- 1Department of Pediatric Dentistry and Orthodontics, College of Dentistry, King Saud University, Riyadh, Saudi Arabia
- 2Department of Periodontics and Community Dentistry, College of Dentistry, King Saud University, Riyadh, Saudi Arabia
Objectives: To assess oral health and its implication on oral health-related quality of life (OHRQoL) among groups of foundling and delinquent children compared to mainstream children in Riyadh, Saudi Arabia.
Materials and Methods: This cross-sectional observational study was conducted on children in care houses and mainstream school-going children. The following variables were measured for each group: Demographic data (age, gender); subjective oral health condition; (OHRQoL); clinical oral health condition including the decayed, missing, and filled teeth (DMFT) index; pulpally involved, ulceration, fistula, and abscess (PUFA) index; Dental Aesthetic Index (DAI) for malocclusion, and traumatic dental injuries (TDI).
Statistical Analysis: A one-way ANOVA test, Chi-square test, and Pearson correlation coefficient were used.
Results: The total OHRQoL score was significantly higher for the delinquent compared to the mainstream group. In addition, the DMFT and mean PUFA scores were significantly higher for the delinquent group than the others. The DAI revealed statistical significance in occlusion status within the foundling and delinquent groups, and the prevalence of TDI was significantly higher in the delinquent vs. the mainstream group.
Conclusion: Oral health status appeared to have an association with the OHRQoL among foundling, delinquent, and mainstream children.
Introduction
Good health has been defined by the World Health Organization (WHO), as “a state of absolute physical, psychological, and social well-being and not just the absence of disease or infirmity” (1). This definition remains the most acceptable definition (2). Oral health, defined as the health of the oral cavity, is known to reflect the general health of an individual (3). Subsequently, a new definition was given by Glick and coworkers for oral health and it contemplates that oral health is multi-faceted and includes the ability to speak, smile, smell, taste, touch, chew, swallow, and convey a range of emotions through facial expressions with confidence and without pain discomfort and disease of craniofacial complex (4). This has a variety of functions in clinical research and surveys (4–7). Social well-being was included in the description of health; the concept of oral health was also become broadened by its inclusion (8). Yewe–Dyer (9) described oral health as a state of the oral cavity and its associated structures wherein disease was contained, and future disease was prohibited, occlusion was adequate for masticating food, and teeth were in a socially acceptable position. Dolan (10) described oral health as a convenient and functional dentition that permits individuals to carry on in their desired social roles. The WHO defines oral health as a state free from any long-standing oral or facial pain, mouth ulcers, cancer in the throat and oral cavity, birth deformities like cleft lip or palate, periodontal diseases, dental caries, teeth loss, or any other condition that affects the oral cavity (11). “Oral diseases” refers to any condition that causes pain, chewing, and appearance problems (12).
For the past decades, dental caries has been assessed globally using DMFT/dmft index (13). However, to quantify the various progressive stages of a carious lesion, a new measuring system was developed the PUFA index (P–Pulpal involvement, U-Ulceration, F-Fistula, and A-abscess) (14). Dental caries, malocclusion is also considered a dental problem since it may lead to undesirable esthetics, speech difficulties, impaired oral function, increased susceptibility to dental trauma, temporomandibular joint disorders, and periodontal diseases (15). Traumatic Dental injuries (TDI) are among the most frequent injuries to the body and have become a matter of concern for public health dentists. They may lead to physical impairment, pain, and emotional distress, which can reduce the social and mental quality of life (16). In 1920, the British economist Arthur Pigou was the first to use the term “Quality of life” (QoL) (17). According to the Center for Health Promotion at the University of Toronto, quality of life is concerned with the extent to which an individual appreciates the significant prospects of life (18). OHRQoL is the personal perception regarding an individual's potential to carry out the essential activities that are influenced by his or her health status (19). Hence, the evaluation of OHRQoL must consider the person's living conditions, cultural background, hopes, and accomplishments (8).
