JOURNAL OF INFECTIOUS DISEASES & MICROBIOLOGY
On this page
Dietary Habits and Gut Microbiome: An Influence on Gut Brain Axis
Sanjana Bhat, Gyan Vandana Yadav*, Kirty Rani, Suman Dhayal and Meenal Rehman
Department of Microbiology, Jaipur National University, Jaipur Jagatpura, Rajasthan, India
*Corresponding Author: Gyan Vandana Yadav, Department of Microbiology, Jaipur National University, Jaipur Jagatpura, Rajasthan, India.
| ReceivedAug 9, 2023 | RevisedAug 20, 2023 | AcceptedAug 24, 2023 | PublishedSep 3, 2023 |
Abstract
Intimate connections between the brain and the human gut provide a system of neurohumoral communication that may exist both ways. The link between the GI tract and the brain is so effectively-established that the central nervous system's health is always correlated with how well the gut performs. The majority of research on the gut-brain axis focuses on how mental health influences how effectively the GI system works. Recent research, however, suggests that the gut flora communicates with the brain via this axis to govern phenotypic alterations in the brain and behavior. The involvement of the microbes found in the stomach in the gut-brain axis is a significant breakthrough in identifying precise differences of the microbiota in the gut microbial constitution. However, because to the large number of intestinal bacteria and the difficulties associated with cultivating gut microbes, identifying the microbes that form the gut microbiota has emerged as the most serious scientific issue today. The current methods for identifying the microorganisms that comprise the gut microbiota rely heavily on emerging technologies and omics research techniques. In this article, we focus on the relationship between an individual's gut microbiota and the link between the gut and the brain, and we also consider the benefits and drawbacks of the present technology with high throughput for identifying the bacteria that together make up the gut microbiota, in order to further comprehend the role of gut microbiota in the gut-brain axis. The relationship between the gut and the brain is the topic of this review. The narrative overview explores the relevant scientific literature to provide a comprehensive account of this extensive concern.
Keywords
Gut brain axis; Microbiome; Diet; Signaling; Human gut; Nutrition; Gut brain interaction
Introduction
The gut controls both the digestive and immune systems, and it frequently maintains an array of microbe ecology. The gut microbiota regulates the advancement and functioning of the immunological, metabolic, and neurological systems in collaboration with the host [1].
It has the ability to influence both intestinal and extra intestinal organ disease processes, as well as those in the brain. The gut connects with the central nervous system via dynamic, bidirectional communication along the gut-brain axis. The connection between the brain and the gut may have a clear impact on the host's behavior and state of mind. Several brain diseases have been linked to microbial ecosystem deviations [1,2].
All of the layers of the gut mucosa act as an effective barrier against damaging luminal substances. Pluripotent intestinal stem cells (ISCs) near the base of the crypt constantly replace the intestinal epithelium. To prevent microbial invasion, secretory epithelial cells create a mucous physicochemical barrier [3]. This barrier contains antimicrobial peptides. The junctions that link the intestinal epithelial cells together tightly. An immune surveillance mechanism located under the gut epithelium finally fights off outside invaders. Few cases have been seen where human gut microbes gradually colonies shortly after birth [4]. The difference between caesarean section and normally born babies' gut bacterial numbers at one month of age. It's likely to be found that the oral microbial community affects intestinal complications, despite the fact that there hasn't been enough research to demonstrate a link between the microbial ecology of the mouth space and the intestinal system [5]. The study of the mouth-gut microbiome axis and the changes in microbial composition between healthy individuals and patients with oral health conditions are thus of great significance.
Abnormal calorie consumption and inactivity are linked to obesity. Any changes in microbial communities linked to obesity may be greatly impacted by exercise [6]. Thus, an increase in the diversity of gut microbial populations in elite performers in response to exercise and the accompanying diet highlights this. Stress is another lifestyle factor that affects colonic movement by affecting the gut-brain axis. This can change the profiles of the gut microbiota, particularly the proportion of potentially beneficial Lactobacillus that is present [7,8]. The central nervous system (CNS) may be involved in IBS, one of the most common functioning bowel diseases, and the changes in bacterial populations that accompany it [9]. Because the hormones and neuronal networks that comprise the interaction between the gut and the brain are reversible, changes in the gut microbiota may have an effect on brain function, particularly mood. A neurological disease called autism is found to be linked to major differences in the composition of the gut microbiome [10]. Different microbe-produced enzymes regulate digestion and health. Indeed, many of the different microorganisms in the human gut may be attributed to the multitude of microbial enzymes required to break down nutrients, particularly the different kinds of complex polysaccharides consumed by humans [11]. Gut microbes can produce a wide range of products, and the availability of nutrients and the luminal atmosphere, specifically pH, may influence the synthesis of these products [12,13]. The influence of nutrition and other environmental factors on the composition and metabolism action of the microbiota of the gut, which can have an immediate influence on wellness, is becoming more widely acknowledged [14,15].
