- 1Center for Advancing Population Science (CAPS), Medical College of Wisconsin, Milwaukee, WI, United States
- 2Division of General Internal Medicine, Department of Medicine, Froedtert & The Medical College of Wisconsin, Milwaukee, WI, United States
Objectives: To assess sex and racial/ethnic differences in the relationship between multiple cardiovascular disease (CVD) risk factors and mortality among a nationally representative sample of adults with diabetes.
Methods: Data were analyzed from 3,503 adults with diabetes from the National Health and Nutrition Examination Survey 2001–2010 and its linked mortality data through 31 December 2011. The outcome was mortality; the independent variables were sex and race/ethnicity. Covariates included demographics, comorbidity, and lifestyle variables. Cox proportional hazards regression was used to test associations between mortality and CVD risk factors.
Results: In adjusted analyses, the association between diastolic blood pressure and mortality was significantly different by sex and race/ethnicity (unadjusted p = 0.009; adjusted p = 0.042). Kaplan-Meier survival curves showed Hispanic women had the highest survival compared to Hispanic men and Non-Hispanic Black (NHB) and Non-Hispanic White (NHW) men and women; NHW men had the lowest survival probability.
Conclusion: In this nationally representative sample, stratified analyses showed women had higher survival rates compared to men within each race/ethnicity group, and Hispanic women had the highest survival compared to all other groups.
Introduction
More than 34 million Americans have diabetes, which represents 10.5% of the US population (1). Of all diabetes cases, 90–95% are classified as being type 2 diabetes mellitus (T2DM) (1). The national prevalence of diabetes has been on the rise for decades, and the number of adults with the disease is projected to increase to 60.6 million, or 17.9% by 2060, with the highest prevalence existing among minorities (2, 3). The prevalence of diabetes by sex differs by race and ethnicity with American Indian/Alaska Native (AI/AN) and Non-Hispanic Black (NHB) women having a higher prevalence of diabetes compared to AI/AN and NHB men, respectively (1). Hispanic, Non-Hispanic Asian, and Non-Hispanic White (NHW) men have a higher prevalence of diabetes compared to women of the same race and ethnicity.
Sex and racial/ethnic differences among individuals with T2DM may contribute to disparity trends observed in mortality (4–7). Evidence suggests women with T2DM have less favorable CVD risk factor profiles compared to men, and fewer women achieve target levels for hemoglobin A1c (HbA1c), low-density lipoprotein cholesterol (LDL-C), and systolic blood pressure (SBP) (4, 8–10). While men with T2DM have a higher absolute risk of mortality (2, 11), the increased risk factor burden observed in women with diabetes is thought to contribute to a significantly increased relative risk of CVD and mortality (9, 13, 14). In women with diabetes, the cardioprotective effect of the female sex is attenuated (15, 16).
Similarly, compared to NHWs, racial/ethnic minorities have poorer control of CVD risk factors (6, 7, 17). While there has been an overall increase in CVD risk factor control between 2001–2009, NHBs display less control of HbA1c, BP, LDL-C, and composite control of all three factors compared to NHWs (7). Furthermore, national data indicate that NHBs and Hispanics are 2.3 and 1.5 times more likely to die, respectively, from poorly controlled T2DM compared to NHWs (18). However, while national mortality rates among racial/ethnic minorities with diabetes are higher compared to NHWs, many studies have shown a “reverse disparity” in the relationship between race/ethnicity and mortality where NHWs display a higher mortality risk (19, 20) Therefore, the aim of this study is to assess sex and racial/ethnic differences in the relationship between multiple CVD risk factors and mortality among a nationally representative sample of adults with diabetes.
Methods
This was a cohort study that analyzed 2001–2010 data from the National Health and Nutrition Examination Survey (NHANES) and its linked mortality data through 31 December 2011. NHANES is a survey program that combines interviews and physical examinations from a nationally representative sample of adults and children to assess the health and nutritional status of the United States. We investigated disparities in mortality by race/ethnicity, sex, and the influence of key modifiable risk factors among persons with diabetes.
Study Population
The study population included men and women aged 20 years and older, who completed both the survey interview and Mobile Exam Center (MEC) examination and had mortality follow-up information. In total, 26,269 participants were selected. Among them, 3,664 participants were identified as having diabetes; we excluded 161 other minorities and 3,503 were included in the analyses.
Diabetes Classification
Participants with diabetes were defined based on their responses to diabetes-related questions and their measured HbA1c. Participants were considered to have diabetes if they answered “yes” to any of the following three questions: “Have you ever been told by a doctor or other health professional that you have diabetes or sugar diabetes?”; “Are you now taking insulin?”; or “Are you now taking diabetic pills to lower your blood sugar?”; or if they answered “no” to all three questions, but had a measured HbA1c≥6.5%.
