Psychological Distress During COVID-19 Confinement in Persons After Metabolic Surgery.
DOI:
https://doi.org/10.56935/hij.v1i1.2Keywords:
Structural Equation Modelling, COVID-19, Gastrectomy, Psychological Distress, metabolic surgeryAbstract
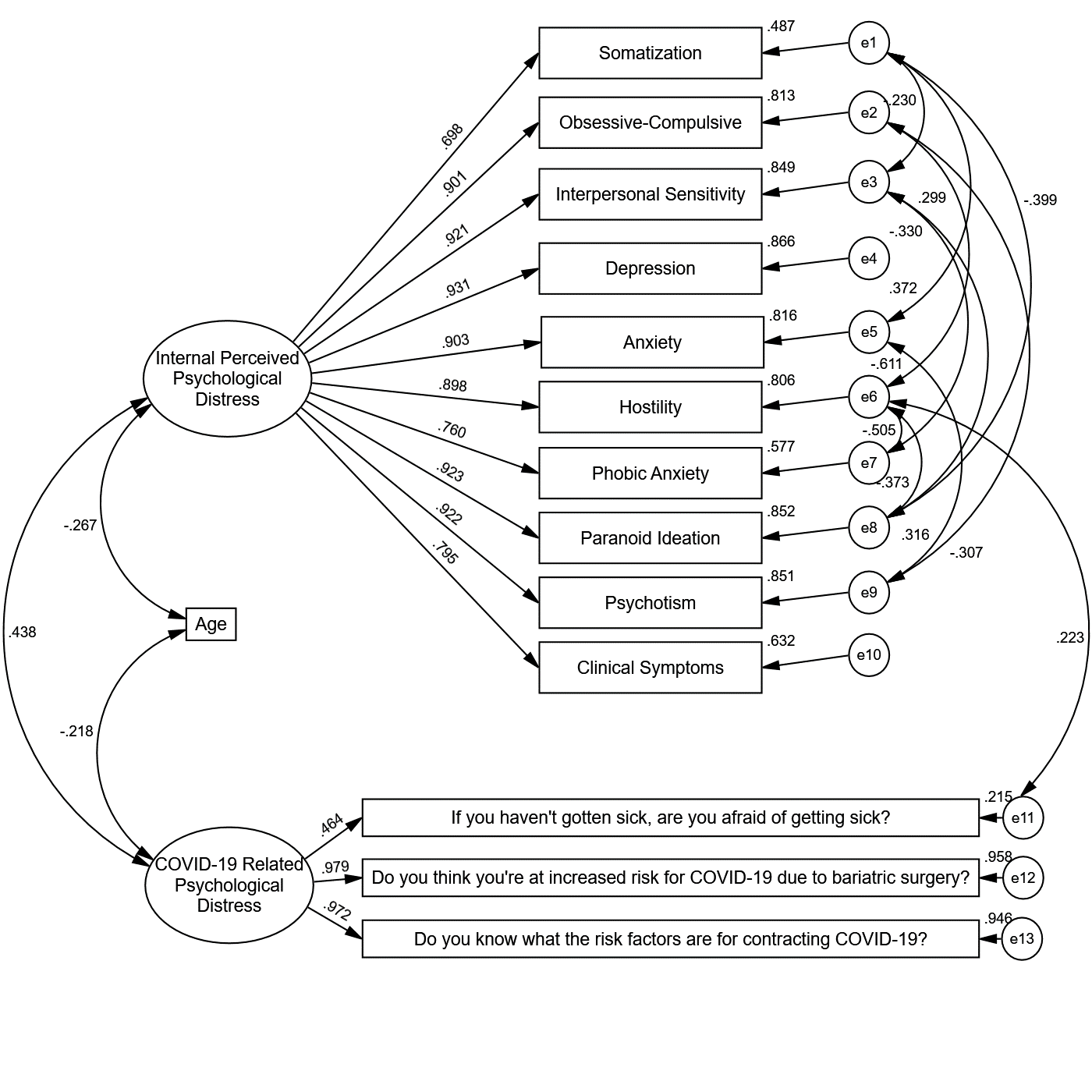
Background: People suffering from obesity often experience distress and psychopathological symptoms that decrease after undergoing metabolic surgery; the confinement caused by the COVID-19 pandemic impacted the whole population in this regard. Given that individuals undergoing metabolic surgery are at increased risk of developing these disorders, it is important to identify them in order to prevent or treat them appropriately. Therefore, this study aims to determine the relationship between COVID-19-related psychological distress and psychopathological symptoms in people who underwent metabolic surgery. Methods: A cross-sectional study was conducted including 102 participants more than six months after undergoing metabolic surgery. Sociodemographic information was collected, as well as psychological distress related to COVID-19 and psychopathological symptoms measured using the SCL-90R. A Structural Equation Model was developed to evaluate the effects and correlation between variables. Results: 90.2% of the participants were women, 84% had undergone gastric sleeve surgery while the rest had undergone Roux-en-Y gastric bypass surgery. The model obtained showed a significant correlation between the subscales of the SCL 90-R and COVID-19 related psychological distress and both were negatively correlated with the age of the participants. The COVID-19-related psychological distress factor had a significant effect on fear of contagion, perception and knowledge of risk of contagion, with risk perception being the most explained with 95.8% of variance explained. In addition, the final model showed adequate goodness-of-fit indicators. Conclusions: Psychological distress caused by pandemic and confinement is evidenced by higher scores on the SCL-90R instrument in persons with metabolic surgery. However, further studies and psychometric testing with more homogeneous samples in terms of sex and surgical technique are required.
