Abstract
Background:
Positive communication between staff and parents is considered a basic principle for the successful implementation of family-centered care (FCC) and the formation of a good relationship between parents and neonates. Moreover, involvement in care depends on the communication and interaction of parents with healthcare providers, and cooperation between them leads to high-quality care for neonates. However, interaction and communication are still considered major challenges in the neonatal intensive care unit (NICU) environment. Since these challenges and communication barriers are different in various cultures and environments, they should be identified in the field. A literature review shows that no study has assessed the views of different members of the treatment team and parents on communication barriers in Iran.Objectives:
The present study aimed to investigate the communication barriers related to personnel and parents for implementing FCC from the perspective of parents, physicians, nurses, and nursing managers.Methods:
A qualitative study was conducted in 2021 - 2022 using the conventional content analysis approach in a NICU in Tehran, Iran. In this study, 26 semi-structured interviews and 10 field notes were used to collect data to reach data saturation.Results:
Data analysis led to the emergence of two themes. The first theme was the unprofessional relationships of personnel, including two main categories of inappropriate professional behavior and lack of attention to personnel and working conditions of the ward. The second theme was mutually ineffective relationships between personnel and parents, including two main categories of the inappropriate attitude of personnel and parents toward each other and unsympathetic communication between personnel and parents. The themes showed the participants’ experiences of communication barriers to the implementation of FCC in NICUs in Iran.Conclusions:
Removing communication barriers between healthcare providers and parents requires developing a coherent, comprehensive, and unified training program to prepare and create integrated coordination among the treatment team and the family, creating a positive attitude toward FCC and the presence of parents, improving relationships, and giving further attention and support by managers to personnel and the conditions of the ward.Keywords
Family-Centered Care Communication Relationship Obstacle Barrier Parents Neonatal Intensive Care Unit Qualitative Study
1. Background
Every year, about 12.5 million neonates are born with low weight, and about 9.6% of neonates in developing countries are born prematurely and need hospitalization in the neonatal intensive care unit (NICU) (1). Today, the NICU environment reflects advances in technology and the medical treatment of premature and sick infants. These advances have led to the reduction of morbidity and mortality of neonates in recent decades (2, 3). Many neonates spend several weeks in the NICU while they grow and develop; this is a devastating life event for parents that greatly affects the family’s health. In this period, parents must assume new and unknown roles under adverse conditions, such as physical separation from the infant and restrictions on visits due to the severity of the infant’s or mother’s illness. In addition, they have fear for their child’s present and future life and suffer guilt, along with feeling hope, love, and happiness. Therefore, these parents need more support from the personnel of the neonatal ward (3, 4).
Family-centered care (FCC) is a way to support and involve parents in caring for their neonates. Family-centered care is a paradigm, care model, philosophy, or theory that is emphasized as an important factor in improving care outcomes in the NICU (2, 5), and the basic components that distinguish FCC from traditional care include dignity and respect, communication, information sharing, participation, and family cooperation in care. The purpose of the FCC is that families should be included in the planning, implementation, and evaluation of care, and their opinions should be important as the opinions of healthcare professionals (2, 4). Research in the neonatal field has shown various beneficial effects of FCC for both infants and parents, including reduced length of hospital stay for NICU infants, improved neurobehavioral outcomes in preterm infants, faster infant growth, infant preference for breastfeeding when discharged, and less stress and more satisfaction in parents (2). The American Academy of Pediatrics (AAP) defines FCC as an approach to policies of programs, facility design, healthcare management, and daily interactions among patients, families, physicians, nurses, and other members of the healthcare team. The core of this care includes honest and transparent communication between parents and members of the healthcare team (6). For the formation of a good partnership between parents and healthcare professionals, it is important to pay attention to communication because insufficient communication might lead to role stress, disruption of conversation, feeling of insecurity, and stress for both parents and professionals (2).
Communication is a multidimensional, complex, and dynamic process. Many have defined it as the exchange of information, feelings, and thoughts between individuals. Using effective therapeutic communication skills is a valuable tool for assessing patients’ needs and providing appropriate physical care and emotional support for them (7). The purpose of communication in the NICU is not limited to providing information to parents about their infant’s clinical condition; healthcare providers must educate and guide parents to act proactively and participate in their infant’s care and decision-making process. Healthcare personnel should use communication skills to find and control parents’ worries and feelings and support them in critical situations (6). The AAP recommends three key factors for good communication, namely: (1) the quality and quantity of provided information; (2) the interpersonal dimension (i.e., active listening and genuine interest in parents’ feelings and concerns); and (3) the link between professionals and parents and children. In the neonatal ward, the communication between the doctor and patient is not linear. An important part of communication is directed at parents, and the relationship between specialists, infants, and parents is known as the “infant triangle” (3). A lack of effective communication is considered a potentially important barrier to providing standard services in care settings and can lead to anxiety, misunderstanding, misdiagnosis, possible abuse, exposure to complications, increased length of hospital stay, and waste of resources (7). If effective communication is not provided, the implementation of the FCC will face serious challenges (6).
