Introduction
Rheumatoid arthritis (RA) is a multisystemic inflammatory disease that may lead to disability, significant functional impairment, and premature death [1]. It is a leading cause of disability worldwide and impacts 0.5–1% of the population, with a female preponderance [2]. Rheumatoid arthritis can cause significant morbidity, and managing this disease can be challenging, particularly in lower-middle-income countries where clinical expertise and direct cost of treatment are substantial constraints [3]. If the condition is not recognized and appropriately managed, pain due to active disease, loss of function due to structural damage, and decreased quality of life adversely impact physical and mental health [4].
The goal of care is to maximize the patient’s long-term health-related quality of life by controlling disease symptoms, preventing structural damage, and improving the patient’s ability to function in the community [4]. Rheumatoid arthritis activity impacts physical and social functional domains [3]. They include role limitations due to physical health problems, participation in usual activities, and bodily pain [5]. Therefore, self-reported data by the patient best describe the social and physical consequences of this disease, which is frequently debilitating, and constitutes a patient-reported outcomes measure that should be quantified during a clinical assessment of disease activity [6].
The quantification of RA disease activity is paramount to determine the course of treatment [7]. In this regard, several measures of disease activity have been proposed and incorporated into the routine clinical assessment of patients with RA [8]. One of the most commonly used measures of disease activity is the Disease Activity Score 28 (DAS28) with ESR and the C-reactive protein (CRP) determination. The DAS28 has been validated in multiple cohorts of RA across continents [9]. However, the cumbersome computation of this score has prompted the development of the Simplified Disease Activity Index (SDAI) and the Clinical Disease Activity Index (CDAI) [10]. The various composite measures have advantages and disadvantages in assessing RA disease activity [10–12]. The CDAI relies on an objective clinical assessment of disease activity without considering the value of acute phase reactants [13].
In several studies, the physician and patient’s global assessment components were discordant among different populations using CDAI and SDAI compared to DAS28 [14]. Therefore, many rheumatologists prefer clinical disease activity assessment with the DAS28–ESR or DAS28–CRP, depending on the cost and availability of acute phase reactants [15].
Despite similar components of disease activity in all the various assessment indices, which include a numerical score for the tender and swollen joint counts, and an assessment of global health by the patient and physician, there remains a debate as to which instrument is ideal and cost-effective in a busy outpatient clinical setting [16]. Moreover, there are instances when a patient may report a subjective worsening of the disease symptoms that do not reflect the measurement of acute phase reactants, i.e., CRP and ESR. This discordance confounds an accurate evaluation of disease activity [17], crucial for targeting therapies to attain low disease activity or remission in RA [16]. Precise determination of disease activity with a validated clinical index is required before intensifying disease-modifying therapy to treat the target, low disease activity, or clinical remission [18].
Another essential aspect of routine ambulatory care of patients with RA is an assessment of the functional status [19]. One of the most validated tools for evaluating functional ability is the modified Health Assessment Questionnaire (mHAQ), readily available for outpatients [20]. Compared to the original HAQ, the mHAQ is easier to use in a busy outpatient setting and provides a reasonable assessment of physical functioning in patients with rheumatoid arthritis. It informs patient-reported outcomes and forms a key component of disease activity assessment [17].
According to the 2010 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) classification criteria, the RA diagnosis also considers rheumatoid factor titers and anti-cyclic citrullinated peptide antibodies (ACPA) [21]. Studies have shown a positive correlation of ACPA with the DAS28 [22]. Whether this association helps determine disease activity requires further validation in different ethnic and geographical regions, considering the heterogeneity of demographics, environment, and social determinants of health affecting predisposition to RA. Therefore, we sought to determine the disease activity in RA with the DAS28 score. Our secondary objectives were to evaluate the correlation of the DAS28 with multidimensional HAQ and components of disease activity and assess the concordance of acute phase reactants with the DAS28.
