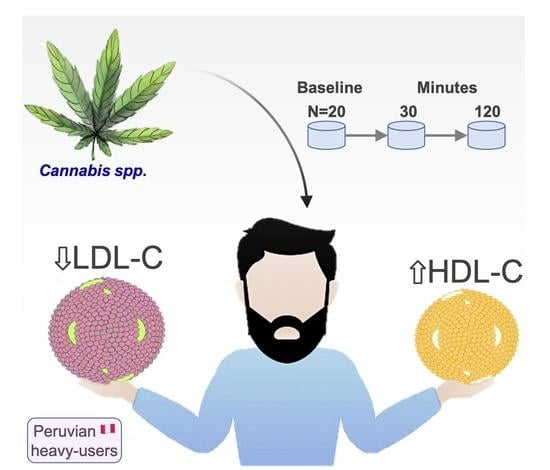
Changes in High-Density Lipoprotein (HDL), Low-Density Lipoprotein (LDL) and Cholesterol Concentration in Heavy Cannabis Users: A Single-Centre Study in Cusco, Peru
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Subjects, and Samples
2.2. Assessment of Cannabis Use, Determination of Lipoproteins and Cannabinoids in Urine
2.3. Data Analysis
3. Results
3.1. Baseline Cholesterol Concentration
3.2. Changes in Lipoproteins Due to Cannabis Use
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Iqbal, J.; Al Qarni, A.; Hawwari, A.; Alghanem, A.F.; Ahmed, G. Metabolic Syndrome, Dyslipidemia and Regulation of Lipoprotein Metabolism. Curr. Diabetes Rev. 2018, 14, 427–433. [Google Scholar] [CrossRef]
- Moya-Salazar, J.; Pio-Davila, L. Lipid disorders in Hispano-American patient in Primary health-care at Lima, Peru. Rev. Cub. Salud Pública 2020, 46, e1161. [Google Scholar]
- Thakur, R.B. Plasma lipoprotein lipase activity in ganja smokers. J. Indian Med. Assoc. 1984, 82, 191–194. [Google Scholar]
- Hawkins, M.N.; Horvath, T.L. Cannabis in fat: High hopes to treat obesity. J. Clin. Investig. 2017, 127, 3918–3920. [Google Scholar] [CrossRef]
- Rajavashisth, T.B.; Shaheen, M.; Norris, K.C.; Pan, D.; Sinha, S.K.; Ortega, J.; Friedman, C.T. Decreased prevalence of diabetes in marijuana users: Cross-sectional data from the National Health and Nutrition Examination Survey (NHANES) III. BMJ Open 2012, 2, e000494. [Google Scholar] [CrossRef]
- Ngueta, G. Lifetime Average Cannabis Use in Relation to Hypertriglyceridemic Waist Phenotype in U.S. Adults: A Population-Based Cross-Sectional Study. Cannabis Cannabinoid Res. 2020, 5, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Jayanthi, S.; Buie, S.; Moore, S.; Herning, R.I.; Better, W.; Wilson, N.M.; Contoreggi, C.C.; Cadet, J.L. Heavy marijuana users show increased serum apolipoprotein C-III levels: Evidence from proteomic analyses. Mol. Psychiatry 2010, 15, 101–112. [Google Scholar] [CrossRef]
- Levendal, R.A.; Frostin, C.L. In vivo effects of Cannabis sativa l. extract on blood coagulation, fat and glucose metabolism in normal and streptozocin-induced diabetic rats. Afr. J. Trad. CAM 2006, 3, 1–12. [Google Scholar] [CrossRef]
- Panee, J.; Pomozi, V.; Franke, A.A.; Le Saux, O.; Gerschenson, M. Chronic marijuana use moderates the correlations of serum cholesterol with systemic mitochondrial function and fluid cognition. Mitochondrion 2020, 52, 135–143. [Google Scholar] [CrossRef]
- Wei, T.T.; Chandy, M.; Nishiga, M.; Zhang, A.; Kumar, K.K.; Thomas, D.; Manhas, A.; Rhee, S.; Justesen, J.M.; Chen, I.Y.; et al. Cannabinoid receptor 1 antagonist genistein attenuates marijuana-induced vascular inflammation. Cell 2022, 185, 1676–1693.e23. [Google Scholar] [CrossRef]
- Feng, Q.; Jiang, L.; Berg, R.L.; Antonik, M.; MacKinney, E.; Gunnell-Santoro, J.; McCarty, C.A.; Wilke, R.A. A common CNR1 (cannabinoid receptor 1) haplotype attenuates the decrease in HDL cholesterol that typically accompanies weight gain. PLoS ONE 2010, 5, e15779. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Liu, Q.; Hou, P.; Li, F.; Guo, S.; Song, W.; Zhang, H.; Liu, X.; Zhang, S.; Zhang, J.; et al. Stilbenoids and cannabinoids from the leaves of Cannabis sativa f. sativa with potential reverse cholesterol transport activity. Food. Funct. 2018, 9, 6608–6617. [Google Scholar] [CrossRef]