References
Albaugh, V. L., Williams, D. B., Aher, C. V., Spann, M. D., & English, W. J. (2021). Prevalence of thiamine deficiency is significant in patients undergoing primary bariatric surgery. Surgery for Obesity and Related Diseases, 17(4), 653–658. https://doi.org/10.1016/j.soard.2020.11.032 DOI: https://doi.org/10.1016/j.soard.2020.11.032
Alonso, R., & Olivos, C. (2020). La relación entre la obesidad y estados depresivos The relationship between obesity and depressive states. Revista Clínica Las Condes, 31(2), 130–138. https://doi.org/10.1016/j.rmclc.2020.02.004 DOI: https://doi.org/10.1016/j.rmclc.2020.02.004
Andreu, A., Flores, L., Molero, J., Mestre, C., Obach, A., Torres, F., Moizé, V., Vidal, J., Navinés, R., Peri, J. M., & Cañizares, S. (2022). Patients Undergoing Bariatric Surgery: a Special Risk Group for Lifestyle, Emotional and Behavioral Adaptations During the COVID-19 Lockdown. Lessons from the First Wave. Obesity Surgery, 32(2), 441–449. https://doi.org/10.1007/s11695-021-05792-1 DOI: https://doi.org/10.1007/s11695-021-05792-1
Antoine, D., Li, Z., Quilliot, D., Sirveaux, M.-A., Meyre, D., Mangeon, A., Brunaud, L., Guéant, J.-L., & Guéant-Rodriguez, R.-M. (2021). Medium term post-bariatric surgery deficit of vitamin B12 is predicted by deficit at time of surgery. Clinical Nutrition, 40(1), 87–93. https://doi.org/10.1016/j.clnu.2020.04.029 DOI: https://doi.org/10.1016/j.clnu.2020.04.029
Arbuckle, J. L. (2019). IBM SPSS Amos 26 User´s Guide. ftp://public.dhe.ibm.com/software/analytics/spss/documentation/statistics/25.0/es/client/Manuals/IBM_SPSS_Statistics_Core_System_User_Guide.pdf
Baloch, S., Baloch, M. A., Zheng, T., & Pei, X. (2020). The coronavirus disease 2019 (COVID-19) pandemic. Tohoku Journal of Experimental Medicine, 250(4), 271–278. https://doi.org/10.1620/tjem.250.271 DOI: https://doi.org/10.1620/tjem.250.271
Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. https://doi.org/10.1037/0033-2909.107.2.238 DOI: https://doi.org/10.1037/0033-2909.107.2.238
