SARS-CoV-2 vertical transmission supports innate fetal protection: A narrative review
- 1Society for the Investigation of Early Pregnancy (SIEP), New York, NY, United States
- 2Associate Member Childbirth and Postpartum Haemorrhage Committee F.I.G.O., Geneva, Switzerland
- 3BioIncept LLC, New York, NY, United States
- 4Humanitas University Department of Biomedical Sciences, Humanitas University, Milan, Italy
- 5IRCCS Humanitas Research Hospital, Milan, Italy
- 6Institute of Biology and Immunology of Reproduction, Bulgarian Academy of Sciences, Sofia, Bulgaria
- 7Department of Woman and Child Health and Public Health, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy
Prenatal infections that have been exhaustively studied help frame the current Severe Acute Respiratory Syndrome related coronavirus-2 (SARS-CoV-2) pandemic, with the caveat that asymptomatic SARS-CoV-2 infected patients are not tested, while those symptomatic are delivered and/or treated with drug(s) available on-site. Thus, management and therapy are still heterogeneous. SARS-CoV-2 induced respiratory infection remains mostly local, unless severe, which lessens transplacental vertical transmission (VT). Vaccination prior to or during pregnancy significantly changes the prognosis for both the mother and newborn. The virus spread to the fetus can be binding to ACE2 and TMPRSS2 protein receptors. A recent study demonstrated ACE2 and TMPRSS2 fetal expression in the intestine from the second trimester. Most placental infections are subclinical unless severe villitis and apoptosis are observed. The placenta is rarely tested, and it is highly probable that most are positive for the virus, requiring sophisticated diagnostics to document. Other VT modalities, such as vaginal, rectal or through amniotic fluid contamination, are very rare. Therefore, vaginal delivery is preferable when clinically feasible. It has not yet been determined whether the placenta is a shield or if it transmits infection, while, on the other hand, recent data support fetal resilience, which is plausible due to the major difference between the placental and fetal rates of infection: only 3%–5% of documentable VT compared with up to 100% expected placental exposure to viremia. Newborn Polymerase Chain Reaction (PCR) from nasal swab is more practical as an option for VT diagnosis compared to ocular or anal swab, with low yield. The maternal infection leads to antiviral IgG production of 100% in severe cases, which is transferred to the fetus and breast milk. Postpartum-documenting VT is difficult since horizontal viral transmission may be common and minimized by mother/staff/family-preventive measures. Breastfeeding is safe and encouraged because, beyond nutrition, it promotes protective antibody transfer and maternal bonding. Lessons learned from other Betacorona viruses (SARS-CoV and Middle East Respiratory Syndrome related coronavirus [MERS-CoV]) virulence are relevant since mutations can increase or decrease vulnerability. Overall, data support fetal/newborn resilience against SARS-CoV-2 VT. However, viremia monitoring by sensitive tests and assessment for delayed sequelae shown in adults is necessary.
Introduction
In the last few decades, research has shown that viral infections are difficult to understand due to the intricate mechanisms underlying those infections compared to bacteria-induced diseases. These latter ones can be readily diagnosed by common laboratory tests and cultures and, often, easily treated by using targeted antibiotics. During pregnancy, patients are routinely screened for various infections caused by bacteria and viruses, such as syphilis, human immunodeficiency virus (HIV), Hepatitis B virus (HBV), Hepatitis C virus (HCV), Rubella virus (RV or RUBV), and Human Cytomegalovirus (HCMV or HuBHV5), Toxoplasma gondii, tuberculosis, and malaria, in endemic areas. Once diagnosed, effective countermeasures, including antibiotics, antivirals, and hyperimmune serum, can be administered to treat the infection. At the same time, the vaccine administration before or during pregnancy (namely those against diphtheria, pertussis, and tetanus (DPT) or against flu) protects the newborn, minimizing maternal–fetal transmission (1). Unfortunately, for other infections, like the Zika virus, a vaccine has not been developed yet, and therefore, the consequences of VT are severe, leading, among other things, to fetal microcephaly. As progress is continuously being made for Severe Acute Respiratory Syndrome-related coronavirus-2 [SARS-CoV-2] infection, vaccination continues to play a major role, especially when it is administered before conception (2).
Further, specific antiviral, monoclonal antibodies, convalescent plasma, and recently oral therapies were shown to be effective in the context of mild to severe disease, significantly decreasing morbidity and mortality in both pregnant and non-pregnant patients. These are very welcome additions since there have been more than 15 million deaths since the start of the pandemic and, not less relevant, in those who survived, long-haul symptoms developed frequently.
Aims of the review
In this narrative review, we summarize and present sources of infection and sites of detection of the SARS-CoV-2 from conception until delivery, a maternal infection that facilitates placental infection and potentially VT. We plan to critically examine true and documented VT compared to horizontal transmission; we also aim to describe the possible dual role as shield-or promoter of infection of the fetus of the placenta. We will delineate the mechanisms involved in innate fetal protection, anti-SARS-CoV-2 antibodies transferred to the fetus by the virus-infected mother, and their potential protective effects. We will also analyze and compare current epidemic mechanisms with those of two other severe coronaviruses previously studied.
SARS-CoV-2 diagnosis: Too late to stop the infection
Effective countermeasures against previously unidentified novel emerging viral infections remain an unmet need. The infection spreads quickly in the general population since they are asymptomatic and, therefore, the development of effective diagnostics is delayed (3). This is the case with HIV, which can be asymptomatic for a long time, but whose consequences are devastating unless readily treated. It took years to identify effective treatments and minimize the transfer of the virus by employing preventive measures. However, no effective vaccine has yet been developed against this virus (4). In other cases, precise diagnostic tests are available. However, every year a new vaccine must be developed and, among several reasons for this annual visit, one is the quick mutation of the virus—a case in point is influenza. A better understanding of various viral infection-induced diseases is important. Pregnancy exposure to pathogens, and specifically to viruses, can start at conception, up to delivery, and even postdelivery. Therefore, maternal–fetal transmission can be viewed as a continuum (5). Early exposure is critical for certain viral infections; in the case of measles, it is critical for disease development. In the case of maternal SARS-CoV-2 infection, the diagnosis is made in the respiratory tract by direct detection through RT-PCR of SARS-CoV-2 on an oropharyngeal swab. Currently, circulating viral titers detection remains a suboptimal diagnostic tool as viral load peaks during the prodromal phase of illness or at the time of symptom onset provide a rationale for the efficient spread of SARS-CoV-2 and may lead to an underestimate of the transplacental hematogenous spread. Antibody development following maternal respiratory infection is variable, while cellular memory response may prevail, but it is not used currently as a diagnostic tool.
