Participatory design of a virtual reality life review therapy system for palliative care
- 1Augmented Materiality Lab, School of Creative Media, City University of Hong Kong, Kowloon, Hong Kong SAR, China
- 2Department of Psychology, University of Hong Kong, Kowloon, Hong Kong SAR, China
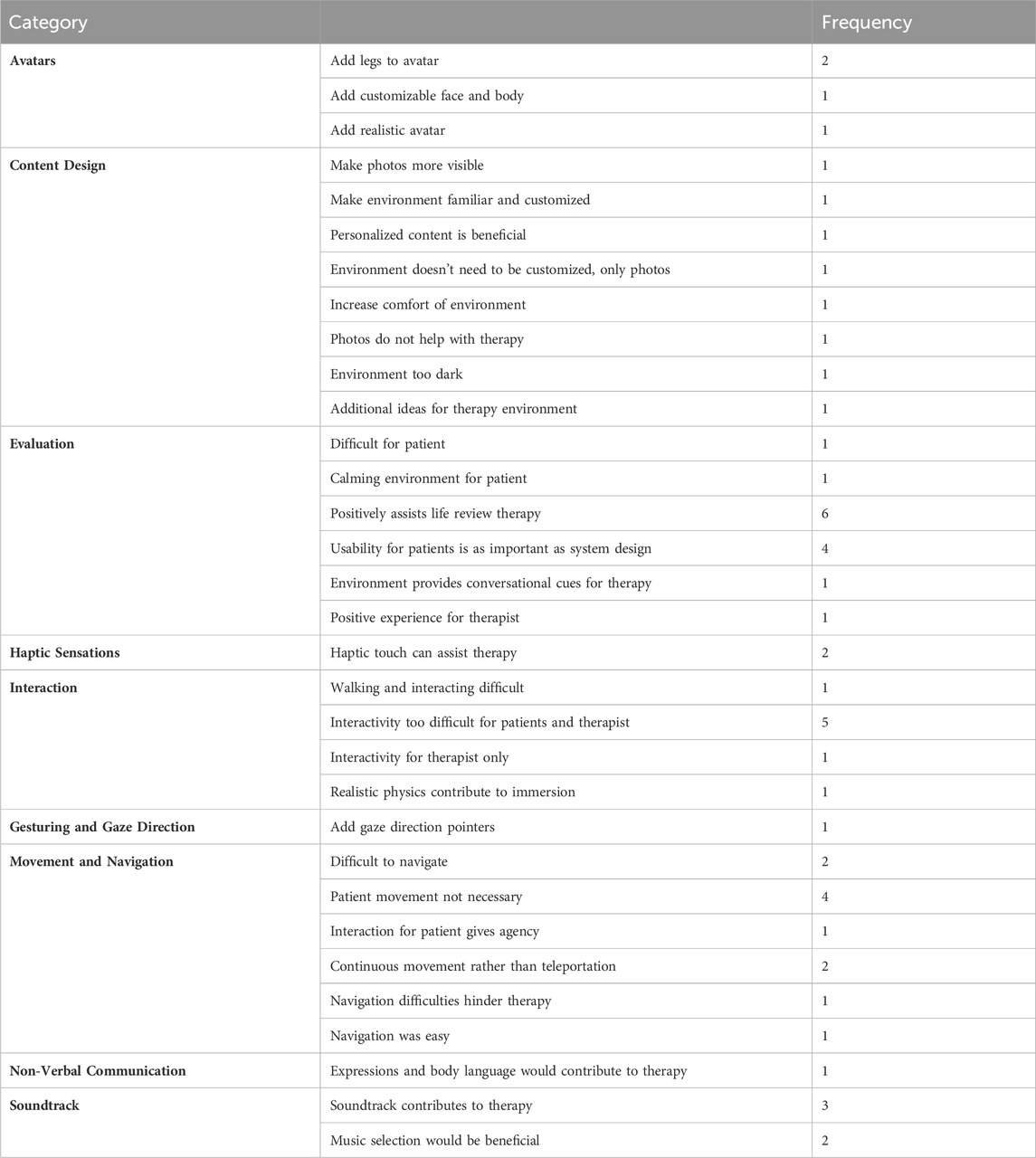
We present a novel Virtual Reality (VR) life review therapy system. Life review therapy is an intervention used by clinical psychologists, counselors, and social workers for patients under palliative care to systematically examine various life experiences to resolve conflicts and complete life tasks. The goal of the therapy is to narrativize the patient’s life before death in order to come to terms with their mortality. Our VR life review therapy system allows therapists to perform their interventions in customized virtual spaces designed to encourage the patient to reflect and reminisce about their life experiences. Our system is also developed in response to mobility restrictions and COVID-19 pandemic-related quarantine measures that have separated patients under palliative care from family and friends, resulting in emotional and psychological distress. As VR systems related to health are increasingly being used by therapists in their interventions, it is of utmost importance that the health professionals who will be the end users of these systems are involved in the design process to create ethical healthcare technologies. In response, we initiated the participatory design and evaluation of our VR life review therapy system prototype with six clinical psychologists who have practical experience delivering life review therapy to patients in palliative care in the Hong Kong hospital system. In the study, each participant experienced the VR life review therapy system and evaluated its strengths and weaknesses through semi-structured interviews. The qualitative data gathered from these interviews was coded according to nine different categories; avatars, content design, evaluation, haptic sensations, interaction, gesturing and gaze direction, movement and navigation, non-verbal communication, soundtrack. These conceptual categories were chosen based on our analysis of common themes reported by the clinical psychologists’ experience of the system. Feedback from clinical psychologists on each of these categories was incorporated into the redesign and update of the final system. Overall, participants generally evaluated the system as feasible and effective for use with patients under palliative care, while movement and interaction were the features requiring the most improvement.
1 Introduction
Virtual reality has become an increasingly useful tool for psychotherapists working in palliative care, with a recent review conducted by (Blomstrom et al., 2022) of novel interventions in palliative care listing the technology alongside psychotherapy, meditation and psychedelics. The majority of clinical work using VR in palliative care has focused on its positive effects for pain relief through “distraction” and the inducement of “awe” in the patient (Chirico et al., 2017; Ferguson et al., 2020; Johnson et al., 2020; Groninger et al., 2021). Much of this research is a response to the COVID-19 pandemic quarantine restrictions in which patients in palliative care were isolated from family and friends, with communication often restricted to 2D interfaces on phones, tablets and laptops. Research has already been conducted assessing the negative psychological impact of COVID restrictions and isolation on patients under palliative care placed in end-of-life care (Beng et al., 2022; Roulston et al., 2023; Zee et al., 2023). As a result, an innovative intervention that is able to address all of these psychological problems while overcoming the constraints of physical isolation is of pressing demand. VR can play an important role in these circumstances, allowing patients and their families to communicate remotely with greater senses of immersion and presence.
