Evaluation of urodynamic pattern in short and long-standing diabetic patients
Accepted: January 6, 2023
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
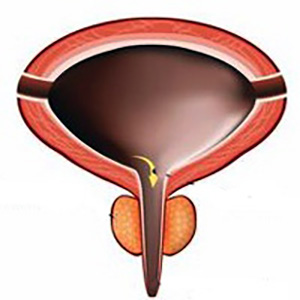
Purpose: To address the pattern of urodynamic findings in diabetic patients with lower urinary tract symptoms (LUTS), comparing short-standing and long-standing type 2 diabetes mellitus (T2DM).
Methods: A prospective study was conducted on 50 patients presenting with LUTS and a concurrent diagnosis of T2DM, between February 2016 and May 2018. Patients were classified and evaluated according to the duration of diabetes into two groups: short-standing DM (< 15 years, n = 31), and long-standing DM (≥ 15 years, n = 19) groups. The impact of LUTS and quality of life were assessed in female patients using ICIQ-FLUTS and male patients using ICIQ-MLUTS.
Results: A total of 50 patients were included in the study. The mean duration of T2DM was 10 ± 0.7 years. The mean age was 56.3 ± 1.2 years, and the mean HbA1c was 7.5 ± 1.2%. Urodynamic evaluation detected significantly higher detrusor overactivity (DO) and increased bladder sensation with the short-standing DM group (35.5 vs. 15.8%, p = 0.01 and 32.3 vs. 5.3%, p = 0.01, respectively). Comparatively, weak, or absent detrusor contractility were more frequent in patients with long-standing DM (52% and 26% respectively p = 0.01). As expected, overflow incontinence and straining during voiding were significantly higher in the long-standing DM group (p = 0.04 and p = 0.03, respectively). Surprisingly, there was no significant correlation between patients presenting with urgency in their voiding diary (subjective) and urodynamic detection of DO (p = 0.07).
Conclusions: There are different patterns in urodynamic characterizations of T2DM. Patients with short-standing DM present more commonly with storage symptoms and detrusor overactivity on urodynamics. Contrastingly, patients with long-standing DM present more frequently with voiding symptoms and detrusor underactivity on urodynamics. Thus, screening for an underactive bladder is advisable in patients with long-standing T2DM.
Bansal R, Agarwal MM, Modi M, et al. Urodynamic profile of diabetic patients with lower urinary tract symptoms: association of diabetic cystopathy with autonomic and peripheral neuropathy. Urology. 2011; 77:699-705.
Geerlings SE, Stolk RP, Camps MJ, et al. Diabetes Women Asymptomatic Bacteriuria Utrecht Study Group. Risk factors for symptomatic urinary tract infection in women with diabetes. Diabetes Care. 2000; 23:1737-41.
Lee WC, Wu HP, Tai TY, et al. Effects of diabetes on female voiding behavior. J Urol. 2004; 17:989-92.
Yuan Z, Tang Z, He C, Tang W. Diabetic cystopathy: a review. J Diabetes. 2015; 7:442-7.
Gomez CS, Kanagarajah P, Gousse AE. Bladder dysfunction in patients with diabetes. Curr Urol Rep. 2011; 12:419-26.
Chancellor MB. The overactive bladder progression to underactive bladder hypothesis. Int Urol Nephrol. 2014; 46(Suppl 1):S23.
Bolgeo T, Maconi A, Bertolotti M, et al. Physiopathology of the dia- betic bladder. Arch Ital Urol Androl. 2020; 92:314.
Majima T, Matsukawa Y, Funahashi Y, et al. Urodynamic analysis of the impact of diabetes mellitus on bladder function. Int J Urol. 2019; 26:618-622.
Jackson S, Donovan J, Brookes S, et al. The Bristol Female Lower Urinary Tract Symptoms questionnaire: development and psychometric testing. Br J Urol. 1996; 77:805-12.
De Ridder D, Roumeguère T, Kaufman L. Urgency and other lower urinary tract symptoms in men aged ≥ 40 years: a Belgian epi- demiological survey using the ICIQ-MLUTS questionnaire. Int J Clin Pract. 2015; 69:358-65.
Capon G, Caremel R, de Sèze M, et al. The impact of mellitus diabetes on the lower urinary tract: A review of Neuro-urology Committee of the French Association of Urology. Prog Urol. 2016; 26:245-53.
Daneshgari F, Moore C. Diabetic uropathy. Semin Nephrol. 2006; 26:182-5.
Kaplan SA, Te AE, Blaivas JG. Urodynamic findings in patients with diabetic cystopathy. J Urol. 1995; 153:342-4.
Kebapci N, Yenilmez A, Efe B, et al. Bladder dysfunction in type 2 diabetic patients. Neurourol Urodyn. 2007; 26:814-9.
Yamaguchi C, Sakakibara R, Uchiyama T, et al. Overactive bladder in diabetes: a peripheral or central mechanism? Neurourol Urodyn. 2007; 26:807-13.
Malik RD, Cohn JA, Volsky J, et al. A Modern Comparison of Urodynamic Findings in Diabetic Versus Nondiabetic Women. Female Pelvic Med Reconstr Surg. 2020; 26:44-50.
Shin YS, On JW, Kim MK. Clinical significance of diabetes melli- tus on detrusor functionality on stress urinary incontinent women without bladder outlet obstruction. Int Urogynecol J. 2016; 27:1557-61.
Esteghamati A, Rashidi A, Nikfallah A, Yousefizadeh A. The association between urodynamic findings and microvascular complications in patients with long-term type 2 diabetes but without voiding symptoms. Diabetes Res Clin Pract. 2007; 78:42-50.
Hill SR, Fayyad AM, Jones GR. Diabetes mellitus and female lower urinary tract symptoms: a review. Neurourol. Urodyn. 2008; 27:362-7.
Copyright (c) 2023 the Author(s)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.


 https://doi.org/10.4081/aiua.2023.11072
https://doi.org/10.4081/aiua.2023.11072



