Influence of using simulated or real patients on undergraduate medical students acquiring competencies in medical conversations in surgery: A prospective, controlled study
- 1Medical Faculty, Frankfurt Interdisciplinary Simulation Center FIneST, Goethe University Frankfurt/Main, Frankfurt, Germany
- 2Department of General, Visceral, Transplantation and Thoracic Surgery, Goethe University Frankfurt/Main, University Hospital Frankfurt, Frankfurt, Germany
- 3Department of Pediatric Surgery, University Medical Center of the Johannes Gutenberg University Mainz, Mainz, Germany
- 4Department of Trauma-, Hand- and Reconstructive Surgery, University Hospital Frankfurt, Goethe University, Frankfurt, Germany
Background: Communication with patients and their relatives as well as with colleagues and students is an essential part of every physician's daily work. An established method for teaching communication skills is using simulated patients (SPs). However, teaching with SPs is often subjectively perceived by medical students as less instructive than teaching with real patients (RPs). Studies that analyze the influence of SPs compared to RPs for acquiring competencies are lacking. The aim of the present study was therefore to investigate the impact of SPs on long-term learning success for communication skills compared to RPs.
Material and Methods: Study participants were undergraduate third-year medical students who attended a communication unit and were randomized into three groups. The first group trained the role-play part with a SP (SP-group). The second group trained with a SP but thought that the patient was a RP because the students and the tutors were told that they were a RP by the principal investigator (incognito patient group [IP-group]). The third group and their tutors trained with a RP and were told that the patient was a RP (real patient group [RP-group]). Five to 12 weeks after completing the training, the study participants completed a curricular summative objective standardized clinical examination.
Results: There were 146 students who participated in the study. There were no significant differences between the three study groups at the informed consent stations and for those conducting anamnesis interviews.
Conclusion: Communication skills training with SPs appears to be equivalent to training with RPs in terms of competency development in communication-based assessments in surgery. Therefore, SPs should be used in these curricula, especially at an early stage, to enable the students to practice adequate communication skills.
Introduction
Communication with patients and their relatives as well as with colleagues and students is an essential part of every physician's daily work. As early as 1958, Lauda showed that up to 70% of all diagnoses can be made with an adequate anamnesis (1). A well-taken anamnesis can currently at best save unnecessary diagnostics that have no therapeutic effect.
Communication skills are important in every medical discipline that deals with direct patient contact but especially in Urology. Besides the common requirements such medical history taking and leading informed consent discussions in a language that the patient can understand, sensitive topics such as potency, sexuality, or continence also have to be discussed. Although Ernstmann et al. showed that good doctor–patient communication in Urology can improve treatment success (2), Urology residents are confronted with challenging communication situations, such as conversation with patients who have a demanding attitude or emotionally stressful situations where they can sometimes be overwhelmed (3). They, therefore, suggest that learning objectives for communication skills should be integrated into undergraduate and postgraduate medical training (3).
An established method for communication skills training is to use simulated patients (SPs). To support clinical skill learning, the concept of SPs was first presented by Barrows and Abrahamson in 1964 (4). SPs have now been established in almost all medical universities in German-speaking countries (Germany, Austria, and Switzerland) (5). These SPs are defined as “lay people who are trained to portray a patient with a specific condition in a realistic way, sometimes in a standardized way (where they give a consistent presentation, which does not vary from student to student)” (6).
Numerous studies show that SPs are appreciated and accepted by students (7–9). Good acceptance of SPs and the positive influence of SP use on knowledge acquisition and behavior change in learners has been proven (9, 10). For example, Zabel et al. showed that undergraduate medical students performed a knee or shoulder examination significantly better if they trained this examination on a SP who provided feedback than if they trained together under the supervision of a surgeon (11). Additionally, Herbstreit et al. showed that medical students performed slightly but significantly better when handling medical emergencies after they were trained using SPs compared with a traditional seminar cohort (12).
