JOURNAL OF ANESTHESIA AND SURGICAL RESEARCH
Pancreatic Trauma; Surgical Management, 4 Cases Reported
Belkhane Asma* and Harbi Farouk
Surgical Emergency Department, Badji Mokhtar Annaba Faculty of Medicine, IBN ROCHD University Hospital Center, ANNABA, Algeria
*Corresponding Author: Belkhane Asma, General Surgery, Surgical Emergency Department, Badji Mokhtar Annaba Faculty of Medicine, IBN ROCHD University Hospital Center, ANNABA, Algeria.
| ReceivedOct 4, 2023 | RevisedOct 12, 2023 | AcceptedOct 31, 2023 | PublishedJan 3, 2024 |
Abstract
Pancreatic traumas are rare, but particularly serious. Their management involves diagnostic and therapeutic difficulties. The mechanism of injury generally corresponds to crush injuries or direct trauma during public road accidents. They most often occur during polytrauma and the associated lesions then determine the prognosis and treatment methods. In stable patients, an imaging assessment using CT, magnetic resonance imaging, or even endoscopic retrograde pancreatography determines the type and topography of pancreatic lesions and specifies the damage of the main pancreatic duct, which accounts for the seriousness of the pancreatic trauma.
The treatment of pancreatic trauma essentially depends on the integrity or not of the Wirsung duct. Treatment can be solely medical, but above all surgical and endoscopic when canal is damaged. There is report of 4 patient observations who were treated in the surgical emergency department at Annaba Algeria University Hospital during the year 2023 for isolated trauma of the pancreas. There are diagnostic circumstances and description of therapeutic conduct and the surgical consequences.
Keywords
Pancreas; Trauma; Magnetic resonance; Surgery; Lesions; Therapeutic; Endoscopy
Introduction
Pancreatic traumas are rare but can be fatal; they are frequently associated with other lesions in the context of major trauma. They constitute 0.2 to 6% of all abdominal trauma and they are frequently associated with other lesions in the context of major trauma in 90% of adults [1-3]. It falls within the framework of high-energy abdominal contusions and involves crushing of the retroperitoneal structures against the spine. Located deep in the abdomen, this retroperitoneal organ is surrounded and masked by neighboring organs, for this reason, its lesions, open or closed, can have a hemorrhage type expression, the duodenal or biliary rupture type expression or even of the pure pancreatic contusion type expression. It is because of this anatomical complexity, the proximity of neighboring organs that this organ harbors of evolving into acute pancreatitis. That is why signs and symptoms caused by the lesions are nonspecific and difficult to objectify. The initial clinical expression varies from the absence of all initial clinical sign to frank peritoneal syndrome, and in the case of an injury pancreatic, unfortunately it is not possible to prejudge a lesion canal depending on the symptomatology. Over the past two decades, the management of abdominal contusion has been largely modified by progress made in imaging.
Non-operative treatment of pancreatic trauma, has become feasible, it is thanks to the possibility of diagnosing Wirsung canal lesion, whose rupture transforms the prognosis and therapeutic indication. They have a morbidity and mortality of up to 39% [4,5] especially if diagnosis delay. Furthermore, the diversity and complexity of these lesions pose a constant challenge to the surgeon regarding the choice of treatment, which must be adapted to the type of lesion and its anatomical site, especially in situations emergency.
Observations
There is report of a series of 04 patients who were treated in the department during the year 2023 for isolated trauma of the pancreas. The diagnostic circumstances and description of the therapeutic conduct and the surgical consequences are recalled.
Case 1
A 35-year-old patient admitted to the emergency department for treatment of multiple trauma secondary to a traffic accident (crushing against the dashboard). Initial clinical examination as well as CT scan were normal apart from a sutured frontal wound and fractures of the 4th, 5th, 6th uncomplicated left ribs immobilized by elastoblast. 72 hours later, generalized abdominal pain appeared. a new clinical examination noted epigastric defense and moderate dullness of the flanks, stable hemodynamic state, normal consciousness with a Glasgow score 15/15, Lipasemia level at 7x Nle, GB: 14000 e/mm3. Scan /Pancreatic MRI: pancreatic trauma classified as Lucas stage II with partial section of the Wirsung duct complicated by stage D acute pancreatitis (Figure 1).
