Dynamic Expression of Follicle-Stimulating Hormone and Estrogen mRNA Receptors Associated with microRNAs 34a and -let-7c in Canine Follicles during the Estrous Cycle
Abstract
:Simple Summary
Abstract
1. Introduction
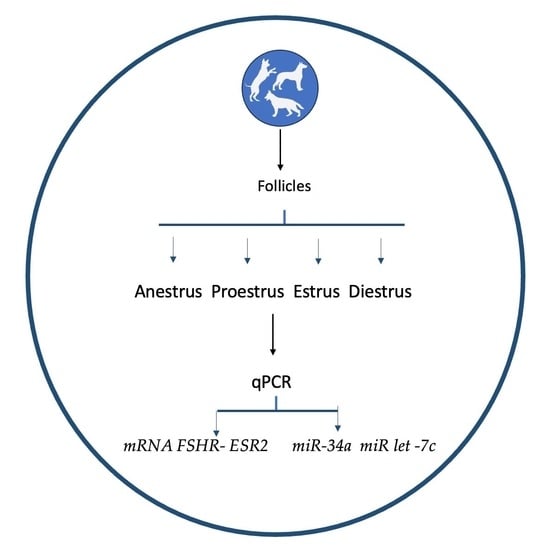
2. Materials and Methods
2.1. Animals
2.2. Ovaries Processing and Follicles Isolation
2.3. microRNA Selection
2.4. RNA Isolation, Primers, and qPCR Analysis
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bosch, E.; Alviggi, C.M.; Conforti, A.; Hanyaloglu, A.C.; Chuderland, D.; Simoni, M.; Raine-Fenning, N.; Crépieux, P.; Kol, S.; Rochira, V.; et al. Reduced FSH and LH action: Implications for medically assisted reproduction. Hum. Reprod. 2021, 36, 1469–1480. [Google Scholar] [CrossRef] [PubMed]
- George, J.; Dille, E.A.; Heckert, L.L. Current Concepts of Follicle-Stimulating Hormone Receptor Gene Regulation. Biol. Reprod. 2011, 84, 7–17. [Google Scholar] [CrossRef] [PubMed]
- McDonald, R.; Sadler, C.; Kumar, T.R. Gain–of–Function Genetic Models to Study FSH Action. Front. Endocrinol. 2019, 10, 28. [Google Scholar] [CrossRef] [PubMed]
- Tisdall, D.J.; Watanabe, N.L.; Hudson, P.; McNatty, K.P. FSH receptor gene expression during ovarian follicle development in sheep. J. Mol. Endocrinol. 1995, 15, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Wandji, S.A.; Eppig, J.J.; Fortune, J.E. FSH and growth factors affect the growth and endocrine function in vitro of granulosa cells of bovine preantral follicles. Theriogenology 1996, 45, 817–832. [Google Scholar] [CrossRef]
- De Cock, H.; Ducatelle, R.; Logghe, J.P. Immunohistochemical localization of estrogen receptor in the normal canine female genital tract. Dom. Anim. Endocrinol. 1997, 14, 133–147. [Google Scholar] [CrossRef]
- McBride, M.W.; Aughey, E.; O’Shaughnessy, P.J.; Jeffcoate, I.A. Ovarian function and FSH receptor characteristics during canine anoestrus. J. Reprod. Fertil. Suppl. 2001, 57, 3–10. [Google Scholar]
- Saint-Dizier, M.; Jaffré, N.; Reynaud, K.; Remy, B.; Thoumire, S.; Chastant-Maillard, S. Expression of follicle-stimulating hormone and luteinising hormone binding sites in the bitch ovary during the follicular phase. Reprod. Fertil. Dev. 2008, 20, 925–934. [Google Scholar] [CrossRef]
- Klinge, C.M. Estrogen Regulation of MicroRNA Expression. Curr. Genom. 2009, 10, 169–183. [Google Scholar] [CrossRef]
- O’Lone, R.; Frith, M.C.; Karlsson, E.K.; Hansen, U. Genomic Targets of Nuclear Estrogen Receptors. Mol. Endocrinol. 2004, 18, 1859–1875. [Google Scholar] [CrossRef]
- Tang, Z.R.; Zhang, R.; Lian, Z.X.; Deng, S.L.; Yu, K. Estrogen-Receptor Expression and Function in Female Reproductive Disease. Cells 2019, 8, 1123. [Google Scholar] [CrossRef] [PubMed]
- Hatoya, S.; Torii, R.; Kumagai, D.; Sugiura, K.; Kawate, N.; Tamada, H.; Sawada, T.; Inaba, T. Expression of estrogen receptor a and b genes in the medio basal hypothalamus, pituitary and ovary during the canine estrous cycle. Neurosci. Let. 2003, 347, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.B.; Chakravarthi, V.P.; Wolfe, M.W.; Rumi, M.A. ERβ Regulation of Gonadotropin Responses during Folliculogenesis. Int. J. Mol. Sci. 2021, 22, 10348. [Google Scholar] [CrossRef] [PubMed]