However, teaching with SPs is often subjectively perceived by medical students as less instructive than teaching with real patients (RPs). Generally, students considered RP interactions to be more instructive than interactions with SPs (7, 13). In a qualitative study that included 38 medical students, Bokken et al. showed that these students perceived RP encounters as more instructive and more authentic than conversations with SPs. The participants in this study also described that they saw the conversations with SPs as good preparation for conversations with RPs and that particularly difficult situations such as dealing with angry patients can be practiced well with SPs (7). However, studies that have analyzed not only the evaluations of the students, but also the influence of SPs compared to RPs on the acquisition of competencies are lacking.
The aim of the present study was to investigate the impact of using SPs on long-term learning success in communication skills compared to RPs.
Material and methods
Participants and background
This study had a prospective design and was performed in accordance with the ethical principles of the World Medical Association Declaration of Helsinki (Ethical Principles for Medical Research Involving Human Subjects). It was also reviewed by the ethics committee of the University Hospital of Frankfurt (Johann Wolfgang Goethe University), which indicated that no further approval was required.
Study participants were third-year undergraduate medical students. These students participated in the study after they received a detailed oral and written explanation of the study and provided written informed consent. Participation in the study was voluntary and could be terminated at any time without explanation. Epidemiologic data from each participant were gathered before the start of the study.
The study was performed during the mandatory 1-week long surgical skills lab training (14). This training contained 12 teaching units for practical basic surgery skills such as communication training and a teaching unit on abdominal ultrasound. The prerequisite for participation in the skills lab training was attendance at the main lecture on surgery and passing the associated written exam. The skills lab training was followed by a 2-week surgical internship.
Communication unit
The study took place during the 210 min of the communication training unit and aimed for the students to correctly take a patient's medical history and to meaningfully structure informed consent discussions for surgical interventions. The unit was conducted by student peer tutors. The quality of the units was monitored and maintained using tutor manuals, standardized presentations, and mandatory tutor training on a regular basis.
The teaching unit began with the students working out the essential components involved in taking a medical history under the guidance of the tutors before they practiced taking a patient's history. After the exercise, the students received 360° feedback on the content and on how they treated the patient. Special focus was placed upon communication competencies such as empathetic behavior and strategies to deal with sensitive topics. The second part focused on informed consent discussions and was conducted in the same manner. At the end of the unit, each student had at least taken one history or led an informed consent discussion.
Intervention
Regardless of study participation, students were assigned to groups by the Office of the Dean before the study. Bias was reduced because the principal investigator was not involved in the group assignments. Individual randomization was not possible because this study was integrated into the curriculum.
The participants attended the communication unit according to their group allocation. Both the theoretical part and the time limit were identical for all groups. The first group trained the role-play part using SPs (SP-group), and the participants were informed that SPs were used. The second group trained with a SP, but they thought that the patient was a RP because the students and the tutors were told that they were RPs by the principal investigator (incognito patient group [IP-group]). The third group together with their tutors trained with a RP and were correctly informed about it (real patient group [RP-group]).
Measurement
Five to 12 weeks after completing the training, the study participants completed a curricular summative objective standardized clinical examination (OSCE). During the study period, this OSCE consisted of eight stations and three to four of these stations were communication-based (taking a patient’s medical history or obtaining informed consent before surgery). Each station included 2 min to read the task and 5 min to solve the task.
The individual stations were evaluated using a two-part evaluation sheet. On the one hand, the station consisted of a standardized content-related checklist (part A). Individual content-related items (e.g., question about allergies and the nature of the pain) were evaluated using a three-part scale (0 = not performed/asked, 1 = partially/incorrectly performed/asked, 2 = correctly performed/completely asked). The total number of items differed depending on the task. The second part of the evaluation sheet assessed the overriding aspects of the interaction with the patient, such as communicating in language that was understandable to the patient or responding to the patient's questions. Five items were evaluated on a five-point Likert scale using fixed anchor criteria for 1, 3, and 5 points. For the overall assessment of the individual stations, the first part was weighted as two-thirds and the second part as one-third of the score. The evaluation sheets used in the present study were primarily piloted in previous undergraduate training. The content validity was ensured through the creation as part of an expert workshop with didactic and surgical experts as well as through the repeated application and adaption in the context of previous OSCE exams.