There are many barriers that can hinder these communications in the NICU, including the infant’s medical conditions, parents’ emotional conditions and differences in spoken language, lack of privacy, mothers’ lack of health literacy and poor education level, NICU environment conditions, and parents’ interactions with different healthcare providers that cause misunderstandings, misinterpretation, and more conflict, and working and emotional conditions of medical and nursing personnel, such as heavy workload, lack of time, lack of support, fatigue, conflict of employees, and lack of skills to deal with mothers’ nervous reactions (6, 7). A lack of communication skills in sensitive situations also increases the stress of the personnel and causes job burnout (8). Identifying the factors that hinder effective communication is the first step to solving problems related to the communication process for FCC implementation. These barriers are different in different environments, and as a result, they should be identified in context (6). A review of the literature shows that there are few studies on the investigation of communication barriers between personnel and families in the NICU in Iran, and there has been no study that assessed the views of different members of the treatment team and parents in this field.
2. Objectives
The present study aimed to investigate communication barriers related to personnel and parents for implementing FCC from the perspective of doctors, nurses, nursing managers, and parents.
3. Methods
3.1. Study Design and Participants
Conventional qualitative content analysis was used to understand the opinions of the caregivers and parents in the NICU about the barriers to implementing FCC. Qualitative research helps achieve in-depth data analysis and provides a cultural and contextual description and interpretation of social phenomena that cannot be obtained using the quantitative research tradition (9). Moreover, content analysis as a research method is used to interpret the content of textual data through the regular classification process of coding and identifying subcategories and categories by immersing in the data to gain new insight (10). The inclusion criteria included individuals who would participate and could express their opinions and experiences. The study objective was to obtain optimal information with the help of targeted sampling and a maximum diversity of the sample by characteristics, such as work history, education, job position, and positive and negative attitudes toward implementing FCC. Furthermore, various levels of personnel and parents of infants admitted to the NICU of Imam Khomeini Hospital Complex in Tehran, Iran, were invited to the study. Due to the restrictions of the ward during the coronavirus disease 2019 pandemic, fathers’ participation in the study was not possible. A total of 26 participants, including 1 head nurse, 1 matron, 2 supervisors, 3 medical professors, 14 nurses, and 5 mothers of neonates in the NICU, took part in this study.
3.2. Data Collection
A total of 26 semi-structured interviews and 10 field notes were used in 2021 - 2022. The interviews were conducted individually in a private room at a predetermined time, and each session depended on the willingness and tolerance of the participants (average duration: 34 minutes). The interviews began with open-ended questions about expressing experiences of how to communicate in the implementation of FCC. Then, the interviewees were asked to talk more deeply about related problems and issues by asking probing and in-depth questions, such as “Please explain more what does this mean and why?”.
3.3. Data Analysis
Data analysis was performed using the method of Lindgren et al. (11). The recorded interviews were transcribed verbatim after each interview, and then the entire text was read repeatedly until reaching a general understanding of the participants’ statements. Afterward, specific meaning units and corresponding codes were assigned. Through constant comparison of similarities and differences between codes, they were classified and grouped into categories and subcategories. As a thread to connect them, the main theme of the study was developed. The samples were collected simultaneously with data analysis until data saturation and obtaining no new information.
3.4. Rigor and Trustworthiness
According to Lincoln and Guba’s criteria, the criteria of transferability, credibility, dependability, and confirmability were used to increase accuracy (12). To provide rigor, efforts were made to spend enough time collecting data and analyzing and validating the data in periodic meetings with the research team and considering the maximum diversity of the sample. The transcripts were given to data participants for verification and correction, and a brief description of the findings was provided to half of the participants to confirm whether their views and experiences were reflected. Additionally, the findings were reviewed by other researchers familiar with qualitative research inside and outside the research team, and their opinions were taken into account during the analysis.
3.5. Ethical Considerations
This study was extracted from part of the nursing Ph.D. thesis of the first author and was approved by the Ethics Committee of Tarbiat Modares University, Tehran, Iran (IR.MODARES.REC.1398.020). At the beginning of the interviews, the participants were adequately given explanations about the research purpose, work, interview methods, confidentiality of information, audio recording, the right to participate or withdraw from the study, and informed consent.
4. Results
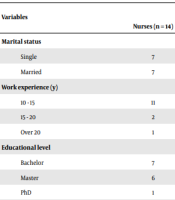
A total of 26 subjects participated in the present study. Table 1 shows the demographic characteristics of the study subjects. Data analysis resulted in the emergence of 2 themes (i.e., unprofessional relationships of personnel and mutually ineffective relationships between personnel and parents), 4 main categories, 14 subcategories, and 261 primary codes, which showed the barriers related to communication between personnel and parents for the implementation of FCC in the study environment (Table 2).
