Influence of Shortened Tongue Frenulum on Tongue Mobility, Speech and Occlusion
Abstract
:1. Introduction
2. Materials and Methods
- -
- No history of frenulectomy (surgical excision of the frenulum), frenotomy (the snipping and slightly relocation of the frenulum), frenulotomy (transverse incision of the frenulum at its base) or any soft tissue surgery in the oral cavity (except tooth extractions or chiseling);
- -
- No history of speech or swallowing therapy;
- -
- No previous or ongoing orthodontic treatment;
- -
- Preserved supporting zones in the lateral sections (with possible single teeth missing);
- -
- Present permanent lower central and lateral incisors;
- -
- Lack of calculus on the lingual surfaces of the lower anterior teeth.



- Lifting the tongue up towards the palate;
- Lowering the tongue;
- Touching the incisive papilla with the tip of the tongue;
- Touching the inside of the cheeks on both sides with the tip of the tongue;
- Moving the tongue sideways to the corners of the mouth;
- Protrusion of the tongue on the chin.
3. Results
3.1. The Effect of Ankyloglossia on Tongue Function during Swallowing
3.2. The Effect of Ankyloglossia on Tongue Mobility
3.3. The Effect of Ankyloglossia on the Presence of Dysglossia
3.4. The Effect of Shortened Tongue Frenulum on the Occurrence of Malocclusion or Crowding
3.5. The Effect of Ankyloglossia on Periodontal Status
4. Discussion
4.1. Effect of Shortened Tongue Frenulum on Tongue Function during Swallowing
4.2. Effect of Ankyloglossia on Tongue Mobility
4.3. Effect of Ankyloglossia on Speech Abnormalities and Dysglossia Prevalence
4.4. Effect of Ankyloglossia on Dental and Malocclusion Disorders
4.5. Effect of Ankyloglossia on Periodontium
5. Conclusions
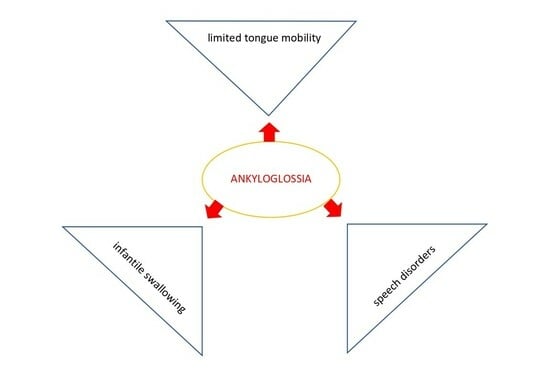
- A short tongue frenulum negatively influences swallowing and is associated with an “infantile swallowing pattern”.
- Moderate or severe ankyloglossia significantly limits tongue mobility.
- A short tongue frenulum negatively influences speech.
- Ankyloglossia is associated with higher prevalence of malocclusion.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wallace, A.F. Tongue tie. Lancet 1963, 2, 377–378. [Google Scholar] [CrossRef] [PubMed]
- Marchesan, I.Q. Lingual frenulum: Quantitative evaluation proposal. Int. J. Orofacial. Myol. 2005, 31, 39–48. [Google Scholar] [CrossRef]
- Stańczyk, K.; Ciok, E.; Perkowski, K.; Zadurska, M. Ankyloglossia—A literature review. Forum Ort. 2015, 11, 123–133. [Google Scholar]
- Ballard, J.L.; Auer, C.E.; Khoury, J.C. Ankyloglossia assessment, incidence and effect of frenuloplasty on the breastfeeding. Pediatrics 2002, 110, 63. [Google Scholar] [CrossRef] [PubMed]
- Segan, L.M.; Stephenson, S.; Dawes, M.; Feldman, P. Prevalence, diagnosis, and treatment of ankyloglossia. Methodologic review. Can. Fam. Physician 2007, 53, 1027–1033. [Google Scholar]
- Messner, A.H.; Lalakea, M.L. Ankyloglossia: Controversies in management. Int. J. Pediatr. Otorhinolaryngol. 2000, 54, 123–131. [Google Scholar] [CrossRef]
