P-Wave Axis of Schoolchildren Who Were Once Breastfed
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Ethics Requirements
2.3. ECG Methodology
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Study Population
3.2. Association between Any Breastfeeding and ECG or Somatometric Characteristics
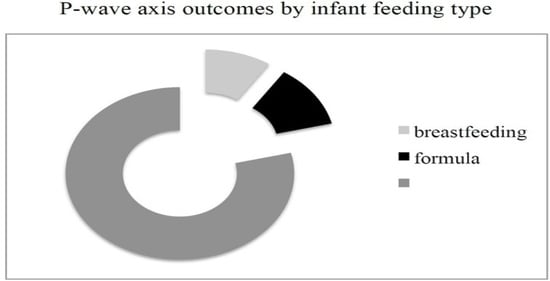
3.3. P-Wave Axis Description
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Villamor-Martínez, E.; Pierro, M.; Cavallaro, G.; Mosca, F.; Kramer, B.W.; Villamor, E. Donor Human Milk Protects against Bronchopulmonary Dysplasia: A Systematic Review and Meta-Analysis. Nutrients 2018, 20, 238. [Google Scholar] [CrossRef] [Green Version]
- Bachrach, V.R.; Schwarz, E.; Bachrach, L.R. Breastfeeding and the risk of hospitalization for respiratory disease in infancy: A meta-analysis. Arch. Pediatr. Adolesc. 2003, 157, 237. [Google Scholar] [CrossRef]
- Mineva, G.M.; Purtill, H.; Dunne, C.P.; Philip, R.K. Impact of breastfeeding on the incidence and severity of respiratory syncytial virus (RSV)-associated acute lower respiratory infections in infants: A systematic review highlighting the global relevance of primary prevention. BMJ Glob. Health 2023, 8, e009693. [Google Scholar] [CrossRef]
- Xue, M.; Dehaas, E.; Chaudhary, N.; O’Byrne, P.; Satia, I.; Kurmi, O.P. Breastfeeding and risk of childhood asthma: A systematic review and meta-analysis. ERJ Open Res. 2021, 7, 00504. [Google Scholar] [CrossRef] [PubMed]
- Waidyatillake, N.T.; Allen, K.J.; Lodge, C.J.; Dharmage, S.C.; Abramson, M.J.; Simpson, J.A.; Lowe, A.J. The impact of breastfeeding on lung development and function: A systematic review. Expert. Rev. Clin. Immunol. 2013, 9, 1253. [Google Scholar] [CrossRef]
- Singhal, A.; Cole, T.J.; Lucas, A. Early nutrition in preterm infants and later blood pressure: Two cohorts after randomised trials. Lancet 2001, 10, 413. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.M.; Ebrahim, S.; Griffin, M.; Davey Smith, G.; Nicolaides, A.N.; Georgiou, N.; Watson, S.; Frankel, S.; Holly, J.M.; Gunnell, D. Breastfeeding and atherosclerosis: Intima-media thickness and plaques at 65-year follow-up of the Boyd Orr cohort. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 1482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evelein, A.M.; Geerts, C.C.; Visseren, F.L.; Bots, M.L.; van der Ent, C.K.; Grobbee, D.E.; Uiterwaal, C.S. The association between breastfeeding and the cardiovascular system in early childhood. Am. J. Clin. Nutr. 2011, 93, 712. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewandowski, A.J.; Lamata, P.; Francis, J.M.; Piechnik, S.K.; Ferreira, V.M.; Boardman, H.; Neubauer, S.; Singhal, A.; Leeson, P.; Lucas, A. Breast Milk Consumption in Preterm Neonates and Cardiac Shape in Adulthood. Pediatrics 2016, 138, e20160050. [Google Scholar] [CrossRef] [Green Version]
- El-Khuffash, A.; Lewandowski, A.J.; Jain, A.; Hamvas, A.; Singh, G.K.; Levy, P.T. Cardiac Performance in the First Year of Age Among Preterm Infants Fed Maternal Breast Milk. JAMA Netw. Open 2021, 4, e2121206. [Google Scholar] [CrossRef]
