Exo Supportive Devices: Summary of Technical Aspects
Abstract
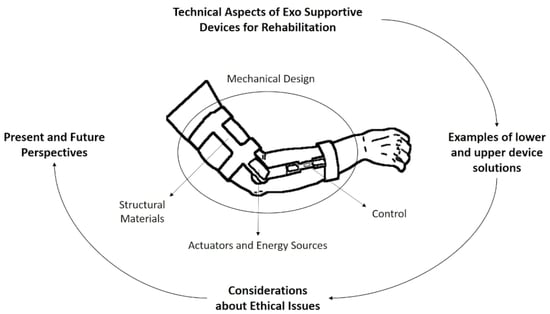
:1. Introduction
1.1. Context and Demographics
1.2. Concept of an External Device
2. External Devices in Rehabilitation Context
2.1. Mechanical Design
2.2. Structural Materials
Rigid vs. Soft Materials
2.3. Actuators and Energy Sources
2.3.1. Traditional Actuators
2.3.2. Soft Actuators
2.4. Control
2.4.1. Control System Architectures
2.4.2. Sensors
3. Device Solutions
3.1. Ankle/Foot Solutions
3.2. Hand/Arm Solutions
4. Ethical Issues
5. Present and Future Perspectives
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AFO | Ankle-foot orthosis |
| DEA | Dielectric elastomer actuator |
| DOF | Degrees of freedom |
| EAP | Electroactive polymer |
| ECP | Electrically conducting polymer |
| EEG | Electroencephalogram |
| EMG | Electromyography |
| FEUP | Faculty of Engineering of University of Porto |
| INEGI | Institute of Science and Innovation in Mechanical and Industrial Engineering |
| IR | Infrared |
| LAETA | Associated laboratory of Energy, Transports and Aeronautics |
| MCP | Metacarpophalangeal |
| MMG | Mechanomyography |
| PID | Proportional integral derivative |
| PLA | Polylactic acid |
| PU | Polyurethane |
| PVDF | Polyvinylidene fluoride |
| QOL | Quality of life |
| RFID | Radio frequency identification |
| SC | Spinal cord |
| SMA | Shape memory alloy |
| SMG | Sonomyography |
| SMM | Shape memory materials |
| SMP | Shape memory polymers |
| UBS | Biomechanical and Health Unity |
| UN | United Nations |
| USA | United States of America |
| VR | Virtual reality |
References
- Miranda, A.B.W.; Yasutomi, A.Y.; Souit, C.; Forner-Cordero, A. Bioinspired mechanical design of an upper limb exoskeleton for rehabilitation and motor control assessment. In Proceedings of the 2012 4th IEEE RAS and EMBS International Conference on Biomedical Robotics and Biomechatronics (BioRob), Rome, Italy, 24–27 June 2012. [Google Scholar] [CrossRef]
- Dima-Cozma, C.; Gavrilută, C.; Cojocaru, D. The importance of healthy lifestyle in modern society: A medical, social and spiritual perspective. Eur. J. Sci. Theol. 2014, 10, 111–120. [Google Scholar]
- Chen, B.; Zi, B.; Qin, L.; Pan, Q. State-of-the-art research in robotic hip exoskeletons: A general review. J. Orthop. Transl. 2020, 20, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Moreno, J.C.; Mohammed, S.; Sharma, N.; del Ama, A.J. Hybrid Wearable Robotic Exoskeletons for Human Walking. In Wearable Robotics; Elsevier: Amsterdam, The Netherlands, 2020; pp. 347–364. [Google Scholar] [CrossRef]
- Nas, K. Rehabilitation of spinal cord injuries. World J. Orthop. 2015, 6, 8. [Google Scholar] [CrossRef] [PubMed]
- Katz, S. Assessing Self-maintenance: Activities of Daily Living, Mobility, and Instrumental Activities of Daily Living. J. Am. Geriatr. Soc. 1983, 31, 721–727. [Google Scholar] [CrossRef]
- European Union. Eurostat Regional Yearbook, 2020 Edition; Publications Office of the European Union: Luxembourg, 2020. [Google Scholar]
- Chen, B.; Ma, H.; Qin, L.Y.; Gao, F.; Chan, K.M.; Law, S.W.; Qin, L.; Liao, W.H. Recent developments and challenges of lower extremity exoskeletons. J. Orthop. Transl. 2016, 5, 26–37. [Google Scholar] [CrossRef] [PubMed]
- United Nations Publications. World Population Ageing 2019 Highlights; United Nations Environment Programme: Nairobi, Kenya, 2020. [Google Scholar]
- Nunes, P.F.; dos Santos, W.M.; Siqueira, A.A. Control Strategy Based on Kinetic Motor Primitives for Lower Limbs Exoskeletons. IFAC-PapersOnLine 2018, 51, 402–406. [Google Scholar] [CrossRef]
- Levesque, L.; Doumit, M. Study of human–machine physical interface for wearable mobility assist devices. Med. Eng. Phys. 2020, 80, 33–43. [Google Scholar] [CrossRef]
- Nichols, E.; Szoeke, C.E.I.; Vollset, S.E.; Abbasi, N.; Abd-Allah, F.; Abdela, J.; Aichour, M.T.E.; Akinyemi, R.O.; Alahdab, F.; Asgedom, S.W.; et al. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 88–106. [Google Scholar] [CrossRef]
- Bellou, E.; Stevenson-Hoare, J.; Escott-Price, V. Polygenic risk and pleiotropy in neurodegenerative diseases. Neurobiol. Dis. 2020, 142, 104953. [Google Scholar] [CrossRef]
- UN. Dementia. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 13 October 2023).
- Vos, T.; Allen, C.; Arora, M.; Barber, R.M.; Bhutta, Z.A.; Brown, A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef]
- Hobson, E.V.; McDermott, C.J. Supportive and symptomatic management of amyotrophic lateral sclerosis. Nat. Rev. Neurol. 2016, 12, 526–538. [Google Scholar] [CrossRef] [PubMed]
- National Spinal Cord Injury Statistical Center. Available online: https://www.nscisc.uab.edu/ (accessed on 23 August 2023).