Timeline and consequences of maternal exposure to SARS-CoV-2
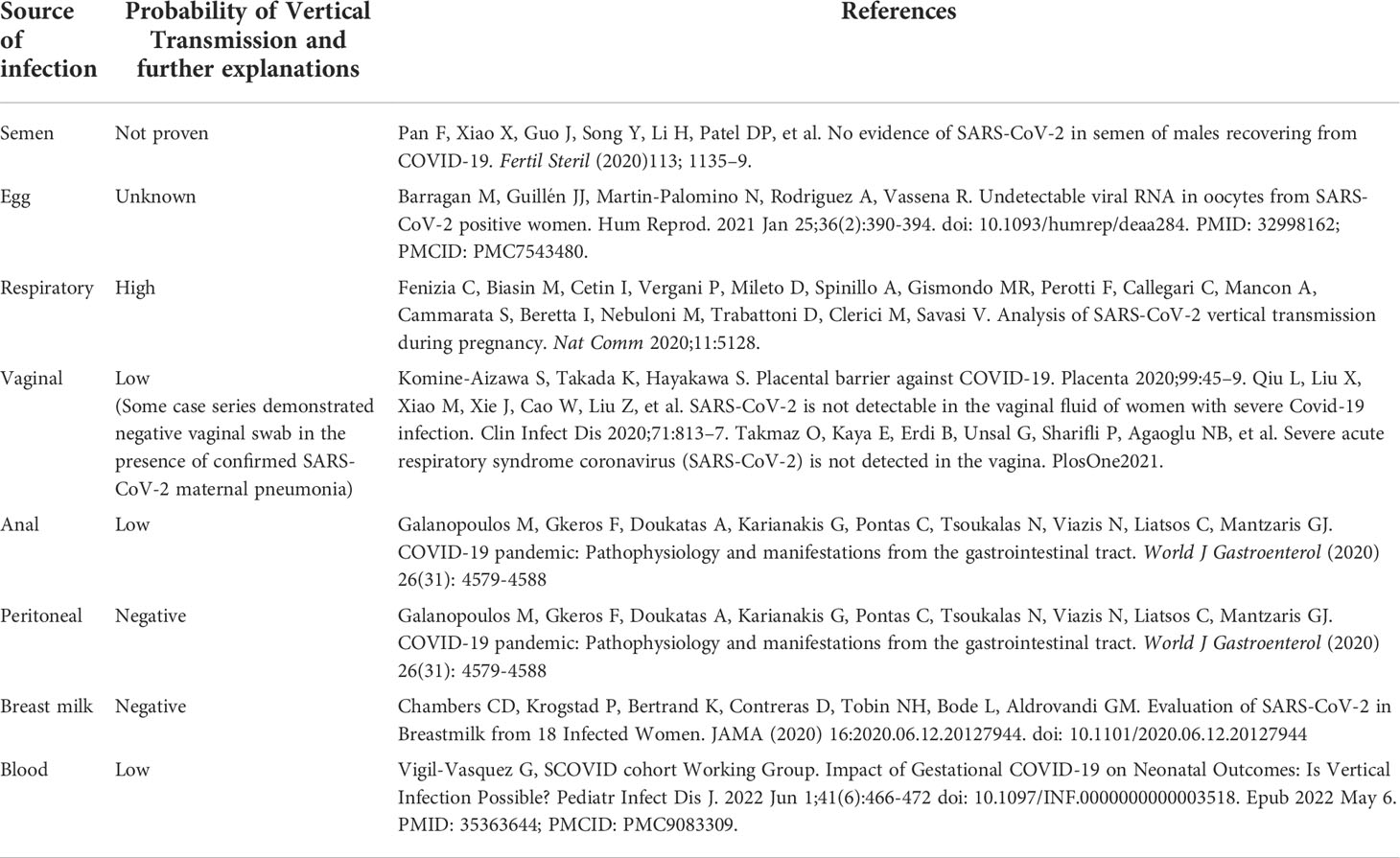
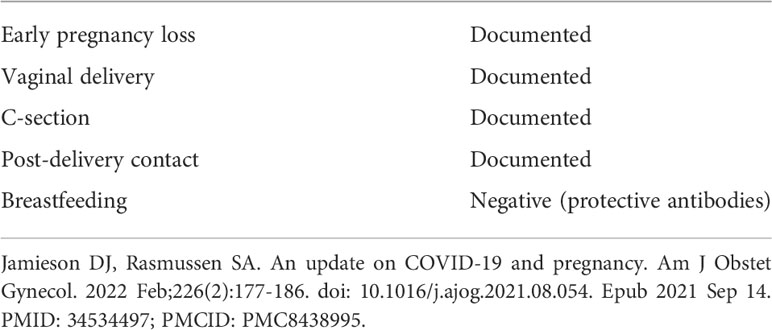
This novel virus has infected patients for more than the past 2 years. Therefore, detailed information can be gathered on the risk of infection from conception until delivery. The rate of maternal infection is similar to that of the general population, with a reproductive age of 20–44. Thus, unless underlying conditions are severe, maternal mortality is comparable in the age group to the general population. Table 1 shows the possible sources of infection. Among them, semen as a source of viral transmission was not documented (6). The correlation between SARS-CoV-2 infection, stillbirths, and miscarriages is still debated, as some authors have not found an increase in miscarriages among COVID-19 pregnant women (7–9), while others have found an increased incidence (10). Further, which is reassuring, anti-COVID19 vaccination is also safe and strongly advocated before and after conception. For VT to occur, both a susceptible host and a recipient are required; a possible definition of “susceptible recipient” is a placenta that may co-express high levels of the primary factors that facilitate SARS-CoV-2 entry into cells, such as angiotensin-converting enzyme 2 (ACE2) and transmembrane serine protease 2 (TMPRSS2) (11).
The maternal infection is usually mild, further minimizing VT. However, SARS-CoV-2 infection in pregnancy is associated with an increased risk of pregnancy complications, such as preeclampsia and preterm birth (12, 13). The infection is frequently asymptomatic—the patient is not seeking medical care and thereby not being tested. The mother must be exposed to a significant viral load to become infected since there is a threshold below which the infection will not develop-likely due to innate immune protection (13). A higher prevalence of detectable SARS-CoV-2 plasma viral load is associated with poorer respiratory disease severity (14). The S1 subunit of the spike protein is responsible for the receptor binding activity, while the S2 subunit houses the functional elements used for membrane fusion. The binding to the abundant ACE2 receptors and TMPRSS2 co-receptors expressed in the lung tissue is key for infecting the host. Once SARS-CoV-2 infects the host, the normal inflammatory response is functional in viral eradication and survival. However, the cytokine release is responsible for the onset of symptoms in the patient. The ensuing pneumonia ranges from mild to severe where bacterial superinfections can develop, followed, in some cases, by a cytokine storm (12). Maternal comorbidities increase the severity of infection (obesity and lung disease increase by more than 5-fold, cardiovascular disease by 4-fold, and diabetes by 2-fold). Moreover, due to infection, pregnancy-associated specific pathologies like severe pre-eclampsia rate increase 5-fold, stillbirth 4-fold, coagulation disorders, endothelial cell dysfunction, or complement activation, which further worsen and aggravate both maternal and fetal conditions (13). Furthermore, if the fetus has a congenital abnormality or intrauterine growth retardation, the infection will further increase the pre-existing morbidity and mortality. Whether VT occurs or not, the virus can severely affect the maternal–newborn dyad.
Mode of SARS-CoV-2 vertical transmission
Concerning sources of infection that can lead to VT, the hematogenous route from the mother through the placenta is the most plausible, despite the observed low rate of virus detection in the placenta, since most cases are not tested and tests made are not precise (15). Pregnancy events related to VT are summarized in Table 2. Another source of viral infection and transmission to the fetus is through the vaginal route, either ascending to the uterus, particularly with premature rupture of membranes, or occurring during delivery, however this is very rarely found. Also, contamination from the gastrointestinal tract is rare as well (16). This is documented using both polymerase chain reaction (PCR) based vaginal and anal swab testing. The virus detection in amniotic fluid and breast milk is also exceedingly rarely, and most importantly, although SARS-CoV-2 RNA was detected in the breast milk of infected women, the viral cultures for that breast milk were negative, suggesting that SARS-CoV-2 RNA found in breast milk does not represent a replication-competent virus (17).
This is highly reassuring considering the important role that breastfeeding provides regarding nutrition, protection against diseases, protective antibodies transfer including those against SARS-CoV-2 infection (18), and maternal–infant bonding. The virus can be detected in the blood (hematogenous transfer) and VT can occur through the placenta (19). Consequently, the placenta and fetus are a single functional unit, which can be compromised. Since the vaginal delivery route is safe, the decision for the C section should only be based on clinical judgment and not be based on the sole presence of maternal SARS-CoV-2 infection (20). As for the postpartum period, the utmost attention must be paid to preventing horizontal contamination through newborn handling by an infected mother/staff/family since it does not occur through breastfeeding (21). Overall, beyond maternal assessment, examination of the newborn, mostly by using a nasal swab, is the most economical and informative method to determine whether VT has occurred.
Interval between maternal SARS-CoV-2 diagnosis and delivery frequently is short, minimizing VT
Timeline of maternal exposure to the virus is critical since, frequently as soon as the maternal infection is diagnosed, if it is close to term, induction of labor or CS is planned with the first aim of minimizing the maternal and fetal complications and then minimizing VT. This is because, despite the high rate of maternal infection, the overall VT rate remains low at ~3%–5%. The Society for Maternal and Fetal Medicine (SMFM) advice is that cesarean sections should only be performed when medically justified. The mode of birth should be individualized and based on the preferences of the woman alongside obstetric indications (22, 23).
Generally, there is a clear reluctance to enroll pregnant patients in clinical trials for testing new drugs. The situation is not dissimilar to the case of SARS-CoV-2 infection. However, due to the perceived severity of the current situation, many patients were until recently treated with any non-specific medications available on site, and such treatment was continued even after delivery. Luckily, the introduction of vaccines and rapidly generated safety data on maternal vaccination before and during pregnancy have been widely implemented, reducing the use of non-specific drugs. Such large-scale vaccine implementation has led to a major decrease in both maternal and newborn morbidity and mortality before, during, and after pregnancy (24). Postpartum management of maternal infection is more effective due to the major physiological changes that occur after delivery (25). Also, pregnancy-associated pathologies like pre-eclampsia tend to resolve because of a reduced burden on the respiratory and cardiovascular systems. Notably, the newborn can be removed from the potential source of infection and managed effectively.