Demographic Information of Personnel and Mothers
| Variables | Participating Personnel | Participating Mothers (n = 5) | ||
|---|---|---|---|---|
| Nurses (n = 14) | Nursing Managers (n = 4) | Doctors (n = 3) | ||
| Marital status | ||||
| Single | 7 | 1 | ||
| Married | 7 | 3 | 3 | |
| Work experience (y) | ||||
| 10 - 15 | 11 | 2 | 1 | |
| 15 - 20 | 2 | |||
| Over 20 | 1 | 2 | 2 | |
| Educational level | ||||
| Bachelor | 7 | 2 | 1 | |
| Master | 6 | 2 | ||
| PhD | 1 | |||
| Neonatal specialist | 3 | |||
| Diploma | 3 | |||
| Under diploma | 1 | |||
| Neonate’s duration of hospitalization (day) | ||||
| 10 - 15 | 3 | |||
| 15 - 30 | 2 | |||
| Gestational age (week) | ||||
| Under 28 | 1 | |||
| 28 - 32 | 4 | |||
Results of Qualitative Data Analysis
| Themes | Categories | Subcategories |
|---|---|---|
| Unprofessional relationships among personnel | Inappropriate professional behavior | Derogatory behavior of doctors |
| Accusing the head nurse | ||
| Unfriendly interpersonal relationships between nurses | ||
| Lack of attention to personnel and working conditions of the ward | Inadequate support of personnel | |
| Neglect of providing appropriate human resources | ||
| Lack of attention to the conditions of the ward | ||
| Mutually ineffective relationships between personnel and parents | The inappropriate attitude of personnel and parents toward each other | The uselessness of parents’ presence |
| Loss of each other’s privacy | ||
| Evasion of responsibility for care | ||
| Disruption of personnel’s work process | ||
| Unsympathetic communication between personnel and parents | Judgment of personnel | |
| Misplaced sensitivities and expectations | ||
| Cultural and linguistic differences | ||
| Informing parents |
4.1. Theme 1. Unprofessional Relationships of Personnel
This theme focuses on inappropriate professional behavior and lack of attention to personnel and the working conditions of the ward.
4.1.1. Inappropriate Professional Behavior
From the point of view of nurses, the communication problems of implementing FCC and the unprofessional behavior of the personnel toward each other have caused a lack of a friendly atmosphere in the ward, and this is considered a barrier to the effective communication of the personnel with the parents and their participation in FCC. This category includes three subcategories: derogatory behavior of doctors, accusing the head nurse, and unfriendly interpersonal relationships between nurses.
4.1.1.1. Derogatory Behavior of Doctors
From the point of view of nurses, the humiliating behavior of the doctors as humiliation, impertinence, and superiority of some medical professors near the parents caused the parents to take advantage of this situation and take an inappropriate approach to treat those personnel, which led to discomfort of the personnel. One nurse said:
“Some doctors are disrespectful to the nurses; the way you saw Dr. X talking in front of the companion, telling me everything the nurse does. This has caused mothers to mistrust and treat nurses badly.” (Nurse No. 8)
4.1.1.2. Accusing the Head Nurse
From the point of view of nurses, the head nurse does not treat the staff appropriately in front of the parents, or she checks how they are doing their work through the parents. If there is a problem or tension with the parents, she calls the tired staff after the work shift and blames and accuses them. This unprofessional behavior of the head nurse has caused the staff to be upset, oppose parents’ presence in the ward, and cause an ineffective relationship with parents. In this regard, one of the nurses said:
“I do not accept the behavior of the head nurse. Sometimes, she came into the crowd among all these people and families and behaved so insultingly that I could not raise my head; I cried for an hour; it was not about anything special; it was on shift schedule; we are also human beings; we all have privacy; we have personality; we have families; we are educated. This behavior should be corrected.” (Nurse No. 8)
4.1.1.3. Unfriendly Interpersonal Relationship Between Nurses
Some personnel have unhealthy competition with their colleagues and try to destroy and eliminate each other out of jealousy. These unfriendly relationships among nurses have damaged the coordination and teamwork of personnel and doctors to implement FCC, involving parents in care and working as a team with them. In this regard, the education supervisor said:
“Experience has shown that in wards where there is a more friendly atmosphere, personnel work easily, they accept the difficulty of work better, they are better personnel, and parents feel comfortable there. One of our problems in the NICU is that there is no friendly atmosphere. Many personnel habituate to this environment, and they are working in this atmosphere; they do not even notice that their behavior can bring people tension.” (Education supervisor)
4.1.2. Lack of Attention to Personnel and Working Conditions of the Ward
From the point of view of nurses, hospital and nursing managers pay little attention to the working conditions of NICU personnel, facilitating FCC implementation conditions, supporting and motivating, selecting individuals, and having training programs and regulations. This category includes three subcategories: inadequate support of personnel, neglect of providing appropriate human resources, and lack of attention to the conditions of the ward.
4.1.2.1. Inadequate Support of Personnel
From the point of view of nurses, the insufficient encouragement of personnel, lack of motivation to implement FCC by managers, lack of support by nursing managers for personnel when there is tension between them and parents, and favoring parents and not establishing peace between them by the head nurse cause discouragement of personnel to implement FCC and establish effective communication with parents. One of the nurses stated:
“When I have a problem with a family, neither the head nurse supports nor the nursing department; I think the manager should support both sides; a manager should manage in all ways and not destroy one side; then, I cannot communicate with that family, you see X (head nurse) argues in front of the family, questions me. I say that you, as the head of the ward, should not just listen to their words, you should say yes, you are right, and she is also one of my good personnel. Families should know that we are not their slaves; it is our job, and they treat us rudely. X (head nurse) also defended.” (Nurse No. 8).
