Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 58(2); 2024 > Article
-
Case Study
Fibrin-associated large B-cell lymphoma arising in an endovascular graft: first case report in Korea -
Min Gyoung Pak
 , Mee Sook Roh
, Mee Sook Roh
-
Journal of Pathology and Translational Medicine 2024;58(2):87-90.
DOI: https://doi.org/10.4132/jptm.2023.12.28
Published online: January 24, 2024
Department of Pathology, Dong-A University College of Medicine, Busan, Korea
- Corresponding Author: Mee Sook Roh, MD, PhD, Department of Pathology, Dong-A University College of Medicine, 32 Daesingongwon-ro, Seo-gu, Busan 49201, Korea Tel: +82-51-240-2833, E-mail: 'msroh@dau.ac.kr'
© 2024 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,090 Views
- 170 Download
Abstract
- Fibrin-associated large B-cell lymphoma (FA-LBCL) is an extremely rare subtype of LBCL that consists of microscopic aggregates of atypical large B cells in the background of fibrin. Here, we report the first case of FA-LBCL in Korea. A 57-year-old male presented with a large amount of thrombus in the thoracic aorta during follow-up for graft replacement of the thoracoabdominal aorta 8 years prior. The removed thrombus, measuring 4.3 × 3.1 cm, histologically exhibited eosinophilic fibrinous material with several small clusters of atypical lymphoid cells at the periphery. The atypical cells were positive for CD20 by immunohistochemistry and for Epstein-Barr virus by in situ hybridization. The Ki-67 proliferation rate was 85%. The patient was still alive with no recurrence at the 7-year follow-up after thrombectomy. Although the diagnosis can be very difficult and challenging due to its paucicellular features, pathologists should be aware of FALBCL, which has likely been underestimated in routine evaluations of thrombi.
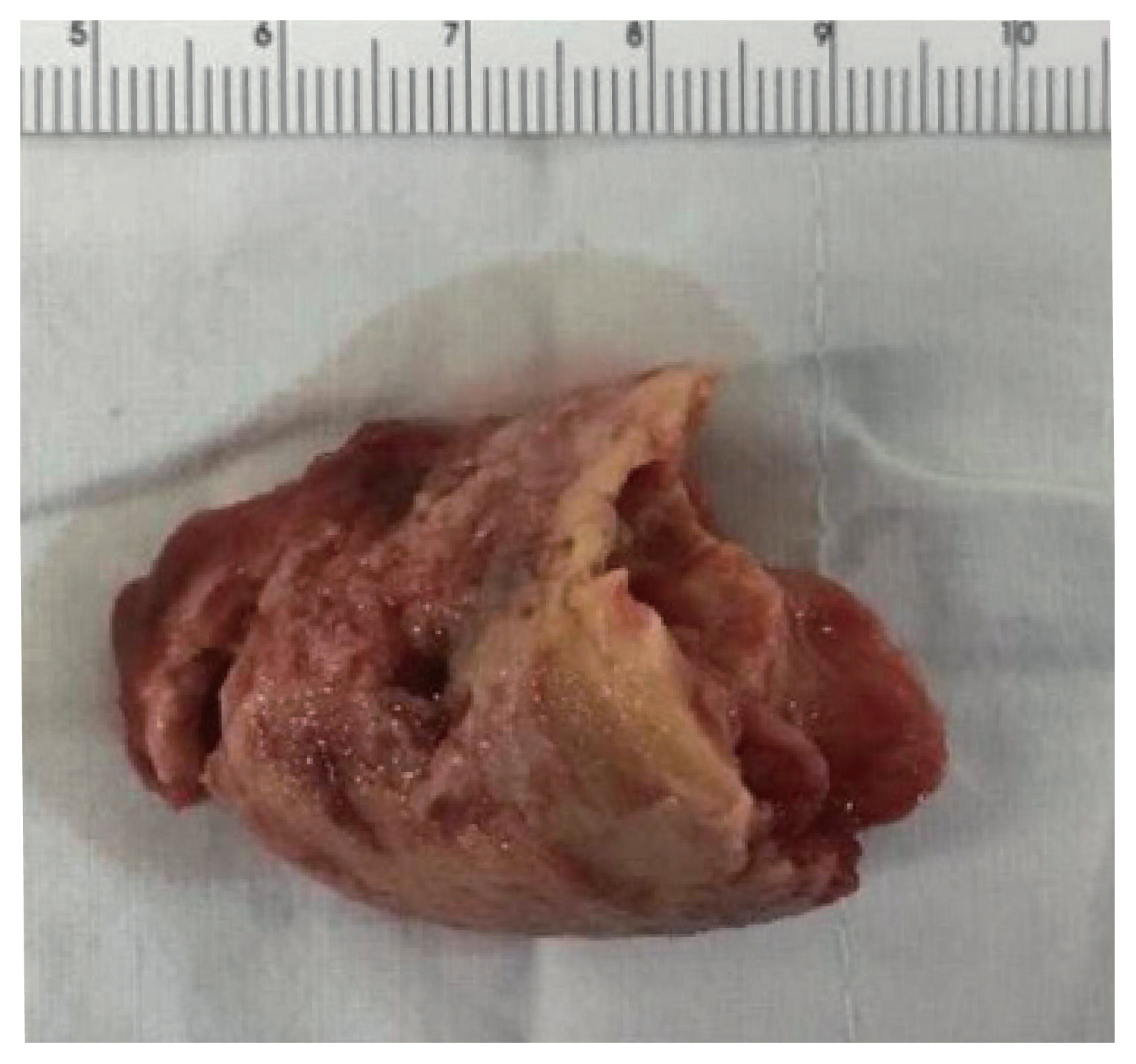
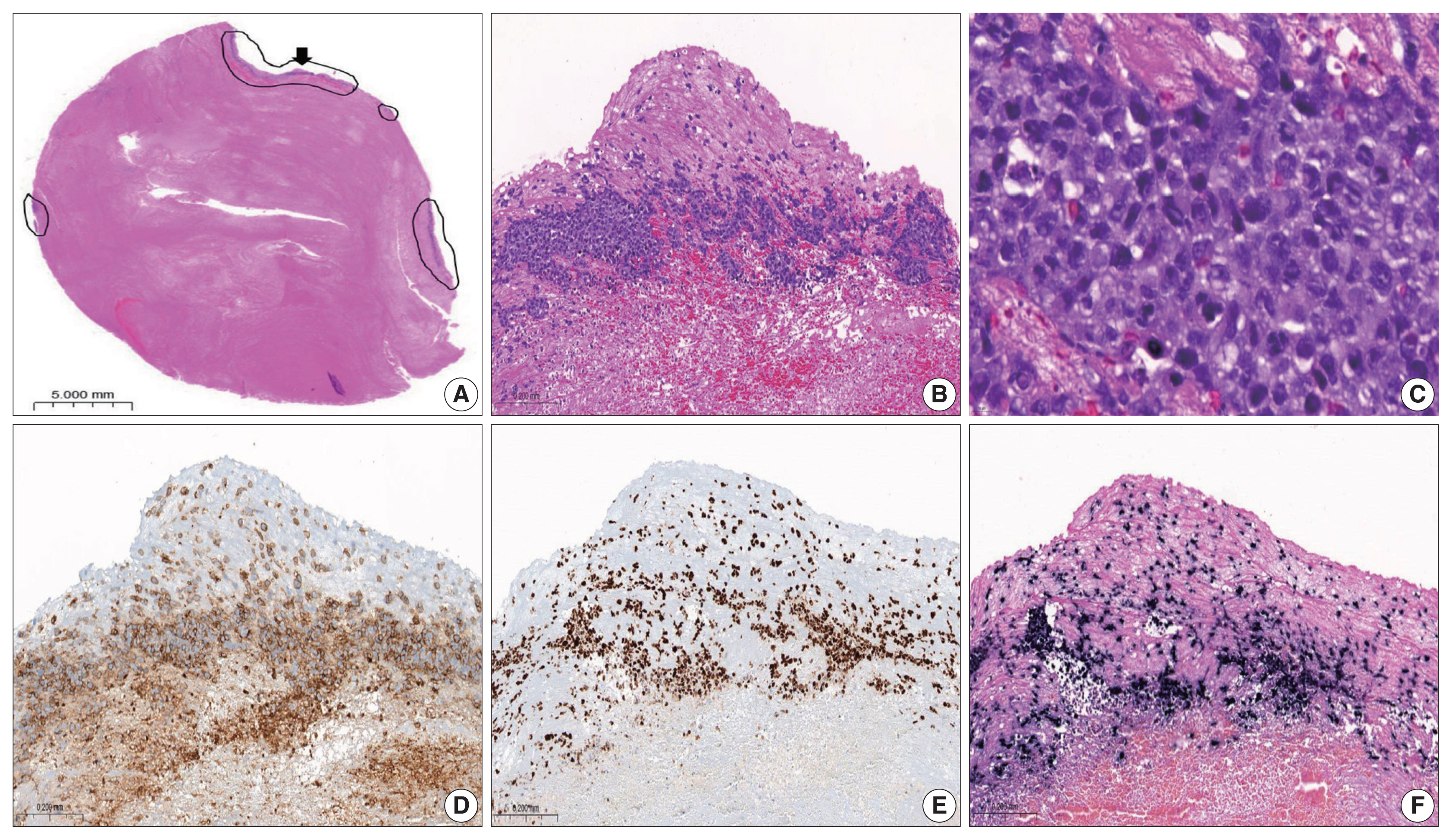
- A 57-year-old male presented with a large amount of intraluminal thrombus in the thoracic aorta during a periodic follow-up after graft replacement of the thoracoabdominal aorta. He had previously been diagnosed with a thoracic aortic aneurysm and received graft replacement of the thoracoabdominal aorta at another hospital in 2008. Approximately 8 years after this procedure, computed tomography angiography of the chest revealed a parastent occlusive thrombus at the distal portion of the previous graft-connected segment during a periodic follow-up. The patient underwent thoracic aortic thrombectomy and open thoracic endovascular aneurysm repair in the descending aorta in October 2016. The