Cardiology in a Digital Age: Opportunities and Challenges for e-Health: A Literature Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results
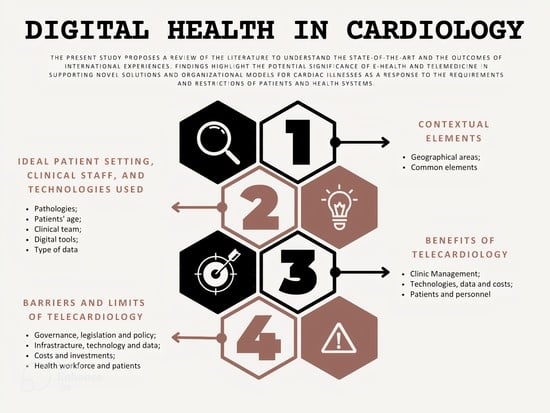
3.1. Contextual Elements
3.2. Ideal Patient Setting, Clinical Staff, and Technologies Used
3.2.1. Ideal Patient Setting
3.2.2. Clinical Staff
3.2.3. Technologies Used
3.3. The Benefits of Telecardiology
3.3.1. Clinical Management
3.3.2. Technology, Data, and Costs
3.3.3. Professionals and Patients
3.4. Barriers and Limits of Telecardiology
3.4.1. Governance, Legislation, and Policies
3.4.2. Infrastructure, Technology, and Data
3.4.3. Costs and Investments
3.4.4. Staff and Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McClellan, M.; Brown, N.; Califf, R.M.; Warner, J.J. Call to Action: Urgent Challenges in Cardiovascular Disease: A Presidential Advisory from the American Heart Association. Circulation 2019, 139, e44–e54. [Google Scholar] [CrossRef] [PubMed]
- Bloom, D.E.; Cafiero, E.T.; Jané-Llopis, E.; Abrahams-Gessel, S.; Bloom, L.R.; Fathima, S.; Feigl, A.B.; Gaziano, T.; Mowafi, M.; Pandya, A.; et al. The Global Economic Burden of Noncommunicable Diseases; World Economic Forum: Geneva, Switzerland, 2011; Available online: https://www3.weforum.org/docs/WEF_Harvard_HE_GlobalEconomicBurdenNonCommunicableDiseases_2011.pdf (accessed on 28 May 2023).
- Weintraub, N.L.; Collins, S.P.; Pang, P.S.; Levy, P.D.; Anderson, A.S.; Arslanian-Engoren, C.; Gibler, W.B.; McCord, J.K.; Parshall, M.B.; Francis, G.S.; et al. Acute heart failure syndromes: Emergency department presentation, treatment, and disposition: Current approaches and future aims: A scientific statement from the American Heart Association. Circulation 2010, 122, 1975–1996. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tromp, J.; Jindal, D.; Redfern, J.; Bhatt, A.B.; Séverin, T.; Banerjee, A.; Ge, J.; Itchhaporia, D.; Jaarsma, T.; Lanas, F.; et al. World Heart Federation Roadmap for Digital Health in Cardiology. Glob. Heart 2022, 17, 61. [Google Scholar] [CrossRef]
- Biancuzzi, H.; Mas, F.D.; Bidoli, C.; Pegoraro, V.; Zantedeschi, M.; Negro, P.A.; Campostrini, S.; Cobianchi, L. Economic and Performance Evaluation of E-Health before and after the Pandemic Era: A Literature Review and Future Perspectives. Int. J. Environ. Res. Public Health 2023, 20, 4038. [Google Scholar] [CrossRef] [PubMed]
- Cobianchi, L.; Pugliese, L.; Peloso, A.; Dal Mas, F.; Angelos, P. To a New Normal: Surgery and COVID-19 during the Transition Phase. Ann. Surg. 2020, 272, e49–e51. [Google Scholar] [CrossRef] [PubMed]
- Dal Mas, F.; Massaro, M.; Rippa, P.; Secundo, G. The Challenges of Digital Transformation in Healthcare: An Interdisciplinary Literature Review, Framework, and Future Research Agenda. Technovation 2023, 123, 102716. Available online: https://www.sciencedirect.com/science/article/pii/S0166497223000275 (accessed on 28 May 2023). [CrossRef]
- Molinari, G.; Brunetti, N.D.; Nodari, S.; Molinari, M.; Spagna, G.; Ioakim, M.; Migliore, G.; Dattoli, V.; Di Cillo, O. Impact of 2020 SARS-CoV-2 outbreak on telemedicine management of cardiovascular disease in Italy. Intern. Emerg. Med. 2021, 16, 1191–1196. [Google Scholar] [CrossRef]
- Lin, Z.; Sim, T.B.; Ong, V.Y.K.; bin Ab Hamid, Z.; Ho, W.H. Telemedicine in the acute care setting during the COVID-19 pandemic. Intern. Emerg. Med. 2020, 15, 1591–1593. [Google Scholar] [CrossRef]
- Parretti, C.; La Regina, M.; Tortu, C.; Candido, G.; Tartaglia, R. Telemedicine in Italy, the starting point. Intern. Emerg. Med. 2023, 18, 949–951. [Google Scholar] [CrossRef]
