Abstract
Background:
The aspartate aminotransferase to platelet ratio index (APRI) is a non-invasive method used to investigate liver fibrosis in patients with hepatitis C virus (HCV).Objectives:
This study aimed to determine the APRI before and after the treatment of HCV patients with sofosbuvir/daclatasvir (Sovodak) in the city of Rafsanjan, southeast Iran.Methods:
This study was conducted on 45 patients with HCV from March 2021 to March 2022 in Rafsanjan. Demographic information, including age, gender, a history of human immunodeficiency virus (HIV) infection, and intravenous (IV) drug injection, was collected. Polymerase chain reaction (PCR) was performed after treatment with Sovodak to calculate sustained virological response (SVR). Also, the APRI was calculated before and after treatment.Results:
Among 45 HCV patients (97.8% = male, 2.2% = female, age range = 26 to 59 years), the administration of Sovodak to all patients resulted in an efficacy of 100% in the assessment of SRV in 12 weeks (SVR12). Also, the APRI level decreased significantly after treatment with Sovodak (0.35 vs. 0.68, P-value: 0.000), even in HCV patients with a history of HIV (0.77 vs. 1.47, P-value: 0.028) or HCV patients with a history of injecting drugs in the last 12 months (0.38 vs. 0.66, P-value: 0.000).Conclusions:
The present study indicated that the APRI level in HCV patients decreased significantly after treatment with Sovodak, regardless of having a history of HIV infection or a history of drug injection. Therefore, Sovodak in HCV patients can reduce the odds of liver fibrosis and subsequent hepatocellular carcinoma (HCC) by reducing the APRI level.Keywords
Hepatitis C Aspartate Aminotransferase to Platelet Ratio Index Direct-acting Antiviral Combination Therapy Sofosbuvir/Daclatasvir Iran
1. Background
In 2019, about 58 million people worldwide were infected with the hepatitis C virus (HCV). Approximately 290,000 deaths from this virus occurred, mainly due to liver cancer and cirrhosis (1) In Iran, the prevalence of HCV is less than 0.5% in the general population, 16.6% in individuals with thalassemia, 54% in individuals with hemophilia, 8.3% in individuals undergoing dialysis, and 51.4% in injecting drug addicts (2, 3).
The lack of effective prophylaxis and vaccination methods against HCV has stopped the eradication and reduction of cases worldwide (4). Therefore, effective drugs are necessary to destroy the virus. They also reduce the level of viremia significantly and achieve an acceptable sustained virological response in 12 or 24 weeks (SVR12 or SVR24) after the completion of antiviral treatment (5).
Direct-acting antivirals (DAAs) are molecules that target specific non-structural proteins of the virus and prevent its multiplication and infection (6). Chronic infection can be treated with antiviral drugs, such as sofosbuvir or simeprevir, in more than 95% of cases (4). Peginterferon and ribavirin were previous-generation treatments that had less than 50% recovery rate and caused more side effects (7). The medicinal combination of sofosbuvir as a polymerase inhibitor and daclatasvir as a non-structural protein 5A (NS5A) inhibitor is one of the DAA compounds approved by the European Association for the Study of the Liver (EASL) in 2014 for the treatment of all HCV genotypes and by the Food and Drug Administration (FDA) and Infectious Diseases Society of America (IDSA) in 2015 and 2016 for the treatment of genotypes 1, 2, and 3. In clinical studies, SVR12 of this treatment has been 98% for genotype 1, 92% for genotype 2, and 89% for genotype 3 (8). The combination of sofosbuvir and daclatasvir in one tablet is available in Iran (commercial name: Sovodak). It can be used without checking the genotype because it is effective on all genotypes (9).
Among non-invasive methods, the aspartate aminotransferase to platelet ratio index (APRI) is a very simple and low-cost method available to all healthcare centers to evaluate fibrosis and cirrhosis in HCV patients (10). The APRI is used in patients with HCV, human immunodeficiency virus (HIV), and alcoholic liver disease, with 77% sensitivity and 72% specificity to diagnose advanced fibrosis and 76% sensitivity and 72% specificity to predict cirrhosis (10). Zhang, et al.’s study showed a significant relationship between the increased APRI and the increased risk of hepatocellular carcinoma (HCC) in patients with chronic hepatitis C, indicating that the APRI can be a valuable predictor for the risk of HCC in patients with chronic hepatitis C (11).
