Preformulation and Long-Term Stability Studies of an Optimized Palatable Praziquantel Ethanol-Free Solution for Pediatric Delivery
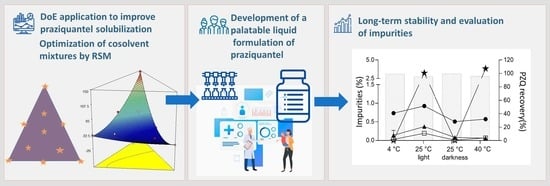
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Design of Experiments
2.3. Drug Solubility Assay
2.4. Taste Masking Assay
2.5. Preparation of PZQ Liquid Dosage Form
2.6. Stability Studies
2.7. HPLC Analysis
2.8. Statistical Analysis
3. Results and Discussions
3.1. Drug Solubility Assay
3.2. Solvents Daily Intake
3.3. Taste Masking Assay
3.4. Stability Studies
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ito, A.; Li, T.; Wandra, T.; Dekumyoy, P.; Yanagida, T.; Okamoto, M.; Budke, C.M. Taeniasis and cysticercosis in Asia: A review with emphasis on molecular approaches and local lifestyles. Acta Trop. 2019, 198, 105075. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Chen, X.; Wang, H.; Openshaw, J.J.; Zhong, B.; Felt, S.A.; Ito, A.; Luby, S.P. High prevalence of taeniasis and Taenia solium cysticercosis in children in western Sichuan, China. Acta Trop. 2019, 199, 105133. [Google Scholar] [CrossRef]
- Rodríguez-Morales, A.J.; Yepes-Echeverri, M.C.; Acevedo-Mendoza, W.F.; Marín-Rincón, H.A.; Culquichicón, C.; Parra-Valencia, E.; Cardona-Ospina, J.A.; Flisser, A. Mapping the residual incidence of taeniasis and cysticercosis in Colombia, 2009–2013, using geographical information systems: Implications for public health and travel medicine. Travel Med. Infect. Dis. 2018, 22, 51–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia, H.H.; del Brutto, O.H. Taenia solium cisticercosis. Infect. Dis. Clin. N. Am. 2000, 14, 97–119. [Google Scholar] [CrossRef] [PubMed]
- Symeonidou, I.; Arsenopoulos, K.; Tzilves, D.; Soba, B.; Gabriël, S.; Papadopoulos, E. Human taeniasis/cysticercosis: A potentially emerging parasitic disease in Europe. Ann. Gastroenterol. 2018, 31, 406–412. [Google Scholar] [CrossRef]
- Raoul, F.; Li, T.; Sako, Y.; Chen, X.; Long, C.; Yanagida, T.; Wu, Y.; Nakao, M.; Okamoto, M.; Craig, P.S.; et al. Advances in diagnosis and spatial analysis of cysticercosis and taeniasis. Parasitology 2013, 140, 1578–1588. [Google Scholar] [CrossRef]
- Carabin, H.; Ndimubanzi, P.C.; Budke, C.M.; Nguyen, H.; Qian, L.D.; Cowan, Y.; Stoner, J.A.; Rainwater, E.; Dickey, M. Clinical manifestations associated with neurocysticercosis: A systematic review. PLoS Negl. Trop. Dis. 2011, 5, e1152. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization Model List of Essential Medicines—22nd List. 2021. Available online: https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2021.02 (accessed on 24 April 2022).