thrombus was sent for pathologic examination. Upon gross examination, the specimen, measuring 4.3 × 3.1 cm, presented as a usual yellowish-brown thrombus. No gross evidence of a lesion thought to be a tumor was identified on the cut surface (Fig. 1). The histologic sections revealed abundant acellular eosinophilic fibrinous material with several small, viable atypical cellular clusters at the periphery of the fibrin thrombus (Fig. 2A). The cellular areas were characterized by atypical, large lymphoid cells with vesicular nuclei, irregular nuclear membranes, and conspicuous nucleoli. Mitotic figures and admixed apoptotic bodies were easily located (Fig. 2B, C). No chronic inflammatory cell infiltration in the background or vicinity was observed. The atypical cells were positive for CD20 by immunohistochemistry (Fig. 2D). Systemic evaluation was recommended to rule out occult malignancy, especially hematopoietic malignancy. However, the workup revealed no evidence of lymphoma or any other malignancy. A diagnosis of lymphoproliferative disorder was made in October 2016 using the most appropriate classification of this lesion in the then-current fourth edition of the WHO classification at the time of diagnosis. Due to uncertainty as to whether the neoplasms should be classified as DLBCL, an accurate diagnosis was not made at the time. As the entity of FA-DLBCL is defined in the revised fourth edition of the WHO classification in 2017 as arising in the context of long-standing chronic inflammation and Epstein-Barr virus (EBV) infection, the slides were re-reviewed, and additional studies were conducted. Immunohistochemical study revealed that the atypical cells were positive for MUM1 and negative for CD10 and BCL6, consistent with the non-germinal center B-cell phenotype by the Hans classifier [8]. The Ki-67 proliferation rate was 85% (Fig. 2E), and in situ hybridization of EBV-encoded RNA was positive (Fig. 2F), but there was no staining for human herpesvirus 8. Finally, a diagnosis of FA-DLBCL was made, which was recently renamed FA-LBCL according to the fifth edition of the WHO classification. At the 7-year follow-up (October 2023), the patient exhibited no evidence of recurrence, although he received no further treatment except thrombectomy.
CASE REPORT
- In the novel fifth edition of the WHO classification, “FADLBCL” was modified to “FA-LBCL” for consistency by acknowledging that a diffuse growth pattern is not apparent. In addition, FA-LBCL, which has an indolent clinical outcome, is now separate from chronic inflammation-associated DLBCL, which is an aggressive tumor [2].