2. Objectives
Despite previous studies on the effect of Sovodak on SVR, the studies evaluating the reduction of liver fibrosis levels by receiving this drug are limited. The present study aimed to investigate the effect of Sovodak on liver fibrosis levels using the APRI as an alternative method to liver biopsy or fibroscan.
3. Methods
In this interventional study, conducted from March 2021 to March 2022, all HCV patients were referred to a hepatitis clinic located in the central healthcare setting of Rafsanjan, southeast Iran. The patients were selected by census method.
As part of a hepatitis C eradication plan, this study was implemented in 2017 by the Ministry of Health on all high-risk individuals living in Rafsanjan. The components of this project were screening, treatment, and education. The inclusion criteria for the study included all HCV polymerase chain reaction (PCR)+ subjects who received the Sovodak regimen, and their information was recorded in the comprehensive system of hepatitis C patients. This study was approved by the Ethics Committee of Rafsanjan University of Medical Sciences (IR.RUMS.REC.1400.158). The informed consent was completed by the patients. Based on on-site tests, blood samples were collected from all individuals suspected of having HCV infection, including all prisoners, individuals who lived in de-addiction camps, and individuals who lived in hangouts or went to these places to use drugs. Then, the HCV antibody (Ab) test was performed for rapid testing, and if the test was positive, the person was referred to the hepatitis clinic, which is run by primary care clinicians. Blood samples were taken from all subjects, and after the definite diagnosis of hepatitis C using HCV RNA, the other patient's laboratory data were collected. The viral infection was checked by PCR using the MIC device (real-time thermal cycler Mic, Australia), hematology was tested using the NIHON KODEN (MEK-651 OK, Japan), and liver enzymes were measured by a biotechnical analyzer (BT 1500, Italy) at the Central Laboratory in the Cohort Center (12). The other collected data included age, gender, a history of HIV infection, and a history of IV drug injection in the last 12 months.
Also, the patient's APRI was calculated using aspartate aminotransferase (AST) and platelets using the following formula.
APRI= [(AST/upper limit of the normal AST range) × 100]/Platelet Count
All the mentioned data were recorded in the Comprehensive Hepatitis Eradication System (WWW.STOP-HEPATITIS.COM).
Then, one Sovodak tablet (sofosbuvir [400 mg] + daclatasvir [60 mg] made in Rojan Pharma, Tehran, Iran) was prescribed daily for all patients. A decision was made regarding the length of the treatment period based on the APRI level before treatment so that individuals with APRI <1 were treated for 12 weeks, and those with APRI >1 were treated for 24 weeks. Then, 12 weeks after the treatment, HCV PCR was performed again in order to evaluate the response to the treatment and achieve SVR. In order to check the reduction of the level of liver fibrosis and subsequent HCC, the APRI was simultaneously calculated, and its changes were evaluated compared to the value before the treatment.
3.1. Statistical Analysis
Data were analyzed by STATA statistical software version 14. The findings of qualitative variables were expressed as frequency and percentage, and quantitative variables were expressed as mean and standard deviation. The Kolmogorov-Smirnov statistical test and the kurtosis and skewness indices were used to check the normality of the data. According to the results of the Kolmogorov-Smirnov test and the kurtosis and skewness indices, the data did not have a normal distribution, so the non-parametric Wilcoxon signed-rank test was used to evaluate the APRI score before and after treatment. Also, in order to compare the APRI before and after treatment, the categories of APRI (<1 and >1) were used through the Mcnemar test. The significance level of the tests was considered to be less than 0.05.
