- 1College of Health Science, Oda Bultum University, Chiro, Ethiopia
- 2School of Public Health, College of Health and Medical Sciences, Mizan-Tepi University, Mizan-Aman, Ethiopia
Background: Cultural malpractices are accepted cultural norms and socially shared practices that have a negative impact on health. Cultural malpractices vary in type and number in different communities. This study aimed to determine the prevalence of cultural malpractice during the perinatal period and identify its predictors among reproductive-age women in rural communities of southwestern Ethiopia.
Methods: A community-based cross-sectional study was conducted from May 5 to 31, 2019 in Semen Bench district, southwestern Ethiopia; among reproductive-age women who had experienced at least one prior delivery. A systematic random sampling technique was employed to select 422 women for the interview. After collection, the data were entered into EpiData and exported to STATA-14 for further analysis. Descriptive analyses were performed and presented in texts and tables. Besides, binary and multivariable logistic regressions were computed to identify determinants of cultural malpractice.
Result: A total of 414 women completed the survey, resulting in a response rate of 98%. We found that 26.33% (95% CI: 22.15, 30.85%) had food taboos during pregnancy, 31.88% (95% CI: 27.42, 36.61%) delivered their last child at home, and 33.82% (95% CI: 29.27, 38.6%) practiced pre-lacteal feeding. Lack of formal education (AOR: 11.22, 95% CI: 6.24, 20.15), lack of ANC follow-up (AOR: 10.82, 95% CI: 5.46, 21.42), rural residence (AOR: 6.23, 95% CI: 2.18, 17.78), and avoiding colostrum (AOR: 21.94, 95% CI: 9.73, 49.48) were significantly associated with cultural malpractice during the perinatal period.
Conclusion: The prevalence of cultural malpractice is notably high in the study area. Hence, community-based measures including expansion of education and promotion of maternal health services are important to reduce cultural malpractice during the perinatal period.
Introduction
Different communities have socially shared practices that are deeply rooted in their culture and have an important association with their health (1). Cultural malpractices are accepted cultural norms and socially shared practices that have a negative impact on health (2, 3). The perinatal period, which includes pregnancy, delivery, and the post-natal period, is accompanied by various cultural malpractices that substantially affect the health of the mother and her children (4, 5).
Globally, several types of cultural malpractices have been reported (2, 6, 7). Ethiopia, as a multi-ethnic nation, is one of the countries where assorted cultural malpractices particularly during pregnancy, delivery, and post-natal period are practiced; among these, home delivery, pre-lacteal feeding, food prohibition, abdominal massage, and avoiding of colostrum were commonly documented (5, 8–11). Bench Maji Zone is also a home for such malpractices where home delivery, food prohibition, pre-lacteal feeding, and abdominal massage are commonly exercised (8, 12). These malpractices were found to have a significant association with residence, educational status, antenatal care (ANC) follow-up, gravidity, and distance from the health facility (5, 10, 13–15).
Cultural malpractices not only hinder women from utilizing maternal, reproductive, and child health services, but they also have a direct impact on the wellbeing and survival of both the mother and her offspring (2, 7, 16). Previously, studies have concentrated on the biomedical causes and management of maternal death; yet, they ignored cultural and traditional practices that can deter maternal morbidity and mortality (6, 17).
Maternal mortality is extremely high worldwide, accounting for 295,000 pregnancy-related deaths in 2017; almost all (94%) of these deaths occurred in resource-constrained settings (18, 19). Ethiopia is one of the nations where a higher number of maternal deaths are reported; a recent demographic and health survey estimated that there were around 412 maternal deaths per 100,000 live births (20). Various strategies, like improving access to reproductive health care and maternal death surveillance and response systems, have been implemented to reduce maternal mortality in Ethiopia; however, it persists as a major public health concern (21, 22). Cultural malpractices are among the important contributors to the high maternal mortality rate (23). It is estimated that about 5–15% of maternal deaths are due to cultural malpractice (6, 10, 24).
Cultural malpractices vary in type and number across different communities (8, 9, 25, 26). Thus, comprehensive evidence about the magnitude and determinant factors of cultural malpractices, especially during the perinatal period across different societies is crucial to reduce maternal mortality. Hence, this study was conducted to determine the prevalence of cultural malpractice during the perinatal period and identify associated factors among reproductive-age women in rural communities of Semen Bench district, southwestern Ethiopia.
Materials and methods
Study area, design, and period
A community-based, cross-sectional study was conducted from May 5 to 31, 2019 in the Semen Bench district. It is one of the ten decentralized districts in the Bench Maji zone, Southern Nation, Nationalities, and Peoples Region (SNNP) of Ethiopia. The district is composed of thirty-one Kebeles (the smallest administrative unit in Ethiopia), of which twenty-eight were rural. The estimated total population of the district was 159,480; of which 87,748 (51.26%) were females; the majority of the population in the district (152,973) are rural residents, with agriculture serving as their main economic source (27). There are four health centers and thirty-one health posts that provide maternal and child health services in the district.
Study participants
Source population
All reproductive-age women in the Semen Bench district who had experienced at least one prior delivery.
Study population
All reproductive-age women in randomly selected kebeles of the Semen Bench district who had experienced at least one prior delivery.
Inclusion criteria
All women who had experienced at least one delivery and were available during the period of data collection were included in the study.
Exclusion criteria
Women who were seriously ill and/or had difficulties to communicate were excluded.
Sample size determination and sampling procedure
The sample size was determined based on the single population proportion formula considering a 95% confidence interval, 5% margin of error, and cultural malpractice proportion of 50.9% from a previous study (28).
where,
n = is the desired sample size.
Zα/2 = the value of standard normal distribution corresponding to the significance level at α of 5%, which is 1.96.
P = is the proportion of cultural malpractice.
Therefore,
Adding 10% non-response; n = 384 + (10*384/100) = 422.
Therefore, the final sample size for the study was 422 women of reproductive age.