Mortality Outcome
The survey data were linked to the most recently available mortality data, the public-use 2011 Linked Mortality File. All survey participants were followed from interview date through to 31 December 2011. Mortality outcome of interest in these analyses included all-cause mortality.
Cardiovascular Disease Risk Factors
Traditional CVD risk factors including LDL-C, HbA1c, SBP, diastolic blood pressure (DBP), and body mass index (BMI) were assessed in this study. BMI was classified as normal weight (<25 kg/m2), overweight (25–29 kg/m2), obese (30–39 kg/m2), and morbidly obese (40+ kg/m2). SBP was defined as normal blood pressure (<120 mmHg), prehypertension (120–139 mmHg), stage 1 hypertension (140–159 mmHg), and stage 2 hypertension (≥160 mmHg). DBP was defined and categorized as normal blood pressure (<80 mmHg), prehypertension (80–89 mmHg), stage 1 hypertension (90–99 mmHg), and stage 2 hypertension (≥100 mmHg). LDL-C was defined and classified as normal (<130 mg/dl), borderline (130–159 mg/dl), and high (≥160 mg/dl). HbA1c was categorized into <6.5%; 6.5–6.9%; 7.0–7.9%; and ≥8.0%.
Covariates
Covariates included demographics, comorbidity, and lifestyle variables. Demographic variables included age and ratio of family income to poverty. Comorbidity was defined as count of the following diseases: congestive heart failure, coronary heart disease, angina, heart attack, stroke, and cancer. It ranged from 0 to 6. Lifestyle variables included physical activity and smoking status. Physical activity, based on the individual’s engagement in work and recreational activities, was categorized as vigorous/moderate and none. Smoking was grouped as never/former or current smoker.
Statistical Analysis
National Center for Health Statistics (NCHS) recommendations were followed in the analyses to account for the complex survey design. Statistical Analysis System (SAS) procedures for survey sampling were used to calculate correct standard errors (SEs) and p-values. To correct unequal probability sampling bias and nonresponse bias, MEC exam weights were used to represent the US population for BMI, SBP, DBP, and HbA1c outcomes; fasting weights were used for the LDL-C outcome. Survey Cox proportional hazards regression models were used to calculate mortality. All statistical analyses were performed with SAS version 9.4 (SAS Institute).
Cox proportional hazards regression analysis was used to test the association between CVD risk factor and mortality stratified by sex and race and ethnicity for individuals with diabetes. Five CVD risk factors were explored separately. First, each CVD risk factor was treated as continuous; univariate and multivariable Cox regression was modelled for each sex and race interaction. Multivariable models were adjusted for demographics (age, ratio of family income to poverty as continuous), comorbidity (continuous), and lifestyle variables [physical activity (none vs. vigorous/ moderate) and smoking status (current smoker vs. former smoker/none smoker)]. Second, these models were also tested by treating CVD risk as categorical variable.
Results
The weighted sample population characteristics for adults with diabetes are presented in Table 1 by sex and race/ethnicity. A total of 3,503 participants (representing 19,434,189 US non-institutionalized residents) over the age of 20 years had diagnosed or undiagnosed diabetes and had mortality data available through 2010. Approximately 50.2% were females. While the majority of the population was NHW (66.4%), 18.1% were NHB, and 15.5% were Hispanic. Approximately 45.4% of the sample was between the age of 45–64 years, where the average age was 59 years old. Approximately 55.4% had at least a high school education. Approximately 42.2% were not married, and 23.3% earned below the poverty level based on 130% or less ratio of family income to the poverty line. Approximately 35.7% of the sample had 1 or more comorbidities, where 50.5% reported no physical activity and 53.5% were current or former smokers.