Presence in VR systems has been defined by Slater et al. as, “the strong illusion of being in a place in spite of the sure knowledge that you are not there,” which means the extent to which the user perceives a virtual environment to be real (Slater, 2009). Presence is generated in VR via immersion, which is a technical feature of media displays that surround the viewer so that the virtual landscape (including auditory space) can be perceived from any direction. This contrasts with the 2D, rectangular displays found in phones, tablets, laptops and PC’s which produce little to no sense of presence. It is important to note that presence is not simply a feeling, but a physiological response in the human autonomic nervous system that can be measured through changes in galvanic skin response, heart rate and brainwaves. Given this, one of the primary advantages and benefits of using VR is its ability to generate psychological and physiological presence that facilitate responses which other, non-immersive interfaces cannot.
Another benefit of VR is it can be used to create customized virtual environments which therapists can use to assist their therapeutic interventions, while also offering patients the ability to escape the confines of their body and the hospital through the use of VR as a telepresence technology. This research project involves the development of a VR system designed for a clinical psychologist to interact with their patients in a customized virtual environment based on emotionally, culturally and historically significant spaces for the patient that also incorporate photos and videos from their lives. These virtual social spaces will have a positive therapeutic function as embodied and networked versions of “life review” and “dignity” therapy which also give patients the ability to communicate and collaborate with family and friends in creating positive spaces for memory and reflection on their lives.
The interchangeably used “life review”, “dignity” or “reminiscence” therapy (Ando et al., 2006), involves the systematic examination of various life experiences with the aim of resolving conflict and completion of life tasks in order to help the patient come to terms with death. Examples of the therapeutic outcomes of this intervention is the writing of texts in collaboration with a therapist and the production of picture books, audio recordings or cookbooks as a “legacy” gift for family members after the patients death (Allen et al., 2008). A constraint of this therapy is that it consists entirely of spoken, textual or 2D visual communication and generally does not directly involve friends and family members who were participants in the patient’s life experiences. Recent research has demonstrated the positive effects of VR for pain relief in patients under palliative care through virtual travel, music therapy and presentation of soothing imagery (Johnson et al., 2020; Brungardt et al., 2021; Perna et al., 2021), indicating VR systems like ours can offer novel and unprecedented opportunities for the fulfillment of patients unmet psychological and physical needs. In order to improve the usability and effectiveness of our VR life review therapy system, we initiated a participatory design session with clinical psychologists working with patients under palliative care in Hong Kong. The key research questions we wanted to answer through our study were:
RQ1: Is VR life review therapy a feasible and effective tool for palliative care therapists?; RQ2: What are the key features of a VR life review therapy system that may be most beneficial to therapists and patients?
There is a small but growing body of research on the use and effectiveness of VR in palliative care, with a systematic meta-analysis conducted by Mo et al., 2022 having examined all eight studies produced so far concluding that while the technique is feasible and acceptable, the quality of the extant studies was graded as very low. Several of the articles analyzed involve patients who experience guided walks in VR environments based on natural landscapes (Baños et al., 2013; Ferguson et al., 2020; Groninger et al., 2021). Two articles feature personalized experiences and virtual travel (Niki et al., 2019; Perna et al., 2021), and two others involve music therapy and visualization of relaxing still images (Johnson et al., 2020; Brungardt et al., 2021). From the review, two out of the eight studies reported a decrease in pain scores among patients after a guided VR experience (Groninger et al., 2021; Perna et al., 2021), while in six of the studies patients reported positive attitudes towards the use of VR (Baños et al., 2013; Brungardt et al., 2021; Dang et al., 2021; Groninger et al., 2021). On the other hand, four papers reported difficulties in operating software and hardware (Baños et al., 2013; Ferguson et al., 2020; Brungardt et al., 2021). The only study so far to incorporate VR into life review therapy was conducted by Dang et al., 2021 which developed a virtual avatar to lead a life review therapy session with patients under palliative care, which bears similarity to research conducted by Tominari et al., 2021 which developed a virtual reminiscence therapy for dementia sufferers using 360 videos presented on touchscreen pads. In contrast to these examples, our research instead focuses on the clinical psychologists collaborative customization of a virtual space with patients to develop legacy outcomes equivalent to those which result from traditional life review and reminiscence therapy interventions. In addition, the creation of customized virtual environments will serve as posthumous archives of patients’ experiences and memories for family members before and even after death.
Participatory design has been defined by Simonsen and Robertson, 2012, as a process by which multiple participants take on the role of both user and designer in order to support mutual learning between multiple participants in collective “reflection-in-action”. Evaluation by end users is an important part of participatory design practices, most often utilizing qualitative methods of data collection such as participant observation and interviews after which evaluative criteria for assessing the design is extracted from the collected material. Bødker et al., have further outlined several key principles of participatory design for researchers in human-computer interaction (HCI): 1) Researchers and participants work collaboratively to design new products; 2) Designers and end users reflect critically on the design process to achieve the end goal; 3) The design process should enrich all collaborators 4). The process and outcome are equally important in participatory design studies (Bødker and Dindler, 2022). Kopeć et al., 2019 discussed the importance of participatory design processes, particularly when implementing cutting-edge information and communication technology (ICT) with older adults. Their study utilized participatory design methods to develop a VR ATM training simulation for the elderly and found that the process greatly improved the likelihood of acceptance by end users. In the case of palliative care, it is important to consult with all stakeholders that the VR intervention may involve including the patients, healthcare professionals, hospital staff, family and friends who are the most knowledgeable about the specific needs and vulnerabilities of patients.
