- 1Department of Biomedical Sciences, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- 2Department of Clinical Midwifery, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- 3Department of Reproductive Health and Nutrition, School of Public Health, Woliata Sodo University, Woliata Sodo, Ethiopia
- 4Department of Pharmacy, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- 5Department of Medical Biochemistry, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Pregnant women are a critical part of the community to assess various determinants of their future breastfeeding practice. This study aimed to assess the levels and determinants of breastfeeding knowledge, attitude, and intention among pregnant women.
Methods: A hospital-based cross-sectional study was conducted among 422 pregnant women from January 18 to February 27, 2022, at Debre Tabor Comprehensive Specialized Hospital (DTCSH) in Northwest Ethiopia. Data were collected via face-to-face interviews from participants selected by convenience sampling technique. Data analysis was made using Stata version 16.0. Multiple logistic regression analysis was used to assess the determinants of the knowledge, attitude, and intention of pregnant women, with a p-value < 0.05 considered statistically significant.
Result: About 57.8% of participants had adequate breastfeeding knowledge and only 46.9% had a positive attitude. Almost two-thirds (65.4%) of them had good intentions to breastfeed. Pregnant women attaining secondary education (AOR = 2.0; 95% CI: 1.31, 3.19), achieving college or university education (AOR = 3.13; 95% CI: 1.63, 7.41), being multiparous (AOR = 2.11; 95% CI: 1.33, 3.43), having four or more ANC visits (AOR:1.45; 95% CI: 1.21, 4.31), and having prior breastfeeding experience (AOR: 3.53; 95% CI: 2.22, 5.65) were significant predictors of adequate knowledge. Attending college or university education (AOR = 2.71;95% CI: 2.33, 5.13), being multiparous (AOR = 1.56; 95% CI: 1.32, 8.25), and having adequate knowledge (AOR = 2.02; 95% CI: 1.88,7.14) were determinants of a positive breastfeeding attitude. Whereas, advanced age (AOR = 1.44; 95% CI: 1.12, 5.59), adequate knowledge (AOR: 5.21; 95% CI: 1.51,8.04), and positive attitude (AOR = 2.41;95% CI:1.50, 4.27) were independent predictors of good breastfeeding intention.
Conclusion: The breastfeeding knowledge and attitude of pregnant women were generally suboptimal. Their overall breastfeeding intention was also unsatisfactory. This highlights the need to develop culture-specific interventions aimed at improving breastfeeding knowledge, attitudes, and intention to enhance the appropriate breastfeeding practice of their future children.
Introduction
Appropriate breastfeeding practice involves exclusive breastfeeding (EBF) of infants for the first 6 months of life and continuing breastfeeding up to 2 years or beyond, with the introduction of complementary food at the age of 6 months (1). Appropriate breastfeeding practice is the most effective global public health intervention to ensure optimal health and development in infants (2–4). It decreases the risk of developing illnesses and disease severity during childhood, and has the highest life-saving potential by avoiding half a million infant deaths and 13% of child deaths globally (5–8).
Even though appropriate infant feeding practice is the most cost-effective intervention, its global implementation is still suboptimal (9, 10). Suboptimal infant feeding practices adversely affect the child's health and nutritional status, mainly in the first year of life (11). Breastfeeding in Ethiopia is a common practice by the majority of mothers, but appropriate breastfeeding remains disproportionately low. Nearly 70% of infants in Ethiopia were reported to be suboptimally breastfed and 24% of infant mortality and 58% of child mortality were attributed to poor and inappropriate breastfeeding practice (12, 13). This may be due to various factors affecting optimal breastfeeding traditions.
Appropriate breastfeeding practice is highly influenced by various psychosocial factors, including breastfeeding knowledge, attitude, and intention/decision (14, 15). Women begin motherhood with infant feeding knowledge and attitudes that they have adopted passively throughout their lives as part of their larger social, cultural, and environmental context (16). This concept may also be supplemented during pregnancy by prenatal advice from health professionals. More importantly, proactive personal information-seeking during pregnancy and early infancy may lead to the acquisition of knowledge and attitudes (17). The acquired maternal knowledge and attitudes toward breastfeeding are likely to influence their breastfeeding decisions and ultimately their breastfeeding behavior (18).
Breastfeeding intention is regarded as a primary driver that determines women's breastfeeding behavior. Health behaviors, in general, and breastfeeding practice, in particular, are unlikely to occur without the intention of attaining them (19–24). Based on the Theory of Planned Behavior and Theory of Reasoned Action, the intention is found to be a good predictor of behavior that plays a critical role in determining breastfeeding behavior (20, 25). Breastfeeding decisions of the future mothers are usually made before conception per their socio-cultural context before the birth of the baby, during pregnancy, or even before (26). The stronger the intention to breastfeed during the prenatal period, the more likely the mother will exclusively breastfeed after the baby is born (27). However, intention by itself is many steps distant from implementation since various individual-level variables are known to affect breastfeeding decisions, including women's sociodemographic factor and their current breastfeeding knowledge and attitude (28, 29). Thus, breastfeeding intention and its antecedents are modifiable factors that can be used as a point of programmatic intervention to enhance breastfeeding (30–32).
Several studies on breastfeeding knowledge, attitude, and intention have been undertaken among pregnant women globally (19, 33–38). But there is a paucity of data in Ethiopia that shows the levels of breastfeeding knowledge, attitude, and intention among pregnant women. Hence, this study aimed to assess breastfeeding knowledge, attitude, intention, and determinants among pregnant women. Gaining a deeper insight on levels and specific determinants of breastfeeding knowledge, attitude, and intention during pregnancy is crucial for policymakers to design area-appropriate programmatic interventions aimed to foster the mothers' preparation for breastfeeding.
Methods and Materials
Study Design, Period, and Setting
A hospital-based cross-sectional study was done from January 18 to February 27, 2022, at the Debre Tabor Comprehensive Specialized Hospital (DTCSH) in Debre Tabor Town, Northwest Ethiopia. DTCSH is currently providing comprehensive healthcare services for about 2.3 million people. It comprises outpatient, inpatient, and emergency departments, delivering antenatal care (ANC), delivery, laboratory, ART, psychiatry, pharmacy, radiology, and other services. This study was conducted particularly in the maternal and child health (MCH) clinic of DTCSH among pregnant women who came for ANC service.
Population
All pregnant women who had attended the MCH clinic of DTCSH for ANC service were considered as the source population, while all pregnant women who visited the MCH clinic of DTCSH and who were available during the study period were taken as the study population.
Inclusion and Exclusion Criteria
All volunteer pregnant women (aged 18 years or above) who came for ANC visits at DTCSH were included in this study. However, women who had severe medical or psychiatric illnesses were excluded from the study. Besides, pregnant women aged <18 years were excluded from the study, since their educational level is lower and their knowledge, attitude, and decision-making ability about breastfeeding are most likely different from that of older women.
Study Variables
Breastfeeding knowledge, attitude, and intention of participants were taken as dependent variables. But sociodemographic characteristics (age, marital status, religion, ethnicity, education, occupation, and residence) and obstetric history (gestational age, gravidity, parity, medical illness, number of ANC visits, breastfeeding experience, place of delivery, and mode of delivery of their last-child) were considered as independent variables in all regression analyses. Whereas, breastfeeding knowledge was taken as an independent variable during the analysis of attitude and intention as outcome variables. The attitude was considered as a predictor variable to check its association with breastfeeding intention.
Sample Size Determination and Sampling Procedures
The sample size was calculated using the single population proportion formula:
Where n is the sample size; Z1−α/2 is the standard normal variable, at 95% confidence level = 1.96; P is the estimated proportion of mothers with adequate breastfeeding knowledge (P = 52.4%) from a prior study (36); and d is the margin of error = 0.05. The calculated sample size was 422 after adding a 10% non-response rate. A convenience sampling technique was used to recruit participants during data collection.
