JOURNAL OF DENTAL REPORTS
The Use of a Synthetic Putty Graft in Extraction Sockets Combined with Immediate Implant Installation: 3 Cases
Maarten J Boogaard1* and Curd M L Bollen2
1Private Practice, Churchill-laan 162hs, 1078 ER, Amsterdam, The Netherlands
2College of Medicine & Dentistry, Ulster University, Birmingham, UK, Lead Advanced Implant Diploma, Tipton Training, Manchester, UK
*Corresponding Author: Maarten J Boogaard, Private Practice, Churchill-laan 162hs, 1078 ER, Amsterdam, The Netherlands.
| ReceivedJan 15, 2022 | RevisedJan 31, 2022 | AcceptedFeb 28, 2022 | PublishedMar 15, 2022 |
Abstract
In these three different cases, synthetic putty graft material has proven to be a reliable alternative to autologous bone for implant placement, directly into the anterior extraction socket of the maxilla. This study presents three different patients who require implants in the anterior maxilla. Immediate implant placement was the treatment solution of choice. Because the aesthetic expectations and the initial screw-in torque are different however, a differentiation between direct loading, a phase 1 or a phase 2 approaches was made. Clinical results show that synthetic putty is an effective alternative to transplantations with xenograft or allogeneic graft materials in single-phase, two-phase, and direct loading.
Keywords
Implant placement; Bone graft; Synthetic putty; Immediate loading; Extraction socket
Introduction
In the 1980s, implant placement in the extraction socket after tooth extraction was introduced [1]. For over 20 years, clinical protocols for the immediate placement of anterior implants in recent extraction sockets have evolved from a two-step protocol to a one-step, often even flapless. In some cases, even immediate provisional restorations may be placed in the same appointment [2]. Most changes in the contour of the alveolar ridge occur in the first 12 months after tooth extraction. These changes are primarily horizontal. They are also more prominent on the buccal side than on the lingual surface [3]. The buccal bone plate is more easily absorbed than the lingual plate due to its limited thickness [4]. CT scans of 250 patients showed that the thickness of the anterior facial plate was between 0.31mm-1mm. 50% of the wall thickness is even thinner than 0.5mm. These results suggest that extraction of the maxillary anterior teeth results in many patients in the loss of the entire buccal plate [5]. Implant location, buccal crest width, and horizontal buccal gap size can have a significant impact on changes in the alveolar crest after tooth extraction [6]. Simply placing the implant in a new extraction socket does not prevent bone remodelling. However, filling the gap between the extraction socket wall and the implant with a mineralized collagenous bone substitute creates an additional amount of hard tissue at the socket entrance. This minimal graft improves the level of contact between the marginal bone and the implant [7]. Immediate loading is possible: the temporary crown should not interfere with the implant's osseointegration when the load is properly adjusted. In addition, the implant must have sufficient primary stability [8]. Synthetic putty graft material can also be used to fill this buccal void. The putty applied in this case series consists of calcium phosphate silicate encapsulated in a carrier. It is a bioactive regenerative material that not only acts as a bone conduction scaffold, but also interacts with surrounding tissues and mediates bone stimulating effects [1]. The material is ready to use and has a temporary haemostatic effect. It has optimal retention and can be directly adapted to the shape of defects [9]. Studies show that 80-90% of the material is reabsorbed within 4-6 months of application. In the meantime, bone regeneration occurs. Putty has been clearly demonstrated to regenerate new bone when used in socket transplants, periodontal defect transplants, or maxillary sinus elevations [10-14].
Materials and Methods
Three patients were selected for this case series. Their age raged between 60 and 79 years. The 3 patients were randomly divided into the 3 different treatment concepts: 1 patient received the immediate loading protocol, 1 patient the 1-stage approach, and 1 patient the 2-stage approach. All patients received 2 g of amoxicillin and 600 mg of ibuprofen 1 hour before surgery. They were also asked to rinse with chlorhexidine mouthwash for 60 seconds before surgery. Surgery was performed using a local anaesthetic (UltracainDS Forte). The concept of Goené and van Daelen was followed [15]. When considering immediate implant placement, flapless non-traumatic extraction is essential for maxillary anterior teeth. After removal of the tooth, the integrity of the extraction socket should be investigated with a periodontal probe (Figure 1 a,b).
