- 1Department of Preventive Medicine, School of Public Health, Guangzhou Medical University, Guangzhou, China
- 2Department of Clinical Medicine, Basic Medicine College, Zunyi Medical University, Zunyi, China
- 3Department of Environmental Hygiene, Guangzhou Center for Disease Control and Prevention, Guangzhou, China
- 4Department of Environmental Health, Institute of Public Health, Guangzhou Medical University, Guangzhou, China
This study examined the short-term relationship between ambient air pollutants and children's outpatient visits, and identified the effect of modifications by season. Daily recordings of air pollutants (CO, NO2, O3, SO2, PM10, and PM2.5) and children's outpatient visit data were collected in Guangzhou from 2015 to 2019. A generalized additive model adjusted for potential confounding was introduced to verify the association between ambient air pollution and outpatient visits for children. Subgroup analysis by season was performed to evaluate the potential effects. A total of 5,483,014 children's outpatient visits were recorded. The results showed that a 10 μg/m3 increase in CO, NO2, O3, SO2, PM10, and PM2.5 corresponded with a 0.19% (95% CI: 0.15–0.24%), 2.46% (2.00–2.92%), 0.27% (0.07–0.46%), 7.16% (4.80–9.57%), 1.16% (0.83–1.49%), and 1.35% (0.88–1.82%) increase in children's outpatient visits on the lag0 of exposure, respectively. The relationships were stronger for O3, PM10, and PM2.5 in the warm seasons, and for CO, NO2, and SO2 in the cool seasons. When adjusting for the co-pollutants, the effects of CO, NO2, and PM10 were robust. The results of this study indicate that six air pollutants might increase the risk of children's outpatient visits in Guangzhou, China, especially in the cool season.
Highlights
- The air pollutants were associated with children's outpatient visits.
- The E–R curves between pollutants and outpatient visits sometimes were positive.
- The links between air pollution and outpatient visits were different in seasons.
- Most robust associations of CO, NO2, and PM10 with children's outpatient risk.
1. Introduction
Ambient air pollution is a major global health issue with significant impacts worldwide, especially in developing countries. According to the Global Disease Burden, air pollution is a main cause of the global disease burden (1). Air pollution is a serious problem in China (2) due to rapid industrialization and urbanization over the past few decades. As the fourth largest environmental risk factor, air pollutants caused about 1.58 million deaths in China in 2016 (3).
Many epidemiological studies have demonstrated that exposure to air pollution, including carbon monoxide (CO), nitrogen dioxide (NO2), ozone (O3), sulfur dioxide (SO2), particulate matter with an aerodynamic diameter < 10 μm (PM10), and particulate matter with an aerodynamic diameter < 2.5 μm (PM2.5), can cause a range of adverse health effects. PM10 and PM2.5 are significantly associated with cardiorespiratory mortality risks, and even an increased risk of respiratory mortality (4). SO2, PM10, and PM2.5 are positively correlated with lung cancer mortality in Guangzhou (5). One study showed that ambient NO2 and PM2.5 exposure are significantly contacted with aggrandized all-cause non-accidental mortality (6). The adverse impacts of PM2.5 on cardiovascular emergency have been observed in previous studies (7, 8). Studies have also shown a positive correlation between PM2.5 exposure and daily medical treatment for respiratory diseases (9, 10). Moreover, SO2 and PM10 exposure are linked to increasing the risk of hospitalization for mental disorders (11). In short, previous studies have mostly reported the relationships between some of the six major air pollutants and human health effects, whereas there are few studies on the short-term relationships between six ambient air pollutants and health impacts.
Ambient outdoor and indoor air pollution caused the death of ~660,000 children in 2012 (12). Children are perhaps more sensitive than adults to the adverse health influences of air pollutants due to biological, behavioral, and environmental reasons (12). Children's exposure to ambient air pollution can have harmful and irreversible affections on organ systems because of their immature immune systems and developing lung functions (13). Compared with adults, children may inhale higher doses of air pollutants because they breathe more frequently and spend more time outdoors engaging in physical activity (14). Exposure to air pollution in infancy can cause lasting damage to cells and tissues, increase the risk of disease in children, and may have lifelong effects (15). Ambient air pollution exposure can affect child's development, so it is necessary to study the impacts of air pollutants on children's health.
Associations between children's health effects, specifically respiratory diseases, and ambient air pollutants have been well established. For example, lower respiratory diseases (16), upper respiratory tract infection (17), acute bronchitis (18), acute respiratory infections (14), pneumonia (19), and asthma (20) are significantly correlated with ambient air pollution. However, most studies have generally focused on a specific outpatient disease, and there is a lack of studies on the relationship between air pollution and children's outpatient visits for general diseases. In addition, many previous time-series studies lasted 2–4 years (18, 19, 21–23), and 5-year time-series studies have been limited.
Therefore, this study uses the time-series analysis method of quasi-Poisson generalized additive model to evaluate the acute effects of ambient air pollution (CO, NO2, O3, SO2, PM10, and PM2.5) on outpatient visits for children in Guangzhou, China from 2015 to 2019.
2. Materials and methods
2.1. Study location
Guangzhou (113°17′E 23°8'N), a crucial central city in China, is a comprehensive transportation hub and an international trade center (Supplementary Figure S1). Guangzhou has an oceanic subtropical monsoon climate, with a yearly average relative humidity of 77%, an average temperature of 23°C, and annual rainfall of about 1,720 mm. It has high temperatures and much rain water in the summer, and is mild and comparatively dry in winter (24). Guangzhou covers an area of 7,434.4 km2 and is divided into 11 municipal districts, with a resident population of 18.81 million by 2021.
2.2. Outpatient data
The data of children's outpatient visits were collected from January 1, 2015 to December 31, 2019 from the Guangdong Provincial Center for Disease Control and Prevention. The outpatient visits for children were obtained from six hospitals: Guangzhou Conghua District Hospital of Traditional Chinese Medicine, Guangzhou Panyu Central Hospital, Guangzhou First People's Hospital, The First Affiliated Hospital of Guangzhou Medical University, He Xian Memorial Affiliated Hospital of Southern Medical University, and the Clifford Hospital (Supplementary Figure S1).
2.3. Ambient air pollutants and meteorological data
During the study period, daily 24-h average concentrations of CO, NO2, SO2, PM10, and PM2.5, and maximum daily 8-h average concentration for O3 were obtained from the Urban Air Quality Real-Time Release Platform (https://air.cnemc.cn:18007/) of the Ministry of Ecology and Environment of the People's Republic of China. The routine average concentrations of these air pollutants were from 21 air monitoring stations spread in the urban area of Guangzhou (Supplementary Figure S1). Meteorological indicators, including the daily mean temperature and average relative humidity, were collected from the Guangdong Meteorological Service at the same time. Those two parameters were included in the model to adjust for the effects of confounding factors.
2.4. Statistical analyses
A children's outpatient visit is a low probability event, conforming to the Poisson distribution. A time-series quasi-Poisson generalized additive model was introduced to verify the relationships between ambient air pollution and children's outpatient visits. According to the results of previous time-series studies (25, 26), several covariates were adjusted in the model. In this main smoothing model, degrees of freedom (df) were set on the basis of previous studies (24, 27):
where E (Yt) is the expected number of routine children's outpatient visits on everyday t, β is the regression coefficient, Zt represents the pollutant concentration at day t, ns() is the natural cubic curve, and DOWt is the dummy variable indicating the day of the week of day t.