A neglected but essential segment of the community includes foundling and delinquent children and adolescents. “Foundling” refers to a child that has been stranded by his or her parents and under the care of other people (20). In contrast, “delinquent” refers to a child who has broken the law or is involved in the indecent or immoral activity and requires rehabilitation (21). A search for relevant literature revealed that no study had been undertaken to assess the oral health condition of Saudi foundling or delinquent children and its influence on their ORHQoL. According to a data availability study by United Nations, the prevalence was 23.8% in children up to 3 years, while for children aged 3–6, it was 57.3% (22). According to a systematic review (13), the prevalence of dental caries in primary dentition is approximately 80%, and for permanent dentition, it is about 70% in Saudi children (23). The high prevalence of dental caries in Saudi children and adolescents is well documented as is their poor oral hygiene (23). The prevalence of dental caries has been the subject of many studies. Foundling and delinquent children in Riyadh, Saudi Arabia, are an inseparable part of the community, yet a literature search regarding the evaluation of their oral health condition and treatment revealed a scarcity of relevant data. The literature also lacks research into the relationship between ORHQoL and dental decay, malocclusion, and TDI. Thus the present study evaluated oral health and its implications on the OHRQoL among these children compared with mainstream children in Riyadh, Saudi Arabia. Thus, the study aimed to assess the oral health status, including the DMFT and PUFA indices, DAI, and TDIs, and their impact on OHRQoL of foundling and delinquent children compared with mainstream school children.
Materials Additionally, Methods
The research proposal was submitted to the Institutional Review Board at King Saud University and was given approval number E-19-3797. Legal guardians were requested to sign an informed consent form prior to the recruitment of children for the study, and the oral assent of each child was documented.
Study Sample and Design
The study was designed as a cross-sectional, observational study involving foundling and delinquent children in care houses and mainstream school children in Riyadh city. Only children were recruited in the study and unwilling children and those who were unable to respond to the study due to mental or physical disability were excluded.
Variables Measured
Demographic information (age and gender), subjective oral health condition, OHRQoL, clinical oral health condition including the decayed, missing, and filled teeth (DMFT) and pulpally involved, ulceration, fistula, and abscess (PUFA) indices, Dental Aesthetic Index (DAI) index for malocclusion, and TDIs were used for the analysis in the study. A validated Arabic Version of the Child Perception Questionnaire (CPQ) (11–14) was used to determine the OHRQoL (11), in all three groups. This questionnaire was divided into four parts concerning oral symptoms (6), functional impediments (9), emotional well-being (9), and social well-being (12). Each response was scored according to the following rubric: 0, never; 1, once/twice; 2, sometimes; 3, often; and 4, every day. The total of the 36 questions gave a general assessment of the extent of a child's oral health status on his or her quality of life. The highest and lowest possible scores for the total scale were 144 and 0, respectively. The principal investigator filled in the questionnaire through an interview with the child and kappa statistics showed an excellent intra examiner reliability (K = 0.89).
The dental caries assessment was done using the DMFT index (12): D is for teeth with dental decay; M is for missing teeth resulting from dental caries; F is for filled teeth. The PUFA index was recorded as follows: P for the involvement of pulp when the pulp chamber orifice was noticeable due to dental caries; U for ulcer following trauma from the sharp parts of a displaced tooth; F for fistula registered in the presence of a sinus tract pus release linked to a pulpally involved tooth; and A for abscess when swelling was present with pus linked to a tooth with pulpal involvement (14). The DAI (15) was used to score malocclusion: (i) normal or minor malocclusion (minimal or no orthodontic treatment required, ≤ 25; (ii) Definite malocclusion (optional orthodontic treatment, 26–30); (iii) Severe malocclusion (orthodontic correction highly desirable, 31–35); (iv) Very severe malocclusion (orthodontic correction is mandatory, >36). TDI was recorded using epidemiological classifications, including the codes of the WHO International Classification of Dental and Stomatology Diseases (15). The scores and codes are as follows: Code 0—no injury (The tooth is sound); Code 1—Treated dental injury (presence of composite restoration, prosthesis replacing missing teeth as a result of trauma); Code 2—enamel fracture only (Trauma confined to enamel); Code 3—enamel dentin fracture (Trauma affecting enamel and dentin); Code 4—pulp injury (Trauma affecting enamel, dentin, and pulp); Code 5—teeth missing due to trauma (tooth avulsed due to trauma only, and not due to dental caries or periodontal disease); Code 9—excluded tooth (Tooth extracted due to dental caries without any signs of dental trauma).