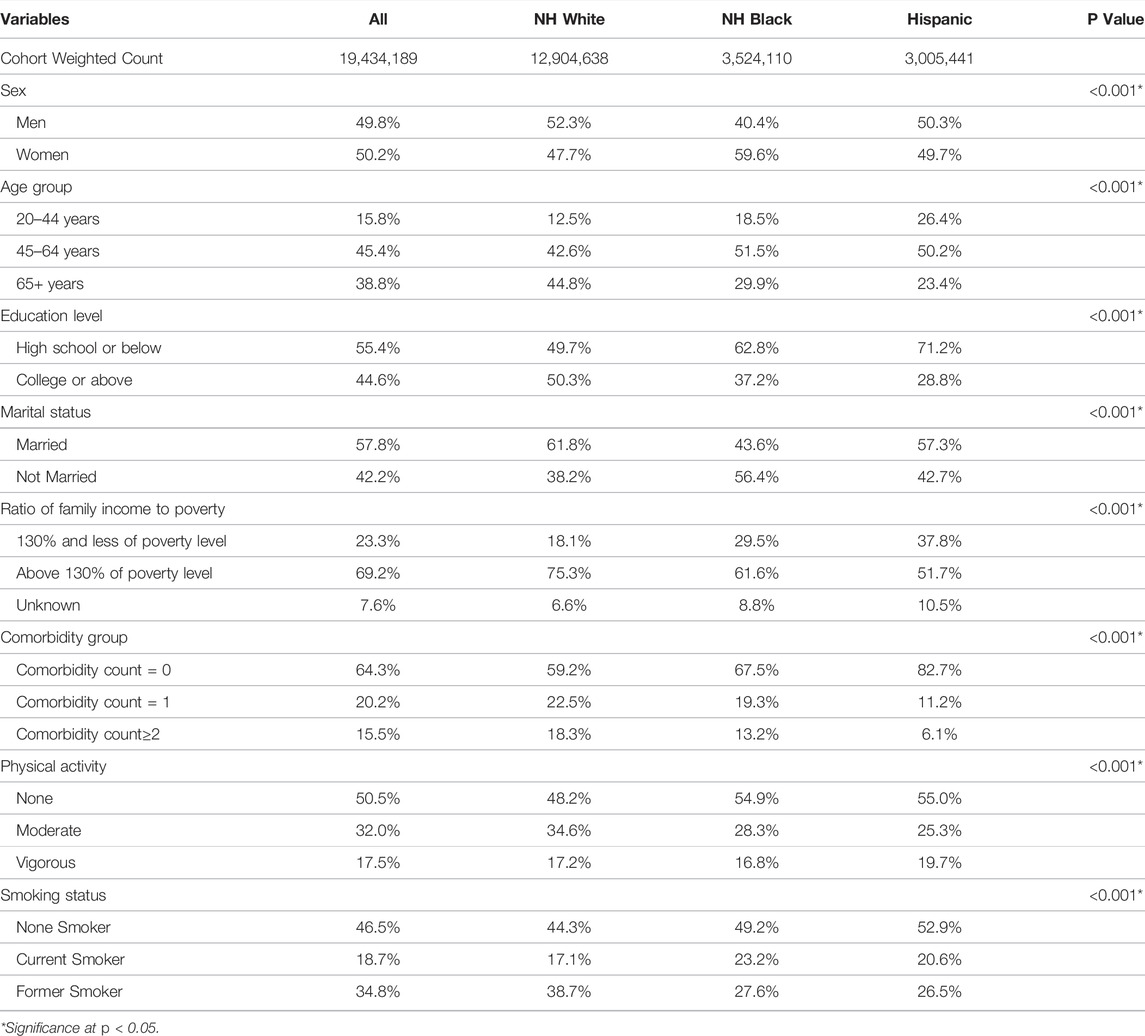
TABLE 1. Weighted Sample Characteristics for Adults with Diabetes (sample n = 3,503). (National Health and Nutrition Examination Survey, United States, 2001-2010).
Table 2 shows the mean values of CVD risk factors for adults with diabetes by sex and race/ethnicity. NHB women had highest mean BMI (35.5 ± 0.5), and Hispanic men had lowest (30.6 ± 0.4) (p < 0.001). NHB women had highest mean SBP (134.5 ± 1.1%), and NHW men had lowest mean SBP (127.8 ± 0.9) (p < 0.001). NHB and Hispanic men had the highest mean DBP (73.3 ± 1.1 and 73.4 ± 0.8, respectively), and NHW women had the lowest (64.8 ± 0.7) (p < 0.001). NHB men had highest mean LDL-C (119.0 ± 3.7), and NHW women had the lowest (109.9 ± 2.6) (p < 0.001). Hispanic men had the highest mean HbA1c at 8.0%, and NHW women had the lowest at 6.9% (p < 0.001).
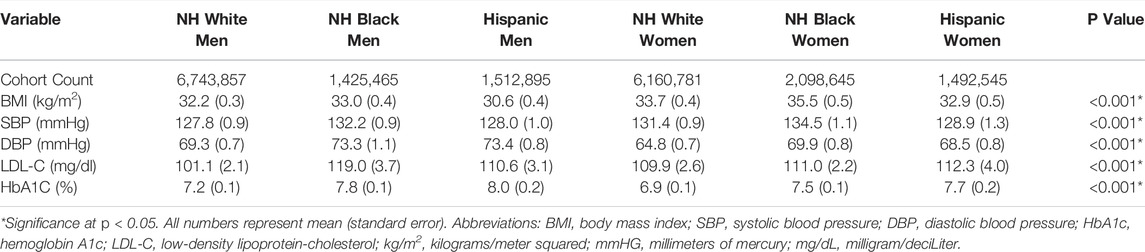
TABLE 2. Mean values of cardiovascular disease risk factors for adults with diabetes stratified by race/ethnicity and sex. (National Health and Nutrition Examination Survey, United States, 2001-2010).