- Olliaro, P.L.; Vaillant, M.; Hayes, D.J.; Montresor, A.; Chitsulo, L. Practical dosing of praziquantel for schistosomiasis in preschool-aged children. Trop. Med. Int. Health 2013, 18, 1085–1089. [Google Scholar] [CrossRef]
- Liu, F.; Ranmal, S.; Batchelor, H.K.; Orlu-Gul, M.; Ernest, T.B.; Thomas, I.W.; Flanagan, T.; Kendall, R.; Tuleu, C. Formulation factors affecting acceptability of oral medicines in children. Int. J. Pharm. 2015, 492, 341–343. [Google Scholar] [CrossRef] [PubMed]
- Temer, A.C.; Teixeira, M.T.; Sa-Barreto, L.L.; Gratieri, T.; Gelfuso, G.M.; Silva, I.C.; Traveira, S.F.; Marreto, R.N.; Cunha-Filho, M. Subdivision of tablets containing modified delivery technology: The case of orally disintegrating tablets. J. Pharm. Innov. 2018, 13, 261–269. [Google Scholar] [CrossRef]
- Meyer, T.; Sekljic, H.; Fuchs, S.; Bothe, H.; Schollmeyer, D.; Miculka, C. Taste, a new incentive to switch to (R)-praziquantel in schistosomiasis treatment. PLoS Negl. Trop. Dis. 2009, 3, e357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garba, A.; Lamine, M.S.; Djibo, A.; Tahirou, A.; Aouami, M.A.; Alfari, A.; Phillips, A.E.; Fenwick, A.; Utzinger, J. Safety and efficacy of praziquantel syrup (Epiquantel®) against Schistosoma haematobium and Schistosoma mansoni in preschool-aged children in Niger. Acta Trop. 2013, 128, 318–325. [Google Scholar] [CrossRef]
- Gonzalez-Esquivel, D.; Rivera, J.; Castro, N.; Yepez-Mulia, L.; Helgi, J.C. In vitro characterization of some biopharmaceutical properties of praziquantel. Int. J. Pharm. 2005, 295, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Ferreira Marques, C.S.; Rezende, P.; Andrade, L.N.; Mendes, T.M.F.; Allegretti, M.; Bani, C.; Vinicius Chaud, M.; Batista de Almeida, M.; Souto, E.B.; Pereira da Costa, L.; et al. Solid dispersion of praziquantel enhanced solubility and improve the efficacy of the schistosomiasis treatment. J. Drug Deliv. Sci. Technol. 2018, 45, 124–134. [Google Scholar] [CrossRef]
- Borrego-Sánchez, A.; Sánchez-Espejo, R.; García-Villén, F.; Viseras, C.; Sainz-Díaz, I. Praziquantel–clays as accelerated release systems to enhance the low solubility of the drug. Pharmaceutics 2020, 12, 914. [Google Scholar] [CrossRef]
- The Pediatric Praziquantel Consortium. 2022. Available online: https://www.pediatricpraziquantelconsortium.org/ (accessed on 24 April 2022).
- Gonzalez, M.A.; Ramírez Rigo, M.; Gonzalez Vidal, N.L. Orphan formulations in pediatric Schistosomiasis treatment: Development and characterization of praziquantel nanoparticle-loaded powders for reconstitution. AAPS PharmSciTech 2019, 20, 318. [Google Scholar] [CrossRef]
- Münster, M.; Schoch, C.; Schmidt, C.; Breitkreutz, J. Multiparticulate system combining taste masking and immediate release properties for the aversive compound praziquantel. Eur. J. Pharm. Sci. 2017, 109, 446–454. [Google Scholar] [CrossRef]
- Albertini, B.; Perissutti, B.; Bertoni, S.; Zanolla, D.; Franceschinis, E.; Voinovich, D.; Lombardo, F.; Keise, J.; Passerini, N. Combining mechanochemistry and spray congealing for new praziquantel pediatric formulations in schistosomiasis treatment. Int. J. Mol. Sci. 2019, 20, 1233. [Google Scholar] [CrossRef] [Green Version]
- Boniatti, J.; Januskaite, P.; da Fonseca, L.B.; Viçosa, A.L.; Amendoeira, F.C.; Tuleu, C.; Basit, A.W.; Goyanes, A.; Ré, M.I. Direct powder extrusion 3d printing of praziquantel to overcome neglected disease formulation challenges in paediatric populations. Pharmaceutics 2021, 13, 1114. [Google Scholar] [CrossRef]
- Reinhard-Rupp, K.; Klohe, K. Developing a comprehensive response for treatment of children under 6 years of age with schistosomiasis: Research and development of a pediatric formulation of praziquantel. Infect. Dis. Poverty 2017, 6, 122. [Google Scholar] [CrossRef]
- Vieira, I.; Sousa, J.J.; Vitorino, C. Paediatric medicines—Regulatory drivers, restraints, opportunities and challenges. J. Pharm. Sci. 2021, 110, 1545–1556. [Google Scholar] [CrossRef]
- Pole, D.L. Physical and biological considerations for the use of nonaqueous solvents in oral bioavailability enhancement. J. Pharm. Sci. 2008, 97, 1071–1088. [Google Scholar] [CrossRef]
- Standing, J.F.; Tuleu, C. Paediatric formulations—Getting to the heart of the problem. Int. J. Pharm. 2005, 300, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Vogt, F.G.; Kord, A.S. Development of quality-by-design analytical methods. J. Pharm. Sci. 2011, 100, 797–812. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.X.; Amidon, G.; Khan, M.A.; Hoag, S.W.; Polli, J.; Raju, G.K.; Woodcock, J. Understanding pharmaceutical quality by design. AAPS J. 2014, 16, 771–783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soni, G.; Yadav, K.S.; Gupta, M.K. QbD based approach for formulation development of spray dried microparticles of erlotinib hydrochloride for sustained release. J. Drug Deliv. Sci. Technol. 2020, 57, 101684. [Google Scholar] [CrossRef]
- Rouaz, K.; Chiclana-Rodríguez, B.; Nardi-Ricart, A.; Suñé-Pou, M.; Mercadé-Frutos, D.; Suñé-Negre, J.M.; Pérez-Lozano, P.; García-Montoya, E. Excipients in the paediatric population: A review. Pharmaceutics 2021, 13, 387. [Google Scholar] [CrossRef]
- Drug Bank-Praziquantel. 2022. Available online: https://go.drugbank.com/drugs/DB01058 (accessed on 24 April 2022).