2 Materials and methods
2.1 Participatory design and evaluation
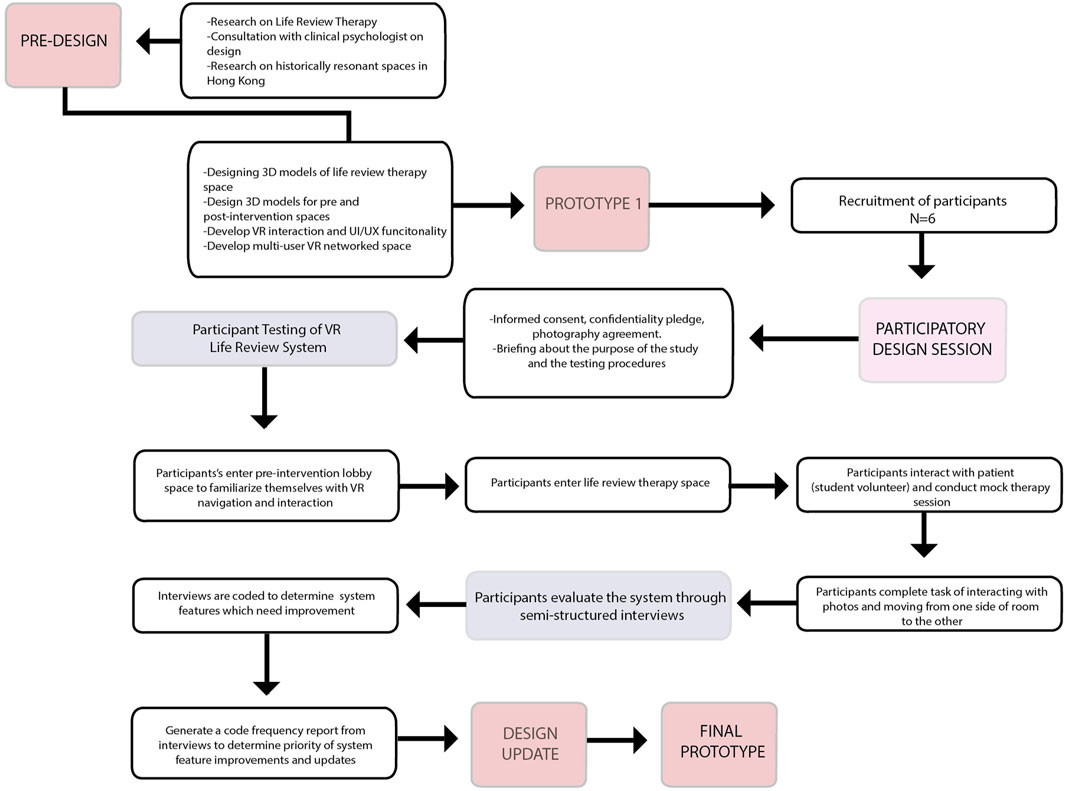
This research involves the participatory design and evaluation of a VR life review therapy system with clinical psychologists working in palliative care in the Hong Kong hospital system. We utilize a cooperative prototyping method (see Figure 1). In this method, clinical psychologists test the prototype version of the VR life review therapy system and are then asked to evaluate its features and functionality. The first stage involves the clinical psychologists entering the virtual environment, in which they are allowed to familiarize themselves with the controls for navigating the VR environment in a pre-intervention lobby space. Once they are comfortable, the clinical psychologists enter the “therapy” space, where they conduct a mock therapy session with one of the researchers who takes the passive role of the “patient”. The clinical psychologists are then asked to perform a simple task of selecting and organizing photos from photo frames in the therapy space. After completing the task and removing the VR headset, the clinical psychologists are asked to evaluate the prototype through semi-structured interviews with the principal investigators beginning with open-ended questions to prompt discussion such as; ‘how effective is the VR life review therapy system?’ and ‘what are its strengths and weaknesses?’ Based on the interviewee responses, the interviewers asked follow up questions to explore different subjects further. An initial descriptive coding of the interview transcripts is conducted to assign broad labels to the different topics addressed by the interviewees. These topics are further refined using a structured coding technique, in which related topics are grouped within larger conceptual categories to identify patterns and correlations between topics. The specific terminology we use for the conceptual categories is derived from the glossary of VR terminology proposed by Manetta and Blade in 1995 (Manetta and Blade, 1995). Further subcodes are assigned to each of these categories in order to identify specific details in the data and cross-reference them with each other. Finally, we compile a code-frequency report which tabulates the data according to conceptual categories and subcodes to identify patterns in the data “at a glance” and hierarchically prioritize which features we incorporate into the final update of the prototype (Table 1).
2.2 Participants
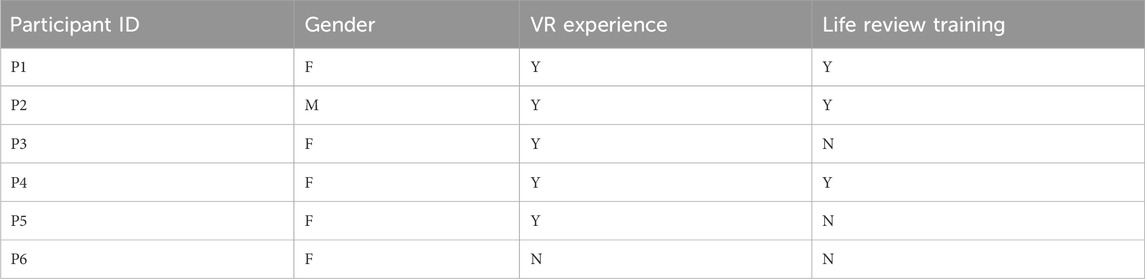
Six clinical psychologists working with patients under palliative care in Hong Kong public hospitals were invited to take part, recruited from within the investigators professional networks. Participants were asked to provide information on their prior use of VR and their experience conducting life review therapy with patients in palliative care (see Table 2). Exclusion criteria included participants with visual and hearing impairment, severe cognitive impairment, epilepsy or seizures, hypersensitivity to motion, active nausea or vomiting, and physical disability. Only participants who had provided informed consent were eligible to take part in the experiment.