Gut brain axis
The connection between the brain and the gut is a communication network across the gastrointestinal tract and brain. Both physically and biochemically, there are multiple relationships involving these two parts. Neurons are cells in your brain and central nervous system that give instructions to your body on how to respond. On average, the human brain has 100 billion neurons. The fact that 500 million of your gut's neurons communicate with your brain through nerves in your nervous system is significant [16,17]. Vagus nerve, that transmits and receives messages, is one of the major nerves that connect your gut to your brain. Your mind and intestines have a connection through a family of chemicals called neurotransmitters. Neurotransmitters are chemicals made by the brain that control emotions and sensory perceptions. In this regard, the neurotransmitter serotonin boosts feelings of pleasure while it also helps in the regulation of your biological clock. It's important to note that many of these neurotransmitters also originate from the countless numbers of microbes that reside in the gut [18].
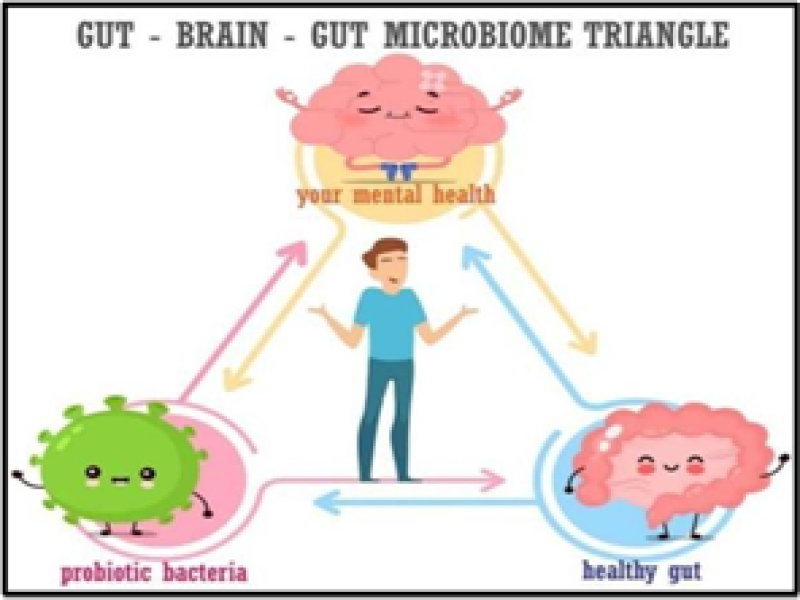
Figure 1: Shows a diagrammatical representation.
Diet can influence the brain through a variety of processes
The significance of adequate vitamins and minerals for a healthy brain's growth, in addition to the link between deficiency in nutrition in adolescence and decreased functioning of the brain, has long been established. Molecules of nourishment that are too large to be absorbed intact in the proximate gut and whose absorption is mostly dependent on bacteria from the gut metabolic in the small intestine and colon at the distal end have piqued the curiosity of researchers20 [21]. Until recently, the majority of study has been on dietary components such amino acids and micronutrients that are completely absorbed in the proximal small intestine. The ability of these non-digestible ingredients in food to improve wellness is critically dependent on the composition and functioning of the gut bacteria.
Food intake and its influence on gut-brain axis
A few specific dietary categories are particularly good for the connection between gut and brain. Some of the most significant ones are listed below:
- Omega-3 fats: These fats are abundant in the human brain and can be found in fatty seafood. Studies on both humans and animals have shown that omega-3s can boost the growth of useful bacteria in the gut and lower the chance of developing brain problems [22].
- Fermented foods: Lactic acid-producing bacteria are present in cheese, yogurt, sauerkraut, and other fermented foods. There are strong evidences that justifies eating fermented foods develops brain activity [23].