Table 3 shows the unadjusted results of the survey Cox proportional hazard models for the relationship between CVD risk factors and mortality stratified by race/ethnicity and sex in adults with diabetes. BMI was significantly associated with lower mortality in Hispanic men (HR = 0.87, 95% CI 0.78–0.98). SBP was significantly associated with a higher risk of mortality in Hispanic men (HR = 1.02, 95% CI 1.01–1.04), NHW women (HR = 1.01, 95% CI 1.01–1.02), NHB women (HR = 1.02, 95% CI 1.01–1.03), and Hispanic women (HR = 1.02, 95% CI 1.01–1.03). DBP was significantly associated with lower mortality in NHW men (HR = 0.97, 95% CI 0.96–0.98) and NHW women (HR = 0.98, 95% CI 0.97–0.99). HbA1c was significantly associated with lower mortality in NHB women (HR = 0.82, 95% CI 0.68–0.99). LDL-c was not associated with mortality by race/ethnicity or sex in adults with diabetes in the unadjusted models.
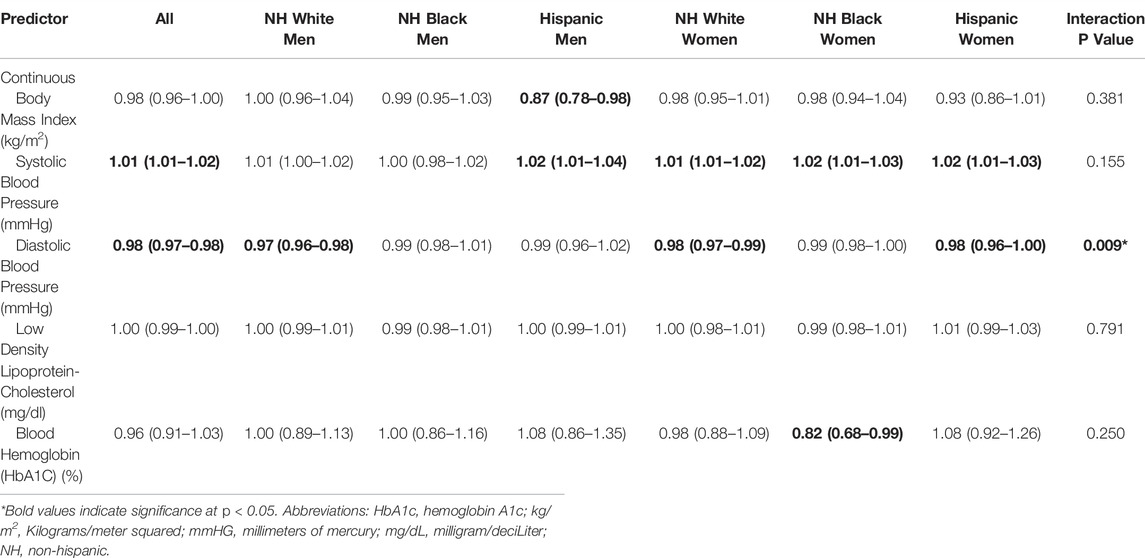
TABLE 3. Unadjusted cox proportion hazard models for cardiovascular disease risk factors and mortality stratified by race/ethnicity and sex for adults with diabetes. (National Health and Nutrition Examination Survey, United States, 2001-2010).
Table 4 shows the adjusted results of the survey Cox proportional hazard models for the relationship between CVD risk factors and mortality stratified by race/ethnicity and sex in adults with diabetes. BMI was significantly associated with lower mortality in Hispanic men (HR = 0.87, 95% CI 0.79–0.96). SBP was significantly associated with a higher risk of mortality in Hispanic men (HR = 1.02, 95% CI 1.01–1.03). DBP was significantly associated with lower mortality in NHW men (HR = 0.97, 95% CI 0.96–0.98). HbA1c and LDL-C were not associated with mortality by race/ethnicity or sex in adults with diabetes after adjusting for relevant covariates.
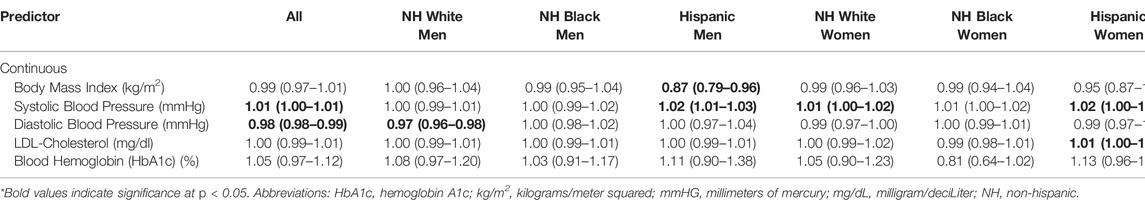
TABLE 4. Adjusted cox proportion hazard models for cardiovascular disease risk factors and mortality stratified by race/ethnicity and sex for adults with diabetes. (National Health and Nutrition Examination Survey, United States, 2001-2010).