Out of the thirty-one kebeles in the district, seven kebeles (one urban and six rural) were randomly selected. The study participants were recruited using systematic random sampling by considering household lists of randomly selected kebeles as sampling frames. For a household without eligible women, the next household was considered. Conversely, for households with more than one eligible woman, one of the women was selected randomly (Figure 1).
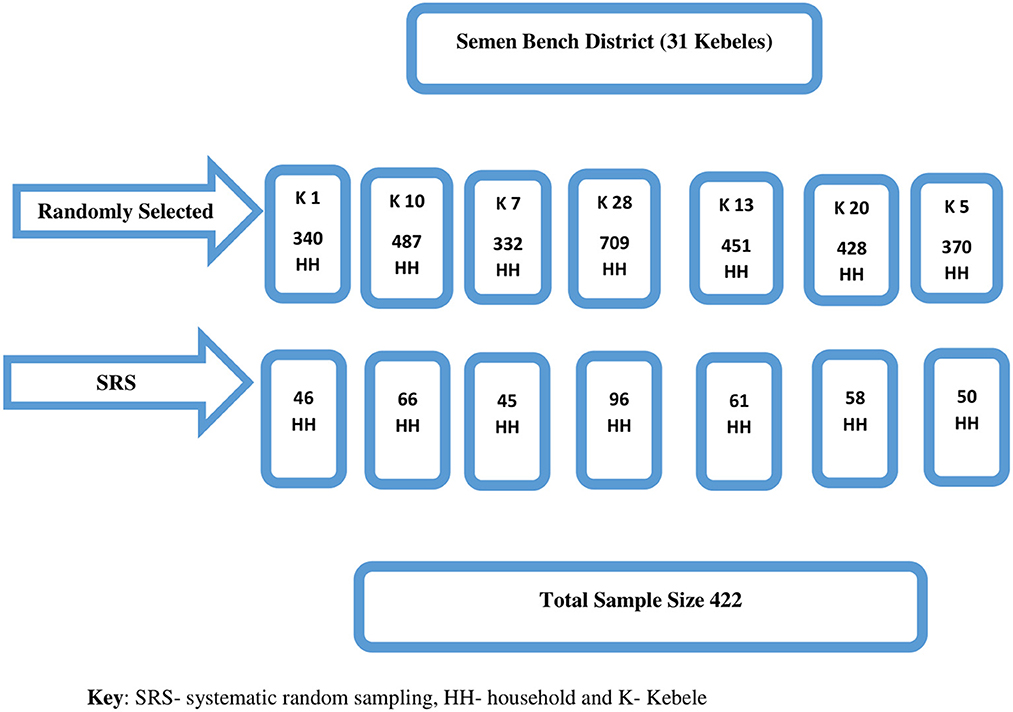
Figure 1. Schematic presentation of the sampling procedure to assess cultural malpractice during the perinatal period in southwest Ethiopia.
Data collection tool, procedure, and quality control
A structured questionnaire (see Supplementary material), that was adapted from different literature was used (10, 11, 28). A face-to-face interview was employed to collect the data through house to house survey. The data were collected by seven midwives and they were supervised by two public health professionals. To assure the quality of the study, 2 days training was given to data collectors and supervisors about the objectives of the study and techniques of data collection. The tool was also pretested on 5% of the calculated sample size in one of the kebeles not included in this study. Furthermore, the collected data were checked every day for quality, completeness, and consistency.
Operational definitions
Perinatal period: denotes the period during pregnancy, delivery, and postnatal period (5).
Cultural malpractice: accepted cultural practices that have a negative impact on health (5, 10).
Food taboo: avoiding certain foods during some occasions, like pregnancy, due to cultural beliefs (3, 10).
Pre-lacteal feeding: feeding the neonate something other than breast milk in the first 3 days after birth (29).
Data processing and analysis
The collected data were entered into EpiData and exported to STATA version 14 for cleaning, categorizing, and further statistical analysis. Consequently, descriptive and inferential statistics were computed using the software. The bi-variable and multi-variable logistic regressions were employed to identify factors associated with cultural malpractice after checking for assumptions and assessing multicollinearity. Variables with a P-value ≤ 0.25 during bi-variable analyses were chosen for subsequent multi-variable logistic regression. In the multi-variable analysis, significant statistical association was declared at a P-value < 0.05. Besides, the Hosmer-Lemeshow goodness-of-fit test and classification table were used to verify the fitness of the final models.
Results
Socio-demographic characteristics of participants
From the total calculated sample size of 422 reproductive-age women, 414 women completed the survey resulting in a response rate of 98%. Almost two out of every five women had no formal education. More than two-thirds of the respondents were rural dwellers. Most (84.3%) of the women were married, and the rest were either widowed (11.8%) or divorced (3.9%). More than half of the participants were housewives (Table 1).
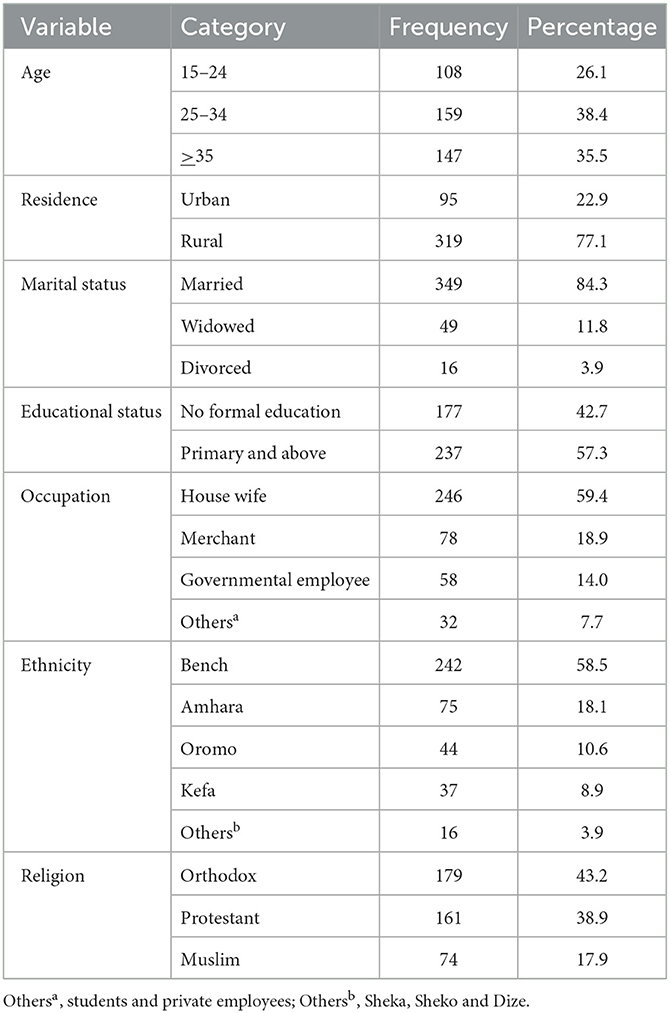
Table 1. Socio-demographic characteristics of study participants to assess cultural malpractice during the perinatal period in southwest Ethiopia.