- Since the description of this entity is relatively recent, the overall incidence remains unclear. Approximately 50 to 60 cases of FA-LBCL have been reported in the English literature [1–7], and it has been described in cases throughout the body at sites of chronic fibrin deposition, including in the walls of pseudocysts (splenic, renal, adrenal, paratesticular, and ovarian teratomas), hydroceles, chronic subdural and testicular hematomas, breast implant capsules, materials located in the cardiovascular system (cardiac myxoma, cardiac prosthesis, cardiac fibrinous thrombus, and synthetic vascular grafts), and wear debris associated with metallic implants [1–7]. Although these lesions have been described in distinct locations, the histology is remarkably similar to atypical B cells embedded in a fibrinous background. Cardiac myxoma represents one of the most frequent sites of occurrence, with 16 cases identified, whereas only six cases of FA-LBCL arising in an endovascular graft have been reported prior to our study [3–6].
- The clinicopathologic features, which are based on the analysis of a relatively limited number of cases, remain poorly known. FALBCL does not exert a mass effect or infiltrate normal tissues. The majority of the cases is associated with excellent outcomes, regardless of therapy (surgery alone or chemotherapy), although several patients with primary cardiac or vascular diseases experienced recurrent or persistent disease compared to other sites that are more amenable to complete resection [6].
- Including the single case we describe, seven cases of FA-LBCL associated with endovascular grafts have been reported [4–6]. The clinicopathological features of these cases are summarized in Table 1. The patients’ ages ranged from 48 to 79 years, with an average age of 62 years. The cases have been reported in more men than women (male:female = 6:1). The mean duration of the time from endovascular graft to diagnosis was 7.9 years (range, 1 to 24 years). Although follow-up data are limited, patients who received no further therapy exhibited no evidence of disease recurrence. To our knowledge, the patient in the present case is the longest surviving case, at 7 years, even though he was not treated. The findings support that this type of lymphoma does not warrant excessive or unnecessary treatment after complete resection, with postoperative chemotherapy potentially being unnecessary. However, studies of additional cases of this rare entity are needed to support our findings.