- Emori, C.; Kanke, T.; Ito, H.; Akimoto, Y.; Fujii, W.; Naito, K.; Sugiura, K. Expression and regulation of estrogen receptor 2 and its coregulators in mouse granulosa cells. J. Reprod. Dev. 2022, 68, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Couse, J.F.; Yates, M.M.; Deroo, B.J.; Korach, K.S. Estrogen receptor-beta is critical to granulosa cell differentiation and the ovulatory response to gonadotropins. Endocrinology 2005, 146, 3247–3262. [Google Scholar] [CrossRef]
- Toms, D.; Pan, B.; Li, J. Endocrine Regulation in the Ovary by MicroRNA during the Estrous Cycle. Front. Endocrinol. 2018, 8, 378. [Google Scholar] [CrossRef]
- Yang, S.; Wang, S.; Luo, A.; Ding, T.; Lai, Z.; Shen, W. Expression patterns and regulatory functions of microRNAs during the initiation of primordial follicle development in the neonatal mouse ovary. Biol. Reprod. 2013, 89, 126. [Google Scholar] [CrossRef]
- Sen, A.; Prizant, H.; Light, A.; Biswas, A.; Hayes, E.; Lee, H.J.; Barad, D.; Gleicher, N.; Hammes, S.R. Androgens regulate ovarian follicular development by increasing follicle stimulating hormone receptor and microRNA-125b expression. Proc. Natl. Acad. Sci. USA 2014, 111, 3008–3013. [Google Scholar] [CrossRef]
- Dehghan, Z.; Mohammadi-Yeganeh, S.; Rezaee, D.; Salehi, M. MicroRNA-21 is involved in oocyte maturation, blastocyst formation, and pre-implantation embryo development. Dev. Biol. 2021, 480, 69–77. [Google Scholar] [CrossRef]
- Ro, S.; Song, R.; Park, C.; Zheng, H.; Sanders, K.M.; Yan, W. Cloning and expression profiling of small RNAs expressed in the mouse ovary. RNA 2007, 13, 2366–2380. [Google Scholar] [CrossRef]
- Tesfaye, D.; Gebremedhn, S.; Salilew-Wondim, D.; Hailay, T.; Hoelker, M.; Grosse-Brinkhaus, C.; Schellander, K. MicroRNAs: Tiny molecules with a significant role in mammalian follicular and oocyte development. Reproduction 2018, 155, R121–R135. [Google Scholar] [CrossRef] [PubMed]
- Ambros, V. MicroRNAs: Tiny regulators with great potential. Cell 2001, 107, 823–826. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, J.; Hayder, H.; Zayed, Y.; Peng, C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018, 9, 402. [Google Scholar] [CrossRef] [PubMed]
- Vasudevan, S.; Tong, Y.C.; Steitz, J.A. Switching from repression to activation: microRNAs can up-regulate translation. Science 2007, 318, 1931–1934. [Google Scholar] [CrossRef] [PubMed]
- Yin, M.; Wang, X.; Yao, G. Transactivation of micrornA-320 by microRNA-383 regulates granulosa cell functions by targeting E2F1 and SF-1 proteins. J. Biol. Chem. 2014, 289, 18239–18257. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Chen, C.Z.; Xu, M.Q.; Zhang, L.Q.; Liu, J.B.; Gao, Y.; Jiang, H.; Yuan, B.; Zhang, J.B. MiR-31 and miR-143 affect steroid hormone synthesis and inhibit cell apoptosis in bovine granulosa cells through FSHR. Theriogenology 2018, 123, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Yin, M.; Lu, M.; Yao, G.; Tian, H.; Lian, J.; Liu, L.; Liang, M.; Wang, Y.; Sun, F. Transactivation of microRNA-383 by steroidogenic factor-1 promotes estradiol release from mouse ovarian granulosa cells by targeting RBMS1. Mol. Endocrinol. 2012, 26, 1129–1143. [Google Scholar] [CrossRef]
