Simultaneous PSI-Based Orthognathic and PEEK Bone Augmentation Surgery Leads to Improved Symmetric Facial Appearance in Craniofacial Malformations
Abstract
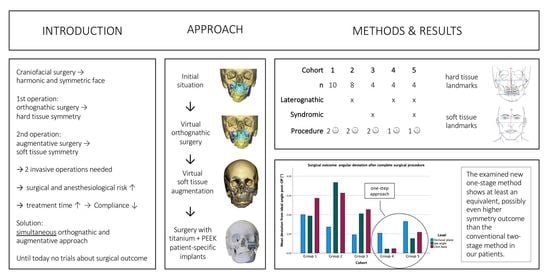
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Planning Protocol
2.3. Surgical Approach
2.4. Collection of Landmarks and Axes
2.4.1. Photographic Analysis
2.4.2. Radiological Analysis
2.5. Analyses of Symmetry
2.6. Statistical Analyses
2.7. Error Study
3. Results
3.1. Comparing Angular Deviations Pre- versus Postoperatively
3.2. Angular Normalization in Soft Tissue
3.3. Angular Normalization in Hard Tissue
3.4. Comparing Linear Distance Discrepancy Pre- versus Post-Op
3.5. Correlation between Asymmetry and Extent of Normalization
3.6. Multivariable Regression
3.7. Difference of Normalization between Pure Conventional Surgery and Simultaneous PEEK Bone Augmentation
3.8. Outcome after Surgical Treatment
4. Discussion
4.1. Results
4.1.1. Correlation between Severity of Disease and Extent of Normalization
4.1.2. Multivariable Regression
4.1.3. Comparison between Conventional Orthognathic Procedure and Simultaneous PEEK Bone Augmentation
4.1.4. Complications of PEEK Implants
4.2. Validity and Reliability
4.3. Limitations
4.4. Clinical Considerations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kronmiller, J.E. Development of asymmetries. In Seminars in Orthodontics; Elsevier: Amsterdam, The Netherlands, 1998. [Google Scholar]
- Cao, J.; Shen, S.; Liu, Z.; Dai, J.; Wang, X. Evaluation of mandibular symmetry in patients with condylar osteochondroma who underwent intro-oral condylar resection and simultaneous bimaxillary orthognathic surgery. J. Craniofacial Surg. 2020, 31, 1390–1394. [Google Scholar] [CrossRef] [PubMed]
- Bailey, L.J.; Collie, F.M.; White, R.P., Jr. Long-term soft tissue changes after orthognathic surgery. Int. J. Adult Orthod. Orthognath. Surg. 1996, 11, 7–18. [Google Scholar]
- Betts, N.J.; Dowd, K.F. Soft tissue changes associated with orthognathic surgery. Atlas Oral Maxillofac. Surg. Clin. 2000, 8, 13–38. [Google Scholar] [CrossRef]
- Jung, J.; Lee, C.H.; Lee, J.W.; Choi, B.J. Three dimensional evaluation of soft tissue after orthognathic surgery. Head Face Med. 2018, 14, 21. [Google Scholar] [CrossRef]
- Vásquez, B.; Olate, S.; Cantín, M.; Sandoval, C.; Fariña, R.; Del Sol, M. Histopathological analysis of unilateral condylar hyperplasia: Difficulties in diagnosis and characterization of the disease. Int. J. Oral Maxillofac. Surg. 2016, 45, 601–609. [Google Scholar] [CrossRef]
- Mommaerts, M.Y. Guidelines for patient-specific jawline definition with titanium implants in esthetic, deformity, and malformation surgery. Ann. Maxillofac. Surg. 2016, 6, 287. [Google Scholar] [CrossRef] [Green Version]
- Hull, C.W. Apparatus for Production of Three-Dimensional Objects by Stereolithography. U.S. Patent No. 638905, 11 March 1986. [Google Scholar]
- Tack, P.; Victor, J.; Gemmel, P.; Annemans, L. 3D-printing techniques in a medical setting: A systematic literature review. Biomed. Eng. Online 2016, 15, 115. [Google Scholar] [CrossRef] [Green Version]
- Whitaker, M. The history of 3D printing in healthcare. Bull. R. Coll. Surg. Engl. 2014, 96, 228–229. [Google Scholar] [CrossRef]
- Hsu, S.S.-P.; Gateno, J.; Bell, R.B.; Hirsch, D.L.; Markiewicz, M.R.; Teichgraeber, J.F.; Zhou, X.; Xia, J.J. Accuracy of a computer-aided surgical simulation protocol for orthognathic surgery: A prospective multicenter study. J. Oral Maxillofac. Surg. 2013, 71, 128–142. [Google Scholar] [CrossRef] [Green Version]
