can return to the community faster and gain previous functioning, and finally, the number of hospitalizations is reduced. It is suggested that future research should investigate the impact of nursing care at home on the severity of symptoms of other psychiatric disorders, as well as on the recurrence rate of BID and the rate of patient rehospitalization.
Acknowledgements
References
-
1.
Hayes JF, Marston L, Walters K, Geddes JR, King M, Osborn DP. Adverse renal, endocrine, hepatic, and metabolic events during maintenance mood stabilizer treatment for bipolar disorder: A population-based cohort study. PLoS Med. 2016;13(8). e1002058. [PubMed ID: 27483368]. [PubMed Central ID: PMC4970809]. https://doi.org/10.1371/journal.pmed.1002058.
-
2.
Kocsis RN. Book review: diagnostic and statistical manual of mental disorders: (DSM-5). Los Angeles, CA: Sage Publications Sage CA; 2013.
-
3.
Rosenthal SJ, Josephs T, Kovtun O, McCarty R. Seasonal effects on bipolar disorder: A closer look. Neuroscience Biobehav Rev. 2020;115:199-219.
-
4.
Diniz BS, Teixeira AL, Cao F, Gildengers A, Soares JC, Butters MA, et al. History of Bipolar Disorder and the Risk of Dementia: A Systematic Review and Meta-Analysis. Am J Geriatr Psychiatry. 2017;25(4):357-62. [PubMed ID: 28161155]. [PubMed Central ID: PMC5365367]. https://doi.org/10.1016/j.jagp.2016.11.014.
-
5.
Phillips ML, Kupfer DJ. Bipolar disorder diagnosis: Challenges and future directions. Lancet. 2013;381(9878):1663-71. [PubMed ID: 23663952]. [PubMed Central ID: PMC5858935]. https://doi.org/10.1016/S0140-6736(13)60989-7.
-
6.
Rolin D, Whelan J, Montano CB. Is it depression or is it bipolar depression? J Am Assoc Nurse Pract. 2020;32(10):703-13. [PubMed ID: 33017361]. https://doi.org/10.1097/JXX.0000000000000499.
-
7.
Rowland TA, Marwaha S. Epidemiology and risk factors for bipolar disorder. Ther Adv Psychopharmacol. 2018;8(9):251-69. [PubMed ID: 30181867]. [PubMed Central ID: PMC6116765]. https://doi.org/10.1177/2045125318769235.
-
8.
Kosger F, Essizoglu A, Baltacioglu M, Ulkgun N, Yenilmez C. Executive function in parents of patients with familial versus sporadic bipolar disorder. Compr Psychiatry. 2015;61:36-41. [PubMed ID: 26072266]. https://doi.org/10.1016/j.comppsych.2015.05.013.
-
9.
Bennett F, Hodgetts S, Close A, Frye M, Grunze H, Keck P, et al. Predictors of psychosocial outcome of bipolar disorder: Data from the stanley Foundation Bipolar Network. Int J Bipolar Disord. 2019;7(1):28. [PubMed ID: 31840207]. [PubMed Central ID: PMC6911815]. https://doi.org/10.1186/s40345-019-0169-5.
-
10.
Bull A. Screening for bipolar disorder in primary care. The J Nurse Practitioners. 2010;6(1):65-6. https://doi.org/10.1016/j.nurpra.2009.09.018.
-
11.
Dell'Aglio JJ, Basso LA, Argimon ,I, Arteche A. Systematic review of the prevalence of bipolar disorder and bipolar spectrum disorders in population-based studies. Trends Psychiatry Psychother. 2013;35(2):99-105. [PubMed ID: 25923299]. https://doi.org/10.1590/s2237-60892013000200002.
-
12.
Ghanbari Jolfaei A, Ghadamgahi P, Ahmadzad-Asl M, Shabani A. Comparison of demographic and diagnostic characteristics of iranian inpatients with bipolar I disorder to western counterparts. Iran J Psychiatry Behav Sci. 2015;9(2). e839. [PubMed ID: 26288646]. [PubMed Central ID: PMC4539587]. https://doi.org/10.17795/ijpbs839.
-
13.
Vejdani-aram S, Fardmal J, Roshanaei G, Najafi-Vosough R, Mahjub H, Ghaleiha A. [Identifying the factors influencing the recurrence time of bipolar I disorder using frailty model]. J Mazandaran Univ Med Sci. 2017;27(148):56-67. Persian.
-
14.
Studart PM, Bezerra Filho S, Studart ABD, Almeida AG, Miranda-Scippa Â. Social support and bipolar disorder. Archives of Clinical Psychiatry (São Paulo). 2015;42(4):95-9. https://doi.org/10.1590/0101-60830000000057.
-
15.