Data Collection Tools and Procedure
Data were collected using a pretested questionnaire prepared in the local Amharic language through face-to-face interviews by three trained nurses normally working at the MCH clinic of DTCSH. The questionnaire was designed to collect data on sociodemographic characteristics, obstetric history, and prior breastfeeding experience of respondents. Besides, the questionnaire involved the validated Amharic version of the Breastfeeding Knowledge Questionnaire (BFKQ-A) to measure their knowledge, Iowa Infant Feeding Attitude Scale (IIFAS-A) to assess attitude, and locally adapted questions for breastfeeding intention (39).
The BFKQ-A consists of 10 multiple-choice questions and 10 true-false questions, with scores ranging from 0 to 20 and higher scores indicating better knowledge about breastfeeding. The BFKQ-A measure has been shown to have adequate reliability in the Ethiopian context, with Cronbach's α of 0.81 and 0.79 in our evaluation and previous Ethiopian study, respectively (39). Participants who responded to the “correct” answers to any of the 20 questions were given a score of 1 and “wrong” responses to any of these questions were given a score of 0. The total BFKQ-A score of all respondents was categorized as adequate knowledge, if they scored the median value (correctly answered 10 questions) of the total BFKQ-A scale or above, otherwise considered as having inadequate knowledge of breastfeeding (36).
On the other hand, the validated Amharic version IIFAS-A consists of 17 items with a five-point Likert scale, ranging between 1 (strongly disagree) and 5 (strongly agree). The scale was found to be a valid and reliable measure of an individual's attitude toward breastfeeding in the Ethiopian context, with acceptable internal consistency in this study (Cronbach's α = 0.80) and a prior study in Ethiopia (Cronbach's α = 0.72) (39). The IIFAS score ranges from 17 to 85 and the attitudes of pregnant women were classified as a positive attitude (if the IIFAS score ≥70) and a negative attitude (if the IIFAS score <70) toward breastfeeding (14).
The breastfeeding intention of participants was assessed using a questionnaire constructed by reviewing other published literature (28, 40), and consisted of eight-point intention scale questions, with scores ranging from 0 to 8. A score of 1 point was given for each correct response and 0 for any incorrect or “undecided” responses to each question. The overall score was categorized into good breastfeeding intention, when participants scored ≥ midpoint of the scale (median intention scale = 4), and poor breastfeeding intention, when participants scored below the midpoint of the scale. Cronbach's alpha for this set of questions was 0.83, indicating an acceptable internal consistency.
Data Processing and Analysis
The collected data were first checked for completeness and internal consistency and then cleaned data were entered into Epi Info version 7.2.4.0 and exported into Stata version 16.0 software for statistical analysis. Summary statistics were reported using frequency and percentage for categorical variables and using mean and standard deviation (SD) to describe continuous variables. A logistic regression model was used to identify determinants of breastfeeding knowledge, attitude, and intentions. Those variables with a p-value of 0.2 in simple regression were entered into multiple regression models. Using multiple logistic regression, the results were expressed as adjusted odds ratio (AOR) with 95% confidence intervals (CI) and p-values. P-values <0.05 were considered statistically significant.
Data Quality Management
Data were collected using a structured questionnaire prepared in English and translated into Amharic and then retranslated back into English to check its consistency. Questionnaires were checked and made comments for content validity by an expert panel. In addition, to ascertain the understanding, validity, and reliability of the questionnaire and to examine practical issues in selecting participants, a pilot study was carried out before the actual data collection period among 25 pregnant women in Addis Zemen Primary Hospital. Before the initiation of data collection, extensive training was given to data collectors and supervisors to enable them to have an understanding of the objectives of the study and each of the questionnaires. All the data collection was done by three trained nurses under the supervision of two trained supervisors during the data collection period. Questionnaires were checked daily for completeness, and daily feedback on data collection activities was given by supervisors.
Ethical Approval and Consent to Participate
The study was conducted after getting ethical approval from the Ethical Review Committee of Debre Tabor University and also a written collaboration letter was obtained from the DTCSH administrative office. Written informed consent was taken from each selected participant after a brief explanation of the study objective. Participants were also informed that participation is voluntary that they can withdraw from the study at any time and that their decision to continue or not in the study will not influence their provision of healthcare services. Confidentiality of information as well as anonymity of the data collection procedure were kept. Appropriate infection prevention measures and principles related to COVID-19 were also considered during data collection.
Results
Sociodemographic Characteristics
A total of 422 participants have completed the questionnaire and were included in this study. The mean (±SD) age of the respondents was 30.1 ± 5.02 years and the age ranged from 18 to 51 years. Most of the participants were Orthodox Christian 408 (96.7%), married 412 (97.6%), and Amhara ethnicity 416 (98.6%). The greatest proportion of respondents had achieved primary education 167 (39.6%) and a sizable portion were housewives 187 (44.3%) and urban dwellers 273 (64.3%) (Table 1).
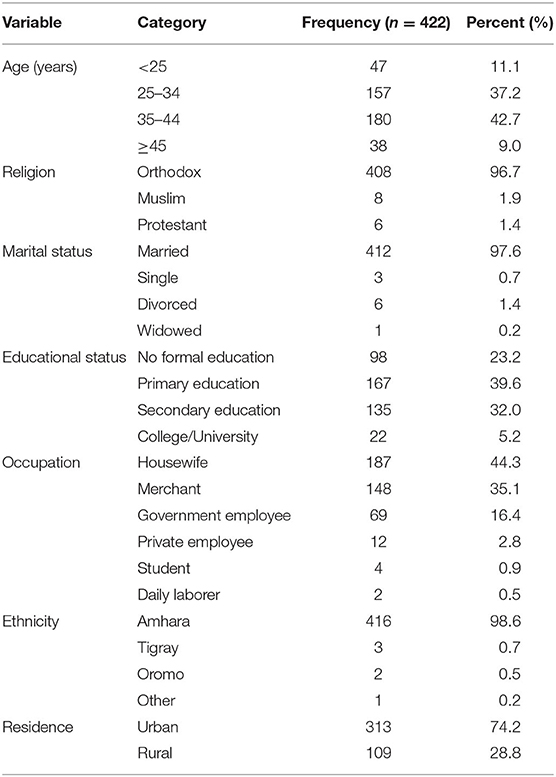
Table 1. Sociodemographic characteristics of pregnant women attending the MCH clinic of DTCSH in Debre Tabor, Northwest Ethiopia, 2022.
Obstetric and Breastfeeding History
A total of 371 (87.9%) women were multigravida who had a history of two or above pregnancies, including the current one. About 57 (13.5%) participants were nulliparous who never had a live birth, but the majority 365 (86.5%) were primiparous who had a prior history of one live birth and multiparous having two or above live births. Almost all 415 (98.3%) respondents had planned current pregnancy. Nearly half 208 (49.3%) of them were in the third trimester (≥28 weeks) of the current pregnancy. Above half 245 (58.1%) of women were having <4 ANC visits at the time of the interview. Around 94.1% of them replied that they did not experience any medical illness during their current pregnancy. Of those women who had a prior history of delivery, most of them gave birth to their last child vaginally (90.1%) in health institutions (86.6%). About 86.5% had prior breastfeeding experience (Table 2).
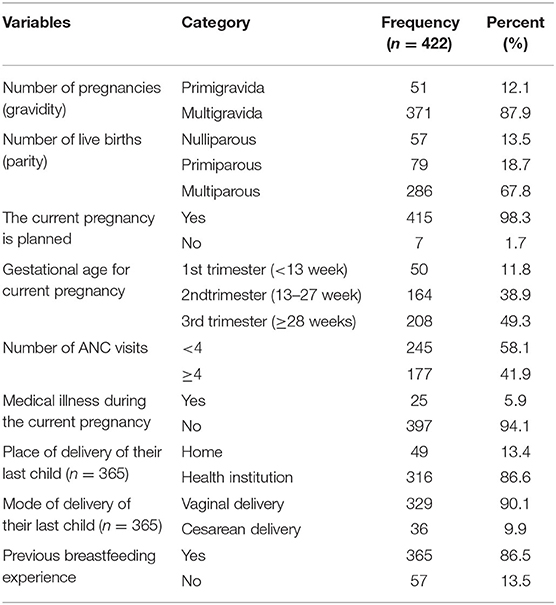
Table 2. Obstetric and breast-feeding history of pregnant women attending the MCH clinic of DTCSH in Debre Tabor, Northwest Ethiopia, 2022.