Adjusted survival curves of adult diabetes population are shown in Figure 1. Hispanic women with diabetes had the highest survival, and NHW men with diabetes had the lowest survival (NHW men compared with Hispanic women p = 0.001).
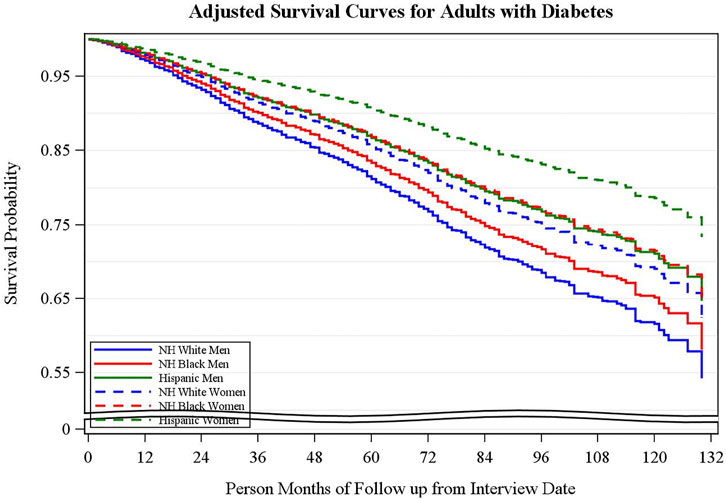
FIGURE 1. Survival curves for adults with diabetes stratified by race/ethnicity and sex. Adjusted survival curves using the corrected group prognosis method adjusted by age, PIR, comorbidity, smoking status, physical activity. (National Health and Nutrition Examination Survey, United States, 2001-2010).
Discussion
In this sample of adults with diabetes, a significant relationship was found between CVD risk factors and mortality stratified by sex and race/ethnicity, adjusting for relevant confounding factors. In unadjusted Cox Proportion Hazard regression analyses, DBP was significantly associated with a lower risk of mortality in both NHW men and women and Hispanic women. However, after adjusting for relevant covariates, the relationship between mortality and CVD risk factors for NHW and Hispanic women no longer persisted; the relationship remained significant only for NHW men. In addition, adjusted survival curves demonstrated Hispanic women to have the highest survival probability compared to all other racial/ethnic groups; NHW men had the lowest survival probability. There were no statistically significant race/ethnicity and sex interactions for relationship between HbA1c, SBP, LDL-C or body mass index (BMI) and mortality. These findings suggest DBP control should be a goal for management in adults with diabetes, especially among NHW men, to decrease the risk of mortality. Additionally, research is needed to understand the factors associated with higher survival probability in Hispanic women.
Our findings are supported by evidence from previous studies evaluating the relationship between CVD risk factors and mortality. Our study found a significant relationship between DBP and mortality, such that DBP was associated with lower mortality risk. Our findings are supported by Vamos et al., who indicated that in some cases, patients with T2DM and uncontrolled DBP had lower risk of mortality (21). Specifically, they found that in patients with T2DM and CVD, an uncontrolled DBP of 85–89 mmHg was associated with a lower mortality risk (21). Previous studies have reported an increased mortality risk with elevated SBP and DBP in patients with diabetes (22, 23). In their study of NHB and NHW patients with T2DM, Li et al. found that DBP ≥100 mmHg was associated with an increased risk of mortality among both NHB and NHW men and women with diabetes (23). However, the authors also reported that the lowest risk of mortality was associated with a DBP of 80–90 mmHg (23). Similarly, Kontopantelis et al. reported that in patients with T2DM, the lowest risk of mortality was associated with a DBP of 82.5–87.5 mmHg (24). The association between DBP and lower mortality risk found in our study for NHW men suggests more NHW men have a DBP that is in the hypertensive, yet potentially protective range.
Additionally, the results of our study indicated that Hispanic women had the highest survival compared to NHB and NHW racial groups, which could be explained by the “Hispanic paradox,” or the observation that in the US, the mortality rates for Hispanics remain below NHWs despite lower socioeconomic status (SES), worse disease profiles, and increased risk and prevalence for some diseases (25, 26). Explanations for this phenomenon include low smoking prevalence, protective sociocultural practices (e.g., dietary practices, social support, family cohesion, etc.), and the selective migration of immigrants with significant health issues back to their home countries (26, 27). Another reason for this advantage is a mortality rate that is two-thirds that of NHWs for the leading causes of death—heart disease, cancer, and lung disease—among Hispanics (25). Finally, we also observed that women had higher survival rates compared to men in every race/ethnicity category. This finding is supported by other studies that found higher mortality rates and mortality risk in men with diabetes compared to women with diabetes (11, 12, 28). For example, using nationally representative data, Gregg et al. investigated trends in death rates among adults with and without diabetes between 1997 and 2006. Overall, they found that men with diabetes had higher mortality rates compared to women with diabetes (28).