- Whiting, P.F.; Wolff, R.F.; Deshpande, S.; Di Nisio, M.; Duffy, S.; Hernandez, A.V.; Keurentjes, J.C.; Lang, S.; Misso, K.; Ryder, S.; et al. Cannabinoids for Medical Use: A Systematic Review and Meta-analysis. JAMA 2015, 313, 2456–2473. [Google Scholar] [CrossRef]
- World Health Organization. The Health and Social Effects of Nonmedical Cannabis Use; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Prohibition Partners. The Latin America and Caribbean Report November 2020, 2nd ed.; Prohibition Partners Press: London, UK, 2020. [Google Scholar]
- Congreso de la Republica. Ley Nº 30681 Ley que Regula el Uso Medicinal y Terapéutico del Cannabis y sus Derivados; Gobierno del Perú: Lima, Perú, 2017; Available online: https://busquedas.elperuano.pe/normaslegales/ley-que-regula-el-uso-medicinal-y-terapeutico-del-cannabis-y-ley-n-30681-1587374-1/ (accessed on 20 May 2022).
- Congreso de la Republica. Ley Nº 30681 Ley que Incorpora y Modifica Artículos de la Ley 30681, ley que Regula el uso Medicinal y Terapéutico del Cannabis y sus Derivados; Gobierno del Perú: Lima, Perú, 2017; Available online: https://busquedas.elperuano.pe/normaslegales/ley-que-incorpora-y-modifica-articulos-de-la-ley-30681-ley-ley-n-31312-1976352-1/#:~:text=Se%20autorizan%20el%20uso%20informado,terap%C3%A9uticos%2C%20de%20acuerdo%20con%20las (accessed on 20 May 2022).
- Clinical and Laboratory Standard Institute. CLSI H18-A4. Procedures for the Handling and Processing of Blood Specimens for Common. Laboratory Tests, Approved Guideline-Fourth Edition; CLSI document H18-A4; Clinical and Laboratory Standard Institute: Wayne, PA, USA, 2007. [Google Scholar]
- Díaz, R.C.; Arias, L.J.J.; Díaz, F.E.J.F.; Golding, F.S. A comparison of methods for the analysis of cannabinoids in urine. Anál Clín. 2000, 25, 9–16. [Google Scholar]
- Debruyne, D.; Albessard, F.; Bigot, M.C.; Moulin, M. Comparison of three advanced chromatographic techniques for Cannabis identification. Forensic Sci. Int. 1999, 106, 135–146. [Google Scholar]
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- Fearby, N.; Penman, S.; Thanos, P. Effects of Δ9-Tetrahydrocannibinol (THC) on Obesity at Different Stages of Life: A Literature Review. Int. J. Environ. Res. Public Health 2022, 19, 3174. [Google Scholar] [CrossRef]
- Muniyappa, R.; Sable, S.; Ouwerkerk, R.; Mari, A.; Gharib, A.M.; Walter, M.; Courville, A.; Hall, G.; Chen, K.Y.; Volkow, N.D.; et al. Metabolic effects of chronic cannabis smoking. Diabetes Care 2013, 36, 2415–2422. [Google Scholar] [CrossRef]
- Lazarte, J.; Hegele, R.A. Cannabis effects on lipoproteins. Curr. Opin. Lipidol. 2019, 30, 140–146. [Google Scholar] [CrossRef]
- Ngueta, G.; Ndjaboue, R. Lifetime marijuana use in relation to insulin resistance in lean, overweight, and obese US adults. J. Diabetes 2020, 12, 38–47. [Google Scholar] [CrossRef] [PubMed]
- United Nations Office on Drugs and Crime. World Drug Report 2017; United Nations Publication: Vienna, Austria, 2017; Available online: https://www.unodc.org/wdr2017/ (accessed on 10 May 2022).
