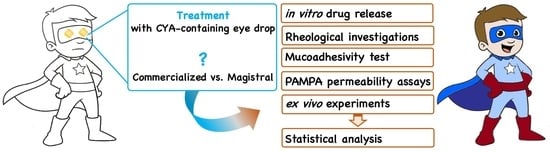
A Comparative Pharmacokinetic Study for Cysteamine-Containing Eye Drops as an Orphan Topical Therapy in Cystinosis
Abstract
:1. Introduction
2. Results
2.1. Physicochemical Parameters of Eye Drops
2.2. Comparison of the Mucoadhesivity
2.3. In Vitro Drug Release Study
2.4. In Vitro Corneal Permeability Study
2.5. Ex Vivo Corneal Permeability on Porcine Eyes
3. Discussion
4. Materials and Methods
4.1. Chemicals
4.2. Preparation of Compounded Eye Drops
4.3. Characterization of Eye Drops
4.4. Investigation of the Mucoadhesivity
4.5. Rapid Equilibrium Dialysis (RED) Experiments
4.6. High Performance Liquid Chromatography (HPLC)
4.7. In Vitro Corneal Permeability Measurements
4.8. Ex Vivo Penetration Test
4.9. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al-Hemidan, A.; Shoughy, S.S.; Kozak, I.; Tabbara, K.F. Efficacy of topical cysteamine in nephropathic cystinosis. Br. J. Ophthalmol. 2017, 101, 1234–1237. [Google Scholar] [CrossRef] [PubMed]
- Emma, F.; Nesterova, G.; Langman, C.; Labbé, A.; Cherqui, S.; Goodyer, P.; Janssen, M.C.; Greco, M.; Topaloglu, R.; Elenberg, E.; et al. Nephropathic cystinosis: An international consensus document. Nephrol. Dial. Transplant. 2014, 29, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Pinxten, A.M.; Hua, M.T.; Simpson, J.; Hohenfellner, K.; Levtchenko, E.; Casteels, I. Clinical Practice: A Proposed Standardized Ophthalmological Assessment for Patients with Cystinosis. Ophthalmol. Ther. 2017, 6, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Labbe, A.; Niaudet, P.; Loirat, C.; Charbit, M.; Guest, G.; Baudouin, C. In vivo confocal microscopy and anterior segment optical coherence tomography analysis of the cornea in nephropathic cystinosis. Ophthalmology 2009, 116, 870–876. [Google Scholar] [CrossRef] [PubMed]
- Csorba, A.; Maka, E.; Szabo, A.; Kelen, K.; Reusz, G.; Nagy, Z.Z. Ocular treatment of cystinosis with eye drop containing cysteamine. Orv. Hetil. 2022, 163, 846–852. [Google Scholar] [CrossRef] [PubMed]
- Shams, F.; Livingstone, I.; Oladiwura, D.; Ramaesh, K. Treatment of corneal cystine crystal accumulation in patients with cystinosis. Clin. Ophthalmol. 2014, 8, 2077–2084. [Google Scholar] [CrossRef] [PubMed]
- Biswas, S.; Sornalingam, K. The Ocular Status of Cystinosis Patients Receiving a Hospital Pharmacy-Made Preparation of Cysteamine Eye Drops: A Case Series. Ophthalmol. Ther. 2019, 8, 125–136. [Google Scholar] [CrossRef]
- Biswas, S.; Gaviria, M.; Malheiro, L.; Marques, J.P.; Giordano, V.; Liang, H. Latest Clinical Approaches in the Ocular Management of Cystinosis: A Review of Current Practice and Opinion from the Ophthalmology Cystinosis Forum. Ophthalmol. Ther. 2018, 7, 307–322. [Google Scholar] [CrossRef]
- Labbe, A.; Baudouin, C.; Deschenes, G.; Loirat, C.; Charbit, M.; Guest, G.; Niaudet, P. A new gel formulation of topical cysteamine for the treatment of corneal cystine crystals in cystinosis: The Cystadrops OCT-1 study. Mol. Genet. Metab. 2014, 111, 314–320. [Google Scholar] [CrossRef]
- MacDonald, I.M.; Noel, L.P.; Mintsioulis, G.; Clarke, W.N. The effect of topical cysteamine drops on reducing crystal formation within the cornea of patients affected by nephropathic cystinosis. J. Pediatr. Ophthalmol. Strabismus 1990, 27, 272–274. [Google Scholar] [CrossRef]
- Hsu, K.H.; Fentzke, R.C.; Chauhan, A. Feasibility of corneal drug delivery of cysteamine using vitamin E modified silicone hydrogel contact lenses. Eur. J. Pharm. Biopharm. 2013, 85, 531–540. [Google Scholar] [CrossRef] [PubMed]