The examiners were surgeons who participated in the OSCE as part of their regular teaching duties. Examiner training was mandatory to become an examiner. This included training on how to use the checklists as well as taking a neutral role in the background. Examiners were blinded to the students' group allocation.
Statistical methods
Data were processed using Microsoft Excel (Microsoft Inc., Redmond, WA, USA). Statistical analysis was performed using IBM SPSS version 24 (IBM Corp., Armonk, NY, USA).
Tests between the groups were calculated using a parametric variant analysis of variance (ANOVA). If variant homogeneity was present, p-values for comparing groups were analyzed using Tukey's test. For variant heterogeneity, a corrected ANOVA (Welch's test) was used, and for p-value analyses between groups, the Games–Howell test was applied. Significance was defined as p < 0.05. An a priori sample size calculation was performed using G * Power (University Düsseldorf, Düsseldorf, Germany). Assuming a mean effect size of f = 0.4, the required group size was 34.
Results
One hundred forty-six students agreed to participate in the study, and 38.36% of them were men, while the mean age was 22.9 ± 2.8 years. The study group is thus representative of the sixth semester at the Goethe University in Frankfurt, Germany where the study was conducted. Table 1 shows the composition of the three study groups. Among the 146 participants, 131 (89.73%) completed the summative OSCE. The remaining students either did not meet the qualifications for the final examination or did not return.
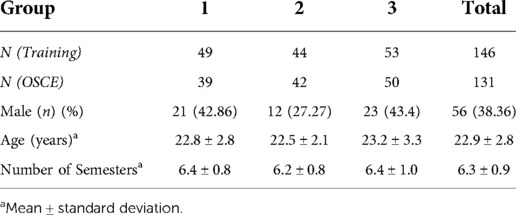
Figures 1–3 show the results of the individual study groups in the OSCE. There were no significant differences between the three study groups in the first and second part or in the overall evaluation.
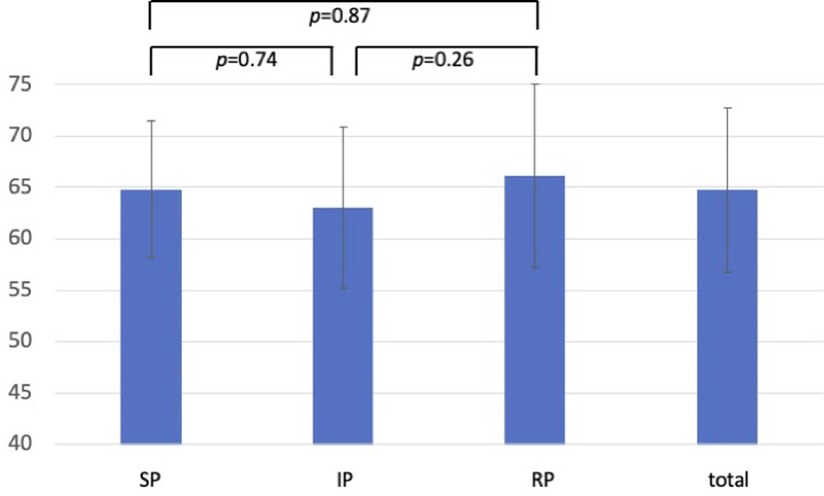
Figure 1. OSCE results for content-related items (first part of the evaluation sheet). Results of the rating for the content-related items. Data are presented as the mean ± standard deviation of the achieved results as a percentage. (SP-group, simulated patient group; IP-group, incognito patient group; RP-group, real patient group).