- Donadeu, F.X.; Schauer, S.N.; Sontakke, S.D. Involvement of miRNAs in ovarian follicular and luteal development. J. Endocrinol. 2012, 215, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Fabová, Z.; Loncová, B.; Sirotkin, A.V. MicroRNA miR-125b can suppress ovarian granulosa cell functions: Interrelationships with FSH. Cell Biochem. Funct. 2022, 41, 177–188. [Google Scholar] [CrossRef]
- De Los Reyes, M.; Palomino, J.; Araujo, A.; Flores, J.; Ramirez, G.; Parraguez, V.H.; Aspee, K. Cyclooxygenase 2 messenger RNA levels in canine follicular cells: Interrelationship with GDF- 9, BMP-15 and progesterone. Dom. Anim. Endocrinol. 2021, 74, 106529. [Google Scholar] [CrossRef]
- Ramirez, G.; Palomino, J.; Aspee, K.; De los Reyes, M. GDF-9 and BMP-15 mRNA levels in canine cumulus cells related to cumulus expansion and the maturation process. Animals 2020, 10, 462. [Google Scholar] [CrossRef]
- Fernandez, T.; Palomino, J.; Parraguez, V.H.; Peralta, O.A.; De los Reyes, M. Differential expression of GDF-9 and BMP- 15 during follicular development in canine ovaries evaluated by flow cytometry. Anim. Reprod. Sci. 2016, 167, 59–67. [Google Scholar] [CrossRef] [PubMed]
- De los Reyes, M.; Palomino, J.; Parraguez, V.H.; Ramírez, F. Analysis of LH receptor in canine ovarian follicles throughout the estrous cycle. Theriogenology 2017, 93, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Kozomara, A.; Birgaoanu, M.; Griffiths-Jones, S. miRBase: From microRNA sequences to function. Nucleic Acids Res. 2019, 47, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Sticht, C.; De La Torre, C.; Parveen, A.; Gretz, N. miRWalk: An online resource for prediction of microRNA binding sites. PLoS ONE 2018, 13, 0206239. [Google Scholar] [CrossRef] [PubMed]
- Riolo, G.; Cantara, S.; Marzocchi, C.; Ricci, C. miRNA Targets: From Prediction Tools to Experimental Validation. Methods Protoc. 2021, 4, 1. [Google Scholar] [CrossRef]
- Craig, K.K.; Wood, G.A.; Keller, S.; Mutsaers, A.J.; Wood, R.D. MicroRNA profiling in canine multicentric lymphoma. PLoS ONE 2019, 14, e0226357. [Google Scholar] [CrossRef]
- Narita, M.; Nishida, H.; Asahina, R.; Nakata, K.; Yano, H.; Ueda, T.; Inden, M.; Akiyoshi, H.; Maeda, S.; Kamishina, H. Identification of reference genes for microRNAs of extracellular vesicles isolated from plasma samples of healthy dogs by ultracentrifugation, precipitation, and membrane affinity chromatography methods. Am. J. Vet. Res. 2019, 80, 449–454. [Google Scholar] [CrossRef]
- Goncalves, J.S.A.; Vannucchi, C.I.; Braga, F.C.; Paula-Lopes, F.F.; Milazzotto, M.P.; Assumpcao, M.E.O.A.; Visintin, J.A. Oestrogen and Progesterone receptor gene expression in canine oocytes and cumulus cells throughout the oestrous cycle. Reprod. Dom. Anim. 2009, 44 (Suppl. S2), 239–242. [Google Scholar] [CrossRef]
- Palomino, J.; De los Reyes, M. Temporal expression of GDF-9 and BMP-15 mRNAs in canine ovarian follicles. Theriogenology 2016, 86, 1541–1549. [Google Scholar] [CrossRef]