4. Results
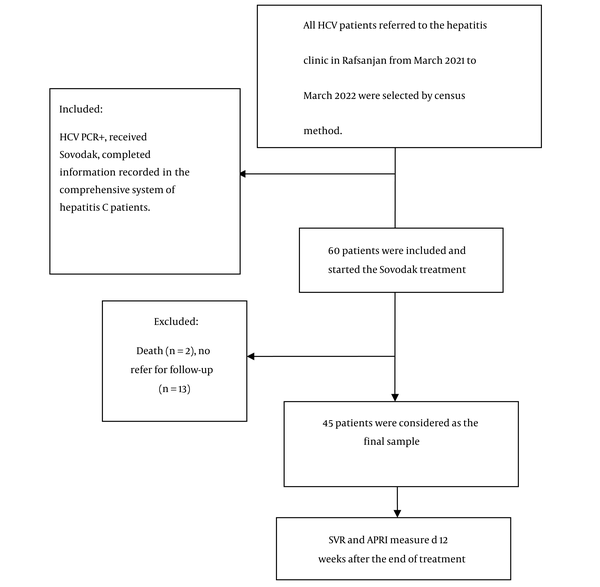
As presented in Figure 1, based on the inclusion criteria, 60 patients (55 men and 5 women) were entered into the study. All 60 patients received the treatment, but 2 people died during the study, and 13 people who did not refer to the hepatitis clinic for follow-up were excluded from the study. Finally, data analysis was performed on 45 patients.
Flow chart of the study design of Aspartate aminotransferase to platelet ratio index (APRI) before and after treatment of chronic hepatitis C patients with SovodaK
The mean age of HCV patients was 44.46 ± 8.12 years, with the minimum and maximum ages of 26 and 59 years, respectively. As shown in Table 1, about 97.8% were male, and 15.6% had a history of HIV infection. Also, 66.7% had a history of drug injection in the last 12 months.
Baseline Characteristics of the Study Patients (n = 45)
| Characteristic | Frequency (%) |
|---|---|
| Age, y | |
| ≤ 45 | 23 (51.1) |
| >46 | 22 (48.9) |
| Gender | |
| Male | 44 (97.8) |
| Female | 1 (2.2) |
| History of HIV infection | |
| No | 38 (84.4) |
| Yes | 7 (15.6) |
| History of Intravenous drug injection in the last 12 months | |
| No | 15 (33.3) |
| Yes | 30 (66.7) |
Findings related to the PCR test in patients revealed that the administration of Sovodak in all patients resulted in an efficacy of 100% in the assessment of SVR12. As shown in Table 2, the APRI level decreased significantly after treatment with Sovodak (0.35 versus 0.68, P-value: 0.000) in two age groups, even in HCV patients with a history of HIV (0.77 versus 1.47, P-value: 0.028) or a history of injecting drugs in the last 12 months (0.38 versus 0.66, P-value: 0.000).
Comparison of the Aspartate Aminotransferase to Platelet Ratio Index Median Before and After Treatment in Patients with Chronic Hepatitis C (n = 45)
| Characteristic | Median (IQR) Before Treatment | Median (IQR) After Treatment | P-Value |
|---|---|---|---|
| Age, y | |||
| Total | 0.68 (0.44 - 1.17) | 0.35 (0.25 - 0.48) | 0.000 |
| ≤ 45 | 0.73 (0.47 - 1.14) | 0.31 (0.23 - 0.49) | 0.000 |
| >46 | 0.66 (0.40 - 1.21) | 0.39 (0.31 - 0.47) | 0.001 |
| History of HIV infection | |||
| No | 0.64 (0.44 - 0.95) | 0.31 (0.24 - 0.45) | 0.000 |
| Yes | 1.47 (1.08 - 2.75) | 0.77 (0.41 - 1.47) | 0.028 |
| History of intravenous drug injection in the last 12 months | |||
| No | 0.74 (0.38 - 1.14) | 0.34 (0.25 - 0.41) | 0.001 |
| Yes | 0.66 (0.46 - 1.21) | 0.38 (0.25 - 0.51) | 0.000 |
Also, a comparison of APRI before and after treatment using the categories of APRI (<1 and >1) showed that among 14 patients with pre-treatment APRI≥1, 78.6% (n = 11) significantly had post-treatment APRI<1 (P = 0.006, Table 3).