Best, R., Strough, J. N., & Bruine de Bruin, W. (2023). Age differences in psychological distress during the COVID-19 pandemic: March 2020 – June 2021. Frontiers in Psychology, 14. https://doi.org/10.3389/FPSYG.2023.1101353/FULL DOI: https://doi.org/10.3389/fpsyg.2023.1101353
Bianciardi, E., Di Lorenzo, G., Niolu, C., Betrò, S., Zerbin, F., Gentileschi, P., & Siracusano, A. (2019). Body image dissatisfaction in individuals with obesity seeking bariatric surgery: Exploring the burden of new mediating factors. Rivista Di Psichiatria, 54(1), 8–17. https://doi.org/10.1708/3104.30935
Carabotti, M., Annibale, B., & Lahner, E. (2021). Common pitfalls in the management of patients with micronutrient deficiency: Keep in mind the stomach. Nutrients, 13(1), 1–18. https://doi.org/10.3390/nu13010208 DOI: https://doi.org/10.3390/nu13010208
Chamberlain, C., Terry, R., Shtayyeh, T., & Martinez, C. (2021). Recognizing postoperative nutritional complications of bariatric surgery in the primary care patient: a narrative review. Journal of Osteopathic Medicine, 121(1), 105–112. https://doi.org/10.7556/jaoa.2020.135 DOI: https://doi.org/10.7556/jaoa.2020.135
Cruz Fuentes, C. S., López Bello, L., Blas García, C., González Macías, L., & Chávez Balderas, R. A. (2005a). Datos sobre la validez y confiabilidad de la Symptom Check List 90 (SCL 90) en una muestra de sujetos Mexicanos. Salud Mental, 28(1), 72–81. http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0185-33252005000100072&lng=es&nrm=iso
Cruz Fuentes, C. S., López Bello, L., Blas García, C., González Macías, L., & Chávez Balderas, R. A. (2005b). Datos sobre la validez y confiabilidad de la Sympton Check List 90 (SCL 90) en una muestra de sujetos mexicanos. Salud Mental, 28(1), 72–81.
Cruzat-Mandich, C., Díaz-Castrillón, F., García Troncoso, A., & Díaz Paredes, P. (2019). Imagen corporal antes y después de cirugía bariátrica: Percepciones de mujeres jóvenes-adultas. Revista Mexicana de Trastornos Alimentarios, 10(1), 95–108. https://doi.org/10.22201/fesi.20071523e.2019.1.496 DOI: https://doi.org/10.22201/fesi.20071523e.2019.1.496
Derogatis, L. R. (1994). SCL-90-R: Symptom checklist-90-R: administration, scoring & procedures manual. National Computer Systems, Inc.