2.3 VR system architecture
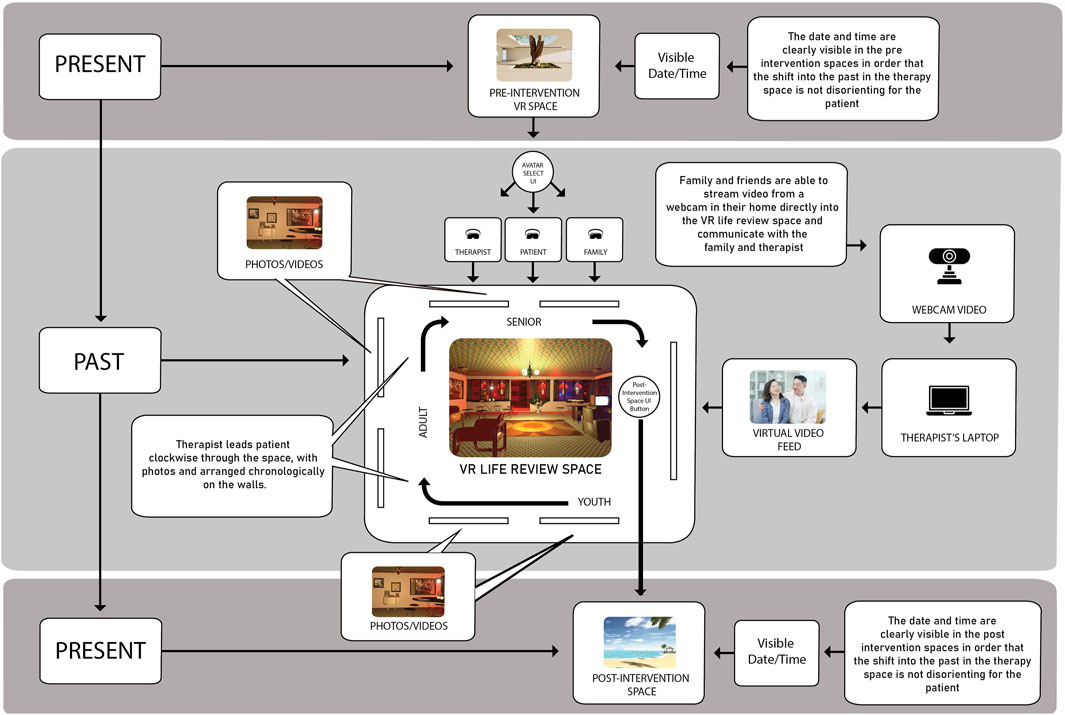
Our VR life review therapy system was designed using the 3D game engine Unity and deployed on the Meta Quest 2 VR head-mounted display. The system features two modes: a therapist mode giving clinical psychologists control over various features of the system, and a patient mode that ascribe a passive role to the user (Figure 2). The design of the therapy space is inspired by a typical Tong Lau building, a style of architecture common in Hong Kong from the late 19th century to the 1960s which the majority of elderly patients in palliative care are familiar with. It is furnished with “nostalgic” items, such as books, magazines, TV programs, calendars, furniture and decor from 1960s, 70 s and 80 s Hong Kong, to create a space resonant with memory and history in order to encourage reflection in the patient (Figure 3B).
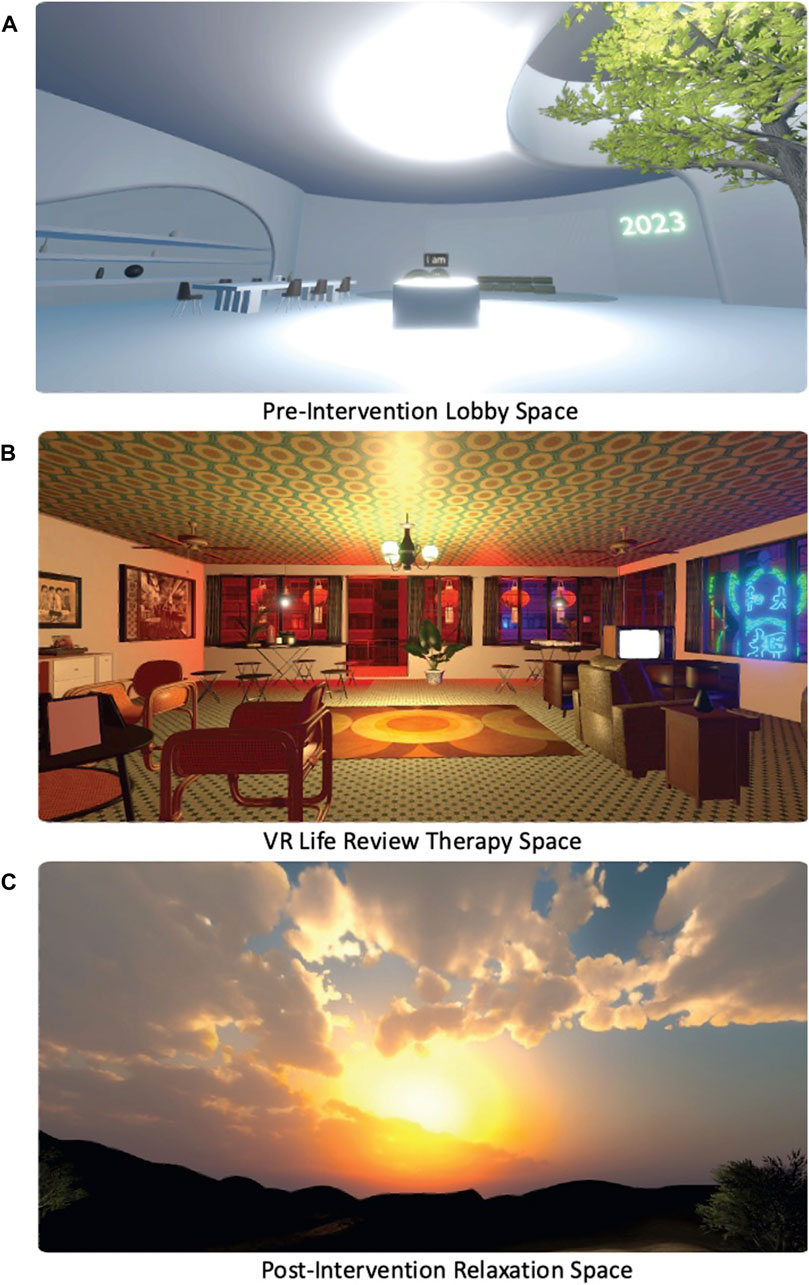
Figure 3. User’s view of the virtual pre-intervention lobby (A), life review therapy space (B), and post-intervention relaxation space (C).
In the initial prototype, we chose generic historical photos taken from the Hong Kong Museum of History historical photos archive. In the future versions of the VR life review therapy system we implement with patients under palliative care in hospitals, photos will be sourced from family and friends of the patients as part of initial screening and registration procedures and uploaded directly into the therapy environment which can be customized within the virtual therapy space. A video feed within the environment can connect to a webcam so that family and friends can enter the space as passive visitors or if they have a VR headset, can join as active participants in the therapy process. In order to minimize disorientation, the VR system includes pre-and post-intervention spaces, with clearly visible year, date and time in order to mediate the transitions between the present to the past for the patient, and re-situate them in the present after the intervention is complete. The pre-intervention space (Figure 3A) is designed to resemble a neutral “clinical” space in order to psychologically prepare the patient in a formal setting, while the post intervention space (Figure 3C) is a Hong Kong beach environment so that the patient can return from the “past” to the “present” smoothly. The post-intervention environment also functions as a de-briefing and relaxation space after the main therapy has been completed, in order for the psychologist to consolidate the experience with the patient. This space also gives the psychologist the opportunity to supplement the life review therapy with psychological elements that the VR intervention may not able to deliver, e.g., identifying positive memories from the patients life to enhance self-esteem in a low-stress environment.