4.1.2.2. Neglect to Providing Appropriate Human Resources
The lack of nurses who agree with the implementation of FCC and the lack of hiring other specialists required for the implementation of FCC, such as social workers, psychologists, or psychiatrists, to remove the fear and anxiety of parents and staff to improve the effective communication between them are considered barriers of this type. In this regard, the education supervisor said:
“Maybe many of the nurses who work in the NICU are not very suitable for that ward in terms of personality, ethics, and communication. It is true that we do not select, and many personnel were placed in the ward by mistake; maybe if we had such an option, maybe there would be a limited number of personnel who are against FCC. If staff would go there that agree with FCC, they would help the continuity of care rather than trying to be a barrier to care with their opposition. Unfortunately, we have very few choices.” (Education supervisor)
In this regard, a nurse said:
“There is a time when the ward is so busy, with few nurses; you do not have time to do routine work; even if you want to spend time talking with the family, it is necessary for a fixed nurse to be in charge of training. For example, there have been so many misbehaving parents that no one wants to be their infant nurse. If we had a psychologist in the ward, he/she would treat the mothers’ psychological problems. If a nurse has a problem, she is nervous and aggressive, and psychologists should find the root of the problem so that the problem can be solved and the mother and the staff can reach to interact.” (Nurse No. 1)
4.1.2.3. Lack of Attention to the Conditions of the Ward
From the point of view of nurses, managers paid little attention to developing a codified program for the introduction of personnel, notification of specific duties of personnel and parents in FCC, how to implement FCC and their participation in neonate care in the ward, and codified regulations on sending out or allowing parents to be present in the ward during procedures, hand over, and visits, which has led to tension between parents and staff. One of the nurses stated:
“We should have regulations regarding FCC, and the nurses should be justified; it should not be like that when the head nurse is present, the nurse should do it in the morning shift; then in the evening or night shifts, the nurse says no, I will not let the mother come to the ward, I am doing gavage for example, or I do not want the mother to do kangaroo mother care (KMC) at night. It happened that there was a fight and reached X ears (the head nurse) at her house, and she said why did you say go out or, for example, you said to go out in a bad tone. If there are no written laws and regulations, it will be treated according to taste.” (Nurse No. 1)
In this regard, a nurse said:
“Our problem is that we do not have a familiarization protocol. When the family enters the ward, we should tell them who the nurse is, what their role is, who the resident, fellow, and head nurse are, or for example, if the neonate is NPO or nothing per mouth under a ventilator, parents think we inject empty water, but they do not know we inject total parental nutrition, protein, and fat; otherwise, the neonate loses weight and cannot bear it; this is very important to explain. When the father sees what my role is, he respects me, and he does not insult me, and mutually if I understand what the parent’s role is, I will not tell the mother to get out.” (Nurse No. 6)
4.2. Theme 2. Mutually Ineffective Relationships Between Personnel and Parents
This theme focuses on the inappropriate attitude of personnel and parents toward each other and unsympathetic communication between personnel and parents.
4.2.1. Inappropriate Attitude of Personnel and Parents Toward Each Other
This category is formed from the subcategories of the uselessness of parents’ presence, loss of each other’s privacy, evasion of responsibility for care, and disruption of personnel’s work process.
4.2.1.1. Uselessness of Parents’ Presence
Some personnel do not have a proper attitude toward the implementation of FCC and the presence of parents of sick neonates in the ward. They do not have the desire to communicate with parents and avoid being face-to-face and answering or giving them information. In this regard, a nurse said:
“In a ward where there are sicker children, it is not necessary for parents to come so much inside for a child who is NPO, a child who does not want to be touched and changed diapers; what would parents want to do for a child who is intubated and falls oxygen saturation by changing the position? If the mother does KMC, the child gets infected with pneumothorax. We also cannot perform KMC in neonates with a urinary catheter. Family-centered care has no advantage here; in my opinion, the only way is to limit the presence of parents, similar to many other hospitals.” (Nurse No. 2)
4.2.1.2. Loss of Each Other’s Privacy
Being tormented arising from being heard by the private discussions and conversations of the personnel and being under surveillance while doing work have caused a violation of privacy and problems in accepting the presence and work with parents, especially fathers, in the ward environment. In this field, a nurse said:
“We do not have privacy. Fathers do not look at the children; they look at the nurses; Iranian fathers only listen to our words; they look at us; we do not have this culture, and we will not have it a hundred years later.” (Nurse No. 8)
4.2.1.3. Evasion of Responsibility for Care
Some parents do not have a proper attitude about being entrusted the responsibility of the infant’s care to parents by nurses and consider it as the nurses’ refusal to do the work; therefore, they treat personnel demanding. One of the nursing managers stated:
“One of the conflicts and tensions we have in the NICU is that some mothers do not like to be entrusted with the care of the neonate, and they consider it a failure of the staff and protest against it.” (Clinical supervisor)
One of the mothers said:
“There are several nurses here who would entrust their own work to mothers; for example, changing a diaper is easy, they say, change it so learn; if I take my child home, I will not be alone; there are many people who help me. How do some nurses say nothing and change diapers themselves?” (Mother No. 4)
4.2.1.4. Disruption of Personnel’s Work Process
Most of the nurses believe that the presence of parents, asking frequent questions and disrupting the staff’s concentration by parents, especially when the ward is busy performing emergency procedures, interfering in the treatment and even other hospitalized neonates, and choosing the nurse to take care of their neonate disturb the work of the staff, and these annoying behaviors prevent effective communication between staff and parents. In this case, one nurse said:
“There has been a case of a golden neonate, and parents say that some should not be their neonate’s nurse. They choose who works well and who works badly. Well, this is how the work burden falls on the shoulders of a series of nurses; then, they (mothers) go to the room and talk, and they choose who is the best nurse or when the nurse wants to insert an intravenous line, the mother says “Can Mrs. X come and insert it?” No nurse will accept this kind of interference and disrespect. If I were, I would be upset.” (Nurse No. 1)
4.2.2. Unsympathetic Communication Between Personnel and Parents
This category includes the subcategories of judgment of personnel, misplaced sensitivities and expectations, cultural and linguistic differences, and informing parents.