- Faragli, A.; Abawi, D.; Quinn, C.; Cvetkovic, M.; Schlabs, T.; Tahirovic, E.; Düngen, H.-D.; Pieske, B.; Kelle, S.; Edelmann, F.; et al. The role of non-invasive devices for the telemonitoring of heart failure patients. Heart Fail. Rev. 2021, 26, 1063–1080. [Google Scholar] [CrossRef]
- Grenda, T.R.; Whang, S.; Evans, N.R. Transitioning a Surgery Practice to Telehealth During COVID-19. Ann. Surg. 2020, 272, e168–e169. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Corica, B.; Romiti, G.F.; Proietti, M.; Zhang, H.; Lip, G.Y.H. Efficacy of mobile health-technology integrated care based on the ‘Atrial fibrillation Better Care’ (ABC) pathway in relation to sex: A report from the mAFA-II randomized clinical trial. Intern. Emerg. Med. 2023, 18, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.; Du Toit, A.; Jameson, B.; Liu, A.; Harris, M. The Effectiveness of ‘Virtual Hospital’ Models of Care: A Rapid Evidence Scan the effectiveness of Virtual Hospital Models of Care, Sydney. 2020. Available online: https://www.saxinstitute.org.au/wp-content/uploads/20.04_Rapid-Evidence-Scan_The-effectiveness-of-virtual-hospitals.pdf (accessed on 28 May 2023).
- Bidoli, C.; Pegoraro, V.; Mas, F.D.; Bagnoli, C.; Bert, F.; Bonin, M.; Butturini, G.; Cobianchi, L.; Cordiano, C.; Minto, G.; et al. Virtual hospitals: The future of the healthcare system? An expert consensus. J. Telemed. Telecare 2023. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Boriani, G.; Maisano, A.; Bonini, N.; Albini, A.; Imberti, J.F.; Venturelli, A.; Menozzi, M.; Ziveri, V.; Morgante, V.; Camaioni, G.; et al. Digital literacy as a potential barrier to implementation of cardiology tele-visits after COVID-19 pandemic: The INFO-COVID survey. J. Geriatr. Cardiol. 2021, 18, 739–747. [Google Scholar] [PubMed]
- Kario, K.; Harada, N.; Okura, A. The first software as medical device of evidence-based hypertension digital therapeutics for clinical practice. Hypertens. Res. 2022, 45, 1899–1905. [Google Scholar] [CrossRef]
- Hsia, J.; Guthrie, N.L.; Lupinacci, P.; Gubbi, A.; Denham, D.; Berman, M.A.; Bonaca, M.P. Randomized, Controlled Trial of a Digital Behavioral Therapeutic Application to Improve Glycemic Control in Adults with Type 2 Diabetes. Diabetes Care 2022, 45, 2976–2981. [Google Scholar] [CrossRef]
- Canonico, M.E.; Hsia, J.; Guthrie, N.L.; Simmons, M.; Mehta, P.; Lupinacci, P.; Edwards, K.; Mosesso, K.; Gearhart, M.; Skuban, A.; et al. Cognitive behavioral therapy delivered via digital mobile application for the treatment of type 2 diabetes: Rationale, design, and baseline characteristics of a randomized, controlled trial. Clin. Cardiol. 2022, 45, 850–856. [Google Scholar] [CrossRef]
- Massaro, M.; Dumay, J.C.; Guthrie, J. On the shoulders of giants: Undertaking a structured literature review in accounting. Account. Audit. Acc. J. 2016, 29, 767–901. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. Available online: https://www.bmj.com/content/372/bmj.n71 (accessed on 28 May 2023). [CrossRef]
- Mishra, K.; Edwards, B. Cardiac Outpatient Care in a Digital Age: Remote Cardiology Clinic Visits in the Era of COVID-19. Curr. Cardiol. Rep. 2022, 24, 1–6. [Google Scholar] [CrossRef]
- Ghilencea, L.-N.; Chiru, M.-R.; Stolcova, M.; Spiridon, G.; Manea, L.-M.; Stănescu, A.-M.A.; Bokhari, A.; Kilic, I.D.; Secco, G.G.; Foin, N.; et al. Telemedicine: Benefits for Cardiovascular Patients in the COVID-19 Era. Front. Cardiovasc. Med. 2022, 9, 868635. [Google Scholar] [CrossRef] [PubMed]
- Kędzierski, K.; Radziejewska, J.; Sławuta, A.; Wawrzyńska, M.; Arkowski, J. Telemedicine in Cardiology: Modern Technologies to Improve Cardiovascular Patients’ Outcomes. A Narrative Review. Medicina 2022, 58, 210. [Google Scholar] [CrossRef] [PubMed]