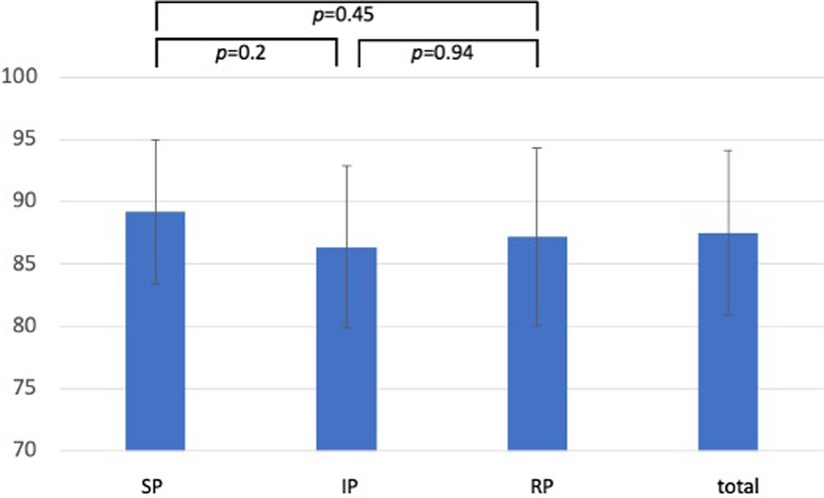
Figure 2. OSCE results for the second part (aspects of interaction) of the evaluation sheet. Results of the rating for aspects of interaction. Data are presented as the mean ± standard deviation of the achieved results as a percentage. (SP-group, simulated patient group; IP-group, incognito patient group; RP-group, real patient group).
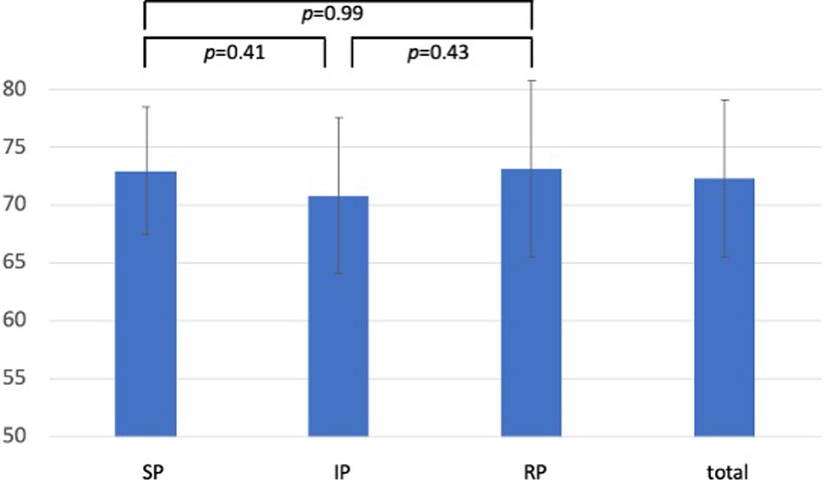
Figure 3. OSCE results: total rating. Results of the overall OSCE rating with the first part of the evaluation sheet weighted as two-thirds and the second part weighted as one-third of the score. Data are presented as the mean ± standard deviation of the achieved results as a percentage. (SP-group, simulated patient group; IP-group, incognito patient group; RP-group, real patient group)a.
Discussion
Since their first description in 1964 (4), SPs have been established in almost all medical schools in German-speaking countries (5). However, the influence of using SPs on the acquisition of competencies compared to RPs has not been conclusively examined.
In the present study, we showed that SPs are equivalent to RPs in terms of learning success in competency-based assessments. Thus, our results are consistent with those of McGraw et al. (15). However, in their study, 20 of 75 students were selected to train with SPs, and the remaining students formed the control group and trained with RPs. There was no difference in long-term success between the two study groups (15). However, the present study was conducted with a larger number of participants, a homogeneous group distribution, and an a priori sample size calculation.
Other studies reported that students described their subjective perception of the contact with RPs to be more instructive than their contact with SPs (7, 13). For example, Bokken et al. conducted a qualitative study in which medical students reported that they were better prepared for discussions with RPs than with SPs and that they found the discussions with RPs more instructive (7). On the basis of these results, we included a third study group in the present study that used incognito SPs to analyze students' subjective preference for RPs and its influence on the students' learning behavior.
We showed that there were no differences in the assessment of the content-related items or in the aspects of interaction with the patient compared to the other two study groups. Thus, the present study showed that using SPs leads to comparable results regarding the acquired competencies in taking a patient history and obtaining informed consent.