- Cismaru, G.; Lazea, C.; Mureşan, L.; Gusetu, G.; Rosu, R.; Pop, D.; Zdrenghea, D.; Farcaş, A.D.; Căinap, S.S. Validation of Normal P-Wave Parameters in a Large Unselected Pediatric Population of North-Western Romania: Results of the CARDIOPED Project. Dis. Markers 2021, 6, 6657982. [Google Scholar] [CrossRef]
- Kiess, A.; Körner, A.; Dähnert, I.; Vogel, M.; Markel, F.; Gebauer, R.A.; Kiess, W.; Paech, C. Does obesity have an effect on the ECG in children? J. Pediatr. Endocrinol. Metab. 2020, 26, 585. [Google Scholar] [CrossRef]
- Ng, J.; Sahakian, A.V.; Swiryn, S. The effect of body position on P-wave axis. Comput. Cardiol. 2001, 28, 313. [Google Scholar]
- Snyder, M.L.; Soliman, E.Z.; Whitsel, E.A.; Gellert, K.S.; Heiss, G. Short-term repeatability of electrocardiographic P wave indices and PR interval. J. Electrocardiol. 2014, 47, 257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horta, B.L.; Loret de Mola, C.; Victora, C.G. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 30. [Google Scholar] [CrossRef]
- Berlanga-Macías, C.; Álvarez-Bueno, C.; Martínez-Hortelano, J.A.; Garrido-Miguel, M.; Pozuelo-Carrascosa, D.P.; Martínez-Vizcaíno, V. Relationship between exclusive breastfeeding and cardiorespiratory fitness in children and adolescents: A meta-analysis. Scand. J. Med. Sci. Sports 2020, 30, 828. [Google Scholar] [CrossRef] [PubMed]
- Heshmati, J.; Sepidarkish, M.; Shidfar, F.; Shokri, F.; Vesali, S.; Akbari, M.; Omani-Samani, R. Effect of Breastfeeding in Early Life on Cardiorespiratory and Physical Fitness: A Systematic Review and Meta-Analysis. Breastfeed. Med. 2018, 13, 248. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.; Green, F.C.; Forsyth, J.S.; Greene, S.A.; Newton, D.J.; Belch, J.J. The beneficial effects of breastfeeding on microvascular function in 11- to 14-year-old children. Vasc. Med. 2009, 14, 137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gishti, O.; Jaddoe, V.W.; Duijts, L.; Franco, O.H.; Hofman, A.; Ikram, M.K.; Gaillard, R. Influence of breastfeeding on retinal vessel calibers in school-age children. The Generation R Study. Eur. J. Clin. Nutr. 2016, 70, 72. [Google Scholar] [CrossRef]
- Krishnan, S.S.; Stewart, J.; Amin, N.; Griffin, R.T.; Dozer, A.J. Electrocardiographic prediction of hyperinflation in children. Am. J. Respir. Crit. Care Med. 1997, 156, 2011. [Google Scholar] [CrossRef]
- Chhabra, L.; Sareen, P.; Perli, D.; Srinivasan, I.; Spodick, D.H. Vertical P-wave axis: The electrocardiographic synonym for pulmonary emphysema and its severity. Indian Heart J. 2012, 64, 40. [Google Scholar] [CrossRef] [Green Version]
- Di Filippo, P.; Lizzi, M.; Raso, M.; Di Pillo, S.; Chiarelli, F.; Attanasi, M. The Role of Breastfeeding on Respiratory Outcomes Later in Childhood. Front. Pediatr. 2022, 28, 829414. [Google Scholar] [CrossRef]
- Ogbuanu, I.U.; Karmaus, W.; Arshad, S.H.; Kurukulaaratchy, R.J.; Ewart, S. Effect of breastfeeding duration on lung function at age 10 years: A prospective birth cohort study. Thorax 2009, 64, 62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tennant, P.W.; Gibson, G.J.; Parker, L.; Pearce, M.S. Childhood respiratory illness and lung function at ages 14 and 50 years: Childhood respiratory illness and lung function. Chest 2010, 137, 146. [Google Scholar] [CrossRef] [PubMed]