- Kulbayeva, S.; Tazhibayeva, K.; Seiduanova, L.; Smagulova, I.; Mussina, A.; Tanabayeva, S.; Fakhradiyev, I.; Saliev, T. Recent Advances of Mobile Healthcare in Cardiology Practice. Acta Inf. Med. 2022, 30, 236–250. [Google Scholar] [CrossRef] [PubMed]
- Mohammadzadeh, N.; Rezayi, S.; Tanhapour, M.; Saeedi, S. Telecardiology interventions for patients with cardiovascular Disease: A systematic review on characteristics and effects. Int. J. Med. Inform. 2022, 158, 104663. [Google Scholar] [CrossRef] [PubMed]
- Senarath, S.; Fernie, G.; Roshan Fekr, A. Influential Factors in Remote Monitoring of Heart Failure Patients: A Review of the Literature and Direction for Future Research. Sensors 2021, 21, 3575. [Google Scholar] [CrossRef]
- Kinast, B.; Lutz, M.; Schreiweis, B. Telemonitoring of Real-World Health Data in Cardiology: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 9070. [Google Scholar] [CrossRef]
- Piskulic, D.; McDermott, S.; Seal, L.; Vallaire, S.; Norris, C.M. Virtual visits in cardiovascular disease: A rapid review of the evidence. Eur. J. Cardiovasc. Nurs. 2021, 20, 816–826. [Google Scholar] [CrossRef]
- Khanna, S.; Harzand, A. Preventive Cardiology in the Digital and COVID-19 Era: A Brave New World within the Veterans Health Administration. Healthcare 2021, 9, 1623. [Google Scholar] [CrossRef]
- Adam, S.; Zahra, S.A.; Chor, C.Y.T.; Khare, Y.; Harky, A. COVID-19 pandemic and its impact on service provision: A cardiology prospect. Acta Cardiol. 2021, 76, 830–837. [Google Scholar] [CrossRef]
- Vervoort, D.; Marvel, F.A.; Isakadze, N.; Kpodonu, J.; Martin, S.S. Digital Cardiology: Opportunities for Disease Prevention. Curr. Cardiovasc. Risk Rep. 2020, 14, 10. [Google Scholar] [CrossRef]
- Lotman, E.-M.; Viigimaa, M. Digital Health in Cardiology: The Estonian Perspective. Cardiology 2020, 145, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.C.; Skoll, D.; Saxon, L.A. Home Monitoring of Cardiac Devices in the Era of COVID-19. Curr. Cardiol. Rep. 2020, 23, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sayer, G.; Horn, E.M.; Farr, M.A.; Axsom, K.; Kleet, A.; Gjerde, C.; Latif, F.; Sobol, I.; Kelley, N.; Lancet, E.; et al. Transition of a Large Tertiary Heart Failure Program in Response to the COVID-19 Pandemic: Changes That Will Endure. Circ. Heart Fail. 2020, 13, e007516. [Google Scholar] [CrossRef]
- Tully, J.; Dameff, C.; Longhurst, C.A. Wave of Wearables: Clinical Management of Patients and the Future of Connected Medicine. Clin. Lab. Med. 2020, 40, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Woo, K.; Dowding, D. Factors Affecting the Acceptance of Telehealth Services by Heart Failure Patients: An Integrative Review. Telemed. e-Health 2018, 24, 292–300. [Google Scholar] [CrossRef]
- Treskes, R.W.; Van der Velde, E.T.; Schoones, J.W.; Schalij, M.J. Implementation of smart technology to improve medication adherence in patients with cardiovascular disease: Is it effective? Expert Rev. Med. Devices 2018, 15, 119–126. [Google Scholar] [CrossRef]
- Dal Mas, F.; Massaro, M.; Lombardi, R.; Garlatti, A. From Output to Outcome Measures in the Public Sector. A Structured Literature Review. Int. J. Organ. Anal. 2019, 27, 1631–1656. [Google Scholar] [CrossRef]
- Massaro, M.; Dumay, J.; Garlatti, A. Public sector knowledge management: A structured literature review. J. Knowl. Manag. 2015, 19, 530–558. [Google Scholar] [CrossRef]
- Guthrie, J.; Dumay, J.; Puntillo, P. IC and public sector: A structured literature review. J. Intellect. Cap. 2015, 16, 267–284. [Google Scholar]