The potential delay effect was analyzed using various delay effect constructions. These lag models were divided into two classifications: single lag effects (lag0–lag5) and cumulative lag effects (lag01–lag05). Then, by adding a natural spline function with 4 df to the above GAM model, the exposure–response association between children's outpatient visits and ambient air pollutants were plotted. In addition, stratified analysis was carried out according to the season. The cool period was from October 1 to April 30, and the warm period was from May 1 to September 30.
The significance of a difference between two groups was examined by determining the 95% confidence interval (CI) as follows: , where SE1 and SE2 are their standard errors, and β1 and β2 are estimate value for every subgroup (28, 29). To test the robustness of the estimated relationships, we changed the df with 4–10 per year (30, 31). Furthermore, co-pollutant models were constructed to check the stability of the results.
We regulated all statistical analyses with R software (version 4.1.1) using the mgcv package. The effects are expressed as the excess risk (ER), figured out by the (relative risk – 1) × 100%, and 95% CI of children's outpatient visits per 10 μg/m3 increase in ambient air pollutants. P < 0.05 was considered statistically significant.
3. Results
Supplementary Figure S2 shows the time-series distributions of CO, NO2, O3, SO2, PM10, PM2.5, and children's outpatient visits from 1 January 2015 to 31 December 2019 in Guangzhou. A total of 5,483,014 children's outpatient visits were recorded in the six hospitals. Table 1 shows the descriptive statistics of daily ambient air pollutants, children's outpatient visits, and meteorological conditions. The daily average concentrations of CO, NO2, O3, SO2, PM10, and PM2.5 were 892.8, 46.8, 90.1, 10.4, 55.3, and 34.5 μg/m3, respectively. These values for CO, NO2, SO2, PM10, and PM2.5 were about 0.2, 1.2, 0.2, 0.8, and 1.0 times the secondary standard limits of GB 3095-2012 set by China (4,000.0, 40.0, 60.0, 70.0, and 35.0 μg/m3 annually), and 0.2, 4.7, 0.3, 3.7, and 6.9 times the ambient air quality standards in World Health Organization (WHO) (4,000.0, 10.0, 40.0, 15.0, and 5 μg/m3 annually), respectively. O3 concentrations on 193 and 699 days exceeded the daily criteria set by China (160 μg/m3) and the WHO (100 μg/m3), respectively. The daily average value of relative humidity was 80.3%, and the annual mean temperature was 22.3°C in Guangzhou.
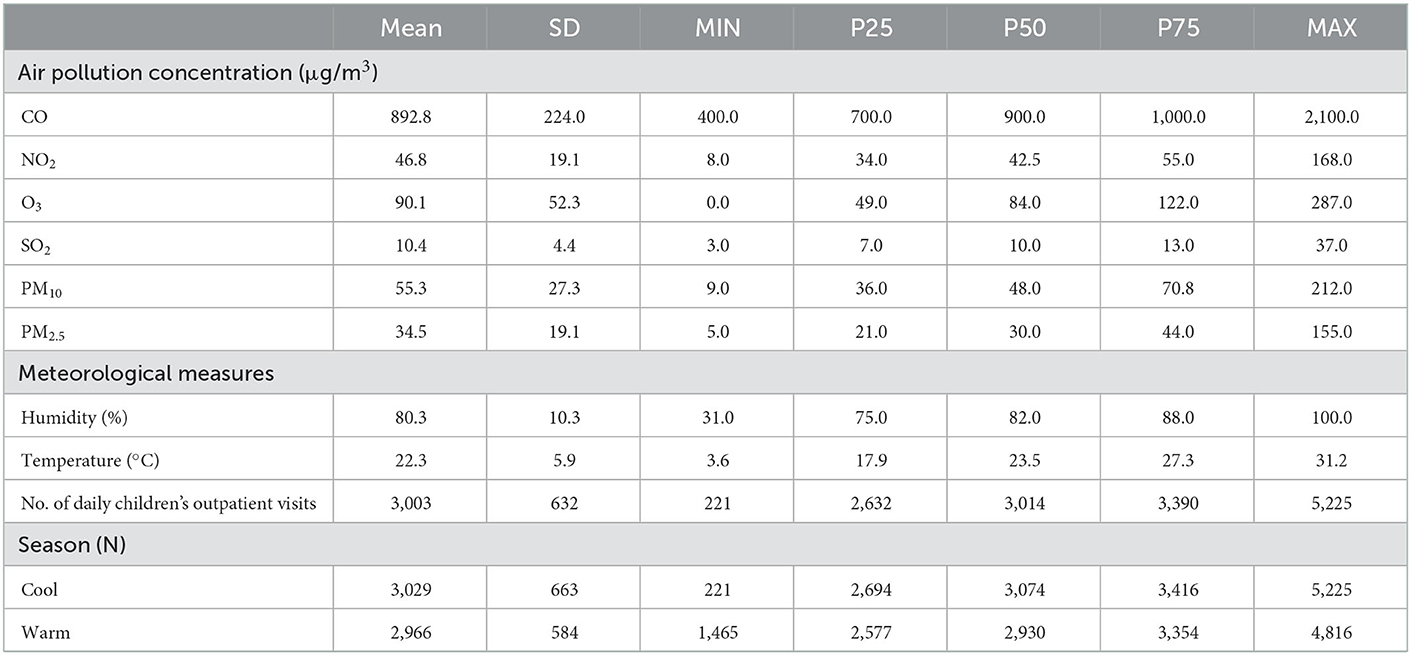
Table 1. Daily air pollutants, meteorological data, and children's outpatient visits during the study.
Table 2 displays the Spearman correlation coefficients among ambient air pollution and meteorological elements in Guangzhou, China. The six air pollutants were positively correlated with each other, except O3 and CO, and negatively correlated with temperature, except O3. Moreover, relative humidity was negatively correlated with O3, SO2, PM10, and PM2.5, and positively correlated with temperature, CO, and NO2. Significant correlations were observed between the exposure variables, except between SO2 and temperature and between NO2 and relative humidity.
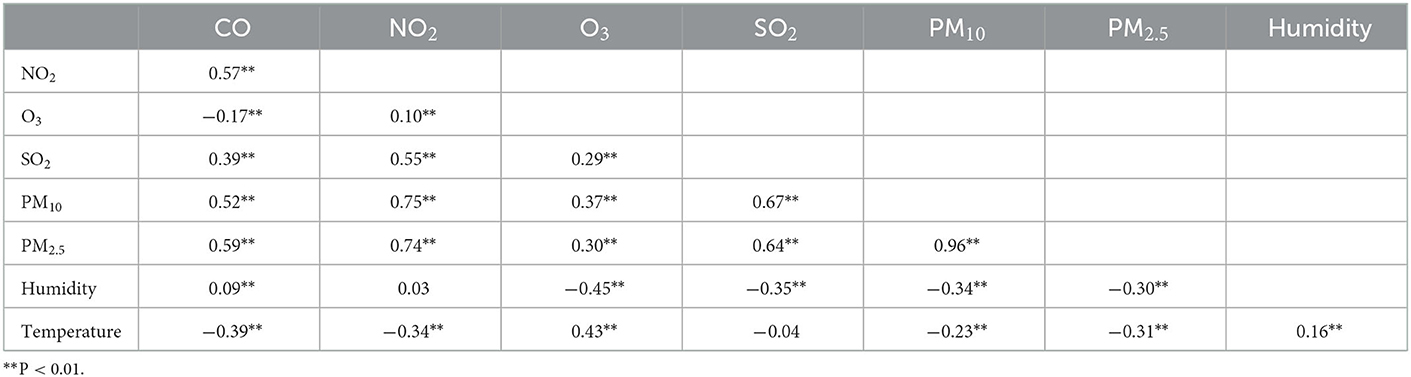
Table 2. Spearman's correlations between daily average air pollution concentrations and meteorological factors during the study period.