Obstetrical characteristics of participants
Among the participants, 178 had an antenatal care (ANC) follow-up. About one-third (35.3%) of the women had an illness during their last pregnancy. Most of the home deliveries were attended by families, and about one-fourth of women avoided feeding colostrum (Table 2).
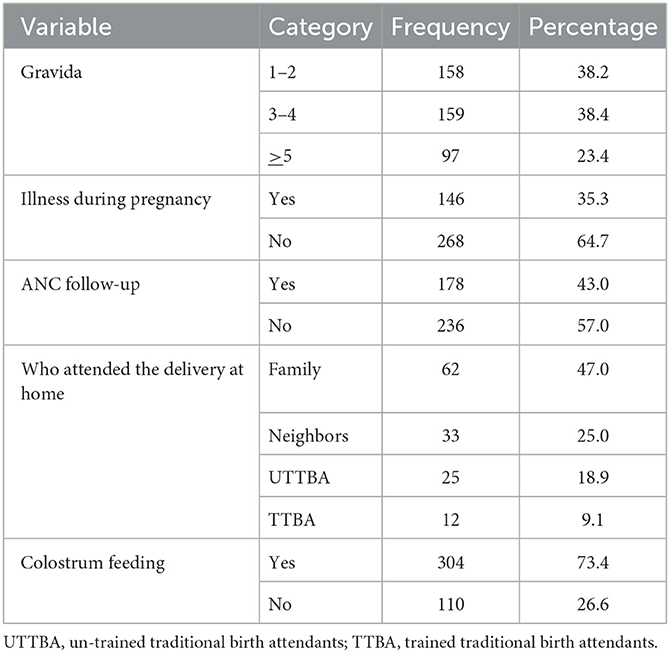
Table 2. Obstetrical characteristics of study participants to assess cultural malpractice during the perinatal period in southwest Ethiopia.
Prevalence of cultural malpractice
Out of 414 women who completed this survey; 26.33% (95% CI: 22.15, 30.85%) had food restrictions during pregnancy, 31.88% (95% CI: 27.42, 36.61%) delivered their last child at home, and 33.82% (95% CI: 29.27, 38.6%) practiced pre-lacteal feeding on their newborn. Other cultural malpractices like abdominal massage, uterine massage, using an unclean blade to cut the umbilical cord, shaking of the abdomen or uterus, applying cow dung or butter on the umbilical stump, late initiation of breastfeeding, and avoiding the colostrum were also reported (Figure 2).
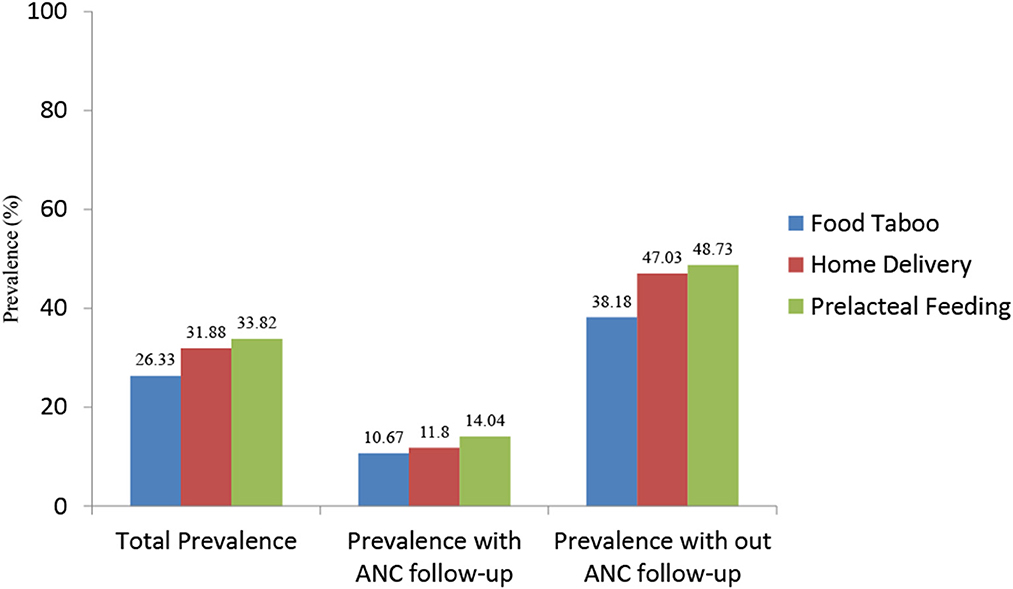
Figure 2. Prevalence of cultural malpractice during the perinatal period, by ANC follow-up status of women in southwest Ethiopia.
Factors associated with cultural malpractice
Various factors were found to have a statistically significant association with the most commonly reported cultural malpractices (food taboo, home delivery, and pre-lacteal feeding).