The attitude was NOT (Non-Operative Treatment) based on the medical TRT of pancreatitis, clinical and biological monitoring. The evolution was favorable without after-effects with a return to normal of the pancreatic assessment. Exit authorized on day 15.
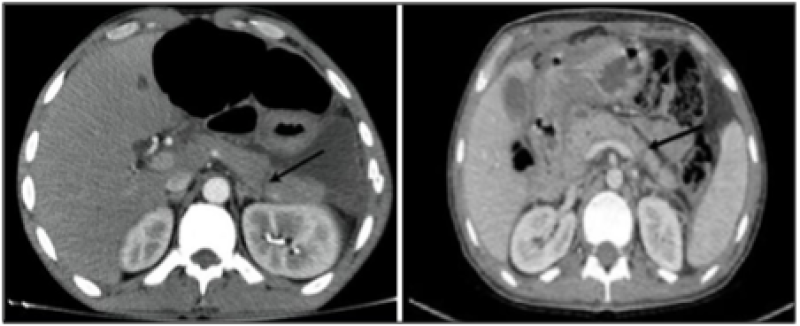
Figure 1: Lucas stage II with partial section of the Wirsung duct.
Case 2
A 56-year-old man victim of a motorcycle accident with the handlebars hitting the epigastrium. He consulted two days after the accident; The examination on admission noted generalized abdominal pain. Blood pressure 12/5mm/Hg. Lipasemia level 30x normal, white blood cells 15000 e/mm3. The emergency ultrasound showed a large intraperitoneal effusion and the scan showed stage E pancreatitis associated with a fracture of the corporeo-caudal region (Lucas Class II).
The therapeutic attitude was initially a NOT (Non operative Traitement); 5 days after and faced with hemodynamic instability and the appearance of an infectious syndrome associated with abdominal defense, it was decided to operate on the patient. Surgical exploration revealed a large peritoneal effusion with a total section of the tail of the pancreas (Figure 2); a left pancreatectomy was performed (Figure 3). The establishment of a pancreatic fistula well managed by somatostatin marked the evolution.
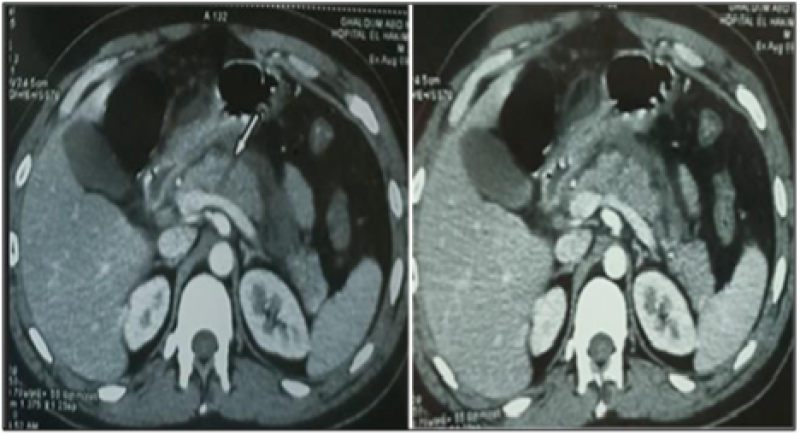
Figure 2: Pancreatic Trauma (Lucas Class II).
Case 3
A 21-year-old man with no particular pathological history evacuated from peripheral Hospital Establishment for treatment of closed abdominal trauma with abdominal impact, following a work accident 3 days ago.
Clinically the patient was conscious, blood pressure at 9/05 mm/hg, presenting with epigastric pain, generalized abdominal defense on palpation. Hg 10gr/dl.
WBC: 20000e/mm3, white blood cells 20000e/mm3, lipasemia rate 9x nle.
CT scan: Grade II caudal body pancreatic lesion, with infiltration of mesenteric fat, Medium abundance effusion, peripancreatic collection measuring 54 × 75mm (Figure 4).