- Kirshblum, S.; O’Dell, M.W.; Ho, C.; Barr, K. Rehabilitation of persons with central nervous system tumors. Cancer 2001, 92, 1029–1038. [Google Scholar] [CrossRef] [PubMed]
- Yip, P.K.; Malaspina, A. Spinal cord trauma and the molecular point of no return. Mol. Neurodegener. 2012, 7, 6. [Google Scholar] [CrossRef] [PubMed]
- Reeve, A.; Simcox, E.; Turnbull, D. Ageing and Parkinson’s disease: Why is advancing age the biggest risk factor? Ageing Res. Rev. 2014, 14, 19–30. [Google Scholar] [CrossRef]
- Rantanen, T. Promoting Mobility in Older People. J. Prev. Med. Public Health 2013, 46, S50–S54. [Google Scholar] [CrossRef]
- Andersen, C.K.; Wittrup-Jensen, K.U.; Lolk, A.; Andersen, K.; Kragh-Sørensen, P. Ability to perform activities of daily living is the main factor affecting quality of life in patients with dementia. Health Qual. Life Outcomes 2004, 2, 52. [Google Scholar] [CrossRef]
- Lee, W.S.; Cheung, W.H.; Qin, L.; Tang, N.; Leung, K.S. Age-associated Decrease of Type IIA/B Human Skeletal Muscle Fibers. Clin. Orthop. Relat. Res. 2006, 450, 231–237. [Google Scholar] [CrossRef]
- McDonald, J.W.; Sadowsky, C. Spinal-cord injury. Lancet 2002, 359, 417–425. [Google Scholar] [CrossRef]
- Kim, Y.; Lee, J.; Lee, S.; Kim, M. A Force Reflected Exoskeleton-Type Masterarm for Human–Robot Interaction. IEEE Trans. Syst. Man Cybern. Part A Syst. Hum. 2005, 35, 198–212. [Google Scholar] [CrossRef]
- van den Bogert, A.J. Exotendons for assistance of human locomotion. BioMed. Eng. OnLine 2003, 2, 17. [Google Scholar] [CrossRef]
- Sado, F.; Yap, H.J.; Ghazilla, R.A.R.; Ahmad, N. Design and control of a wearable lower-body exoskeleton for squatting and walking assistance in manual handling works. Mechatronics 2019, 63, 102272. [Google Scholar] [CrossRef]
- Yang, C.J.; Zhang, J.F.; Chen, Y.; Dong, Y.M.; Zhang, Y. A Review of exoskeleton-type systems and their key technologies. Proc. Inst. Mech. Eng. Part C J. Mech. Eng. Sci. 2008, 222, 1599–1612. [Google Scholar] [CrossRef]
- Alcobendas-Maestro, M.; Esclarín-Ruz, A.; Casado-López, R.M.; Muñoz-González, A.; Pérez-Mateos, G.; González-Valdizán, E.; Martín, J.L.R. Lokomat Robotic-Assisted Versus Overground Training within 3 to 6 Months of Incomplete Spinal Cord Lesion. Neurorehabilit. Neural Repair 2012, 26, 1058–1063. [Google Scholar] [CrossRef]
- Belforte, G.; Gastaldi, L.; Sorli, M. Pneumatic active gait orthosis. Mechatronics 2001, 11, 301–323. [Google Scholar] [CrossRef]
- Kazerooni, H. The human power amplifier technology at the University of California, Berkeley. Robot. Auton. Syst. 1996, 19, 179–187. [Google Scholar] [CrossRef]
- Young, A.J.; Ferris, D.P. State of the Art and Future Directions for Lower Limb Robotic Exoskeletons. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Haghshenas-Jaryani, M.; Patterson, R.M.; Bugnariu, N.; Wijesundara, M.B. A pilot study on the design and validation of a hybrid exoskeleton robotic device for hand rehabilitation. J. Hand Ther. 2020, 33, 198–208. [Google Scholar] [CrossRef]
- Iqbal, J.; Tsagarakis, N.G.; Caldwell, D.G. A human hand compatible optimised exoskeleton system. In Proceedings of the 2010 IEEE International Conference on Robotics and Biomimetics, Tianjin, China, 14–18 December 2010. [Google Scholar] [CrossRef]
- Iqbal, J.; Baizid, K. Stroke rehabilitation using exoskeleton-based robotic exercisers: Mini Review. Biomed. Res. 2015, 26, 197–201. [Google Scholar]
- Porciuncula, F.; Roto, A.V.; Kumar, D.; Davis, I.; Roy, S.; Walsh, C.J.; Awad, L.N. Wearable Movement Sensors for Rehabilitation: A Focused Review of Technological and Clinical Advances. PM&R 2018, 10, S220–S232. [Google Scholar] [CrossRef]
- Baser, O.; Kizilhan, H.; Kilic, E. Biomimetic compliant lower limb exoskeleton (BioComEx) and its experimental evaluation. J. Braz. Soc. Mech. Sci. Eng. 2019, 41, 226. [Google Scholar] [CrossRef]
- Mihaleva, G.; Kow, F.C.S.F. Development of an Aesthetic for a Stroke Rehabilitation System. In Proceedings of the 2021 International Symposium on Wearable Computers, Virtual Event, 21–26 September 2021. [Google Scholar] [CrossRef]
- Bae, J.; Siviy, C.; Rouleau, M.; Menard, N.; Odonnell, K.; Geliana, I.; Athanassiu, M.; Ryan, D.; Bibeau, C.; Sloot, L.; et al. A Lightweight and Efficient Portable Soft Exosuit for Paretic Ankle Assistance in Walking After Stroke. In Proceedings of the 2018 IEEE International Conference on Robotics and Automation (ICRA), Brisbane, Australia, 21–26 May 2018. [Google Scholar] [CrossRef]
- Asbeck, A.T.; Dyer, R.J.; Larusson, A.F.; Walsh, C.J. Biologically-inspired soft exosuit. In Proceedings of the 2013 IEEE 13th International Conference on Rehabilitation Robotics (ICORR), Seattle, DC, USA, 24–26 June 2013. [Google Scholar] [CrossRef]
- Grimmer, M.; Quinlivan, B.T.; Lee, S.; Malcolm, P.; Rossi, D.M.; Siviy, C.; Walsh, C.J. Comparison of the human-exosuit interaction using ankle moment and ankle positive power inspired walking assistance. J. Biomech. 2019, 83, 76–84. [Google Scholar] [CrossRef]
- Aggogeri, F.; Mikolajczyk, T.; O’Kane, J. Robotics for rehabilitation of hand movement in stroke survivors. Adv. Mech. Eng. 2019, 11. [Google Scholar] [CrossRef]
- O’Neill, C.T.; Phipps, N.S.; Cappello, L.; Paganoni, S.; Walsh, C.J. A soft wearable robot for the shoulder: Design, characterization, and preliminary testing. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017. [Google Scholar] [CrossRef]
- Zhou, L.; Chen, W.; Chen, W.; Bai, S.; Zhang, J.; Wang, J. Design of a passive lower limb exoskeleton for walking assistance with gravity compensation. Mech. Mach. Theory 2020, 150, 103840. [Google Scholar] [CrossRef]
- Gopura, R.A.R.C.; Kiguchi, K.; Li, Y. SUEFUL-7: A 7DOF upper-limb exoskeleton robot with muscle-model-oriented EMG-based control. In Proceedings of the 2009 IEEE/RSJ International Conference on Intelligent Robots and Systems, St. Louis, MO, USA, 10–15 October 2009. [Google Scholar] [CrossRef]
- Garcia, D.; Soto, V.; Lurbe, Y.; Morris, M.; Tosunoglu, S. Development of a rehabilitative exoskeletal arm. ASME Early Career Tech. J. 2012, 11, 11–17. [Google Scholar]
- Hensel, R.; Keil, M. Subjective Evaluation of a Passive Industrial Exoskeleton for Lower-back Support: A Field Study in the Automotive Sector. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 213–221. [Google Scholar] [CrossRef]
- Koopman, A.S.; Kingma, I.; de Looze, M.P.; van Dieën, J.H. Effects of a passive back exoskeleton on the mechanical loading of the low-back during symmetric lifting. J. Biomech. 2020, 102, 109486. [Google Scholar] [CrossRef]
- Xiloyannis, M.; Cappello, L.; Binh, K.D.; Antuvan, C.W.; Masia, L. Preliminary design and control of a soft exosuit for assisting elbow movements and hand grasping in activities of daily living. J. Rehabil. Assist. Technol. Eng. 2017. [Google Scholar] [CrossRef]
- Zoss, A.; Kazerooni, H.; Chu, A. Biomechanical design of the Berkeley lower extremity exoskeleton (BLEEX). IEEE/ASME Trans. Mechatron. 2006, 11, 128–138. [Google Scholar] [CrossRef]
- Hansen, C.; Gosselin, F.; Mansour, K.B.; Devos, P.; Marin, F. Design-validation of a hand exoskeleton using musculoskeletal modeling. Appl. Ergon. 2018, 68, 283–288. [Google Scholar] [CrossRef]