- High-fiber foods: Prebiotic fibers are healthy for your gut flora and can be found in whole grains, nuts, seeds, fruits, and vegetables. Prebiotics can lower stress hormone levels in people [24].
- Foods high in polyphenols: Include cocoa, green tea, olive oil, and coffee. Polyphenols are plant compounds that your gut flora breakdown. Polyphenols boost beneficial gut flora and may enhance mental function [22].
- Foods high in tryptophan: Tryptophan is an amino acid that is turned into serotonin, a neurotransmitter. Tryptophan-rich foods include turkey, eggs, and cheese [25].
Factors affecting gut-brain axis
The microbiota and its impact on the gut-brain axis can be influenced by a number of factors, including nutrition, genetics, the delivery method used during childbirth, stress, sleep, and drugs. Intestinal bacteria, which have evolved with ways of communicating with human organ systems, greatly impact the gut-brain axis.
Brain chemicals like serotonin, altered permeability in the intestinal tract, regulated immunology, and the synthesis of bacterial molecules by gut microbes can all have an impact within the gut-brain axis. Gut microbes have been studied. Scientifically found to influence early central and enteric nervous system development in neonates. Infection, pain, inflammation, and mother-child separation are examples of stressful or detrimental early life experiences that might alter the composition of the gut microbiota and the regulation of the gut-brain axis later in life. According to a number of studies, long-term antibiotic usage, which can alter the structure of the microbiota in one's gut, can be altered. Exacerbate the symptoms of anxiety and depression. Researchers have found links between the gut microbiome and autism spectrum disorder (ASD), and also have discovered that some bacterial strains emit chemicals that affect social development and brain function [26-28]. Lab animals with ASD-like symptoms lack specific bacterial strains, and children with ASD have a distinct mix of germs from other kids. Depending on the makeup of the foods we eat, the microbial composition of the gut may fluctuate. As opposed to starch and sugar-rich diets, which provide both good and harmful bacteria with energy, foods high in dietary fiber and prebiotics can favor particular types of helpful bacteria. Salt, lipids, and proteins all have an impact on the gut flora. Even individuals who consumed only animal products had very different microbiomes than those who only consumed plant products, according to a study. According to research, eating just animal products caused microbial changes in the gut that may have an impact on the onset of inflammatory bowel disease in people [18]. The gut-brain axis is a bidirectional communication system between the gastrointestinal tract (the gut) and the central nervous system (the brain). It involves complex interactions between various components, including neurotransmitters, hormones, immune cells, and the gut microbiota. Glutamate and norepinephrine (NE) are two important factors involved in the gut-brain axis. Glutamate signaling is involved in transmitting signals from the gut to the brain and vice versa which plays a role in influencing mood, emotions, and responses to stress. Whereas stress induced release of NE influences gut permeability and thus this shows it’s affected also on the composition and activity of the gut microbiota. Similarly, in turn, microbes affect NE levels, creating a bidirectional relationship between NE and the gut microbiota. Both glutamate and NE contribute to the complex interactions that occur between the gut and the brain. Dysregulation of these neurotransmitters can contribute to gastrointestinal disorders, mood disorders, and other conditions.
Sustainability of gut microbes due to changes in gut-brain interaction
The sustainability of gut microbes is essential for overall health as these microorganisms play key roles in nutrient metabolism, immune function, and protecting against pathogens. Dysbiosis, defined as an imbalance in the gut microbial community, has been linked to a variety of health problems, including gastrointestinal illnesses, disorders of metabolism, as well as specific psychological disorders. To promote the sustainability of gut microbes, it's essential to prioritize factors that positively have an impact on the relationship between brain and gut. This includes managing stress, adopting a balanced and nutritious diet, avoiding unnecessary antibiotic use, engaging in regular physical activity, and ensuring adequate sleep. By taking care of the gut- brain axis, individuals can support a healthy and diverse gut microbial community, which in turn contributes to overall well-being [29-31]. However, it's worth noting that individual responses may vary, and the field of gut microbiota research is continually evolving.
Psychometric effects of gut and brain signaling
The psychometric consequences of the gut and the brain transmission, also known as the gut- brain bidirectional interaction, are a new area of study that looks into the gastrointestinal tract and the central nervous system, which consists of the cerebral cortex, have the bilateral connection. Various channels, including neurological, hormonal, and immunological processes, enable this communication [16,32]. The connection involving the digestive tract and brain is now recognized as an important regulator of not just gastrointestinal functions but also elements of mental health, mental processes, and personality.