- Suter, V.; Bornstein, M.M. Ankyloglossia: Facts and myths in diagnosis and treatment. J. Periodontol. 2009, 80, 1204–1219. [Google Scholar] [CrossRef]
- Moore, G.E.; Ivens, A.; Chambers, J.; Farrall, M.; Williamson, R.; Page, D.C.; Bjornsson, A.; Arnason, A.; Jensson, O. Linkage of an X-chromosome cleft palate gene. Nature 1987, 326, 91–92. [Google Scholar] [CrossRef]
- Pola, M.; Garcia, M.G.; Martin, J.M.G.; Gallas, M.; Lestón, J.S. A study of pathology associated with short lingual frenum. ASDC J. Dent. Child. 2002, 69, 59–62. [Google Scholar]
- Burdick, A.B.; Ma, L.A.; Dai, Z.H.; Gao, N.N. Van der Woude syndrome in two families in China. J. Craniofac. Genet. Dev. Biol. 1987, 7, 413–418. [Google Scholar]
- Morowati, S.; Yasini, M.; Ranjbar, R.; Peivandi, A.A.; Ghadami, M. Familial ankyloglossia (tongue-tie): A case report. Acta Medica Iran. 2010, 48, 123–124. [Google Scholar]
- Kantaputra, P.N.; Paramee, M.; Kaewkhampa, A.; Hoshino, A.; Lees, M.; McEntagart, M.; Masrour, N.; Moore, G.E.; Pauws, E.; Stanier, P. Cleft lip with cleft palate, ankyloglossia, and hypodontia are associated with TBX22 mutations. J. Dent. Res. 2011, 90, 450–455. [Google Scholar] [CrossRef] [PubMed]
- Meinecke, P.; Blunck, W.; Rodewald, A. Opitz syndrome. Am. J. Med. Genet. 1987, 28, 735–739. [Google Scholar] [CrossRef] [PubMed]
- Neri, G.; Gurrieri, F.; Zanni, G.; Lin, A. Clinical and molecular aspects of the Simpson Golabi Behmel syndrome. Am. J. Med. Genet. 1998, 79, 279–283. [Google Scholar] [CrossRef]
- Braybrook, C.; Doudney, K.; Marçano, A.C.B.; Arnason, A.; Bjornsson, A.; Patton, M.A.; Goodfellow, P.J.; Moore, G.E.; Stanier, P. The T-box transcription factor gene TBX22 is mutated in X-linked cleft palate and ankyloglossia. Nat. Genet. 2001, 29, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Han, S.H.; Kim, M.C.; Choi, Y.S.; Lim, J.S.; Han, K.T. A study on the genetic inheritance of ankyloglossia based on pedigree analysis. Arch. Plast. Surg. 2012, 39, 329–332. [Google Scholar] [CrossRef] [PubMed]
- Janiszewska-Olszowska, J.; Gawrych, E.; Dydyk, A.; Studniak, E.; Biaduń-Popławska, A.; Zajączek, S. Oropalatal dysplasia Bettex-Graf–clinical findings, genetic background, treatment. J. Craniomaxillofac. Surg. 2013, 41, 29–32. [Google Scholar] [CrossRef]
- Hacham-Zadeh, S.; Garfunkel, A.A. Kindler syndrome in two related Kurdish families. Am. J. Med. Genet. 1985, 20, 43–48. [Google Scholar] [CrossRef]
- Yoon, A.; Zaghi, S.; Weitzman, R.; Ha, S.; Law, C.S.; Guilleminault, C.; Liu, S.Y. Toward a functional definition of ankyloglossia: Validating current grading scales for lingual frenulum length and tongue mobility in 1052 subjects. Sleep Breath. 2017, 21, 767–775. [Google Scholar] [CrossRef]
- Ruffoli, R.; Giambelluca, M.A.; Scavuzzo, M.C.; Bonfigli, D.; Cristofani, R.; Gabriele, M.; Giuca, M.R.; Giannessi, F. Ankyloglossia: A morphofunctional investigation in children. Oral Dis. 2005, 11, 170–174. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: https://www.R-project.org/ (accessed on 27 November 2023).