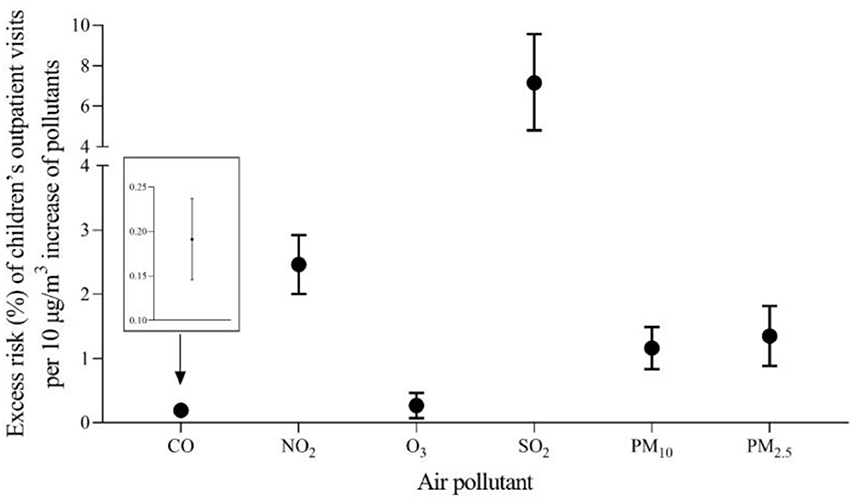
As shown in Figure 1, a 10 μg/m3 increase in CO, NO2, SO2, PM10, and PM2.5 was connected with excess risk of outpatient visits for children after adjusting for relative humidity and temperature. The estimated effects on risk of air pollutant concentrations were tested using models with different single lag days. The relationships between air pollution and children's outpatient visits were statistically significant, except for O3 in the model with lag3–5 in the single-pollutant. According to the model fit statistics, this means that each 10 μg/m3 increase in ambient CO, NO2, SO2, PM10, and PM2.5 corresponded to a 0.19% (95% confidence interval:0.15–0.24%), 2.46% (2.00–2.92%), 0.27% (0.07–0.46%), 7.16% (4.80–9.57%), 1.16% (0.83–1.49%), and 1.35% (0.88–1.82%) increase in children's outpatient visits on the day (lag0) of exposure, respectively. The cumulative lag days, like single lag days, ranging from lag01 to lag05. Overall, the influences of six air pollutants on the cumulative lag days were stronger than on the single days. The maximum cumulative effects were observed on lag02 for O3, 0.35% (0.12–0.57%), and lag05 for CO, 0.34% (0.28–0.41%), NO2, 4.27% (3.55–5.00%), SO2, 12.01% (8.50–15.64%), PM10, 2.03% (1.53–2.53%), and PM2.5, 2.51% (1.79–3.23%).
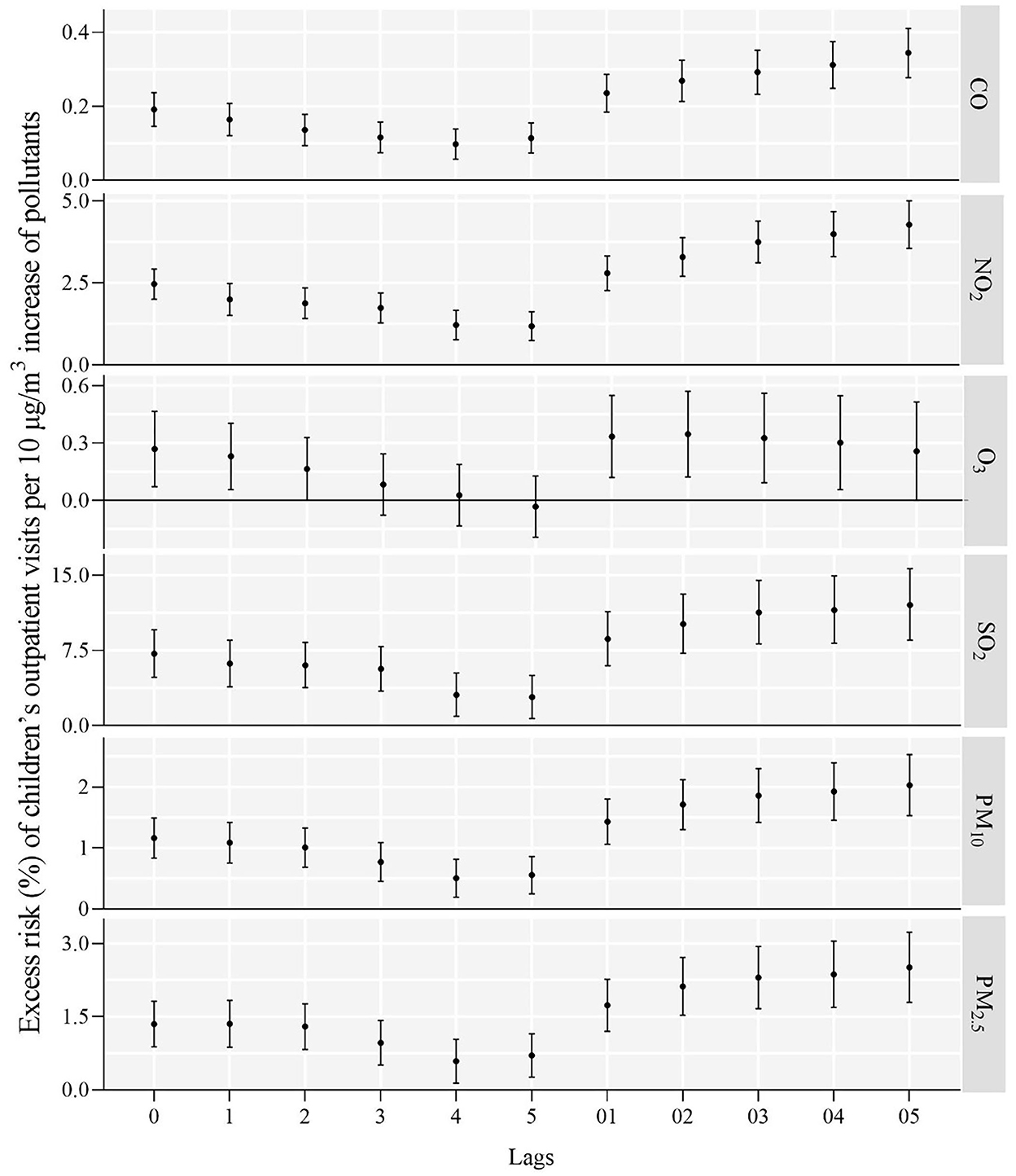
Figure 1. Excess risk (%) and 95% confidence intervals of children's outpatient visits a 10 μg/m3 increase in various ambient air pollutant concentrations along different lag days.