4.2.2.1. Judgment of Personnel
Not receiving the necessary explanations about the condition of the neonate by nurses and doctors or the use of medical terminology has caused misunderstanding and judgment of the personnel by some parents. One of the nurses said:
“It happened that the neonate could not tolerate milk for several shifts, and the physician reduced his/her milk. The mother thought that I gave the neonate less milk. She came and asked why did you give too little milk? If personnel had explained it to her before, she would not have accused me this way, or it happened that, for example, the neonate’s blood culture became positive; the mother said nurse X did not wash her hands, and my child is infected; this makes me unwilling to communicate with that mother anymore.” (Nurse No. 1)
4.2.2.2. Misplaced Sensitivities and Expectations
Most of the nurses believe that one reason for the ineffective communication between parents and staff, which hinders the proper interaction and participation of parents in FCC, is the obsessive sensitivities of some parents and the expectations of perception of nurses by parents regarding their anger and fatigue due to their excessive work. A nurse said:
“Mothers are very sensitive to the neonate’s milk and whether it is received on time. They are even satisfied with not taking antibiotics; how many times occurred I said antibiotics are more important, let me prepare the antibiotics first, you do not eat at home on time. It does not happen if the neonate receives milk later, but 99% of mothers would like to be given it on time, and they have challenges with nurses about this.” (Nurse No. 7)
One nurse said:
“Some colleagues have a series of expectations; for example, they turn their back and expect the mother will come to say hello. Well, first, I have to show a happy face and give her a smile; then, for example, she will say, who is the neonate’s nurse today? Then, we interact with each other, but when I see the mother coming, I sit behind the station so that I do not face her at all if she wants to ask me a question. So, how are we going to implement FCC in such a situation?” (Nurse No. 6)
4.2.2.3. Cultural and Linguistic Differences
The referral of parents from different cities with different cultures, beliefs, spoken languages, and levels of education to this large referral center of the country is considered a barrier to effective communication and participation in the neonate’s care.
In this regard, a nurse said:
“Many times, our challenge with the family has been due to the cultural and linguistic differences that they want to do everything in their own culture. A worried mother once came to the station and asked a question in Turkish. None of us understood what the mother was saying, and we told her we did not understand what she was saying. Without saying a word, the mother left with a desperate expression.” (Nurse No. 2)
4.2.2.4. Informing Parents
From the point of view of nurses, parents feel close to each other by being in the ward for a long time and, due to that, interfere in the treatment of other neonates or give false information, which leads to worry and confusion. In this study, the head nurse said:
“Our main problem is that the parents who are present in the ward sit and listen to the visit or handover of another child; they understand incompletely; they convey this incomplete information to the parents who are not present, and it becomes a problem; these scared and agitated parents come or call. Parents may not trust the nurse but rely on the words of other parents who do not have much information.” (Head nurse)
5. Discussion
The findings of the present study showed that one of the first and most significant barriers to implementing FCC is the communication barrier between the doctors, the head nurse, and the nurses in the ward. Moreover, the participants acknowledged that the successful implementation of FCC depends on effective communication between staff with each other, parents/staff, and parents with each other. In line with the findings of the inappropriate professional behavior category, in Hadian Shirazi et al.’s study, nurses attributed the most important communication barriers in the NICU to organizational factors, including weak communication between nurses and between nurses and doctors (6). In Mirlashari et al.’s study, most nurses described the communication challenge of nurses with nursing managers and conflict with doctors, especially doctors who did not support FCC, as daily work stress (13). Additionally, they were concerned about the hierarchical relationship and power inequality between Iranian nurses and doctors. Doctors feel dominated and empowered in relation to nurses, and the source of these conflicts is the traditional patriarchal models of care, the lack of familiarity of doctors with the roles and profession of nurses, and the lack of communication skills training for nurses and doctors in Iran (13).