Additionally, in the present study, the IPs were not recognized by the tutors or the study participants. This finding is consistent with other studies, in which IPs are often not even recognized by the attending physicians (16–18).
Based on the principle of constructive alignment (19), the assessment of the acquired practical competencies was conducted using an assessment tool that measures the acquisition of practical competencies. However, previous studies that compared the impact of RPs and SPs used different assessment tools for their analysis. For example, Zhang et al. examined the influence of SPs on the acquisition of skills in conversational situations in gynecology (20). The students included in their study trained either with SPs, with RPs, or first with SPs and then with RPs. Their learning success was evaluated based on the analysis of the written case reports that were prepared by the students. The best results were achieved by those students who spoke to SPs, but those students who first spoke to SPs and then to RPs outperformed those who only spoke to RPs (20). Their study also indicates that conversations with SPs had a positive influence on learning success. However, the learning success was not assessed in a communication-based test, but, rather, by creating written case reports, which must be considered as a limitation of the validity of these results. Conversely, in the present study, it was possible to teach and test on the same level of competence.
Lane et al. also examined the use of SPs in teaching motivational interviewing to health care professionals, and they showed that it made no difference in terms of competence acquisition whether training was performed using an SP or via role play (21). In contrast to the present study, however, the participants in their study were health care professionals and not novice medical students. Medical students found the practice of speaking with SPs more useful the earlier they were in their training, which helped them to prepare for contact with RPs (7). Overall the present research suggests that it seems reasonable to integrate SPs or IPs into medical studies at an early stage so that students can derive the most benefit from their use and can initially train their communication skills in a protected environment. This appears to be particularly important in areas where sensitive issues need to be addressed, such as in urology or proctology. Practicing with SPs allows the students to first practice dealing with these topics with SPs and receive feedback regarding their behavior and handling before speaking with RPs. This method prevents careless handling of these topics that can unsettle patients or have a negative effect on the doctor–patient relationship; it also prevents the students from being disadvantaged in terms of learning success.
The positive influence of feedback from SPs on learning success has been shown in numerous studies (7, 11, 22, 23). In qualitative studies, for example, students reported that they found the feedback from SPs more useful than that from RPs (7). In addition, they reported that they receive authentic feedback-in-action through conversations with SPs, i.e. they noticed through the SP’s response during the conversation whether the conversation was going well, and thus, they were learning during the conversation (23). To prevent this from influencing the learning success in the present study, the authors decided to also recruit the RPs from the pool of SPs at Goethe University. While in their role as SPs, they received standardized role scripts and were trained for the assignment, and as RPs, they reported on their own illness and their own medical history without having received previous training or further instructions.
The present study has some limitations that need to be discussed. On the one hand, it was a single-center study within the framework of a single course curriculum. However, almost an entire semester could be included without the risk of selection bias due to participation in a voluntary, extracurricular course. The results of this study, therefore, appear to be representative and transferable to other faculties. Another limitation that needs to be discussed results from the fact that the interviews with the SPs and RPs were conducted in the skills lab. The skills lab itself is a simulated environment which holds it's own level of psychological safety. This may influence transferability to real-life scenarios. Another limitation is the choice of the curricular summative OSCE as the end point of the study because the influence of summative examinations on the learning behavior of students has been well documented (24, 25). Furthermore, there was a significant time interval between the exposure of students to SPs, IPs, or RPs during their skills lab training and the OSCE. During that time, students probably had opportunity to practice their communication skills on real patients regardless of their original exposure to SPs, IPs or RPs during the study. This may have influenced the results of the present study. Because the study was conducted as part of a well-established course curriculum, no other end point was possible. Future studies should investigate whether the results can also be verified using formative tests.