The exposure–response curves of the correlations between ambient air pollution and children's outpatient visits are given in Figure 2. The curves of the ambient air pollution were obviously positive in the meaningful exposure range. The exposure–response curves of CO, PM10, and PM2.5 displayed a sharp pitch at concentrations < 1,500 μg/m3, < 100 μg/m3, and < 100 μg/m3 and then a decrease. The curves of O3 were nearly S-shaped, sharply rising at concentrations ≥100 μg/m3 and flattening for concentrations ≥200 μg/m3. The exposure–response curves of NO2 and SO2 showed steep hill at concentrations < 50 and < 15 μg/m3, rapidly ascended at concentrations ≥100 and ≥25 μg/m3, and became flattened at mid-range concentrations.
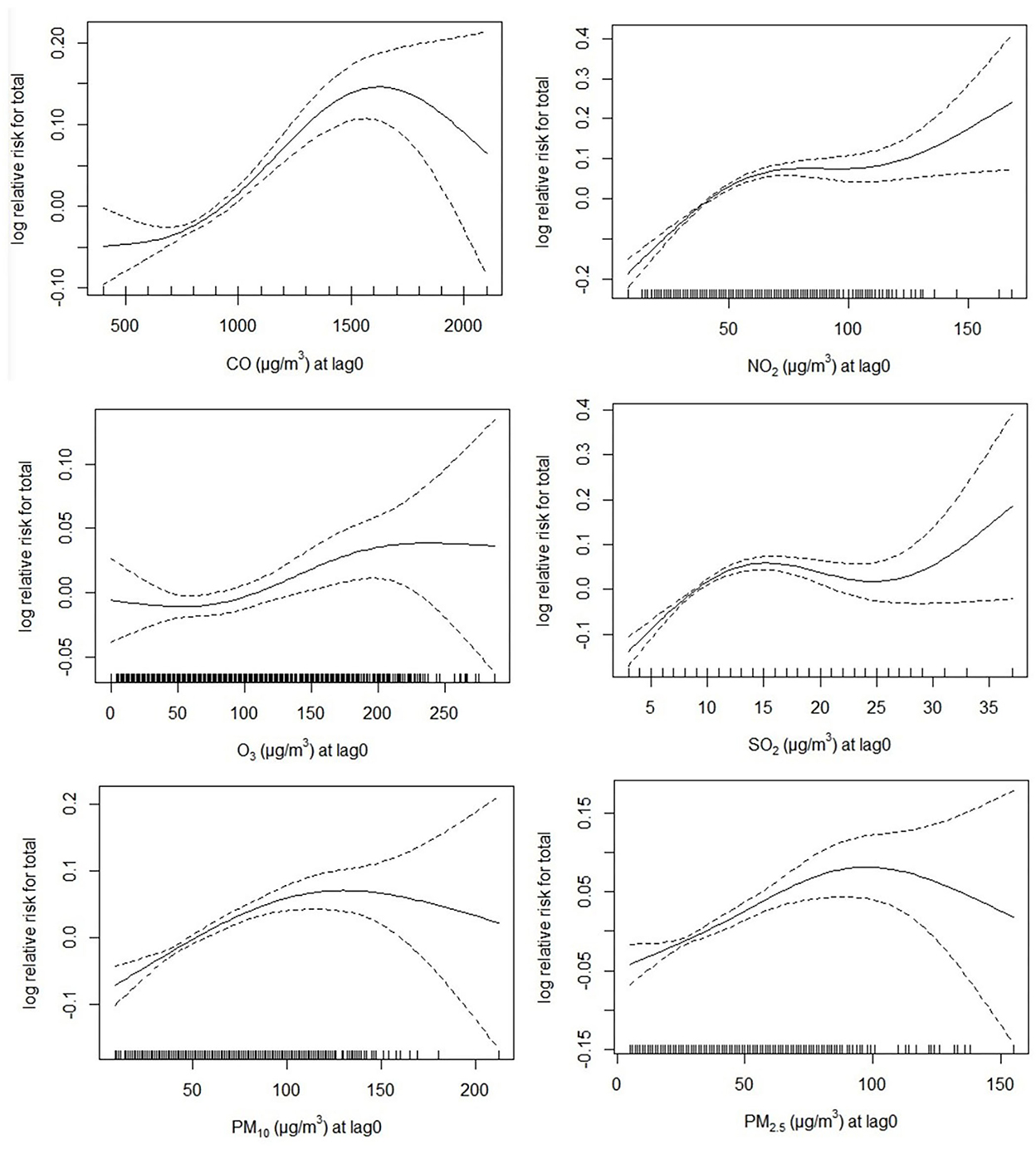
Figure 2. The exposure–response curves of the associations of different air pollution with the risk of children's outpatient visits in single-pollutant model. The black line represents the average relative risk of the pollutant concentration, and the dashed lines are the 95% confidence interval of the risk estimates.
Table 3 shows the estimated ER of children's outpatient visits and 95% CI by season breakdown of the concentrations of ambient air pollution. Season stratification revealed significant differences in the links between ambient air pollutants and the risk of children's outpatient visits. The associations with O3, PM10, and PM2.5 were more prominent in warm than in cool seasons, and the links with CO, NO2, and SO2 were much stronger in cool seasons. Specifically, relationships between O3 and children's outpatient visits were non-significant in the cool seasons.
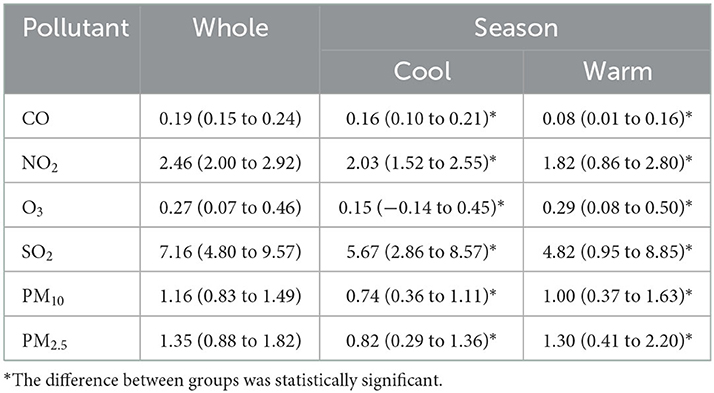
Table 3. Estimated ER and 95% CI of children's outpatient visits a 10 μg/m3 increase in the concentrations of air pollution stratified by season.