- Wickham, H.; Bryan, J. Readxl: Read Excel Files R Package Version 1.3.1. 2019. Available online: https://CRAN.R-project.org/package=readxl (accessed on 27 November 2023).
- Lüdecke, D. sjmisc: Data and variable transformation functions. J. Open Source Softw. 2018, 3, 754. [Google Scholar] [CrossRef]
- Lüdecke, D. sjPlot: Data Visualization for Statistics in Social Science. R Package Version 2.8.9. 2021. Available online: https://CRAN.R-project.org/package=sjPlot (accessed on 27 November 2023).
- Makowski, D.; Ben-Shachar, M.S.; Patil, I.; Lüdecke, D. Automated Results Reporting as a Practical Tool to Improve Reproducibility and Methodological Best Practices Adoption. CRAN. 2020. Available online: https://github.com/easystats/report (accessed on 27 November 2023).
- Mangiafico, S. rcompanion: Functions to Support Extension Education Program Evaluation. R Package Version 2.4.13. 2022. Available online: https://CRAN.R-project.org/package=rcompanion (accessed on 27 November 2023).
- Jang, S.J.; Cha, B.K.; Ngan, P.; Choi, D.S.; Lee, S.K.; Jang, I. Relationship between the lingual frenulum and craniofacial morphology in adults. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Messner, A.H.; Lalakea, M.L. The effect of ankyloglossia on speech in children. Otolaryngol. Head Neck Surg. 2002, 127, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Park, H.S.; Park, B.S.; Choi, J.W.; Koo, S.K. The improvement of tongue mobility and articulation after frenotomy in patient with ankyloglossia. Korean J. Otorhinolaryngol. Head Neck Surg. 2010, 53, 491–496. [Google Scholar] [CrossRef]
- Meenakshi, S.; Jagannathan, N. Assessment of lingual frenulum lengths in skeletal malocclusion. J. Clin. Diagn. Res. 2014, 8, 202–204. [Google Scholar] [PubMed]
- Vaz, A.C.; Bai, P.M. Lingual frenulum and malocclusion: An overlooked tissue or a minor issue. Indian J. Dent. Res. 2015, 26, 488–492. [Google Scholar] [CrossRef]
- Kotlow, L.A. Ankyloglossia (tongue-tie): A diagnostic and treatment quandary. Quintessence Int. 1999, 30, 259–262. [Google Scholar]
- Huang, Y.S.; Quo, S.; Berkowski, A.; Guilleminault, C. Short lingual frenulum and obstructive sleep apnea in children. Int. J. Pediatr. Res. 2015, 1, 273. [Google Scholar] [CrossRef]
- Wright, J.E. Tongue-tie. J. Paediatr. Child. Health 1995, 31, 276–278. [Google Scholar] [CrossRef]
- Lalakea, M.L.; Messner, A.H. Ankyloglossia: The adolescent and adult perspective. Otolaryngol. Head Neck Surg. 2003, 128, 746–752. [Google Scholar] [CrossRef]
- Messner, A.H.; Walsh, J.; Rosenfeld, R.M.; Schwartz, S.R.; Ishman, S.L.; Baldassari, C.; Brietzke, S.E.; Darrow, D.H.; Goldstein, N.; Levi, J.; et al. Clinical consensus statement: Ankyloglossia in children. Otolaryngol. Head Neck Surg. 2020, 162, 597–611. [Google Scholar] [CrossRef] [PubMed]
- Ostapiuk, B. Rodzaje i jakość dźwiękowych realizacji polskiego fonemu/r/w ankyloglosji. Logopedia 2002, 30, 91–103. [Google Scholar]