Conclusion
Training with SPs appears to be equivalent to training with RPs in terms of competency development in communication-based assessments for surgery. Therefore, SPs should be used in the curriculum, especially at an early stage of the course. This will enable the students to practice adequate communication with patients in a protected space, especially for sensitive issues, before expanding this knowledge with RPs later in the course. Using both SPs and RPs will prevent student from experiencing disadvantages toward learning success, and it will also prevent patients from being unsettled by insensitive handling, whether conscious or unconscious, of sensitive topics.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author contributions
VB, MR and JS were project leader and were responsible for study conception and had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. MR, JS, YK and UZ designed the role script for simulated patients and incognito patients. UZ trained the simulated patients. MR, JS, YK, MCS, VB and TS supervised the course units and the OSCE. YK, VB and JS were responsible for the data analysis and interpretation. YK, MR and JS conducted the statistical analysis. TS, MCS, UZ, and VB contributed to this statistical analysis and were involved in the interpretation of the data. VB, JS and MR wrote the final draft of the manuscript. YK, MCS, TS and UZ contributed to the final draft. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors would like to thank all students, SPs and RPs who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lauda E. [Clinical symptomatology of liver and biliary tract diseases]. Dtsch Med Wochenschr. (1958) 83(29):1217–24. doi: 10.1055/s-0028-1113760
2. Ernstmann N, Weissbach L, Herden J, Winter N, Ansmann L. Patient–physician communication and health-related quality of life of patients with localised prostate cancer undergoing radical prostatectomy–a longitudinal multilevel analysis. BJU Int. (2017) 119(3):396–405. doi: 10.1111/bju.13495
3. Necknig U, Deis N, Sterz J, Jünger J. [How do urological training residents experience the physician-patient conversation? : promotion of communication competence in the context of medical residency training]. Urologe. (2019) 58(7):781–9. doi: 10.1007/s00120-019-0913-6
4. Barrows HS, Abrahamson S. The programmed patient: a technique for appraising student performance in clinical neurology. Acad Med. (1964) 39(8):802–5.
5. Sommer M, Fritz AH, Thrien C, Kursch A, Peters T. Simulated patients in medical education–a survey on the current status in Germany, Austria and Switzerland. GMS J Med Educ. (2019) 36(3):Doc 27. doi: 10.3205/zma001235
6. Cleland JA, Abe K, Rethans JJ. The use of simulated patients in medical education: AMEE Guide No 42. Med Teach. (2009) 31(6):477–86. doi: 10.1080/01421590903002821
7. Bokken L, Rethans JJ, van Heurn L, Duvivier R, Scherpbier A, van der Vleuten C. Students’ views on the use of real patients and simulated patients in undergraduate medical education. Acad Med. (2009) 84(7):58–963. doi: 10.1097/ACM.0b013e3181a814a3
8. Sterz J, Gutenberger N, Stefanescu M-C, Zinßer U, Bepler L, Linßen S, et al. Manikins versus simulated patients in emergency medicine training - a comparative analysis. Eur J Trauma Emerg Surg. (2021). doi: 10.1007/s00068-021-01695-z. [Epub ahead of print]34331074
9. Kaplonyi J, Bowles KA, Nestel D, Kiegaldie D, Maloney S, Haines T, et al. Understanding the impact of simulated patients on health care learners’ communication skills: a systematic review. Med Educat. (2017) 51(12):1209–19. doi: 10.1111/medu.13387
10. May W, Park JH, Lee JP. A ten-year review of the literature on the use of standardized patients in teaching and learning: 1996–2005. Med Teacher. (2009) 31(6):487–92. doi: 10.1080/01421590802530898
11. Zabel J, Sterz J, Höfer SH, Stefanescu M-C, Lehman M, Sakmen DK. The use of teaching associates for knee and shoulder examination: a comparative effectiveness analysis. J Surg Educat. (2019) 76(5):1440–9. doi: 10.1016/j.jsurg.2019.03.006