- Nagashima, J.B.; Wildt, D.E.; Alexander, T.J.; Songsasen, N. Activin Promotes Growth and Antral Cavity Expansion in the Dog Ovarian Follicle. Theriogenology 2019, 15, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Kishi, H.; Kitahara, Y.; Imai, F.; Nakao, K.; Suwa, H. Expression of the gonadotropin receptors during follicular development. Reprod. Med. Biol. 2018, 17, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Concannon, P.W. Research challenges in endocrine aspects of canine ovarian cycles. Reprod. Dom. Anim. 2012, 47 (Suppl. S6), 6–12. [Google Scholar] [CrossRef] [PubMed]
- Viswanathan, P.; Wood, M.A.; Walker, W.H. Follicle-stimulating hormone (FSH) transiently blocks FSH receptor transcription by increasing inhibitor of deoxyribonucleic acid binding/differentiation-2 and decreasing upstream stimulatory factor expression in rat Sertoli cells. Endocrinology 2009, 150, 3783–3791. [Google Scholar] [CrossRef] [PubMed]
- Imani, S.; Wu, R.C.; Fu, J. MicroRNA-34 family in breast cancer: From research to therapeutic potential. J. Cancer 2018, 9, 3765–3775. [Google Scholar] [CrossRef] [PubMed]
- Fabová, Z.; Loncová, B.; Bauer, M.; Sirotkin, A.V. Interrelationships Between miR-34a and FSH in the Control of Porcine Ovarian Cell Functions. Reprod. Sci. 2023, 30, 1789–1807. [Google Scholar] [CrossRef] [PubMed]
- Jefferson, W.N.; Couse, J.F.; Banks, E.P.; Korach, K.S.; Newbold, R.R. Expression of estrogen receptor beta is developmentally regulated in reproductive tissues of male and female mice. Biol. Reprod. 2000, 62, 310–317. [Google Scholar] [CrossRef]
- Drummond, A.E.; Fuller, P.J. The importance of ERbeta signalling in the ovary. J. Endocrinol. 2010, 205, 15–23. [Google Scholar] [CrossRef]
- Rumi, M.A.K.; Singh, P.; Roby, K.F.; Zhao, X.; Iqbal, K.; Ratri, A.; Lei, T.; Cui, W.; Borosha, S.; Dhakal, P.; et al. Defining the Role of Estrogen Receptor β in the Regulation of Female Fertility. Endocrinology 2017, 158, 2330–2343. [Google Scholar] [CrossRef] [PubMed]
- Bao, B.; Kumar, N.; Karp, R.M.; Garverick, H.A.; Sundaram, K. Estrogen receptor-beta expression in relation to the expression of luteinizing hormone receptor and cytochrome P450 enzymes in rat ovarian follicles. Biol. Reprod. 2000, 63, 1747–1755. [Google Scholar] [CrossRef]
- Wildt, D.E.; Panko, W.B.; Chakraborty, P.K.; Seager, S.W.J. Relationship of serum estrone, estradiol-17b and progesterone to LH, sexual behavior, and time of ovulation in the bitch. Biol. Reprod. 1979, 20, 648–658. [Google Scholar] [CrossRef] [PubMed]
- Pan, B.; Zhan, X.; Li, J. MicroRNA-574 Impacts Granulosa Cell Estradiol Production via Targeting TIMP3 and ERK1/2 Signaling Pathway. Front. Endocrinol. 2022, 13, 2127. [Google Scholar] [CrossRef] [PubMed]
- Søkilde, R.; Persson, H.; Ehinger, A.; Pirona, A.C.; Fernö, M.; Hegardt, C.; Larsson, C.; Loman, N.; Malmberg, M.; Rydén, L.; et al. Refinement of breast cancer molecular classification by miRNA expression profiles. BMC Genom. 2019, 20, 503. [Google Scholar] [CrossRef] [PubMed]