- Diaz, A.A.; Come, C.E.; Ross, J.C.; San José Estépar, R.; Han, M.K.; Loring, S.H.; Silverman, E.K.; Washko, G.R.; COPDGene Investigators. Association between airway caliber changes with lung inflation and emphysema assessed by volumetric CT scan in subjects with COPD. Chest 2012, 141, 736–744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qiao, J.; Dai, L.J.; Zhang, Q.; Ouyang, Y.Q. A Meta-Analysis of the Association Between Breastfeeding and Early Childhood Obesity. J. Pediatr. Nurs. 2020, 53, 57. [Google Scholar] [CrossRef]
- Amitay, E.L.; Keinan-Boker, L. Breastfeeding and Childhood Leukemia Incidence: A Meta-analysis and Systematic Review. JAMA Pediatr. 2015, 169, e151025. [Google Scholar] [CrossRef] [Green Version]
| Variables | Ever-Breastfed Schoolchildren N = 105 | Never-Breastfed Schoolchildren N = 33 | p Value |
|---|---|---|---|
| 1. Any breastfeeding duration, days | 349.50 (369.16) | 0 | |
| 2. N = 99 | |||
| 3. ≤30 | 1. 13% | ||
| 4. ≤90 | 2. 22% | ||
| 5. ≤180 | 3. 42% | ||
| 6. ≤365 | 4. 67% | ||
| 7. >365 | 5. 33% | ||
| Girls/Boys | 58/47 | 16/18 | 0.434 |
| Years of age | 8.76 (3.08) | 9.27 (3.03) | 0.405 |
| Weight, kg | 33.03 14.43 | 36.09 14.01 | 0.292 |
| Weight percentile | 53.99 (26.80) | 55.24 (28.12) | 0.818 |
| Height, cm | 133.64 (21.63) | 140.00 (21.56) | 0.153 |
| Height percentile | 62.78 (26.44) | 63.10 (25.65) | 0.953 |
| Body mass index | 17.22 (3.10) | 18.59 (3.11) | 0.069 |
| Body mass index percentile | 45.32 (26.01) | 49.50 (29.79) | 0.445 |
| Heart rate, bpm | 82.97 (14.07) | 86.88 (16.08) | 0.181 |
| PR interval, msec | 129.52 (18.54) | 127.91 (16.37) | 0.654 |
| QRS duration, msec | 83.59 (8.49) | 84.67 (7.97) | 0.487 |
| QT interval, msec | 363.32 (29.75) | 359.30 (30.01) | 0.501 |
| QTc interval, msec | 423.38 (22.72) | 427.85 (19.49) | 0.310 |
| P-wave axis, degrees | 37.99 (24.53) | 47.12 (17.09) | 0.048 * |
| QRS-wave axis, degrees | 58.65 (28.30) | 55.15 (25.10) | 0.526 |
| T-wave axis, degrees | 38.93 (18.80) | 45.06 (11.56) | 0.079 |
| Percentiles of Somatometric Characteristics | |||
|---|---|---|---|
| ECG Parameters | Weight | Height | Body Mass Index |
| Heart rate | −0.036 (0.683) | −0.108 (0.219) | 0.021 (0.811) |
| P-wave | −0.106 (0.231) | −0.057 (0.231) | −0.050 (0.573) |
| T-wave | 0.014 (0.873) | 0.158 (0.071) | −0.100 (0.255) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, J.-A.; Rodriguez-Trabal, C.; Pareja, I.; Tur, A.; Mambié, M.; Fernandez-Hidalgo, M.; Verd, S. P-Wave Axis of Schoolchildren Who Were Once Breastfed. Children 2023, 10, 1255. https://doi.org/10.3390/children10071255
Costa J-A, Rodriguez-Trabal C, Pareja I, Tur A, Mambié M, Fernandez-Hidalgo M, Verd S. P-Wave Axis of Schoolchildren Who Were Once Breastfed. Children. 2023; 10(7):1255. https://doi.org/10.3390/children10071255
Chicago/Turabian StyleCosta, Juan-Antonio, Carla Rodriguez-Trabal, Ignacio Pareja, Alicia Tur, Marianna Mambié, Mercedes Fernandez-Hidalgo, and Sergio Verd. 2023. "P-Wave Axis of Schoolchildren Who Were Once Breastfed" Children 10, no. 7: 1255. https://doi.org/10.3390/children10071255