12. Herbstreit F, Merse S, Schnell R, Noack M, Dirkmann D, Besuch A, et al. Impact of standardized patients on the training of medical students to manage emergencies. Medicine (Baltimore). (2017) 96(5):e5933. doi: 10.1097/MD.0000000000005933
13. Clever SL, Dudas RA, Solomon BS, Yeh HC, Levine D, Bertram A, et al. Medical student and faculty perceptions of volunteer outpatients versus simulated patients in communication skills training. Acad Med. (2011) 86(11):1437–42. doi: 10.1097/ACM.0b013e3182305bc0
14. Rüsseler M, Weber R, Braunbeck A, Flaig W, Marzi I, Walcher F, et al. [Training of practical clinical skills in surgery - a training concept for medical students]. Zentralbl Chir. (2010) 135(03):249–56. doi: 10.1055/s-0030-1247355
15. McGraw R, O’Connor H. Standardized patients in the early acquisition of clinical skills. Med Educat. (1999) 33(8):572–8. doi: 10.1046/j.1365-2923.1999.00381.x
16. Maiburg BH, Rethans JJE, van Erk IM, Mathus-Vliegen LMH, van Ree JW. Fielding incognito standardised patients as ‘known’ patients in a controlled trial in general practice. Med Educat. (2004) 38(12):1229–35. doi: 10.1111/j.1365-2929.2004.02015.x
17. Gorter SL, Rethans JJ, Scherpbier AJJA, van Der Linden S, van Santen-Hoeufft MHM, van Der Heijde DMFM, et al. How to introduce incognito standardized patients into outpatient clinics of specialists in rheumatology. Med Teacher. (2001) 23(2):138–44. doi: 10.1080/014215931048
18. Rethans JJ, Gorter S, Bokken L, Morrison L. Unannounced standardised patients in real practice: a systematic literature review. Med Educat. (2007) 41(6):537–49. doi: 10.1111/j.1365-2929.2006.02689.x
19. Biggs J. Enhancing teaching through constructive alignment. Higher Educat. (1996) 32(3):347–64. doi: 10.1007/BF00138871
20. Zhang J, Cheng M, Guo N, Xing A, Xu L. ‘Standardized patients’ in teaching the communication skill of history-taking to four-year foreign medical undergraduates in the department of obstetrics and gynaecology. BMC Med Educat. (2019) 19(1):1–9. doi: 10.1186/s12909-018-1418-5
21. Lane C, Hood K, Rollnick S. Teaching motivational interviewing: using role play is as effective as using simulated patients. Med Educat. (2008) 42(6):637–44. doi: 10.1111/j.1365-2923.2007.02990.x
22. Wright B, McKendree J, Morgan L, Allgar VL, Brown A. Examiner and simulated patient ratings of empathy in medical student final year clinical examination: are they useful? BMC Med Educat. (2014) 14:199. doi: 10.1186/1472-6920-14-199
23. Lovink A, Groenier M, van der Niet A, Miedema H, Rethans JJ. The contribution of simulated patients to meaningful student learning. Perspect Med Educat. (2021) 10(6):341–6. doi: 10.1007/s40037-021-00684-7
24. Raupach T, Brown J, Anders S, Hasenfuss G, Harendza S. Summative assessments are more powerful drivers of student learning than resource intensive teaching formats. BMC Med. (2013) 11(1):1–10. doi: 10.1186/1741-7015-11-61
Keywords: simulated patients, medical education, medical conversations, undergraduate students, surgical education
Citation: Britz V, Koch Y, Schreckenbach T, Stefanescu MC, Zinßer U, Sterz J and Ruesseler M (2022) Influence of using simulated or real patients on undergraduate medical students acquiring competencies in medical conversations in surgery: A prospective, controlled study. Front. Surg. 9:986826. doi: 10.3389/fsurg.2022.986826
Received: 5 July 2022; Accepted: 23 August 2022;
Published: 12 September 2022.
Edited by:
Ulrike Necknig, Ludwig Maximilian University of Munich, GermanyReviewed by:
Christian P. Meyer, Ruhr University Bochum, GermanyFuad Moussa, Sunnybrook Health Science Centre, University of Toronto, Canada
© 2022 Britz, Koch, Schreckenbach, Stefanescu, Zinßer, Sterz and Ruesseler. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jasmina Sterz jasmina.sterz@kgu.de
†These authors have contributed equally to this work and share last authorship.
Specialty Section: This article was submitted to Genitourinary Surgery, a section of the journal Frontiers in Surgery
 Vanessa Britz
Vanessa Britz Yannic Koch1
Yannic Koch1  Jasmina Sterz
Jasmina Sterz