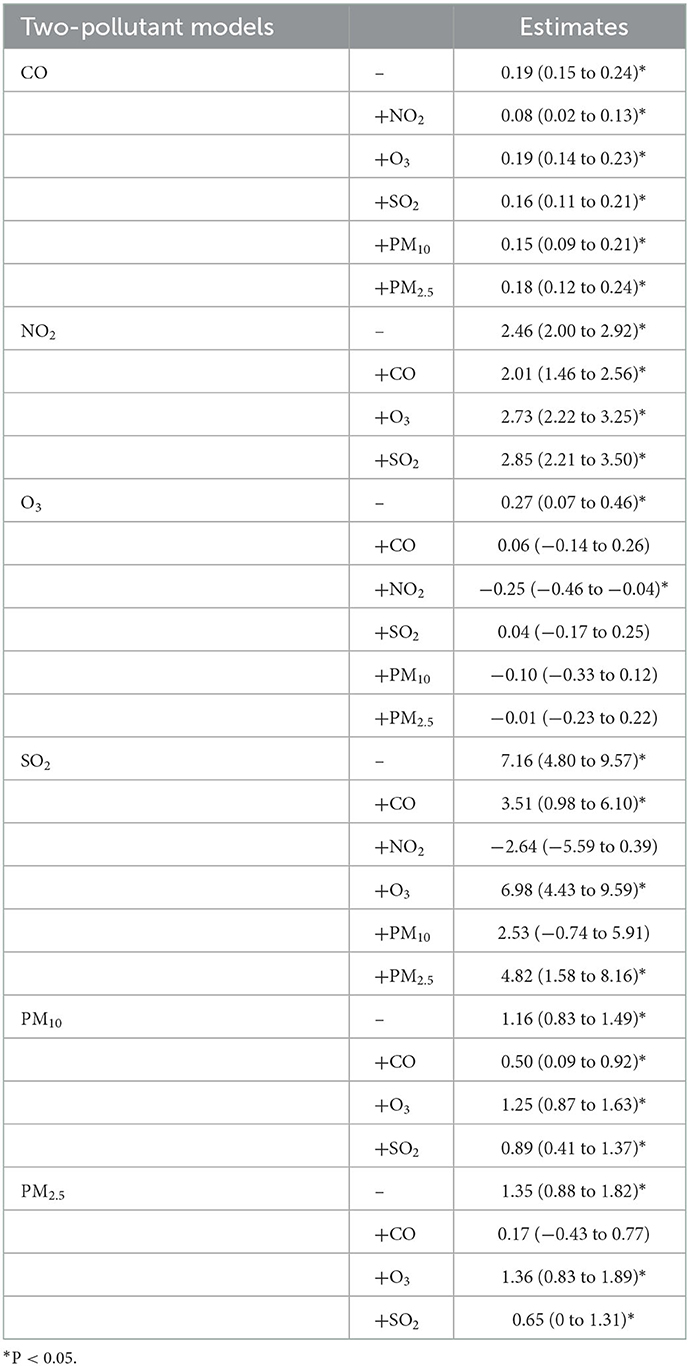
In the sensitivity analysis, when we use df to adjust the smoothness of time from 5 to 9, the results did not change substantially, except for O3 (Figure 3). Table 4 establishes the relationships between all ambient pollutants and children's outpatient visits in two-pollutant models, as assessed by another sensitivity analysis. In the two-pollutants analysis, the Spearman's correlation coefficients < 0.7 were introduced into the co-pollutant models. The correlations of CO, NO2, and PM10 in the risk of children's outpatient visits remained robust in the co-pollutant models. However, after adjusting for four air pollutants, the effects of O3 became non-significant, while the adjustment for NO2 yielded significant results. When adjusting for NO2 and PM10, the influences of SO2 decreased and became not significant, respectively. After adjusting for CO, the effects of PM2.5 decreased and became non-significant. Together, these results indicate that CO, NO2, and PM10 may play more alone role in children's outpatient risk.
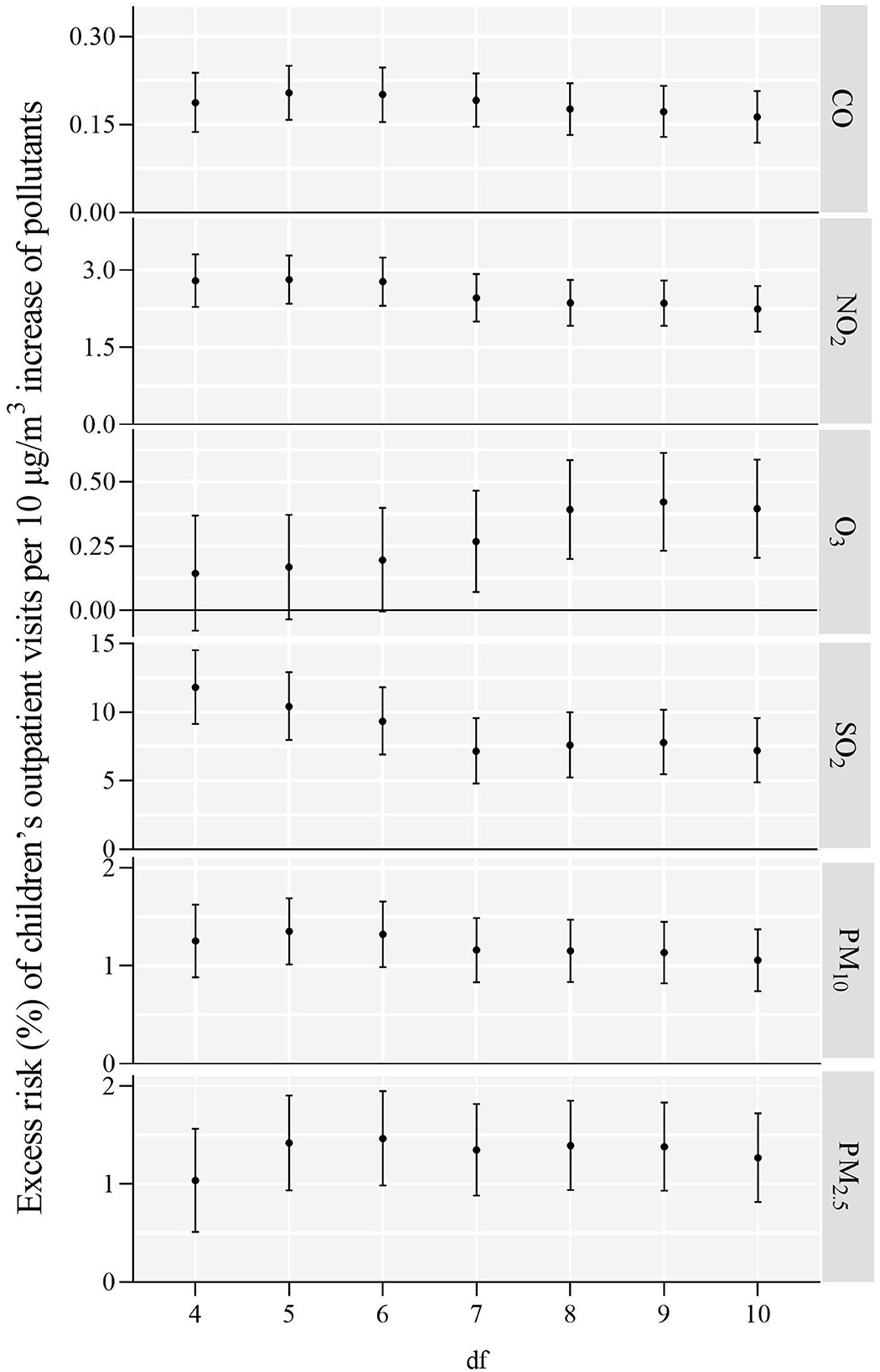
Figure 3. ER (%) and 95% CI of children's outpatient visits a 10 μg/m3 increase in air pollution concentrations on the day of exposure.