- Since few cases of FA-LBCL have been described such as case reports and small series, the pathogenesis is not well-known. The presence of foreign material and associated chronic inflammation may be contributing factors in some cases [6]. A previous study reported that cytokines derived from the chronic inflammatory cells in the enclosed space allowed EBV-transformed B cells to evade T cell immune surveillance, resulting in a site-specific microenvironment that promoted the development of lymphoma [9]. EBV infection is strongly associated with FA-LBCL, as all cases with endovascular grafts were EBV-positive (Table 1). However, rare EBV-negative lymphoproliferations with features similar to those of typical FA-LBCL have also been described [7]. In addition, not all cases are associated with a foreign body, and the sparse inflammatory component in some cases argues against these features as unifying aspects underlying the pathogenesis [7]. No specific genetic abnormalities have been associated with FA-LBCL [3]. Therefore, further studies of more reported cases are required to identify the pathogenesis of this disease.
- We herein report the fortuitous discovery of a case of FA-LBCL after reviewing the slides again, as the disease concept was newly established. This case report aims to present the diagnostic challenge of an extremely rare case encountered in clinical practice. Although FA-LBCL does not exhibit mass-forming features with a paucity of neoplastic cells and was incidentally found in the pathologic examination of a thrombus, we would like to draw attention to this entity when observing homogeneous fibrinous materials. In addition, the initial diagnostic difficulty in this case was potentially related to multiple factors, mainly because the entity of FA-LBCL was not defined. Furthermore, it is difficult for a general pathologist not specialized in hematolymphoid pathology to be aware of a recently described, very rare disease entity such as FA-LBCL. With the constant discovery of new disease entities, it is necessary for pathologists to continue tracking unresolved cases to make accurate diagnoses, as a missed diagnosis could significantly impact clinical care.
DISCUSSION
-
Ethics Statement
The case report was approved by the Institutional Review Board of Dong-A University Hospital (DAUHIRB-22-083) and informed consent was waived.
-
Availability of Data and Material
The datasets generated or analyzed during this study was available from the corresponding authors on responsible request.
-
Code Availability
Not applicable.
-
Author Contributions
Conceptualization; MGP, MSR. Data curation: MGP, MSR. Investigation: MGP, MSR. Writing—original draft: MGP. Writing—review & editing: MSR. Approval of final manuscript: all authors.
-
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
-
Funding Statement
No funding to declare.
Notes


- 1. Swerdlow SH, Campo E, Harris NL, et al. WHO classification of tumours of haematopoietic and lymphoid tissues. Revised 4th ed. Lyon: IARC Press, 2017.
- 2. Alaggio R, Amador C, Anagnostopoulos I, et al. The 5th edition of the World Health Organization classification of haematolymphoid tumours: lymphoid neoplasms. Leukemia 2022; 36: 1720–48. PubMedPMC
- 3. WHO Classification of Tumours Editorial Board. WHO classification of tumors: thoracic tumours. 5th ed. Lyon: IARC Press, 2021.
- 4. Miller DV, Firchau DJ, McClure RF, Kurtin PJ, Feldman AL. Epstein-Barr virus-associated diffuse large B-cell lymphoma arising on cardiac prostheses. Am J Surg Pathol 2010; 34: 377–84. ArticlePubMed
- 5. Gruver AM, Huba MA, Dogan A, Hsi ED. Fibrin-associated large B-cell lymphoma: part of the spectrum of cardiac lymphomas. Am J Surg Pathol 2012; 36: 1527–37. PubMed
- 6. Boyer DF, McKelvie PA, de Leval L, et al. Fibrin-associated EBV-positive large B-cell lymphoma: an indolent neoplasm with features distinct from diffuse large B-cell lymphoma associated with chronic inflammation. Am J Surg Pathol 2017; 41: 299–312. PubMed
- 7. Di Napoli A, Soma L, Quintanilla-Martinez L, et al. Cavity-based lymphomas: challenges and novel concepts. A report of the 2022 EA4HP/SH lymphoma workshop. Virchows Arch 2023; 483: 299–316. ArticlePubMedPMCPDF
- 8. Hans CP, Weisenburger DD, Greiner TC, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 2004; 103: 275–82. ArticlePubMed
- 9. Loong F, Chan AC, Ho BC, et al. Diffuse large B-cell lymphoma associated with chronic inflammation as an incidental finding and new clinical scenarios. Mod Pathol 2010; 23: 493–501. ArticlePubMedPDF
References
Figure & Data
References
Citations

 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure

 E-submission
E-submission