Here are some of the psychometric effects associated with gut-brain signaling:
1. Emotional Regulation and Mood: The gut-brain axis regulates mood and emotional regulation. The microbiota in the gastrointestinal tract produces neurotransmitters such as dopamine, serotonin, serotonin and gamma-amino butyric acid (GABA), which are necessary for emotions and the state of mind control. Changes in gut microbial composition might influence neurotransmitter production and availability, potentially affecting mood and psychological health [33].
2. Stress Response: The gut and the brain bidirectional connection are closely involved in the body's stress response. Chronic stress can lead to alterations in gut microbial diversity and function, which, in turn, may affect stress-related behaviors and susceptibility to stress-induced mood disorders.
3. Anxiety and Depression: There is growing evidence linking gut dysbiosis to anxiety and depression. In both the animal and human research, imbalances in the intestinal microbiota have been linked to depression and anxious symptoms.
4. Cognition and Brain Function: The association between the gut and has the potential to alter mental processes and brain function. Metabolites produced by the bacteria that make up the gut can affect the functioning of neurons and brain functioning, potentially affecting cognitive abilities such as recall, focus, and remembering.
5. Neuro developmental Disorders: Research suggests that disruptions in the gut-brain axis during early development may be linked to the development of neurodevelopment disorders such as autism spectrum disorders.
6. Brain Disorders and Neuro inflammation: Various neurological illnesses, including Parkinson's disease and multiple sclerosis, are believed to be correlated to an imbalance of the gastrointestinal tract. Inflammation of the brain that has been scientifically linked to a number of brain disorders is another aspect of the gut-brain axis.
7. Psychiatric Disorders: The axis that connects gut and brain is being investigated as a possible component in the emergence and evolution of psychiatric diseases like schizophrenic and bipolar disorder [34,35].
It's essential to keep in mind that the gut-brain axis is a complex, dynamic system that is continuously being addressed. Even while there is emerging evidence that gut-brain signaling plays a part in cognitive outcomes, specific mechanisms and specific associations are still being explored. The modulation of the gut-brain axis is now considered a potential target for therapeutic interventions aimed at improving mental health and cognitive function.
Diet, exercise, and stress management are examples of lifestyle factors that might alter gut microbial composition and function, and so have consequences for psychological well-being. Additionally, probiotic and prebiotic therapies are being investigated as a way to positively alter the gut microbiome and perhaps enhance emotional outcomes. As the research progresses, a deeper understanding of the gut-brain axis and its psychometric effects may lead to novel and personalized approaches to promote mental health and well-being [12,36].
Discussion
A balanced diet rich in a variety of nutrient-dense foods can have a positive impact on the composition and interaction of gut microbes. This, in turn, can contribute to overall health, proper nutrient absorption, immune function, and even mental well-being. A balanced diet that includes a variety of whole foods such as fruits, vegetables, whole grains, lean proteins, and healthy fats can promote a diverse gut microbiota [37]. Different types of dietary fiber, for instance, serve as a source of nutrients for certain beneficial bacteria in the gut, promoting the growth and diversity. Whereas, in context to the high fat intake, the microbial diversity might be reduced due to host mucosal-microbe interaction. Mucosal microbe symbiosis refers to the mutually beneficial relationship between the host and the resident microbes in mucosal tissues. These microbes help regulate the immune system, maintain the integrity of the mucosal barrier, and prevent colonization by harmful pathogens.
This symbiotic relationship is crucial for the overall health and proper functioning of the host organism. This could alter the brain signalling and trigger immunity by rendering activation of microglia and astrocytes [38,39].
The gut microbiota can produce metabolites and bioactive compounds that influence neurotransmitter production, immune responses, and inflammation. These substances can affect brain function and behavior. For example, certain gut microbes produce neurotransmitters like serotonin, which is often referred to as the "feel-good" neurotransmitter and has an impact on mood regulation.
Conclusion
It is impossible to overestimate the relevance of nutrition in the gut-brain axis. Diet regulates the makeup and function of the gut microbiota, which impacts brain health and function via a complex bidirectional communication system. The link that exists between the alimentary tract and the central nervous system, termed as the "gut-brain axis," is dynamic and significant. It influences several aspects of mental and emotional health [39].