Factors associated with food taboo: residence, educational status, and ANC follow-up were significantly associated with food taboo during pregnancy. Accordingly, rural dwellers were 2.25 (95% CI: 1.15, 4.38) times at higher risk of food taboo than urban residents. Similarly, women who did not attend formal education were having a 2.25 (95% CI: 1.15, 4.38) times higher risk of food taboo as compared to women who attended primary and above education. The odds of food taboo were 4.56 (95% CI: 2.61, 7.97) times higher among women who did not have ANC follow-up than among women who had (Table 3).
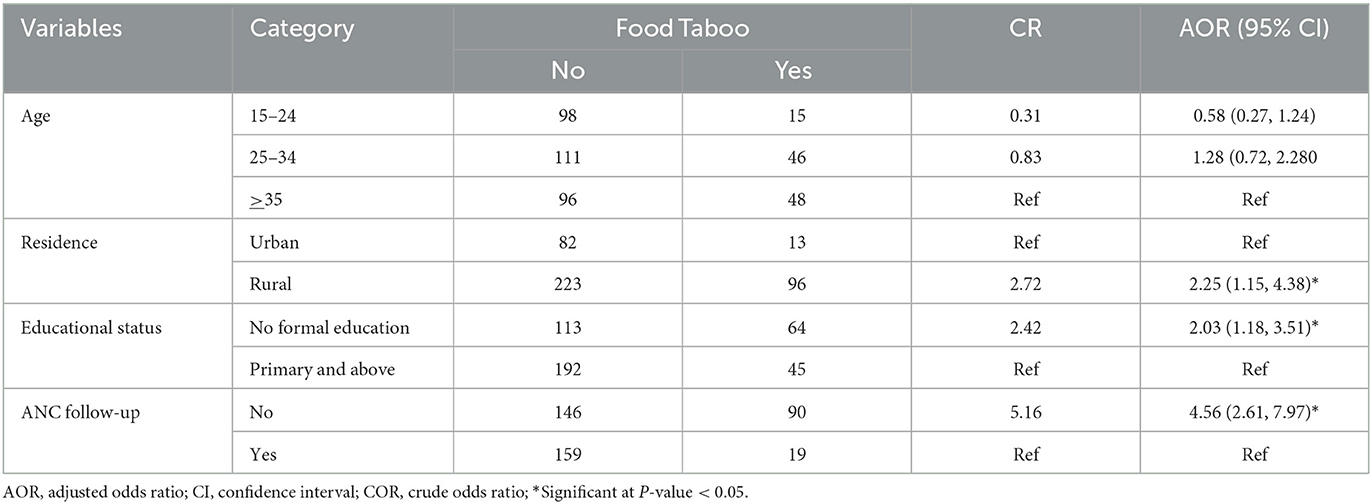
Table 3. Factors associated with food taboo during pregnancy among reproductive age women in southwest Ethiopia.
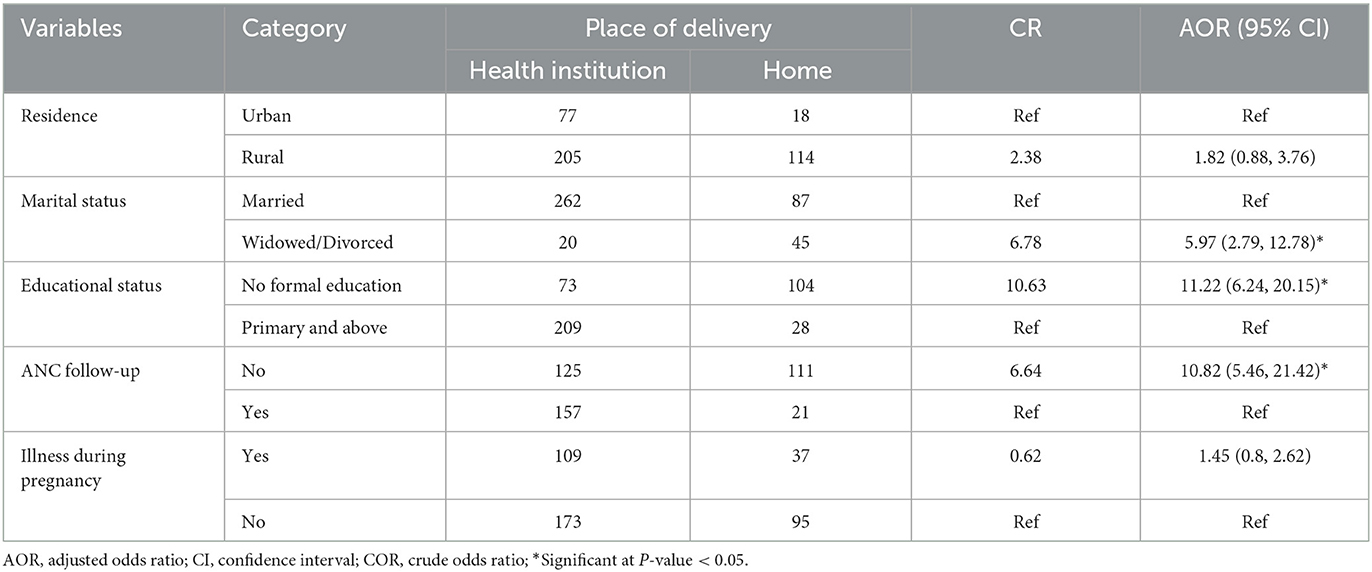
Factors associated with home delivery: marital status, educational status, and ANC follow-up significantly determined home delivery practice. Widowed and divorced women had a 5.97 (95% CI: 2.79, 12.78) times higher risk of home delivery than married ones. Women with no formal education were 11.22 (95% CI: 6.24, 20.15) times more likely to give birth at home as compared to women who attended primary and above education. Likewise, women who didn't have ANC follow-up were having a 10.82 (95% CI: 5.46, 21.42) times higher risk of home delivery than women who had ANC follow-up (Table 4).