Material and methods
A cross-sectional study was conducted at the Aga Khan University Hospital Karachi Rheumatology Outpatient Clinic after approval by the institution’s ethics review committee (ERC ID: 4551-Med-ERC-17). The study was conducted according to the Declaration of Helsinki. The eligible patients were informed about the study objectives, and written consent was obtained. Consecutive patients who fulfilled the 2010 ACR-EULAR classification criteria for rheumatoid arthritis were enrolled in the clinic for 24 weeks.
Inclusion criteria of patient recruitment included:
fulfillment of the ACR/EULAR 2010 classification criteria,
age ≥ 18 years,
fluent communication in Urdu or English.
Patients with a psychiatric history of intellectual and cognitive impairments and those with significant comorbidities were excluded. In total, 155 patients were prospectively enrolled in the study.
Pertinent patient demographics including age, gender, duration of disease, radiographs of the hands and feet joints, clinical characteristics including swollen and tender joints, morning stiffness, and degree of pain as rated by the patient on a Visual Analogue Scale (VAS; on a scale of 1 to 10), were noted in a proforma by the principal investigator and a research team member. The DAS28 score includes patients’ global health score on a VAS as reported by each individual patient to the principal investigator. A list of current medications, as well as the results of laboratory investigations such as ACPA, rheumatoid factor (RF), CRP, and erythrocyte sedimentation rate (ESR), was also captured by the research personnel in the rheumatology clinic.
All study participants completed a mHAQ to evaluate physical and social domains.
Clinical assessment of disease activity: Disease Activity Score 28
The disease activity was determined using the DAS28 score. The DAS28 includes evaluation of 28 swollen joint (SJC-28) and tender joint counts (TJC-28), ESR, CRP, and patient’s global health (GH status) on a 0–100 VAS to calculate a score. We used an online DAS28 calculator, which uses the following equation to compute a score for disease activity.
DAS28 = 0.56 × √(TJC28) + 0.28 × √(SJC28) + 0.70 × in (ESR) + 0.014 × GH.
The DAS28 can range from 0.49 to 9.07. High disease activity is defined as a DAS28 > 5.1, moderate activity as a DAS28 between 3.2 and 5.1, and low activity as a DAS28 between 2.6 and 3.2. A patient is in remission if the DAS28 is less than 2.6.
Measurement of functional status using the modified Health Assessment Questionnaire
We assessed activities of daily living for our patients using mHAQ. The mHAQ is a simplified version of the Health Assessment Questionnaire (HAQ). The mHAQ consists of eight questions with one question from each category of the HAQ. The questions are divided into eight categories. The mHAQ score is the mean of the individual scores for each activity. Scores range from 0 to 3, with higher scores indicating worse function and more significant disability, while a score of ≤ 0.3 is considered normal.
Biochemical analysis of rheumatoid factors and anti-cyclic citrullinated peptide antibody
Blood samples of patients were analyzed for RF antibodies by a latex-enhanced immunoturbidimetric method on an automated routine chemistry analyzer, ADVIA 1800 (Siemens Diagnostics, US). Three-level controls were run with each batch of patient samples for quality control. Serum ACPA assay was performed by a solid phase, two-cycle sequential chemiluminescent immunometric assay on the IMMULITE 2000 (Siemens Diagnostics, US). Two-level controls were run with each batch of patient samples for quality control. During the study period, the College of American Pathologists (CAP) proficiency checks were performed, and all results were accurate and acceptable. Samples with titers ≥ 14 IU/ml and > 4 U/ml were positive for RF and ACPA.
Statistical analysis
Data were analyzed using SPSS version 21.0 for Windows. The continuous mean ±SD was calculated for continuous numerical variables; otherwise, the median (interquartile range [IQR 1–3]) was computed. Categorical or qualitative variables were presented as frequency and percentages and generated accordingly. Patients were categorized into RA activity status based on the DAS28 score. Frequencies of patients who tested positive for RA factor and ACPA were generated. The χ2 test assessed the relationship between DAS28–CRP, DAS28–ESR, ACPA, and RF. Pearson’s correlation coefficients were computed to determine the correlation between DAS28, ACPA, RF, tender and swollen joint counts, and mHAQ. A two-sided tailed test with a p-value < 0.05 was considered statistically significant.