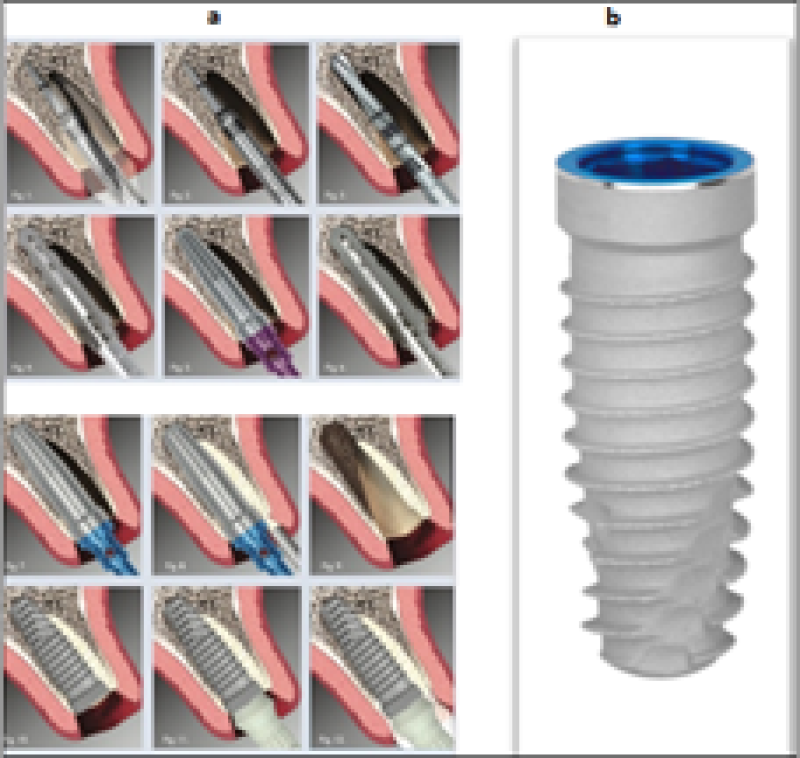
Figure 1: (a) Schematic overview of the Goene; (b) & van Daelen protocol-Biomet 3i T3 implant.
After the osteotomy preparation, a direction indicator was placed into the osteotomy. In the 3 cases NovaBone® putty 0.25ml (NovaBone® Dental Putty, Jacksonville, FL, USA) was added as graft material in de open gap between the extraction socket wall and the direction indicator (Figure 2 a,b).
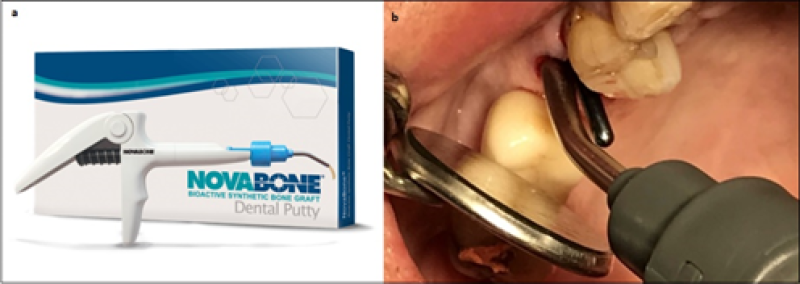
Figure 2: (a) Novabone;(b) Application of the synthetic putty.
Afterwards, a T3 Biomet3i® implant (Biomet3i®, West Palm Beach, Florida, USA) was installed. These T3 implants utilize Osseotite® surface technology on their coronal side. In a five-year study, double-etched surfaces of Osseotite® implants showed no increased risk of peri-implantitis or soft tissue complications compared to machined surfaces [16].
Finally, a PEEK temporary abutment (Biomet3i®, West Palm Beach, Florida, USA) was inserted for the immediate loading with a temporary crown, made of bisacryl composite (Protemp3®, 3M ESPE, Seefeld, Germany) (Figure 3). The 2 other cases got a delayed loading and a further standard implant restoration protocol.