- Chayasirisobhon, S. Mechanisms of action and pharmacokinetics of cannabis. Perm. J. 2020, 25, 19.200. [Google Scholar] [CrossRef]
- Kogan, N.M.; Mechoulam, R. Cannabinoids in health and disease. Dialogues Clin. Neurosci. 2007, 9, 413–430. [Google Scholar] [CrossRef]
- Cheng, D.; Spiro, A.S.; Jenner, A.M.; Garner, B.; Karl, T. Long-term cannabidiol treatment prevents the development of social recognition memory deficits in Alzheimer’s disease transgenic mice. J. Alzheimer’s Dis. 2014, 42, 1383–1396. [Google Scholar] [CrossRef]
- Vidot, D.C.; Prado, G.; Hlaing, W.M.; Florez, H.J.; Arheart, K.L.; Messiah, S.E. Metabolic Syndrome Among Marijuana Users in the United States: An Analysis of National Health and Nutrition Examination Survey Data. Am. J. Med. 2016, 129, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Ekenedilichukwu, O.J.; Obioma, O.J.; Chukwuemeka, O.E.; Priscilla, E.I.; Loveth, E.; Kalu, A.U.; Nwabunwanne, O.V.; Chukwuemeka, M.S. Evaluation of serum lipid profile in male cannabis smokers of college of health sciences, Nnamdi Azikiwe university, Nnewi campus, Anambra state, Nigeria. Int. J. Health Sci. Res. 2018, 8, 1–6. [Google Scholar]
- Kim, D.; Kim, W.; Kwak, M.S.; Chung, G.E.; Yim, J.Y.; Ahmed, A. Inverse association of marijuana use with nonalcoholic fatty liver disease among adults in the United States. PLoS ONE 2017, 12, e0186702. [Google Scholar] [CrossRef]
- Ponce, O.C.; Roldan, P.; Sibbitt, W.; Qualls, C.; Roldan, C. Abstract 577: Medical Marijuana Use: Effect on Lipid Metabolism and Atherosclerosis. Art. Thromb. Vas. Biol. 2015, 35, A577. [Google Scholar] [CrossRef]
- Pacher, P.; Steffens, S.; Haskó, G.; Schindler, T.H.; Kunos, G. Cardiovascular effects of marijuana and synthetic cannabinoids: The good, the bad, and the ugly. Nat. Rev. Cardiol. 2018, 15, 151–166. [Google Scholar] [CrossRef]
- Baye, T.M.; Zhang, Y.; Smith, E.; Hillard, C.J.; Gunnell, J.; Myklebust, J.; James, R.; Kissebah, A.H.; Olivier, M.; Wilke, R.A. Genetic variation in cannabinoid receptor 1 (CNR1) is associated with derangements in lipid homeostasis, independent of body mass index. Pharmacogenomics 2008, 9, 1647–1656. [Google Scholar] [CrossRef]


| Variable | Categories | f | % | p-Value * |
|---|---|---|---|---|
| Age (year) | ||||
| <25 | 3 | 15 | 0.088 | |
| 25–35 | 12 | 60 | ||
| 36–45 | 5 | 25 | ||
| Body Mass Index | ||||
| Underweight | 1 | 5 | 0.071 | |
| Normal | 18 | 90 | ||
| Overweight | 1 | 5 | ||
| Self-reported Cannabis use | ||||
| Inter-daily | 3 | 15 | 0.201 | |
| Daily | 17 | 85 |