4. Discussion
We conducted a time-series study to assess the short-term relationships between ambient air pollution and children's outpatient visits and observed significant relationships. Exposure–response relationships between six ambient air pollutants and the risk of children's outpatient visits were positive in the meaningful exposure range. The associations with O3, PM10, and PM2.5 were more prominent in warm than in cool seasons, and the links with CO, NO2, and SO2 were stronger in cool than in warm seasons. The correlations of O3, SO2, and PM2.5 with children's outpatient visits were likely affected by other air pollutants, whereas CO, NO2, and PM10 appeared to play more alone role in the risk of children's outpatient visits. This analysis provides the latest evidence to establish the relationships between air pollutants and harmful health effects.
Significant relationships between CO, NO2, O3, SO2, PM10, PM2.5, and children's outpatient visits were found in this research, which was commonly consistent with previous time-series studies (22, 32–34). Each 10 μg/m3 increase of O3 and PM2.5 corresponded to 0.27% (0.07–0.46%) and 1.35% (0.88–1.82%) increments in the risk of children's outpatient visits in the single-pollutant model, respectively, but these were not significant in the co-pollutant models, match with previous studies (31, 35). In the co-pollution model, the adverse effects of O3 disappeared or even reversed may be explained by the relative instability of ozone (36). A weak but significant relationship between CO and children's outpatient visits was found, in line with a previous study (30, 37). In the analysis of the two pollutant models, the associations with NO2 and PM10 remained robust, which may reveal that NO2 and PM10 had more independent effects on children's outpatient visits. Previous studies have indicated that the level of significance did not increase when SO2 be analyzed in co-pollutant model (38, 39).
Although exposure–response relationships may change due to a variety of limitations, including climatic characteristics, geographical location, air pollution mixtures, and population sensitivity (11, 31), the results still have reminders for human health assessment. In this research, a linear and limitation association between CO, PM10, and PM2.5 the risk of children's outpatient visits were identified within a certain range, whereas a linear and not threshold association between O3, NO2, SO2 and children's outpatient visits were confirmed. The curve for NO2 tended to plateau at mid-range concentrations. The S-shaped curve for O3 tended to plateau at high concentrations. As a result, ambient air pollutant concentrations should be constantly reduced to protect human health and reduce the risks of outpatient visits among children.
The differences in the effects of CO, NO2, O3, SO2, PM10, and PM2.5 on the risk of children's outpatient visits between cold and warm seasons were statistically significant. The influences of PM10 and PM2.5 on this risk were significantly stronger in warm seasons, consistent with previous studies (31, 40). The possible reason may be that children spend more time outdoors in warm than in cold seasons. So their exposure dose perhaps lower during the cold seasons (31). The relationships of SO2 and NO2 with children's outpatient visits were stronger in the cool season. This finding was in agreement with several studies (41, 42) but contradictory to others (33, 35). The specific reason for these differences between warm and cool seasons must be clarified in the future.
The observed influences of ambient air pollution on children's outpatient visits are biologically plausible. NO2 and SO2 can augment the permeability of airway mucosa and increase allergic diseases (43). NO2 can also induce airway inflammation and may restrict the smaller airways and terminal bronchioles (44). PM2.5 and PM10 can be deeply inhaled into the lungs (45), causing various inflammatory reactions (46–48), and local inflammation of alveoli can further develop into systemic inflammatory (49). O3 affects airway inflammation in children by increasing the levels of cationic proteins associated with leukocytes and eosinophils (50). PM2.5, SO2, and NO2 can increase airway oxidative stress and reduce small airway function (51).
This study has a few limitations. First, we used in average pollutant concentrations from fixed-site monitors rather than individual monitoring data, which might have resulted in exposure errors (52). Second, although we used data on children's outpatient visits from six hospitals in the study city, selection bias might have existed. Third, due to the limitations of the collected children's outpatient records, we can only get the number of children's outpatients per day, without studying other stratification analyses and finding multiple visits during a course of illness (26). Fourth, none of the hospitals is a children's hospital which has the largest number of children's outpatient visits in the city. In addition, the matching between environmental exposure and illness is not enough because of the lack of the children's residential address and monitoring data from the nearest monitoring stations according to the location of hospitals, which is also the inadequacy of this study. Finally, we did not include confounding factors at the personal level (e.g., lifestyles and indoor pollution exposure) (53), which might affect the relationships between ambient air pollution and individual vulnerability.
5. Conclusions
This time-series analysis suggests that ambient air pollution, especially CO, NO2, and PM10, can significantly increase the risk of children's outpatient visits in Guangzhou, China. The relationships were stronger for CO, NO2, and SO2 in the cool seasons, and for O3, PM10, and PM2.5 in the warm seasons. The findings of this study suggest that persistent efforts to reduce air pollution levels in Guangzhou would have health benefits, resulting in a decrease in children's outpatient visits. These results can only be generalized to cities with similar populations, societies, and environments.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
QY designed the study and supervised the research, including funding, text review, and overall quality assurance and control. SC helped with the formulation of research methods, software analysis, and wrote the original draft of the text. BX helped with the investigation and review of the data and assisted in the preparation of the original draft of the text. TS assisted in the implementation of research, data management, investigation, and supervision. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (Grant Number: 81773385 to QY), Natural Science Foundation of Guangdong Province (Grant Numbers: 2019A1515011298 and 2022A1515010727 to QY), and Key Scientific Research Projects of Guangdong Provincial Department of Education (Grant Number: 2022ZDZX2047 to QY).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1058368/full#supplementary-material
Supplementary Figure S1. The locations of 21 ambient air monitoring stations and 6 hospitals in Guangzhou between 1 January 2015 and 31 December 2019.
Supplementary Figure S2. The time-series distributions of CO, NO2, O3, SO2, PM10, PM2.5 and outpatient visits from 1 January 2015 to 31 December 2019 in Guangzhou.