- Cenciarini, M.; Dollar, A.M. Biomechanical considerations in the design of lower limb exoskeletons. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 29 June–1 July 2011. [Google Scholar] [CrossRef]
- Privitera, M.B.; Evans, M.; Southee, D. Human factors in the design of medical devices—Approaches to meeting international standards in the European Union and USA. Appl. Ergon. 2017, 59, 251–263. [Google Scholar] [CrossRef]
- Hamill, J.; Knutzen, K.; Derrick, T. Biomechanical Basis of Human Movement; LWW: Philadelphia, PA, USA, 2021; p. 496. [Google Scholar]
- Rosen, J.; Perry, J.; Manning, N.; Burns, S.; Hannaford, B. The human arm kinematics and dynamics during daily activities—Toward a 7 DOF upper limb powered exoskeleton. In Proceedings of the ICAR 05, 12th International Conference on Advanced Robotics, Seattle, WA, USA, 18–20 July 2005. [Google Scholar] [CrossRef]
- Jarrasse, N.; Morel, G. A formal method for avoiding hyperstaticity when connecting an exoskeleton to a human member. In Proceedings of the 2010 IEEE International Conference on Robotics and Automation, Anchorage, AK, USA, 3–7 May 2010. [Google Scholar] [CrossRef]
- Thalman, C.M.; Lee, H. Design and Validation of a Soft Robotic Ankle-Foot Orthosis (SR-AFO) Exosuit for Inversion and Eversion Ankle Support. In Proceedings of the 2020 IEEE International Conference on Robotics and Automation (ICRA), Paris, France, 31 May–4 June 2020. [Google Scholar] [CrossRef]
- Rus, D.; Tolley, M.T. Design, fabrication and control of soft robots. Nature 2015, 521, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Zatsiorsky, V.M.; Gregory, R.W.; Latash, M.L. Force and torque production in static multifinger prehension: Biomechanics and control. I. Biomechanics. Biol. Cybern. 2002, 87, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Butz, K.D.; Merrell, G.; Nauman, E.A. A biomechanical analysis of finger joint forces and stresses developed during common daily activities. Comput. Methods Biomech. Biomed. Eng. 2012, 15, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Soechting, J.F.; Flanders, M. Flexibility and Repeatability of Finger Movements during Typing: Analysis of Multiple Degrees of Freedom. J. Comput. Neurosci. 1997, 4, 29–46. [Google Scholar] [CrossRef] [PubMed]
- Serbest, K.; Cilli, M.; Yildiz, M.Z.; Eldogan, O. Development of a human hand model for estimating joint torque using MATLAB tools. In Proceedings of the 2016 6th IEEE International Conference on Biomedical Robotics and Biomechatronics (BioRob), Singapore, 26–29 June 2016. [Google Scholar] [CrossRef]
- Miller, L.; Zimmermann, A.; Herbert, W. Clinical effectiveness and safety of powered exoskeleton-assisted walking in patients with spinal cord injury: Systematic review with meta-analysis. Med. Devices Evid. Res. 2016, 2016, 455–466. [Google Scholar] [CrossRef]
- Granados, D.F.P.; Kadone, H.; Suzuki, K. Unpowered Lower-Body Exoskeleton with Torso Lifting Mechanism for Supporting Sit-to-Stand Transitions. In Proceedings of the 2018 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Madrid, Spain, 1–5 October 2018. [Google Scholar] [CrossRef]
- Kagirov, I.; Kapustin, A.; Kipyatkova, I.; Klyuzhev, K.; Kudryavcev, A.; Kudryavcev, I.; Loskutov, Y.; Ryumin, D.; Karpov, A. Medical exoskeleton “Remotion” with an intelligent control system: Modeling, implementation, and testing. Simul. Model. Pract. Theory 2021, 107, 102200. [Google Scholar] [CrossRef]
- Liu, J.; Gao, Y.; Lee, Y.J.; Yang, S. Responsive and Foldable Soft Materials. Trends Chem. 2020, 2, 107–122. [Google Scholar] [CrossRef]
- Kushner, A.M.; Guan, Z. Modular Design in Natural and Biomimetic Soft Materials. Angew. Chem. Int. Ed. 2011, 50, 9026–9057. [Google Scholar] [CrossRef]
- Chiaradia, D.; Xiloyannis, M.; Solazzi, M.; Masia, L.; Frisoli, A. Comparison of a Soft Exosuit and a Rigid Exoskeleton in an Assistive Task. In Biosystems and Biorobotics; Springer International Publishing: Cham, Switzerland, 2018; pp. 415–419. [Google Scholar] [CrossRef]
- Bogue, R. Robotic exoskeletons: A review of recent progress. Ind. Robot. Int. J. 2015, 42, 5–10. [Google Scholar] [CrossRef]
- Vertechy, R.; Frisoli, A.; Dettori, A.; Solazzi, M.; Bergamasco, M. Development of a new exoskeleton for upper limb rehabilitation. In Proceedings of the 2009 IEEE International Conference on Rehabilitation Robotics, Kyoto, Japan, 23–26 June 2009. [Google Scholar] [CrossRef]
- Ansys. Granta Edupack Software. Available online: https://www.ansys.com/products/materials/granta-edupack/ (accessed on 1 October 2023).
- González-Vargas, J.; Ibáñez, J.; Contreras-Vidal, J.L.; Van der Kooij, H.; Pons, J.L. Wearable Robotics: Challenges and Trends, Proceedings of the 2nd International Symposium on Wearable Robotics, WeRob2016, Segovia, Spain, 18–21 October 2016; Springer: Cham, Switzerland, 2016; p. 449. [Google Scholar]
- Asbeck, A.T.; Rossi, S.M.D.; Holt, K.G.; Walsh, C.J. A biologically inspired soft exosuit for walking assistance. Int. J. Robot. Res. 2015, 34, 744–762. [Google Scholar] [CrossRef]
- Almenara, M.; Cempini, M.; Gómez, C.; Cortese, M.; Martín, C.; Medina, J.; Vitiello, N.; Opisso, E. Usability test of a hand exoskeleton for activities of daily living: An example of user-centered design. Disabil. Rehabil. Assist. Technol. 2015, 12, 84–96. [Google Scholar] [CrossRef] [PubMed]
- Hoľvová, P. Analysis of Design Today Exoskeletons in the Health Field. Appl. Mech. Mater. 2014, 613, 320–324. [Google Scholar] [CrossRef]
- Correia, D.M.; Barbosa, J.C.; Costa, C.M.; Reis, P.M.; Esperança, J.M.S.S.; de Zea Bermudez, V.; Lanceros-Méndez, S. Ionic Liquid Cation Size-Dependent Electromechanical Response of Ionic Liquid/Poly(vinylidene fluoride)-Based Soft Actuators. J. Phys. Chem. C 2019, 123, 12744–12752. [Google Scholar] [CrossRef]
- Bar-Cohen, Y.; Anderson, I.A. Electroactive polymer (EAP) actuators—Background review. Mech. Soft Mater. 2019, 1, 5. [Google Scholar] [CrossRef]
- Ansari, R. Polypyrrole Conducting Electroactive Polymers: Synthesis and Stability Studies. e-J. Chem. 2006, 3, 186–201. [Google Scholar] [CrossRef]
- Jager, E.W.; Martinez, J.G.; Zhong, Y.; Persson, N.K. Soft actuator materials for textile muscles and wearable bioelectronics. In Wearable Bioelectronics; Elsevier: Amsterdam, The Netherlands, 2020; pp. 201–218. [Google Scholar] [CrossRef]
- Chiaradia, D.; Xiloyannis, M.; Antuvan, C.W.; Frisoli, A.; Masia, L. Design and embedded control of a soft elbow exosuit. In Proceedings of the 2018 IEEE International Conference on Soft Robotics (RoboSoft), Livorno, Italy, 24–28 April 2018. [Google Scholar] [CrossRef]
- Roveda, L.; Savani, L.; Arlati, S.; Dinon, T.; Legnani, G.; Tosatti, L.M. Design methodology of an active back-support exoskeleton with adaptable backbone-based kinematics. Int. J. Ind. Ergon. 2020, 79, 102991. [Google Scholar] [CrossRef]
- Xie, L.; Huang, G.; Huang, L.; Cai, S.; Li, X. An Unpowered Flexible Lower Limb Exoskeleton: Walking Assisting and Energy Harvesting. IEEE/ASME Trans. Mechatron. 2019, 24, 2236–2247. [Google Scholar] [CrossRef]
- Mooney, L.M.; Rouse, E.J.; Herr, H.M. Autonomous exoskeleton reduces metabolic cost of human walking during load carriage. J. NeuroEng. Rehabil. 2014, 11. [Google Scholar] [CrossRef]