Factors associated with pre-lacteal feeding: rural dwellers were 6.23 (95% CI: 2.18, 17.78) times more likely to practice pre-lacteal feeding than urban residents. Respondents who were Amhara in their ethnicity were 4.94 (95% CI: 2.09, 11.66) times more likely to practice pre-lacteal feeding than Bench ethnic groups. Similarly, women who didn't attend formal education had a 6.30 (95% CI: 2.67, 14.87) times higher risk of pre-lacteal feeding as compared to women who attended primary and above education. Women who had five or more gravida were 7.17 (95%: 2.95, 17.44) times more likely to practice pre-lacteal feeding than women who had fewer gravida. Likewise, women who didn't have ANC follow-up were having 6.73 (95% CI: 3.1, 14.61) times higher risk of pre-lacteal feeding as compared to women who had ANC follow-up. Women who avoided feeding colostrum to their newborns were 21.94 (95% CI: 9.73, 49.48) times more likely to practice pre-lacteal feeding than their counterparts (Table 5).
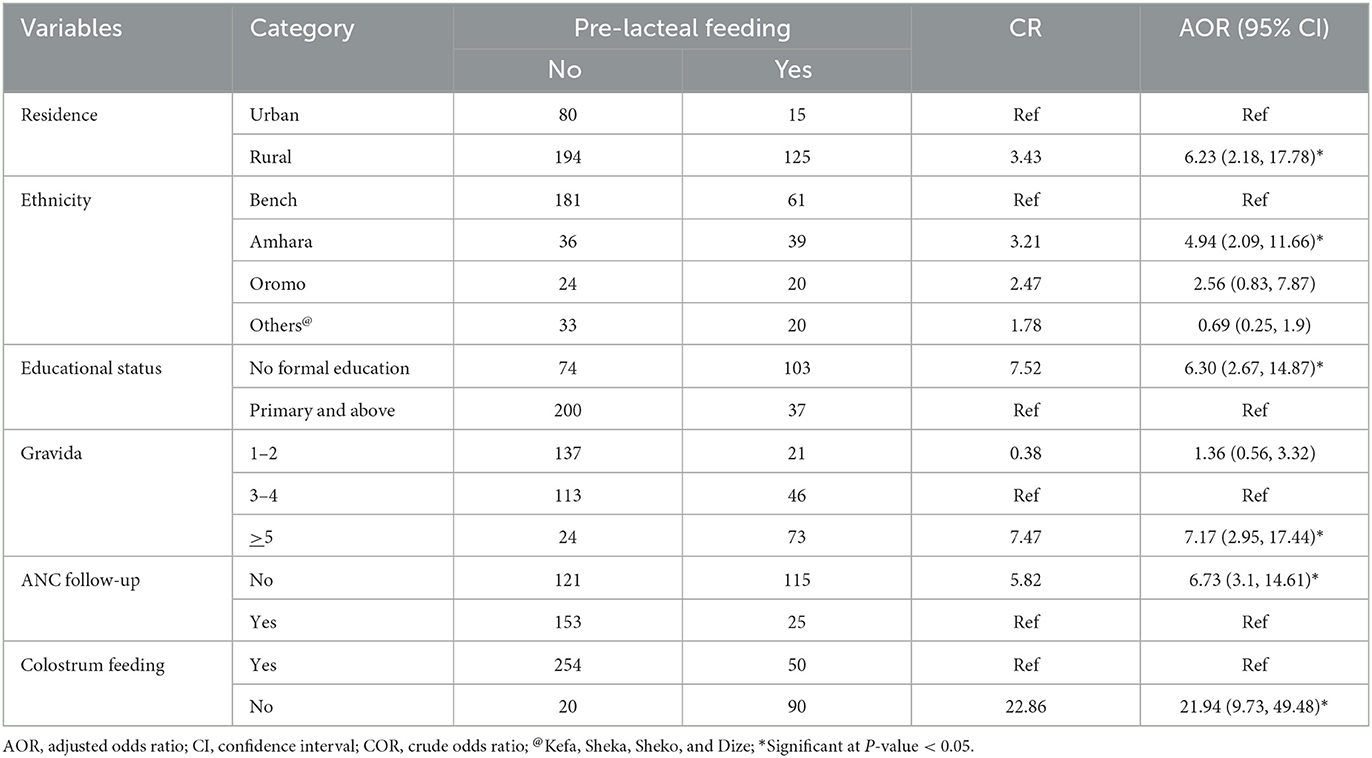
Table 5. Factors associated with pre-lacteal feeding among reproductive age women in southwest Ethiopia.
Discussion
This study was conducted to estimate the prevalence of cultural malpractice during the perinatal period and identify factors associated with it among reproductive-age women in rural communities of southwest Ethiopia. Consequently, the prevalence of food taboo during pregnancy, home delivery, and pre-lacteal feeding were 26.33, 31.88, and 33.82% respectively. Besides; residence, marital status, educational status, ANC follow-up, gravidity, and avoidance of colostrum were found to have a significant association with cultural malpractices.
We found that the prevalence of food taboo during pregnancy was 26.33% (95% CI: 22.15, 30.85%). This finding was higher than previous reports from different parts of Ethiopia (10, 11, 28, 30). The possible explanation could be due to differences in residence and period of study. Previous studies were conducted among urban dwellers whereas the current study mainly included rural women. Besides, this study estimated food taboos during pregnancy, whereas the previous studies investigated food taboos during delivery and the postnatal period. On the other hand, this finding was lower than previous researches from Ethiopia (5, 31), and Nepal (25). This could be partly because of socio-cultural variations.
Our study also found that the prevalence of home delivery was 31.88% (95% CI: 27.42, 36.61%). This result was higher than previous reports in Ethiopia (13, 15, 32). This might be due to the difference in the study setting; the previous studies were institutional based while our study was community-based. However, our finding was lower than studies conducted in the Afar and Benishangul Gumuz Regions of Ethiopia (33–36). The possible explanation could be due to the poor infrastructure in the underserved regions of the country, thus leading to poor access to health care.
Furthermore, this analysis indicated that the prevalence of pre-lacteal feeding was 33.82% (95% CI: 29.27, 38.6%). This finding is lower than previous researches conducted in the same country (37–39), this might be due to the difference in time of study; these studies were conducted in earlier times when access and quality of health care were relatively suboptimal. In contrast, our finding was higher than previous reports from various parts of Ethiopia (40–43). This might be attributed to the socio-cultural variation across the country.