Poor communication between nurses and doctors is also observed in foreign studies. In a study by Radwan and Mohamed to investigate the communication barriers between nurses and mothers, about half of the participants considered the poor communication between nurses and doctors as a communication barrier (7). Therefore, in order to remove the communication barriers between staff and parents, first of all, nurses and doctors should establish a friendly and compatible relationship with each other, especially in front of parents, and a suitable atmosphere and paradigm shift should take place in order to do teamwork in the ward.
According to the experience of the participants in the present study, related to the category of lack of attention to personnel and working conditions of the ward, the lack of attention of the managers to motivating, supporting, and facilitating the conditions of the ward, protocols, and regulations, hiring and choosing the appropriate personnel for the implementation of FCC, and the fatigue and boredom of the personnel due to the high workload are factors that prevent effective communication between staff and parents. In line with the aforementioned finding, in a study by Hadian Shirazi et al., other important communication barriers were authoritarian management, lack of support by managers, lack of income as a lack of motivational factor, and an inefficient system for selecting staff, training communication skills, and evaluating them (6). In a study by Mirlashari et al., the key factors of effective FCC implementation have been mentioned as teaching knowledge and communication skills, and healthcare policies (14). In other words, doctors and nurses found the biggest challenge to be the lack of leadership in the field of FCC and in-service training, organizational infrastructure, and clear policies. They reported that due to the lack of knowledge and communication skills, medical personnel did not have a proper understanding of the parents’ conditions (14).
On the other hand, as the technology in the NICU improved, the workload of nurses increased, and they faced challenges to support and understand the needs of parents (1). In Hadian Shirazi et al.’s study, communication barriers related to nurses in the NICU include psychological, physical, social, and cultural factors, such as fatigue, long shifts, heavy workload, and lack of time (6). Barriers related to this category are also observed in foreign studies. Hall et al. reported in a study that many nurses and neonatologists do not feel that they have enough skills to support and communicate with anxious and disturbed parents (8), and sometimes although nurses think they have the competence in communication skills, patients do not think so (6). Therefore, there is always a need to teach the aforementioned skill. In Radwan and Mohamed’s study, 100% of participants considered the workload, lack of nurses, fatigue, and the crowded environment of the ward as communication barriers (7). The guidance published in 2017 emphasizes the publication of policies and documentation of information for parents. One of the studies that examined the FCC’s approach stated that the lack of protocols and documentation of providing information was the most important shortfall for families in intensive care. Moreover, 68.7% of nurses stated that the intensive care unit did not have a protocol for FCC, and 38% stated that there was no documentation for providing information to parents (15).
In Carvalho et al.’s study, parents found the most important facilitators of communication to be providing full information about NICU rules and clinical issues, clarifying doubts, reducing uncertainty, active listening, managing parents’ expectations, empathic attitude, and psychological and emotional support (3). Therefore, in order to remove communication barriers between staff and parents, managers should pay attention to encouraging staff and facilitating the implementation of FCC with the help of the necessary program and regulations regarding FCC issues, the presence of parents and communication training with them, using the necessary and efficient personnel of the ward, and trying to reduce the workload of personnel, such as appointing a mentor or training a nurse and psychologist.
Based on the shared experiences of the participants in this study, another communication barrier for the optimal implementation of FCC is the inappropriate attitude of personnel and parents toward each other, which is caused by the attitude of personnel toward the ineffectiveness of FCC and the presence of parents, the inappropriate attitude of parents toward personnel and entrusting the care of the neonate to them, disturbing each other’s privacy, and disruption of the work process of the personnel. In line with the existing findings, studies in this regard have shown that the first step in the implementation of FCC is to change the attitude, behavior, and understanding of individuals. Some of the misunderstandings and lack of understanding of parents and personnel are caused by different attitudes toward health and unfair treatment (6, 14, 16). Today, although FCC has been approved at the policy level of developed countries, in these countries, there is also concern about why FCC has not been successfully implemented, and it is not uncommon to hear that families find their relationships with healthcare providers difficult and intimidating (15).
In Williams et al.’s study, mothers consider the time of meeting and performing skin-to-skin care as dependent on how the staff communicates with them (17). In a study by Radwan and Mohamed, the negative attitude and misperception of the nurse about communication and lack of attention to the mother’s privacy are mentioned as barriers to communication between them (7). It has also been reported in Iranian and foreign studies that medical staff is concerned about parental interference and monitoring routine procedures. Moreover, some parental behaviors, such as checking ward issues and nurses’ skills, manipulation of equipment, and untimely and frequent questions, especially during unstable and busy times, have caused challenges and conflicts with the medical staff (16, 18, 19). Other communication barriers have been raised in only Iranian studies. The issues of lack of communication and inappropriate behavior of NICU personnel toward fathers, lack of social and emotional support of fathers, and preventing the presence and participation of fathers in FCC by female personnel have been due to the influence of the dominant religious and cultural background of Iranians on the limitation of communication (6, 14, 20). In order to solve this group of barriers, it is suggested that managers hold training workshops to create a positive attitude of staff and parents toward FCC and parents’ participation and develop basic communication skills with parents, especially fathers of neonates hospitalized in the ward, according to the opinions of the staff in the ward.