Evidence suggests controlling modifiable cardiovascular disease (CVD) risk factors that include diabetes, hypertension, dyslipidemia, and obesity reduce morbidity and mortality in patients with T2DM (29–31). Maintaining target levels for CVD risk factors among patients with diabetes is an important standard of care given the significant negative health outcomes associated with uncontrolled risk factors such as the development of microvascular and macrovascular complications and mortality (32). In addition, there is evidence that diabetes confers an independent risk for the development of atherosclerotic CVD, which includes coronary heart disease, cerebrovascular disease, and peripheral arterial disease of atherosclerotic origin (33–35). In the US, improved risk factor control has been accompanied by significant improvements in mortality among individuals with diabetes (36). However, despite these improvements, individuals with diabetes still have increased risk of CVD and mortality compared to individuals without the disease (11, 37). Findings from this study provide additional information for targeted interventions to address sex and racial/ethnic disparities and reduce mortality among adults with T2DM.
There are study limitations that should be mentioned. First, in using cross-sectional data, we were unable to determine causality. Second, there are potential confounders not accounted for in the analyses including acculturation, length of diabetes duration, diabetes knowledge, and self-management practices. These factors may have influenced the findings; however, we are not able to substantiate their impact. Third, the sample size for some of the minority racial/ethnic groups was limited and smaller in comparison to the majority group. Finally, given the structure of the national dataset, we were unable to distinguish between T2DM and other types of diabetes including Type 1 Diabetes. Although 95% of adults with diabetes have T2DM, we recognize that individuals younger than 30 years, especially those being treated with insulin, may have Type 1 Diabetes. We were not able to distinguish those individuals from adults with T2DM, so this may have impacted the results.
Conclusion
The results of our study are important because they provide new information about the relationship between CVD risk factors and mortality by sex and race/ethnicity. In this nationally representative sample, significant associations were found in this relationship: DBP was associated with lower mortality risk in NHW men, and Hispanic women had the highest survival probability, after adjusting for relevant confounders. These results suggest the need for increased investigation and targeting of specific CVD risk factors, clinically, that influence mortality risk in men and women with diabetes across racial and ethnic groups. More studies are needed to determine the mechanisms driving the association between DBP and mortality in NHW men. Finally, additional research is needed to understand the underlying mechanisms associated with increased survival probability in Hispanic women with diabetes.
Data Availability Statement
The dataset generated and analyzed during the current study is publicly available at https://meps.ahrq.gov/data_stats/download_data_files.jsp.
Ethics Statement
The studies involving human participants were reviewed and approved by NCHS Research Ethics Review Board (ERB). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
KS, JW, and LE designed the study. EG acquired and analyzed the data. EG and LE developed the analyses, and KS, JW, EG, and LE interpreted the data. KS, EG, JW, and LE critically revised the manuscript for important intellectual content. All authors approved the final manuscript.
Funding
This study is partially supported by the National Institute of Diabetes and Digestive and Kidney Diseases K24DK093699, R01DK118038, and R01DK120861 (PI: LEE) and R21DK123720 (PI: JSW).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.Centers for Disease Control and Prevention. National Diabetes Statistics Report. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services (2020).
2.International Diabetes Federation. IDF Diabetes Atlas. 8th ed. Brussels, Belgium: International Diabetes Federation (2017). Available at: http://www.diabetesatlas.org.
3. Menke, A, Casagrande, S, Geiss, L, and Cowie, CC. Prevalence of and Trends in Diabetes Among Adults in the United States, 1988-2012. JAMA (2015) 314(10):1021–9. doi:10.1001/jama.2015.10029