Anderson C, Quante A. Acute interventions and referral of patients with bipolar disorder by the psychiatric consultation liaison service in a general hospital in germany: A retrospective analysis. Prim Care Companion CNS Disord. 2014;16(2). [PubMed ID: 25133062]. [PubMed Central ID: PMC4116291]. https://doi.org/10.4088/PCC.13m01602.
-
16.
Lee KK, Yang J, Hernandez AF, Steimle AE, Go AS. Post-discharge follow-up characteristics associated with 30-day readmission after heart failure hospitalization. Med Care. 2016;54(4):365-72. [PubMed ID: 26978568]. [PubMed Central ID: PMC4800825]. https://doi.org/10.1097/MLR.0000000000000492.
-
17.
Kripalani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing hospital readmission rates: Current strategies and future directions. Annu Rev Med. 2014;65:471-85. [PubMed ID: 24160939]. [PubMed Central ID: PMC4104507]. https://doi.org/10.1146/annurev-med-022613-090415.
-
18.
Zheng MC, Zhang JE, Qin HY, Fang YJ, Wu XJ. Telephone follow-up for patients returning home with colostomies: Views and experiences of patients and enterostomal nurses. Eur J Oncol Nurs. 2013;17(2):184-9. [PubMed ID: 22748946]. https://doi.org/10.1016/j.ejon.2012.05.006.
-
19.
Jayakody A, Bryant J, Carey M, Hobden B, Dodd N, Sanson-Fisher R. Effectiveness of interventions utilising telephone follow up in reducing hospital readmission within 30 days for individuals with chronic disease: A systematic review. BMC Health Serv Res. 2016;16(1):403. [PubMed ID: 27538884]. [PubMed Central ID: PMC4990979]. https://doi.org/10.1186/s12913-016-1650-9.
-
20.
Darcy AM, Murphy GA, DeSanto-Madeya S. Evaluation of discharge telephone calls following total joint replacement surgery. Orthop Nurs. 2014;33(4):188-95: quiz 196-7. [PubMed ID: 25058721]. https://doi.org/10.1097/NOR.0000000000000062.
-
21.
Liebmann EP, Richter KP, Scheuermann T, Faseru B. Effects of post-discharge counseling and medication utilization on short and long-term smoking cessation among hospitalized patients. Prev Med Rep. 2019;15:100937. [PubMed ID: 31338281]. [PubMed Central ID: PMC6630019]. https://doi.org/10.1016/j.pmedr.2019.100937.
-
22.
Newnham H, Barker A, Ritchie E, Hitchcock K, Gibbs H, Holton S. Discharge communication practices and healthcare provider and patient preferences, satisfaction and comprehension: A systematic review. Int J Qual Health Care. 2017;29(6):752-68. [PubMed ID: 29025093]. https://doi.org/10.1093/intqhc/mzx121.
-
23.
Costantino ME, Frey B, Hall B, Painter P. The influence of a postdischarge intervention on reducing hospital readmissions in a Medicare population. Popul Health Manag. 2013;16(5):310-6. [PubMed ID: 23537154]. [PubMed Central ID: PMC3771544]. https://doi.org/10.1089/pop.2012.0084.
-
24.
Amini H, Alimadadi Z, Nejatisafa A, Sharifi V, Ahmadi-Abhari SA. [Quality of life in a group of patients with bipolar disorder and some of their clinical characteristics. Iranian journal of psychiatry and clinical psychology]. Iran J Psychiatry Clinical Psychol. 2009;15(2):175-82. Persian.
-
25.
Harrow M, Goldberg JF, Grossman LS, Meltzer HY. Outcome in manic disorders. A naturalistic follow-up study. Arch Gen Psychiatry. 1990;47(7):665-71. [PubMed ID: 2113802]. https://doi.org/10.1001/archpsyc.1990.01810190065009.
-
26.
Shaabani A, Eftekhar M, Danesh Amouz B, Khaniha H, Hakim Shoushtari M, Ghaleh Band M, et al. Degree of recurrence of type i bipolar disorder: A 17 month follow-up of patients with first-episode mania. Advances in Cognitive Science. 2006;8(3):33-42.
-
27.
Clarke JL, Bourn S, Skoufalos A, Beck EH, Castillo DJ. An innovative approach to health care delivery for patients with chronic conditions. Popul Health Manag. 2017;20(1):23-30. [PubMed ID: 27563751]. [PubMed Central ID: PMC5278805]. https://doi.org/10.1089/pop.2016.0076.
-
28.
Huang XY, Lin MJ, Yang TC, Hsu YS. The functions of hospital-based home care for people with severe mental illness in Taiwan. J Clin Nurs. 2010;19(3-4):368-79. [PubMed ID: 20500276]. https://doi.org/10.1111/j.1365-2702.2009.03052.x.