3 Results
Below is a summary of the key findings of our qualitative data grouped into their respective conceptual code categories and sub codes. Quotations from the interviewees are included verbatim without corrections for syntax or grammar. Full transcripts of coded interviews are available upon request to correspondence author.
3.1 Avatars
The VR life review therapy system features head, arm and torso-only avatars of the psychologist and the patient with simplified, “cartoon” style faces with touch controller based hand-tracking. Two interviewees commented that the addition of legs to the avatar would contribute to the overall realism of the system. An initial design consideration for the first prototype was whether using photo-realistic avatars would make the experience more distressing for patients who are already facing extreme discomfort due to their fragile physical and psychological condition. This is because photo-realistic avatars can elicit the “uncanny valley” effect (Mori, 2012), adding to common side effects of VR experiences such as motion sickness (Chang et al., 2020).
However, one interviewee provided feedback suggesting that realistic avatars would be more preferable. This is because they would also enhance the sense of immersion for the patients:
“It would be better if it was a realistic avatar rather than a cartoon avatar. I think having the cartoon face makes me only be able to immerse using verbal language. If I can see their real face, rather than a cartoon face, the whole picture will be better.” (P3)
This interviewee also commented on customization aspects:
“it would better if we could select our face and dress, whether I wear glasses and my hairstyle.”
3.2 Content design
Regarding the content and design of the system itself, the aspect that received the most comments was the ability to customize photos and videos based on the patient’s own life. As one interviewee reported:
“When it comes to showing personal pictures and stuff, we could be sitting and the patient and I could view an album together. The movability (sic) is not a consideration, we can just focus on the pictures. Talking is the most important. Particularly when the patient cannot do much interaction anyway. Showing them the familiar environment and viewing the photos together would be the most beneficial way to design the system.” (P2)
While photos play an important role as catalysts for conversation between the psychologist and patient, it was suggested by some interviewees that these do not have to be personal and that generic old photos could also be effective triggers of personal memories and foster introspective reflection.
“I think personal photos would invite them to talk more. I mean now the environment has their personal photos, but it could just be a generic traditional environment, and then an album with all the personal touches. Because when you place the photos around the environment it might be difficult for the patient to navigate. It might just be a generic environment to give you the feeling of being immersed in another place. Then you dwell on your own memories with the ease of just reading an album.“(P2)
However, the importance of customization of photos in the therapy space is underscored by another interviewee who reported, “if they can choose their photos it can help them talk about their experience.” (P5).
For both of these interviewees, the nostalgic objects and environment are more important than the photos for encouraging the patient to reflect on their life experiences:
“I feel like the tong lau environment is very suitable for the old people, they will feel more comfortable … But I think having those items in the room is good, because it can help conversation, the TV and the mahjong table can help.” (P5)
Another interviewee pointed to the importance of comfort as a way to maximize the effectiveness of the therapy:
“When we provide counseling, it is important to have a comfortable place. So mostly we will sit down on a very soft sofa, or the patient is sitting on the bed. A more comfortable environment. If there was a sit down function it would be better. “(P3)
3.3 Evaluation
All interviewees positively evaluated the feasibility and overall effectiveness of the VR life review therapy system, acknowledging its potential benefits in a palliative care setting. The two most common benefits identified by the interviewees are that the system may 1) enable patients to virtually escape not only from the prison-like confines of the hospital room, but also from the limitations imposed by a declining body, and that 2) the life review therapy space provides a better catalyst for dialogue between the therapist and patient than a simple one-on-one therapy using photos or videos presented on a 2D interface:
“I think introducing this to the patients would be actually quite interesting and new for them. I think they would actually benefit from it a lot, if they find it not too difficult to use. Because they can see the things that they miss maybe and the people and photos that they miss. I guess sometimes you just want to escape from the hospital I think sometimes if you can even offer the patient one minute or five minutes of escape, it is very useful.” (P2)
“I think definitely this is better than doing the therapy in real life. The photos and the whole environment, if I was laying on the bed I cannot imagine this, but then I use the VR it can help the patient think about the past, it is really a great tool to help me elaborate my memories about the past. I think it is a very great tool for life review therapy.” (P3)
3.4 Haptic sensations
Two interviewees reported that the addition of haptic sensations to the system would increase the level of immersion and potentially help with the therapy. Haptic sensation can also contribute to patients sense of proprioception in the virtual space, especially in light of the weak visual acuity of some patients.
“If the patient is standing opposite me, and I want to touch them, it would be good to feel them and they are an object.” (P3)
3.5 Interaction
Interaction in the virtual environment was the most prevalent difficulty reported by the interviewees, specifically the ability of the psychologist to pick up and show a particular picture to the patient. As one interviewee reported:
“I really think showing the pictures or viewing the pictures together with the patient could be simpler. So at times we had difficulty referring to the same picture. I was trying to talk to the patients, but because the photo frames are placed on the table at different angles it is exceedingly hard to arrange the angle of the photos and make sure that both of us could see it. At one time, I needed to grab it and turn around to make sure the front is facing the patient to make sure they can see it.” (P2)
Another interviewee reported on the difficulty of moving through the space while trying to interact with the patient, while also pointing to a broader problem with interaction in the system; patients are often too physically weak to lift their hands, making operation of the VR controllers necessary for interaction virtually impossible.
“From my experience, some of the patients would have trouble even moving their heads. So I think us moving the photos together could be too difficult a task for the patient.” (P1)
One interviewee suggested enabling interaction exclusively for the therapist in order to mitigate this problem:
“They [the patients] could just be still and I am like a tour guide, asking if different features in the tong lau bring up any past experiences and then we can view the photos together and talk about their life.” (P2)
3.6 Gesturing and gaze direction
One interviewee commented on the difficulty of gesturing and recognizing the direction of the avatar’s gaze while having a dialogue in the virtual space. Their suggestion was to implement a gaze tracker visible to both the therapist and patient while they were talking:
“And maybe for the therapist, they can see what the patient is looking at right now, if from the therapist’s view, you can see a ray of what the patient is looking at. The patient does see it, only the therapist. I was just thinking when I was trying to see what picture he was referring to I had a difficulty, and he had to go through the trouble of telling me ‘this one on the right’. It would be much easier if only the therapist can see where his vision is directed at.” (P4)
3.7 Movement and navigation
The majority of interviewees reported difficulty using the controllers to navigate in the virtual environment. In the prototype, navigation was conducted via teleportation on both controllers, in which the avatar “jumps” from one point to another by directing a ray emanating from the controllers at the desired destination point. While this makes movement across large distances easier, it renders close distance movement impossible. This in turn affects the ease of communication between the therapist and the patient. This is evidenced by statements made by these interviewees.