In the current study, the participants have experienced unsympathetic communication between personnel and parents for the optimal implementation of FCC in the form of judgment of personnel, misplaced sensitivities and expectations, cultural and linguistic differences, and informing parents. The evidence in this regard shows that positive communication between parents and personnel is considered a basic principle for a successful FCC. In addition, although the formation of a good relationship between parents and neonates and involvement in caring for their neonates depends on the communication and interaction of parents with healthcare providers and their cooperation leads to the quality care of newborns, interaction, and communication are still considered major challenges in the NICU environment. Since this issue is different in different cultures and environments, it must be identified in the context (6, 20). Success in the communication process does not only depend on the communication skills of the message sender; the receiver’s ability and willingness to listen, conditions, and various reasons are also involved (3). Therefore, some communication challenges and barriers are related to parents, their sensitivities, and conditions. Not accepting the condition of the neonate and not being able to change it, not responding to treatment, blaming the nurses for the bad condition and not managing the difficult condition of the neonate, long-term hospitalization of the neonate, various reactions toward the ward, and anger are some of these conditions (6, 7, 19).
Hassankhani et al. stated in a study that some of the tensions between parents and nurses are due to conflicting expectations, unclear roles, and a lack of trust (21). They stated that some mothers, especially those who are under high stress, are sensitive to the smallest movements of neonates; if nothing abnormal is found after the nurse’s examination, the nurses consider them anxious and do not trust them (21). In Radwan and Mohamed’s study, some communication barriers were attributed to the lack of education and health literacy, the use of technical words, and the mother’s reluctance to communicate (7). In Hadian Shirazi et al.’s study, they also pointed out communication barriers related to parents, such as parents’ different and unknown cultures and their low social and economic levels (6). In Mirlashari et al.’s study, it was also stated that educating families with a low level of literacy is one of the main challenges, and personnel have to spend much time answering their frequent questions (16).
Another similar concern in this study is informing parents about each other in the ward, which has caused interference in the issues of other neonates and created tension for the personnel and interaction with them. Although it was a common experience among the participants of the present study, no study was found in this field, and the reason can be attributed to the difference in culture and the prevailing atmosphere attributed to different environments. According to the experiences obtained in this category of barriers, it is suggested to the wards’ heads who might experience such barriers created by parents that the personnel gain the trust of parents upon admission and in different conditions and provide the necessary explanations to parents through a unique training program about the rules and culture of the ward. The duties of parents and equipment should be considered, and all personnel should follow these rules uniformly to prevent misinterpretation, judgment, discrimination, additional sensitivities, and protests and problems caused by them.
5.1. Conclusions
Based on the findings of the present study, communication barriers between personnel and parents caused unfavorable conditions in the NICU, which has challenged the successful implementation of FCC. In order to remove these barriers in similar environments, it is suggested that a coherent, comprehensive, and unified training program be developed and implemented to prepare and create integrated coordination between the treatment team and the family to create a positive attitude toward the presence of parents and the implementation of FCC. Additionally, managers should give further attention and support to personnel and ward conditions.
Acknowledgements
References
-
1.
Ladani MT, Abdeyazdan Z, Sadeghnia A, Hajiheidari M, Hasanzadeh A. Comparison of Nurses and Parents' Viewpoints Regarding the Needs of Parents of Premature Infants in Neonatal Intensive Care Units. Iran J Nurs Midwifery Res. 2017;22(5):367-71. [PubMed ID: 29033991]. [PubMed Central ID: PMC5637145]. https://doi.org/10.4103/1735-9066.215672.
-
2.
Oude Maatman SM, Bohlin K, Lillieskold S, Garberg HT, Uitewaal-Poslawky I, Kars MC, et al. Factors Influencing Implementation of Family-Centered Care in a Neonatal Intensive Care Unit. Front Pediatr. 2020;8:222. [PubMed ID: 32435628]. [PubMed Central ID: PMC7219204]. https://doi.org/10.3389/fped.2020.00222.
-
3.
Carvalho C, Vale A, Magalhães S. Communication and Decision Making in Neonatal Intensive Care: Why Narrative Medicine Matters. In: Pope E, Brandão C, Rosario A, Costa AP, editors. Qualitative Research: practices and challenges. Aveiro, Portugal: Ludomedia; 2020. p. 104-21. https://doi.org/10.36367/ntqr.1.2020.104-121.
-
4.
Reid S, Bredemeyer S, Chiarella M. Integrative Review of Parents' Perspectives of the Nursing Role in Neonatal Family-Centered Care. J Obstet Gynecol Neonatal Nurs. 2019;48(4):408-17. [PubMed ID: 31150595]. https://doi.org/10.1016/j.jogn.2019.05.001.
-
5.
Maureen MM, Mwape L, Maimbolwa M, Chirwa E. Family - professional partnership a core principle of family centered care in the neonatal intensive care unit: Review of literature. J Res Nurs Midwifery. 2018;7(1):24-9.