-
29.
Keeling D. Homecare user needs from the perspective of the patient and carers: A review. Smart Homecare Technology and TeleHealth. 2014. https://doi.org/10.2147/shtt.S42673.
-
30.
Zeighami R, Raeisolhagh A, Ranjbaran M. Effect of home nursing care on the severity of symptoms in patients with bipolar I disorder: A randomized clinical trial. Home Health Care Management & Practice. 2020;33(2):81-7. https://doi.org/10.1177/1084822320969122.
-
31.
Ghoshchian Chobmasjedi S, Makvan Hosseini S, Najafi M, Bigdeli I. Comparing effectiveness of complementary family and individual psycho-education on depression and maniac episodes of the bipolar disordered patients under medical therapy. Clinical Psychology Studies. 2017;7(27):179-201.
-
32.
Hashemian P, Sedaghati ME. Evaluation of Family Dysfunction in Patients with Schizophrenia and Bipolar I Disorder. J Biosciences Med. 2016;4(2):1-5. https://doi.org/10.4236/jbm.2016.42001.
-
33.
Mohammadi Z, Pourshahbaz A, Poshtmashhadi M, Dolatshahi B, Barati F, Zarei M. Psychometric properties of the young mania rating scale as a mania severity measure in patients with bipolar I disorder. Practice in Clinical Psychology. 2018;6(3):175-82.
-
34.
Cakir S, Ozerdem A. [Psychotherapeutic and psychosocial approaches in bipolar disorder: A systematic literature review]. Turk Psikiyatri Derg. 2010;21(2):143-54. [PubMed ID: 20514565].
-
35.
Navidian A, Pahlavanzadeh S, Yazdani M. The effectiveness of family training on family caregivers of inpatients with mental disorders. Iran J Psychiatry Clinical Psychol. 2010;16(2):99-106.
-
36.
Hubbard AA, McEvoy PM, Smith L, Kane RT. Brief group psychoeducation for caregivers of individuals with bipolar disorder: A randomized controlled trial. J Affect Disord. 2016;200:31-6. [PubMed ID: 27116364]. https://doi.org/10.1016/j.jad.2016.04.013.
-
37.
Tomita A, Herman DB. The impact of critical time intervention in reducing psychiatric rehospitalization after hospital discharge. Psychiatr Serv. 2012;63(9):935-7. [PubMed ID: 22810163]. [PubMed Central ID: PMC3989527]. https://doi.org/10.1176/appi.ps.201100468.
-
38.
Lee SY, Kim KH, Kim T, Kim SM, Kim JW, Han C, et al. Outpatient Follow-Up Visit after Hospital Discharge Lowers Risk of Rehospitalization in Patients with Schizophrenia: A Nationwide Population-Based Study. Psychiatry Investig. 2015;12(4):425-33. [PubMed ID: 26508952]. [PubMed Central ID: PMC4620298]. https://doi.org/10.4306/pi.2015.12.4.425.
-
39.
Pan YJ, Kuo KH, Chan HY, Yeh LL. Cost-effectiveness and cost-utility analysis of outpatient follow-up frequency in relation to three-year mortality in discharged patients with bipolar disorder. Psychiatry Res. 2019;272:61-8. [PubMed ID: 30579183]. https://doi.org/10.1016/j.psychres.2018.12.067.
-
40.
Roos E, Bjerkeset O, Steinsbekk A. Health care utilization and cost after discharge from a mental health hospital; an RCT comparing community residential aftercare and treatment as usual. BMC Psychiatry. 2018;18(1):363. [PubMed ID: 30419894]. [PubMed Central ID: PMC6233284]. https://doi.org/10.1186/s12888-018-1941-2.
-
41.
Li C, Chen C, Qiu B, Yang G. A 2-year follow-up study of discharged psychiatric patients with bipolar disorder. Psychiatry Res. 2014;218(1-2):75-8. [PubMed ID: 24794029]. https://doi.org/10.1016/j.psychres.2014.04.029.
-
42.
Khaleghparast S, Ghanbari B, Kahani S, Malakouti K, SeyedAlinaghi S, Sudhinaraset M. The effectiveness of discharge planning on the knowledge, clinical symptoms and hospitalisation frequency of persons with schizophrenia: A longitudinal study in two hospitals in Tehran, Iran. J Clin Nurs. 2014;23(15-16):2215-21. [PubMed ID: 24329909]. https://doi.org/10.1111/jocn.12499.
-
43.
Amini H, Sharifi V, Nejatisafa A, Arbabi M, Tabatabaie M, Alimadadi Z, et al. [One year follow-up of patients with bipolar disorder admitted to Roozbeh Hospital]. Iran J Psychiatry Clinical Psychol. 2009;15(2):168-74. Persian.