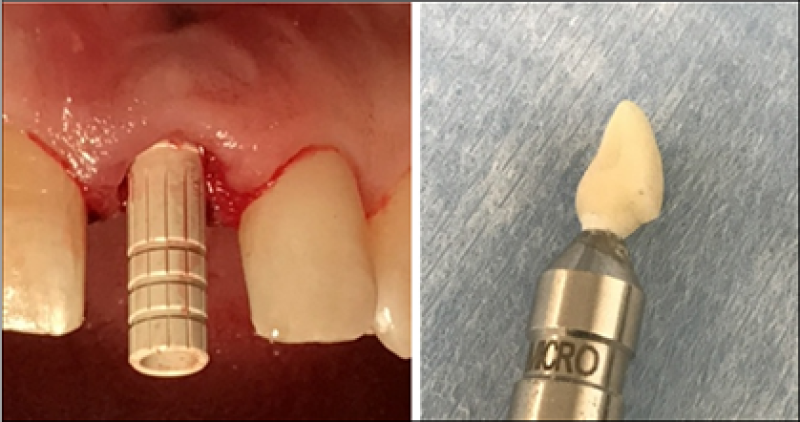
Figure 3: PEEK temporary abutment in place and temporary crown.
Results
Immediate loading
A 60-year-old healthy woman presented with a broken 21. She was a non-smoker. The tooth had an endodontic treatment more than 20 years ago. An apex resection was performed 5 years ago after recurrent infection. Scar tissue is clearly visible on the surrounding gingiva. (Figure 4 a,b).
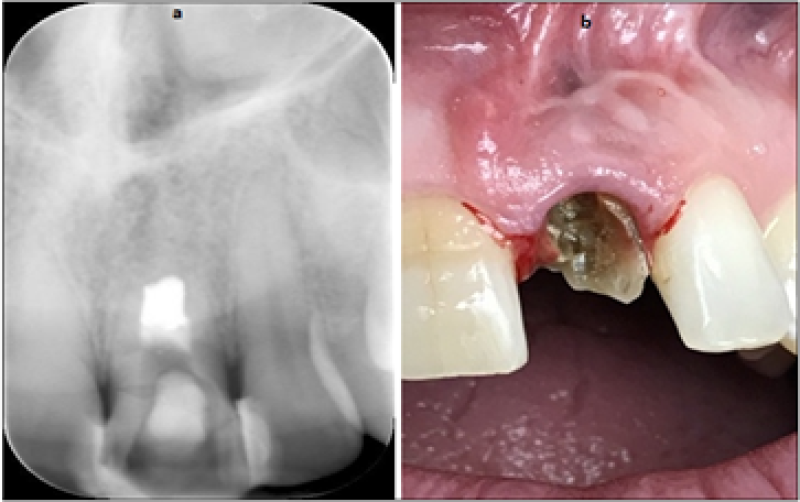
Figure 4: (a) Initial radiograph; (b) Intra-oral situation of element 21.
The tooth was flapless and a traumatically removed. The buccal area was grafted with NovaBone® putty (0.25ml). Immediately, a 4x13mm Biomet 3i®-T3 implant was placed with a final torque of 35Ncm (Figure 5 a,b). A temporary composite crown was installed on a PEEK abutment (Figure 6 a,b,c).
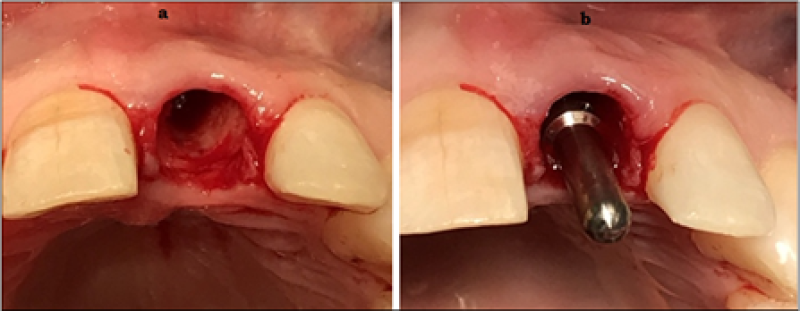
Figure 5: (a) Extraction socket; (b) Direction indicator before putty appliance.