Knowledge About Breastfeeding
The BFKQ-A scores of the study participant ranged between 4 and 18, with a mean ±SD score of 11.0 ± 4.8. Two hundred forty-four (57.8%) of the study participants were evaluated to have adequate knowledge, the remaining 178 (42.2%), however, were below the median score and considered to have inadequate knowledge (Figure 1). Generally, the knowledge scale pertained to the domains of the benefits of breastfeeding to the baby, and effective feeding was the most high-scoring item (highest mean ± SD score). Whereas, the knowledge domains including the benefits of breastfeeding to the mother, problems with breastfeeding, colostrum, breast milk expression, breast engorgement, and the practical aspect of breastfeeding were shown to be low-scoring items (lowest mean ± SD score). For instance, the majority of the study participant was not aware that breastfeeding reduces the risk of bleeding after childbirth and achieves pre-pregnancy weight faster with breastfeeding, which accounted for 71.3% and 75.2%, respectively. Similarly, about 79.3% of participants generally have poor knowledge regarding breast milk expression. A sizable proportion (61.7%) of women also did not know about the need for water after each breastfeeding. Another knowledge gap among participants was indicated by the belief that colostrum is difficult to digest by the baby and needs to be discarded, which took 45.5%. The main source of information for respondents regarding breastfeeding was health workers followed by mass media and family or neighbors, accounting for 298 (70.6%), 244 (57.8%), and 114 (27.0%), respectively (Figure 2).
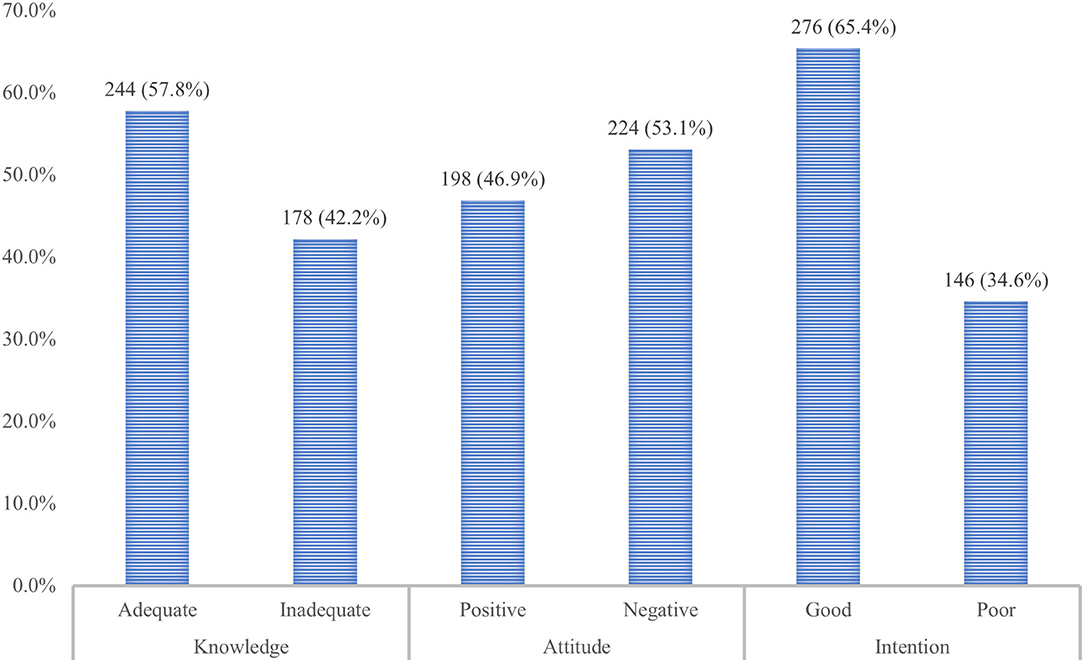
Figure 1. The overall breastfeeding knowledge, attitude, and intention of pregnant women attending the MCH clinic of DTCSH in Debre Tabor, Northwest Ethiopia, 2022.
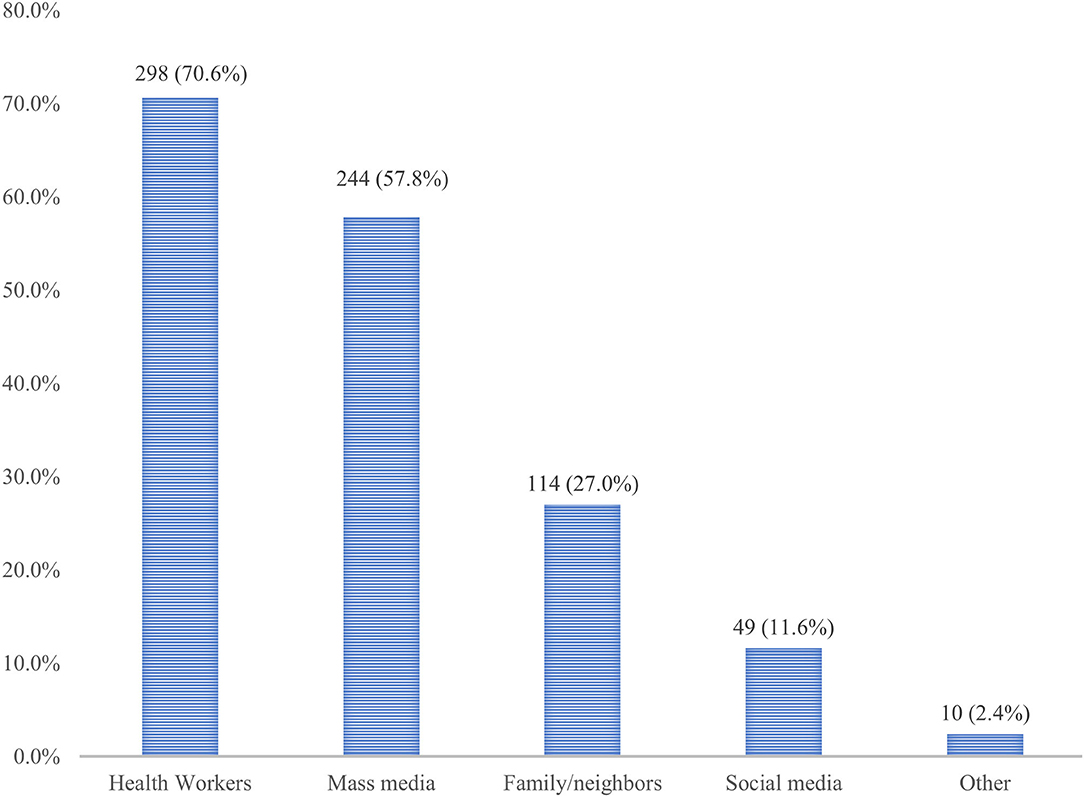
Figure 2. Source of information regarding breastfeeding among pregnant women attending MCH clinic of DTCSH in Debre Tabor, Northwest Ethiopia, 2022.
Attitude Toward Breastfeeding
The overall IIFAS-A score in our study ranged from 31 to 82, with a mean ± SD value of 54.7 ± 3.12. The overall attitude score indicated that only 198 (46.9%) of respondents had a positive attitude toward breastfeeding, while more than half 224 (53.1%) of them had a negative attitude toward breastfeeding (Figure 1). There were some IIFAS-A items with the highest mean ± SD, involving perceived breastfeeding as the ideal food for babies (90.1%), improving the health of the baby than formula-fed babies (87.1%), an important bonding factor between the mother and baby (86.4%), and one of the great joys of motherhood (83.1%). There were, however, some misconceptions explained with the lowest means ± SD and perceived as barriers to continuing breastfeeding. For example, nearly half (51.3%) of them agreed that a mother who occasionally consumes alcohol should not breastfeed her baby. Almost two-thirds (67.9%) of participants also disagreed that formula feeding is a better choice for women who plan to work.