“I think I just needed time to get used to the system. Moving around in the lobby I was struggling. It was a bit hard to navigate. And I think sometimes just now, there was not enough space to turn and move around.” (P1)
“If moving around involves using the controller, I imagine most of the patients can’t do it.” (P2)
“The distance between me in one location and the target I wanted to go to was too fast and too far. When I press the button I want to go in front of my patient but it teleported across him instead.” (P3)
“It’s quite interesting, but its a bit difficult to use the controllers. I don’t feel like I’m really interacting with the client because I can’t see them at all. But it might be my problem because I don’t really know how to navigate. So when I’m using the VR, I don’t remember that I need to look at the client, I just focus on speaking to him. I think it’s too much to handle at first, maybe when I’m more skillful at navigating, this will be less of a problem.” (P5)
One interviewee suggested that since navigation was so difficult in the virtual space for both the therapist and the patient, movement in the virtual space may not be necessary at all and can be removed from the virtual environment.
“Maybe moving around in the space is not 100% necessary. For example having the patient in the lobby immersed in that calming atmosphere without having them move around will be enough, the music that you put in there and the greenery, its sort of an escape from the hospital environment, so I’m not sure that having them move around is absolutely necessary.” (P1)
This suggestion was echoed by two additional interviewees:
“Instead of letting us both move around the room, maybe it can be stationary. As long as you can turn 360 degrees and you can see everything, that can be enough. You can still interact with the things, but you don’t need to move.” (P5)
“If they sit there and I sit there and we flip through the pictures together, I think its better if the patient is stationary. So they get less confused. But I can imagine some of them would want to walk around and be curious about the space. And that’s why it is good to use VR, because they are sitting in a bed anyway.” (P6)
However, another interviewee suggested that while movement in the system was currently problematic, it was an important feature to include as it provides the patient with the agency and mobility they lack in real life.
“I think the patient moving around is important, because in reality they maybe hardly move around, so in the VR world, it is better for them.” (P3)
Two other interviewees suggested that enabling continuous movement instead of teleportation could help make the experience more natural and control more precise:
“I think its good if they can move around, but it’s the way they move around, like sometimes when you play video games, you have that first person view and you can move at a quite normal walking speed, I dont know if the system supports it.” (P4)
3.8 Non-verbal communication
Two interviewees reported that the addition of non-verbal cues such as facial expressions and body language would facilitate ease of communication between the therapist and patient.
“I also thought some body gestures would be good, like nodding your head, I think this can enhance your communication. Because when we communicate, our verbal language only contributes a small percentage of our therapy, body language contributes a lot. Nodding our head, shaking our heads. And also, its better if we could smile.” (P3)
3.9 Soundtrack
The virtual therapy space features an ambient soundtrack which consists of: 1) Field recordings of street sounds from Hong Kong; 2) Hong Kong news reports dating back to the 70s and 80s that comes from a vintage TV set in the room (diegetic content); 3) Popular and familiar music from Hong Kong in the 1960s. Three of the interviewees stated that this soundscape positiviely contributes to creating a “nostalgic” atmosphere which can assist life review therapy by providing another sensory mode to complement the visual environment.
4 Discussion
We conducted a participatory design session with clinical psychologists working with patients in palliative care in the Hong Kong public hospital system, to investigate the question of whether; 1) a VR life review therapy system could be a feasible and effective tool for palliative care therapists and 2) what features of such a system would be most beneficial to therapists and patients. The results demonstrated that all therapists found the VR system “positively assists life review therapy” by offering the patient the ability to escape from the confines of their deteriorating physical condition and the isolation of the hospital environment. The “nostalgic” tong lau virtual environment was also deemed useful by the therapists who viewed it as a good catalyst for conversations by vividly visualizing the patient’s past—a key aspect of life review therapy. In addition to the overall positive evaluation of our VR life review therapy system, the study also identified several key features which the clinical psychologists reported would be beneficial to their interventions. These include the use of photo-realistic avatars with greater facial expressions, personalized media such as photos and videos which would make the VR environment more relatable to the patient and the addition of haptics in the controllers and gaze direction pointers to improve the fluidity of interaction between therapists and patients.
This study also helped identify several problems early on related to the user’s movement and/or interaction with elements in the virtual space, namely:
1. Free movement gives patients a sense of control, which has a significant positive impact on their psychological wellbeing. However, difficulties in using VR controllers can lead to frustration and increased distress, ultimately reducing the effectiveness of the therapy. In particular poor choices in the design of the navigation interface create usability issues, especially for patients with weak physical conditions.
2. If movement is offered, both continuous joystick movement and dis-continuous teleportation should be available to facilitate difference types of interaction and navigation. i.e., continuous motion is useful for moving short distances while teleportation is useful for longer distances.
3. Interaction with objects is less important for patients than therapists given the aforementioned interaction and navigation issues for vulnerable patients.
Based on these findings, we can conclude that while free movement can provide users with a greater sense of autonomy, an uplifting and positive feature than can help patients forget about their real-life, bed-ridden situation, any difficulties with interaction and navigation experienced can also undermine user acceptance and negatively impact on the overall sense of immersion and presence. In light of this tension, it is paramount that the system can accommodate this variability of user experience into the design itself. In a study conducted by Yu et al. (2023), on the effects of virtual audience feedback on the performance of elderly users in VR-based exercise games, they found that it significantly improved their ability to perform complex gestures and gesture combinations, while having no effect on users levels of physical exertion. In response, the authors suggested that providing patients with more options to select and customize the types of gestures and movements possible in the system might help to increase its positive effects, rather than trying to design a perfect one-size-fits-all experience or interface. In these terms, rather than re-designing the system to restrict agency, it would be more beneficial to provide an option menu at the beginning where the therapist can choose to activate interaction and movement tools based on the patients needs.
For the large proportion of elderly patients in palliative care who are also suffering from progressive mental and physical deterioration, Harrington et al. have proposed a number of user-centered considerations for the design of all digital health information and communication technologies Harrington et al. (2020). These include designing systems to account for impaired vision, hearing difficulties, reduced haptic sensation, decreased cognitive function as well as specific psychological needs such as senses of autonomy, competence and relatedness. Examples of adaptations to these factors affecting the elderly include re-designing the environment with less detail to account for visual acuity problems, increasing the volume of environmental and interface audio to cater to hearing impairment and adjusting the level of haptic feedback to compensate for reduced sensitivity. To respond to the needs of users with motor issues who are unable to use the controllers, we would also provide an additional ‘automated’ option where the user is guided through a passive, pre-programmed version of the system which is experienced in the same way as watching a television program or online video, but with the added elements of immersion and presence. Further to this, future updates of the system for patients with motor issues will provide a “lying down” mode, so that the scene can be viewed from a reclining position.
