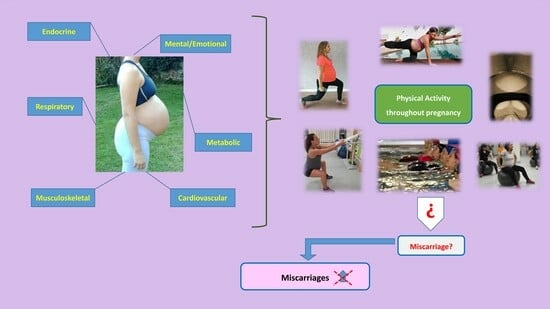
The Influence of Physical Activity during Pregnancy on Miscarriage—Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population
2.2. Intervention
2.3. Comparison
2.4. Outcomes
2.5. Study Design and Selection Process
2.6. Statistical Analysis, Quality of Evidence Assessment, and Risk of Bias
| Author | Year | Country | Type | N | EG | CG | Intervention, Physical Exercise Program | Main Variables Analyzed | Secondary Variables Analyzed | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Freq | Intensity | Duration of Program | Type of Exercise | Superv Class | Duration of Class | Adh. | |||||||||
| Brik [15] | 2019 | Spain | RCT | 120 | 75 | 45 | 3 | 55–60% Max HR | 29 w | Aerobic, strength, coordination and balance, and pelvic floor exercises | Yes | 60 min | 70% | Gestational weight gain, miscarriage | Type of delivery, birth weight, gestational age |
| Daly [16] | 2017 | Ireland | RCT | 88 | 44 | 44 | 3 | Mod | 26 w | Aerobic, resistance, pelvic floor exercises | Yes | 50–60 min | - | Maternal fasting plasma glucose, gestational weight gain | Type of delivery and, birth weight, miscarriage |
| Petrov Fieril [17] | 2014 | Sweden | RCT | 92 | 51 | 41 | 2 | Mod | 12 w | Resistance training | Yes | 60 min | - | Health-related quality of life, physical strength | Birth weight, gestational age, miscarriage |
| Garnaes [4] | 2017 | Norway | RCT | 91 | 46 | 45 | 5 | Mod | 24 w | Endurance and strength training. Pelvic floor muscle exercises every day | Yes (3) No (2) | 60 min 50 min | 50% | Birth weight, gestational age miscarriage | Type of delivery |
| Guelfi [18] | 2016 | Australia | RCT | 172 | 85 | 87 | 3 | Mod | 14 w | Home-based stationary cycling program | Yes | 20–60 min | - | Gestational diabetes, miscarriage | Type of delivery, birth weight |
| Kluge [19] | 2011 | South Africa | RCT | 50 | 26 | 24 | 7 | Low–Mod | 10 w | Five instruction exercise class + transverse abdominal and pelvic floor muscles training. | No | 30 min | - | Pain intensity and functional ability | Type of delivery, birth weight, duration of labor, miscarriage |
| Navas [20] | 2021 | Spain | RCT | 294 | 148 | 146 | 3 | 55–65% Max HR | 20 w | Aquatic exercise | Yes | 45 min | - | Postpartum depression, quality of life, and quality of sleep | Miscarriage, gestational age, and birth weight |
| Pelaez [6] | 2019 | Spain | RCT | 345 | 115 | 230 | 3 | 65–70% Max HR | 24 w | Aerobic and resistance training | Yes | 60–65 min | 80% | Gestational weight gain, macrosomia, type of delivery | Miscarriage |
| Renault [21] | 2014 | Denmark | RCT | 283 | 142 | 141 | 7 | Low | 24 w | Daily 11,000 steps, hypocaloric low-fat diet | No | 60 + min | - | Gestational weight gain, miscarriage | Gestational age |
| Sagedal [22] | 2017 | Norway | RCT | 591 | 296 | 295 | 2 | Mod | 24 w | Aerobic, strength training. Dietary counselling | Yes | 60 min | - | Gestational weight gain, birth weight | Gestational age, perineal tear, miscarriage |
| Ussher [23] | 2015 | UK | RCT | 789 | 394 | 395 | 2–3 | Mod | 6 w | Treadmill exercise | Yes | 20 + min | - | Continuous smoking abstinence, miscarriage | Type of delivery, birth weight |
| Vinter [5] | 2011 | Denmark | RCT | 360 | 180 | 180 | 7 | Mod | 25 w | Aerobic and light strength training, + dietary counseling | Yes (1) No (6) | 60 min 30–60 m | 77% | Gestational weight gain, gestational diabetes | Type of delivery, birth weight, macrosomia, miscarriage |