- Pruitt, A.; Anyan, W.; Hill, R.; Kauffman, R.; Mofenson, H.C.; Rumack, B.H.; Singer, H.S.; Spielberg, S. Ethanol in liquid preparations intended for children. Pediatrics 1984, 73, 405–407. [Google Scholar] [CrossRef]
- Marek, E.; Kraft, W.K. Ethanol pharmacokinetics in neonates and infants. Curr. Ther. Res. 2014, 76, 90–97. [Google Scholar] [CrossRef] [Green Version]
- Strickley, R.G. Solubilizing excipients in oral and injectable formulations. Pharm. Res. 2004, 21, 201–230. [Google Scholar] [CrossRef]
- Jelveghari, M.; Nokhodchi, A. Development and chemical stability studies of alcohol-free phenobarbital solution for use in pediatrics: A technical note. AAPS PharmSciTech 2008, 9, 939–943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos Souza, H.F.; Real, D.; Leonardi, D.; Rocha, S.C.; Alonso, V.; Serra, E.; Silber, A.M.; Salomon, C. Development and in vitro/in vivo evaluation of a novel benznidazole liquid dosage form using a quality-by-design approach. Trop. Med. Int. Health 2017, 22, 1514–1522. [Google Scholar] [CrossRef] [Green Version]
- Zheng, X.S.; Duan, C.Z.; Xiao, Z.D.; Yao, B.A. Transdermal delivery of praziquantel: Effects of solvents on permeation across rabbit skin. Biol. Pharm. Bull. 2008, 31, 1045–1048. [Google Scholar] [CrossRef] [Green Version]
- Li, W.; Farajtabar, A.; Xing, R.; Zhu, Y.; Zhao, H. Solubility of d-Histidine in aqueous cosolvent mixtures of N,N-dimethylformamide, ethanol, dimethyl sulfoxide, and N-methyl-2-pyrrolidone: Determination, preferential solvation, and solvent effect. J. Chem. Eng. Data 2020, 65, 1695–1704. [Google Scholar] [CrossRef]
- Agrawal, A.G.; Kumar, A.; Gide, P.S. Formulation of solid self-nanoemulsifying drug delivery systems using N-methyl pyrrolidone as cosolvent. Drug Dev. Ind. Pharm. 2015, 41, 594–604. [Google Scholar] [CrossRef]
- Rezaei, H.; Jouyban, A.; Acree, W.E.; Barzegar-Jalali, M.; Rahimpour, E. Solubility of codeine phosphate in N-methyl-2-pyrrolidone + 2-propanol mixture at different temperatures. J. Mol. Liq. 2020, 316, 113859. [Google Scholar] [CrossRef]
- Hatefi, A.; Rahimpour, E.; Ghafourian, T.; Martinez, F.; Barzegar-Jalali, M.; Jouyban, A. Solubility of ketoconazole in N-methyl-2-pyrrolidone + water mixtures at T = (293.2 to 313.2) K. J. Mol. Liq. 2019, 281, 150–155. [Google Scholar] [CrossRef]
- Moradi, M.; Rahimpour, E.; Zhao, H.; Martinez, F.; Jouyban, A. Solubility study of ketoconazole in the mixtures of N-methyl-2-pyrrolidone and ethanol at different temperatures. J. Mol. Liq. 2021, 326, 115287. [Google Scholar] [CrossRef]
- Gullapalli, R.P.; Mazzitelli, C.L. Polyethylene glycols in oral and parenteral formulations—A critical review. Int. J. Pharm. 2015, 496, 219–239. [Google Scholar] [CrossRef]