- Centenero, S.A.-H.; Hernández-Alfaro, F. 3D planning in orthognathic surgery: CAD/CAM surgical splints and prediction of the soft and hard tissues results–our experience in 16 cases. J. Cranio-Maxillofac. Surg. 2012, 40, 162–168. [Google Scholar] [CrossRef]
- Zinser, M.J.; Mischkowski, R.A.; Sailer, H.F.; Zöller, J.E. Computer-assisted orthognathic surgery: Feasibility study using multiple CAD/CAM surgical splints. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 113, 673–687. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Alfaro, F.; Guijarro-Martinez, R. New protocol for three-dimensional surgical planning and CAD/CAM splint generation in orthognathic surgery: An in vitro and in vivo study. Int. J. Oral Maxillofac. Surg. 2013, 42, 1547–1556. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Zhang, L.; Sun, H.; Yuan, J.; Shen, S.G.; Wang, X. A novel method of computer aided orthognathic surgery using individual CAD/CAM templates: A combination of osteotomy and repositioning guides. Br. J. Oral Maxillofac. Surg. 2013, 51, e239–e244. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Wei, H.; Jiang, T.; Qian, Y.; Zhang, T.; Yu, H.; Zhang, L.; Wang, X. Randomized Clinical Trial of the Accuracy of Patient-Specific Implants versus CAD/CAM Splints in Orthognathic Surgery. Plast. Reconstr. Surg. 2021, 148, 1101–1110. [Google Scholar] [CrossRef] [PubMed]
- Alasseri, N.; Alasraj, A. Patient-specific implants for maxillofacial defects: Challenges and solutions. Maxillofac. Plast. Reconstr. Surg. 2020, 42, 15. [Google Scholar] [CrossRef] [PubMed]
- Olate, S.; Huetequeo-Molina, C.; Requena, R.; Uribe, F. Patient Specific Implants to Solve Structural Facial Asymmetry after Orthognathic Surgery. J. Craniofacial Surg. 2021, 32, e269–e271. [Google Scholar] [CrossRef]
- Saponaro, G.; Doneddu, P.; Gasparini, G.; Staderini, E.; Boniello, R.; Todaro, M.; D’Amato, G.; Pelo, S.; Moro, A. Custom made onlay implants in peek in maxillofacial surgery: A volumetric study. Child’s Nerv. Syst. 2020, 36, 385–391. [Google Scholar] [CrossRef]
- Gander, T.; Bredell, M.; Eliades, T.; Rücker, M.; Essig, H. Splintless orthognathic surgery: A novel technique using patient-specific implants (PSI). J. Cranio-Maxillofac. Surg. 2015, 43, 319–322. [Google Scholar] [CrossRef]
- Suojanen, J.; Leikola, J.; Stoor, P. The use of patient-specific implants in orthognathic surgery: A series of 30 mandible sagittal split osteotomy patients. J. Cranio-Maxillofac. Surg. 2017, 45, 990–994. [Google Scholar] [CrossRef] [Green Version]
- Suojanen, J.; Leikola, J.; Stoor, P. The use of patient-specific implants in orthognathic surgery: A series of 32 maxillary osteotomy patients. J. Cranio-Maxillofac. Surg. 2016, 44, 1913–1916. [Google Scholar] [CrossRef] [Green Version]
- Rückschloß, T.; Ristow, O.; Müller, M.; Kühle, R.; Zingler, S.; Engel, M.; Hoffmann, J.; Freudlsperger, C. Accuracy of patient-specific implants and additive-manufactured surgical splints in orthognathic surgery—A three-dimensional retrospective study. J. Cranio-Maxillofac. Surg. 2019, 47, 847–853. [Google Scholar] [CrossRef]
- Rammos, C.K.; Cayci, C.; Castro-Garcia, J.A.; Feiz-Erfan, I.; Lettieri, S.C. Patient-specific polyetheretherketone implants for repair of craniofacial defects. J. Craniofacial Surg. 2015, 26, 631–633. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jalbert, F.; Boetto, S.; Nadon, F.; Lauwers, F.; Schmidt, E.; Lopez, R. One-step primary reconstruction for complex craniofacial resection with PEEK custom-made implants. J. Cranio-Maxillofac. Surg. 2014, 42, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Song, W.-C.; Koh, K.-S.; Kim, S.-H.; Hu, K.-S.; Kim, H.-J.; Park, J.-C.; Choi, B.-Y. Horizontal angular asymmetry of the face in korean young adults with reference to the eye and mouth. J. Oral Maxillofac. Surg. 2007, 65, 2164–2168. [Google Scholar] [CrossRef] [PubMed]