- Collins, S.H.; Wiggin, M.B.; Sawicki, G.S. Reducing the energy cost of human walking using an unpowered exoskeleton. Nature 2015, 522, 212–215. [Google Scholar] [CrossRef]
- Speakman, J.R.; Selman, C. Physical activity and resting metabolic rate. Proc. Nutr. Soc. 2003, 62, 621–634. [Google Scholar] [CrossRef]
- Yandell, M.B.; Tacca, J.R.; Zelik, K.E. Design of a Low Profile, Unpowered Ankle Exoskeleton That Fits under Clothes: Overcoming Practical Barriers to Widespread Societal Adoption. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 712–723. [Google Scholar] [CrossRef] [PubMed]
- Witte, K.A.; Fiers, P.; Sheets-Singer, A.L.; Collins, S.H. Improving the energy economy of human running with powered and unpowered ankle exoskeleton assistance. Sci. Robot. 2020, 5. [Google Scholar] [CrossRef] [PubMed]
- Ramlee, M.R.H.B.; Yusoff, H.M. Design and development of gripping assistive device for post-Stroke rehabilitation. In Proceedings of the 2017 IEEE 4th International Conference on Smart Instrumentation, Measurement and Application (ICSIMA), Putrajaya, Malasia, 28–20 November 2017. [Google Scholar] [CrossRef]
- El-Atab, N.; Mishra, R.B.; Al-Modaf, F.; Joharji, L.; Alsharif, A.A.; Alamoudi, H.; Diaz, M.; Qaiser, N.; Hussain, M.M. Soft Actuators for Soft Robotic Applications: A Review. Adv. Intell. Syst. 2020, 2. [Google Scholar] [CrossRef]
- Dao, D.M.; Pham, P.D.; Tran, T.X.; Le, T.T.T. Study on the transient response of lower limb rehabilitation actuator using the pneumatic cylinder. J. Mechatron. Electr. Power Veh. Technol. 2018, 9, 65–72. [Google Scholar] [CrossRef]
- Al-Fahaam, H.; Davis, S.; Nefti-Meziani, S. Wrist rehabilitation exoskeleton robot based on pneumatic soft actuators. In Proceedings of the 2016 International Conference for Students on Applied Engineering (ISCAE), Newcastle upon Tyne, UK, 20–21 October 2016. [Google Scholar] [CrossRef]
- Stienen, A.; Hekman, E.; ter Braak, H.; Aalsma, A.; van der Helm, F.; van der Kooij, H. Design of a Rotational Hydroelastic Actuator for a Powered Exoskeleton for Upper Limb Rehabilitation. IEEE Trans. Biomed. Eng. 2010, 57, 728–735. [Google Scholar] [CrossRef] [PubMed]
- Glowinski, S.; Krzyzynski, T.; Bryndal, A.; Maciejewski, I. A Kinematic Model of a Humanoid Lower Limb Exoskeleton with Hydraulic Actuators. Sensors 2020, 20, 6116. [Google Scholar] [CrossRef]
- Qiu, Y.; Zhang, E.; Plamthottam, R.; Pei, Q. Dielectric Elastomer Artificial Muscle: Materials Innovations and Device Explorations. Acc. Chem. Res. 2019, 52, 316–325. [Google Scholar] [CrossRef]
- Michel, S.; Zhang, X.Q.; Wissler, M.; Löwe, C.; Kovacs, G. A comparison between silicone and acrylic elastomers as dielectric materials in electroactive polymer actuators. Polym. Int. 2009, 59, 391–399. [Google Scholar] [CrossRef]
- Madsen, F.B.; Daugaard, A.E.; Hvilsted, S.; Skov, A.L. The Current State of Silicone-Based Dielectric Elastomer Transducers. Macromol. Rapid Commun. 2016, 37, 378–413. [Google Scholar] [CrossRef]
- Gallone, G.; Galantini, F.; Carpi, F. Perspectives for new dielectric elastomers with improved electromechanical actuation performance: Composites vs. blends. Polym. Int. 2010, 59, 400–406. [Google Scholar] [CrossRef]
- Shintake, J.; Rosset, S.; Schubert, B.; Floreano, D.; Shea, H. Versatile Soft Grippers with Intrinsic Electroadhesion Based on Multifunctional Polymer Actuators. Adv. Mater. 2015, 28, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Yang, J.; Wu, J.; Xin, X.; Li, Z.; Yuan, X.; Shen, X.; Dong, S. Piezoelectric Actuators and Motors: Materials, Designs, and Applications. Adv. Mater. Technol. 2019, 5. [Google Scholar] [CrossRef]
- Costa, C.M.; Cardoso, V.F.; Brito-Pereira, R.; Martins, P.; Correia, D.M.; Correia, V.; Ribeiro, C.; Martins, P.M.; Lanceros-Méndez, S. Electroactive poly(vinylidene fluoride)-based materials: Recent progress, challenges, and opportunities. In Fascinating Fluoropolymers and Their Applications; Elsevier: Amsterdam, The Netherlands, 2020; pp. 1–43. [Google Scholar] [CrossRef]
- Ren, B.; Cho, H.; Lissenden, C. A Guided Wave Sensor Enabling Simultaneous Wavenumber-Frequency Analysis for Both Lamb and Shear-Horizontal Waves. Sensors 2017, 17, 488. [Google Scholar] [CrossRef] [PubMed]
- da Cunha Rodrigues, G.; Zelenovskiy, P.; Romanyuk, K.; Luchkin, S.; Kopelevich, Y.; Kholkin, A. Strong piezoelectricity in single-layer graphene deposited on SiO2 grating substrates. Nat. Commun. 2015, 6, 7572. [Google Scholar] [CrossRef] [PubMed]
- Someya, T. Stretchable Electronics; Wiley-VCH Verlag GmbH: Weinheim, Germany, 2012; p. 462. [Google Scholar]
- Chorsi, M.T.; Curry, E.J.; Chorsi, H.T.; Das, R.; Baroody, J.; Purohit, P.K.; Ilies, H.; Nguyen, T.D. Piezoelectric Biomaterials for Sensors and Actuators. Adv. Mater. 2018, 31, 1802084. [Google Scholar] [CrossRef]
- Hu, F.; Xue, Y.; Xu, J.; Lu, B. PEDOT-Based Conducting Polymer Actuators. Front. Robot. AI 2019, 6, 114. [Google Scholar] [CrossRef]
- Naarmann, H. Polymers, Electrically Conducting. In Ullmann’s Encyclopedia of Industrial Chemistry; Wiley: Hoboken, NJ, USA, 2000. [Google Scholar] [CrossRef]
- Mazar, F.M.; Martinez, J.G.; Tyagi, M.; Alijanianzadeh, M.; Turner, A.P.F.; Jager, E.W.H. Artificial Muscles Powered by Glucose. Adv. Mater. 2019, 31, 1901677. [Google Scholar] [CrossRef]
- Maziz, A.; Concas, A.; Khaldi, A.; Stålhand, J.; Persson, N.K.; Jager, E.W.H. Knitting and weaving artificial muscles. Sci. Adv. 2017, 3, e1600327. [Google Scholar] [CrossRef]
- Hines, L.; Petersen, K.; Lum, G.Z.; Sitti, M. Soft Actuators for Small-Scale Robotics. Adv. Mater. 2016, 29, 1603483. [Google Scholar] [CrossRef]
- Diller, E.; Zhuang, J.; Lum, G.Z.; Edwards, M.R.; Sitti, M. Continuously distributed magnetization profile for millimeter-scale elastomeric undulatory swimming. Appl. Phys. Lett. 2014, 104, 174101. [Google Scholar] [CrossRef]
- Garstecki, P.; Tierno, P.; Weibel, D.B.; Sagués, F.; Whitesides, G.M. Propulsion of flexible polymer structures in a rotating magnetic field. J. Phys. Condens. Matter 2009, 21, 204110. [Google Scholar] [CrossRef] [PubMed]
- Mu, T.; Liu, L.; Lan, X.; Liu, Y.; Leng, J. Shape memory polymers for composites. Compos. Sci. Technol. 2018, 160, 169–198. [Google Scholar] [CrossRef]
- Bilodeau, R.A.; Miriyev, A.; Lipson, H.; Kramer-Bottiglio, R. All-soft material system for strong soft actuators. In Proceedings of the 2018 IEEE International Conference on Soft Robotics (RoboSoft), Livorno, Italy, 24–28 April 2018. [Google Scholar] [CrossRef]
- Lobo, P.S.; Almeida, J.; Guerreiro, L. Shape Memory Alloys Behaviour: A Review. Procedia Eng. 2015, 114, 776–783. [Google Scholar] [CrossRef]
- Renata, C.; Huang, W.M.; He, L.W.; Yang, J.J. Shape change/memory actuators based on shape memory materials. J. Mech. Sci. Technol. 2017, 31, 4863–4873. [Google Scholar] [CrossRef]
- Kang, D.J.; An, S.; Yarin, A.L.; Anand, S. Programmable soft robotics based on nano-textured thermo-responsive actuators. Nanoscale 2019, 11, 2065–2070. [Google Scholar] [CrossRef] [PubMed]
- Florea, L.; Diamond, D.; Benito-Lopez, F. Photo-Responsive Polymeric Structures Based on Spiropyran. Macromol. Mater. Eng. 2012, 297, 1148–1159. [Google Scholar] [CrossRef]