Another important factor which was brought up a number of times by the expert participants was the question of representational realism and its impact on the users sense of presence in the system. Several of the participants suggested that a more photo-realistic avatar, with responsive facial expressions and the ability to customize its appearance could help to improve the patients ability to emotionally identify and connect with the avatars. As mentioned, the initial decision to choose “cartoon-like” avatars was to avoid adverse reactions to the “uncanny valley effect” of realistic avatars which might inhibit the users receptiveness to the therapeutic intervention Mori (2012). However, there is a third option which straddles the divide between realism and cartoon-like representation, which is abstraction. In David Glowacki’s 2024 perspective paper “VR models of death and psychedelics: an aesthetic paradigm for design beyond day-to-day phenomenology,” which is a follow up to his 2022 study “Group VR experiences can produce ego attenuation and connectedness comparable to psychedelics,” he proposes and implements the idea that completely abstract, non-representational avatars and environments can provide an alternative approach to the design of VR systems for the dying (Glowacki et al., 2022; Glowacki, 2024). As opposed to the humanoid-type avatars found in the majority of social psychology experiments and therapies using VR, Glowacki suggests the use of amorphous, multi-colored clouds of light for self-representation in virtual environments. Not only does the use of these abstracted avatars exploit the imaginary potential of VR to create ‘awe’ inspiring environments which can further heighten the users experience, it also accords with the phenomenological descriptions of bodies perceived during near-death-experiences (NDE’s). In addition, by using abstract, non-humanoid avatars the VR system could create a stronger sense of connection between the therapist and patient by eliding the visible boundaries between their virtual selves. The VR environments of the systems designed by Glowacki and his colleagues are also not traditionally realistic, but views of the “cosmos” from outer space, which can further help to generate an “awe-inspiring” and “spiritual” experience for the patient. Notwithstanding these design advantages, it is pertinent to consider the potential drawbacks of incorporating luminous imagery based on NDE’s, particularly the possibility that it may evoke the experience of dying or the afterlife for patients under palliative care, or be associated with common religious or folk depictions of disembodied ethereal souls or ghosts, and further increase their psychological distress. In addition, without the possibility to anthropomorphize and emotionally connect with a humanoid avatar, patients might feel disconnected from the environment. Nonetheless, these alternative visual representation strategies are worth exploring in future, user-based participatory design research.
Considering the vulnerabilities of patients in palliative care, any VR system must be designed with utmost consideration for its appropriateness regarding content and interface usability from the point-of-view of the therapists who may 1 day consider adding it to their clinical toolkit but also more importantly, from the patients themselves. Our next step is to conduct a pilot study to assess the effectiveness of our VR life review therapy system with elderly patients in Hong Kong, a demographic similar to patients in palliative care who also face physical deterioration and isolation. We are particularly interested in what factors might help contribute to elderly and dying patients accepting VR based therapies, and plan to utilize a mixed methods approach combining the qualitative methodology adopted in the present study with quantitative measures. Specifically, by using the Technology Acceptance Model (TAM) originally proposed by Davis Davis (1989) which examines the three core factors of perceived usefulness, perceived ease of use and user acceptance, we can systematically determine whether our VR life review therapy system can be accepted by our target user groups. In addition, we will also take into consideration socio-cultural factors as facilitators and barriers to technology acceptance, by using the adaptations of the TAM model to elderly Chinese populations proposed by Peng et al. (2023) which incorporate additional factors which influence acceptance including perceived incentives, the support of family and friends, social relationships, self-satisfaction, education, economic status and personal factors.
4.1 Conclusion
We hope that this study will set the stage for a full clinical trial to implement our VR life review therapy system in the Hong Kong hospital system as a novel and effective therapeutic tool for therapists which can improve the psychological wellbeing of patients under palliative care in the last chapter of their lives.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Research Office of the City University of Hong Kong. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
RN: Conceptualization, Software, Writing–original draft, Writing–review and editing, Methodology. OW: Conceptualization, Investigation, Methodology, Writing–review and editing. DE: Conceptualization, Methodology, Software, Writing–original draft, Writing–review and editing. MZ: Software, Writing–review and editing. AL: Supervision, Writing–review and editing. AC: Conceptualization, Funding acquisition, Supervision, Writing–original draft, Writing–review and editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was supported by the Augmented Materiality Lab, School of Creative Media, City University of Hong Kong. Space and funds were provided by grants from the Center for Applied Computing and Interactive Media (ACIM) and Inter-institutional Collaborative Activities for Virtual Teaching and Learning (No. 6430910), University Grants Committee (UGC) of Hong Kong.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Allen, R. S., Hilgeman, M. M., Ege, M. A., Shuster, J. L., and Burgio, L. D. (2008). Legacy Activities as interventions approaching the end of life. J. Palliat. Med. 11, 1029–1038. doi:10.1089/jpm.2007.0294
Ando, M., Tsuda, A., and Moorey, S. (2006). Preliminary study of reminiscence therapy on depression and self-esteem in cancer patients. Psychol. Rep. 98, 339–346. doi:10.2466/pr0.98.2.339-346
Baños, R. M., Espinoza, M., García-Palacios, A., Cervera, J. M., Esquerdo, G., Barrajón, E., et al. (2013). A positive psychological intervention using virtual reality for patients with advanced cancer in a hospital setting: a pilot study to assess feasibility. Support. Care Cancer 21, 263–270. doi:10.1007/s00520-012-1520-x