- Scolozzi, P.; Martinez, A.; Jaques, B. Complex orbito-fronto-temporal reconstruction using computer-designed PEEK implant. J. Craniofacial Surg. 2007, 18, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Panayotov, I.V.; Orti, V.; Cuisinier, F.; Yachouh, J. Polyetheretherketone (PEEK) for medical applications. J. Mater. Sci. Mater. Med. 2016, 27, 1–11. [Google Scholar] [CrossRef]
- Lommen, J.; Schorn, L.; Sproll, C.; Haussmann, J.; Kübler, N.R.; Budach, W.; Rana, M.; Tamaskovics, B. Reduction of CT Artifacts Using Polyetheretherketone (PEEK), Polyetherketoneketone (PEKK), Polyphenylsulfone (PPSU), and Polyethylene (PE) Reconstruction Plates in Oral Oncology. J. Oral Maxillofac. Surg. 2022, 80, 1272–1283. [Google Scholar] [CrossRef]
- Scolozzi, P. Computer-aided design and computer-aided modeling (CAD/CAM) generated surgical splints, cutting guides and custom-made implants: Which indications in orthognathic surgery? Rev. Stomatol. Chir. Maxillo-Faciale Chir. Orale 2015, 116, 343–349. [Google Scholar] [CrossRef]
- Staal, F.; Pluijmers, B.; Wolvius, E.; Koudstaal, M. Patient-specific implant for residual facial asymmetry following orthognathic surgery in unilateral craniofacial microsomia. Craniomaxillofacial Trauma Reconstr. 2016, 9, 264–267. [Google Scholar] [CrossRef] [Green Version]
- Neovius, E.; Engstrand, T. Craniofacial reconstruction with bone and biomaterials: Review over the last 11 years. J. Plast. Reconstr. Aesthetic Surg. 2010, 63, 1615–1623. [Google Scholar] [CrossRef]
- Lee, J.H.; Kaban, L.B.; Yaremchuk, M.J. Refining post–orthognathic surgery facial contour with computer-designed/computer-manufactured alloplastic implants. Plast. Reconstr. Surg. 2018, 142, 747–755. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Marcinkiewicz, A.G.; Stricker, P.A. Craniofacial surgery and specific airway problems. Pediatr. Anesth. 2020, 30, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Nurminen, L.; Pietilä, T.; Vinkka-Puhakka, H. Motivation for and satisfaction with orthodontic-surgical treatment: A retrospective study of 28 patients. Eur. J. Orthod. 1999, 21, 79–87. [Google Scholar] [CrossRef] [Green Version]
- Sannino, G.; Gloria, F.; Schiavetti, R.; Ottria, L.; Barlattani, A. Dental Wings CAD/CAM system precision: An internal and marginal fit sperimental analisys. Oral Implant. (Rome) 2009, 2, 11–20. [Google Scholar]
- Perrett, D.I.; Burt, D.M.; Penton-Voak, I.S.; Lee, K.J.; Rowland, D.A.; Edwards, R. Symmetry and human facial attractiveness. Evol. Hum. Behav. 1999, 20, 295–307. [Google Scholar] [CrossRef]
- Spiessl, B. Osteosynthesis in sagittal osteotomy using the Obwegeser-Dal Pont method. Fortschr. Der Kiefer-Und Gesichts-Chir. 1974, 18, 145–148. [Google Scholar]
- Ko, E.W.-C.; Huang, C.S.; Chen, Y.R. Characteristics and corrective outcome of face asymmetry by orthognathic surgery. J. Oral Maxillofac. Surg. 2009, 67, 2201–2209. [Google Scholar] [CrossRef]
- Ma, H.; Suonan, A.; Zhou, J.; Yuan, Q.; Liu, L.; Zhao, X.; Lou, X.; Yang, C.; Li, D.; Zhang, Y.-G. PEEK (Polyether-ether-ketone) and its composite materials in orthopedic implantation. Arab. J. Chem. 2021, 14, 102977. [Google Scholar] [CrossRef]
- Hajeer, M.Y.; Ayoub, A.F.; Millett, D.T. Three-dimensional assessment of facial soft-tissue asymmetry before and after orthognathic surgery. Br. J. Oral Maxillofac. Surg. 2004, 42, 396–404. [Google Scholar] [CrossRef]