- Roush, S.; Slack, F.J. The let-7 family of microRNAs. Trends Cell Biol. 2008, 18, 505–516. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Shen, H.R.; Yu, M.; Du, M.R.; Li, X.L. MicroRNA let-7i inhibits granulosa-luteal cell proliferation and oestradiol biosynthesis by directly targeting IMP2. RBMO 2022, 44, 803–816. [Google Scholar] [CrossRef]
- Dai, T.; Kang, X.; Yang, C.; Mei, S.; Wei, S.; Guo, X.; Ma, Z.; Shi, Y.; Chu, Y.; Dan, X. Integrative Analysis of miRNA-mRNA in Ovarian Granulosa Cells Treated with Kisspeptin in Tan Sheep. Animals 2022, 12, 2989. [Google Scholar] [CrossRef]
- Zhang, X.D.; Zhang, Y.H.; Ling, Y.H.; Liu, Y.; Cao, H.G.; Yin, Z.-J.; Ding, J.P.; Zhang, X.R. Characterization and differential expression of microRNAs in the ovaries of pregnant and non-pregnant goats (Capra hircus). BMC Genom. 2013, 14, 157. Available online: http://www.biomedcentral.com/1471-2164/14/157 (accessed on 1 November 2023). [CrossRef]
- Sun, X.; Xu, C.; Tang, S.C.; Wang, J.; Wang, H.; Wang, P.; Du, N.; Qin, S.; Li, G.; Xu, S.; et al. Let-7c blocks estrogen-activated Wnt signaling in induction of self-renewal of breast cancer stem cells. Cancer Gene Ther. 2016, 23, 83–89. [Google Scholar] [CrossRef]






| Target Gene | miRNA | Primer |
|---|---|---|
| ESR2 | cfa-miR-8881 | UUUGUUUUCUCUGGUUCUGUACC |
| cfa-miR-8837 | UUCUUGCUGGAGUCCGGUUGUCU | |
| cfa-let-7c | UGAGGUAGUAGGUUGUAUGGUU *** | |
| FSH-R | cfa-miR-8900 | UAGGACUUUAAUGGCUGGAGAGA |
| cfa-miR-34c | AGGCAGUGUAGUUAGCUGAUUGC | |
| cfa-miR-34a | UGGCAGUGUCUUAGCUGGUUGU. *** | |
| ref miRNAs | cfa-miR-16 | 5′-UAGCAGCACGUAAAUAUUGGCG-3′ |
| ref miRNAs | cfa-miR-26 | 5′-UUCAAGUAAUCCAGGAUAGGCU-3′ |
| Gene | Sequence 5′-3′ | Accession Number | Amplicon | Tm °C | Efficence |
|---|---|---|---|---|---|
| ACTB | F:ATTGTCATGGACTCTGGGGATG | AF021873.2 | 191 bp | 56.7 | 1.99 |
| R:TCCTTGATGTCACGCACGAT | |||||
| H2A | F:AGTACCTGACGGCCGAGAT | XM545419.4 | 245 bp | 59.6 | 1.97 |
| R:AGGGCAAATCAATCCAGAGA | |||||
| ESR2 | F: TTCTATAGCCCTGCTGTGATGAAT | AF389885.1 | 204 bp | 60.0 | 2.01 |
| R: ATTATGTCCTTGAATGCTTCTTT | |||||
| FSH-R | F:AACTCATTTGGCCATCCTTG | NC051814.1 | 212 bp | 60.0 | 1.98 |
| R:TGACTGCACCTTAGGCAGTG |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De los Reyes, M.; Dettleff, P.; Palomino, J.; Peralta, O.A.; Vergara, A. Dynamic Expression of Follicle-Stimulating Hormone and Estrogen mRNA Receptors Associated with microRNAs 34a and -let-7c in Canine Follicles during the Estrous Cycle. Animals 2024, 14, 214. https://doi.org/10.3390/ani14020214
De los Reyes M, Dettleff P, Palomino J, Peralta OA, Vergara A. Dynamic Expression of Follicle-Stimulating Hormone and Estrogen mRNA Receptors Associated with microRNAs 34a and -let-7c in Canine Follicles during the Estrous Cycle. Animals. 2024; 14(2):214. https://doi.org/10.3390/ani14020214
Chicago/Turabian StyleDe los Reyes, Monica, Phillip Dettleff, Jaime Palomino, Oscar A. Peralta, and Ana Vergara. 2024. "Dynamic Expression of Follicle-Stimulating Hormone and Estrogen mRNA Receptors Associated with microRNAs 34a and -let-7c in Canine Follicles during the Estrous Cycle" Animals 14, no. 2: 214. https://doi.org/10.3390/ani14020214