True VT rates are rare and require precise diagnosis
Detecting the exact rate of vertical and newborn viral infection is not expected to be precise and will remain so. There is no universal screening for SARS-CoV-2 in the mother and the newborn unless symptomatic and most asymptomatic infection rates remain unknown. Furthermore, caretakers and family members are not routinely tested for the virus. To document VT, stringent, readily available, and accurate diagnostic validation of the newborn is needed after delivery. However, those tests are only rarely available and performed. The mother is often admitted to the hospital while in labor or in the context of an emergency, where she is followed by supportive measures, medication(s), and, if close to term, delivered by either vaginal or cesarean section (26). Consequently, maternal evaluation may occur only after delivery. This will expose the newborn to a non-controlled environment where horizontal transmission can and frequently does occur.
What about the newborn, considering that the SARS-CoV-2-positive mother is likely to transfer the virus throughout pregnancy once she is infected? VT can occur but only in ~3%–5% of cases (27–32). Examining 19 cases of possible VT, after closer scrutiny, only in three to five instances, there was clear unambiguous support for VT as documented by either a positive swab by PCR shortly after birth or IgM in the newborn blood that it was not transferred by the placenta (33). Therefore, unless studies are examined as a dyad, it is difficult to document VT. In a large-scale study, only 16/610 cases were documented as having VT, out of which only one newborn was in the Intensive Care Unit (ICU) (29). The possibility of VT, whether it is documented or not, continues to be discussed.
A recent study on SARS-CoV-2 infected mothers reported that all nasal PCR tests of 82 newborns were negative. However, no data on blood tests or antibody titers were reported, thus questions do remain on true infection rates (34). A closer examination revealed a few important issues: Maternal respiratory tract infection was only present in 14% of the mothers—this would markedly decrease the likelihood of VT. However, since some patients had symptoms for more than two weeks, the length of exposure would have enabled VT if the virus had localized beyond the lung. Irrespective of the mode of delivery, VT did not occur. Infants born preterm >32 weeks did not appear to be compromised. However, these infants are expected to receive steroids for lung maturity and this drug has antiviral properties, helping the mother as well. Direct evidence for VT-induced newborn pathology leading to neurological compromise was observed (35). Whether the fetal compromise was due to the maternal condition or/and VT is unclear (36). Notably, irrespective of whether the placenta and membranes are positive for infection, it does not necessarily translate in most cases to evidence of VT presence, as revealed by the recent findings of a prospective cohort study where the VT has been extensively studied through viral research on the placenta, amniotic fluid, cord blood, and neonatal swabs (32).
Thus, real VT is difficult to demonstrate since labor is a highly active process and immediately post-delivery, the patient, staff, and family members can readily become the virus transmitter. Even when a maternal nasal swab is positive, the placenta and membranes are frequently not evaluated or discarded. Moreover, an asymptomatic newborn is seldom tested. Documenting VT requires the following arduous tasks: the presence of maternal infection, placental infection (not always found), and newborn infection need to be assessed; whether postpartum mother-to-newborn virus transmission has occurred; newborns are tested for infection using a nasal swab, which must be confirmed through PCR testing for the precise detection of the virus. However, the reliability of tests in many cases remains uncertain (37). Rarely, anal and eye RT PCR swabs are required as a secondary confirmatory site. Despite the hematogenous route of spread, newborn blood is seldom tested—below the detection limit. This should change as newer assays develop. In newborns, SARS-CoV-2 IgM must be present since these large antibodies do not cross the placenta. For the antibody development, a significant viral load is required, which can take more than 4 days and requires confirmation at two weeks by the presence of specific IgG titers. Although suggestive, tests of T-cell immunity as a marker for protection against infection are not routinely used and their value in documenting immunity against the virus needs confirmation (32).
A recent study demonstrated that ACE2 and TMPRSS2 fetal expression in the intestine from the second trimester. They performed a retrospective analysis of a single cell data repository. The data were then validated at both gene and protein level by performing RT-qPCR and two-color immunohistochemistry on a library of second-trimester human fetal tissues. This dataset indicates that the lungs are unlikely to be a viable route of SARS-CoV2 fetal infection. The fetal kidney, despite presenting both the proteins required for the infection, is anatomically protected from exposure to the virus. However, the gastrointestinal tract is probably susceptible to infection due to its high co-expression of both proteins, as well as its exposure to potentially infected amniotic fluid (38).
Feto-placental paradox: Resilience vs susceptibility for SARS-CoV-2
The placenta is the interface between the mother and fetus. Throughout pregnancy, it has several vital functions, not only related to maternal tolerance but also enabling effective embryo–maternal interaction through implantation and trophoblast invasion. The placenta plays a vital role in the transfer of nutrients and oxygen and serves as a shield for the fetus against many environmental toxins and pathogens. Therefore, there is an obvious paradox in the case of SARS COV-2: infection of the placental tissue is associated with a minimal or null infection of the newborn (39). This deserves and requires further attention, especially considering that the biology and development of these two structures, placenta and fetus, share their embryological origin, while they are directed toward different destinies. The fetus progressively adapts to extrauterine life while the placenta, toward the end of gestation, undergoes progressive senescence, which is required for labor to spontaneously start and, following delivery, the placenta will promptly separate and be expelled by uterine contractions.
The placenta acts both as shield and as conduit for fetal infection
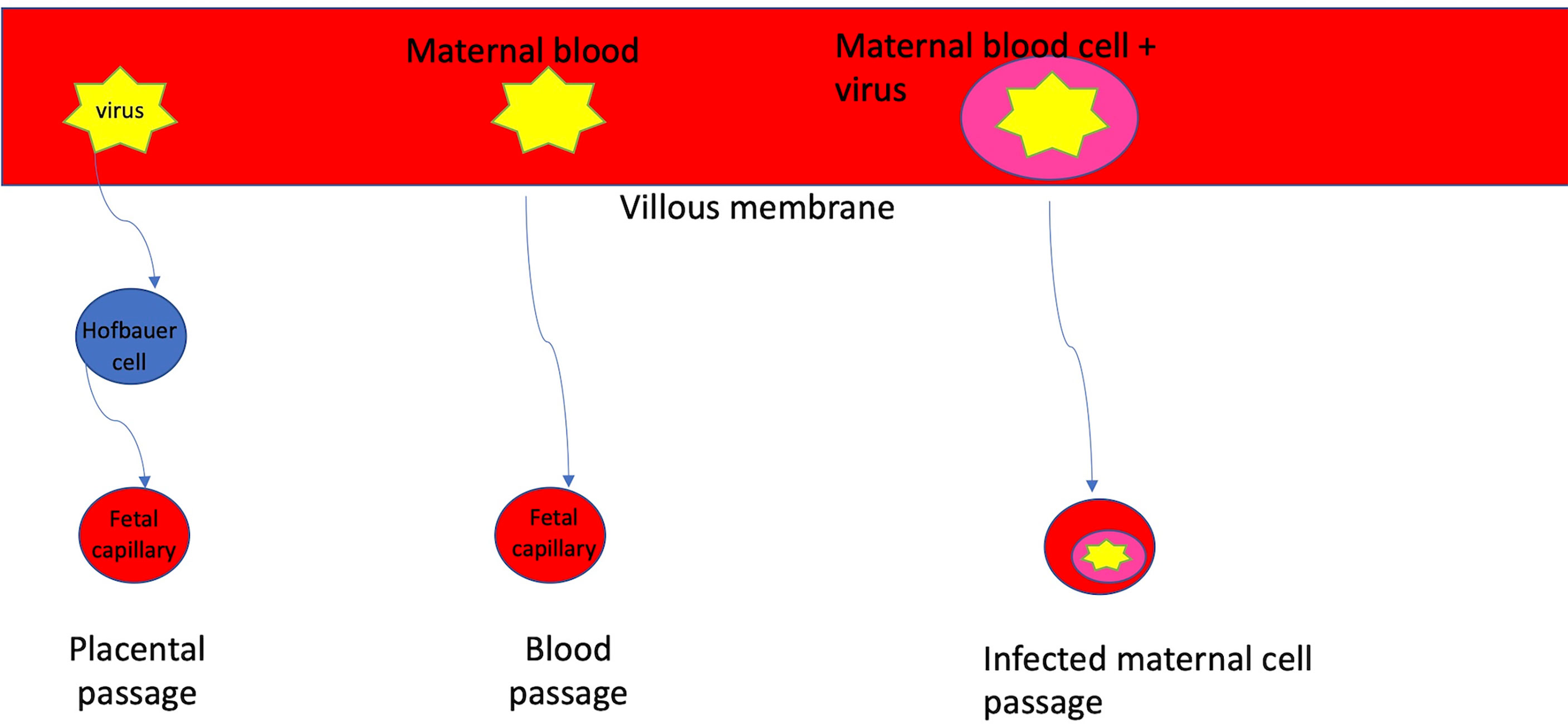
To reach the placenta from the infected upper respiratory tract or lung, it is hypothesized that the virus should travel through the maternal circulation as a free virion, engulphed by infected circulating immune cells, and can target local Hoffbauer cells via fetal capillaries, as shown in Figure 1 (40–42). Through the uterine vessels, the virus crosses the decidual layer, reaching the invading trophoblast cells. The decidual layer consists of numerous immune cells, including uterine NK cells, whose local role in invasion or protection against SARS-CoV-2 and other pathogens is unclear. However, since no virus was shown to be present in the chorionic plate or in the decidua, it may reflect a local antiviral protection preventing the virus replication prior to reaching the placenta. To diagnose VT, it is imperative that the maternal infection be confirmed before delivery and the route of virus spread to the newborn must be documented. Is there a confirmed transplacental infection? Once the virus reaches the placenta, it binds to trophoblast cell receptors (36).