- Verpaalen, R.C.P.; da Cunha, M.P.; Engels, T.A.P.; Debije, M.G.; Schenning, A.P.H.J. Liquid Crystal Networks on Thermoplastics: Reprogrammable Photo-Responsive Actuators. Angew. Chem. Int. Ed. 2020, 59, 4532–4536. [Google Scholar] [CrossRef]
- Kwon, J.; Park, J.H.; Ku, S.; Jeong, Y.; Paik, N.J.; Park, Y.L. A Soft Wearable Robotic Ankle-Foot-Orthosis for Post-Stroke Patients. IEEE Robot. Autom. Lett. 2019, 4, 2547–2552. [Google Scholar] [CrossRef]
- Taniguchi, H. Flexible Artificial Muscle Actuator Using Coiled Shape Memory Alloy Wires. APCBEE Procedia 2013, 7, 54–59. [Google Scholar] [CrossRef]
- Anam, K.; Al-Jumaily, A.A. Active Exoskeleton Control Systems: State of the Art. Procedia Eng. 2012, 41, 988–994. [Google Scholar] [CrossRef]
- Peternel, L.; Noda, T.; Petrič, T.; Ude, A.; Morimoto, J.; Babič, J. Adaptive Control of Exoskeleton Robots for Periodic Assistive Behaviours Based on EMG Feedback Minimisation. PLoS ONE 2016, 11, e0148942. [Google Scholar] [CrossRef]
- Gorgey, A.S. Robotic exoskeletons: The current pros and cons. World J. Orthop. 2018, 9, 112–119. [Google Scholar] [CrossRef]
- Proietti, T.; Crocher, V.; Roby-Brami, A.; Jarrasse, N. Upper-Limb Robotic Exoskeletons for Neurorehabilitation: A Review on Control Strategies. IEEE Rev. Biomed. Eng. 2016, 9, 4–14. [Google Scholar] [CrossRef]
- Pons, J. Wearable Robots; Wiley: Hoboken, NJ, USA, 2008; p. 360. [Google Scholar]
- Lo, H.S.; Xie, S.Q. Exoskeleton robots for upper-limb rehabilitation: State of the art and future prospects. Med. Eng. Phys. 2012, 34, 261–268. [Google Scholar] [CrossRef]
- Yang, X.; Lihua, G.; Yang, Z.; Gu, W. Lower Extreme Carrying Exoskeleton Robot Adative Control Using Wavelet Neural Networks. In Proceedings of the 2008 Fourth International Conference on Natural Computation, Jinan, China, 18–20 October 2008. [Google Scholar] [CrossRef]
- Agarwal, P.; Deshpande, A.D. Impedance and force-field control of the index finger module of a hand exoskeleton for rehabilitation. In Proceedings of the 2015 IEEE International Conference on Rehabilitation Robotics (ICORR), Singapore, 11–14 August 2015. [Google Scholar] [CrossRef]
- Cavallaro, E.; Rosen, J.; Perry, J.; Burns, S.; Hannaford, B. Hill-Based Model as a Myoprocessor for a Neural Controlled Powered Exoskeleton Arm—Parameters Optimization. In Proceedings of the 2005 IEEE International Conference on Robotics and Automation, Barcelona, Spain, 18–22 April 2005. [Google Scholar] [CrossRef]
- Rosen, J.; Fuchs, M.B.; Arcan, M. Performances of Hill-Type and Neural Network Muscle Models—Toward a Myosignal-Based Exoskeleton. Comput. Biomed. Res. 1999, 32, 415–439. [Google Scholar] [CrossRef]
- Rosen, J.; Brand, M.; Fuchs, M.; Arcan, M. A myosignal-based powered exoskeleton system. IEEE Trans. Syst. Man Cybern. Part A Syst. Hum. 2001, 31, 210–222. [Google Scholar] [CrossRef]
- Kwon, B.; il Kim, S. Recursive Optimal Finite Impulse Response Filter and Its Application to Adaptive Estimation. Appl. Sci. 2022, 12, 2757. [Google Scholar] [CrossRef]
- Shafer, B.A.; Philius, S.A.; Nuckols, R.W.; McCall, J.; Young, A.J.; Sawicki, G.S. Neuromechanics and Energetics of Walking with an Ankle Exoskeleton Using Neuromuscular-Model Based Control: A Parameter Study. Front. Bioeng. Biotechnol. 2021, 9, 615358. [Google Scholar] [CrossRef]
- Song, G.; Huang, R.; Qiu, J.; Cheng, H.; Fan, S. Model-based Control with Interaction Predicting for Human-coupled Lower Exoskeleton Systems. J. Intell. Robot. Syst. 2020, 100, 389–400. [Google Scholar] [CrossRef]
- Huang, R.; Cheng, H.; Guo, H.; Chen, Q.; Lin, X. Hierarchical Interactive Learning for a HUman-Powered Augmentation Lower EXoskeleton. In Proceedings of the 2016 IEEE International Conference on Robotics and Automation (ICRA), Stockholm, Sweden, 16–21 May 2016. [Google Scholar] [CrossRef]
- Dinh, B.K.; Xiloyannis, M.; Antuvan, C.W.; Cappello, L.; Masia, L. Hierarchical Cascade Controller for Assistance Modulation in a Soft Wearable Arm Exoskeleton. IEEE Robot. Autom. Lett. 2017, 2, 1786–1793. [Google Scholar] [CrossRef]
- Copaci, D.; Serrano, D.; Moreno, L.; Blanco, D. A High-Level Control Algorithm Based on sEMG Signalling for an Elbow Joint SMA Exoskeleton. Sensors 2018, 18, 2522. [Google Scholar] [CrossRef] [PubMed]
- Nef, T.; Guidali, M.; Riener, R. ARMin III—Arm therapy exoskeleton with an ergonomic shoulder actuation. Appl. Bionics Biomech. 2009, 6, 127–142. [Google Scholar] [CrossRef]
- Balasubramanian, S.; Wei, R.; He, J. RUPERT closed loop control design. In Proceedings of the 2008 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Vancouver, BC, Canada, 20–24 August 2008. [Google Scholar] [CrossRef]
- Tsukahara, A.; Hasegawa, Y.; Sankai, Y. Gait support for complete spinal cord injury patient by synchronized leg-swing with HAL. In Proceedings of the 2011 IEEE/RSJ International Conference on Intelligent Robots and Systems, San Francisco, CA, USA, 25–30 September 2011. [Google Scholar] [CrossRef]
- Winkler, A.; Suchý, J. Robot Force/Torque Control in Assembly Tasks. IFAC Proc. Vol. 2013, 46, 796–801. [Google Scholar] [CrossRef]
- Hogan, N. Impedance Control: An Approach to Manipulation: Part I—Theory. J. Dyn. Syst. Meas. Control 1985, 107, 1–7. [Google Scholar] [CrossRef]
- Unluhisarcikli, O.; Pietrusinski, M.; Weinberg, B.; Bonato, P.; Mavroidis, C. Design and control of a robotic lower extremity exoskeleton for gait rehabilitation. In Proceedings of the 2011 IEEE/RSJ International Conference on Intelligent Robots and Systems, San Francisco, CA, USA, 25–30 September 2011. [Google Scholar] [CrossRef]
- Carignan, C.R.; Roderick, S.N.; Naylor, M.P. Distributed Control and Safety System for a Rehabilitation Arm Exoskeleton. In Proceedings of the ASME 2007 International Mechanical Engineering Congress and Exposition, Seattle, DC, USA, 11–15 November 2007. [Google Scholar] [CrossRef]
- Wu, Q.; Wang, X.; Du, F.; Xi, R. Modeling and position control of a therapeutic exoskeleton targeting upper extremity rehabilitation. Proc. Inst. Mech. Eng. Part C J. Mech. Eng. Sci. 2016, 231, 4360–4373. [Google Scholar] [CrossRef]
- Carignan, C.; Tang, J.; Roderick, S. Development of an exoskeleton haptic interface for virtual task training. In Proceedings of the 2009 IEEE/RSJ International Conference on Intelligent Robots and Systems, St. Louis, MO, USA, 11–15 October 2009. [Google Scholar] [CrossRef]
- Frisoli, A.; Borelli, L.; Montagner, A.; Marcheschi, S.; Procopio, C.; Salsedo, F.; Bergamasco, M.; Carboncini, M.C.; Tolaini, M.; Rossi, B. Arm rehabilitation with a robotic exoskeleleton in Virtual Reality. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 12–15 June 2007. [Google Scholar] [CrossRef]
- Nef, T.; Mihelj, M.; Kiefer, G.; Perndl, C.; Muller, R.; Riener, R. ARMin—Exoskeleton for Arm Therapy in Stroke Patients. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 12–15 June 2007. [Google Scholar] [CrossRef]
- Rahman, M.H.; K-Ouimet, T.; Saad, M.; Kenne, J.P.; Archambault, P.S. Tele-operation of a robotic exoskeleton for rehabilitation and passive arm movement assistance. In Proceedings of the 2011 IEEE International Conference on Robotics and Biomimetics, Karon Beach, Thailand, 7–11 December 2011. [Google Scholar] [CrossRef]