A diversified and balanced gut flora is facilitated by a diet high in fiber, fruits, vegetables, and probiotics that highlights nutrient-dense, whole foods. The improvement of overall health, including mental and emotional well-being, has been correlated with this microbial diversity. On the other side, eating a lot of processed foods, refined sugars, and unhealthy fats can lead to inflammation in the stomach, microbial imbalances, and a higher risk of mental health problems. Diet affects neurotransmitter synthesis, the body's response to stress, cognitive function, and even neuroplasticity-the brain's potential for change-through the gut-brain axis. Neuroinflammation, which is related to brain illnesses and cognitive decline, is also impacted by it. Early dietary influences are essential for healthy neurodevelopment, making a balanced diet during key growth phases necessary for the optimal possible cognitive and behavioral outcomes [40].
As the understanding of the gut-brain axis deepens, it becomes clear that the choices we make regarding the diet can profoundly impact the mental well-being and cognitive abilities. By adopting a diet that supports a healthy gut-brain axis, individuals can take proactive steps towards promoting better mental health, emotional balance, and overall brain function. Other factors like stress, sleep, physical activity, and genetics also play roles. However, a balanced diet provides a solid foundation for supporting both gut health and brain function, contributing to an overall sense of well-being. Ultimately, prioritizing a nutritious and balanced diet is a key factor in maintaining a harmonious and thriving relationship between the gut and the brain interaction.
Acknowledgments
None.
Conflict of interest
No conflict of interest.
Funding
None.
Ethics statement
Not applicable.
Author's contribution
All of the authors named have made a significant, direct, and intellectual contribution to the work and have given their permission for it to be published.
References
1. Chunduri A, Reddy SD, Jahanavi M, Reddy CN. Gut-Brain Axis, Neurodegeneration and Mental Health: A Personalized Medicine Perspective. Indian J Microbiol. 2022;62(4):505-15. PubMed | CrossRef
2. Khan T, Khanna P, Pangasa N. Gut Brain axis: The Gut Microbiome in Peri-Operative Medicine. Indian J Anaesth. 2023;67(2):235-6. PubMed | CrossRef
3. McQuaid S, Cunnea P, McMahon J, Fitzgerald U. The Effects of Blood–Brain Barrier Disruption on Glial Cell Function in Multiple Sclerosis. Biochem Soc Trans. 2009;37(1):329-31. PubMed | CrossRef
4. Majumdar A, Siva Venkatesh IP, Basu A. Short-Chain Fatty Acids in the Microbiota–Gut–Brain Axis: Role in Neurodegenerative Disorders and Viral Infections. ACS Chem Neurosci. 2023;14(6):1045-62. PubMed | CrossRef
5. Balasubramanian R, Bazaz MR, Pasam T, Sharief N, Velip L, Samanthula G, et al. Involvement of Microbiome Gut–Brain AxisiIn Neuroprotective Effect of Quercetin in Mouse Model of Repeated Mild Traumatic Brain Injury. Neuromolecular Med. 2022:1-3. PubMed | CrossRef
6. Narengaowa, Kong W, Lan F, Awan UF, Qing H, Ni J. The Oral-Gut-Brain AXIS: The Influence of Microbes in Alzheimer’s Disease. Front Cell Neurosci. 2021;15:633735. PubMed | CrossRef
7. Kaur H, Bose C, Mande SS. Tryptophan Metabolism by Gut Microbiome and Gut-Brain-Axis: An In-Silico Analysis. Front Neurosci. 2019;13:493713. PubMed | CrossRef
8. Torres-Fuentes C, Schellekens H, Dinan TG, Cryan JF. The Microbiota–Gut–Brain Axis in Obesity. Lancet Gastroenterol Hepatol. 2017;2(10):747-56. PubMed | CrossRef