Results
Of 155 patients, complete baseline data on DAS28, ESR, CRP, mHAQ were available for 132, and these patients were included in the final analyses. Table I summarizes the core variables and dataset. The mean age of patients was 46 years; there were 113 females and 19 males with a male/female ratio of 1 : 5.9. The mean duration of illness was 5.7 ±6.4 years. The mean values of RA core dataset measures were as follows: the mean ESR was 29 mm/h (median IQR 15.7–50), mean CRP was 4.1 mg/l (median IQR 2–16.8). The mean DAS28 was 3.4 ±1.8 (mean ±SD), and the mean mHAQ score was 0.77 ±0.68 (mean ±SD). The PGA of pain was 45.1 ±29.1 (mean ±SD) (median IQR 50 [20–70]) on a 0–100 VAS.
Table I
Mean and median values of rheumatoid arthritis dataset measures
Table II shows the demographics of the study population relative to the disease activity state. According to the DAS28 calculation, low, moderate, and high disease activity was observed in 46.2% (n = 61), 40.1% (n = 53), and 13.6% (n = 18) respectively. Multiple DMARDs use was associated with moderate to high DAS28 scores (p-value < 0.001), as well as treatment with prednisone (p = 0.07) and NSAIDs (p = 0.04), shown in Table II.
Table II
Descriptive characteristics in relation to clinical profile, Disease Activity Score 28 and functional status
[ii] ACPA – anti-cyclic citrullinated peptide antibody, ALT – alanine aminotransferase, CRP – C-reactive protein, DAS28 – Disease Activity Score 28, DMARDs – disease-modifying anti-rheumatic drugs, ESR – erythrocyte sedimentation rate, HCT – hematocrit, mHAQ – modified Health Assessment Questionnaire, NSAIDs – non-steroidal anti-inflammatory drugs, PGA – Patient’s Global Assessment, TNF – tumor necrosis factor, VAS – Visual Analogue Scale.
A comparison of mHAQ with the mean DAS28 scores showed that the patients with moderate to high disease activity had higher mHAQ scores than those in remission or had low disease activity (p-value < 0.001). None of the patients had a mHAQ score < 0.3. There was also a significant association between mHAQ and all three categories of pain scores on the VAS (p-value < 0.001).
Low hemoglobin and hematocrit (p = 0.08, p = 0.004) and thrombocytosis (p = 0.004) were also associated with moderately to severely active disease.
DAS28–ESR and DAS28–CRP correlation with disease activity and functional status is presented in Table III A. The individual components of disease activity, including tender and swollen joint counts, ESR, CRP, the mHAQ score, and the patient’s global pain assessment, strongly correlated with the mean DAS28 score (p-value < 0.001). The tender and swollen joint count 28 also demonstrated a significant positive correlation with DAS28, Pearson correlation coefficient r = 0.64 (p-value < 0.001).
Table III A
Correlation of DAS28 with measures of disease activity and functional status
| Variables | Mean ±SD | DAS28 (Pearson correlation) |
|---|---|---|
| Rheumatoid factor | 169.2 ±176.5 | r = 0.009 |
| ESR | 35.6 ±27.5 | r = 0.49** |
| CRP | 13.5 ±21.6 | r = 0.39** |
| ACPA | 214.9 ±206.1 | r = -0.01 |
| mHAO score | 0.77 ±0.68 | r = 0.47** |
| PGA | 45.1 ±29.1 | r = 0.45** |
| Tender joint count (TJC-28) | 2.3 ±5.6 | R = 0.64** |
| Swollen joint count (SJC-28) | 2.4 ±5.7 | R = 0.64** |
Correlation of mHAQ with acute phase reactants and components of disease activity is presented in Table III B. The correlation matrix between mHAQ and the mean DAS28 showed a strong correlation (r = 0.478). In contrast, there was no correlation between RA factor (r = –0.035) and ACPA (r = −0.094). A reasonable correlation of mHAQ was observed with the acute phase reactants CRP and ESR with Pearson correlation coefficient r = 0.242 and r = 0.225, respectively (p-value < 0.001).