After radiological drainage, faced with no clinical improvement, it was decided to operate on the patient. The exploration revealed the presence of necrosis, and total section of the tail of the pancreas at the level of the isthmus. A caudal spleno-pancreatectomy was performed with closure of the pancreatic section/epiploplasty/wide drainage. The evolution was marked by the formation of a septic collection in the splenic compartment and retrogastric drained by radiology. The control at 3 months was satisfactory with disappearance of all the lesions.
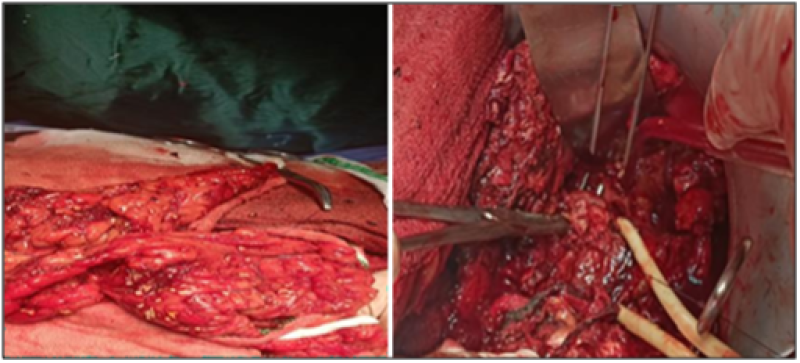
Figure 3: Total section of the tail of Pancreas.
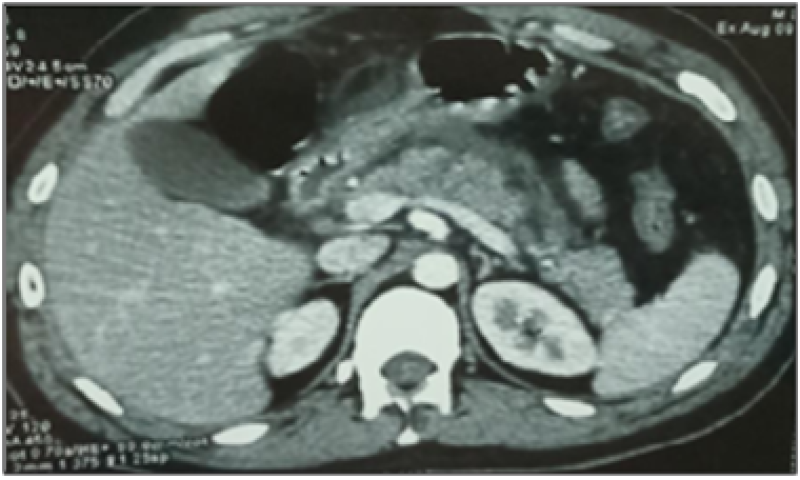
Figure 4: CT scan, Grade II caudal body pancreatic lesion.
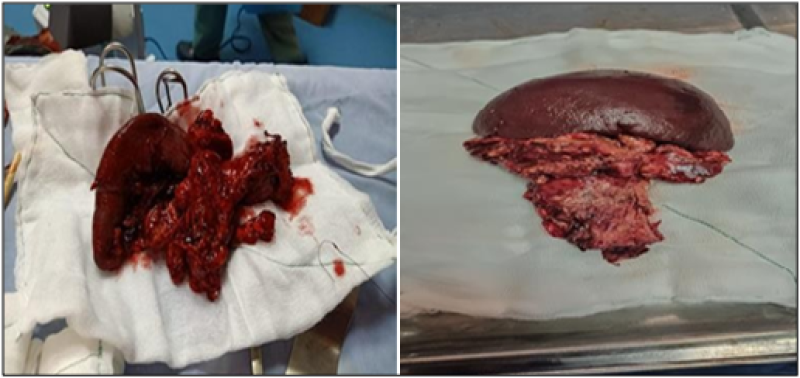
Figure 5: A caudal spleno pancreatectomy.
Case 4
A 19-year-old man victim of an attack by punch to the epigastric level. Initial examination was normal; 15 days later the patient presented with intense epigastric pain associated with vomiting. A mass extending from the epigastrium to the left hypochondrium painful on palpation. Lipasemia 6x was normal. CT scan supplemented with pancreatic MRI objectified stage E pancreatitis complicated by enormous pseudo cyst of the pancreas. It was operated after 2 months of medical TRT having benefited from a jejunal cyst anastomosis on a Y intestinal loop. Favorable evolution exit authorized on day 7th.