Comparison of the Aspartate Aminotransferase to Platelet Ratio Index Before and After Treatment Using the Categories of the Aspartate Aminotransferase to Platelet Ratio Index (< 1 and > 1) in Patients with Chronic Hepatitis C (n = 45)
| Characteristic | After Treatment | P-Value | ||
|---|---|---|---|---|
| Total | APRI < 1 | APRI ≥ 1 | ||
| Before treatment | 0.006 | |||
| APRI < 1 | 31 (100) | 30 (96.8) | 1 (3.2) | |
| APRI ≥ 1 | 14 (100) | 11 (78.6) | 3 (21.4) | |
| Total | 45 (100) | 41 (91.1) | 4 (8.9) | |
5. Discussion
The present study aimed to determine the APRI before and after treatment with Sovodak in HCV patients from Rafsanjan, southeast Iran. The study results indicated a statistically significant decrease in the APRI level in 45 HCV patients (mean age = 44.46 ± 8.12 years) after treatment with Sovodak in the two age groups in HCV patients with or without a history of HIV infection and with or without a history of drug injection.
In Abdel-Aziz et al.’s study, the administration of Sovodak, with or without ribavirin, in HCV genotype 4 patients resulted in an efficacy of over 90% and high safety in the assessment of SVR12, which was effective in reducing liver fibrosis (13). In a prospective study conducted in Greece on 145 HCV patients who achieved an SVR after combination therapy with PegIFN-a/ribavirin, APRI values decreased significantly with treatment (0.95 versus 0.66, P < 0.001) and continued to decrease after a mean age of 5.7 years (14). The results of the present study were consistent with this study, showing that ADD agents can reduce the odds of liver fibrosis in HCV patients by reducing APRI when SVR is achieved.
A meta-analysis study conducted by Zhang et al. on cohort studies showed the existence of a significant relationship between the increased APRI and the increased risk of HCC in patients with chronic hepatitis C, indicating that APRI may be a valuable predictor for the risk of HCC in HCV patients (11). In a retrospective study conducted in Taiwan, predictors of HCC among 105 HCV cirrhotic patients after treatment with pegylated interferon and ribavirin were evaluated. Multivariate analysis showed that those with a high APRI had a significantly higher risk of HCC (HR 5.548). Further, the cumulative incidence of HCC was significantly higher in patients with a high APRI compared to those with a low APRI. The authors suggested that in HCV cirrhotic patients, after treatment with combination therapy, APRI and SVR are the two important predictors of HCC development (15).
In a retrospective study on 598 HCV patients with an SVR after interferon-based therapy, APRI before and after treatment was found to be associated with HCC development during 5 years of follow-up. They reported that stratification of patients based on both APRI before and after treatment was helpful in estimating the future risk of HCC. They concluded that the APRI before treatment at a cutoff of 1.0 had a 100% negative predictive value for up to 10 years after SVR (16). In a cohort study on 642 HCV patients with an SVR after peginterferon/ribavirin treatment in Taiwan, older non-cirrhotic patients with high gamma-glutamyltransferase (GGT) levels at baseline were at the same risk of HCC as cirrhotic patients during the follow-up period. They identified that HCC was significantly associated with GGT among non-cirrhotic patients (17). The mentioned studies support the potential role of APRI as a predictor of HCC in HCV patients.
Regarding the relationship between age and hepatitis C treatment outcomes, in the present study, the decreased level of APRI in HCV patients less than 45 years old was higher than in subjects over 45 years after treatment with Sovodak. Villa et al. reported that women less than 40 years of age treated with interferon-alpha had a higher SVR rate than women over 40 years of age (18).
In Jonathan et al.’s study, measurement of liver fibrosis was performed on 29 patients with HCV/HIV co-infection using APRI and fibrosis index-4 (FIB-4) before treatment with Sovodak and when SVR-24 was achieved. Most of the research subjects were male, with a mean age of 40.38 ± 3.48 years. A decrease in APRI and FIB-4 showed that Sovodak treatment was very effective and could reduce liver fibrosis in patients with HCV/HIV co-infection (19). The results of the present study were consistent with this study in terms of the effect of Sovodak on reducing the APRI in patients with HCV/HIV, as well as gender and the mean age of patients.
Also, Grebely et al.’s study showed that in HCV subjects with a history of recently injected drugs after treatment with sofosbuvir and velpatasvir, SVR12 was 94% regardless of injectable drug use before or during treatment (20). The results of the present study showed that even in HCV patients with a history of injection, Sovodak resulted in an efficacy of 100% in the assessment of SVR12 and was effective in reducing the APRI in patients.