- Liu, Z.; Wang, L.; Chen, C.C.L.; Zeng, X.; Zhang, Y.; Wang, Y. Energy-Efficiency-Based Gait Control System Architecture and Algorithm for Biped Robots. IEEE Trans. Syst. Man Cybern. Part C (Appl. Rev.) 2012, 42, 926–933. [Google Scholar] [CrossRef]
- Park, J.; Kim, S.J.; Kyeong, S.; Kim, J.; Na, Y. Feasibility of proportional EMG control for a hand exoskeleton: A Fitts’ Law approach. IFAC-PapersOnLine 2018, 51, 214–219. [Google Scholar] [CrossRef]
- Xu, D.; Feng, Y.; Mai, J.; Wang, Q. Real-Time On-Board Recognition of Continuous Locomotion Modes for Amputees with Robotic Transtibial Prostheses. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 2015–2025. [Google Scholar] [CrossRef]
- Venkatagiri, R. Optimization of Robotic Exoskeleton with Ameliorated Stability System. Int. J. Innov. Sci. Res. Technol. 2017, 2, 522–525. [Google Scholar]
- Naik, G.R.; Pendharkar, G.; Nguyen, H.T. Wavelet PCA for automatic identification of walking with and without an exoskeleton on a treadmill using pressure and accelerometer sensors. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016. [Google Scholar] [CrossRef]
- Simon, A.M.; Ingraham, K.A.; Spanias, J.A.; Young, A.J.; Finucane, S.B.; Halsne, E.G.; Hargrove, L.J. Delaying Ambulation Mode Transition Decisions Improves Accuracy of a Flexible Control System for Powered Knee-Ankle Prosthesis. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 1164–1171. [Google Scholar] [CrossRef]
- Zhang, K.; de Silva, C.W.; Fu, C. Sensor Fusion for Predictive Control of Human-Prosthesis-Environment Dynamics in Assistive Walking: A Survey. arXiv 2019. [Google Scholar] [CrossRef]
- Pratt, J.; Krupp, B.; Morse, C.; Collins, S. The RoboKnee: An exoskeleton for enhancing strength and endurance during walking. In Proceedings of the IEEE International Conference on Robotics and Automation, ICRA ’04, New Orleans, LA, USA, 26 April–1 May 2004. [Google Scholar] [CrossRef]
- Kong, K.; Jeon, D. Design and control of an exoskeleton for the elderly and patients. IEEE/ASME Trans. Mechatron. 2006, 11, 428–432. [Google Scholar] [CrossRef]
- Fleischer, C.; Hommel, G. A Human–Exoskeleton Interface Utilizing Electromyography. IEEE Trans. Robot. 2008, 24, 872–882. [Google Scholar] [CrossRef]
- Rettinger, J.; Schwarz, S.; Schwarz, W. Electrophysiology Basics, Modern Approaches and Applications; Springer: Cham, Switzerland, 2016; p. 175. [Google Scholar]
- André, A.D.; Teixeira, A.M.; Martins, P. EMG Signals as a Way to Control Soft Actuators. In Computer Methods, Imaging and Visualization in Biomechanics and Biomedical Engineering II; Springer International Publishing: Cham, Switzerland, 2022; pp. 50–58. [Google Scholar] [CrossRef]
- Péter, A.; Arndt, A.; Hegyi, A.; Finni, T.; Andersson, E.; Alkjær, T.; Tarassova, O.; Rönquist, G.; Cronin, N. Effect of footwear on intramuscular EMG activity of plantar flexor muscles in walking. J. Electromyogr. Kinesiol. 2020, 55, 102474. [Google Scholar] [CrossRef] [PubMed]
- Qi, J.; Jiang, G.; Li, G.; Sun, Y.; Tao, B. Surface EMG hand gesture recognition system based on PCA and GRNN. Neural Comput. Appl. 2019, 32, 6343–6351. [Google Scholar] [CrossRef]
- Oskoei, M.A.; Hu, H. Myoelectric control systems—A survey. Biomed. Signal Process. Control 2007, 2, 275–294. [Google Scholar] [CrossRef]
- Lenzi, T.; Rossi, S.M.M.D.; Vitiello, N.; Carrozza, M.C. Intention-Based EMG Control for Powered Exoskeletons. IEEE Trans. Biomed. Eng. 2012, 59, 2180–2190. [Google Scholar] [CrossRef]
- Noda, T.; Furukawa, J.; Teramae, T.; Hyon, S.H.; Morimoto, J. An electromyogram based force control coordinated in assistive interaction. In Proceedings of the 2013 IEEE International Conference on Robotics and Automation, Karlsruhe, Germany, 6–10 May 2013. [Google Scholar] [CrossRef]
- Farina, D.; Merletti, R.; Indino, B.; Nazzaro, M.; Pozzo, M. Surface EMG crosstalk between knee extensor muscles: Experimental and model results. Muscle Nerve 2002, 26, 681–695. [Google Scholar] [CrossRef]
- Wilson, S.; Vaidyanathan, R. Upper-limb prosthetic control using wearable multichannel mechanomyography. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017. [Google Scholar] [CrossRef]
- Orizio, C. Muscle sound: Bases for the introduction of a mechanomyographic signal in muscle studies. Crit. Rev. Biomed. Eng. 1993, 21, 201–243. [Google Scholar]
- Dallali, H.; Demircan, E.; Rastgaar, M. Powered Prostheses Design, Control, and Clinical Applications; Elsevier Science and Technology: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Rabe, K.G.; Jahanandish, M.H.; Hoyt, K.; Fey, N.P. Use of Sonomyography for Continuous Estimation of Hip, Knee and Ankle Moments During Multiple Ambulation Tasks. In Proceedings of the 2020 8th IEEE RAS/EMBS International Conference for Biomedical Robotics and Biomechatronics (BioRob), New York, NY, USA, 29 November–1 December 2020. [Google Scholar] [CrossRef]
- He, J.; Luo, H.; Jia, J.; Yeow, J.T.W.; Jiang, N. Wrist and Finger Gesture Recognition with Single-Element Ultrasound Signals: A Comparison with Single-Channel Surface Electromyogram. IEEE Trans. Biomed. Eng. 2019, 66, 1277–1284. [Google Scholar] [CrossRef]
- Mitchell, W.K.; Phillips, B.E.; Williams, J.P.; Rankin, D.; Smith, K.; Lund, J.N.; Atherton, P.J. Development of a new Sonovue™ contrast-enhanced ultrasound approach reveals temporal and age-related features of muscle microvascular responses to feeding. Physiol. Rep. 2013, 1, e00119. [Google Scholar] [CrossRef] [PubMed]
- Noda, T.; Sugimoto, N.; Furukawa, J.; Sato, M.A.; Hyon, S.H.; Morimoto, J. Brain-controlled exoskeleton robot for BMI rehabilitation. In Proceedings of the 2012 12th IEEE-RAS International Conference on Humanoid Robots (Humanoids 2012), Osaka, Japan, 29 November–1 December 2012. [Google Scholar] [CrossRef]
- Vinoj, P.G.; Jacob, S.; Menon, V.G.; Rajesh, S.; Khosravi, M.R. Brain-Controlled Adaptive Lower Limb Exoskeleton for Rehabilitation of Post-Stroke Paralyzed. IEEE Access 2019, 7, 132628–132648. [Google Scholar] [CrossRef]
- Páris, C.; Barbosa, J.; Ferreira, E.; Gomes, A. BITalino use and applications for health, education, home automation and industry. In Proceedings of the 8th International Conference on Society and Information Technologies, Orlando, FL, USA, 21–24 March 2017; pp. 21–24. [Google Scholar]
- pluX. pluX—Bitalino. Available online: https://www.pluxbiosignals.com (accessed on 13 October 2023).
- Mannatunga, K.S.; Ali, S.H.M.; Crespo, M.L.; Cicuttin, A.; Samarawikrama, J.G. High Performance 128-Channel Acquisition System for Electrophysiological Signals. IEEE Access 2020, 8, 122366–122383. [Google Scholar] [CrossRef]
- TMSi. Available online: https://www.tmsi.com (accessed on 12 October 2023).
- Rewalk. Available online: https://rewalk.com (accessed on 5 October 2023).
- Ekso Bionics. Available online: https://eksobionics.com/research/ (accessed on 12 October 2023).
- Cyberdyne. Available online: https://www.cyberdyne.jp/english/ (accessed on 12 October 2023).
- RB3D. Available online: https://www.rb3d.com (accessed on 23 December 2020).