- Savelieva, I.; Fumagalli, S.; Kenny, R.A.; Anker, S.; Benetos, A.; Boriani, G.; Bunch, J.; Dagres, N.; Dubner, S.; Fauchier, L.; et al. EHRA expert consensus document on the management of arrhythmias in frailty syndrome, endorsed by the Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), Latin America Heart Rhythm Society (LAHRS), and Cardiac Arrhythmia Society of Southern Africa (CASSA). Europace 2023, 25, 1249–1276. [Google Scholar] [PubMed]
- Molinari, G.; Molinari, M.; Di Biase, M.; Brunetti, N.D. Telecardiology and its settings of application: An update. J. Telemed. Telecare 2017, 24, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Boriani, G.; Svennberg, E.; Guerra, F.; Linz, D.; Casado-Arroyo, R.; Malaczynska-Rajpold, K.; Duncker, D.; Boveda, S.; Merino, J.L.; Leclercq, C. Reimbursement practices for use of digital devices in atrial fibrillation and other arrhythmias: A European Heart Rhythm Association survey. Europace 2022, 24, 1834–1843. [Google Scholar] [CrossRef] [PubMed]
- Svennberg, E.; Tjong, F.; Goette, A.; Akoum, N.; Di Biase, L.; Bordachar, P.; Boriani, G.; Burri, H.; Conte, G.; Deharo, J.C.; et al. How to use digital devices to detect and manage arrhythmias: An EHRA practical guide. Europace 2022, 24, 979–1005. [Google Scholar] [CrossRef]
- Brandes, A.; Stavrakis, S.; Freedman, B.; Antoniou, S.; Boriani, G.; Camm, A.J.; Chow, C.K.; Ding, E.; Engdahl, J.; Gibson, M.M.; et al. Consumer-Led Screening for Atrial Fibrillation: Frontier Review of the AF-SCREEN International Collaboration. Circulation 2022, 146, 1461–1474. [Google Scholar] [CrossRef]
- Veenis, J.F.; Radhoe, S.P.; Hooijmans, P.; Brugts, J.J. Remote Monitoring in Chronic Heart Failure Patients: Is Non-Invasive Remote Monitoring the Way to Go? Sensors 2021, 21, 887. [Google Scholar] [CrossRef]
- Boriani, G.; Imberti, J.F.; Bonini, N.; Carriere, C.; Mei, D.A.; Zecchin, M.; Piccinin, F.; Vitolo, M.; Sinagra, G. Remote multiparametric monitoring and management of heart failure patients through cardiac implantable electronic devices. Eur. J. Intern. Med. online ahead of print. 2023. [Google Scholar] [CrossRef]
- Boriani, G.; Vitolo, M.; Svennberg, E.; Casado-Arroyo, R.; Merino, J.L.; Leclercq, C. Performance-based risk-sharing arrangements for devices and procedures in cardiac electrophysiology: An innovative perspective. Europace 2022, 24, 1541–1547. [Google Scholar] [CrossRef]
- Bekfani, T.; Fudim, M.; Cleland, J.G.; Jorbenadze, A.; von Haehling, S.; Lorber, A.; Rothman, A.M.; Stein, K.; Abraham, W.T.; Sievert, H.; et al. A current and future outlook on upcoming technologies in remote monitoring of patients with heart failure. Eur. J. Heart Fail. 2021, 23, 175–185. [Google Scholar] [CrossRef]
- Imberti, J.F.; Tosetti, A.; Mei, D.A.; Maisano, A.; Boriani, G. Remote monitoring and telemedicine in heart failure: Implementation and benefits. Curr. Cardiol. Rep. 2021, 23, 55. [Google Scholar] [CrossRef]
- Alvarez, P.; Sianis, A.; Brown, J.; Ali, A.; Briasoulis, A. Chronic disease management in heart failure: Focus on telemedicine and remote monitoring. Rev. Cardiovasc. Med. 2021, 22, 403–413. [Google Scholar] [CrossRef]
- Vitolo, M.; Ziveri, V.; Gozzi, G.; Busi, C.; Imberti, J.F.; Bonini, N.; Muto, F.; Mei, D.A.; Menozzi, M.; Mantovani, M.; et al. DIGItal Health Literacy after COVID-19 Outbreak among Frail and Non-Frail Cardiology Patients: The DIGI-COVID Study. J Pers Med. 2022, 13, 99. [Google Scholar] [CrossRef]
- Sgreccia, D.; Mauro, E.; Vitolo, M.; Manicardi, M.; Valenti, A.C.; Imberti, J.F.; Ziacchi, M.; Boriani, G. Implantable cardioverter defibrillators and devices for cardiac resynchronization therapy: What perspective for patients’ apps combined with remote monitoring? Expert Rev. Med. Devices 2022, 19, 155–160. [Google Scholar] [CrossRef]