The first limitation of the present study was its small size. So, it is suggested to conduct further studies with a larger sample size. The second limitation was a failure to follow up with patients. Another limitation was that the study did not include data on other factors that may affect liver fibrosis, such as the concurrent use of other medications alongside Sovodak, alcohol use, and other diseases, such as metabolic syndrome, that may cause liver fibrosis. Additionally, this study lacked a control group receiving a placebo or alternative treatment for comparison.
5.1. Conclusions
The study results indicated that the APRI level in HCV patients decreased significantly after treatment with Sovodak, regardless of having a history of HIV infection or a history of drug injection. Therefore, Sovodak in HCV patients can reduce the odds of liver fibrosis and subsequent HCC by reducing the APRI level.
Acknowledgements
References
-
1.
World Health Organization. Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021. World Health Organization; 2021.
-
2.
Mahmud S, Akbarzadeh V, Abu-Raddad LJ. The epidemiology of hepatitis C virus in Iran: Systematic review and meta-analyses. Sci Rep. 2018;8(1):150. [PubMed ID: 29317673]. [PubMed Central ID: PMC5760657]. https://doi.org/10.1038/s41598-017-18296-9.
-
3.
European Association for the Study of the Liver. EASL Recommendations on Treatment of Hepatitis C 2018. J Hepatol. 2018;69(2):461-511. [PubMed ID: 29650333]. https://doi.org/10.1016/j.jhep.2018.03.026.
-
4.
Lanini S, Ustianowski A, Pisapia R, Zumla A, Ippolito G. Viral Hepatitis: Etiology, Epidemiology, Transmission, Diagnostics, Treatment, and Prevention. Infect Dis Clin North Am. 2019;33(4):1045-62. [PubMed ID: 31668190]. https://doi.org/10.1016/j.idc.2019.08.004.
-
5.
Gupta E, Bajpai M, Choudhary A. Hepatitis C virus: Screening, diagnosis, and interpretation of laboratory assays. Asian J Transfus Sci. 2014;8(1):19-25. [PubMed ID: 24678168]. [PubMed Central ID: PMC3943138]. https://doi.org/10.4103/0973-6247.126683.
-
6.
Jakobsen JC, Nielsen EE, Feinberg J, Katakam KK, Fobian K, Hauser G, et al. Direct-acting antivirals for chronic hepatitis C. Cochrane Database Syst Rev. 2017;9(9). CD012143. [PubMed ID: 28922704]. [PubMed Central ID: PMC6484376]. https://doi.org/10.1002/14651858.CD012143.pub3.
-
7.
Chou R, Hartung D, Rahman B, Wasson N, Cottrell EB, Fu R. Comparative effectiveness of antiviral treatment for hepatitis C virus infection in adults: a systematic review. Ann Intern Med. 2013;158(2):114-23. [PubMed ID: 23437439]. https://doi.org/10.7326/0003-4819-158-2-201301150-00576.
-
8.
Geddawy A, Ibrahim YF, Elbahie NM, Ibrahim MA. Direct Acting Anti-hepatitis C Virus Drugs: Clinical Pharmacology and Future Direction. J Transl Int Med. 2017;5(1):8-17. [PubMed ID: 28680834]. [PubMed Central ID: PMC5490957]. https://doi.org/10.1515/jtim-2017-0007.
-
9.
Somi MH, Sepehri B, Nikniaz Z, Sedghi R. Efficacy of Sovodak in the Management of Patients Co-infected with HIV/HCV. Adv Pharm Bull. 2020;10(4):662-5. [PubMed ID: 33072543]. [PubMed Central ID: PMC7539312]. https://doi.org/10.34172/apb.2020.080.
-
10.
Shaheen AA, Myers RP. Diagnostic accuracy of the aspartate aminotransferase-to-platelet ratio index for the prediction of hepatitis C-related fibrosis: a systematic review. Hepatology. 2007;46(3):912-21. [PubMed ID: 17705266]. https://doi.org/10.1002/hep.21835.
-
11.