Table III B
Correlation of mHAQ with acute phase reactants and components of disease activity
| Variables | Mean ±SD | mHAQ Score median (IQR) | Pearson correlation |
|---|---|---|---|
| DAS28 score | 3.77 ±1.61 | r = 0.478* | |
| ESR | 38.08 ±26.76 | r = 0.242* | |
| CRP | 17.81 ±23.35 | 1.07 ±0.56 | r = 0.225* |
| RA factor | 1.07 ±0.25 | r = -0.035 | |
| ACPA | 189.35 ±207.94 | r = -0.094 |
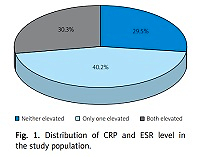
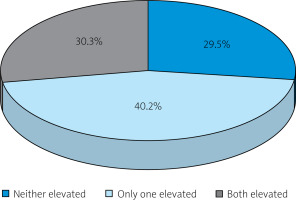
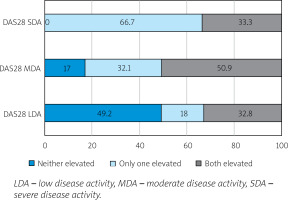
According to the DAS28–CRP and DAS28–ESR, the patients were further sub-grouped into three categories (Table IV). An ESR value of 28 mm/h and a CRP value of more than 8 mg/l was considered the cut-off for active RA. The distribution of disease activity differed significantly depending on the elevation of the acute phase reactants (APR). The level of acute phase reactants was categorized as neither elevated, one elevated, or both elevated. Both ESR and CRP levels were elevated in 30.3% of the patients, while only one marker was increased by 40.2% (Fig. 1). None of the inflammatory markers were elevated in the remaining 29.5% of the study subjects (Fig. 1). Both DAS28 and mHAQ scores increased sequentially with the increase in the level of acute phase reactants (Table IV). Multiple DMARDs use was associated with moderate to high DAS28 scores (p-value < 0.001). In patients with severely active disease, one of the acute phase reactants was elevated in 66.7%, whereas 33.3% had increased levels of both markers. Patients in the moderate and low disease activity states also showed discordance in the level of acute phase reactants compared with the disease activity (Fig. 2).
Table IV
Clinical and functional status according to levels of acute phase reactants (CRP and ESR)
Discussion
In this study, a model that included a modified Health Assessment Questionnaire (mHAQ), DAS28–ESR, and acute phase reactant best evaluated disease activity in an outpatient cohort of RA patients visiting a rheumatology clinic within a resource-limited setting. The specific elements of disease activity assessment included the DAS28 score, the patient’s global health assessment, mHAQ, and elevated acute phase reactants. From Pakistan, where data on rheumatoid arthritis are scarce [23, 24], our study is unique in assessing disease activity in a cohort of RA patients visiting the outpatient department. What makes our study important compared to similar studies from South Asia [8, 13] is the fact that we determined the concordance of acute phase reactants (APR) with the DAS28 score.
Compared with CDAI, which omits acute phase reactants and employs only clinical variables, the utility of DAS28 in the clinical assessment of disease status is evident from the results obtained in our cohort. The mean DAS28 score in our study cohort was 3.4 ±1.8 (mean ±SD), and most patients had moderately active disease. In contrast, other South Asian cohorts from India have reported the mean DAS28 of 5.5 ±1.49 (mean ±SD) [25] and 5.97 ±1.21 (mean ±SD) [13], signifying high disease activity in their population.