- Chen, B.; Zi, B.; Zeng, Y.; Qin, L.; Liao, W.H. Ankle-foot orthoses for rehabilitation and reducing metabolic cost of walking: Possibilities and challenges. Mechatronics 2018, 53, 241–250. [Google Scholar] [CrossRef]
- Yamamoto, S.; Ebina, M.; Kubo, S.; Hayashi, T.; Akita, Y.; Hayakawa, Y. Development of an Ankle-Foot Orthosis with Dorsiflexion Assist, Part 2. J. Prosthet. Orthot. 1999, 11, 24–28. [Google Scholar] [CrossRef]
- Ramsey, J.A. Development of a method for fabricating polypropylene non-articulated dorsiflexion assist ankle foot orthoses with predetermined stiffness. Prosthet. Orthot. Int. 2011, 35, 54–69. [Google Scholar] [CrossRef]
- Furusho, J.; Kikuchi, T.; Tokuda, M.; Kakehashi, T.; Ikeda, K.; Morimoto, S.; Hashimoto, Y.; Tomiyama, H.; Nakagawa, A.; Akazawa, Y. Development of Shear Type Compact MR Brake for the Intelligent Ankle-Foot Orthosis and Its Control; Research and Development in NEDO for Practical Application of Human Support Robot. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 12–15 June 2007. [Google Scholar] [CrossRef]
- Takahashi, K.Z.; Lewek, M.D.; Sawicki, G.S. A neuromechanics-based powered ankle exoskeleton to assist walking post-stroke: A feasibility study. J. NeuroEng. Rehabil. 2015, 12, 23. [Google Scholar] [CrossRef]
- Dong, W.; Liu, C.; Zhang, Q.; Xiong, C. Design and Evaluation of an Active Ankle Exoskeleton in Gait Assistance. In Proceedings of the 2019 IEEE/ASME International Conference on Advanced Intelligent Mechatronics (AIM), Hong Kong, China, 8–12 July 2019. [Google Scholar] [CrossRef]
- Awad, L.N.; Bae, J.; O’Donnell, K.; Rossi, S.M.M.D.; Hendron, K.; Sloot, L.H.; Kudzia, P.; Allen, S.; Holt, K.G.; Ellis, T.D.; et al. A soft robotic exosuit improves walking in patients after stroke. Sci. Transl. Med. 2017, 9, eaai9084. [Google Scholar] [CrossRef]
- Etenzi, E.; Borzuola, R.; Grabowski, A.M. Passive-elastic knee-ankle exoskeleton reduces the metabolic cost of walking. J. Neuroeng. Rehabil. 2020, 17, 104. [Google Scholar] [CrossRef]
- Galle, S.; Malcolm, P.; Collins, S.H.; Clercq, D.D. Reducing the metabolic cost of walking with an ankle exoskeleton: Interaction between actuation timing and power. J. Neuroeng. Rehabil. 2017, 14, 35. [Google Scholar] [CrossRef]
- Bougrinat, Y.; Achiche, S.; Raison, M. Design and development of a lightweight ankle exoskeleton for human walking augmentation. Mechatronics 2019, 64, 102297. [Google Scholar] [CrossRef]
- Brown, P.; Jones, D.; Singh, S.; Rosen, J. The exoskeleton glove for control of paralyzed hands. In Proceedings of the [1993] IEEE International Conference on Robotics and Automation, Atlanta, GA, USA, 2–6 May 1993. [Google Scholar] [CrossRef]
- Ferguson, P.W.; Shen, Y.; Rosen, J. Hand Exoskeleton Systems—Overview. In Wearable Robotics; Elsevier: Amsterdam, The Netherlands, 2020; pp. 149–175. [Google Scholar] [CrossRef]
- Muellbacher, W.; Richards, C.; Ziemann, U.; Wittenberg, G.; Weltz, D.; Boroojerdi, B.; Cohen, L.; Hallett, M. Improving Hand Function in Chronic Stroke. Arch. Neurol. 2002, 59, 1278. [Google Scholar] [CrossRef] [PubMed]
- Lucas, L.; DiCicco, M.; Matsuoka, Y. An EMG-Controlled Hand Exoskeleton for Natural Pinching. J. Robot. Mechatron. 2004, 16, 482–488. [Google Scholar] [CrossRef]
- In, H.; Cho, K.J.; Kim, K.; Lee, B. Jointless structure and under-actuation mechanism for compact hand exoskeleton. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 29 June–1 July 2011. [Google Scholar] [CrossRef]
- Rose, C.G.; O’Malley, M.K. Hybrid Rigid-Soft Hand Exoskeleton to Assist Functional Dexterity. IEEE Robot. Autom. Lett. 2019, 4, 73–80. [Google Scholar] [CrossRef]
- Wege, A.; Hommel, G. Development and control of a hand exoskeleton for rehabilitation of hand injuries. In Proceedings of the 2005 IEEE/RSJ International Conference on Intelligent Robots and Systems, Edmonton, AB, Canada, 2–6 August 2005. [Google Scholar] [CrossRef]
- Kawasaki, H.; Ito, S.; Ishigure, Y.; Nishimoto, Y.; Aoki, T.; Mouri, T.; Sakaeda, H.; Abe, M. Development of a Hand Motion Assist Robot for Rehabilitation Therapy by Patient Self-Motion Control. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 12–15 June 2007. [Google Scholar] [CrossRef]
- Shields, B.; Main, J.; Peterson, S.; Strauss, A. An anthropomorphic hand exoskeleton to prevent astronaut hand fatigue during extravehicular activities. IEEE Trans. Syst. Man Cybern. Part A Syst. Hum. 1997, 27, 668–673. [Google Scholar] [CrossRef]
- Hasegawa, Y.; Mikami, Y.; Watanabe, K.; Sankai, Y. Five-fingered assistive hand with mechanical compliance of human finger. In Proceedings of the 2008 IEEE International Conference on Robotics and Automation, Pasadena, CA, USA, 19–23 May 2008. [Google Scholar] [CrossRef]
- Stergiopoulos, P.; Fuchs, P.; Laurgeau, C. Design of a 2-finger hand exoskeleton for VR grasping simulation. In Proceedings of the Eurohaptics, Dublin, Ireland, 6–9 July 2003; pp. 80–93. [Google Scholar]
- Park, Y.; Jo, I.; Lee, J.; Bae, J. A Dual-cable Hand Exoskeleton System for Virtual Reality. Mechatronics 2018, 49, 177–186. [Google Scholar] [CrossRef]
- Yap, H.K.; Ang, B.W.K.; Lim, J.H.; Goh, J.C.H.; Yeow, C.H. A fabric-regulated soft robotic glove with user intent detection using EMG and RFID for hand assistive application. In Proceedings of the 2016 IEEE International Conference on Robotics and Automation (ICRA), Stockholm, Sweden, 16–21 May 2016. [Google Scholar] [CrossRef]
- Díez, J.A.; Catalán, J.M.; Lledó, L.D.; Badesa, F.J.; Garcia-Aracil, N. Multimodal robotic system for upper-limb rehabilitation in physical environment. Adv. Mech. Eng. 2016, 8. [Google Scholar] [CrossRef]
- Díez, J.A.; Blanco, A.; Catalán, J.M.; Badesa, F.J.; Lledó, L.D.; García-Aracil, N. Hand exoskeleton for rehabilitation therapies with integrated optical force sensor. Adv. Mech. Eng. 2018, 10. [Google Scholar] [CrossRef]
- Agarwal, P.; Yun, Y.; Fox, J.; Madden, K.; Deshpande, A.D. Design, control, and testing of a thumb exoskeleton with series elastic actuation. Int. J. Robot. Res. 2017, 36, 355–375. [Google Scholar] [CrossRef]
- Klug, F.; Hessinger, M.; Koka, T.; Witulla, P.; Will, C.; Schlichting, T.; Endl, C.; Albenstetter, A.; Champagne, P.O.; Gagnon, D.H.; et al. An Anthropomorphic Soft Exosuit for Hand Rehabilitation. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019. [Google Scholar] [CrossRef]
- Bulboacă, A.E.; Bolboacă, S.D.; Bulboacă, A.C. Ethical considerations in providing an upper limb exoskeleton device for stroke patients. Med. Hypotheses 2017, 101, 61–64. [Google Scholar] [CrossRef]
- Burton, S.D. Responsible use of exoskeletons and exosuits: Ensuring domestic security in a European context. Paladyn J. Behav. Robot. 2020, 11, 370–378. [Google Scholar] [CrossRef]
- Greenbaum, D. Ethical, legal and social concerns relating to exoskeletons. ACM SIGCAS Comput. Soc. 2016, 45, 234–239. [Google Scholar] [CrossRef]
- Bao, G.; Pan, L.; Fang, H.; Wu, X.; Yu, H.; Cai, S.; Yu, B.; Wan, Y. Academic Review and Perspectives on Robotic Exoskeletons. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 2294–2304. [Google Scholar] [CrossRef] [PubMed]
- Hill, D.; Holloway, C.S.; Ramirez, D.Z.M.; Smitham, P.; Pappas, Y. What are user perspectives of exoskeleton technology? A literature review. Int. J. Technol. Assess. Health Care 2017, 33, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Li, N.; Xue, X.; Lu, X.; Li, D.; Hong, Q. Effects of lower limb exoskeleton gait orthosis compared to mechanical gait orthosis on rehabilitation of patients with spinal cord injury: A systematic review and future perspectives. Gait Posture 2023, 102, 64–71. [Google Scholar] [CrossRef]