- Wermker, K.; Kleinheinz, J.; Jung, S.; Dirksen, D. Soft tissue response and facial symmetry after orthognathic surgery. J. Cranio-Maxillofac. Surg. 2014, 42, e339–e345. [Google Scholar] [CrossRef]
- Da Pozzo, F.; Gibelli, D.; Beltramini, G.A.; Dolci, C.; Giannì, A.B.; Sforza, C. The effect of orthognathic surgery on soft-tissue facial asymmetry: A longitudinal three-dimensional analysis. J. Craniofacial Surg. 2020, 31, 1578–1582. [Google Scholar] [CrossRef] [PubMed]
- Punchak, M.; Chung, L.K.; Lagman, C.; Bui, T.T.; Lazareff, J.; Rezzadeh, K.; Jarrahy, R.; Yang, I. Outcomes following polyetheretherketone (PEEK) cranioplasty: Systematic review and meta-analysis. J. Clin. Neurosci. 2017, 41, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Trpkova, B.; Major, P.; Nebbe, B.; Prasad, N. Craniofacial asymmetry and temporomandibular joint internal derangement in female adolescents: A posteroanterior cephalometric study. Angle Orthod. 2000, 70, 81–88. [Google Scholar] [PubMed]
- Yousefi, F.; Rafiei, E.; Mahdian, M.; Mollabashi, V.; Saboonchi, S.S.; Hosseini, S.M. Comparison efficiency of posteroanterior cephalometry and cone-beam computed tomography in detecting craniofacial asymmetry: A systematic review. Contemp. Clin. Dent. 2019, 10, 358. [Google Scholar]
- Rossi, M.; Ribeiro, E.; Smith, R. Craniofacial asymmetry in development: An anatomical study. Angle Orthod. 2003, 73, 381–385. [Google Scholar]
- Namano, S.; Behrend, D.A.; Harcourt, J.K.; Wilson, P.R. Angular asymmetries of the human face. Int. J. Prosthodont. 2000, 13, 41–46. [Google Scholar]
- Giovanoli, P.; Tzou, C.-H.; Ploner, M.; Frey, M. Three-dimensional video-analysis of facial movements in healthy volunteers. Br. J. Plast. Surg. 2003, 56, 644–652. [Google Scholar] [CrossRef]
- Ferrario, V.F.; Sforza, C.; Poggio, C.E.; Tartaglia, G. Distance from symmetry: A three-dimensional evaluation of facial asymmetry. J. Oral Maxillofac. Surg. 1994, 52, 1126–1132. [Google Scholar] [CrossRef]
- Garrahy, A.M. Three-Dimensional Assessment of Dentofacial Deformity in Children with Clefts; University of Glasgow: Glasgow, Scotland, 2002. [Google Scholar]
- McIntyre, G.; Mossey, P. Asymmetry of the parental craniofacial skeleton in orofacial clefting. J. Orthod. 2002, 29, 299–305. [Google Scholar] [CrossRef]
- World Health Organization. The International Statistical Classification of Diseases and Health Related Problems ICD-10: Tenth Revision. Volume 1: Tabular List; World Health Organization: Geneva, Switzerland, 2004; Volume 1. [Google Scholar]
- Gateno, J.; Alfi, D.; Xia, J.J.; Teichgraeber, J.F. A geometric classification of jaw deformities. J. Oral Maxillofac. Surg. 2015, 73, S26. [Google Scholar] [CrossRef] [Green Version]
- Kotaniemi, K.V.; Heliövaara, A.; Kotaniemi, M.; Stoor, P.; Leikola, J.; Palotie, T.; Suojanen, J. Comparison of postoperative skeletal stability of maxillary segments after Le Fort I osteotomy, using patient-specific implant versus mini-plate fixation. J. Cranio-Maxillofac. Surg. 2019, 47, 1020–1030. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goodson, M.; Farr, D.; Keith, D.; Banks, R. Use of two-piece polyetheretherketone (PEEK) implants in orbitozygomatic reconstruction. Br. J. Oral Maxillofac. Surg. 2012, 50, 268–269. [Google Scholar] [CrossRef] [PubMed]
- Kalmar, C.L.; Humphries, L.S.; Zimmerman, C.E.; Vu, G.H.; Swanson, J.W.; Bartlett, S.P.; Taylor, J.A. Orthognathic Hardware Complications in the Era of Patient-Specific Implants. Plast. Reconstr. Surg. 2020, 146, 609e–621e. [Google Scholar] [CrossRef]