Derogatis, L. R., & Cleary, P. A. (1977). Confirmation of the dimensional structure of the scl-90: A study in construct validation. Journal of Clinical Psychology, 33(4), 981–989. https://doi.org/https://doi.org/10.1002/1097-4679(197710)33:4<981::AID-JCLP2270330412>3.0.CO;2-0 DOI: https://doi.org/10.1002/1097-4679(197710)33:4<981::AID-JCLP2270330412>3.0.CO;2-0
Esquivias, H., Reséndiz, A. M., García, F., & Elías-López, D. (2016). La salud mental en el paciente con obesidad en protocolo para cirugía bariátrica. Salud Mental, 39(3), 165–173. https://doi.org/10.17711/SM.0185-3325.2016.015 DOI: https://doi.org/10.17711/SM.0185-3325.2016.015
Fancourt, D., Steptoe, A., & Bu, F. (2021). Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. The Lancet Psychiatry, 8(2), 141–149. https://doi.org/10.1016/S2215-0366(20)30482-X DOI: https://doi.org/10.1016/S2215-0366(20)30482-X
Fitzpatrick, K. M., Drawve, G., & Harris, C. (2020). Facing new fears during the COVID-19 pandemic: The State of America’s mental health. Journal of Anxiety Disorders, 75(August). https://doi.org/10.1016/j.janxdis.2020.102291 DOI: https://doi.org/10.1016/j.janxdis.2020.102291
Fukase, Y., Ichikura, K., Murase, H., & Tagaya, H. (2022). Age-related differences in depressive symptoms and coping strategies during the COVID-19 pandemic in Japan: A longitudinal study. Journal of Psychosomatic Research, 155, 110737. https://doi.org/10.1016/J.JPSYCHORES.2022.110737 DOI: https://doi.org/10.1016/j.jpsychores.2022.110737
González-Santos, L., Mercadillo, R. E., Graff, A., & Barrios, F. A. (2007). Versión computarizada para la aplicación del Listado de Síntomas 90 (SCL 90) y del Inventario de Temperamento y Carácter (ITC). Salud Mental, 30(4), 31–40. http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0185-33252007000400031&lng=es&tlng=es
Grande, T. L., Newmeyer, M. D., Underwood, L. A., & Williams, C. R. (2014). Path analysis of the SCL-90-R: Exploring use in outpatient assessment. Measurement and Evaluation in Counseling and Development, 47(4), 271–290. https://doi.org/10.1177/0748175614538061 DOI: https://doi.org/10.1177/0748175614538061
Hoyle, R. H., & Smith, G. T. (1994). Formulating clinical research hypotheses as structural equation models: A conceptual overview. Journal of Consulting and Clinical Psychology, 62(3), 429–440. https://doi.org/10.1037/0022-006X.62.3.429 DOI: https://doi.org/10.1037/0022-006X.62.3.429
Hu, L.-T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. https://doi.org/10.1080/10705519909540118 DOI: https://doi.org/10.1080/10705519909540118
Jia, R., Ayling, K., Chalder, T., Massey, A., Broadbent, E., Coupland, C., & Vedhara, K. (2020). Mental health in the UK during the COVID-19 pandemic: cross-sectional analyses from a community cohort study. BMJ Open, 10(9), e040620. https://doi.org/10.1136/bmjopen-2020-040620 DOI: https://doi.org/10.1136/bmjopen-2020-040620
khan, B., Shafiq, H., Abbas, S., Jabeen, S., Khan, S. A., Afsar, T., Almajwal, A., Alruwaili, N. W., Al-disi, D., Alenezi, S., Parveen, Z., & Razak, S. (2022). Vitamin D status and its correlation to depression. Annals of General Psychiatry, 21(1), 32. https://doi.org/10.1186/s12991-022-00406-1 DOI: https://doi.org/10.1186/s12991-022-00406-1
Kim, S. Y., Jeon, S. W., Lim, W. J., Oh, K. S., Shin, D. W., Cho, S. J., Park, J. H., Kim, Y. H., & Shin, Y. C. (2020). Vitamin D deficiency and suicidal ideation: A cross-sectional study of 157,211 healthy adults. Journal of Psychosomatic Research, 134. https://doi.org/10.1016/J.JPSYCHORES.2020.110125 DOI: https://doi.org/10.1016/j.jpsychores.2020.110125