- Luaces-Rodriguez, A.; Diaz-Tome, V.; Gonzalez-Barcia, M.; Silva-Rodríguez, J.; Herranz, M.; Gil-Martínez, M.; Rodríguez-Ares, M.T.; García-Mazás, C.; Blanco-Mendez, J.; Lamas, M.J.; et al. Cysteamine polysaccharide hydrogels: Study of extended ocular delivery and biopermanence time by PET imaging. Int. J. Pharm. 2017, 528, 714–722. [Google Scholar] [CrossRef] [PubMed]
- Marcano, D.C.; Shin, C.S.; Lee, B.; Isenhart, L.C.; Liu, X.; Li, F.; Jester, J.V.; Pflugfelder, S.C.; Simpson, J.; Acharya, G. Synergistic Cysteamine Delivery Nanowafer as an Efficacious Treatment Modality for Corneal Cystinosis. Mol. Pharm. 2016, 13, 3468–3477. [Google Scholar] [CrossRef] [PubMed]
- Liang, H.; Labbe, A.; Le Mouhaer, J.; Plisson, C.; Baudouin, C. A New Viscous Cysteamine Eye Drops Treatment for Ophthalmic Cystinosis: An Open-Label Randomized Comparative Phase III Pivotal Study. Investig. Ophthalmol. Vis. Sci. 2017, 58, 2275–2283. [Google Scholar] [CrossRef]
- Grassiri, B.; Zambito, Y.; Bernkop-Schnürch, A. Strategies to prolong the residence time of drug delivery systems on ocular surface. Adv. Colloid Interface Sci. 2021, 288, 102342. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Liu, H.; Zhang, Z.; Sun, B.; Zhang, J.; Lou, W. Research on the effects of liquid viscosity on droplet size in vertical gas–liquid annular flows. Chem. Eng. Sci. 2020, 220, 115621. [Google Scholar] [CrossRef]
- Mirzahosseini, A.; Noszál, B. The species-and site-specific acid–base properties of biological thiols and their homodisulfides. J. Pharm. Biomed. Anal. 2014, 95, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Avdeef, A. pH-metric log P. Part 1. Difference plots for determining ion-pair octanol-water partition coefficients of multiprotic substances. Quant. Struct.-Act. Relatsh. 1992, 11, 510–517. [Google Scholar] [CrossRef]
- Moiseev, R.V.; Morrison, P.W.; Steele, F.; Khutoryanskiy, V.V. Penetration enhancers in ocular drug delivery. Pharmaceutics 2019, 11, 321. [Google Scholar] [CrossRef]
- Garrett, Q.; Simmons, P.A.; Xu, S.; Vehige, J.; Zhao, Z.; Ehrmann, K.; Willcox, M. Carboxymethylcellulose binds to human corneal epithelial cells and is a modulator of corneal epithelial wound healing. Investig. Ophthalmol. Vis. Sci. 2007, 48, 1559–1567. [Google Scholar] [CrossRef]
- Review CCD. Clinical Review Report: Cysteamine 38 mg/mL Ophthalmic Solution (Cystadrops): (Recordati Rare Diseases Canada Inc.): Indication: Treatment of Corneal Cystine Crystal Deposits in Adults and Children from Two Years of Age with Cystinosis; CADTH Common Drug Reviews: Ottawa, ON, Canada, 2019. [Google Scholar]
- Ozdemir, H.B.; Ozmen, M.C.; Aktas, Z.; Hasanreisoglu, M. In vivo confocal microscopy and anterior segment optical coherence tomography follow-up of cysteamine treatment in corneal cystinosis. Indian J. Ophthalmol. 2019, 67, 153–155. [Google Scholar] [CrossRef]
- Durand-Cavagna, G.; Delort, P.; Duprat, P.; Bailly, Y.; Plazonnet, B.; Gordon, L.R. Corneal toxicity studies in rabbits and dogs with hydroxyethyl cellulose and benzalkonium chloride. Toxicol. Sci. 1989, 13, 500–508. [Google Scholar] [CrossRef]
- European Medical Agency, Assesment Report Cystadrops EMA/738656/2016. Available online: https://www.ema.europa.eu/en/documents/assessment-report/cystadrops-epar-public-assessment-report_en.pdf (accessed on 18 September 2023).