- Pereira, J.F.B.; Kurnia, K.A.; Freire, M.G.; Coutinho, J.A.P.; Rogers, R.D. Controlling the formation of ionic-liquid-based aqueous biphasic systems by changing the hydrogen-bonding ability of polyethylene glycol end groups. Chem. Phys. Chem. 2015, 16, 2219–2225. [Google Scholar] [CrossRef] [Green Version]
- Sanghvi, R.; Narazaki, R.; Machatha, S.G.; Yalkowsky, S.H. Solubility improvement of drugs using N-methyl pyrrolidone. AAPS PharmSciTech 2008, 9, 366–376. [Google Scholar] [CrossRef] [Green Version]
- Rahman, Z.; Siddiqui, A.; Khan, M.A. Assessing the impact of nimodipine devitrification in the ternary cosolvent system through quality by design approach. Int. J. Pharm. 2013, 455, 113–123. [Google Scholar] [CrossRef]
- Haby, M.M.; Sosa Leon, L.A.; Luciañez, A.; Nicholls, R.S.; Reveiz, L.; Donadeu, M. Systematic review of the effectiveness of selected drugs for preventive chemotherapy for Taenia solium taeniasis. PLoS Negl. Trop. Dis. 2020, 14, e0007873. [Google Scholar] [CrossRef] [PubMed]
- Rowe, V.; Wolf, M. Polyethylene Glycols. In Industrial Hygiene and Toxicology; Clayton, G.D., Clayton, F.E., Eds.; Wiley & Sons: New York, NY, USA, 1982; Volume 2. [Google Scholar]
- Scientific Panel on Food Additives FPA and M in C with F. Opinion of the Scientific Panel on Food Additives, Flavourings, Processing Aids and Materials in Contact with Food on a Request from the Commission Related to an Application on the Use of Polyethylene Glycol (PEG) as a Film Coating Agent for Use in Food Supplement Products. Available online: https://www.efsa.europa.eu/en/efsajournal/pub/414 (accessed on 24 April 2022).
- Thackaberry, E.A.; Kopytek, S.; Sherratt, P.; Trouba, K.; McIntyre, B. Comprehensive investigation of hydroxypropyl methylcellulose, propylene glycol, polysorbate 80, and hydroxypropyl-beta-cyclodextrin for use in general toxicology studies. Toxicol. Sci. 2010, 117, 485–492. [Google Scholar] [CrossRef] [Green Version]
- Allegaert, K. Propylene glycol in neonates: Never prescribed, frequently administered, hardly evaluated. J. Clin. Toxicol. 2012, 2, 1000e113. [Google Scholar] [CrossRef]
- Gad, S.C.; Spainhour, C.B.; Shoemake, C.; Pallman, D.R.; Stricker-Krongrad, A.; Downing, P.A.; Seals, R.E.; Eagle, L.A.; Polhamus, K.J. Daly. Tolerable levels of nonclinical vehicles and formulations used in studies by multiple routes in multiple species with notes on methods to improve utility. Int. J. Toxicol. 2016, 35, 95–178. [Google Scholar] [CrossRef] [Green Version]
- Acute Toxicity. Available online: https://www.ilo.org/legacy/english/protection/safework/ghs/ghsfinal/ghsc05.pdf (accessed on 13 June 2023).