Intention to Practice Breastfeeding
The breastfeeding intention scores of the participants ranged between 3 and 8, with the mean ± SD of the intention scale being 5.4 ± 2.41. Overall, nearly two-thirds (65.4%) of study participants had a good intention to breastfeed, while the remaining (34.6%) were considered to have a poor intention (Figure 1). The study also showed that almost all (99.1%) participants intended to breastfeed their future child. But only a bit more than one-third (37.7%) of them had the intention to initiate breastfeeding within an hour of birth, while 41.0% will introduce breast milk after 1 h of birth and 21.3% were yet to decide. About 77.3% of participants intended to breastfeed exclusively, whereas 13.5% were still uncertain (Table 3).
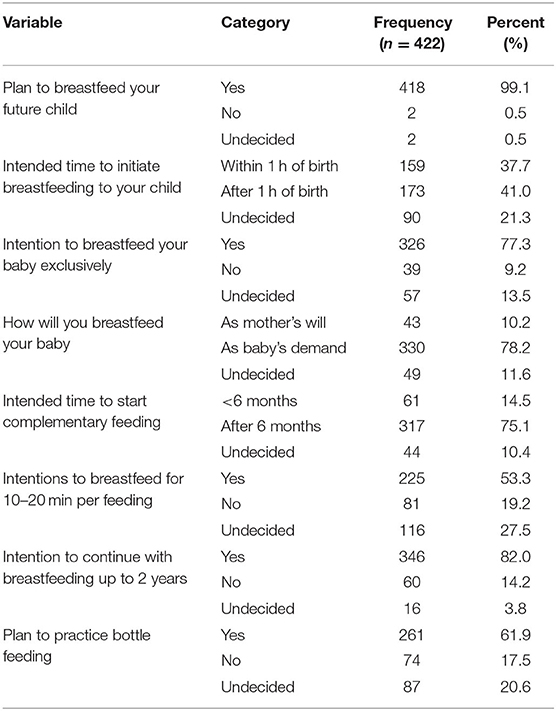
Table 3. Breastfeeding intention among pregnant women attending the MCH clinic of DTCSH in Debre Tabor, Northwest Ethiopia, 2022.
Factors Associated With Breastfeeding Knowledge, Attitude, and Intention
Maternal age, marital status, education, occupation, residence, gestational age, planned current pregnancy, medical illness during the current pregnancy, place of delivery, mode of delivery, parity, and breastfeeding history were entered into the logistic regression model and their associations with breastfeeding knowledge, attitude, and intention were first assessed using simple logistic regression analysis. Those variables with p-values ≤ 0.2 in the simple logistic regression were entered into multiple logistic regression models to control the possible confounders and to assess the factors associated with breastfeeding knowledge, attitude, and intention by expressing the results as AOR with 95% CI and p-values (Table 4). Accordingly, educational status, parity, number of ANC visits, and prior breastfeeding experience were significantly associated with the breastfeeding knowledge of participants. Participants who attended secondary education or college/university were two times (AOR = 2.0; 95% CI:1.31,3.19; p <0.05) and three times (AOR = 3.13; 95% CI: 1.63, 7.41; p <0.01), respectively, more likely to have adequate breastfeeding knowledge than those who did not attend any formal education. Multiparous women had two times (AOR = 2.11; 95% CI: 1.33, 3.43; p <0.05) more likelihood of having adequate knowledge compared to nulliparous mothers. Women with four or higher ANC visits had 1.45 times (AOR:1.45; 95% CI:1.21,4.31; p <0.05) more likely to have adequate knowledge than their counterparts. The odds of mothers who had prior breastfeeding experience having adequate knowledge was 3.53 times (AOR: 3.53; 95% CI: 2.22,5.65; p <0.01) more than those who never had experience.
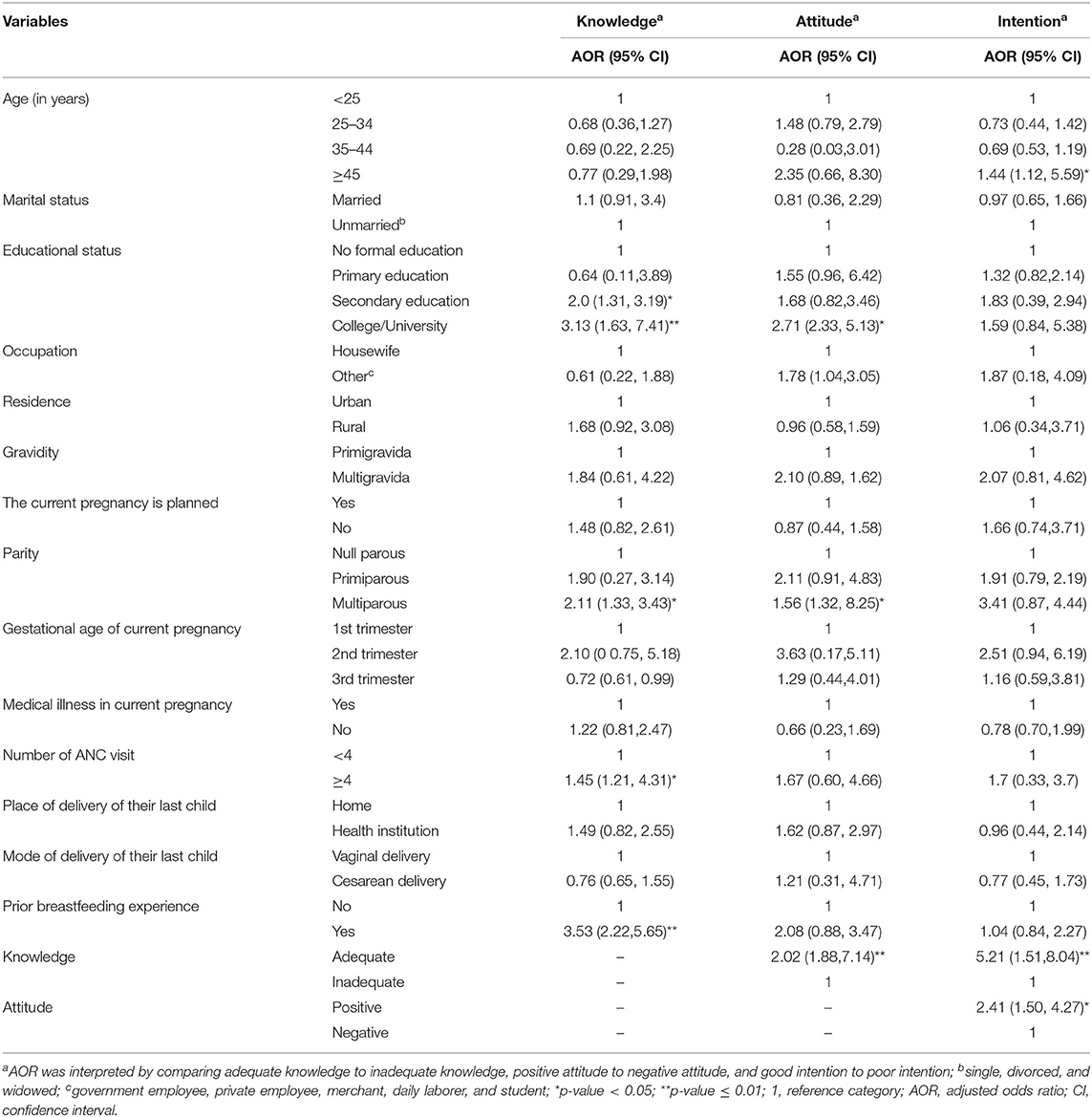
Table 4. Factors associated with breastfeeding knowledge, attitude, and intention among pregnant women attending the MCH clinic of DTCSH in Debre Tabor, Northwest Ethiopia, 2022.