A recent review examined in detail how to document placental infection by the SARS-CoV-2 virus. An evidence-based ranking was generated, ranging from confirmed infection to absent. It illustrated the fact that the reported rate of virus infection in the placenta ranges from 5% to 100%. The virus from the mother through viremia via the umbilical cord will inevitably reach the placenta. Therefore, theoretically, infection rate is expected to be 100%. However, there is a major difference between the virus presence and the associated histological changes. Currently, most postpartum placentas are not tested for viral presence. Advanced methods are required to document infection since there is a clear delay between the presence of the virus and evidence for pathological histological changes. Also, there are methodological limitations, namely how the tissue is preserved and which part of the placenta is analyzed, mostly in trophoblast cells where the virus is likely to reside. Conclusive methods for virus detection in the placenta are sophisticated and not widely available, leading to the current disparate observations. They include in situ hybridization with an antisense probe to detect virus replication; viral particle detection by using messenger RNA; or by using immunohistochemistry to detect spike protein. Additional confirmatory methods use electron microscopy to detect free virus presence. Obviously, those are sophisticated methods rarely available in hospitals where infection rates are high, so such methods are mostly used in a research setting. A widely available method used is RT-PCR-based virus detection. As for histological changes, they vary from subclinical to major inflammatory changes. Generally, short-term viral exposure may not alter placental histology. When infection is significant, both trophoblastic cells and villi structures are altered. There is increased cellular apoptosis and macrophage presence. This infection may cause both maternal and fetal vascular malperfusion, villitis, inter-villosities, and chorioamnionitis (43) Do those changes reflect an enhanced innate immune response to the virus, indicating local anti-viral protection, or do they reflect an adverse proinflammatory response? The current evidence supports the view that the placenta has both these functions, which are in contradiction.
The ACE2 receptors, highly expressed in the lung, are the primary cellular targets for this viral infection. In the human placenta, receptor expression is higher in early gestation, declining significantly toward term. The virus receptors are mostly localized in the trophoblast epithelial layer and not in the stroma or the fetal endothelium, in contrast with the infected lung. However, the progressive increase in the placental surface acting as a sponge may bind most free virions to the local ACE2 receptors. Whether such binding will trigger local infection, or if a further step will be required for virus integration, remains unclear. Overall, close-to-term placental function declines because of calcification, fibrosis, and cell death. The placenta also serves as a physical barrier to the large surface of the fused syncytiotrophoblasts, reaching more than 12 m2. Practically, such a large barrier could absorb all virions while still enabling systemic infected immune cells access to the placenta. However, when the placental barrier is breached, virus transfers to the fetus will occur, leading to VT (44).
The remaining functional placental surface has high oxygen-carrying capacity and, through the formation of oxygen radicals, may protect the fetus by neutralizing free virions present in the extracellular space. Moreover, the trophoblast-derived immune cells, like Hoffbauer cells (fetal macrophages), which are close to fetal capillaries, may also engulf and neutralize the virus. Beyond trophoblasts, other placental cellular elements (fibroblasts, endothelial cells, mesenchymal stem cells, and stromal cells) can act as a shield or increase fetal vulnerability to infection. As Celik et al. (45) suggested, interaction with local caveolin by the virus triggers inflammation and the release of pro-inflammatory cytokines through the NFkB pathway. As for inflammatory mediators, the toll-like receptors (TLR2 and TLR4) act as prime pathogen sensors; they are highly expressed in the trophoblast, while they are weakly expressed in the syncytiotrophoblasts at term. However, E cadherin is expressed in the extra-villous trophoblast and may promote vulnerability to infection (46). As recently reported, ACE2 expression, ADAM17 activity, and serum ACE2 abundance were determined in three groups: symptomatic placenta with COVID-19, and control. Of note, only three of the 16 COVID cases were infected by SARS-CoV-2. In the third vs control and second trimester COVID-19 cases, placental ACE2 mRNA increased vs reduced protein expression coupled with ADAM17 a protease activity. Circulating ACE2 levels increased in both second and third vs control. ACE2 shedding through the protease action may provide an additional protective mechanism against infection by decreasing the binding sites for the virus (44).
Another mechanism related to ACE2 shedding is the release from cells of extracellular vesicles (EV) containing ACE2 (evACE2). These evACE2 are not only able to compete with cellular membrane ACE2, but are significantly more effective than the alpha, beta, and delta variants (47). Considering that multiple EVs are secreted as protectors by the trophoblast, carrying HLA-G and preventing local immune cells from attacking them, it is not surprising that evACE2 has a similar effect.
Patients with severe COVID-19 had EVs in their plasma, carrying as cargo members of the TNF superfamily and IL-6 family, pro-thrombotic/endothelial injury factors (TF, t-PA, vWF), and proteins associated with cardiovascular pathology (MB, PRSS8, REN, HGF). Significantly higher levels of TF, CD163, and EN-RAGE were observed in EVs from patients with severe disease compared with patients with only moderate disease requiring supplemental O2 (48). This could explain why a breach in host defense against SARS-CoV-2 could result in placental inflammation.
Therefore, beyond maternal disease, also, a significant placental infection is required for the fetus to be affected in late gestation. However, when maternal and/or placental pathology is already present, even a mild placental infection can severely affect the fetus. Namely, here, viral infection can only be contributory rather than be the primary cause of the underlying fetal pathology. Consequently, the primary virus-related or indirect maternal–placental pathology must be considered when the newborn is examined.
Innate fetal resilience against vertical transmission
Without the need for VT, SARS-CoV-2 infection can severely affect the mother, and consequently the fetus. Such describes the impact of SARS-CoV-2 infection on mother, fetus/newborn, family and caregiver, delineating the next steps for management. This is observed when the maternal disease is severe, mostly when it is associated with comorbidity requiring up to ICU admission and induced emergency delivery. Luckily, maternal death rates remained relatively low, although they were significantly increased before the availability of vaccines until early 2021. Therefore, we should determine whether the virus directly affected the fetus or newborn, or whether the adverse maternal environment without the virus transfer led to fetal or newborn pathology. If the maternal disease is not severe enough to cause long-term damage, full newborn recovery is expected. However, if the virus lingers in newborn tissues and the infection is not detected by current techniques, a long-term follow-up is required. This is to understand whether such children will develop delayed manifestations similar to older children and young adults. The low rate of VT despite the maternal severe condition, infected placenta, and membranes implies that the fetus may be resistant to the development of active virus-associated pathology.