- Agrawal, A.G.; Kumar, A.; Gide, P.S. Toxicity study of a self-nanoemulsifying drug delivery system containing N-methyl pyrrolidone. Drug Res. 2015, 65, 446–448. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.; Reader, S.; Field, E.; Shephard, A. Open-label taste-testing study to evaluate the acceptability of both strawberry-flavored and orange-flavored amylmetacresol/2,4-dichlorobenzyl alcohol throat lozenges in healthy children. Drugs R&D 2013, 13, 101–107. [Google Scholar] [CrossRef] [Green Version]
- Daruwala, J.B. Chewable Tablets. In Pharmaceutical Dosage Forms; Lieberman, H.L.L., Ed.; Marcel Dekker Inc.: New York, NY, USA, 1981; Volume 1, pp. 387–391. [Google Scholar]
- Mennella, J.A.; Spector, A.C.; Reed, D.R.; Coldwell, S.E. The bad taste of medicines: Overview of basic research on bitter taste. Clin. Ther. 2013, 35, 1225–1246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walsh, J.; Cram, A.; Woertz, K.; Breitkreutz, J.; Winzenburg, G.; Turner, R.; Tuleu, C. Playing hide and seek with poorly tasting paediatric medicines: Do not forget the excipients. Adv. Drug Deliv. Rev. 2014, 73, 14–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bravo, P.; Bertin, L.; Pinon, A.; Tortolano, L.; Fleury, T.; Raimbault, S.; Chachaty, E.; Annereau, M.; Lemare, F. Development and stability of an oral suspension of procarbazine in pediatrics. J. Drug Deliv. Sci. Technol. 2019, 49, 107–112. [Google Scholar] [CrossRef]
- Sohi, H.; Sultana, Y.; Khar, R.K. Taste masking technologies in oral pharmaceuticals: Recent developments and approaches. Drug Dev. Ind. Pharm. 2004, 30, 429–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cherian, S.; Lee, B.S.; Tucker, R.M.; Lee, K.; Smutzer, G. Toward improving medication adherence: The suppression of bitter taste in edible taste films. Adv. Pharmacol. Sci. 2018, 18, 8043837. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Promoting the Quality of Medicines (PQM). Product Information Report: Praziquantel; U.S. Pharmacopeial Convention: Rockville, MD, USA, 2019.
- Cheng, L.; Guo, S.; Wu, W. Characterization and in vitro release of praziquantel from poly(ε-caprolactone) implants. Int. J. Pharm. 2009, 377, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Salazar-Rojas, D.; Maggio, R.M.; Kaufman, T.S. Preparation and characterization of a new solid form of praziquantel, an essential anthelmintic drug. Praziquantel racemic monohydrate. Eur. J. Pharm. Sci. 2020, 146, 10526. [Google Scholar] [CrossRef]






| Cosolvent System 1 | Cosolvent System 2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Factors | Response | Factors | Response | ||||||
| PPG | PEG | W | PZQ (mg/mL) | NMP | PEG | W | PZQ (mg/mL) | ||
| 1 | 0.16 | 0.66 | 0.16 | 14.91 (0.24) | 15 | 0.16 | 0.66 | 0.16 | 10.60 (0.17) |
| 2 | 0.33 | 0.33 | 0.33 | 7.75 (0.42) | 16 | 0.33 | 0.33 | 0.33 | 7.74 (0.32) |
| 3 | 0.00 | 1.00 | 0.00 | 16.15 (0.14) | 17 | 0.00 | 1.00 | 0.00 | 19.19 (1.69) |
| 4 | 0.00 | 1.00 | 0.00 | 17.91 (0.27) | 18 | 0.00 | 1.00 | 0.00 | 17.42 (2.12) |
| 5 | 1.00 | 0.00 | 0.00 | 11.86 (1.06) | 19 | 1.00 | 0.00 | 0.00 | 146.70 (5.49) |
| 6 | 0.16 | 0.16 | 0.66 | 0.89 (0.01) | 20 | 0.16 | 0.16 | 0.66 | 1.73 (0.14) |
| 7 | 0.00 | 0.00 | 1.00 | 0.21 (0.02) | 21 | 0.00 | 0.00 | 1.00 | 0.22 (0.00) |
| 8 | 0.66 | 0.16 | 0.16 | 12.36 (0.33) | 22 | 0.66 | 0.16 | 0.16 | 39.71 (3.74) |