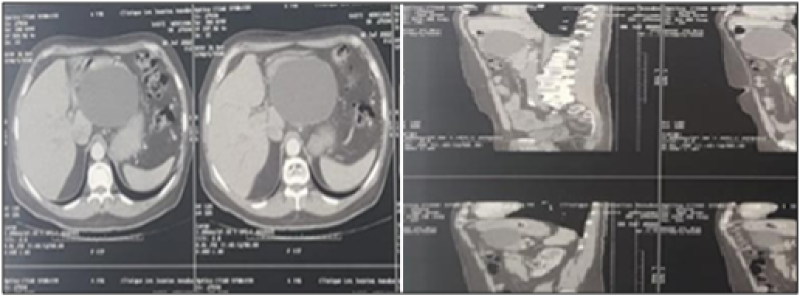
Figure 6: Pseudokyst of the post traumatic pancreas.
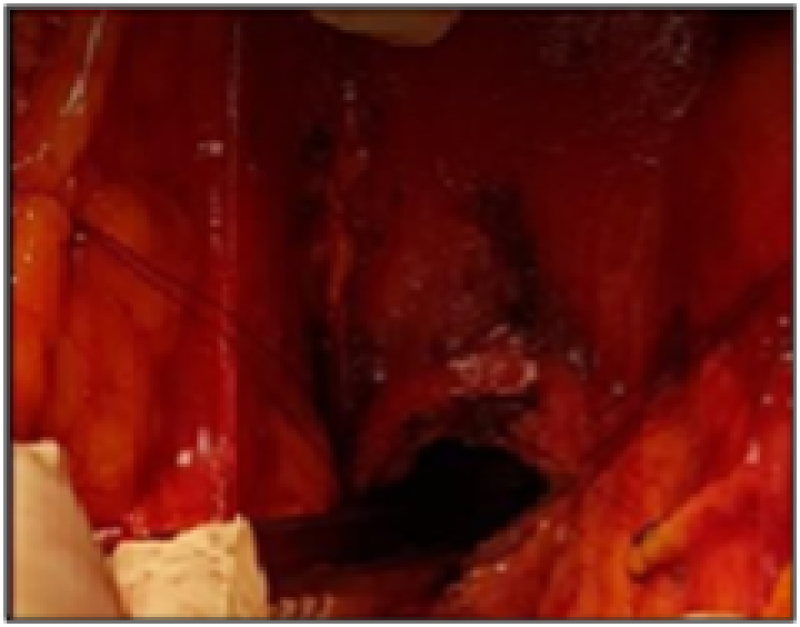
Figure 7: Cystic cavity.
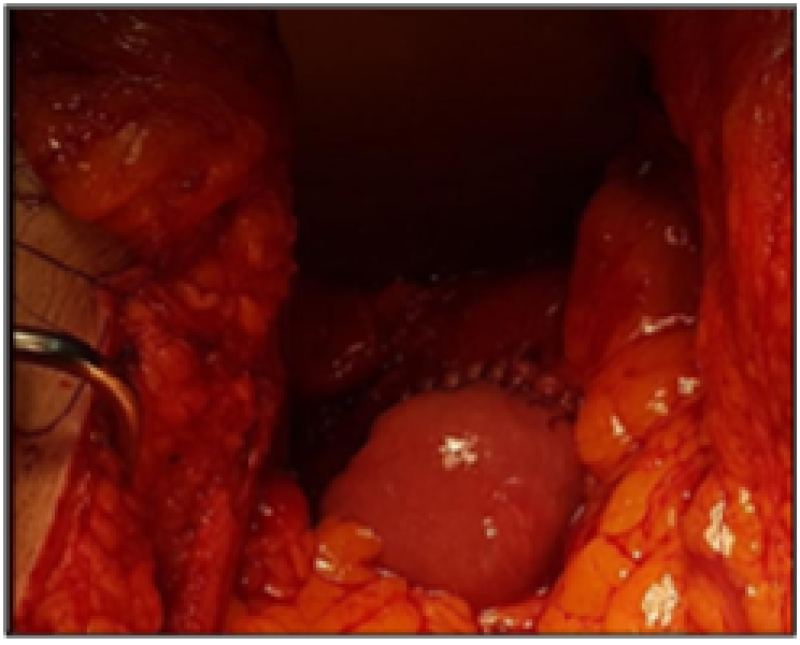
Figure 8: Anastomosis on a Y intestinal loop.