4. Šekerija, M, Poljicanin, T, Erjavec, K, Liberati-Cizmek, AM, Prašek, M, and Metelko, Z. Gender Differences in the Control of Cardiovascular Risk Factors in Patients with Type 2 Diabetes -A Cross-Sectional Study. Intern Med (2012) 51(2):161–6. doi:10.2169/internalmedicine.51.6094
5. Hunt, KJ, Gebregziabher, M, Lynch, CP, Echols, C, Mauldin, PD, and Egede, LE. Impact of Diabetes Control on Mortality by Race in a National Cohort of Veterans. Ann Epidemiol (2013) 23(2):74–9. doi:10.1016/j.annepidem.2012.11.002
6. Holland, AT, Zhao, B, Wong, EC, Choi, SE, Wong, ND, and Palaniappan, LP. Racial/ethnic Differences in Control of Cardiovascular Risk Factors Among Type 2 Diabetes Patients in an Insured, Ambulatory Care Population. J Diabetes Its Complications (2013) 27(1):34–40. doi:10.1016/j.jdiacomp.2012.08.006
7. Wang, Y, Katzmarzyk, PT, Horswell, R, Zhao, W, Li, W, Johnson, J, et al. Racial Disparities in Cardiovascular Risk Factor Control in an Underinsured Population with Type 2 Diabetes. Diabet Med (2014) 31(10):1230–6. doi:10.1111/dme.12470
8. Penno, G, Solini, A, Bonora, E, Fondelli, C, Orsi, E, Zerbini, G, et al. Gender Differences in Cardiovascular Disease Risk Factors, Treatments and Complications in Patients with Type 2 Diabetes: the RIACE Italian Multicentre Study. J Intern Med (2013) 274(2):176–91. doi:10.1111/joim.12073
9. Juutilainen, A, Kortelainen, S, Lehto, S, Rönnemaa, T, Pyörälä, K, and Laakso, M. Gender Difference in the Impact of Type 2 Diabetes on Coronary Heart Disease Risk. Diabetes Care (2004) 27(12):2898–904. doi:10.2337/diacare.27.12.2898
10. Strom Williams, JL, Lynch, CP, Winchester, R, Thomas, L, Keith, B, and Egede, LE. Gender Differences in Composite Control of Cardiovascular Risk Factors Among Patients with Type 2 Diabetes. Diabetes Techn Ther (2014) 16(7):421–7. doi:10.1089/dia.2013.0329
11. Preis, SR, Hwang, S-J, Coady, S, Pencina, MJ, D'Agostino, RB, Savage, PJ, et al. Trends in All-Cause and Cardiovascular Disease Mortality Among Women and Men with and without Diabetes Mellitus in the Framingham Heart Study, 1950 to 2005. Circulation (2009) 119(13):1728–35. doi:10.1161/circulationaha.108.829176
12. Taylor, KS, Heneghan, CJ, Farmer, AJ, Fuller, AM, Adler, AI, Aronson, JK, et al. All-Cause and Cardiovascular Mortality in Middle-Aged People with Type 2 Diabetes Compared with People without Diabetes in a Large U.K. Primary Care Database. Diabetes Care (2013) 36(8):2366–71. doi:10.2337/dc12-1513
13. Huxley, R, Barzi, F, and Woodward, M. Excess Risk of Fatal Coronary Heart Disease Associated with Diabetes in Men and Women: Meta-Analysis of 37 Prospective Cohort Studies. BMJ (2006) 332:73–8. doi:10.1136/bmj.38678.389583.7C
14. Peters, SAE, and Woodward, M. Sex Differences in the Burden and Complications of Diabetes. Curr Diab Rep (2018) 18(6):33. doi:10.1007/s11892-018-1005-5
15. Sattar, N. Gender Aspects in Type 2 Diabetes Mellitus and Cardiometabolic Risk. Best Pract Res Clin Endocrinol Metab (2013) 27(4):501–7. doi:10.1016/j.beem.2013.05.006
16. Wannamethee, SG, Papacosta, O, Lawlor, DA, Whincup, PH, Lowe, GD, Ebrahim, S, et al. Do women Exhibit Greater Differences in Established and Novel Risk Factors between Diabetes and Non-diabetes Than Men? the British Regional Heart Study and British Women's Heart Health Study. Diabetologia (2012) 55(1):80–7. doi:10.1007/s00125-011-2284-4
17. McWilliams, JM, Meara, E, Zaslavsky, AM, and Ayanian, JZ. Differences in Control of Cardiovascular Disease and Diabetes by Race, Ethnicity, and Education: U.S. Trends from 1999 to 2006 and Effects of Medicare Coverage. Ann Intern Med (2009) 150(8):505–15. doi:10.7326/0003-4819-150-8-200904210-00005
18. Spanakis, EK, and Golden, SH. Race/Ethnic Difference in Diabetes and Diabetic Complications. Curr Diab Rep (2013) 13(6):814–23. doi:10.1007/s11892-013-0421-9
19. Conway, BN, May, ME, and Blot, WJ. Mortality Among Low-Income African Americans and Whites with Diabetes. Diabetes Care (2012) 35:2293–9. doi:10.2337/dc11-2495
20. McEwen, LN, Karter, AJ, Waitzfelder, BE, Crosson, JC, Marrero, DG, Mangione, CM, et al. Predictors of Mortality over 8 Years in Type 2 Diabetic Patients: Translating Research into Action for Diabetes (TRIAD). Diabetes Care (2012) 35(6):1301–9. doi:10.2337/dc11-2281
21.UK Prospective Diabetes Study Group. Tight Blood Pressure Control and Risk of Macrovascular and Microvascular Complications in Type 2 Diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ (1998) 317(7160):703–13.