-
6.
Hadian Shirazi Z, Sharif F, Rakhshan M, Pishva N, Jahanpour F. The Obstacles against Nurse-Family Communication in Family-Centered Care in Neonatal Intensive Care Unit: a Qualitative Study. J Caring Sci. 2015;4(3):207-16. [PubMed ID: 26464837]. [PubMed Central ID: PMC4591613]. https://doi.org/10.15171/jcs.2015.021.
-
7.
Radwan RIM, Mohamed HE. Perceived Barriers to Effective Therapeutic Communication between Pediatric Nurses and Mothers of Hospitalized Children at Alexandria University Children Hospital. Am J Nurs Res. 2019;7(5):802-10. https://doi.org/10.12691/ajnr-7-5-13.
-
8.
Hall SL, Famuyide ME, Saxton SN, Moore TA, Mosher S, Sorrells K, et al. Improving Staff Knowledge and Attitudes Toward Providing Psychosocial Support to NICU Parents Through an Online Education Course. Adv Neonatal Care. 2019;19(6):490-9. [PubMed ID: 31306236]. [PubMed Central ID: PMC6882527]. https://doi.org/10.1097/ANC.0000000000000649.
-
9.
Holloway I, Galvin K. Qualitative research in nursing and healthcare. 4th ed. Hoboken, USA: John Wiley & Sons; 2016.
-
10.
Beiranvand S, Kermanshahi SMK, Memarian R. Nursing instructors' perception of clinical education competencies: a qualitative study. Preprint. Research Square. Posted online January 7, 2021. https://doi.org/10.21203/rs.3.rs-118299/v1.
-
11.
Lindgren BM, Lundman B, Graneheim UH. Abstraction and interpretation during the qualitative content analysis process. Int J Nurs Stud. 2020;108:103632. [PubMed ID: 32505813]. https://doi.org/10.1016/j.ijnurstu.2020.103632.
-
12.
Alexander AP. Lincoln and Guba’s quality criteria for trustworthiness. IDC International Journal. 2019;6(4):1-6.
-
13.
Mirlashari J, Brown H, Fomani FK, de Salaberry J, Zadeh TK, Khoshkhou F. The Challenges of Implementing Family-Centered Care in NICU from the Perspectives of Physicians and Nurses. J Pediatr Nurs. 2020;50:e91-8. [PubMed ID: 31300252]. https://doi.org/10.1016/j.pedn.2019.06.013.
-
14.
Mirlashari J, Nikbakht Nasrabadi A, Holsti L, Ghorbani F, Hosseini MB, Fadaei Z. Caring for the Bereaved Parents in the NICU: Fathers-The Missing Piece of the Puzzle. J Perinat Neonatal Nurs. 2022;36(4):E31-9. [PubMed ID: 36288448]. https://doi.org/10.1097/JPN.0000000000000641.
-
15.
Bozkurt G, Duzkaya DS, Oren B. Opinions of intensive care nurses about family-centered care in Turkey. Int J Caring Sci. 2021;14(1):45.
-
16.
Mirlashari J, Valizadeh S, Navab E, Craig JW, Ghorbani F. Dark and Bright-Two Sides of Family-Centered Care in the NICU: A Qualitative Study. Clin Nurs Res. 2019;28(7):869-85. [PubMed ID: 29457482]. https://doi.org/10.1177/1054773818758171.
-
17.
Williams KG, Patel KT, Stausmire JM, Bridges C, Mathis MW, Barkin JL. The Neonatal Intensive Care Unit: Environmental Stressors and Supports. Int J Environ Res Public Health. 2018;15(1). [PubMed ID: 29301343]. [PubMed Central ID: PMC5800159]. https://doi.org/10.3390/ijerph15010060.
-
18.
Yue J, Liu J, Williams S, Zhang B, Zhao Y, Zhang Q, et al. Barriers and facilitators of kangaroo mother care adoption in five Chinese hospitals: a qualitative study. BMC Public Health. 2020;20(1):1234. [PubMed ID: 32791972]. [PubMed Central ID: PMC7427278]. https://doi.org/10.1186/s12889-020-09337-6.
-
19.
Friedman J, Friedman SH, Collin M, Martin RJ. Staff perceptions of challenging parent-staff interactions and beneficial strategies in the Neonatal Intensive Care Unit. Acta Paediatr. 2018;107(1):33-9. [PubMed ID: 28833515]. https://doi.org/10.1111/apa.14025.
-
20.
Ghorbani F, Mirlashari J, Navab E, Higman W, Valizadeh S. Experiences of the Iranian neonatal intensive care unit nurses in implementing family-centered care: walking on an insecure foundation. Iran J Neonatol. 2018;9(2):42-9.
-
21.
Hassankhani H, Negarandeh R, Abbaszadeh M, Craig JW, Jabraeili M. Mutual trust in infant care: the nurses and mothers experiences. Scand J Caring Sci. 2020;34(3):604-12. [PubMed ID: 31657062]. https://doi.org/10.1111/scs.12758.