Figure 9: Distal Anastomosis.
Discussion
The frequency of pancreatic trauma is increasing; their frequency is estimated in the literature between 0.5 and 15% of abdominal trauma [6,7]. These lesions may be overlooked and only discovered at the complication stage. In 3 of our patients the diagnosis was made at the stage of acute pancreatitis. The Fourth was diagnosed at the pseudocyst stage. Patients suffering from isolated pancreatic trauma are often asymptomatic for the first hours. The serum, urine or peritoneal dosage of amylase and/or lipase is of great diagnostic value.
Abdominal CT scan is the reference examination for the detection of pancreatic lesions if hemodynamic stability but with a rate of 40% false negatives in the first hours [5], hence the interest in repeating CT when the initial imaging is atypical. However, Wirsungo pancreatico MRI is the gold standard in the detection of ductal lesions (sensitivity 87 to 100% and specificity 81%) [8,9]. The therapeutic attitude towards TIP will depend on the lesion stage. It is helpful to manage pancreatic injuries according to the American Association for Surgery of Trauma (Maeda, 2013). The non-operative option should be reserved for patients with blunt trauma with isolated pancreatic injury without rupture of the Wirsung duct (Lucas class I) [10-11,13,16]. During a rupture of the Wirsung canal (class II and III) demonstrated by preoperative CPRM and/or ERCP, the placement of endoductal prosthesis gave excellent results [10]. Complete transection of the pancreas (types II-III-IV) is an indication for surgical TRT.
In Lucas class II, surgery will consist of a left pancreatectomy with preservation of the spleen rather than a left spleno-pancreatectomy. In classes III, suture of the cephalic pancreas accompanied by an anastomosis of the left pancreas on a Y loop or on the stomach is a possible intervention [11-16]. It is an alternative to cephalic duodeno-pancreatectomy which is indicated in cases of contusion with destruction of the head of the pancreas making it impossible to preserve it.
Simple contact drainage will be carried out if the patient's hemodynamic state does not allow the procedure to be prolonged [20]. Overall mortality in patients with abdominal trauma with pancreatic involvement varies from 5 to 30% depending on the series [2-4] however, it is only directly attributed to the pancreas in 5 to 10% of these deaths [12,13,19,20].
Conclusion
The rarity of pancreatic trauma and their atypical clinical symptomatology at the beginning stage makes their diagnosis relatively difficult, especially since others more that biology is not specific. This should push us to perform CT scans for any epigastric trauma, even if it is not violent. The installation of a pancreatic prosthesis constitutes a remarkable development in the current treatment of isolated pancreatic trauma (IPT). Pancreatic resection surgery performed in the face of ductal rupture improves the prognosis of IPT despite significant morbidity.
References
1. Sukul K, Lont HE, and Johannes EJ. Management of Pancreatic Injuries. Hepatogastroenterology. 1992;39(5):447-50. PubMed
2. Farrell RJ, Krige JE, Bornman PC, Knottenbelt JD, Terblanche J. Operative Strategies in Pancreatic Trauma. Br J Surg. 1996;83(7):934-7. PubMed | CrossRef
3. Feliciano DV, Martin TD, Cruse PA et al. Management of Combined Pancreatoduodenal Injuries. Ann Surg. 1987; 205(6): 673-80.