Consequently, fetal resilience to infection must be considered. The newborn must adapt to extrauterine life and, unless severely affected, has the necessary tools to survive and thrive. There is a major difference between newborn infection and that of the mother and placenta with respect to the degree and severity of infection. They are different functional units despite the vital dependence of the fetus on the mother and the placenta as the obligatory conduit for its survival. Fetal resilience against infection could be innate since it progressively develops in utero, acquiring intrinsic protective elements that prepare for extrauterine life and thereby counteract adversity. This is paradoxical since in a detailed study of fetal organs, even after second-trimester loss of twins, no VT was documented (46). However, an increased miscarriage risk in the first and second trimesters following exposure to a specific B.1.17 virus variant is reported. Analysis of fetal organs showed that the ACE2 receptor critical for virus spike protein attachment is expressed in the fetal lung, heart, and liver—essential organs. Such vulnerability to infection is mitigated since fetal lung maturation starts only in the last trimester when the receptor expression is expected to increase. Moreover, the fetus is infected through the transplacental-hematogenous route and not through the respiratory tract. The fetal lung is full of liquid, which is exchanged with the surrounding amniotic fluid; thereby, the viral replication rate in the extracellular location may be minimal. The SARS-CoV-2 virus target receptor in the fetus was also found in the liver. Thus, local infections may become evident. However, this is highly unlikely since the liver serves as a primary site for hematopoiesis, and consequently, the local immune system could effectively minimize or eliminate the virus altogether. Such suggested mechanisms should be further confirmed. A potential local vulnerability could paradoxically become a virus neutralizer since both tropism and local protection may be effectively operative. Other sites of infection could also be minimized by local and systemic protection by both innate and adaptive immunity. This can be corroborated by the fact that fetal and immediate post-partum protection from pathogens occurs in all mammals, not only humans, and is associated with relatively low morbidity and mortality of the newborn. Through a complex interplay, both the placenta and the fetus minimize VT. Although titers of circulating anti-SARS-CoV-2 antibodies are low following infection in both pregnant and non-pregnant patients, there is a recent suggestion that antiviral immunity can be conferred through cellular elements of the immune system and not necessarily only by secreted antibodies. Also, in the newborn, certain T cells and/or other elements of the immune system may offer memory cells that would provide continued protection against the virus. Overall, despite the massive pandemic, which involves numerous patients and their offspring, the associated newborn morbidity and mortality remains low. This enables beneficial maternal–newborn interaction.
The case for maternal anti-SARS-CoV-2 antibody transfer induced VT prevention
Antibodies against SARS-CoV-2 or against any virus following maternal infection will lead initially to circulating IgM levels whose presence is only transitory and followed by the development of long-term circulating IgG antibodies a couple of weeks later. However, with respect to the SARS-CoV-2, the antibody development is variable. In pregnancy, it was observed that the viral infection must be at least moderate to develop a detectable level of circulating antibodies (36). This was also observed in non-pregnant subjects. Following the maternal infection, significant titers of anti-SARS-CoV-2 IgG were found both in the circulation and in the umbilical cord blood, reflecting antibody transfer to the fetus (15). The IgG titers are proportional to the severity of maternal disease, where it is found in 100% of cases. The transfer of IgG antibodies to the cord blood at different titer levels was detected both in mild asymptomatic and symptomatic cases. Cord blood antibody concentrations were correlated with maternal antibody concentrations and with the time interval between the onset of infection and delivery.
In line with the reported increased infection severity in male versus female patients following SARS-CoV-2 infection, such a potential sex difference was also examined in the placenta (49). Evidence for differential male versus female responses with respect to the immune response was determined. The authors examined the intersection of maternal–fetal antibody transfer, viral-induced placental interferon responses, and fetal sex in pregnant women infected with SARS-CoV-2. Placental Fc receptor abundance, interferon-stimulated gene (ISG) expression, and SARS-CoV-2 antibody transfer were interrogated in 68 human pregnancies. Sexually dimorphic expression of placental Fc receptors, ISGs and proteins, and interleukin-10 were observed after maternal SARS-CoV-2 infection, with upregulation of these features in placental tissue of pregnant individuals with male fetuses. Reduced maternal SARS-CoV-2—specific antibody titers and impaired placental antibody transfer were also observed in pregnancies with a male fetus. These results demonstrate fetal sex-specific maternal and placental adaptive and innate immune responses to SARS-CoV-2.This was coupled with a reduced transfer of protective antibodies. This also documents reduced protective antibody transfer to the male fetus following mRNA vaccination (49). Beyond antibodies, it is possible that the transfer of T cells could further lead to fetal protection (45). This indicates that both humoral and cellular immunity are coordinated in responding to the viral infection.
Post SARS-CoV-2, infection anti-IgG concentrations at delivery increased coupled with the increased viral load during infection and decreased with the delayed infection-to-delivery interval (9). SARS-CoV-2-specific antibody transfer was reduced compared to influenza- and pertussis-specific antibodies, and cord titers and functional activity were observed following third-trimester infection. This is caused by altered SARS-CoV-2-antibody glycosylation profiles, which were partially mitigated by infection-induced increased IgG and placental FCGR3A expression.
In newborns, either the exposure to SARS-CoV-2 was too short, or the infection was not severe enough to lead to antibody presence, which can also be transitory since titers appear to be variable and may even decline with time. The presence of IgM in a newborn could reflect the presence of VT. However, this is rarely tested and for the antibody to become positive, the prenatal exposure in utero must be significant and of long duration. This is since IgG detection in the newborn can be maternally derived. Thus, the difficulty in determining the real rate of VT is expected to remain significant in the foreseeable future.
Role of viraemia in pregnancy outcomes during SARS-CoV-2 infection
The dissemination of SARS-CoV-2 infection outside the respiratory tract into the circulatory system is a key step in COVID-19 pathogenesis. SARS-CoV-2 viremia has been associated with COVID-19 disease severity and mortality (49) and systemic viral dissemination seems to play a role in mediating tissue damage and fibrosis, hypercoagulable state, and persistent elevation of proinflammatory markers (50).
To date, limited data exist on the SARS-CoV-2 viremia during pregnancy (51) and the rarity of the VT suggests that the hematogenous dissemination of the virus during pregnancy is not a frequent phenomenon. Nevertheless, it is possible that maternal viremia could lead to placentitis (52, 53) by overwhelming placental immune defenses at the level of the syncytiotrophoblast, which comes into direct contact with maternal blood. SARS-CoV-2 placentitis—characterized by the triad of histiocytic inter-villositis, increased perivillous fibrin, and villous trophoblastic necrosis (53–55)—which could be responsible for the higher incidence of stillbirth among the many other adverse outcomes due to SARS-CoV-2 infection during pregnancy (55), as well as the associated fetal distress or demise.
Although COVID-19 placentitis has been described in cases of severe or critical maternal COVID-19 disease (56), it has also been reported in cases of mild COVID-19 disease (57, 58), suggesting that maternal disease severity does not directly correlate with the risk of placentitis.
Therefore, placental damage due to SARS-CoV-2 infection seems to correlate with fetal distress but not with maternal COVID-19 disease severity. This supports the hypothesis that the increased risk of fetal compromise is not related to VT but to functional impairment due to placental infection. However, even with mild maternal disease, for developing placentitis, maternal viraemia may be required, a risk factor for adverse pregnancy outcomes due to COVID-19.
Postpartum management SARS-CoV-2—Support breastfeeding
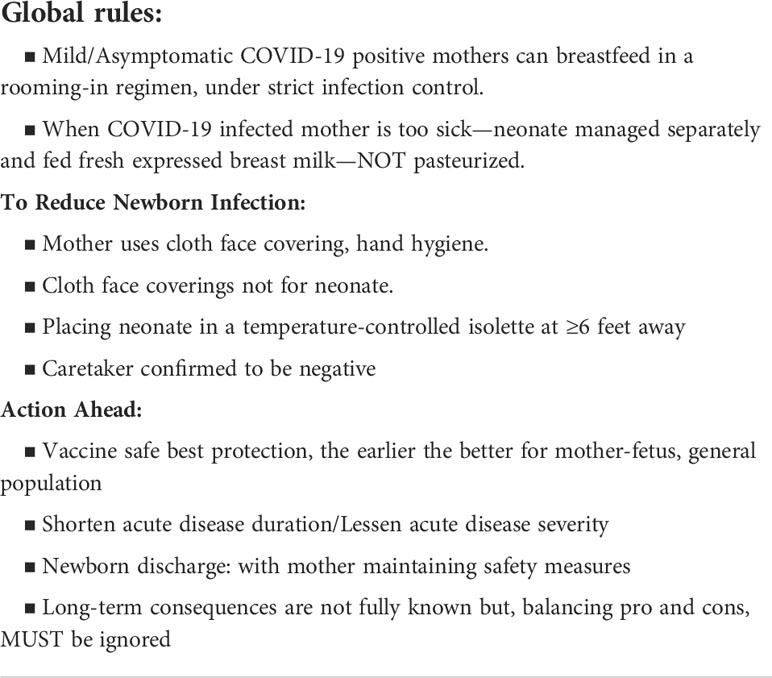
It is essential that the safety and wellbeing of both mother and newborn be preserved following SARS-CoV-2 infection. The following illustrate the steps required for breastfeeding while minimizing the maternal/newborn infection (59). The infected mother, depending on her clinical condition, may or may not require intensive medical management. This activity is more arduous following a cesarean section, and it depends on the severity of the maternal infection and associated co-morbidities. Significant titers of the protective anti-SARS-CoV-2 antibodies were detected in the maternal milk. Overall, circulating anti-viral IgG and breastfeeding add another layer of protection in maximizing newborn health and minimizing consequences of VT beyond that offered by the placenta and innate immune system of the fetus. SARS-CoV-2 spike-specific IgA antibodies were also detected in the infant saliva, supporting newborn resistance to infection (60). Peripartum infection protects both passively via breastmilk secretory IgA and actively by stimulating the neonatal immune system through the breastmilk-associated immune complex. Taking those aspects into consideration, the following general guidance is suggested. The principal goal is to develop a successful mother-infant bond while keeping both safe. Table 3 presents general guidelines that are currently endorsed by different professional societies. The key point is that breast milk does not transfer the virus to the newborn. This is the case even if the mother is severely infected. Also, breast milk may have several endogenous protective compounds that help the newborn not only with nutrition but also in building immunity against infections and diseases. In addition, the maternal transfer of protective antibodies was also documented. Such an environment would limit both the access and replication of the virus in this specific segregated fluid. Therefore, the goal is to breastfeed the newborn or, if the mother is too sick, collect the milk and provide it to the newborn, both in cases where the newborn is infected or not. The milk should not be pasteurized to preserve its nutritional value. Regarding the safety measures while breastfeeding, the mother should wear a facial protective mask while the newborn should not, to ensure an adequate airway access. The concern is for the caretaker. In case the mother is unable to breast feed, he/she must be tested to confirm that they are negative for the virus since post-partum infection can easily occur, as shown in several studies. Although thus far the rate of VT sequalae appear to be extremely low, one should not ignore the long-term consequences. In summary, the affected newborn must be followed long-term to fully understand the impact of vertical or even neonatal exposure when, much more commonly, the mother is asymptomatic and could transfer the virus to the newborn postpartum.