- Deng, L.; Deng, Y.; Xie, K. AgNPs-decorated 3D printed PEEK implant for infection control and bone repair. Colloids Surf. B Biointerfaces 2017, 160, 483–492. [Google Scholar] [CrossRef] [PubMed]
- Thien, A.; King, N.K.; Ang, B.T.; Wang, E.; Ng, I. Comparison of polyetheretherketone and titanium cranioplasty after decompressive craniectomy. World Neurosurg. 2015, 83, 176–180. [Google Scholar] [CrossRef]
- Arcas Pons, A.; Vendrell, G.; Cuesta, F.; Bermejo, L.; Piqué i Clusella, N. Mandibular angle augmentation using customized PEEK implants and guides generated with 3D Planning and Printing: Case estudies. Ann. Case Rep. 2020, 14, 511. [Google Scholar]
















| # | Laterognathy | Syndrome | Surgical Procedure | n |
|---|---|---|---|---|
| 1 | non-laterognathic | non-syndromic | orthognathic surgery | 10 |
| 2 | laterognathic | non-syndromic | orthognathic surgery | 8 |
| 3 | non-laterognathic | syndromic | orthognathic surgery | 4 |
| 4 | laterognathic | non-syndromic | orthognathic surgery + augmentation | 4 |
| 5 | laterognathic | syndromic | orthognathic surgery + augmentation | 4 |
| Points | Abbreviation | Description |
|---|---|---|
| 1–2 | ALE | Axis of lateral eyebrows |
| 3–4 | BL | Bipupillary line |
| 5–6 | AT | Axis of tragi |
| 7–8 | AMA | Axis of mouth angle |
| 9–10 | AJA | Axis of jaw angles |
| 11–12 | CB | Chin baseline |
| 13–14 | MP | Midfacial plane |
| Points | Abbreviation | Description |
|---|---|---|
| 1–2 | ALOR | Axis of lateral orbital walls |
| 3–4 | AOF | Axis of orbital floors |
| 5–6 | ATMJ | Axis of temporomandibular joints |
| 7–8 | OP | Occlusal plane |
| 9–10 | AJA | Axis of jaw angles |
| 11–12 | CB | Chin baseline |
| 13–14 | MP | Midfacial plane |
| Points | Abbreviation | Description |
|---|---|---|
| 1–2; 2–3 | DLZB | Right and left distances of lat. zygomatic bone |
| 4–5; 5–6 | DOP | Right and left distances of occlusal plane |
| 7–8; 8–9 | DJA | Right and left distances of jaw angle |
| Unstd. B | Coeff. Std. Error | Std. Coeff. Beta | t | Sig. | 95 % Conf. Int. | ||
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| (Constant) | −0.285 | 0.295 | −0.966 | 0.345 | −0.900 | 0.330 | |
| PEEK Augmentation yes (1) or no (0) | −0.817 | 0.630 | −0.271 | −1.296 | 0.210 | −2.131 | 0.498 |
| Baseline Soft Tissue Deviation from Ideal | 0.176 | 0.093 | 0.395 | 1.888 | 0.074 | −0.018 | 0.370 |
| Postoperative Bony Deviation from Ideal | −0.146 | 0.132 | −0.220 | −1.106 | 0.282 | −0.422 | 0.130 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kerkfeld, V.; Schorn, L.; Depprich, R.; Lommen, J.; Wilkat, M.; Kübler, N.; Rana, M.; Meyer, U. Simultaneous PSI-Based Orthognathic and PEEK Bone Augmentation Surgery Leads to Improved Symmetric Facial Appearance in Craniofacial Malformations. J. Pers. Med. 2022, 12, 1653. https://doi.org/10.3390/jpm12101653
Kerkfeld V, Schorn L, Depprich R, Lommen J, Wilkat M, Kübler N, Rana M, Meyer U. Simultaneous PSI-Based Orthognathic and PEEK Bone Augmentation Surgery Leads to Improved Symmetric Facial Appearance in Craniofacial Malformations. Journal of Personalized Medicine. 2022; 12(10):1653. https://doi.org/10.3390/jpm12101653
Chicago/Turabian StyleKerkfeld, Valentin, Lara Schorn, Rita Depprich, Julian Lommen, Max Wilkat, Norbert Kübler, Majeed Rana, and Ulrich Meyer. 2022. "Simultaneous PSI-Based Orthognathic and PEEK Bone Augmentation Surgery Leads to Improved Symmetric Facial Appearance in Craniofacial Malformations" Journal of Personalized Medicine 12, no. 10: 1653. https://doi.org/10.3390/jpm12101653