- Ostapiuk, B. Ankyloglosja a wada wymowy. Biuletyn Koła Sekcji Ortodoncji PTS w Szczecinie 2005, 9, 49–53. [Google Scholar]
- Ostapiuk, B. Dziecięca artykulacja czy wada wymowy-między fizjologią a patologią. Logopedia 2002, 31, 95–156. [Google Scholar]
- Ostapiuk, B. Ruchomość języka w ankyloglosji z uwzględnieniem artykulacji. Ann. Acad. Stetin 2006, 3, 37–47. [Google Scholar]
- Marchesan, I.Q. Lingual frenulum: Classification and speech interference. Int. J. Orofac. Myol. 2004, 30, 31–38. [Google Scholar] [CrossRef]
- Charisi, C.; Koutrouli, A.; Moschou, A.; Arhakis, A. Aetiology, diagnosis and treatment of ankyloglossia. Balk J. Dent. Med. 2017, 21, 141–145. [Google Scholar] [CrossRef]
- Wang, J.; Yang, X.; Hao, S.; Wang, Y. The effect of ankyloglossia and tongue-tie division on speech articulation: A systematic review. Int. J. Paediatr. Dent. 2022, 32, 144–156. [Google Scholar] [CrossRef]
- Guilleminault, C.; Huseni, S.; Lo, L. A frequent phenotype for paediatric sleep apnoea: Short lingual frenulum. ERJ Open Res. 2016, 2, 00043–02016. [Google Scholar] [CrossRef]
- Kawala, B.; Szmielewicz, M.; Kozanecka, A. Czy ortodonci są jeszcze potrzebni? Epidemiologia wad zgryzowo-zębowych u dzieci i młodzieży w Polsce w ostatnich 15 latach. Dent. Med. Probl. 2009, 46, 273–278. [Google Scholar]
- Yoon, A.J.; Zaghi, S.; Ha, S.; Law, C.S.; Guilleminault, C.; Liu, S.Y. Ankyloglossia as a risk factor for maxillary hypoplasia and soft palate elongation: A functional—Morphological study. Orthod. Craniofac. Res. 2017, 20, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Pompéia, L.E.; Ilinsky, R.S.; Ortolani, C.L.F.; Faltin, K., Jr. Ankyloglossia and its influence on growth and development of the stomatognathic system. Rev. Paul. Pediatr. 2017, 35, 216–221. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, B.; Chitharanjan, A.B. Skeletal and dental characteristics in subjects with ankyloglossia. Prog. Orthod. 2013, 14, 44. [Google Scholar] [CrossRef] [PubMed]
- Ronsivalle, V.; Quinzi, V.; La Rosa, S.; Leonardi, R.; Lo Giudice, A. Comparative analysis of skeletal changes, occlusal changes, and palatal morphology in children with mild class III malocclusion treated with elastodontic appliances and bimaxillary plates. Children 2023, 10, 1219. [Google Scholar] [CrossRef]
- Carnino, J.M.; Walia, A.S.; Lara, F.R.; Mwaura, A.M.; Levi, J.R. The effect of frenectomy for tongue-tie, lip-tie, or cheek-tie on breastfeeding outcomes: A systematic review of articles over time and suggestions for management. Int. J. Pediatr. Otorhinolaryngol. 2023, 171, 111638. [Google Scholar] [CrossRef]
- Murias, I.; Grzech-Leśniak, K.; Murias, A.; Walicka-Cupryś, K.; Dominiak, M.; Golob Deeb, J.; Matys, J. Efficacy of various laser wavelengths in the surgical treatment of ankyloglossia: A systematic review. Life 2022, 12, 558. [Google Scholar] [CrossRef]
| Sex | Study Group | Control Group | Total | ||
|---|---|---|---|---|---|