| Wang [24] | 2017 | China | RCT | 300 | 150 | 150 | 3 | Mod | 24 w | Stationary cycling program | Yes | 45–60 min | - | Gestational diabetes, gestational weight gain | Birth weight, miscarriage |
3. Results
3.1. Study Selection
3.2. Effect of Physical Activity on the Occurrence of Miscarriage
3.3. Risk of Bias Assessment
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Galeotti, M.; Mitchell, G.; Tomlinson, M.; Aventin, Á. Factors affecting the emotional wellbeing of women and men who experience miscarriage in hospital settings: A scoping review. BMC Pregnancy Childbirth 2022, 22, 70. [Google Scholar] [CrossRef] [PubMed]
- McDonald, A.; McDonald, J.; Armstrong, B.; Cherry, N.; Cote, R.; Lavoie, J.; Nolin, A.; Robert, D. Fetal death and work in pregnancy. J. Saf. Res. 1989, 20, 42–43. [Google Scholar] [CrossRef]
- Davenport, M.H.; Kathol, A.J.; Mottola, M.F.; Skow, R.J.; Meah, V.L.; Poitras, V.J.; Garcia, A.J.; Gray, C.E.; Barrowman, N.; Riske, L. Prenatal exercise is not associated with fetal mortality: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Garnaes, K.K.; Nyrnes, S.A.; Salvesen, K.Å.; Salvesen, Ø.; Mørkved, S.; Moholdt, T. Effect of supervised exercise training during pregnancy on neonatal and maternal outcomes among overweight and obese women. Secondary analyses of the ETIP trial: A randomised controlled trial. PLoS ONE 2017, 12, e0173937. [Google Scholar] [CrossRef]
- Vinter, C.A.; Jensen, D.M.; Ovesen, P.; Beck-Nielsen, H.; Jørgensen, J.S. The LiP (Lifestyle in Pregnancy) study: A randomized controlled trial of lifestyle intervention in 360 obese pregnant women. Diabetes Care 2011, 34, 2502–2507. [Google Scholar] [CrossRef] [PubMed]
- Pelaez, M.; Gonzalez-Cerron, S.; Montejo, R.; Barakat, R. Protective effect of exercise in pregnant women including those who exceed weight gain recommendations: A randomized controlled trial. Mayo Clin. Proc. 2019, 94, 1951–1959. [Google Scholar] [CrossRef]
- Evenson, K.R.; Moos, M.-K.; Carrier, K.; Siega-Riz, A.M. Perceived barriers to physical activity among pregnant women. Matern. Child Health J. 2009, 13, 364–375. [Google Scholar] [CrossRef]
- Evenson, K.R.; Wen, F. Prevalence and correlates of objectively measured physical activity and sedentary behavior among US pregnant women. Prev. Med. 2011, 53, 39–43. [Google Scholar] [CrossRef]
- Barakat, R.; Perales, M.; Garatachea, N.; Ruiz, J.R.; Lucia, A. Exercise during pregnancy. A narrative review asking: What do we know? Br. J. Sports Med. 2015, 49, 1377–1381. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- González, I.F.; Urrútia, G.; Alonso-Coello, P. Systematic reviews and meta-analysis: Scientific rationale and interpretation. Rev. Española Cardiol. (Engl. Ed.) 2011, 64, 688–696. [Google Scholar]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Savović, J.; Page, M.J.; Elbers, R.G.; Sterne, J.A. Assessing risk of bias in a randomized trial. In Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Chichester, UK, 2019; pp. 205–228. [Google Scholar]
- Brik, M.; Fernández-Buhigas, I.; Martin-Arias, A.; Vargas-Terrones, M.; Barakat, R.; Santacruz, B. Does exercise during pregnancy impact on maternal weight gain and fetal cardiac function? A randomized controlled trial. Ultrasound Obstet. Gynecol. 2019, 53, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Daly, N.; Farren, M.; McKeating, A.; O’Kelly, R.; Stapleton, M.; Turner, M.J. A Medically Supervised Pregnancy Exercise Intervention in Obese Women: A Randomized Controlled Trial. Obstet. Gynecol. 2017, 130, 1001–1010. [Google Scholar] [CrossRef]