| 9 | 1.00 | 0.00 | 0.00 | 9.03 (0.38) | 23 | 1.00 | 0.00 | 0.00 | 141.70 (11.29) |
| 10 | 0.00 | 0.50 | 0.50 | 1.55 (0.05) | 24 | 0.00 | 0.50 | 0.50 | 1.42 (0.14) |
| 11 | 0.50 | 0.00 | 0.50 | 2.60 (0.01) | 25 | 0.50 | 0.00 | 0.50 | 4.00 (0.44) |
| 12 | 0.50 | 0.50 | 0.00 | 7.50 (0.19) | 26 | 0.50 | 0.50 | 0.00 | 50.04 (4.58) |
| 13 | 0.00 | 0.00 | 1.00 | 0.38 (0.02) | 27 | 0.00 | 0.00 | 1.00 | 0.21 (0.02) |
| 14 | 0.00 | 0.50 | 0.50 | 1.73 (0.05) | 28 | 0.00 | 0.50 | 0.50 | 1.75 (0.05) |
| Code Name | Composition |
|---|---|
| F1 | PZQ + co-solvent mixture |
| F2 | PZQ + co-solvent mixture + 0.2% of strawberry flavor + 30 mg of sucralose |
| F3 | PZQ + co-solvent mixture + 0.2% of mint flavor + 30 mg of sucralose |
| PZQ | 400 mg |
| PEG 400 | 1.6 mL |
| NMP | 6.6 mL |
| Water | 1.78 mL |
| Methyl paraben sodium salt | 10 mg |
| Sucralose | 30 mg |
| Mint flavor | 20 μL |
| Na2HPO4 | 66 mg |
| NaH2PO4 | 24 mg |
| Source | Sum of Squares | Mean Square | F Value | p-Value | |
|---|---|---|---|---|---|
| Cosolvent system 1 | Model | 514.34 | 102.87 | 85.20 | <0.0001 |
| PEG-PPG | 33.29 | 33.29 | 27.57 | 0.0012 | |
| PEG-water | 9.19 | 9.19 | 7.61 | 0.0281 | |
| PPG-water | 71.90 | 71.90 | 59.54 | 0.0001 | |
| Cosolvent system 2 | Model | 32,247.58 | 6449.52 | 161.37 | <0.0001 |
| PEG-NMP | 1178.95 | 1178.95 | 29.50 | 0.0006 | |
| PEG-water | 4790.56 | 4790.56 | 119.86 | <0.0001 | |
| NMP-water | 63.17 | 63.17 | 1.58 | 0.2441 |
| 1 Year Old (~10 kg) | 2 Years Old (~12.5 kg) | 4 Years Old (~16 kg) | 5 Years Old (~18 kg) | 7 Years Old (~23 kg) | ||
|---|---|---|---|---|---|---|
| A | 17% PPG, 66% PEG 400, 17% water | |||||
| Final volume (mL) to be administrated: | 3.37 | 4.22 | 5.40 | 6.08 | 7.77 | |
| mL PEG: | 2.26 | 2.82 | 3.62 | 4.07 | 5.20 | |
| mL PPG: | 0.57 | 0.71 | 0.91 | 1.03 | 1.32 | |
| 66% PPG, 17% PEG 400, 17% water | ||||||
| Final volume (mL) to be administrated: | 4.08 | 5.10 | 6.53 | 7.35 | 9.39 | |
| mL PEG: | 0.70 | 0.80 | 1.11 | 1.25 | 1.60 | |
| mL PPG: | 2.73 | 3.42 | 4.37 | 4.92 | 6.29 | |
| B | 17% NMP, 66% PEG 400, 17% water | |||||
| Final volume to be administrated: | 4.62 | 5.77 | 7.40 | 8.32 | 10.63 | |
| mL NMP: | 0.76 | 0.96 | 1.23 | 1.38 | 1.76 | |
| mL PEG: | 3.07 | 3.85 | 4.90 | 5.50 | 7.08 | |
| 66% NMP, 17% PEG 400, 17% water | ||||||
| Final volume to be administrated: | 1.13 | 1.41 | 1.80 | 2.03 | 2.60 | |
| mL NMP: | 0.75 | 0.94 | 1.20 | 1.36 | 1.73 | |
| mL PEG: | 0.19 | 0,24 | 0.30 | 0.34 | 0.44 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bedogni, G.; Garcia, P.; Seremeta, K.; Okulik, N.; Salomon, C. Preformulation and Long-Term Stability Studies of an Optimized Palatable Praziquantel Ethanol-Free Solution for Pediatric Delivery. Pharmaceutics 2023, 15, 2050. https://doi.org/10.3390/pharmaceutics15082050
Bedogni G, Garcia P, Seremeta K, Okulik N, Salomon C. Preformulation and Long-Term Stability Studies of an Optimized Palatable Praziquantel Ethanol-Free Solution for Pediatric Delivery. Pharmaceutics. 2023; 15(8):2050. https://doi.org/10.3390/pharmaceutics15082050
Chicago/Turabian StyleBedogni, Giselle, Paula Garcia, Katia Seremeta, Nora Okulik, and Claudio Salomon. 2023. "Preformulation and Long-Term Stability Studies of an Optimized Palatable Praziquantel Ethanol-Free Solution for Pediatric Delivery" Pharmaceutics 15, no. 8: 2050. https://doi.org/10.3390/pharmaceutics15082050