Moreover, we also identified determinants of cultural malpractice among reproductive-age women in southwest Ethiopia. Accordingly, ANC follow-up and educational status had a consistent association with the identified cultural malpractices. In line with previous studies, women who didn't have ANC follow-up had a higher risk of food taboo, home delivery, and pre-lacteal feeding (5, 10, 34). This might be attributed to the effect of counseling and client education during ANC (43, 44). Similarly, women with no formal education were more likely to practice food taboos, home delivery, and pre-lacteal feeding than women with primary and above education. This association was documented elsewhere (5, 10, 13, 15, 29), and could be related to the lack of awareness about the harmful effect of cultural malpractices on the health of the mother and her offspring among women without formal education.
The results of this study indicated that residence is significantly associated with food taboos during pregnancy and pre-lacteal feeding. Rural residents were having a higher risk of food taboo and pre-lacteal feeding than urban women. This finding was also reported by previous studies (5, 10, 45). One possible explanation is that rural residents have limited access to health care and are less exposed to health information (42, 46).
Our study also identified that marital status is significantly associated with home delivery. Divorced and/or widowed women had a higher risk of home delivery as compared to married women. This association was also supported by previous reports (47, 48), and might be due to the enabling effect of partner support on improving maternal and reproductive health care service utilization (49, 50).
This study revealed that respondents who were Amhara in their ethnicity were more likely to practice pre-lacteal feeding than Bench ethnic groups. This could be partly due to the difference in socio-cultural attributes between the two ethnic groups. Consistent with previous studies, women who have had five or more gravidity were more likely to practice pre-lacteal feeding than their counterparts (5, 26). This could be due to the higher prevalence of cultural beliefs among older women. Lastly, we found that avoiding the colostrum was strongly associated with pre-lacteal feeding. This association was documented elsewhere (29, 43, 51) and might be due to the misconception among mothers that colostrum is non-nutritious and causes diarrhea (52).
Limitations
The findings of this study should be interpreted considering the following limitations. Firstly, as we investigated events that occurred in the past, recall bias could not be ruled out. Secondly, the cross-sectional nature of the study makes it difficult to establish a temporal association.
Conclusion
The prevalence of cultural malpractice is notably high in the study area. Educational status, ANC follow-up, residence, marital status, gravidity, and avoiding colostrum had a significant association with cultural malpractices during the perinatal period. Hence, community-based measures, including the expansion of education and promotion of maternal health services are important to reduce cultural malpractice during the perinatal period.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical clearance was obtained from the College of Health Science, Mizan-Tepi University Ethical Review Board. Considering the non-invasive nature of data collection procedures, verbal consent was obtained from each woman who participated in the survey after a detailed explanation of the purpose of the research and the right to withdraw from the study at any time. For women who practiced cultural malpractice, detailed descriptions of possible health consequences and appropriate alternative measures were discussed by data collectors. Besides, confidentiality was assured by not recording personal identifiers and using the data only for the purpose of this study.
Author contributions
ATD conceived the study. ATD, DAF, and HG designed the study, supervised data collection, analyzed the data, wrote the first draft, and critically reviewed the manuscript. All authors have read and approved the final manuscript.
Acknowledgments
We are thankful to Mizan-Tepi University, College of Health Sciences for granting the ethical clearance. We would also like to acknowledge the study participants, data collectors, and supervisors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1064583/full#supplementary-material
Abbreviations
ANC, antenatal care; AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio.
References
1. Gurung RA. Cultural influences on health. Cross Cult Psychol Contemp Themes Perspect. (2019) 15:451–66. doi: 10.1002/9781119519348.ch21
2. Wells Y-O, Dietsch E. Childbearing traditions of Indian women at home and abroad: an integrative literature review. Women Birth. (2014) 27:e1–6. doi: 10.1016/j.wombi.2014.08.006
3. Ebabu A, Muhammed M. Traditional practice affecting maternal health in pastoralist community of afar region, Ethiopia: a facility-based cross-sectional study. J Midwifery Reprod Health. (2021) 9:2817–27. doi: 10.22038/JMRH.2021.46790.1575
4. Chand S. Cultural beliefs and traditional rituals about child birth practice in rural, Nepal. MOJ Public Health. (2016) 5:00106. doi: 10.15406/mojph.2016.04.00106
5. Abebe H, Beyene GA, Mulat BS. Harmful cultural practices during perinatal period and associated factors among women of childbearing age in Southern Ethiopia: community based cross-sectional study. PLoS ONE. (2021) 16:e0254095. doi: 10.1371/journal.pone.0254095
6. Marabele PM, Maputle MS, Ramathuba DU, Netshikweta L. Cultural factors contributing to maternal mortality rate in rural villages of Limpopo Province, South Africa. Int J Women's Health. (2020) 12:691–9. doi: 10.2147/IJWH.S231514
7. Ugboma H, Akani C. Abdominal massage: another cause of maternal mortality. Nigerian J Med J Natl Assoc Resid Doctors Nigeria. (2004) 13:259–62.