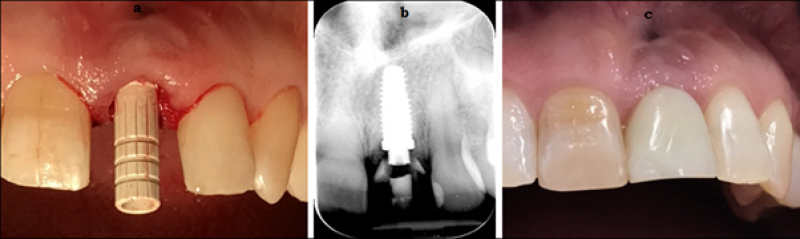
Figure 6: (a) PEEK abutment; (b) X-ray of temporary crown; (c) Intra-oral.
After 4,5 months of osseointegration, the final Monozir crown was digitally fabricated and placed on the osseointegrated implant. The follow-up after 36 months showed a perfectly stable bone level (Figure 7).
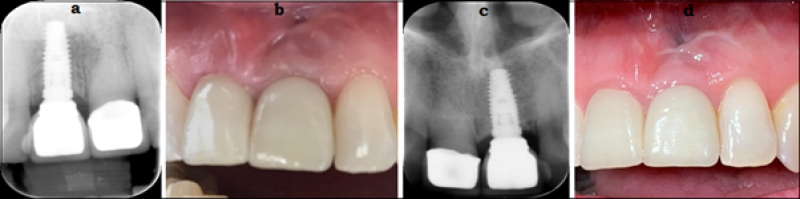
Figure 7: Final crown in situ (X-ray and intra-oral)-Situation after 36 months.
1-phase approach
This 79-year-old non-smoking male patient had a problem at tooth 25. The crown was broken and there was caries in this endodontically treated tooth. The tooth was considered as lost. The patient had a history of hypertension. He used several medications: tamsulosin, isosorbide, purinol, metoprolol, and simvastatin (Figure 8).

Figure 8: X-ray of initial situation 25.
Also, this tooth was removed flapless. Afterwards, immediately a 4x13mm Biomet 3i® - T3 implant was installed with a final torque of >35Ncm. The buccal gap was again grafted with NovaBone® putty (0.25ml). On top of the implant a standard healing abutment was placed that pierced the gingiva (1-phase technique) (Figure 9 a,b,c).

Figure 9: Implant placement with putty application-Implant with healing abutment in situ.
After 5 months of osseointegation a Monozir crown was digitally fabricated. The abutment-crown unit was screwed in the implant (Figure 10 a,b,c).

Figure 10: Crown on printed model-Crown on position 25 in situ.
The final pictures of this case show the 3-year follow-up situation. There is completely no bone loss around the implant on position 25. Tooth 27 is meanwhile removed due to an apical infection (Figure 11 a,b).
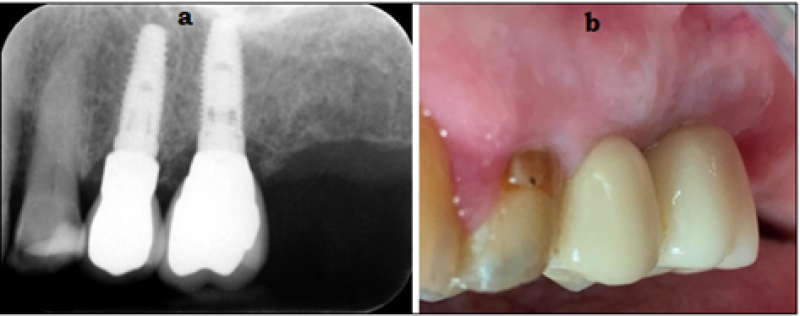
Figure 11: X-ray and intra-oral situation after 36 months.
2-phase approach
A 72-year-old male showed terminal caries under his bridge on element 14. He was completely healthy, used no medication, and didn’t smoke. After the extraction a big bony defect was detected. This was fully excavated, and directly a Biomet 3i® implant 5x10mm T3 was placed at a 25Ncm Torque. Because of the reduced initial stability, a 2-phase protocol was followed. The NovaBone® putty was placed to fill the buccal defect (Figure 12 a,b,c). After 4 months the standard healing abutment was placed in the second stage surgery (Figure 13)
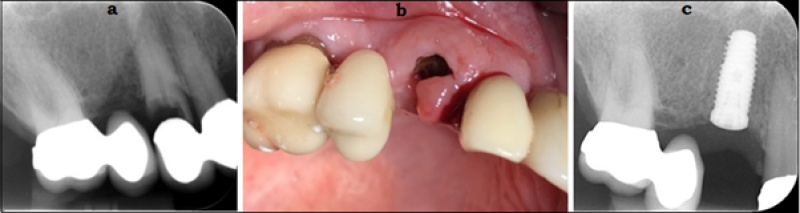
Figure 12: Initial caries 14 – post-extraction – implant in situ.