| Lipidic Biomarkers | Profile | Baseline | 30 min | 120 min | p-Value | |
|---|---|---|---|---|---|---|
| Total Cholesterol (mg/dL) | <200 | Desirable | 12 (60) | 11 (55) | 17 (85) | 0.001 |
| 200–239 | Borderline | 8 (40) | 8 (40) | 3 (15) | ||
| >240 | High risk | 0 (0) | 1 (5) | 0 (0) | ||
| HDL-C (mg/dL) | <40 | At risk | 0 (0) | 0 (0) | 0 (0) | <0.001 |
| 40–60 | Fairly good | 10 (50) | 6 (30) | 4 (20) | ||
| >60 | Desirable | 10 (50) | 14 (70) | 16 (80) | ||
| LDL-C (mg/dL) | <100 | Desirable | 0 (0) | 2 (10) | 1 (5) | 0.001 |
| 100–129 | Fairly good | 11 (55) | 5 (25) | 13 (65) | ||
| 130–159 | Borderline high | 9 (45) | 12 (60) | 5 (25) | ||
| 160–189 | High risk | 0 (0) | 1 (5) | 1 (5) | ||
| Lipidic Biomarkers | Measures | Mean | SD | Range | IC95% | ||
|---|---|---|---|---|---|---|---|
| Total Cholesterol (mg/dL) | Baseline | 193.4 | 20.2 | 153 | to 225 | 184.52 | to 202.21 |
| 30 min | 199.2 | 23.3 | 161 | to 265 | 188.95 | to 209.35 | |
| 120 min | 181 | 19.3 | 150 | to 225 | 172.48 | to 189.42 | |
| HDL-C (mg/dL) | Baseline | 60.1 | 6.4 | 48 | to 69 | 57.26 | to 62.83 |
| 30 min | 63.3 | 7.7 | 48 | to 75 | 59.89 | to 66.61 | |
| 120 min | 69.2 | 18.7 | 53 | to 144 | 60.97 | to 77.33 | |
| LDL-C (mg/dL) | Baseline | 129.7 | 14.5 | 106 | to 159 | 123.30 | to 136 |
| 30 min | 130.7 | 20.6 | 82 | to 175 | 121.63 | to 139.67 | |
| 120 min | 122.4 | 16.3 | 81 | to 166 | 115.18 | to 129.51 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cusihuaman, S.; Moya-Salazar, J.; Wong-Salgado, P.; Moya-Salazar, M.M.; Cañari, B.; Chicoma-Flores, K.; Contreras-Pulache, H. Changes in High-Density Lipoprotein (HDL), Low-Density Lipoprotein (LDL) and Cholesterol Concentration in Heavy Cannabis Users: A Single-Centre Study in Cusco, Peru. Processes 2022, 10, 1597. https://doi.org/10.3390/pr10081597
Cusihuaman S, Moya-Salazar J, Wong-Salgado P, Moya-Salazar MM, Cañari B, Chicoma-Flores K, Contreras-Pulache H. Changes in High-Density Lipoprotein (HDL), Low-Density Lipoprotein (LDL) and Cholesterol Concentration in Heavy Cannabis Users: A Single-Centre Study in Cusco, Peru. Processes. 2022; 10(8):1597. https://doi.org/10.3390/pr10081597
Chicago/Turabian StyleCusihuaman, Sandro, Jeel Moya-Salazar, Pedro Wong-Salgado, Marcia M. Moya-Salazar, Betsy Cañari, Karina Chicoma-Flores, and Hans Contreras-Pulache. 2022. "Changes in High-Density Lipoprotein (HDL), Low-Density Lipoprotein (LDL) and Cholesterol Concentration in Heavy Cannabis Users: A Single-Centre Study in Cusco, Peru" Processes 10, no. 8: 1597. https://doi.org/10.3390/pr10081597