Three Betacorona viruses with disparate maternal fetal outcomes
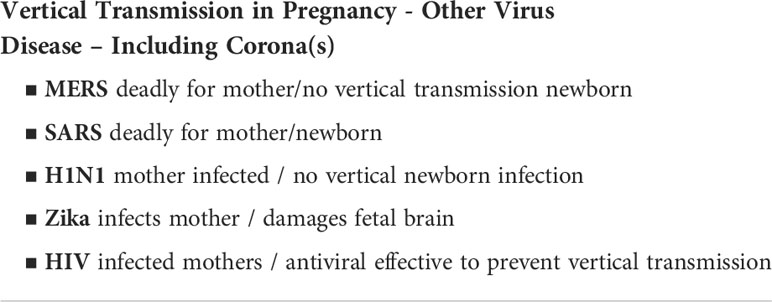
Although considered as epidemics, the rate of infection due to SARS-CoV and Middle East Respiratory Syndrome related coronavirus (MERS-CoV) finds no comparison with the risk to mother and newborn dyad of the current SARS-CoV-2 pandemic. The limited spread by the other severe Betacorona infections may be due to the local environment and mode of spread of the virus itself. However, as compared with current data in both previous epidemics, the death rate was higher. As for maternal infection, the symptoms of the two Betacorona viruses can be mild. However, in case-reports, significant maternal and fetal morbidity and mortality were documented. It is fortunate that those viruses did not reach pandemic proportions! To a degree, this contrasts with the SARS-CoV-2 maternal infection, where in most cases it is mild; fetal transmission is a rarity and is difficult to document. A better understanding of viral properties may clarify clinical aspects observed thus far for the viruses that share a similar structure where the virus spike protein is the leading binder to the host tissue, causing a respiratory infection. The SARS CoV and the SARS-CoV-2 bind to the same primary receptor, ACE2, highly expressed in the lung. In addition, the SARS CoV virus has an alternate site of binding, which is CD209 L, that can affect immune cells as well. The SARS CoV affects CD4 and CD8 T-cell subtypes, including CD25, CD28, and CD69. Instead, the MERS virus binds and negatively regulates the dipeptidyl peptidase 4 (DPP4) receptor, i.e., CD26, further affecting the adaptive immunity. Moreover, by impairing the action of macrophages as antigen-presenting cells, T-cell function is downregulated as well, which, through cellular apoptosis, severely damages the host. This contrasts with the infection caused by SARS-CoV-2, in which the lung tissue is the primary target and, unless the infection becomes severe, it remains localized there.
Although in SARS-CoV-2 the immune system can be affected, this is secondary to the primary lung infection. However, when the immune system is activated, systemic inflammation ensues together with coagulation disorders requiring thrombo-prophylaxis in patients with comorbidities in both pregnant and non-pregnant subjects. As for the clinical manifestations, the SARS-CoV-2 infection appears in most cases to be mild when compared with the severity of SARS and MERS. These two coronaviruses affect directly both mother and fetus directly during gestation, but this is mostly due to maternal disease with no evidence of viral transmission to the fetus/newborn. As such, in all three Betacorona viruses, VT is minimal (Table 4). In case studies regarding twelve patients, SARS CoV caused the deaths of three women and led to miscarriage in 57% of patients. Also, when gestational age was more advanced, it led to intrauterine growth restriction in 2/5 patients and premature birth in 2/5 cases in the third trimester. As for MERS-CoV, in 91% women (10 of 11 patients) had poor outcome and 82% neonates were critically ill and even led to newborn death. The severity of fetal/newborn disease was not related to maternal–fetal VT of the virus. Thus, based on these examples, a clear difference between the three viruses from the same family can be seen. The major difference is that the maternal disease—based on more limited data— appears to be more severe in SARS and MERS. It is hoped that this relative maternal and consequently fetal resiliency against the SARS-CoV-2 will not change as the virus continues to mutate due to the size of the current and still evolving pandemic where the virus mutants continue to emerge and cause infection despite massive ongoing vaccination efforts.
Conclusion
Unless new data emerge, the rate of maternal affliction of the newborn by SARS-CoV-2 is low due to mild maternal disease, which is mostly localized in the lung. Although a large body of data was generated, which is unprecedented in its extent since the short time that this virus has emerged until present, there are many remaining unanswered questions. It is clear at present that the presence of comorbidities significantly aggravates the viral infection. The vertical transmission of the virus is through the placenta, which has declining ACE2 receptor protein with advanced gestational age and TMPRSS2 receptors, serving as a shield and a vehicle to transmit the virus to the fetus. The clear evidence of placental and membrane infection while in the newborn apparent lack of infection is based on current limited diagnostics using nasal swabs, despite the evidence of hematogenous spread. This supports the notion of innate fetal resilience against such infections, which is plausible as it prepares for the inevitable challenges in post-natal life. An emerging hypothesis suggests that fetal expression of ACE2 and TMPRSS2 in the gastrointestinal tract could explain the susceptibility of the fetus to infected amniotic fluid from the late second trimester. Consequently, the newborn can benefit from maternal interaction through breastfeeding since the milk is not infected and contains protective antibodies. Developing sensitive tests to detect viremia beyond antibody-based detection and follow-up will remain an important tool for monitoring long-term sequela in post-natal life. Prevention and minimization of maternal infection throughout pregnancy remains a primary goal where the advent of vaccination continues to exert a major positive impact.
Author contributions
EB conceived and wrote the review. ND, SH, KT, SC, and AI helped in revising and contributing to the manuscript. All authors contributed to the article and approved the submitted version.
Funding
SH and KT received funding from Bulgarian National Science Fund, grant KP-06-DK1/12, 2021.