References
1. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
2. Yu Q, Zhang L, Hou K, Li J, Liu S, Huang K, et al. Relationship between air pollutant exposure and gynecologic cancer risk. Int J Environ Res Public Health. (2021) 18:5353. doi: 10.3390/ijerph18105353
3. Luo L, Zhang Y, Jiang J, Luan H, Yu C, Nan P, et al. Short-term effects of ambient air pollution on hospitalization for respiratory disease in Taiyuan, China: a time-series analysis. Int J Environ Res Public Health. (2018) 15:2160. doi: 10.3390/ijerph15102160
4. Wu R, Zhong L, Huang X, Xu H, Liu S, Feng B, et al. Temporal variations in ambient particulate matter reduction associated short-term mortality risks in Guangzhou, China: a time-series analysis (2006–2016). Sci Total Environ. (2018) 645:491–8. doi: 10.1016/j.scitotenv.2018.07.091
5. Wang N, Mengersen K, Tong S, Kimlin M, Zhou M, Wang L, et al. Short-term association between ambient air pollution and lung cancer mortality. Environ Res. (2019) 179:108748. doi: 10.1016/j.envres.2019.108748
6. Amini H, Nhung NTT, Schindler C, Yunesian M, Hosseini V, Shamsipour M, et al. Short-term associations between daily mortality and ambient particulate matter, nitrogen dioxide, and the air quality index in a Middle Eastern megacity. Environ Pollut. (2019) 254:113121. doi: 10.1016/j.envpol.2019.113121
7. Su C, Breitner S, Schneider A, Liu L, Franck U, Peters A, et al. Short-term effects of fine particulate air pollution on cardiovascular hospital emergency room visits: a time-series study in Beijing, China. Int Arch Occup Environ Health. (2016) 89:641–57. doi: 10.1007/s00420-015-1102-6
8. Chen R, Gao Q, Sun J, Yang H, Li Y, Kang F, et al. Short-term effects of particulate matter exposure on emergency room visits for cardiovascular disease in Lanzhou, China: a time series analysis. Environ Sci Pollut Res. (2020) 27:9327–35. doi: 10.1007/s11356-020-07606-w
9. Zhang Z, Chai P, Wang J, Ye Z, Shen P, Lu H, et al. Association of particulate matter air pollution and hospital visits for respiratory diseases: a time-series study from China. Environ Sci Pollut Res. (2019) 26:12280–7. doi: 10.1007/s11356-019-04397-7
10. Wang Y, Zu Y, Huang L, Zhang H, Wang C, Hu J. Associations between daily outpatient visits for respiratory diseases and ambient fine particulate matter and ozone levels in Shanghai, China. Environ Pollut. (2018) 240:754–63. doi: 10.1016/j.envpol.2018.05.029
11. Chen C, Liu C, Chen R, Wang W, Li W, Kan H, et al. Ambient air pollution and daily hospital admissions for mental disorders in Shanghai, China. Sci Total Environ. (2018) 613:324–30. doi: 10.1016/j.scitotenv.2017.09.098
12. Goldizen FC, Sly PD, Knibbs LD. Respiratory effects of air pollution on children. Pediatr Pulmonol. (2016) 51:94–108. doi: 10.1002/ppul.23262
13. Schraufnagel DE, Balmes JR, Cowl CT, De Matteis S, Jung SH, Mortimer K, et al. (2019). Air pollution and non-communicable diseases a review by the forum of international respiratory societies' environmental committee, Part 1: the damaging effects of air pollution. Chest. (2019) 155:409–16. doi: 10.1016/j.chest.2018.10.042
14. Darrow LA, Klein M, Flanders WD, Mulholland JA, Tolbert PE, Strickland MJ. Air pollution and acute respiratory infections among children 0–4 years of age: an 18-year time-series study. Am J Epidemiol. (2014) 180:968–77. doi: 10.1093/aje/kwu234
15. Barker DJ. The developmental origins of adult disease. J Am Coll Nutr. (2004) 23:588S−95S. doi: 10.1080/07315724.2004.10719428
16. Zhu L, Ge X, Chen Y, Zeng X, Pan W, Zhang X, et al. Short-term effects of ambient air pollution and childhood lower respiratory diseases. Sci Rep. (2017) 7:1–7. doi: 10.1038/s41598-017-04310-7
17. Li YR, Xiao CC, Li J, Tang J, Geng XY, Cui LJ, et al. Association between air pollution and upper respiratory tract infection in hospital outpatients aged 0–14 years in Hefei, China: a time series study. Public Health. (2018) 156:92–100. doi: 10.1016/j.puhe.2017.12.006
18. Bai L, Su X, Zhao D, Zhang Y, Cheng Q, Zhang H, et al. Exposure to traffic-related air pollution and acute bronchitis in children: season and age as modifiers. J Epidemiol Commun Health. (2018) 72:426–33. doi: 10.1136/jech-2017-209948
19. Li D, Wang J-B, Zhang Z-Y, Shen P, Zheng P-W, Jin M-J, et al. Effects of air pollution on hospital visits for pneumonia in children: a two-year analysis from China. Environ Sci Pollut Res. (2018) 25:10049–57. doi: 10.1007/s11356-018-1192-2
20. Zhang Y, Ni H, Bai L, Cheng Q, Zhang H, Wang S, et al. The short-term association between air pollution and childhood asthma hospital admissions in urban areas of Hefei City in China: a time-series study. Environ Res. (2019) 169:510–6. doi: 10.1016/j.envres.2018.11.043
21. Li Y, Li C, Liu J, Meng C, Xu C, Liu Z, et al. An association between PM2.5 and pediatric respiratory outpatient visits in four Chinese cities. Chemosphere. (2021) 280:130843. doi: 10.1016/j.chemosphere.2021.130843
22. Dong J, Wang Y, Wang J, Bao H. Association between atmospheric PM2.5 and daily outpatient visits for children's respiratory diseases in Lanzhou. Int J Biometeorol. (2021) 65:989–99. doi: 10.1007/s00484-021-02080-6
23. Ma Y, Yue L, Liu J, He X, Li L, Niu J, et al. Association of air pollution with outpatient visits for respiratory diseases of children in an ex-heavily polluted Northwestern city, China. BMC Public Health. (2020) 20:1–14. doi: 10.1186/s12889-020-08933-w
24. Yang C, Chen A, Chen R, Qi Y, Ye J, Li S, et al. Acute effect of ambient air pollution on heart failure in Guangzhou, China. Int J Cardiol. (2014) 177:436–41. doi: 10.1016/j.ijcard.2014.09.003
25. Chao L, Lu M, An Z, Li J, Li Y, Zhao Q, et al. Short-term effect of NO2 on outpatient visits for dermatologic diseases in Xinxiang, China: a time-series study. Environ Geochem Health. (2021) 43:3429–39. doi: 10.1007/s10653-021-00831-3
26. Wang HL, Sun J, Qian ZM, Gong YQ, Zhong JB, Yang RD, et al. Association between air pollution and atopic dermatitis in Guangzhou, China: modification by age and season. Br J Dermatol. (2021) 184:1068–76. doi: 10.1111/bjd.19645
27. Tian Y, Liu H, Wu Y, Si Y, Li M, Wu Y, et al. Ambient particulate matter pollution and adult hospital admissions for pneumonia in urban China: a national time series analysis for 2014 through 2017. PLoS Med. (2019) 16:e1003010. doi: 10.1371/journal.pmed.1003010