9. Stasi C, Sadalla S, Milani S. The Relationship between the Serotonin Metabolism, Gut-Microbiota and The Gut-Brain Axis. Curr Drug Metab. 2019;20(8):646-55. PubMed | CrossRef
10. Lee Y, Kim YK. Understanding the Connection between the Gut–Brain Axis and Stress/Anxiety Disorders. Curr Psychiatry Rep. 2021;23:1-7. PubMed | CrossRef
11. Liu Y, Sanderson D, Mian MF, Neufeld KA, Forsythe P. Loss of Vagal Integrity Disrupts Immune Components of the Microbiota-Gut-Brain Axis and Inhibits the Effect of Lactobacillus Rhamnosus on Behavior and the Corticosterone Stress Response. Neuropharmacology. 2021;195:108682. PubMed | CrossRef
12. Zhu S, Jiang Y, Xu K, Cui M, Ye W, Zhao G, et al. The Progress of Gut Microbiome Research Related to Brain Disorders. J Neuroinflammation. 2020;17:1-20. PubMed | CrossRef
13. Oriach CS, Robertson RC, Stanton C, Cryan JF, Dinan TG. Food For Thought: The Role of Nutrition in the Microbiota-Gut–Brain Axis. Clin Nutr Exp. 2016;6:25-38. CrossRef
14. Mayer EA, Knight R, Mazmanian SK, Cryan JF, Tillisch K. Gut Microbes and the Brain: Paradigm Shift in Neuroscience. J Neurosci. 2014;34(46):15490-6. PubMed | CrossRef
15. Gwak MG, Chang SY. Gut-Brain Connection: Microbiome, Gut Barrier, and Environmental Sensors. Immune Netw. 2021;21(3). PubMed | CrossRef
16. Shreiner AB, Kao JY, Young VB. The Gut Microbiome in Health and in Disease. Curr Opin Gastroenterol. 2015;31(1):69. PubMed | CrossRef
17. Carabotti M, Scirocco A, Maselli MA, Severi C. The Gut-Brain Axis: Interactions between Enteric Microbiota, Central and Enteric Nervous Systems. Ann Gastroenterol. 2015;28(2):203. PubMed
18. Gao W, Baumgartel KL, Alexander SA. The Gut Microbiome as a Component of the Gut–Brain Axis in Cognitive Health. Biol Res Nurs. 2020;22(4):485-94. PubMed | CrossRef
19. Fowlie G, Cohen N, Ming X. The Perturbance of Microbiome and Gut-Brain Axis in Autism Spectrum Disorders. Int J Mol Sci. 2018;19(8):2251. PubMed | CrossRef
20. Dumitrescu L, Popescu-Olaru I, Cozma L, Tulbă D, Hinescu ME, Ceafalan LC, et al. Oxidative Stress and The Microbiota-Gut-Brain Axis. Oxid Med Cell Longev. 2018;2018. PubMed | CrossRef
21. Hillestad EM, van der Meeren A, Nagaraja BH, Bjørsvik BR, Haleem N, Benitez-Paez A, et al. Gut Bless You: The Microbiota-Gut-Brain Axis in Irritable Bowel Syndrome. World J Gastroenterol. 2022;28(4):412. PubMed | CrossRef
22. Ding M, Lang Y, Shu H, Shao J, Cui L. Microbiota–Gut–Brain Axis and Epilepsy: A Review on Mechanisms and Potential Therapeutics. Front Immunol. 2021;12:742449. PubMed | CrossRef
23. Deng Y, Zhou M, Wang J, Yao J, Yu J, Liu W, et al. Involvement of the Microbiota-Gut-Brain Axis in Chronic Restraint Stress: Disturbances of the Kynurenine Metabolic Pathway in Both the Gut and Brain. Gut Microbes. 2021;13(1):1869501. PubMed | CrossRef
24. Chen LM, Bao CH, Wu Y, Liang SH, Wang D, Wu LY, et al. Tryptophan-Kynurenine Metabolism: A Link Between the Gut and Brain for Depression in Inflammatory Bowel Disease. J Neuroinflammation. 2021;18(1):1-3. PubMed | CrossRef
25. Góralczyk-Bińkowska A, Szmajda-Krygier D, Kozłowska E. The Microbiota–Gut–Brain Axis in Psychiatric Disorders. Int J Mol Sci. 2022;23(19):11245. PubMed | CrossRef
26. Zhao Z, Ning J, Bao XQ, Shang M, Ma J, Li G, et al. Fecal Microbiota Transplantation Protects Rotenone-Induced Parkinson’s Disease Mice Via Suppressing Inflammation Mediated by The Lipopolysaccharide-TLR4 Signaling Pathway through the Microbiota-Gut-Brain Axis. Microbiome. 2021;9(1):1-27. PubMed | CrossRef