The study also showed that maternal educational status, parity, and knowledge were significant predictors of breastfeeding attitudes. Women who attended college or university education were 2.71 times (AOR = 2.71; 95% CI: 2.33, 5.13; p < 0.05) more likely to have a positive attitude toward breastfeeding than those with no formal education. Compared to nulliparous women, multiparous women had 1.56 times (AOR = 1.56; 95% CI:1.32, 8.25; p < 0.05) greater likelihood of having a positive attitude. Likewise, the odds of having a positive attitude toward breastfeeding were about two times (AOR = 2.02; 95% CI:1.88,7.14; p < 0.01) higher in women with adequate knowledge than their counterparts. In addition, maternal age, breastfeeding knowledge, and attitude were observed to be statistically significant predictors of the intention to practice breastfeeding. Expectant women aged 45 years or above had 1.44 times (AOR = 1.44; 95% CI: 1.12, 5.59; p < 0.05) higher odds than those with age below 25 years. The odds of having good breastfeeding intention among women who had adequate knowledge were 5.21 times (AOR: 5.21, 95% CI: 1.51,8.04; p < 0.01) higher than those with inadequate knowledge. Those who had positive breastfeeding attitudes were a 2.41-fold (AOR = 2.41;95% CI: 1.50, 4.27; p < 0.05) greater likelihood to have good breastfeeding intention than those with a negative attitude.
Discussion
Women begin motherhood with infant feeding knowledge and attitudes that they have adopted during their lives and make breastfeeding decisions before the birth of the child, prenatally if not pre-conceptually. Therefore, this study was aimed at evaluating the levels and determinants of breastfeeding knowledge, attitudes, and intentions among pregnant women. Our study revealed that about 57.8% of pregnant women had adequate knowledge regarding breastfeeding. This is nearly equivalent to the study done in Calabar, Nigeria (56.8%) (41), Gambia (60.2%) (32), and Moshi, Tanzania (61.2%) (42). But the result is larger than that of a similar study done in the Mana district of South West Ethiopia (52.4%) (36). These contrasting findings in the same country could be due to the difference in study settings in which the current study was conducted in those women who came to the hospital for ANC follow-up, who are expected to have good health-seeking behavior and may have a good opportunity to discuss with health professionals about breastfeeding and are more likely to have adequate knowledge. Besides, unlike our study, which was done in an urban area, the latter study was conducted in a rural community. Our result is also higher than the findings from Ibadan in Nigeria (43.1%) (28), Egypt (33.3%) (43), Lebanon and Qatar (25%) (33), and Northern Portugal (40%) (37), but it is lower than the figures from Nigeria (71.3%) (44), Saudi Arabia (86%) (45), and Jordan (78%) (38). This may be attributed to the difference in media exposure, sociodemographic variables (such as education), and knowledge assessment scale and criteria.
In the current study, educational status, parity, number of ANC visits, and prior breastfeeding experience were independently associated with the breastfeeding knowledge of pregnant women. Adequate breastfeeding knowledge was more likely found in women with higher education compared to those who did not attend any formal education. Although the study by Omoronyia et al. (41) observed no significant correlation, several prior studies have shown educational status as a significant predictor of breastfeeding knowledge (37, 46). This may be because women who had attained higher education can easily be well informed about breastfeeding and hence acquire knowledge (20). Thus, pregnant women with no formal education should be given special attention and receive extensive breastfeeding advice during their prenatal visit, as they are less likely to acquire breastfeeding knowledge.
This study further indicated that the parity of women was significantly associated with the level of breastfeeding knowledge, with multiparous women having a more likelihood of having adequate knowledge than their counterparts. In contrast, there was no significant association between the level of knowledge and the parity of women (41). Another study undertaken in Nigeria, on the other hand, reported similar results to our findings (40). Consistently, prior breastfeeding experience was reported to be a significant predictor of adequate knowledge of respondents. This is likely due to the more experiences of motherhood, the more likelihood of having adequate breastfeeding knowledge. This study also reported that mothers with four or higher ANC visits had significantly more odds of having adequate knowledge and this corroborated with a prior study conducted in Southwest Ethiopia (36). The likely explanation is that ANC visits create the best opportunities for pregnant women to get appropriate key breastfeeding messages from the health personnel and thus, women with a greater number of ANC follow-up may have more likelihood to get breastfeeding education. However, this finding is inconsistent with the study done in Nigeria that shows no significant association between ANC visits and breastfeeding knowledge (40).
The overall positive attitude of participants toward breastfeeding in this study was 46.9%. This value is higher than the study finding in Nigeria (7.4%) (41), Southwest Ethiopia (36.9%) (36), and Lebanon and Qatar (9.2%) (33). However, it is lower than the result from Saudi Arabia (62.2%) (47), South West Nigeria (53.8%) (28), and Jordan (72%) (38). The use of different tools and criteria to categorize attitude levels, as well as differences in sociodemographic factors, could explain this discrepancy. Accumulated evidence indicates a positive relationship between attitude and optimum breastfeeding practices (33, 45, 48). The attitude of mothers toward breastfeeding predicts appropriate breastfeeding practices of the expecting mothers, and the attitudes could in turn are affected by various factors. In this study, educational status, parity, and breastfeeding knowledge were found to be significant predictors of their attitude.
Educational status is an independent predictor of a positive attitude toward breastfeeding, implying that women with higher education had more odds of having a positive attitude than those with no education. This is in line with previous studies conducted in Lebanon (49), Ireland (50), China (51), Singapore (52), and Spain (53). A prior study in Ethiopia also indicates that women with lower educational status had a lower attitude score, though not significant (36). One possible explanation is that women with higher educational levels are more likely to adopt an infant feeding attitude via proactive information-seeking behavior that changes their attitudes (17, 54). This study further found that multiparous women had a more positive breastfeeding attitude than nulliparous women, which keeps up with another study done in China (51). This is more likely as a result of multiparous women with better information or prior breastfeeding experience would positively reinforce their attitudes. This is opposing another study done in Southwest Ethiopia, reporting that multiparous women have less positive attitudes than their counterparts (36). This discrepancy could be due to the difference in the study settings. Our study was conducted in the urban area as opposed to the rural area in the earlier study, and so mothers are expected to be less busy with work compared to rural women.
Women with adequate breastfeeding knowledge were also a significant determinant of positive attitude toward breastfeeding. This finding is consistent with a survey done in Saudi Arabia (55), the US (56), Ethiopia (36), and Nigeria (28). This corroborates the theory of the knowledge-attitude-behavior paradigm, which assumes that knowledge of individuals' health is a key factor in engaging in a particular health-related behavior (57). In particular, pregnant women with adequate knowledge can better understand the potential benefits of breastfeeding, resulting in a favorable breastfeeding attitude. Conversely, women with inadequate levels of knowledge may not comprehend the benefits of breastfeeding; instead, they may overconfidently stick to their socio-culturally based misconception (58, 59). But a study from Calabar, Nigeria, documented no significant relationship between infant feeding knowledge and attitude (41).
The study also reported that the intention to practice breastfeeding among pregnant women was 65.4%, suggesting that a greater proportion of women would have a less likelihood to appropriately breastfeed their expecting babies. This figure is lower than the study done in the US (73%) (34), Jordan (75%) (60), and even more significantly lower than Australia (95%) (19), China (99.1, 73.2, and 92.17%) (46, 61, 62), Saudi Arabia (80.8%) (63), and Brazil (96.5% and 98.5%) (64–66). But our finding is higher than the findings from the US (53%) (35), Nigeria (35.7%) (28), and Gambia (38.6%) (32). Differences in intention measuring scales and categories, variation in sociodemographic variables, discrepancies in breastfeeding promotion, and differences in study participants may explain these disparities.