- Pescina, S.; Carra, F.; Padula, C.; Santi, P.; Nicoli, S. Effect of pH and penetration enhancers on cysteamine stability and trans-corneal transport. Eur. J. Pharm. Biopharm. 2016, 107, 171–179. [Google Scholar] [CrossRef]
- Dargó, G.; Vincze, A.; Müller, J.; Kiss, H.J.; Nagy, Z.Z.; Balogh, G.T. Corneal-PAMPA: A novel, non-cell-based assay for prediction of corneal drug permeability. Eur. J. Pharm Sci. 2019, 128, 232–239. [Google Scholar] [CrossRef]







| Components/Dosage form Parameters | Function | CYA-CED | Cystadrops® [24] |
|---|---|---|---|
| Amount (% w/w) | |||
| cysteamine hydrochloride | API | 0.55 | 0.55 |
| hydroxyethylcellulose | mucoadhesive agent | 0.39 | |
| carboxymethylcellulose | mucoadhesive agent | ─ | 5.2 |
| sodium chloride | isotonizing agent | 0.29 | ─ |
| sodium hydrogen carbonate | pH adjustment | 0.54 | ─ |
| citric acid monohydrate | pH adjustment | ─ | N/A * |
| disodium edetate | chelator | ─ | N/A * |
| hydrochloric acid | pH adjustment | ─ | N/A * |
| sodium hydroxide | pH adjustment | ─ | N/A * |
| benzalkonium chloride | preservative agent | ─ | 0.01 |
| water for injection | solvent | 98.23 | N/A * |
| osmolality (mOsm/L) ** | 282 ± 1 | 338 ± 1 | |
| pH ** | 7.60 | 5.22 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Csorba, A.; Katona, G.; Budai-Szűcs, M.; Balogh-Weiser, D.; Molnár, P.; Maka, E.; Kazsoki, A.; Vajna, M.; Zelkó, R.; Nagy, Z.Z.; et al. A Comparative Pharmacokinetic Study for Cysteamine-Containing Eye Drops as an Orphan Topical Therapy in Cystinosis. Int. J. Mol. Sci. 2024, 25, 1623. https://doi.org/10.3390/ijms25031623
Csorba A, Katona G, Budai-Szűcs M, Balogh-Weiser D, Molnár P, Maka E, Kazsoki A, Vajna M, Zelkó R, Nagy ZZ, et al. A Comparative Pharmacokinetic Study for Cysteamine-Containing Eye Drops as an Orphan Topical Therapy in Cystinosis. International Journal of Molecular Sciences. 2024; 25(3):1623. https://doi.org/10.3390/ijms25031623
Chicago/Turabian StyleCsorba, Anita, Gábor Katona, Mária Budai-Szűcs, Diána Balogh-Weiser, Péter Molnár, Erika Maka, Adrienn Kazsoki, Márton Vajna, Romána Zelkó, Zoltán Zsolt Nagy, and et al. 2024. "A Comparative Pharmacokinetic Study for Cysteamine-Containing Eye Drops as an Orphan Topical Therapy in Cystinosis" International Journal of Molecular Sciences 25, no. 3: 1623. https://doi.org/10.3390/ijms25031623