22. Li, W, Katzmarzyk, PT, Horswell, R, Wang, Y, Johnson, J, and Hu, G. Blood Pressure and All-Cause Mortality Among Patients with Type 2 Diabetes. Int J Cardiol (2016) 206:116–21. doi:10.1016/j.ijcard.2016.01.009
23. Kontopantelis, E, Springate, DA, Reeves, D, Ashcroft, DM, Rutter, M, Buchan, I, et al. Glucose, Blood Pressure and Cholesterol Levels and Their Relationships to Clinical Outcomes in Type 2 Diabetes: a Retrospective Cohort Study. Diabetologia (2015) 58(3):505–18. doi:10.1007/s00125-014-3473-8
24. Vamos, EP, Harris, M, Millett, C, Pape, UJ, Khunti, K, Curcin, V, et al. Association of Systolic and Diastolic Blood Pressure and All Cause Mortality in People with Newly Diagnosed Type 2 Diabetes: Retrospective Cohort Study. BMJ (2012) 345:e5567. doi:10.1136/bmj.e5567
25. McDonald, JA, and Paulozzi, LJ. Parsing the Paradox: Hispanic Mortality in the US by Detailed Cause of Death. J Immigrant Minor Health (2018) 1–9:237. doi:10.1007/s10903-018-0737-2
26. Fenelon, A, and Blue, L. Widening Life Expectancy Advantage of Hispanics in the United States: 1990-2010. J Immigrant Minor Health (2015) 17(4):1130–7. doi:10.1007/s10903-014-0043-6
27. Markides, KS, and Eschbach, K. Aging, Migration, and Mortality: Current Status of Research on the Hispanic Paradox. The Journals Gerontol Ser B (2005) 6060:S68–S75. doi:10.1093/geronb/60.special_issue_2.s68
28. Gregg, EW, Cheng, YJ, Saydah, S, Cowie, C, Garfield, S, Geiss, L, et al. Trends in Death Rates Among U.S. Adults with and without Diabetes between 1997 and 2006. Diabetes Care (2012) 35(6):1252–7. doi:10.2337/dc11-1162
29. Chamberlain, JJ, Johnson, EL, Leal, S, Rhinehart, AS, Shubrook, JH, and Peterson, L. Cardiovascular Disease and Risk Management: Review of the American Diabetes Association Standards of Medical Care in Diabetes 2018. Ann Intern Med (2018) 168:640–50. doi:10.7326/M18-0222
30. Gaede, P, Lund-Andersen, H, Parving, HH, and Pedersen, O. Effect of a Multifactorial Intervention on Mortality in Type 2 Diabetes. N Engl J Med (2008) 358:580–91. doi:10.1056/NEJMoa0706245
31. Cavero-Redondo, I, Peleteiro, B, Álvarez-Bueno, C, Rodriguez-Artalejo, F, and Martínez-Vizcaíno, V. Glycated Haemoglobin A1c as a Risk Factor of Cardiovascular Outcomes and All-Cause Mortality in Diabetic and Non-diabetic Populations: a Systematic Review and Meta-Analysis. BMJ Open (2017) 7(7):e015949. doi:10.1136/bmjopen-2017-015949
32.American Diabetes Association. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes-2018. Diabetes Care (2018) 41(Suppl. 1):S86. doi:10.2337/dc18-S009
33. Wei, M, Gaskill, SP, Haffner, SM, and Stern, MP. Effects of Diabetes and Level of Glycemia on All-Cause and Cardiovascular Mortality: The San Antonio Heart Study. Diabetes Care (1998) 21(7):1167–72. doi:10.2337/diacare.21.7.1167
34. Sarwar, N, Sarwar, N, Gao, P, Seshasai, SR, Gobin, R, Kaptoge, S, et al. Diabetes Mellitus, Fasting Blood Glucose Concentration, and Risk of Vascular Disease: a Collaborative Meta-Analysis of 102 Prospective Studies. Lancet (2010) 375:2215–22. doi:10.1016/S0140-6736(10)60484-9
35. Grundy, SM, Bilheimer, D, Chair, A, Clark, LT, Denke, M, Havel, RJ, et al. Summary of the Second Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel II). JAMA (1993) 269:3015–23.
36. Tsujimoto, T, Kajio, H, and Sugiyama, T. Favourable Changes in Mortality in People with Diabetes: US NHANES 1999-2010. Diabetes Obes Metab (2018) 20(1):85–93. doi:10.1111/dom.13039
Keywords: mortality, race, ethnicity, sex, diabetes, cardiovascular disease risk factors, adults
Citation: Savage K, Williams JS, Garacci E and Egede LE (2022) Association Between Cardiovascular Disease Risk Factors and Mortality in Adults With Diabetes: A Stratified Analysis by Sex, Race, and Ethnicity. Int J Public Health 67:1604472. doi: 10.3389/ijph.2022.1604472
Received: 17 September 2021; Accepted: 02 March 2022;
Published: 06 April 2022.
Edited by:
Salvatore Panico, University of Naples Federico II, ItalyReviewed by:
Maria Masulli, Federico II University Hospital, ItalyCopyright © 2022 Savage, Williams, Garacci and Egede. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Leonard E. Egede, legede@mcw.edu
 Kristina Savage1
Kristina Savage1 Joni S. Williams
Joni S. Williams Emma Garacci
Emma Garacci Leonard E. Egede
Leonard E. Egede