27. Ancona A, Petito C, Iavarone I, Petito V, Galasso L, Leonetti A, et al. The Gut–Brain Axis in Irritable Bowel Syndrome and Inflammatory Bowel Disease. Dig Liver Dis. 2021;53(3):298-305. PubMed | CrossRef
28. Zhu F, Tu H, Chen T. The Microbiota–Gut–Brain Axis in Depression: The Potential Pathophysiological Mechanisms and Microbiota Combined Antidepression Effect. Nutrients. 2022;14(10):2081. PubMed | CrossRef
29. Honarpisheh P, Bryan RM, McCullough LD. Aging Microbiota-Gut-Brain Axis in Stroke Risk and Outcome. Circ Res. 2022;130(8):1112-44. PubMed | CrossRef
30. Wachsmuth HR, Weninger SN, Duca FA. Role of The Gut–Brain Axis in Energy and Glucose Metabolism. Exp Mol Med. 2022;54(4):377-92. PubMed | CrossRef
31. Tan AH, Lim SY, Lang AE. The Microbiome–Gut–Brain Axis in Parkinson Disease—From Basic Research to the Clinic. Nat Rev Neurol. 2022;18(8):476-95. PubMed | CrossRef
32. Yu Z, Wang Y, Yu Z, Lu M, Xu B. Crosstalk Between Adipose Tissue and The Microbiota-Gut-Brain Axis in Metabolic Diseases. International Int J Biol Sci. 2022;18(4):1706. PubMed | CrossRef
33. Chen M, Ruan G, Chen L, Ying S, Li G, Xu F, et al. Neurotransmitter and Intestinal Interactions: Focus on The Microbiota-Gut-Brain Axis in Irritable Bowel Syndrome. Front Endocrinol (Lausanne). 2022;13:817100. PubMed | CrossRef
34. Ribeiro FM, Silva MA, Lyssa V, Marques G, Lima HK, Franco OL, et al. The Molecular Signaling of Exercise and Obesity in The Microbiota-Gut-Brain Axis. Front Endocrinol (Lausanne). 2022;13:927170. PubMed | CrossRef
35. Dong S, Sun M, He C, Cheng H. Brain-Gut-Microbiota Axis in Parkinson’s Disease: A Historical Review and Future Perspective. Brain Res Bull. 2022;183:84-93. PubMed | CrossRef
36. Sittipo P, Choi J, Lee S, Lee YK. The Function of Gut Microbiota in Immune-Related Neurological Disorders: A Review. J Neuroinflammation. 2022;19(1):1-7. PubMed | CrossRef
37. Bi C, Guo S, Hu S, Chen J, Ye M, Liu Z. The Microbiota–Gut–Brain Axis and its Modulation in the Therapy of Depression: Comparison of Efficacy of Conventional Drugs and Traditional Chinese Medicine Approaches. Pharmacol Res. 2022:106372. PubMed | CrossRef
38. Daniel N, Lécuyer E, Chassaing B. Host/Microbiota Interactions in Health and Diseases-Time for Mucosal Microbiology. Mucosal Immunol. 2021;14(5):1006-16. PubMed | CrossRef
39. Dowling LR, Strazzari MR, Keely S, Kaiko GE. Enteric Nervous System and Intestinal Epithelial Regulation of The Gut-Brain Axis. J Allergy Clin Immunol. 2022;150(3):513-22. PubMed | CrossRef
40. Tahmasian M, Samea F, Khazaie H, Zarei M, Kharabian Masouleh S, Hoffstaedter F, et al. The Interrelation of Sleep and Mental and Physical Health is Anchored in Grey-Matter Neuroanatomy and Under Genetic Control. Commun Biol. 2020;3(1):171. PubMed | CrossRef
Sanjana Bhat, Gyan Vandana Yadav*, Kirty Rani, Suman Dhayal and Meenal Rehman
Department of Microbiology, Jaipur National University, Jaipur Jagatpura, Rajasthan, India
*Corresponding Author: Gyan Vandana Yadav, Department of Microbiology, Jaipur National University, Jaipur Jagatpura, Rajasthan, India.
Copyright© 2023 by Bhat S, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Bhat S, Yadav GV, Rani K, Dhayal S, Rehman M. Dietary Habits and Gut Microbiome: An Influence on Gut Brain Axis. J Infect Dis Microbiol. 2023; 1(3):25-34. DOI: https://doi.org/10.37191/Mapsci-JIDM-1(3)-014