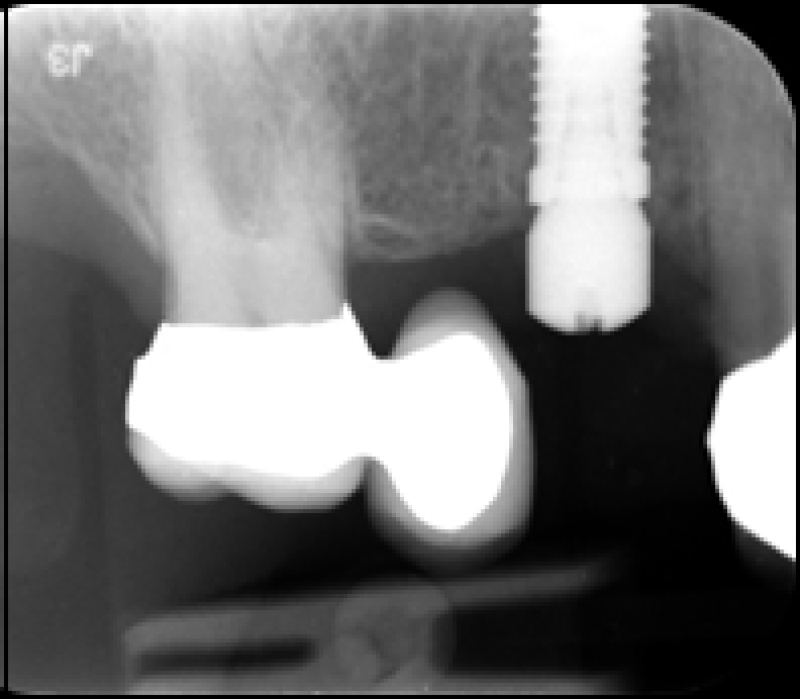
Figure 13: Healing abutment placed after 4 months.
The final Monozir crown was digitally prepared and placed after 9 months since the implant stability was not considered as being sufficient for loading (Figure 14 a.b). The 18-months follow-up showed absolutely no changes in the bone level around the implant (Figure 15).
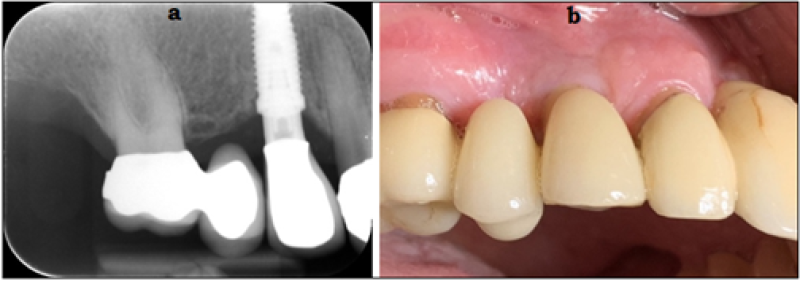
Figure 14: Final restoration in place.
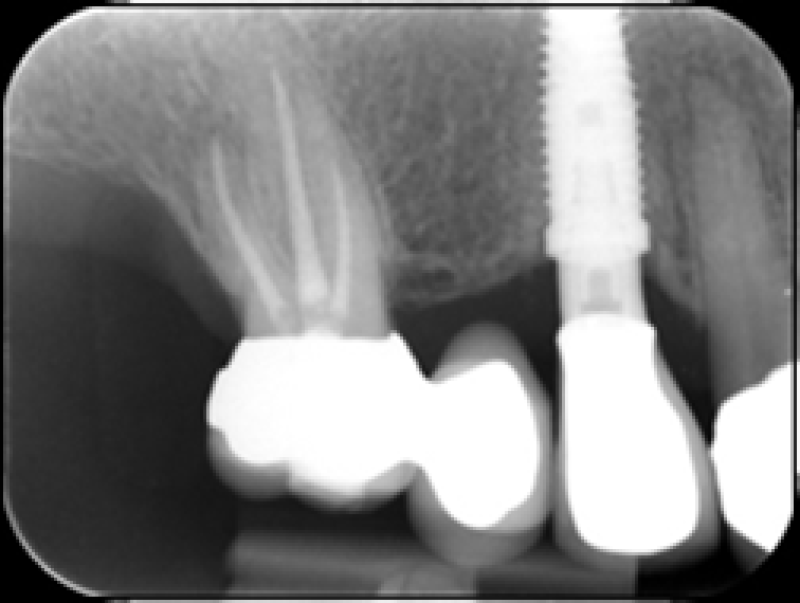
Figure 15: X-ray after 1.5 years.