Rheumatoid arthritis management requires monitoring disease activity to determine the course of treatment. Our results demonstrate that a composite of DAS28–ESR with an assessment of functional status and quality of life utilizing mHAQ determines disease activity. These findings are comparable to those of a study by Egyptian investigators on 130 patients with RA [26]. Their results also demonstrated a significant correlation of DAS28–ESR/DAS28–CRP with other markers of disease activity. They also compared SDAI and CDAI with DAS28 and noted an apparent correlation between disease activity indices and the mHAQ, akin to our cohort [26].
Rheumatoid arthritis is a disabling disease, and therapy aims to improve the patients’ functionality and quality of life [27]. Patients’ physical and mental health correlates with pain, loss of function, work participation, and decreased quality of life. The multidimensional composition of the mHAQ is intended to detect the changes or improvement in patients’ functional status [28] in patients with rheumatoid arthritis. This study found that the DAS28–ESR and DAS28–CRP positively correlated with the mHAQ. However, none of the patients had an mHAQ score ≤ 0.3, and RA patients with high disease activity had significantly higher mHAQ scores than those with low or moderate disease activity.
Similar findings were obtained by Pincus et al. [29]; they reported agreement between mHAQ and DAS28 scores in > 80% of patients with moderate to high disease activity. Inability to work with loss of income, the physical demand for more rest in the presence of active joint inflammation, reduced quality leisure time, and increasing dependence on social services and income support highlight the challenging socio-economic determinants of RA [30]. Therefore, it has become well known that clinical and laboratory markers do not encompass the whole experience of disability resulting from joint inflammation and deformities with RA [30].
Challa et al. [31] highlighted patient and provider discordance as a critical consideration in assessing disease activity in RA with regards to the markers of inflammation and assessment of functional status and disease severity as we observed in our study. In our patients with active rheumatoid arthritis defined by DAS28 > 2.6, the number of elevated acute phase reactants (APRs) positively reflected severely active disease. Both APRs were elevated in only 30.3% of the patients in this category. However, 17% of patients with moderately active RA had neither of the acute phase reactants elevated. This discordance of the disease activity with the level of APR was more striking in the patients with low active RA, where 49.2% of the patients had neither ESR nor CRP elevated.
Similar findings were reported previously by Barton et al. [32] The authors concluded that patients with discordance of the acute phase reactants and disease activity scores were more likely to have a low to moderate disease activity.
We also observed that the DAS28–ESR and DAS28–CRP did not correlate with RF or ACPA. One of the reasons is that the RF and ACPA can aid in the disease diagnosis. In contrast, the DAS28 is a tool for monitoring disease activity in RA patients, independent of the antibody titers [33]. A previous study by Serdaroğlu et al. [34] revealed that ACPA levels were not significantly associated with the DAS28 score (p-value 0.459). From Pakistan, another study by Shah et al. [24] reported similar findings that ACPA levels did not correlate with the DAS28 scores (p-value 0.348).
Our study is the first and the most significant from a university teaching hospital in Pakistan reporting an association between DAS28 scores and mHAQ. We recognize that an essential limitation of our study is that it was a single center’s experience, with a lower number of participants, limiting the study’s power. Secondly, not all the patients had the necessary results available at enrollment, accounting for exclusion from the study.
Conclusions
To conclude, our study demonstrated the utility of DAS28–ESR and DAS28–CRP for assessing disease activity in RA patients by providing evidence that DAS28 strongly correlates with mHAQ, an indicator of functional ability in patients with rheumatic diseases.
The level of acute phase reactants in our study was directly proportional to severely active RA. Invariably, the overall health consequences of active RA are dire and too much for an individual to bear. This situation worsens for patients in developing countries like Pakistan, lacking social infrastructure and support services. Thus in an outpatient setting in a developing country like Pakistan, we suggest that both DAS28–ESR and DAS28–CRP combined with mHAQ can be used for monitoring disease activity and functional status in patients with rheumatoid arthritis.
Future studies from Pakistan should compare other composite measures with longitudinal follow-up to better characterize disease activity and severity to ensure targeted therapy aiming at treatment goals in rheumatoid arthritis.