Beng, T. S., Kim, C. L. C., Shee, C. C., Ching, D. N. L., Liang, T. J., Kumar, M. K. N., et al. (2022). COVID-19, suffering and palliative care: a review. Am. J. Hospice Palliat. Medicine® 39, 986–995. doi:10.1177/10499091211046233
Blomstrom, M., Burns, A., Larriviere, D., and Penberthy, J. K. (2022). Addressing fear of death and dying: traditional and innovative interventions. Mortality 27, 18–37. doi:10.1080/13576275.2020.1810649
Brungardt, A., Wibben, A., Tompkins, A. F., Shanbhag, P., Coats, H., LaGasse, A. B., et al. (2021). Virtual reality-based music therapy in palliative care: a pilot implementation trial. J. Palliat. Med. 24, 736–742. doi:10.1089/jpm.2020.0403
Chang, E., Kim, H. T., and Yoo, B. (2020). Virtual reality sickness: a review of causes and measurements. Int. J. Human–Computer Interact. 36, 1658–1682. doi:10.1080/10447318.2020.1778351
Chirico, A., Cipresso, P., Yaden, D. B., Biassoni, F., Riva, G., and Gaggioli, A. (2017). Effectiveness of immersive videos in inducing awe: an experimental study. Sci. Rep. 7, 1218. doi:10.1038/s41598-017-01242-0
Dang, M., Noreika, D., Ryu, S., Sima, A., Ashton, H., Ondris, B., et al. (2021). Feasibility of delivering an avatar-facilitated life review intervention for patients with cancer. J. Palliat. Med. 24, 520–526. doi:10.1089/jpm.2020.0020
Davis, F. D. (1989). Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 13, 319. doi:10.2307/249008
Ferguson, C., Shade, M. Y., Blaskewicz Boron, J., Lyden, E., and Manley, N. A. (2020). Virtual reality for therapeutic recreation in dementia hospice care: a feasibility study. Am. J. Hospice Palliat. Med. 37, 809–815. doi:10.1177/1049909120901525
Glowacki, D. R. (2024). VR models of death and psychedelics: an aesthetic paradigm for design beyond day-to-day phenomenology. Front. Virtual Real. 4, 1286950. doi:10.3389/frvir.2023.1286950
Glowacki, D. R., Williams, R. R., Wonnacott, M. D., Maynard, O. M., Freire, R., Pike, J. E., et al. (2022). Group VR experiences can produce ego attenuation and connectedness comparable to psychedelics. Sci. Rep. 12, 8995. doi:10.1038/s41598-022-12637-z
Groninger, H., Stewart, D., Fisher, J. M., Tefera, E., Cowgill, J., and Mete, M. (2021). Virtual reality for pain management in advanced heart failure: a randomized controlled study. Palliat. Med. 35, 2008–2016. doi:10.1177/02692163211041273
Harrington, C. N., Koon, L. M., and Rogers, W. A. (2020). “Design of health information and communication technologies for older adults,” in Design for health (Elsevier), 341–363. doi:10.1016/B978-0-12-816427-3.00017-8
Johnson, T., Bauler, L., Vos, D., Hifko, A., Garg, P., Ahmed, M., et al. (2020). Virtual reality use for symptom management in palliative care: a pilot study to assess user perceptions. J. Palliat. Med. 23, 1233–1238. doi:10.1089/jpm.2019.0411
Kopeć, W., Wichrowski, M., Kalinowski, K., Jaskulska, A., Skorupska, K., Cnotkowski, D., et al. (2019). VR with older adults: participatory design of a virtual ATM training simulation. IFAC-PapersOnLine 52, 277–281. doi:10.1016/j.ifacol.2019.12.110
Manetta, C., and Blade, R. A. (1995). Glossary of virtual reality terminology. Int. J. Virtual Real. 1, 35–39. doi:10.20870/IJVR.1995.1.2.2604
Mo, J., Vickerstaff, V., Minton, O., Tavabie, S., Taubert, M., Stone, P., et al. (2022). How effective is virtual reality technology in palliative care? A systematic review and meta-analysis. Palliat. Med. 36, 1047–1058. doi:10.1177/02692163221099584
Mori, M. (2012). The uncanny valley: the original essay by masahiro Mori - IEEE spectrum. IEEE Spectr. doi:10.1109/MRA.2012.2192811
Niki, K., Okamoto, Y., Maeda, I., Mori, I., Ishii, R., Matsuda, Y., et al. (2019). A novel palliative care approach using virtual reality for improving various symptoms of terminal cancer patients: a preliminary prospective, multicenter study. J. Palliat. Med. 22, 702–707. doi:10.1089/jpm.2018.0527
Peng, L., Man, S. S., Chan, A. H. S., and Ng, J. Y. K. (2023). Personal, social and regulatory factors associated with telecare acceptance by Hong Kong older adults: an indication of governmental role in facilitating telecare adoption. Int. J. Human–Computer Interact. 39, 1059–1071. doi:10.1080/10447318.2022.2050539
Perna, L., Lund, S., White, N., and Minton, O. (2021). The potential of personalized virtual reality in palliative care: a feasibility trial. Am. J. Hospice Palliat. Medicine® 38, 1488–1494. doi:10.1177/1049909121994299
Roulston, A., Gerson, S. M., Csikai, E., and Dobrikova, P. (2023). How did the COVID-19 pandemic affect palliative care social work services? A scoping review. Br. J. Soc. Work 53, 2878–2901. doi:10.1093/bjsw/bcad042
J. Simonsen, and T. Robertson (2012). Routledge international handbook of participatory design. 0 edn (New York, NY: Routledge). doi:10.4324/9780203108543
Slater, M. (2009). Place illusion and plausibility can lead to realistic behaviour in immersive virtual environments. Philosophical Trans. R. Soc. B Biol. Sci. 364, 3549–3557. doi:10.1098/rstb.2009.0138
Tominari, M., Uozumi, R., Becker, C., and Kinoshita, A. (2021). Reminiscence therapy using virtual reality technology affects cognitive function and subjective well-being in older adults with dementia. Cogent Psychol. 8, 1968991. doi:10.1080/23311908.2021.1968991
Yu, K., Wen, S., Xu, W., Caon, M., Baghaei, N., and Liang, H.-N. (2023). Cheer for me: effect of non-player character audience feedback on older adult users of virtual reality exergames. Virtual Real. 27, 1887–1903. doi:10.1007/s10055-023-00780-5
Zee, M. S., Bagchus, L., Becqué, Y. N., Witkamp, E., Van Der Heide, A., Van Lent, L. G. G., et al. (2023). Impact of COVID-19 on care at the end of life during the first months of the pandemic from the perspective of healthcare professionals from different settings: a qualitative interview study (the CO-LIVE study). BMJ Open 13, e063267. doi:10.1136/bmjopen-2022-063267
Keywords: virtual reality, palliative care, life review therapy, reminiscence therapy, participatory design
Citation: Ng R, Woo OKL, Eckhoff D, Zhu M, Lee A and Cassinelli A (2024) Participatory design of a virtual reality life review therapy system for palliative care. Front. Virtual Real. 5:1304615. doi: 10.3389/frvir.2024.1304615
Received: 29 September 2023; Accepted: 02 May 2024;
Published: 15 May 2024.
Edited by:
Carine Khalil, Université Paris Cité, FranceReviewed by:
Hai-Ning Liang, Xi’an Jiaotong-Liverpool University, ChinaVangelis Lympouridis, University of Southern California, United States
Copyright © 2024 Ng, Woo, Eckhoff, Zhu, Lee and Cassinelli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Royce Ng, soloroyce@gmail.com
 Royce Ng
Royce Ng Olive Kit Ling Woo
Olive Kit Ling Woo Daniel Eckhoff
Daniel Eckhoff Mengyao Zhu1
Mengyao Zhu1