- Alfawzan, N.; Christen, M.; Spitale, G.; Biller-Andorno, N. Privacy, Data Sharing, and Data Security Policies of Women’s mHealth Apps: Scoping Review and Content Analysis. JMIR mHealth uHealth 2022, 10, e33735. [Google Scholar] [CrossRef] [PubMed]
- Pool, J.; Akhlaghpour, S.; Fatehi, F.; Gray, L.C. Data privacy concerns and use of telehealth in the aged care context: An integrative review and research agenda. Int. J. Med. Inform. 2022, 160, 104707. [Google Scholar] [CrossRef] [PubMed]
- Sousa, M.J.; Dal Mas, F.; Pesqueira, A.; Lemos, C.; Verde, J.M.; Cobianchi, L. The potential of AI in Health Higher Education to Increase the Students’ Learning Outcomes. TEM J. 2021, 10, 488–497. [Google Scholar] [CrossRef]

| N. | Authors | Title | Year | Journal | Ref. |
|---|---|---|---|---|---|
| 1 | Mishra K., Edwards B. | Cardiac Outpatient Care in a Digital Age: Remote Cardiology Clinic Visits in the Era of COVID-19 | 2022 | Current Cardiology Reports | [21] |
| 2 | Ghilencea L.-N., Chiru M.-R., Stolcova M., Spiridon G., Manea L.-M., Stănescu A.-M.A., Bokhari A., Kilic I.D., Secco G.G., Foin N., Di Mario C. | Telemedicine: Benefits for Cardiovascular Patients in the COVID-19 Era | 2022 | Frontiers in Cardiovascular Medicine | [22] |
| 3 | Kędzierski K., Radziejewska J., Sławuta A., Wawrzyńska M., Arkowski J. | Telemedicine in Cardiology: Modern Technologies to Improve Cardiovascular Patients’ Outcomes—A Narrative Review | 2022 | Medicina (Lithuania) | [23] |
| 4 | Kulbayeva S., Tazhibayeva K., Seiduanova L., Smagulova I., Mussina A., Tanabay S. at al. | The Recent Advances of Mobile Healthcare in Cardiology Practice | 2022 | Acta Informatica Medica | [24] |
| 5 | Mohammadzadeh N., Rezayi S., Tanhapour M., Saeedi S. | Telecardiology interventions for patients with cardiovascular Disease: A systematic review on characteristics and effects | 2022 | International Journal of Medical Informatics | [25] |
| 6 | Senarath S., Fernie G., Roshan Fekr A. | Influential factors in remote monitoring of heart failure patients: A review of the literature and direction for future research | 2021 | Sensors (Switzerland) | [26] |
| 7 | Veenis J.F., Radhoe S.P., Hooijmans P., Brugts J.J. | Remote monitoring in chronic heart failure patients: Is non-invasive remote monitoring the way to go? | 2021 | Sensors (Switzerland) | [27] |
| 8 | Kinast B., Lutz M., Schreiweis B. | Telemonitoring of real-world health data in cardiology: A systematic review | 2021 | International Journal of Environmental Research and Public Health | [28] |
| 9 | Faragli A., Abawi D., Quinn C., Cvetkovic M., Schlabs T., Tahirovic E., Düngen H.-D., Pieske B., Kelle S., Edelmann F., Alogna A. | The role of non-invasive devices for the telemonitoring of heart failure patients | 2021 | Heart Failure Reviews | [11] |
| 10 | Piskulic D., McDermott S., Seal L., Vallaire S., Norris C.M. | Virtual visits in cardiovascular disease: a rapid review of the evidence | 2021 | European journal of cardiovascular nursing: journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology | [29] |
| 11 | Khanna S., Harzand A. | Preventive Cardiology in the Digital and COVID-19 Era: A Brave New World within the Veterans Health Administration | 2021 | Healthcare (Basel, Switzerland) | [30] |
| 12 | Adam S., Zahra S.A., Chor C.Y.T., Khare Y., Harky A. | COVID-19 pandemic and its impact on service provision: A cardiology prospect | 2020 | Acta Cardiologica | [31] |
| 13 | Vervoort D., Marvel F.A., Isakadze N., Kpodonu J., Martin S.S. | Digital Cardiology: Opportunities for Disease Prevention | 2020 | Current Cardiovascular Risk Reports | [32] |