Zhang C, Wu J, Xu J, Xu J, Xian J, Xue S, et al. Association between Aspartate Aminotransferase-to-Platelet Ratio Index and Hepatocellular Carcinoma Risk in Patients with Chronic Hepatitis: A Meta-Analysis of Cohort Study. Dis Markers. 2019;2019:2046825. [PubMed ID: 31814857]. [PubMed Central ID: PMC6877976]. https://doi.org/10.1155/2019/2046825.
-
12.
Hakimi H, Ahmadi J, Vakilian A, Jamalizadeh A, Kamyab Z, Mehran M, et al. The profile of Rafsanjan Cohort Study. Eur J Epidemiol. 2021;36(2):243-52. [PubMed ID: 32725579]. https://doi.org/10.1007/s10654-020-00668-7.
-
13.
Abdel-Aziz AM, Ibrahim MA, El-Sheikh AA, Kamel MY, Zenhom NM, Abdel-Raheim S, et al. Effect of Sofosbuvir Plus Daclatasvir in Hepatitis C Virus Genotype-4 Patients: Promising Effect on Liver Fibrosis. J Clin Exp Hepatol. 2018;8(1):15-22. [PubMed ID: 29743792]. [PubMed Central ID: PMC5938328]. https://doi.org/10.1016/j.jceh.2017.06.006.
-
14.
Papastergiou V, Stampori M, Lisgos P, Pselas C, Prodromidou K, Karatapanis S. Durability of a sustained virological response, late clinical sequelae, and long-term changes in aspartate aminotransferase to the platelet ratio index after successful treatment with peginterferon/ribavirin for chronic hepatitis C: a prospective study. Eur J Gastroenterol Hepatol. 2013;25(7):798-805. [PubMed ID: 23395996]. https://doi.org/10.1097/MEG.0b013e32835eb8bf.
-
15.
Ng KJ, Tseng CW, Chang TT, Tzeng SJ, Hsieh YH, Hung TH, et al. Aspartate aminotransferase to platelet ratio index and sustained virologic response are associated with progression from hepatitis C associated liver cirrhosis to hepatocellular carcinoma after treatment with pegylated interferon plus ribavirin. Clin Interv Aging. 2016;11:1035-41. [PubMed ID: 27536084]. [PubMed Central ID: PMC4976814]. https://doi.org/10.2147/CIA.S108589.
-
16.
Lee K, Sinn DH, Gwak GY, Cho HC, Jung SH, Paik YH, et al. Prediction of the Risk of Hepatocellular Carcinoma in Chronic Hepatitis C Patients after Sustained Virological Response by Aspartate Aminotransferase to Platelet Ratio Index. Gut Liver. 2016;10(5):796-802. [PubMed ID: 27114418]. [PubMed Central ID: PMC5003204]. https://doi.org/10.5009/gnl15368.
-
17.
Huang CF, Yeh ML, Tsai PC, Hsieh MH, Yang HL, Hsieh MY, et al. Baseline gamma-glutamyl transferase levels strongly correlate with hepatocellular carcinoma development in non-cirrhotic patients with successful hepatitis C virus eradication. J Hepatol. 2014;61(1):67-74. [PubMed ID: 24613362]. https://doi.org/10.1016/j.jhep.2014.02.022.
-
18.
Villa E, Vukotic R, Camma C, Petta S, Di Leo A, Gitto S, et al. Reproductive status is associated with the severity of fibrosis in women with hepatitis C. PLoS One. 2012;7(9). e44624. [PubMed ID: 22970270]. [PubMed Central ID: PMC3438179]. https://doi.org/10.1371/journal.pone.0044624.
-
19.
Jonathan A, Wisaksana R, Agustanti N. Decreased in Liver Fibrosis in Patients with HCV/HIV Coinfection After Treatment with Sofosbuvir/Daclatasvir. Indones J Gastroenterol Hepatol Digest Endos. 2020;20(2):87-95. https://doi.org/10.24871/202201987-95.
-
20.
Grebely J, Dalgard O, Conway B, Cunningham EB, Bruggmann P, Hajarizadeh B, et al. Sofosbuvir and velpatasvir for hepatitis C virus infection in people with recent injection drug use (SIMPLIFY): an open-label, single-arm, phase 4, multicentre trial. Lancet Gastroenterol Hepatol. 2018;3(3):153-61. [PubMed ID: 29310928]. https://doi.org/10.1016/S2468-1253(17)30404-1.