Breastfeeding intention is a well-known determinant of breastfeeding practice that can be influenced by a variety of interwoven factors (21–24). In this study, the main identified factors that influenced breastfeeding intention were age, breastfeeding knowledge, and attitude. It has been found that older women had higher odds of intending to breastfeed than younger ones. This is corroborated by other studies that show that advanced maternal age is a significant predictor of good breastfeeding intention (60, 63, 64). This might be explained by the fact that breastfeeding is, in many aspects, learned behavior and so old mothers are likely linked to prior breastfeeding experience that influences their intention to breastfeed. In contrast, other reports demonstrate that older women are less likely to breastfeed (32, 40, 67, 68). Another study revealed no association between maternal age and breastfeeding intention (35).
The current study also revealed that breastfeeding knowledge is significantly associated with the intention to breastfeed. Women with adequate knowledge are more likely than their counterparts to have a good breastfeeding intention, confirming that prenatal breastfeeding knowledge has a significant influence on breastfeeding decisions. This agrees with other studies, showing a link between prenatal breastfeeding knowledge and intention (19, 22, 28, 60, 69). Attitude is a measurable factor that has been shown to influence behavior through intention (70). According to the planned behavior theory, along with subjective norms and perceived behavioral control, attitude is suggested to be a strong predictor of maternal intention to breastfeed. In turn, the intention is thought to be a key determinant factor of immediate behavior. This link between attitude and intention has been established by numerous prior studies for different health-related behaviors, such as infant feeding practice (19, 20, 22, 26, 32, 38, 71, 72). Similarly, we found a significant association between prenatal breastfeeding attitude and intention, with those who had positive attitudes having a good intention to breastfeed than those with negative attitudes.
Limitation of the Study
This study has certain drawbacks, despite its inherent strengths. One is that the study employed a cross-sectional study design that inherently limits the temporal relationship between cause and effect. The actual breastfeeding practice and its determinants were not assessed since the study was conducted among pregnant women and was not prospective. Besides, the study findings may be limited in the representativeness of the general population due to the small sample size, use of convenience sampling method, and a hospital-based study.
Conclusion
In general, the level of adequate knowledge and positive attitudes toward breastfeeding were suboptimal. The overall breastfeeding intention of pregnant women was also unsatisfactory, suggesting that women would have a lower likelihood of breastfeeding their expecting babies appropriately. Educational status, parity, number of ANC visits, and prior breastfeeding experience were identified as significant determinants of breastfeeding knowledge. Whereas, educational status, parity, and knowledge were found to be significant predictors of breastfeeding attitude. Age, breastfeeding knowledge, and attitude, on the other hand, were observed to be significantly associated with the intent to practice appropriate breastfeeding.
Since breastfeeding intention is an immediate predictor of future behavior, more emphasis needs to be directed toward breastfeeding promotion during the prenatal period. Although the road between intention and behavioral outcomes is hard, breastfeeding knowledge and attitudes can be changed and improved through prenatal education. Thus, the authors strongly believe in the need for continuous education for pregnant women by healthcare personnel during their ANC visits to encourage breastfeeding practice. This highlights the need for policymakers and managers to devise culture-specific interventions and policies aimed at improving women's breastfeeding knowledge and attitudes, and hence their intention to breastfeed their future babies. We also suggest that large-scale, community-based follow-up studies should be done to assess the impact of these factors on actual breastfeeding practice after a child's birth.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethical Review Committe of Debre Tabor University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
EC contributed to study conception and design and manuscript drafting. GAy, GAs, and TA were involved in manuscript preparation, tables and figures, and critical revision.TM, ZT, AB, and AT contributed to the literature search and manuscript writing. EC, GAy, GAs, TA, TM, ZT, AB, and AT involved in data analysis. TM, ZT, AB, and AT contributed to the interpretation. All authors were involved in reviewing the final draft of the manuscript, revision of the manuscript, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are very grateful for Debre Tabor University, DTCSH staff, study participants, and data collectors.
Abbreviations
ANC, Ante Natal Care; AOR, Adjusted Odds Ratio; BFKQ-A, Breastfeeding Knowledge Questionnaire-Amharic version; CI, Confidence Interval; DTCSH, Debre Tabor Comprehensive Specialized Hospital; EBF, Exclusive Breastfeeding; IIFAS-A, Iowa Infant Feeding Attitude Scale Amharic version; MCH, Maternal and Child Health; SD, Standard Deviation.
References
1. World Health Organization. Indicators for Assessing Infant and Young Child Feeding Practices: Part 1: Definitions: Conclusions of a Consensus Meeting Held 6–8 November 2007. Washington DC, USA: World Health Organization (2008).
2. Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev. (2012). 2012:CD003517. doi: 10.1002/14651858.CD003517.pub2
3. Kramer MS, Aboud F, Mironova E, Vanilovich I, Platt RW, Matush L, et al. Breastfeeding and child cognitive development: new evidence from a large randomized trial. Arch Gen Psychiatry. (2008) 65:578–84. doi: 10.1001/archpsyc.65.5.578
4. Dewey KG, Huffman SL. Maternal, Infant, and Young Child Nutrition: Combining Efforts to Maximize Impacts on Child Growth and Micronutrient Status. Los Angeles, CA: SAGE Publications (2009). p. S187-S9.
5. Alemayehu T, Haidar J, Habte D. Determinants of exclusive breastfeeding practices in Ethiopia. Ethiopian J. Health Dev. (2009) 23. doi: 10.4314/ejhd.v23i1.44832
6. Clark SG, Bungum TJ. Benefits of breastfeeding. Californian J Health Promot. (2003) 1:158–63. doi: 10.32398/cjhp.v1i3.527
7. Hafizan N, Telba Z, Sutan R. Socio-demographic factors associated with duration of exclusive breast feeding practice among mothers in East Malaysia. J Nurs Health Sci. (2014) 31:52–6. doi: 10.9790/1959-03135256
8. Chola L, Nkonki L, Kankasa C, Nankunda J, Tumwine J, Tylleskar T, et al. Cost of individual peer counselling for the promotion of exclusive breastfeeding in Uganda. Cost Effect. Resour Alloc. (2011) 9:1–9. doi: 10.1186/1478-7547-9-11
9. Imdad A, Yakoob MY, Bhutta ZA. Effect of breastfeeding promotion interventions on breastfeeding rates, with special focus on developing countries. BMC Public Health. (2011) 11:1–8. doi: 10.1186/1471-2458-11-S3-S24
10. Organization WH UNICEF. Breastfeeding Advocacy Initiative: For the Best Start in Life. New York, NY: United Nations Children's Fund (UNICEF) (2015).
11. UNICEF. Progress for Children: A Report Card on Nutrition. New York, NY: United Nations Children's Fund (UNICEF) (2006).
12. Teklehaymanot AN, Hailu AG, Wossen BA. Intention of exclusive breast feeding among pregnant women using theory of planed behavior in Medebay Zana district, Tigray region, North Ethiopia. Public Health Res. (2013) 3:162–8.
13. Central Statistical Agency [Ethiopia] and ICF International. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia and Calverton, Maryland, USA: Central Statistical Agency and ICF International (2016).
14. Hamade H, Naja F, Keyrouz S, Hwalla N, Karam J, Al-Rustom L, et al. Breastfeeding knowledge, attitude, perceived behavior, and intention among female undergraduate university students in the Middle East: the case of Lebanon and Syria. Food Nutr Bull. (2014) 35:179–90. doi: 10.1177/156482651403500204
15. Chambers JA, Alder E, Hoddinott P, McInnes R. A systematic review of measures assessing mothers' knowledge, attitudes, confidence and satisfaction towards breastfeeding. Breastfeed Rev. (2007) 15:17–25.