- de Miguel-Fernández, J.; Lobo-Prat, J.; Prinsen, E.; Font-Llagunes, J.M.; Marchal-Crespo, L. Control strategies used in lower limb exoskeletons for gait rehabilitation after brain injury: A systematic review and analysis of clinical effectiveness. J. NeuroEng. Rehabil. 2023, 20, 23. [Google Scholar] [CrossRef]
- Oña, E.D.; Garcia-Haro, J.M.; Jardón, A.; Balaguer, C. Robotics in Health Care: Perspectives of Robot-Aided Interventions in Clinical Practice for Rehabilitation of Upper Limbs. Appl. Sci. 2019, 9, 2586. [Google Scholar] [CrossRef]
- Akbari, A.; Haghverd, F.; Behbahani, S. Robotic Home-Based Rehabilitation Systems Design: From a Literature Review to a Conceptual Framework for Community-Based Remote Therapy During COVID-19 Pandemic. Front. Robot. AI 2021, 8, 612331. [Google Scholar] [CrossRef]
- Wolff, J.; Parker, C.; Borisoff, J.; Mortenson, W.B.; Mattie, J. A survey of stakeholder perspectives on exoskeleton technology. J. NeuroEng. Rehabil. 2014, 11, 169. [Google Scholar] [CrossRef]
- Vélez-Guerrero, M.A.; Callejas-Cuervo, M.; Mazzoleni, S. Artificial Intelligence-Based Wearable Robotic Exoskeletons for Upper Limb Rehabilitation: A Review. Sensors 2021, 21, 2146. [Google Scholar] [CrossRef]










| Type of Materials | Advantages | Disadvantages | References | |
|---|---|---|---|---|
| Higher weight | ||||
| Aluminium | Higher mechanical strength | Diminished ergonomy and comfort | ||
| Rigid | Stainless steel | Higher elastic limit | Larger inertias | [65,69,70,71,72,73,74,75] |
| Titanium | Higher safety | Unnatural motion patterns | ||
| Lead to higher power consumption | ||||
| Safer | ||||
| Allow smoother movements | ||||
| Higher comfort | ||||
| Polymers | Higher portability and flexibility | Lower yield strength | ||
| Soft | Composites | Lightweight | Actuators with lower force/torque and velocity | [57,66,68,69,73,76,77,78,79,80] |
| (e.g., SMPs, EAPs) | Biomimetic | Adequate for smaller assistance levels | ||
| Accommodate large deformations | ||||
| Possible use as actuators | ||||
| Easy to process and mass produce |
| Type of Actuators | Energy Source | Advantages | References | |||
|---|---|---|---|---|---|---|
| Traditional actuators | Purely mechanical actuators | Unpowered | No need for an external source of energy Allow reducing metabolic consumption | [44,84,86,87] | ||
| Mechanical servomotor-based actuators | Powered—electrical input | High-efficiency power conversion Quiet, clean, and create no pollution Less expensive and easy to maintain Easy to implement the remote-control system No limitation of separation between the energy source and system | [88,89] | |||
| Pneumatic actuators | Powered—compressed gas | Affordable Fast working cycle Insensitive to temperature drift No need for mechanical transmission High actuating forces | [89,90,91] | |||
| Hydraulic actuators | Powered—compressed fluid | High stability High stroking velocity Suitable for high loads High actuating force Stiff and incompressible source | [92,93] | |||
| Soft actuators | Electrical responsive actuators | Powered—electrical stimulus | Dielectric actuator | Soft, flexible, and stretchable Scalable High power-to-weight ratio Stores and recovers kinetic energy | [89,94,95,96,97,98] | |
| Piezoelectric actuator | Suitable for high force applications Large operation bandwidth | [77,99,100,101,102,103,104] | ||||
| Conducting polymers | Possibility of being fed through biofuels Processability Good biological muscles emulation | [105,106,107,108] | ||||
| Magnetic responsive actuators | Powered—magnetic stimulus | Linear effect Quick response Capacity to penetrate most materials | [89,109,110,111] | |||
| Thermal responsive actuators | Powered—thermal stimulus | SMM | SMPs | Low cost Biodegradable Low density High elastic deformable Sustain a broad range of temperature drift | [89,112,113] | |
| SMAs | Flexible in nature High energy density Low actuation temperature Provides large frequency response | [114,115,116] | ||||
| Photo-responsive actuators | Powered—light stimulus | Environmentally friendly Full possibility of remote control Easy to control the response Excellent resolution | [89,117,118] | |||
| Sensors | Advantages | Disadvantages | References | |
|---|---|---|---|---|
| EMG | Measures the electrical signals from the muscle contraction | Predict movement intension even if with any movement performed Already tested | Biasable by muscle crosstalk susceptibility, skin conditions, muscle fatigue | [122,151,156,162,163,164,165,166,167] |
| MMG | Measures vibration and volume by changes in muscles | Less sensitive to skin conditions | Biasable by muscle fatigue | [156,168,169] |
| SMG | Measures thickness and deformation of muscles | Able to classify several motions and predict joint kinetics during dynamic activities | Biasable by muscle fatigue | [156,170,171,172] |
| EEG | Measures electrical activity in the brain | No need for sensors in the muscles | Not enough accuracy | [156,174] |
| Weight | Structural Materials | Actuation Method | Control System | Results | References | |
|---|---|---|---|---|---|---|
| Awad et al. | 0.9 kg | Textile materials | Powered—Bowden cables | IMU and load cells | Reduces the metabolic cost | [190] |
| Etenzi et al. | 1.4 kg | Aluminium | Unpowered—Springs | Mechanic | Increases the metabolic cost in 23% | [191] |
| Galle et al. | 0.89 kg | - | Powered—Pneumatic actuators | Iterative Learning Algorithm, load cells and IMU sensors | Reduces the metabolic cost in 12% | [192] |
| Bougrinat et al. | 2.045 kg (considering all components) | Carbon fiber | Powered—Bowden cables | Hierarchic Control Architecture | Reduces significantly the metabolic cost of the plantar flexion muscles | [193] |
| Type | Structural Materials | Actuation Method | Control System | Results | References | |
|---|---|---|---|---|---|---|
| Yap et al. | Assistive | Elastomers textile gloves | Pneumatic Actuators | EMG RFID | Satisfactory results Maximum force achieved 1.57 N | [206] |
| Díez et al. | Rehabilitation | 3D printable material PLA | Electric linear Actuators | EMG controller | 97% success during the trials | [207,208] |
| Agarwal et al. | Rehabilitation | Selective laser sintering materials Metallic load bearing parts | Bowden cables with springs Brushed DC motor | - | Compatible natural motion solution Max. torque 0.4 Nm | [128,209] |
| Klug et al. | Rehabilitation | Glove—microfibers, elastics and PU pleather | Wires Electrical motor | Force sensorsMachine learning algorithm | Max. angle motion 132° Max. force 27.4 N | [210] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
André, A.D.; Martins, P. Exo Supportive Devices: Summary of Technical Aspects. Bioengineering 2023, 10, 1328. https://doi.org/10.3390/bioengineering10111328
André AD, Martins P. Exo Supportive Devices: Summary of Technical Aspects. Bioengineering. 2023; 10(11):1328. https://doi.org/10.3390/bioengineering10111328
Chicago/Turabian StyleAndré, António Diogo, and Pedro Martins. 2023. "Exo Supportive Devices: Summary of Technical Aspects" Bioengineering 10, no. 11: 1328. https://doi.org/10.3390/bioengineering10111328