8. Solomon N, Tesfaye M. Traditional practices during pregnancy and childbirth among mothers in Shey Bench District, South West Ethiopia. SAGE Open Med. (2022) 10:20503121221098139. doi: 10.1177/20503121221098139
9. Tsegaye D, Tamiru D, Belachew T. Food-related taboos and misconceptions during pregnancy among rural communities of Illu Aba Bor zone, Southwest Ethiopia. A community based qualitative cross-sectional study. BMC Pregn Childbirth. (2021) 21:309. doi: 10.1186/s12884-021-03778-6
10. Melesse MF, Bitewa YB, Dessie KN, Wondim DB, Bereka TM. Cultural malpractices during labor/delivery and associated factors among women who had at least one history of delivery in selected Zones of Amhara region, North West Ethiopia: community based cross-sectional study. BMC Pregn Childbirth. (2021) 21:504. doi: 10.1186/s12884-021-03971-7
11. Tola TN, Tadesse AH. Cultural malpractices during pregnancy, child birth and postnatal period among women of child bearing age in Limmu Genet Town, Southwest Ethiopia. Sci J Public Health. (2015) 3:752–6. doi: 10.11648/j.sjph.20150305.32
12. Henok A, Takele E. Assessment of barriers to reproductive health service utilization among Bench Maji Zone Pastoralist Communities. Ethiop J Health Sci. (2017) 27:523–30. doi: 10.4314/ejhs.v27i5.11
13. Hailu D, Tadele H, Tadesse BT, Alemayehu A, Abuka T, Woldegebriel F, et al. Home delivery practice and its predictors in South Ethiopia. PLoS ONE. (2021) 16:e0254696. doi: 10.1371/journal.pone.0254696
14. Ayenew AA, Nigussie AA, Zewdu BF. Childbirth at home and associated factors in Ethiopia: a systematic review and meta-analysis. Arch Public Health Arch Belges de Sante Publique. (2021) 79:48–48. doi: 10.1186/s13690-021-00569-5
15. Siyoum M, Astatkie A, Mekonnen S, Bekele G, Taye K, Tenaw Z, et al. Home birth and its determinants among antenatal care-booked women in public hospitals in Wolayta Zone, southern Ethiopia. PLoS ONE. (2018) 13:e0203609. doi: 10.1371/journal.pone.0203609
16. Turner C, Pol S, Suon K, Neou L, Day NP, Parker M, et al. Beliefs and practices during pregnancy, post-partum and in the first days of an infant's life in rural Cambodia. BMC Pregn Childbirth. (2017) 17:1–8. doi: 10.1186/s12884-017-1305-9
17. Geller SE, Goudar SS, Adams MG, Naik VA, Patel A, Bellad MB, et al. Factors associated with acute postpartum hemorrhage in low-risk women delivering in rural India. Int J Gynaecol Obstet Off Organ Int Feder Gynaecol Obstet. (2008) 101:94–9. doi: 10.1016/j.ijgo.2007.08.025
19. WHO UNFPA World Bank Group and the United Nations Population Division. Trends in maternal mortality 2000–2017: estimates by WHO, UNICEF. In: UNFPA, World Bank Group and the United Nations Population Division. Geneva: WHO (2019).
20. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland: CSA and ICF (2016).
21. Abebe B, Busza J, Hadush A, Usmael A, Zeleke AB, Sita S, et al. ‘We identify, discuss, act and promise to prevent similar deaths': a qualitative study of Ethiopia's Maternal Death Surveillance and Response system. BMJ Global Health. (2017) 2:e000199. doi: 10.1136/bmjgh-2016-000199
22. Yaya Y, Data T, Lindtjørn B. Maternal mortality in rural south Ethiopia: outcomes of community-based birth registration by health extension workers. PLoS ONE. (2015) 10:e0119321. doi: 10.1371/journal.pone.0119321
23. Evans EC, A. review of cultural influence on maternal mortality in the developing world. Midwifery. (2013) 29:490–6. doi: 10.1016/j.midw.2012.04.002
24. Central Statistical Agency [Ethiopia] and ICF International. Ethiopia Demographic and Health Survey 2011. Addis Ababa, Ethiopia and Calverton, Maryland: Central Statistical Agency and ICF International (2012).
25. Ramulondi M, de Wet H, Ntuli NR. Traditional food taboos and practices during pregnancy, postpartum recovery, and infant care of Zulu women in northern KwaZulu-Natal. J Ethnobiol Ethnomed. (2021) 17:1–19. doi: 10.1186/s13002-021-00451-2
26. Igwenyi PI, Nwankwo O, Nwafor JN, Eunice AN, Aleke CO, Obande-Ogbuinya EN, et al. Demographic predictors of cultural practices regarding female genital mutilation among married women in Ebonyi State, Nigeria. J Adv Med Med Res. (2021) 33:23–31. doi: 10.9734/jammr/2021/v33i830882
27. Ethiopian Census Current Year Projection - SNNP - Bench Maji - Semien Bench Navigate the Semien Bench Woreda Population Projection. (2021). Available online at: https://www.qotera.org/en-US/snnp/bench-maji/semien-bench/ (accessed March 19, 2021).
28. Gedamu H, Tsegaw A, Debebe E. The prevalence of traditional malpractice during pregnancy, child birth, and postnatal period among women of childbearing age in Meshenti Town, 2016. Int J Reprod Med. (2018) 2018:5945060. doi: 10.1155/2018/5945060
29. Sorrie MB, Amaje E, Gebremeskel F. Pre-lacteal feeding practices and associated factors among mothers of children aged less than 12 months in Jinka Town, South Ethiopia, 2018/19. PLoS ONE. (2020) 15:e0240583. doi: 10.1371/journal.pone.0240583
30. Tela FG, Gebremariam LW, Beyene SA. Food taboos and related misperceptions during pregnancy in Mekelle city, Tigray, Northern Ethiopia. PLoS ONE. (2020) 15:e0239451. doi: 10.1371/journal.pone.0239451
31. Zepro NB. Food taboos and misconceptions among pregnant women of Shashemene District, Ethiopia, 2012. Sci J Public Health. (2015) 3:410–6. doi: 10.11648/j.sjph.20150303.27
32. Yoseph M, Abebe SM, Mekonnen FA, Sisay M, Gonete KA. Institutional delivery services utilization and its determinant factors among women who gave birth in the past 24 months in Southwest Ethiopia. BMC Health Serv Res. (2020) 20:1–10. doi: 10.1186/s12913-020-05121-9
33. Mitikie KA, Wassie GT, Beyene MB. Institutional delivery services utilization and associated factors among mothers who gave birth in the last year in Mandura district, Northwest Ethiopia. PLoS ONE. (2020) 15:e0243466. doi: 10.1371/journal.pone.0243466
34. Berhe R, Nigusie A. Magnitude of home delivery and associated factors among child bearing age mothers in Sherkole District, Benishangul Gumuz regional state-Western-Ethiopia. BMC Public Health. (2020) 20:1–7. doi: 10.1186/s12889-020-08919-8
35. Mekonnen MG, Yalew KN, Umer JY, Melese M. Determinants of delivery practices among Afar pastoralists of Ethiopia. Pan Afr Med J. (2012) 13:17.