| Ankyloglossia Severity | |||||
| Mild | Moderate | Severe | |||
| Female | 5 (5.2%) | 21 (21.9%) | 16 (16.7%) | 54 (56.2%) | 96 |
| Male | 5 (6.6%) | 28 (36.8%) | 11 (14.5%) | 32 (42.1%) | 76 |
| Total | 10 (5.8%) | 49 (28.5%) | 27 (15.7%) | 86 (50%) | 172 |
| Type of Swallowing | Study Group | Control Group | Total | ||
|---|---|---|---|---|---|
| Ankyloglossia Severity | |||||
| Mild | Moderate | Severe | |||
| Infantile | 5 (11.1%) | 13 (28.9%) | 16 (35.6%) | 11 (24.4%) | 45 |
| Mature | 5 (4%) | 36 (28.6%) | 11 (8.7%) | 74 (58.7%) | 126 |
| Mixtus | 0 | 0 | 0 | 1 (100%) | 1 |
| Total | 10 (5.8%) | 49 (28.5%) | 27 (15.7%) | 86 (50%) | 172 |
| Independence test results: | χ2 = 16.912, df = 6, V = 0.176, pFisher < 0.001 | ||||
| Tongue Mobility | Study Group | Control Group | Total | ||
|---|---|---|---|---|---|
| Ankyloglossia Severity | |||||
| Mild | Moderate | Severe | |||
| Limited | 0 | 5 (29.4%) | 12 (70.6%) | 0 | 17 |
| Normal | 10 (6.5%) | 44 (28.4%) | 15 (9.7%) | 86 (55.5%) | 155 |
| Total | 10 (5.8%) | 49 (28.5%) | 27 (15.7%) | 86 (50%) | 172 |
| Independence test results: | χ2 = 46.743, df = 3, V = 0.521, pFisher < 0.001 | ||||
| Speech | Study Group | Control Group | Total | ||
|---|---|---|---|---|---|
| Ankyloglossia Severity | |||||
| Mild | Moderate | Severe | |||
| Normal | 8 (7.3%) | 27 (24.5%) | 6 (5.5%) | 69 (62.7%) | 110 |
| Rhotacism | 1 (2.1%) | 18 (38.3%) | 18 (38.3%) | 10 (21.3%) | 47 |
| Rhotacism + lisping | 1 (7.1%) | 4 (28.6%) | 3 (21.4%) | 6 (42.9%) | 14 |
| Lisping | 0 | 0 | 0 | 1 (100%) | 1 |
| Total | 10 (5.8%) | 49 (28.5%) | 27 (15.7%) | 86 (50%) | 172 |
| Independence test results: | χ2 = 39.131, df = 6, V = 0.275, pFisher < 0.001 | ||||
| Crowding/Malocclusion | Study Group | Control Group | Total | ||
|---|---|---|---|---|---|
| Ankyloglossia Severity | |||||
| Mild | Moderate | Severe | |||
| Absent | 1 (2%) | 8 (15.7%) | 2 (3.9%) | 40 (78.4%) | 51 |
| Present | 9 (7.4%) | 41 (33.9%) | 25 (20.7%) | 46 (38%) | 121 |
| Total | 10 (5.8%) | 49 (28.5%) | 27 (15.7%) | 86 (50%) | 172 |
| Independence test results: | χ2 = 24.147, df = 3, V = 0.375, pFisher < 0.001 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dydyk, A.; Milona, M.; Janiszewska-Olszowska, J.; Wyganowska, M.; Grocholewicz, K. Influence of Shortened Tongue Frenulum on Tongue Mobility, Speech and Occlusion. J. Clin. Med. 2023, 12, 7415. https://doi.org/10.3390/jcm12237415
Dydyk A, Milona M, Janiszewska-Olszowska J, Wyganowska M, Grocholewicz K. Influence of Shortened Tongue Frenulum on Tongue Mobility, Speech and Occlusion. Journal of Clinical Medicine. 2023; 12(23):7415. https://doi.org/10.3390/jcm12237415
Chicago/Turabian StyleDydyk, Aldona, Marta Milona, Joanna Janiszewska-Olszowska, Marzena Wyganowska, and Katarzyna Grocholewicz. 2023. "Influence of Shortened Tongue Frenulum on Tongue Mobility, Speech and Occlusion" Journal of Clinical Medicine 12, no. 23: 7415. https://doi.org/10.3390/jcm12237415