28. Lin H, Guo Y, Zheng Y, Di Q, Liu T, Xiao J, et al. Long-term effects of ambient PM2.5 on hypertension and blood pressure and attributable risk among older Chinese adults. Hypertension. (2017) 69:806. doi: 10.1161/HYPERTENSIONAHA.116.08839
29. Lin H, Liu T, Xiao J, Zeng W, Li X, Guo L, et al. Mortality burden of ambient fine particulate air pollution in six Chinese cities: results from the Pearl River Delta study. Environ Int. (2016) 96:91–7. doi: 10.1016/j.envint.2016.09.007
30. Song J, Lu M, Lu J, Chao L, An Z, Liu Y, et al. Acute effect of ambient air pollution on hospitalization in patients with hypertension: a time-series study in Shijiazhuang, China. Ecotoxicol Environ Saf. (2019) 170:286–92. doi: 10.1016/j.ecoenv.2018.11.125
31. Lu M, Ding S, Wang J, Liu Y, An Z, Li J, et al. Acute effect of ambient air pollution on hospital outpatient cases of chronic sinusitis in Xinxiang, China. Ecotoxicol Environ Saf. (2020) 202:110923. doi: 10.1016/j.ecoenv.2020.110923
32. Li M, Tang J, Yang H, Zhao L, Liu Y, Xu H, et al. Short-term exposure to ambient particulate matter and outpatient visits for respiratory diseases among children: a time-series study in five Chinese cities. Chemosphere. (2021) 263:128214. doi: 10.1016/j.chemosphere.2020.128214
33. Song J, Lu M, Zheng L, Liu Y, Xu P, Li Y, et al. Acute effects of ambient air pollution on outpatient children with respiratory diseases in Shijiazhuang, China. BMC Pulm Med. (2018) 18:1–10. doi: 10.1186/s12890-018-0716-3
34. Hendricks AJ, Eichenfield LF, Shi VY. The impact of airborne pollution on atopic dermatitis: a literature review. Br J Dermatol. (2020) 183:16–23. doi: 10.1111/bjd.18781
35. Liu L, Liu C, Chen R, Zhou Y, Meng X, Hong J, et al. Associations of short-term exposure to air pollution and emergency department visits for pediatric asthma in Shanghai, China. Chemosphere. (2021) 263:127856. doi: 10.1016/j.chemosphere.2020.127856
36. Braidy N, Izadi M, Sureda A, Jonaidi-Jafari N, Banki A, Nabavi SF, et al. Therapeutic relevance of ozone therapy in degenerative diseases: focus on diabetes and spinal pain. J Cell Physiol. (2018) 233:2705–14. doi: 10.1002/jcp.26044
37. Wang J, Lu M, An Z, Jiang J, Li J, Wang Y, et al. Associations between air pollution and outpatient visits for allergic rhinitis in Xinxiang, China. Environ Sci Pollut Res. (2020) 27:23565–74. doi: 10.1007/s11356-020-08709-0
38. Li A, Fan L, Xie L, Ren Y, Li L. Associations between air pollution, climate factors and outpatient visits for eczema in West China Hospital, Chengdu, south-western China: a time series analysis. J Eur Acad Dermatol Venereol. (2018) 32:486–94. doi: 10.1111/jdv.14730
39. Guo Q, Xiong X, Liang F, Tian L, Liu W, Wang Z, et al. The interactive effects between air pollution and meteorological factors on the hospital outpatient visits for atopic dermatitis in Beijing, China: a time-series analysis. J Eur Acad Dermatol Venereol. (2019) 33:2362–70. doi: 10.1111/jdv.15820
40. Alessandrini ER, Stafoggia M, Faustini A, Berti G, Canova C, De Togni A, et al. Association between short-term exposure to PM2.5 and PM10 and mortality in susceptible subgroups: a multisite case-crossover analysis of individual effect modifiers. Am J Epidemiol. (2016) 184:744–54. doi: 10.1093/aje/kww078
41. Cai J, Zhao A, Zhao J, Chen R, Wang W, Ha S, et al. Acute effects of air pollution on asthma hospitalization in Shanghai, China. Environ Pollut. (2014) 191:139–44. doi: 10.1016/j.envpol.2014.04.028
42. Chen R, Chu C, Tan J, Cao J, Song W, Xu X, et al. Ambient air pollution and hospital admission in Shanghai, China. J Hazard Mater. (2010) 181:234–40. doi: 10.1016/j.jhazmat.2010.05.002
43. Charpin D, Pascal L, Birnbaum J, Armengaud A, Sambuc R, Lanteaume A, et al. Gaseous air pollution and atopy. Clin Exp Allergy. (1999) 29:1474–80. doi: 10.1046/j.1365-2222.1999.00685.x
44. Braman SS. The global burden of asthma. Chest. (2006) 130:S4–12. doi: 10.1378/chest.130.1_suppl.4S
45. Wang S, Li Y, Niu A, Liu Y, Su L, Song W, et al. The impact of outdoor air pollutants on outpatient visits for respiratory diseases during 2012–2016 in Jinan, China. Respir Res. (2018) 19:1–18. doi: 10.1186/s12931-018-0958-x
46. Chen B-Y, Chan C-C, Lee C-T, Cheng T-J, Huang W-C, Jhou J-C, et al. The association of ambient air pollution with airway inflammation in schoolchildren. Am J Epidemiol. (2012) 175:764–74. doi: 10.1093/aje/kwr380
47. Han Y, Zhu T, Guan T, Zhu Y, Liu J, Ji Y, et al. Association between size-segregated particles in ambient air and acute respiratory inflammation. Sci Total Environ. (2016) 565:412–9. doi: 10.1016/j.scitotenv.2016.04.196
48. Bonato M, Gallo E, Bazzan E, Marson G, Zagolin L, Cosio MG, et al. Air pollution relates to airway pathology in children with wheezing. Ann Am Thorac Soc. (2021) 18:2033–40. doi: 10.1513/AnnalsATS.202010-1321OC
49. Li Y, Rittenhouse-Olson K, Scheider WL, Mu L. Effect of particulate matter air pollution on C-reactive protein: a review of epidemiologic studies. Rev Environ Health. (2012) 27:133–49. doi: 10.1515/reveh-2012-0012
50. Kopp MV, Ulmer C, Ihorst G, Seydewitz HH, Frischer T, Forster J, et al. Upper airway inflammation in children exposed to ambient ozone and potential signs of adaptation. Eur Respir J. (1999) 14:854–61. doi: 10.1034/j.1399-3003.1999.14d22.x
51. Liu L, Poon R, Chen L, Frescura A-M, Montuschi P, Ciabattoni G, et al. Acute effects of air pollution on pulmonary function, airway inflammation, and oxidative stress in asthmatic children. Environ Health Perspect. (2009) 117:668–74. doi: 10.1289/ehp.11813
52. Zeger SL, Thomas D, Dominici F, Samet JM, Schwartz J, Dockery D, et al. Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Perspect. (2000) 108:419–26. doi: 10.1289/ehp.00108419
Keywords: time-series study, outpatient, air pollution, short-term, children
Citation: Chen S, Xu B, Shi T and Yang Q (2023) Short-term effect of ambient air pollution on outpatient visits for children in Guangzhou, China. Front. Public Health 11:1058368. doi: 10.3389/fpubh.2023.1058368
Received: 30 September 2022; Accepted: 03 January 2023;
Published: 20 January 2023.
Edited by:
Yunquan Zhang, Wuhan University of Science and Technology, ChinaCopyright © 2023 Chen, Xu, Shi and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiaoyuan Yang,  qiaoyuan_yang@gzhmu.edu.cn
qiaoyuan_yang@gzhmu.edu.cn
 Sili Chen1
Sili Chen1 Qiaoyuan Yang
Qiaoyuan Yang