- Petrov Fieril, K.; Glantz, A.; Fagevik Olsen, M. The efficacy of moderate-to-vigorous resistance exercise during pregnancy: A randomized controlled trial. Acta Obstet. Gynecol. Scand. 2015, 94, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Guelfi, K.J.; Ong, M.J.; Crisp, N.A.; Fournier, P.A.; Wallman, K.E.; Grove, J.R.; Doherty, D.A.; Newnham, J.P. Regular Exercise to Prevent the Recurrence of Gestational Diabetes Mellitus: A Randomized Controlled Trial. Obstet. Gynecol. 2016, 128, 819–827. [Google Scholar] [CrossRef] [PubMed]
- Kluge, J.; Hall, D.; Louw, Q.; Theron, G.; Grové, D. Specific exercises to treat pregnancy-related low back pain in a South African population. Int. J. Gynecol. Obstet. 2011, 113, 187–191. [Google Scholar] [CrossRef]
- Navas, A.; Carrascosa, M.d.C.; Artigues, C.; Ortas, S.; Portells, E.; Soler, A.; Yañez, A.M.; Bennasar-Veny, M.; Leiva, A. Effectiveness of moderate-intensity aerobic water exercise during pregnancy on quality of life and postpartum depression: A multi-center, randomized controlled trial. J. Clin. Med. 2021, 10, 2432. [Google Scholar] [CrossRef]
- Renault, K.M.; Nørgaard, K.; Nilas, L.; Carlsen, E.M.; Cortes, D.; Pryds, O.; Secher, N.J. The Treatment of Obese Pregnant Women (TOP) study: A randomized controlled trial of the effect of physical activity intervention assessed by pedometer with or without dietary intervention in obese pregnant women. Am. J. Obstet. Gynecol. 2014, 210, 134.e131–134.e139. [Google Scholar] [CrossRef]
- Sagedal, L.; Øverby, N.; Bere, E.; Torstveit, M.; Lohne-Seiler, H.; Småstuen, M.; Hillesund, E.; Henriksen, T.; Vistad, I. Lifestyle intervention to limit gestational weight gain: The Norwegian Fit for Delivery randomised controlled trial. BJOG Int. J. Obstet. Gynaecol. 2017, 124, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Ussher, M.; Lewis, S.; Aveyard, P.; Manyonda, I.; West, R.; Lewis, B.; Marcus, B.; Riaz, M.; Taylor, A.H.; Barton, P.; et al. The London Exercise and Pregnant smokers (LEAP) trial: A randomised controlled trial of physical activity for smoking cessation in pregnancy with an economic evaluation. Health Technol. Assess 2015, 19, vii–xxiv, 1–135. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Wei, Y.; Zhang, X.; Zhang, Y.; Xu, Q.; Sun, Y.; Su, S.; Zhang, L.; Liu, C.; Feng, Y.; et al. A randomized clinical trial of exercise during pregnancy to prevent gestational diabetes mellitus and improve pregnancy outcome in overweight and obese pregnant women. Am. J. Obstet. Gynecol. 2017, 216, 340–351. [Google Scholar] [CrossRef]
- Hegaard, H.K.; Kjaergaard, H.; Damm, P.P.; Petersson, K.; Dykes, A.-K. Experiences of physical activity during pregnancy in Danish nulliparous women with a physically active life before pregnancy. A qualitative study. BMC Pregnancy Childbirth 2010, 10, 33. [Google Scholar] [CrossRef]
- Hanghøj, S. When it hurts I think: Now the baby dies. Risk perceptions of physical activity during pregnancy. Women Birth 2013, 26, 190–194. [Google Scholar] [CrossRef]
- Hegaard, H.K.; Ersbøll, A.S.; Damm, P. Exercise in pregnancy: First trimester risks. Clin. Obstet. Gynecol. 2016, 59, 559–567. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO: Recommended definitions, terminology and format for statistical tables related to the perinatal period and use of a new certificate for cause of perinatal deaths. Modifications recommended by FIGO as amended October 14, 1976. Acta Obstet. Gynecol. Scand. 1977, 56, 247–253. [Google Scholar]