Conflict of interest
ERB was employed by the company BioIncept LLC.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Trostle ME, Limaye MA, Avtushka V, Lighter JL, Penfield CA, Roman AS. COVID-19 vaccination in pregnancy: early experience from a single institution. Am J Obstet Gynecol (2021) 8:16. doi: 10.1016/j.ajogmf.2021.100464
2. Etti M, Calvert A, Galiza E, Lim S, Khalil A, Le Doare K, et al. Maternal vaccination: a review of current evidence and recommendations. Am J Obstet Gynecol (2021) 11:S0002–9378(21)01228-X. doi: 10.1016/j.ajog.2021.10.041
3. Khoury R, Bernstein PS, Debolt C, Stone J, Sutton DM, Simpson LL, et al. Characteristics and outcomes of 241 births to women with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection at five new York city medical centers. Obstet Gynecol (2020) 136(2):273–82. doi: 10.1097/AOG.0000000000004025
4. Burton RD. Advancing an HIV vaccine; advancing vaccinology. Nat Rev Immunol (2019) 19(2):77–8. doi: 10.1038/s41577-018-0103-6
5. Poon LC, Leung BW, Ma T, Yu FNY, Kong CW, Lo TK, et al. Relationship between viral load, infection-to-delivery interval and mother-to-child transfer of anti-SARS-CoV-2 antibodies. Ultrasound Obstet Gynecol (2021) 57(6):974–8. doi: 10.1002/uog.23639
6. Pan F, Xiao X, Guo J, Song Y, Li H, Patel DP, et al. No evidence of SARS-CoV-2 in semen of males recovering from COVID-19. Fertil Steril (2020) 113:1135–9. doi: 10.1016/j.fertnstert.2020.04.024
7. Legro R. The COVID-19 pandemic and reproductive health. Fertil Steril (2021) 115(4):0015–282. doi: 10.1016/j.fertnstert.2021.02.003
8. Yan J, Guo J, Fan C, Juan J, Yu X, Li J, et al. Coronavirus disease 2019 in pregnant women: a report based on 116 cases. Am J Obstet Gynecol (2020) 223(1):111.e1–111.e14. doi: 10.1016/j.ajog.2020.04.014
9. Crovetto F, Crispi F, Llurba E, Pascal R, Larroya M, Trilla C, et al. Impact of severe acute respiratory syndrome coronavirus 2 infection on pregnancy outcomes: A population-based study. Clin Infect Dis (2021) 73(10):1768–75. doi: 10.1093/cid/ciab104
10. Gajbhiye RK, Tilve A, Kesarwani S, Srivastava S, Kore SJ, Patil K, et al. Increased rate of miscarriage during second wave of COVID-19 pandemic in India. Ultrasound Obstet Gynecol (2021) 58(6):946–9. doi: 10.1002/uog.24784
11. Jamieson DJ, Rasmussen SA. An update on COVID-19 and pregnancy. Am J Obstet Gynecol (2022) 226(2):177–86. doi: 10.1016/j.ajog.2021.08.054
12. Wright D. Prevention of the cytokine storm in COVID-19. Lancet Infect Dis (2021) 21(1):25–6. doi: 10.1016/S1473-3099(20)30376-5
13. Edlow G, Li JZ, Collier A-RY, Atyeo C, James KE, Boatin AA, et al. Assessment of maternal and neonatal SARS-CoV-2 viral load, transplacental antibody transfer, and placental pathology in pregnancies during the COVID-19 pandemic. JAMA Netw Open (2020) 3:e2030455. doi: 10.1001/jamanetworkopen.2020.30455
14. Fajnzylber J, Regan J, Coxen K, Corry H, Wong C, Rosenthal A, et al. SARS-CoV-2 viral load is associated with increased disease severity and mortality. Nat Comm (2020) 11:5493. doi: 10.1038/s41467-020-19057-5
15. Fenizia C, Biasin M, Cetin I, Vergani P, Mileto D, Spinillo A, et al. Analysis of SARS-CoV-2 vertical transmission during pregnancy. Nat Comm (2020) 11:5128. doi: 10.1038/s41467-020-18933-4
16. Galanopoulos M, Gkeros F, Doukatas A, Karianakis G, Pontas C, Tsoukalas N, et al. COVID-19 pandemic: Pathophysiology and manifestations from the gastrointestinal tract. World J Gastroenterol (2020) 26(31):4579–88. doi: 10.3748/wjg.v26.i31.4579
17. Chambers CD, Krogstad P, Bertrand K, Contreras D, Tobin NH, Bode L, et al. Evaluation of SARS-CoV-2 in breastmilk from 18 infected women. JAMA (2020) 16:20127944. doi: 10.1101/2020.06.12.20127944
18. Nir O, Schwartz A, Toussia-Cohen S, Leibovitch L, Strauss T, Asraf K, et al. Maternal-neonatal transfer of SARS-CoV-2 immunoglobulin G antibodies among parturient women treated with BNT162b2 messenger RNA vaccine during pregnancy. Am J Obstet Gynecol MFM (2022) 4(1):100492. doi: 10.1016/j.ajogmf.2021.100492
19. Vivanti AJ, Vauloup-Fellous C, Escourrou G, Rosenblatt J, Jouannic JM, Laurent-Bellue A, et al. Factors associated with SARS-CoV-2 transplacental transmission. Am J Obstet Gynecol (2022) 11:S0002–9378(22)00359-3. doi: 10.1016/j.ajog.2022.05.015
20. Fenizia C, Saulle I, Di Giminiani M, Vanetti C, Trabattoni D, Parisi F, et al. Unlikely SARS-CoV-2 transmission during vaginal delivery. Reprod Sci (2021) 28(10):2939–41. doi: 10.1007/s43032-021-00681-5
21. Raschetti R, Vivanti AJ, Vauloup-Fellous C, Loi B, Benachi A, De Luca D. Synthesis and systematic review of reported neonatal SARS-CoV-2 infections. Nat Commun (2020) 11(1):5164. doi: 10.1038/s41467-020-18982-9
22. National Institutes of Health. Coronavirus disease 2019 treatment guidelines (2021). Available at: https://www.covid19treatmentguidelines.nih.gov/.
23. SMFM. Management considerations for pregnant patients with COVID-19 (2021). Available at: https://www.smfm.org/covidclinical.
24. Kotlyar AM, Grechukhina O, Chen A, Popkhadze S, Grimshaw A, Tal O, et al. Vertical transmission of coronavirus disease 2019: a systematic review and meta-analysis. Am J Obstet Gynecol (2021) 224(1):35–53.e3. doi: 10.1016/j.ajog.2020.07.049
25. Lopes de Sousa ÁF, Carvalho HEF, Oliveira LB, Schneider G, Camargo ELS, Watanabe E, et al. Effects of COVID-19 infection during pregnancy and neonatal prognosis: What is the evidence? Int J Environ Res Public Health (2020) 17(11):4176. doi: 10.3390/ijerph17114176
26. Conti MG, Terreri S, Piano Mortari E, Albano C, Natale F, Boscarino G, et al. Response of neonates born to mothers infected with SARS-CoV-2. JAMA Netw Open (2021) 4(11):e2132563. doi: 10.1001/jamanetworkopen.2021.32563
27. Ashraf MA, Keshavarz P, Hosseinpour P, Erfani A, Roshanshad A, Pourdast A, et al. Coronavirus disease 2019 (COVID-19): A systematic review of pregnancy and the possibility of vertical transmission. J Reprod Infertil (2020) 21(3):157–68.