16. Hrdy S. Mother Nature: Natural Selection and the Female of the Species London. London, UK: Chatto and Windus (1999).
17. Gage H, Williams P, Rosen-Von Hoewel V, Laitinen K, Jakobik V, Martin-Bautista E, et al. Influences on infant feeding decisions of first-time mothers in five European countries. Eur J Clin Nutr. (2012) 66:914–9. doi: 10.1038/ejcn.2012.56
18. Kong SK, Lee DT. Factors influencing decision to breastfeed. J Adv Nurs. (2004) 46:369–79. doi: 10.1111/j.1365-2648.2004.03003.x
19. Newby R, Brodribb W, Ware RS, Davies PS. Infant feeding knowledge, attitudes, and beliefs predict antenatal intention among first-time mothers in Queensland. Breastfeed Med. (2014) 9:266–72. doi: 10.1089/bfm.2014.0012
20. Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: an introduction to theory and research. Philos Rhetoric. (1977) 10:130–2.
21. Meedya S, Fahy K, Kable A. Factors that positively influence breastfeeding duration to 6 months: a literature review. Women Birth. (2010) 23:135–45. doi: 10.1016/j.wombi.2010.02.002
22. Donath SM, Amir LH, Team AS. Relationship between prenatal infant feeding intention and initiation and duration of breastfeeding: a cohort study. Acta Paediatr. (2003) 92:352–6. doi: 10.1111/j.1651-2227.2003.tb00558.x
23. Humphreys AS, Thompson NJ, Miner KR. Intention to breastfeed in low-income pregnant women: The role of social support and previous experience. Birth. (1998) 25:169–74. doi: 10.1046/j.1523-536X.1998.00169.x
24. Lee HJ, Elo IT, McCollum KF, Culhane JF. Racial/ethnic differences in breastfeeding initiation and duration among low-income inner-city mothers. Soc Sci Q. (2009) 90:1251–71. doi: 10.1111/j.1540-6237.2009.00656.x
25. Manstead AS, Proffitt C, Smart J. Predicting and understanding mothers' infant-feeding intentions and behavior: testing the theory of reasoned action. J Pers Soc Psychol. (1983) 44:657. doi: 10.1037/0022-3514.44.4.657
26. Dykes F. Breastfeeding in Hospital: Mothers, Midwives and the Production Line. England, UK: Routledge (2006).
27. Ismail TAT, Muda WMW, Bakar MI. Intention of pregnant women to exclusively breastfeed their infants: The role of beliefs in the theory of planned behaviour. J Child Health Care. (2014) 18:123–32. doi: 10.1177/1367493512473857
28. Leshi O, Samuel FO, Ajakaye MO. Breastfeeding knowledge, attitude and intention among female young adults in Ibadan, Nigeria. Open J Nurs. (2016) 6:11–23. doi: 10.4236/ojn.2016.61002
29. Scott J, Colin W. Breastfeeding: reasons for starting, reasons for stopping and problems along the way. Breastfeed Rev. (2002) 10:13–9.
30. Onbasi S, Duran R, Ciftdemir NA, Vatansever U, Acunas B, Sut N. The effect of prenatal breast-feeding and breast-milk training given to expectant mothers on the behaviour of breast-feeding. Turkish Pediatrics Arch. (2011) 75–81.
31. Lin SS, Chien LY, Tai CJ, Lee CF. Effectiveness of a prenatal education programme on breastfeeding outcomes in Taiwan. J Clin Nurs. (2008) 17:296–303. doi: 10.1111/j.1365-2702.2008.02289.x
32. Senghore T, Omotosho TA, Ceesay O, Williams DCH. Predictors of exclusive breastfeeding knowledge and intention to or practice of exclusive breastfeeding among antenatal and postnatal women receiving routine care: a cross-sectional study. Int Breastfeed J. (2018) 13:1–8. doi: 10.1186/s13006-018-0154-0
33. Naja F, Chatila A, Ayoub JJ, Abbas N, Mahmoud A, Abdulmalik MA, et al. Prenatal breastfeeding knowledge, attitude and intention, and their associations with feeding practices during the first six months of life: a cohort study in Lebanon and Qatar. Int Breastfeed J. (2022) 17:1–17. doi: 10.1186/s13006-022-00456-x
34. Sipsma HL, Divney AA, Magriples U, Hansen N, Gordon D, Kershaw T. Breastfeeding intentions among pregnant adolescents and young adults and their partners. Breastfeed Med. (2013) 8:374–80. doi: 10.1089/bfm.2012.0111
35. Lee HJ, Rubio MR, Elo IT, McCollum KF, Chung EK, Culhane JF. Factors associated with intention to breastfeed among low-income, inner-city pregnant women. Matern Child Health J. (2005) 9:253–61. doi: 10.1007/s10995-005-0008-5
36. Abdulahi M, Fretheim A, Argaw A, Magnus JH. Determinants of knowledge and attitude towards breastfeeding in rural pregnant women using validated instruments in Ethiopia. Int J Environ Res Public Health. (2021) 18:7930. doi: 10.3390/ijerph18157930
37. Cardoso A. e Silva AP, Marín H. Pregnant women's knowledge gaps about breastfeeding in northern Portugal. Open J Obstet Gynecol. (2017) 7:376–85. doi: 10.4236/ojog.2017.73039
38. Khasawneh W, Kheirallah K, Mazin M, Abdulnabi S. Knowledge, attitude, motivation and planning of breastfeeding: a cross-sectional study among Jordanian women. Int Breastfeed J. (2020) 15:1–9. doi: 10.1186/s13006-020-00303-x
39. Abdulahi M, Fretheim A, Argaw A, Magnus JH. Adaptation and validation of the Iowa infant feeding attitude scale and the breastfeeding knowledge questionnaire for use in an Ethiopian setting. Int Breastfeed J. (2020) 15:1–11. doi: 10.1186/s13006-020-00269-w
40. Ihudiebube-Splendor CN, Okafor CB, Anarado AN, Jisieike-Onuigbo NN, Chinweuba AU, Nwaneri AC, et al. Exclusive breastfeeding knowledge, intention to practice and predictors among primiparous women in Enugu South-East, Nigeria. J Pregnancy. (2019) 2019:9832075. doi: 10.1155/2019/9832075
41. Omoronyia OE, Ayuk AE, Bisong EM, Nwafor KN. Maternal knowledge of effective breastfeeding and its benefits, as potential determinant of attitudes to infant feeding: a survey in Calabar, Nigeria. Afr J Reprod Health. (2020) 24:69–77. doi: 10.29063/ajrh2020/v24i3.8
42. Hashim TH, Mgongo M, Katanga J, Uriyo JG, Damian DJ, Stray-Pedersen B, et al. Predictors of appropriate breastfeeding knowledge among pregnant women in Moshi Urban, Tanzania: a cross-sectional study. Int Breastfeed J. (2016) 12:1–8. doi: 10.1186/s13006-017-0102-4
43. Mahmoud NA, Megahed NM, Essam MM, Marouf O, Hussein E, Mohamed K, et al. Assessment of knowledge and practice of proper breastfeeding among mothers attending-El-Shohada primary health care units, Ismailia City. IJHS. (2014) 2:70–8.
44. Mbada CE, Olowookere AE, Faronbi JO, Oyinlola-Aromolaran FC, Faremi FA, Ogundele AO, et al. Knowledge, attitude and techniques of breastfeeding among Nigerian mothers from a semi-urban community. BMC Res Notes. (2013) 6:1–8. doi: 10.1186/1756-0500-6-552
45. Karim R, Khan A, Khan B, Ullah A, Afridi M. Knowledge, attitude and practice regarding exclusive breastfeeding among mothers attending tertiary care hospital. J Gandhara Med Dental Sci. (2022) 9:44–8. doi: 10.37762/jgmds.9-1.150
46. Wang Y. You H-x, Luo B-r. Exploring the breastfeeding knowledge level and its influencing factors of pregnant women with gestational diabetes mellitus. BMC Pregnancy Childbirth. (2020) 20:1–9. doi: 10.1186/s12884-020-03430-9
47. Gharaii NR, Hesarinejad Z, Nasibi M, Fakari FR, Ghazanfarpour M, Kargarfard L, et al. A systematic review of factorial structure of the iowa infant feeding attitude scale (IIFAS). Int J Pediatrics. (2018) 6:8413–22. doi: 10.22038/ijp.2018.32706.2888
48. Oche M, Umar A, Ahmed H. Knowledge and practice of exclusive breastfeeding in Kware, Nigeria. Afr Health Sci. (2011) 11:518–23.