| 14 | Lotman E.-M., Viigimaa M. | Digital Health in Cardiology: The Estonian Perspective | 2020 | Cardiology (Switzerland) | [33] |
| 15 | Miller J.C., Skoll D., Saxon L.A. | Home Monitoring of Cardiac Devices in the Era of COVID-19 | 2020 | Current Cardiology Reports | [34] |
| 16 | Sayer G., Horn E.M., Farr M.A., Axsom K., Kleet A., Gjerde C., Latif F., Sobol I., Kelley N., Lancet E., Halik C., Takeda K., Naka Y. | Transition of a Large Tertiary Heart Failure Program in Response to the COVID-19 Pandemic: Changes That Will Endure | 2020 | Circulation: Heart Failure | [35] |
| 17 | Tully J., Dameff C., Longhurst, C.A. | Wave of Wearables: Clinical Management of Patients and the Future of Connected Medicine | 2020 | Clinics in Laboratory Medicine | [36] |
| 18 | Woo K., Dowding D. | Factors affecting the acceptance of telehealth services by heart failure patients: An integrative review | 2018 | Telemedicine and e-Health | [37] |
| 19 | Treskes R.W., Van der Velde E.T., Schoones J.W., Schalij M.J. | Implementation of smart technology to improve medication adherence in patients with cardiovascular disease: is it effective? | 2018 | Expert Review of Medical Devices | [38] |
| 20 | Molinari G., Molinari M., Di Biase M., Brunetti N.D. | Telecardiology and its settings of application: An update | 2018 | Journal of Telemedicine and Telecare | [39] |
| Common Elements | Description |
|---|---|
| Spread of heart disease and high mortality rate | Globally, a high mortality rate is associated with the increased incidence of heart disease in the world population. For example, heart failure remains the primary cause of death of patients globally [28,42]. In addition to this, the rate of comorbidities and chronicity is rising because of the aging of the world population [11]. |
| COVID-19 pandemic | The outbreak of the COVID-19 pandemic posed major limitations during the 2020–2022 time frame. This led to a reduction in services offered to cardiac patients and diminished preventive diagnostic activities. The situation incentivized the use of new digital solutions to ensure adequate patient care, as well as continuity of care and the promotion of preventive actions. All these activities proved crucial for cardiac patients, given the higher risk factor associated with cases of COVID-19-infection [35]. Patients’ safety was therefore guaranteed by digital tools, which allowed the delivery of care while maintaining the physical distance required by restrictions [36] |
| Dissemination of technology | Over the past decade, the rapid evolution of technology has boosted the collection of clinical data as well as the development of different fields, such as clinical informatics, which should be intended as a discipline dedicated to organizing, understanding, and using data to improve health care and patient outcomes [43]. In addition, technological advances have made the exchange of information more rapid and frequent, a key factor in clinical management [37]. |
| Clinical management | Telemedicine helps the clinical management of patients with cardiovascular disease, not only at the hospital level but also at the ambulatory care level, even when there are no in-person visits [37]. |
| Costs and personnel | The use of e-health tools can help to address the structural shortage of healthcare workers [11], as well as help to reduce costs by decreasing the number of hospitalizations [44] |
| Description | |
|---|---|
| Clinic Management | |
| Visits | Reduction in the number of unscheduled visits. |
| Diagnostic | Acceleration and optimization of cardiac diagnostics. |
| Centralized model | More proactive management of patients. |