4. Jurczak F, Kahn X, Letessier E, Plattner V, Heloury Y, Le Neel JC. Severe Pancreaticoduodenal Trauma: Review of a Series of 30 Patients. Ann Chir. 1999;53(4):267-72. PubMed
5. Bradley EL, Young Jr PR, Chang MC, Allen JE, Baker CC, Meredith W, et al. Diagnosis and Initial Management of Blunt Pancreatic Trauma: Guidelines from a Multiinstitutional Review. Ann Surg. 1998;227(6):861. PubMed | CrossRef
6. Beyrouti MI, Beyrouti R, Kchaou I, Gharbi W, Elleuch S, Tafech I, et al. Duodeno-pancreatic Trauma. About 14 cases. Tunis Med. 2005;83(2):73-82. PubMed
7. Arvieux C, Voirin D, Létoublon C. Pancreat Trauma Surg. 2009:102-4.
8. Akhrass R, Yaffe MB, Brandt CP, Reigle M, Fallon Jr WF, Malangoni MA. Pancreatic Trauma: A Ten-Year Multiinstitutional Experience. Am Surg. 1997;63(7):598-604. PubMed
9. Gomez MA, Besson M, Scotto B, Roger R, Alison D. MR Imaging in the Evaluation of Blunt Pancreatic Trauma. J Radiol. 2004;85(4 Pt 1):414-7. PubMed | CrossRef
10. Kim HS, Lee DK, Kim IW, Baik SK, Kwon SO, Park JW, et al. The Role of Endoscopic Retrograde Pancreatography in the Treatment of Traumatic Pancreatic Duct Injury. Gastrointest Endosc. 2001;54(1):49-55. PubMed | CrossRef
11. Thanh LN, Duchmann JC, Latrive JP, That BT, Huguier M. Conservation of the Left Pancreas in Rupture of the Pancreatic Isthmus-Apropos of 3 cases. Chirurgie. 1999;124(2):165-70. PubMed | CrossRef
12. Carrel, T, J Lerut, U Niederhauser, W Schweizer, LH Blumgart. Diagnosis and Treatment of Traumatic Injuries of the Duodenum and Pancreas: 21 cases. J Chir (Paris). 1990;127(10):438-44. PubMed
13. Errougani A, Ameur A, Chkoff R, El Alj A, Balafrej S. Duodenopancreatic Injuries. Apropos of 30 Cases. J Chir (Paris). 1997;134(1):9-13. PubMed
14. Wilson RH, Moorehead RJ. Current Management of Trauma to the Pancreas. Br J Surg. 1991;78(10):1196-202. PubMed | CrossRef
15. Zerbib P, Brams A, Chambon JP. Blunt Pancreatic Fractures. Ann Chir. 2001; 126(5):421-6. PubMed | CrossRef
16. SNFGE. Pancréatite aiguë: l’heure du consensus. Gastroentérol Clin Biol. 2001;25(1):155-246. PubMed.
17. Jobst MA, Canty Sr TG, Lynch FP. Management of Pancreatic Injury in Pediatric Blunt Abdominal Trauma. J Pediatr Surg. 1999;34(5):818-24. PubMed | CrossRef
18. Asensio JA, Petrone P, Roldan G, Pak-Art R, Salim A. Pancreatic and Duodenal Injuries. Complex and Lethal. Scand J Surg. 2002;91(1):81-6. PubMed | CrossRef
19. American College of Surgeons. Committee on Trauma. Advanced Trauma Life Support for Doctors: Student Course Manual. American College of Surgeons. 2008.
20. Asensio JA, García JC, Petrone P, Roldán G, Pardo M, García WM, et al. Pancreatic trauma: Complex Lesions, Difficult Treatments. Cirugía Española. 2003;74(3):124-33.
Belkhane Asma* and Harbi Farouk
Surgical Emergency Department, Badji Mokhtar Annaba Faculty of Medicine, IBN ROCHD University Hospital Center, ANNABA, Algeria
*Corresponding Author: Belkhane Asma, General Surgery, Surgical Emergency Department, Badji Mokhtar Annaba Faculty of Medicine, IBN ROCHD University Hospital Center, ANNABA, Algeria.
Copyright© 2023 by Asma B, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Asma B, Farouk H. Pancreatic Trauma; Surgical Management, 4 Cases Reported. J Anaesth Surg Res. 2023;3(2):184-91. DOI: https://doi.org/10.37191/Mapsci-JASR-3(2)-030