Discussion
Appropriate patient selection, non-traumatic tooth extraction, palatal implant placement combined with bone augmentation, and careful prosthetic care are paramount in immediate implant placement [15,17,18]. The difference between thick and thin biotypes does not play the significant role, because implants placed on the buccal side showed a three-fold greater recession than implants located on the lingual side, regardless of the biotype [6]. Placing a bone graft and a provisional crown on an implant simultaneous with the tooth extraction increases the vertical and labio-palatal tissue dimensions with 0.5mm to 1mm. On the contrary, it is no bone graft, nor a provisional restoration is placed at the time of flapless immediate post-extraction, the opposite happens [19]. All implants placed in extraction sockets without flap elevation showed some negative contour change. However, this was minimal compared to studies that elevated full periosteal flaps to extract teeth [18]. The smallest amount of facial-palatal contour change was achieved using bone grafting at the extraction socket at the time of implant placement and stabilization of the graft either by placing a contoured healing abutment or a custom-contoured provisional restoration [18]. A recent study by Amato and colleagues found that horizontal and vertical dimensional soft tissue changes, in immediate single-tooth implant placement, combined with provisionalization at the site of fresh tooth extraction in the aesthetic zone, were minimal [8]. The most important feature of this interim restoration is the transmucosal area, which creates the emergence profile for the final aesthetic result [17]. The lack of filler materials can contribute to the shrinkage of the gingival margin, which impairs the aesthetics of immediate implants, especially in the aesthetic area. Therefore, it is suggested that less resorption appears when the gap is filled with a low resorption biomaterial, such as bovine or equine bone [4]. Several studies suggested the same. Whereas grafting extraction sockets does not prevent bone remodelling, it surely does minimize the buccal bone disintegration [17,18]. In these 3 cases, a synthetic putty has been applied instead of an xeno or allograft. Synthetic putty’s have shown to preserve ridge dimension and have favourable bone density values for implant placement as compared to xenograft materials [12].
Conclusion
A synthetic putty is an excellent material for intra-oral grafting, especially in cases where the gap between the extraction socket and the immediate implant must be bridged. The procedure is easier because of the consistency of the putty, and easy handling with the cartridge and its tip. However, more research is required to assess the comparison of immediate placement and a synthetic putty in anterior maxillary cases. The actual cases show a satisfying result in different treatment protocols and seem to be a good alternative to autoxeno and allografts in combination with immediate implant placement.
References
1. Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9:332-43. PubMed | CrossRef
2. Chu SJ, Salama MA, Salama H, Garber DA, Saito H, Sarnachiaro GO, et al. The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend Contin Educ Dent. 2012;33(7). PubMed | CrossRef
3. Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23(4). PubMed | CrossRef
4. Denardi RJ, da Silva RD, Thomé G, Andrighetto AR, de Freitas RM, Shimizu RH, et al. Bone response after immediate placement of implants in the anterior maxilla: a systematic review. Oral Maxillofac Surg. 2019;23(1):13-25. PubMed |CrossRef
5. Januário AL, Duarte WR, Barriviera M, Mesti JC, Araújo MG, Lindhe J. Dimension of the facial bone wall in the anterior maxilla: a cone‐beam computed tomography study. Clin Oral Implants Res. 2011;22(10):1168-71. PubMed | CrossRef
6. Evans CD, Chen ST. Esthetic outcomes of immediate implant placements. Clin Oral Implants Res. 2008;19(1):73-80. PubMed | CrossRef
7. Araujo MG, Linder E, Lindhe J. Bio‐Oss® Collagen in the buccal gap at immediate implants: a 6‐month study in the dog. Clin Oral Implants Res. 2011;22(1):1-8. PubMed | CrossRef
8. Amato F, Amato G, Polara G, Spedicato GA. Guided Tissue Preservation: Clinical Application of a New Provisional Restoration Design to Preserve Soft Tissue Contours for Single-Tooth Immediate Implant Restorations in the Esthetic Area. Int J Periodontics Restorative Dent. 2020;40(6). PubMed | CrossRef
9. Profeta AC, Prucher GM. Bioactive glass in periodontal surgery and implant dentistry. Dent Mater J. 2015;34(5):559-71. PubMed | CrossRef
10. Gonshor A, Saroff SA, Anderegg CR, Joachim FP, Prasad JACH, Katta S. Histologic and clinical evaluation of a bioactive calcium phosphosilicate bone graft material in postextraction alveolar sockets. Int J Oral Imp & Clin Res. 2011; 2: 79-84.