49. Charafeddine L, Tamim H, Soubra M. de la Mora A, Nabulsi M, Research, et al. Validation of the Arabic version of the Iowa infant feeding attitude scale among Lebanese women. J Hum Lact. (2016) 32:309–14. doi: 10.1177/0890334415586192
50. Sittlington J, Stewart-Knox B, Wright M, Bradbury I, Scott JA. Infant-feeding attitudes of expectant mothers in Northern Ireland. Health Educ Res. (2007) 22:561–70. doi: 10.1093/her/cyl113
51. Hamze L, Mao J, Reifsnider E. Knowledge and attitudes towards breastfeeding practices: a cross-sectional survey of postnatal mothers in China. Midwifery. (2019) 74:68–75. doi: 10.1016/j.midw.2019.03.009
52. Lau Y, Htun TP, Lim PI, Ho-Lim SST, Klainin-Yobas P. Psychometric properties of the Iowa infant feeding attitude scale among a multiethnic population during pregnancy. J Hum Lact. (2016) 32:315–23. doi: 10.1177/0890334415591813
53. Tomás-Almarcha R, Oliver-Roig A, Richart-Martinez M. Reliability and validity of the reduced Spanish version of the Iowa infant feeding attitude scale. J Obstet Gynecol Neonatal Nurs. (2016) 45:e26–40. doi: 10.1016/j.jogn.2016.08.001
54. Gage H, Raats M, Williams P, Egan B, Jakobik V, Laitinen K, et al. Developmental origins of health and disease: the views of first-time mothers in 5 European countries on the importance of nutritional influences in the first year of life. Am J Clin Nutr. (2011) 94:2018S-24S. doi: 10.3945/ajcn.110.001255
55. Saied H, Mohamed A, Suliman A, Al Anazi W. Breastfeeding knowledge, attitude and barriers among Saudi women in Riyadh. J Nat Sci Res. (2013) 3:6–13.
56. Vandewark AC. Breastfeeding attitudes and knowledge in bachelor of science in nursing candidates. J Perinat Educ. (2014) 23:135–41. doi: 10.1891/1058-1243.23.3.135
57. Bettinghaus EP. Health promotion and the knowledge-attitude-behavior continuum. Prevent Med. (1986) 15:475–91. doi: 10.1016/0091-7435(86)90025-3
58. Chan K, Whitfield KC. High confidence, yet poor knowledge of infant feeding recommendations among adults in Nova Scotia, Canada. Matern Child Nutr. (2020) 16:e12903. doi: 10.1111/mcn.12903
59. Jamil NA. The influence of religious belief and sociocultural on breastfeeding practice: a literature review. Malays J Nurs (MJN). (2018) 9:79–85.
60. Al-Sagarat AY, Yaghmour G, Moxham L. Intentions and barriers toward breastfeeding among Jordanian mothers—A cross sectional descriptive study using quantitative method. Women Birth. (2017) 30:e152–e7. doi: 10.1016/j.wombi.2016.11.001
61. Dai H, Hu H. Clinical analysis of breastfeeding in pregnant women with gestational diabetes mellitus. Matern Child Health Care China. (2012) 27:1001–3.
62. Zhang S. Study on breastfeeding status and influencing factors of pregnant women with diabetes mellitus at different postpartum stages. Matern Child Health Care China. (2015) 30:5765–7.
63. Alnasser Y, Almasoud N, Aljohni D, Almisned R, Alsuwaine B, Alohali R, et al. Impact of attitude and knowledge on intention to breastfeed: can mHealth based education influence decision to breastfeed exclusively? Ann Med Surg. (2018) 35:6–12. doi: 10.1016/j.amsu.2018.09.007
64. Moimaz S, Rocha N, Garbin C, Rovida T, Saliba N. Factors affecting intention to breastfeed of a group of Brazilian childbearing women. Women Birth. (2017) 30:e119–e24. doi: 10.1016/j.wombi.2016.10.004
65. Issler H. Sá MBSRd, Senna DM. Knowledge of newborn healthcare among pregnant women: basis for promotional and educational programs on breastfeeding. São Paulo Med J. (2001) 119:07–9. doi: 10.1590/S1516-31802001000100003
66. Machado AKF, Elert VW, Pretto ADB, Pastore CA. Intention to breastfeed and complementary feeding of postpartum women in a teaching hospital in southern Brazil. Ciência Saúde Coletiva. (2014) 19:1983–9. doi: 10.1590/1413-81232014197.03162013
67. Balogun OO, Kobayashi S, Anigo KM, Ota E, Asakura K, Sasaki S. Factors influencing exclusive breastfeeding in early infancy: a prospective study in north central Nigeria. Matern Child Health J. (2016) 20:363–75. doi: 10.1007/s10995-015-1835-6
68. Al-Sahab B, Tamim H, Mumtaz G, Khawaja M, Khogali M, Afifi R, et al. Predictors of breast-feeding in a developing country: results of a prospective cohort study. Public Health Nutr. (2008) 11:1350–6. doi: 10.1017/S1368980008003005
69. Wambach KA. Breastfeeding intention and outcome: a test of the theory of planned behavior. Res Nurs Health. (1997) 20:51–9. doi: 10.1002/(sici)1098-240x(199702)20:1<51::aid-nur6>3.0.co;2-t
70. Walsh A, Moseley J, Jackson W. The effects of an infant-feeding classroom activity on the breast-feeding knowledge and intentions of adolescents. J School Nurs. (2008) 24:164–9. doi: 10.1177/1059840555667788
71. Sheeran P, Norman P, Orbell S. Evidence that intentions based on attitudes better predict behaviour than intentions based on subjective norms. Eur J Soc Psychol. (1999) 29:403-6. doi: 10.1002/(SICI)1099-0992(199903/05)29:2/3<403::AID-EJSP942>3.0.CO;2-A
Keywords: knowledge, attitude, intention, pregnant women, breastfeeding, DTCSH, Ethiopia
Citation: Chekol Abebe E, Ayalew Tiruneh G, Asmare Adela G, Mengie Ayele T, Tilahun Muche Z, Behaile T/Mariam A, Tilahun Mulu A and Asmamaw Dejenie T (2022) Levels and Determinants of Prenatal Breastfeeding Knowledge, Attitude, and Intention Among Pregnant Women: A Cross-Sectional Study in Northwest Ethiopia. Front. Public Health 10:920355. doi: 10.3389/fpubh.2022.920355
Received: 14 April 2022; Accepted: 15 June 2022;
Published: 15 July 2022.
Edited by:
Nicholas P. Hays, Nestle, SwitzerlandReviewed by:
Deepanjali Behera, KIIT University, IndiaRakesh Singh, King George's Medical University, India
Copyright © 2022 Chekol Abebe, Ayalew Tiruneh, Asmare Adela, Mengie Ayele, Tilahun Muche, Behaile T/Mariam, Tilahun Mulu and Asmamaw Dejenie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Endeshaw Chekol Abebe, endeshawchekole@gmail.com
 Endeshaw Chekol Abebe
Endeshaw Chekol Abebe Gebrehiwot Ayalew Tiruneh
Gebrehiwot Ayalew Tiruneh Getachew Asmare Adela
Getachew Asmare Adela Teklie Mengie Ayele
Teklie Mengie Ayele Zelalem Tilahun Muche
Zelalem Tilahun Muche Awgichew Behaile T/Mariam1
Awgichew Behaile T/Mariam1 Anemut Tilahun Mulu
Anemut Tilahun Mulu Tadesse Asmamaw Dejenie
Tadesse Asmamaw Dejenie