Motion Management: The Road Map to Accurate Radiation Treatment Delivery
Abstract
:1. Importance of Motion Management
2. Motion Management for Chest Location
2.1. The Benefit of DIBH for Treating Mediastinal Location
2.2. The Benefit of DIBH for Treating the Axillary Location
2.3. The Impact of Arm Positioning
2.4. The Benefit of Using an Incline Board
3. Motion Management for Abdominal Location
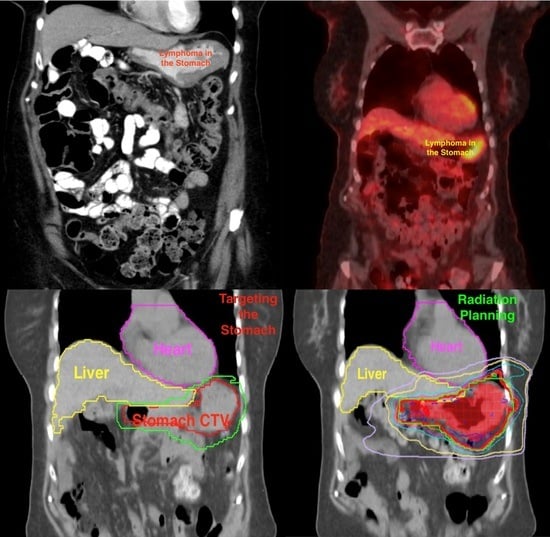
Treatment of the Stomach
4. Onboard Image Guidance and Adaptive Treatment Planning
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dabaja, B.; Perrin, K.J.; Romaguera, J.E.; Horace, P.; Wogan, C.F.; Shihadeh, F.; Salehpour, M.R. Successful treatment of a free-moving abdominal mass with radiation therapy guided by cone-beam computed tomography: A case report. J. Med. Case Rep. 2010, 4, 329. [Google Scholar] [CrossRef] [PubMed]
- Katsuta, T.; Matsuura, K.; Kashiwado, K. Analysis of Chronic Kidney Disease after Radiation Therapy for Gastric/Duodenal Mucosa-Associated Lymphoid Tissue Lymphoma. Adv. Radiat. Oncol. 2021, 6, 100788. [Google Scholar] [CrossRef] [PubMed]
- Chadha, A.S.; Liu, G.; Chen, H.C.; Das, P.; Minsky, B.D.; Mahmood, U.; Delclos, M.E.; Suh, Y.; Sawakuchi, G.O.; Beddar, S.; et al. Does Unintentional Splenic Radiation Predict Outcomes after Pancreatic Cancer Radiation Therapy? Int. J. Radiat. Oncol. Biol. Phys. 2017, 97, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Pinnix, C.C.; Smith, G.L.; Milgrom, S.; Osborne, E.M.; Reddy, J.P.; Akhtari, M.; Reed, V.; Arzu, I.; Allen, P.K.; Wogan, C.F.; et al. Predictors of radiation pneumonitis in patients receiving intensity modulated radiation therapy for Hodgkin and non-Hodgkin lymphoma. Int. J. Radiat. Oncol. Biol. Phys. 2015, 92, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Hahn, E.; Jiang, H.; Ng, A.; Bashir, S.; Ahmed, S.; Tsang, R.; Sun, A.; Gospodarowicz, M.; Hodgson, D. Late Cardiac Toxicity After Mediastinal Radiation Therapy for Hodgkin Lymphoma: Contributions of Coronary Artery and Whole Heart Dose-Volume Variables to Risk Prediction. Int. J. Radiat. Oncol. Biol. Phys. 2017, 98, 1116–1123. [Google Scholar] [CrossRef] [PubMed]
- Mulrooney, D.A.; Yeazel, M.W.; Kawashima, T.; Mertens, A.C.; Mitby, P.; Stovall, M.; Donaldson, S.S.; Green, D.M.; Sklar, C.A.; Robison, L.L.; et al. Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: Retrospective analysis of the Childhood Cancer Survivor Study cohort. BMJ 2009, 339, b4606. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.nccn.org/professionals/physician_gls/pdf/hodgkins.pdf (accessed on 31 August 2023).
- Aznar, M.C.; Maraldo, M.V.; Schut, D.A.; Lundemann, M.; Brodin, N.P.; Vogelius, I.R.; Berthelsen, A.K.; Specht, L.; Petersen, P.M. Minimizing late effects for patients with mediastinal Hodgkin lymphoma: Deep inspiration breath-hold, IMRT, or both? Int. J. Radiat. Oncol. Biol. Phys. 2015, 92, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.M.; Aznar, M.C.; Berthelsen, A.K.; Loft, A.; Schut, D.A.; Maraldo, M.; Josipovic, M.; Klausen, T.L.; Andersen, F.L.; Specht, L. Prospective phase II trial of image-guided radiotherapy in Hodgkin lymphoma: Benefit of deep inspiration breath-hold. Acta Oncol. 2015, 54, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Dabaja, B.S.; Rebueno, N.C.; Mazloom, A.; Thorne, S.; Perrin, K.J.; Tolani, N.; Das, P.; Delclos, M.E.; Iyengar, P.; Reed, V.K.; et al. Radiation for Hodgkin’s lymphoma in young female patients: A new technique to avoid the breasts and decrease the dose to the heart. Int. J. Radiat. Oncol. Biol. Phys. 2011, 79, 503–507. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Milgrom, S.A.; Dabaja, B.S.; Smith, G.L.; Martel, M.; Pinnix, C.C. Daily CT guidance improves target coverage during definitive radiation therapy for gastric MALT lymphoma. Pract. Radiat. Oncol. 2017, 7, e471–e478. [Google Scholar] [CrossRef] [PubMed]
- Christopherson, K.M.; Gunther, J.R.; Fang, P.; Peterson, S.L.; Roach, K.E.; Wong, P.F.; Mirkovic, D.; Lim, T.Y.; Wang, H.; Wang, X.A.; et al. Decreased heart dose with deep inspiration breath hold for the treatment of gastric lymphoma with IMRT. Clin. Transl. Radiat. Oncol. 2020, 24, 79–82. [Google Scholar] [CrossRef] [PubMed]










Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dabaja, B.; Wu, S.; Short, N.J. Motion Management: The Road Map to Accurate Radiation Treatment Delivery. Lymphatics 2024, 2, 1-9. https://doi.org/10.3390/lymphatics2010001
Dabaja B, Wu S, Short NJ. Motion Management: The Road Map to Accurate Radiation Treatment Delivery. Lymphatics. 2024; 2(1):1-9. https://doi.org/10.3390/lymphatics2010001
Chicago/Turabian StyleDabaja, Bouthaina, Susan Wu, and Nicholas J. Short. 2024. "Motion Management: The Road Map to Accurate Radiation Treatment Delivery" Lymphatics 2, no. 1: 1-9. https://doi.org/10.3390/lymphatics2010001