11. Lanka Mahesh BD. Histomorphometric evaluation of a calcium-phosphosilicate putty bone substitute in extraction sockets. Int J Periodontics Restorative Dent. 2014;34:233-9. PubMed | CrossRef
12. Kotsakis GA, Salama M, Chrepa V, Hinrichs JE, Gaillard P. A randomized, blinded, controlled clinical study of particulate anorganic bovine bone mineral and calcium phosphosilicate putty bone substitutes for socket preservation. International Journal of Oral & Maxillofacial Implants. 2014;29(1). PubMed | CrossRef
13. Boogaard MJ. Synthetic Putty and Simultaneous Short Implant Placement in Crestal Sinus Lifting Procedures: 13–36 Months Follow-Up: A Case Series. J Dent Rep. 2021: 2: 1-8. CrossRef
14. Uppal RS, Pal AS, Gupta G, Kaur R. Evaluating the efficacy of a bioactive synthetic graft material in the treatment of intrabony periodontal defects. Int J Cont Dent Ed. 2011; 2: 51-58.
15. Goene RJ, Daelen ACL. Mastering aesthetics in post-extraction sites. J Imp & Reconstr Dent. 2013; 4: 1-8. CrossRef
16. Zetterqvist L, Feldman S, Rotter B, Vincenzi G, Wennström JL, Chierico A, et al. A prospective, multicenter, randomized‐controlled 5‐year study of hybrid and fully etched implants for the incidence of peri‐implantitis. Journal of periodontology. 2010;81(4):493-501. PubMed | CrossRef
17. Amato F, Polara G, Spedicato GA, Grande M, Zuffetti F, Testori T, et al. Tissue Dimensional Changes in Single-Tooth Immediate Extraction Implant Placement. Int J Oral Maxillofac Implants. 2018;33(2):439-47. PubMed | CrossRef
18. Tarnow DP, Chu SJ, Salama MA, J Stappert CF, Salama H, Garber DA, et al. Flapless postextraction socket implant placement in the esthetic zone: part 1. The effect of bone grafting and/or provisional restoration on facial-palatal ridge dimensional change-a retrospective cohort study. International Journal of Periodontics & Restorative Dentistry. 2014;34(3). PubMed | CrossRef
19. Chu SJ, Salama MA, Garber DA, Salama H, Sarnachiaro GO, Sarnachiaro E, et al. Flapless postextraction socket implant placement, part 2: the effects of bone grafting and provisional restoration on peri-implant soft tissue height and thickness-a retrospective study. Int J Periodontics Restorative Dent. 2015;35(6):803-9. PubMed | CrossRef
Maarten J Boogaard1* and Curd M L Bollen2
1Private Practice, Churchill-laan 162hs, 1078 ER, Amsterdam, The Netherlands
2College of Medicine & Dentistry, Ulster University, Birmingham, UK, Lead Advanced Implant Diploma, Tipton Training, Manchester, UK
*Corresponding Author: Maarten J Boogaard, Private Practice, Churchill-laan 162hs, 1078 ER, Amsterdam, The Netherlands.
Copyright© 2022 by Dhande S. All rights reserved. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Boogaard MJ, Bollen CML. The Use of a Synthetic Putty Graft in Extraction Sockets Combined with Immediate Implant Installation: 3 Cases. J Dent Rep. 2022;3(1):1-9. DOI: https://doi.org/10.37191/Mapsci-JDR-3(1)-020