- Toth, B.; Bohlmann, M.; Hancke, K.; Kuon, R.; Nawroth, F.; von Otte, S.; Rogenhofer, N.; Rudnik-Schöneborn, S.; Schleußner, E.; Tempfer, C. Recurrent Miscarriage: Diagnostic and Therapeutic Procedures. Guideline of the DGGG, OEGGG and SGGG (S2k-Level, AWMF Registry No. 015/050, May 2022). Geburtshilfe Frauenheilkd. 2022, 83, 49–78. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.N.; Missmer, S.A.; Cramer, D.W.; Powers, R.D.; McShane, P.M.; Hornstein, M.D. Effects of lifetime exercise on the outcome of in vitro fertilization. Obstet. Gynecol. 2006, 108, 938–945. [Google Scholar] [CrossRef]
- Madsen, M.; Jørgensen, T.; Jensen, M.; Juhl, M.; Olsen, J.; Andersen, P.; Nybo Andersen, A.M. Leisure time physical exercise during pregnancy and the risk of miscarriage: A study within the Danish National Birth Cohort. BJOG Int. J. Obstet. Gynaecol. 2007, 114, 1419–1426. [Google Scholar] [CrossRef]
- Feodor Nilsson, S.; Andersen, P.; Strandberg-Larsen, K.; Nybo Andersen, A.M. Risk factors for miscarriage from a prevention perspective: A nationwide follow-up study. BJOG Int. J. Obstet. Gynaecol. 2014, 121, 1375–1385. [Google Scholar] [CrossRef] [PubMed]
- Sundgot-Borgen, J.; Sundgot-Borgen, C.; Myklebust, G.; Sølvberg, N.; Torstveit, M.K. Elite athletes get pregnant, have healthy babies and return to sport early postpartum. BMJ Open Sport Exerc. Med. 2019, 5, e000652. [Google Scholar] [CrossRef] [PubMed]
- Wowdzia, J.B.; McHugh, T.-L.; Thornton, J.; Sivak, A.; Mottola, M.F.; Davenport, M.H. Elite athletes and pregnancy outcomes: A systematic review and meta-analysis. Med. Sci. Sports Exerc. 2021, 53, 534–542. [Google Scholar] [CrossRef] [PubMed]
- L’Heveder, A.C.M.; Mitra, A.; Kasaven, L.; Saso, S.; Prior, T.; Pollock, N.; Dooley, M.; Joash, K.; Jones, B.P. Sports obstetrics: Implications of Pregnancy in Elite Sportswomen, a Narrative Review. J. Clin. Med. 2022, 11, 4977–4993. [Google Scholar] [CrossRef]
- Meah, V.L.; Davies, G.A.; Davenport, M.H. Why can’t I exercise during pregnancy? Time to revisit medical ‘absolute’ and ‘relative’ contraindications: Systematic review of evidence of harm and a call to action. Br. J. Sports Med. 2020, 54, 1395–1404. [Google Scholar] [CrossRef]
- Maconochie, N.; Doyle, P.; Prior, S.; Simmons, R. Risk factors for first trimester miscarriage—Results from a UK-population-based case-control study. BJOG 2007, 114, 170–186. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barakat, R.; Zhang, D.; Silva-José, C.; Sánchez-Polán, M.; Franco, E.; Mottola, M.F. The Influence of Physical Activity during Pregnancy on Miscarriage—Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 5393. https://doi.org/10.3390/jcm12165393
Barakat R, Zhang D, Silva-José C, Sánchez-Polán M, Franco E, Mottola MF. The Influence of Physical Activity during Pregnancy on Miscarriage—Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(16):5393. https://doi.org/10.3390/jcm12165393
Chicago/Turabian StyleBarakat, Rubén, Dingfeng Zhang, Cristina Silva-José, Miguel Sánchez-Polán, Evelia Franco, and Michelle F. Mottola. 2023. "The Influence of Physical Activity during Pregnancy on Miscarriage—Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 16: 5393. https://doi.org/10.3390/jcm12165393