28. Di Toro F, Gjoka M, Di Lorenzo G, De Santo D, De Seta F, Maso G, et al. Impact of COVID-19 on maternal and neonatal outcomes: a systematic review and meta-analysis. Clin Microbiol Infect (2021) 27(1):36–46. doi: 10.1016/j.cmi.2020.10.007
29. Woodworth KR, Olsen EO, Neelam V, Lewis EL, Galang RR, Oduyebo T, et al. Birth and infant outcomes following laboratory-confirmed SARS-CoV-2 infection in pregnancy - SET-NET, 16 jurisdictions. MMWR Morb Mortal Wkly Rep (2020) 69(44):1635–40. doi: 10.15585/mmwr.mm6944e2
30. Flaherman VJ, Afshar Y, Boscardin WJ, Keller RL, Mardy HA, Prahl MK, et al. Infant Outcomes Following Maternal Infection With Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): First Report From the Pregnancy Coronavirus Outcomes Registry (PRIORITY) Study. Clin Infect Dis (2021) 73(9):e2810–13. doi: 10.1093/cid/ciaa1411
31. Carrasco I, Muñoz-Chapuli M, Vigil-Vázquez S, Aguilera-Alonso D, Hernández C, Sánchez-Sánchez C, et al. SARS-COV-2 infection in pregnant women and newborns in a Spanish cohort (GESNEO-COVID) during the first wave. BMC Pregnancy Childbirth (2021) 21(1):326. doi: 10.1186/s12884-021-03784-8
32. Costa S, Giordano L, Bottoni A, Tiberi E, Fattore S, Pastorino R, et al. Vertical transmission of SARS-COV-2 during pregnancy: a prospective Italian cohort study. Am J Perinatol (2022). doi: 10.1055/a-1792-4535
33. Yuan J, Qian H, Cao S, Dong B, Yan X, Luo S, et al. Is there possibility of vertical transmission of COVID-19: a systematic review. Transl Pediatr (2021) 10(2):423–34. doi: 10.21037/tp-20-144
34. Salvatore CM, Han JY, Acker KP, Tiwari P, Jin J, Brandler M, et al. Neonatal management and outcomes during COVID-19 pandemic: an observation cohort study. Lancet Child Adolesc Health (2020) 4:721–7. doi: 10.1016/S2352-4642(20)30235-2
35. Edlow AG, Castro VM, Shook LL, Kaimal AJ, Perlis RH. Neurodevelopmental outcomes at 1 year in infants of mothers who tested positive for SARS-CoV-2 during pregnancy. JAMA Netw Open (2022) 5(6):e2215787. doi: 10.1001/jamanetworkopen.2022.15787
36. Vivanti AJ, Vauloup-Fellous C, Prevot S, Zupan V, Suffee C, Do Cao J, et al. Transplacental transmission of SARS-CoV-2 infection. Nat Comm (2020) 11:3572. doi: 10.1038/s41467-020-17436-6
37. Chen W, Lan Y, Yuan X, Deng X, Li Y, Cai X, et al. Detectable 2019-nCoV viral RNA in blood is a strong indicator for the further clinical severity. Emerg Microbes Infect (2020) 9:469–73. doi: 10.1080/22221751.2020.1732837
38. Beesley MA, Davidson JR, Panariello F, Shibuya S, Scaglioni D, Jones BC, et al. COVID-19 and vertical transmission: assessing the expression of ACE2/TMPRSS2 in the human fetus and placenta to assess the risk of SARS-CoV-2 infection. BJOG (2022) 129:256–66. doi: 10.1055/s-0041-1726428
39. Thomas J, Sun Y, Debelenko L. Infrequent placental and fetal involvement in SARS-CoV-2 infection: Pathology data from a Large medical center. J Dev Biol (2021) 9(4):45. doi: 10.3390/jdb9040045
40. Egloff C, Vauloup-Fellous C, Picone O, Mandelbrot L, Roques P. Evidence and possible mechanisms of rare maternal-fetal transmission of SARS-CoV-2. J Clin Virol (2020) 128:104447. doi: 10.1016/j.jcv.2020.104447
41. di Gioia C, Zullo F, Bruno Vecchio RC, Pajno C, Perrone G, Galoppi P, et al. Stillbirth and fetal capillary infection by SARS-CoV-2. Am J Obstet Gynecol MFM (2022) 4:100523. doi: 10.1016/j.ajogmf.2021.100523
42. Delorme-Axford E, Sadovsky Y, Coine CB. The placenta as a barrier to viral infections. Annu Rev Virol (2014) 1:133–46. doi: 10.1146/annurev-virology-031413-085524
43. Sharps M, Hayes D, Lee S, Zou Z, Brady CA, Almoghrabi Y, et al. Structured review of placental morphology and histopathological lesions associated with SARS-CoV-2 infection placenta. Placenta (2020) 101:13–29. doi: 10.1016/j.placenta.2020.08.018
44. Taglauer E, Benarroch Y, Rop K, Barnett E, Sabharwal V, Yarrington C, et al. Consistent localization of SARS-CoV-2 spike glycoprotein and ACE2 over TMPRSS2 predominance in placental villi of 15 COVID-19 positive maternal-fetal dyads. Placenta (2020) 100:69–74. doi: 10.1016/j.placenta.2020.08.015
45. Celik O, Saglam A, Baysal B, Derwig IE, Celik N, Ak M, et al. Factors preventing maternal-fetal transmission of SARS-COV2. Placenta (2020) 97:1–5. doi: 10.1016/j.placenta.2020.05.012
46. Albrecht M, Arck PC. Vertically transferred immunity in neonates: Mothers, mechanisms and mediators. Front Immunol (2020) 11:555. doi: 10.3389/fimmu.2020.00555
47. El-Shennawy L, Hoffmann AD, Dashzeveg NK, McAndrews KM, Mehl PJ, Cornish D, et al. Circulating ACE2-expressing extracellular vesicles block broad strains of SARS-CoV-2. Nat Commun (2022) 13:405. doi: 10.1038/s41467-021-27893-2
48. Krishnamachary B, Cook C, Spikes L, Chalise P, Dhillon NK. The potential role of extracellular vescicles in COVID-19 associated endothelial injury and pro-inflammation. medRxiv (2020). doi: 10.1101/2020.08.27.20182808
49. Bordt EA, Shook LL, Atyeo C, Pullen KM, De Guzman RM, Meinsohn MC, et al. Maternal SARS-CoV-2 infection elicits sexually dimorphic placental immune responses. Sci Trans Med (2021) 13:617. doi: 10.1126/scitranslmed.abi7428
50. Souverein D, van Stralen K, van Lelyveld S, van Gemeren C, Haverkort M, Snijders D, et al. Initial severe acute respiratory syndrome coronavirus 2 viral load is associated with disease severity: A retrospective cohort study. Open Forum Infect Dis (2022) 9(7):ofac223. doi: 10.1093/ofid/ofac223
51. Li Y, Schneider AM, Mehta A, Sade-Feldman M, Kays KR, Gentili M, et al. SARS-CoV-2 viremia is associated with distinct proteomic pathways and predicts COVID-19 outcomes. J Clin Invest (2021) 131(13):e148635. doi: 10.1172/JCI148635
52. Mithal LB, Otero S, Simons LM, Hultquist JF, Miller ES, Ozer EA, et al. Low-level SARS-CoV-2 viremia coincident with COVID placentitis and stillbirth. Placenta (2022) 121:79–81. doi: 10.1016/j.placenta.2022.03.003
53. Shook LL, Brigida S, Regan J, Flynn JP, Mohammadi A, Etemad B, et al. SARS-CoV-2 placentitis associated with B.1.617.2 (Delta) variant and fetal distress or demise. J Infect Dis (2022) 225(5):754–8. doi: 10.1093/infdis/jiac008
54. Watkins J, Torous VF, Roberts DJ. Defining severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) placentitis. Arch Pathol Lab Med (2021) 145:1341–9. doi: 10.5858/arpa.2021-0246-SA
55. Linehan L, O’Donoghue K, Dineen S, White J, Higgins JR, Fitzgerald B. SARS-CoV-2 placentitis: an uncommon com- plication of maternal COVID-19. Placenta (2021) 104:261–6. doi: 10.1016/j.placenta.2021.01.012
56. DeSisto CL, Wallace B, Simeone RM, Polen K, Ko JY, Meaney-Delman D, et al. Risk for stillbirth among women with and without COVID-19 at delivery hospitalization - united states, march 2020-September 2021. MMWR Morb Mortal Wkly Rep (2021) 70(47):1640–5. doi: 10.15585/mmwr.mm7047e1
57. Meyer JA, Roman AS, Limaye M, Grossman TB, Flaifel A, Vaz MJ, et al. Association of SARS-CoV-2 placental histopathology findings with maternal-fetal comorbidities and severity of COVID-19 hypoxia. J Matern Fetal Neonatal Med (2021) 20:1–7. doi: 10.1080/14767058.2021.1977791
58. Husen MF, van der Meeren LE, Verdijk RM, Fraaij PLA, van der Eijk AA, Koopmans MPG, et al. Unique severe COVID-19 placental signature independent of severity of clinical maternal symptoms. Viruses (2021) 13(8):1670. doi: 10.3390/v13081670
59. Rostomian L, Angelidou A, Sullivan K, Melvin PR, Shui JE, Telefus Goldfarb I, et al. The effects of COVID-19 hospital practices on breastfeeding initiation and duration postdischarge. Breastfeed Med (2022) 22:1–9. doi: 10.1089/bfm.2022.0039
Keywords: SARS-CoV-2, vertical transmission, pregnancy, prenatal infection, fetal immunity
Citation: Barnea ER, Di Simone N, Hayrabedyan S, Todorova K, Inversetti A, Vento G and Costa S (2022) SARS-CoV-2 vertical transmission supports innate fetal protection: A narrative review. Front. Virol. 2:972452. doi: 10.3389/fviro.2022.972452
Received: 23 June 2022; Accepted: 12 August 2022;
Published: 23 September 2022.
Edited by:
Moises Leon Juarez, Instituto Nacional de Perinatología (INPER), MexicoReviewed by:
Gaurav Shrivastava, National Institute of Allergy and Infectious Diseases (NIH), United StatesJosé M. Reyes-Ruiz, Mexican Social Security Institute (IMSS), Mexico
Jose Bustos Arriaga, National Autonomous University of Mexico, Mexico
Copyright © 2022 Barnea, Di Simone, Hayrabedyan, Todorova, Inversetti, Vento and Costa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eytan R. Barnea, eytan.barnea.@gmail.com
 Eytan R. Barnea
Eytan R. Barnea Nicoletta Di Simone
Nicoletta Di Simone Soren Hayrabedyan
Soren Hayrabedyan Krassimira Todorova6
Krassimira Todorova6  Annalisa Inversetti
Annalisa Inversetti Simonetta Costa
Simonetta Costa