36. Assefa L, Alemayehu M, Debie A. Magnitude of institutional delivery service utilization and associated factors among women in pastoral community of Awash Fentale district Afar Regional State, Ethiopia. BMC Res Notes. (2018) 11:1–6. doi: 10.1186/s13104-018-3261-5
37. Bekele Y, Mengistie B, Mesfine F. Prelacteal feeding practice and associated factors among mothers attending immunization clinic in Harari region public health facilities, Eastern Ethiopia. Open J Prevent Med. (2014) 2014:5339. doi: 10.4236/ojpm.2014.47063
38. Egata G, Berhane Y, Worku A. Predictors of non-exclusive breastfeeding at 6 months among rural mothers in east Ethiopia: a community-based analytical cross-sectional study. Int Breastfeed J. (2013) 8:8. doi: 10.1186/1746-4358-8-8
39. Mekuria G, Edris M. Exclusive breastfeeding and associated factors among mothers in Debre Markos, Northwest Ethiopia: a cross-sectional study. Int Breastfeed J. (2015) 10:1–7. doi: 10.1186/s13006-014-0027-0
40. Mose A, Abebe H. Prelacteal feeding practice and its determinant factors among mothers having children less than 6 months of age in Bure district, Northwest Ethiopia: a community-based cross-sectional study. BMJ Open. (2021) 11:e046919. doi: 10.1136/bmjopen-2020-046919
41. Bililign N, Kumsa H, Mulugeta M, Sisay Y. Factors associated with prelacteal feeding in North Eastern Ethiopia: a community based cross-sectional study. Int Breastfeed J. (2016) 11:1–7. doi: 10.1186/s13006-016-0073-x
42. Tariku A, Biks GA, Wassie MM, Gebeyehu A, Getie AA. Factors associated with prelacteal feeding in the rural population of northwest Ethiopia: a community cross-sectional study. Int Breastfeed J. (2016) 11:14. doi: 10.1186/s13006-016-0074-9
43. Amele EA, Demissie BW, Desta KW, Woldemariam EB. Prelacteal feeding practice and its associated factors among mothers of children age less than 24 months old in Southern Ethiopia. Ital J Pediat. (2019) 45:15. doi: 10.1186/s13052-019-0604-3
44. Ambaw YL, Yirdaw BW, Biwota MA, Mekuryaw AM, Taye BT. Antenatal care follow-up decreases the likelihood of cultural malpractice during childbirth and postpartum among women who gave birth in the last 1-year in Gozamen district, Ethiopia: a community-based cross-sectional study. Arch Public Health. (2022) 80:53. doi: 10.1186/s13690-022-00814-5
45. Temesgen H, Negesse A, Woyraw W, Getaneh T, Yigizaw M. Prelacteal feeding and associated factors in Ethiopia: systematic review and meta-analysis. Int Breastfeed J. (2018) 13:1–12. doi: 10.1186/s13006-018-0193-6
46. Kasaye HK, Endale ZM, Gudayu TW, Desta MS. Home delivery among antenatal care booked women in their last pregnancy and associated factors: community-based cross sectional study in Debremarkos town, North West Ethiopia, January 2016. BMC Pregn Childbirth. (2017) 17:1–12. doi: 10.1186/s12884-017-1409-2
47. Regassa LD, Tola A, Weldesenbet AB, Tusa BS. Prevalence and associated factors of home delivery in Eastern Africa: further analysis of data from the recent Demographic and Health Survey data. SAGE Open Med. (2022) 10:20503121221088083. doi: 10.1177/20503121221088083
48. Scott NA, Henry EG, Kaiser JL, Mataka K, Rockers PC, Fong RM, et al. Factors affecting home delivery among women living in remote areas of rural Zambia: a cross-sectional, mixed-methods analysis. Int J Women's Health. (2018) 10:589–601. doi: 10.2147/IJWH.S169067
49. Tessema KM, Mihirete KM, Mengesha EW, Nigussie AA, Wondie AG. The association between male involvement in institutional delivery and women's use of institutional delivery in Debre Tabor town, North West Ethiopia: community based survey. PLoS ONE. (2021) 16:e0249917. doi: 10.1371/journal.pone.0249917
50. Paul PL. The role of male partners in maternal health service utilization: a secondary analysis using 2015–2016 National Family Health Survey (NFHS) data. Midwifery. (2022) 113:103423. doi: 10.1016/j.midw.2022.103423
51. Liben ML, Yimer NB, Feleke FW. Nearly one-in-five mothers avoid colostrum in North Wollo Zone, Ethiopia: an institution-based cross-sectional study. J Nutr Sci. (2021) 10:e100. doi: 10.1017/jns.2021.97
Keywords: prevalence, cultural malpractice, perinatal period, reproductive age women, Ethiopia
Citation: Tesfaye Diro A, Abdissa Fufa D and Geremew H (2023) Prevalence of cultural malpractice during the perinatal period and its determinants among reproductive age women in southwest Ethiopia: A community-based cross-sectional study. Front. Public Health 11:1064583. doi: 10.3389/fpubh.2023.1064583
Received: 21 October 2022; Accepted: 28 February 2023;
Published: 17 March 2023.
Edited by:
Joao Sollari Lopes, National Statistical Institute of Portugal, PortugalReviewed by:
Adera Debella, Haramaya University, EthiopiaGobopamang Letamo, University of Botswana, Botswana
Copyright © 2023 Tesfaye Diro, Abdissa Fufa and Geremew. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Habtamu Geremew, habteg29@gmail.com
 Abinet Tesfaye Diro
Abinet Tesfaye Diro Dinaol Abdissa Fufa
Dinaol Abdissa Fufa Habtamu Geremew
Habtamu Geremew