| Prevention and decision-making | Improved preventive medicine and decision-making phase. |
| Technologies, data, and costs | |
| Accuracy and reliability | Diagnostic accuracy considered sufficiently high by clinical staff. |
| Advancement of technology | Introduction of new technologies such as artificial intelligence to increase the potential of health technologies and the accuracy of the data collected. |
| Costs | Reduction in the cost of care for both patients and healthcare facilities. |
| Patients and Personnel | |
| Workload | Increased efficiency of clinical staff. |
| Patient empowerment | Direct patient involvement in prevention, monitoring, and treatment processes. |
| Comfort and quality of life | Increased quality of life and overall patient comfort. |
| Logistics and waiting times | Decreased logistical time associated with physical transfer to social-health facilities and reduced waiting time. |
| Description | |
|---|---|
| Governance, legislation, and policy | |
| National guidelines | Lack of national guidelines and e-health strategies focused on appropriate clinical decision-making on the basis of patient-collected data. |
| Ethical and privacy standards | Lack of clear ethical standards and guidelines for both the use of these technologies and the protection of patient privacy. |
| Monitoring and evaluation standards | Lack of clear monitoring and evaluation standards on the effectiveness, scope, and impact of interventions based on specific technological tools. |
| Legislation | Backward national legislation for the management of new e-health models. |
| Infrastructure, technology, and data | |
| Accuracy and reliability | Lack of accuracy, or errors in collected data. |
| Digital infrastructure | Lack of adequate national or regional digital infrastructures. |
| Quality of technology | Low quality of technology. |
| Interoperability | Poor interoperability between information systems. |
| Data management | National and international differences in data collection, storage, and definitions standards. |
| Costs and investments | |
| Device costs and reimbursements | High cost of devices and lack of clear reimbursement pathways for digital technologies. |
| Accessibility | Low Internet accessibility. |
| Health workforce and patients | |
| Workload | Increased workload for healthcare personnel. |
| Digital literacy | Low digital literacy and skills of both patients and health workers. |
| Acceptability | Increased anxiety and low acceptance and perceived effectiveness of the use of devices. |
| Routine and adherence to therapy | Decreased adherence to therapy in the long term. |
| Language | Reduced availability of translation languages. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pegoraro, V.; Bidoli, C.; Dal Mas, F.; Bert, F.; Cobianchi, L.; Zantedeschi, M.; Campostrini, S.; Migliore, F.; Boriani, G. Cardiology in a Digital Age: Opportunities and Challenges for e-Health: A Literature Review. J. Clin. Med. 2023, 12, 4278. https://doi.org/10.3390/jcm12134278
Pegoraro V, Bidoli C, Dal Mas F, Bert F, Cobianchi L, Zantedeschi M, Campostrini S, Migliore F, Boriani G. Cardiology in a Digital Age: Opportunities and Challenges for e-Health: A Literature Review. Journal of Clinical Medicine. 2023; 12(13):4278. https://doi.org/10.3390/jcm12134278
Chicago/Turabian StylePegoraro, Veronica, Chiara Bidoli, Francesca Dal Mas, Fabrizio Bert, Lorenzo Cobianchi, Maristella Zantedeschi, Stefano Campostrini, Federico Migliore, and Giuseppe Boriani. 2023. "Cardiology in a Digital Age: Opportunities and Challenges for e-Health: A Literature Review" Journal of Clinical Medicine 12, no. 13: 4278. https://doi.org/10.3390/jcm12134278