Menon, V., Kar, S., Suthar, N., & Nebhinani, N. (2020). Vitamin D and Depression: A Critical Appraisal of the Evidence and Future Directions. Indian Journal of Psychological Medicine, 42(1), 11. https://doi.org/10.4103/IJPSYM.IJPSYM_160_19 DOI: https://doi.org/10.4103/IJPSYM.IJPSYM_160_19
Patel, S. Y., Mehrotra, A., Huskamp, H. A., Uscher-Pines, L., Ganguli, I., & Barnett, M. L. (2021). Trends in Outpatient Care Delivery and Telemedicine During the COVID-19 Pandemic in the US. JAMA Internal Medicine, 181(3), 388. https://doi.org/10.1001/jamainternmed.2020.5928 DOI: https://doi.org/10.1001/jamainternmed.2020.5928
Pineda-García, G, Serrano-Medina, A., Jm, C.-B., Vh, A.-S., González-Sánchez, A.-R. E., Pineda-García, G., Serrano-Medina, A., Cornejo-Bravo, J. M., Andrade-Soto, H., Armenta-Rojas, E., & Lilian González-Sánchez, D. (2022). Modelo de autocuidado e imagen corporal en adultos post-cirugía bariátrica. Revista Latino-Americana de Enfermagem, 30. https://doi.org/10.1590/1518-8345.5592.3586 DOI: https://doi.org/10.1590/1518-8345.5592.3586
Pineda-García, Gisela, Serrano-Medina, A., Cornejo-Bravo, J. M., Andrade-Soto, V. H., Armenta-Rojas, E., & González-Sánchez, D. L. (2022). Self-care model and body image in adults after a bariatric surgery. Revista Latino-Americana de Enfermagem, 30. https://doi.org/10.1590/1518-8345.5592.3536 DOI: https://doi.org/10.1590/1518-8345.5592.3587
Ransom, D., Ashton, K., Windover, A., & Heinberg, L. (2010). Internal consistency and validity assessment of SCL-90-R for bariatric surgery candidates. Surgery for Obesity and Related Diseases : Official Journal of the American Society for Bariatric Surgery, 6(6), 622–627. https://doi.org/10.1016/j.soard.2010.02.039 DOI: https://doi.org/10.1016/j.soard.2010.02.039
Santos-Ruiz, A., Montero-López, E., Ortego-Centeno, N., & Peralta-Ramírez, M. I. (2021). Efecto del confinamiento por COVID-19 en el estado mental de pacientes con lupus eritematoso sistémico. Medicina Clínica, 156(8), 379–385. https://doi.org/10.1016/j.medcli.2020.12.004 DOI: https://doi.org/10.1016/j.medcli.2020.12.004
Schmitz, N., Holley, P., Meng, X., Fish, L., & Jedwab, J. (2020). COVID-19 and Depressive Symptoms: A Community-based Study in Quebec, Canada. The Canadian Journal of Psychiatry, 65(10), 733–735. https://doi.org/10.1177/0706743720943812 DOI: https://doi.org/10.1177/0706743720943812
Sherman, A. C., Williams, M. L., Amick, B. C., Hudson, T. J., & Messias, E. L. (2020). Mental health outcomes associated with the COVID-19 pandemic: Prevalence and risk factors in a southern US state. Psychiatry Research, 293(January), 113476. https://doi.org/10.1016/j.psychres.2020.113476 DOI: https://doi.org/10.1016/j.psychres.2020.113476
World Health Organization. (2021). Advice for the public. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
Wu, K. K., Chan, S. K., & Ma, T. M. (2005). Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS). Journal of Traumatic Stress, 18(1), 39–42. https://doi.org/10.1002/jts.20004 DOI: https://doi.org/10.1002/jts.20004
Yu, Y., Wan, C., Huebner, E. S., Zhao, X., Zeng, W., & Shang, L. (2019). Psychometric properties of the symptom check list 90 (SCL-90) for Chinese undergraduate students. Journal of Mental Health, 28(2), 213–219. https://doi.org/10.1080/09638237.2018.1521939 DOI: https://doi.org/10.1080/09638237.2018.1521939
Additional Files
Published
How to Cite
License
Copyright (c) 2023 Daniela Lilian González-Sánchez, Efraín Armenta-Rojas

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License 4.0 that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.