Statistical Analysis
A one-way ANOVA test was used when three levels or more were categorical, and the response was numerical. A multiple comparison test followed it if the ANOVA test showed a significant difference. The Chi-squared test was applied to assess the correlation between any two categorical variables. The Pearson correlation test was applied to compare the impact of oral health on the OHRQoL among all three groups. The data were analyzed using SPSS version 25.0 statistical software (IBM Inc., Chicago USA), and p < 0.05 was significant.
Results
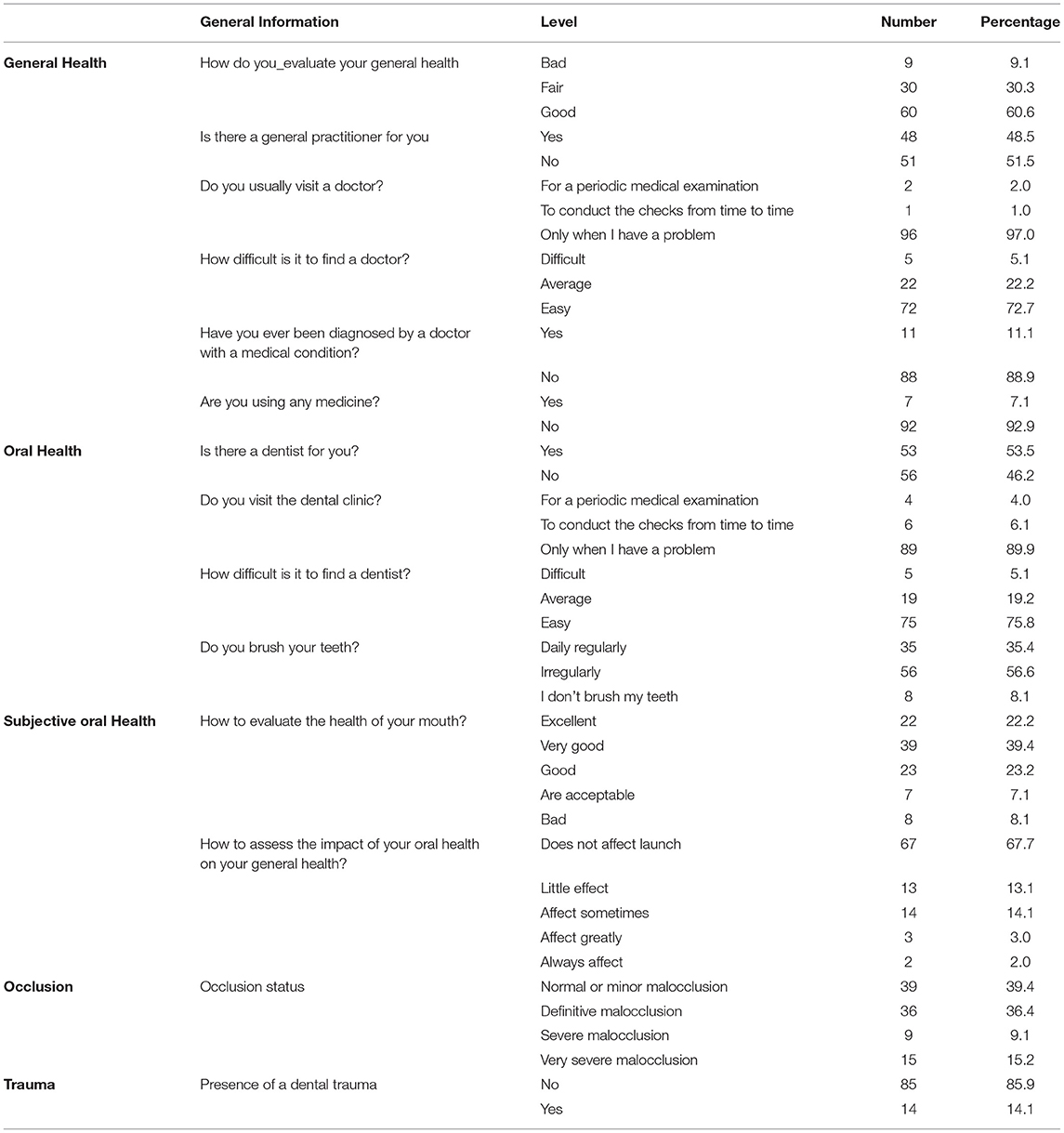
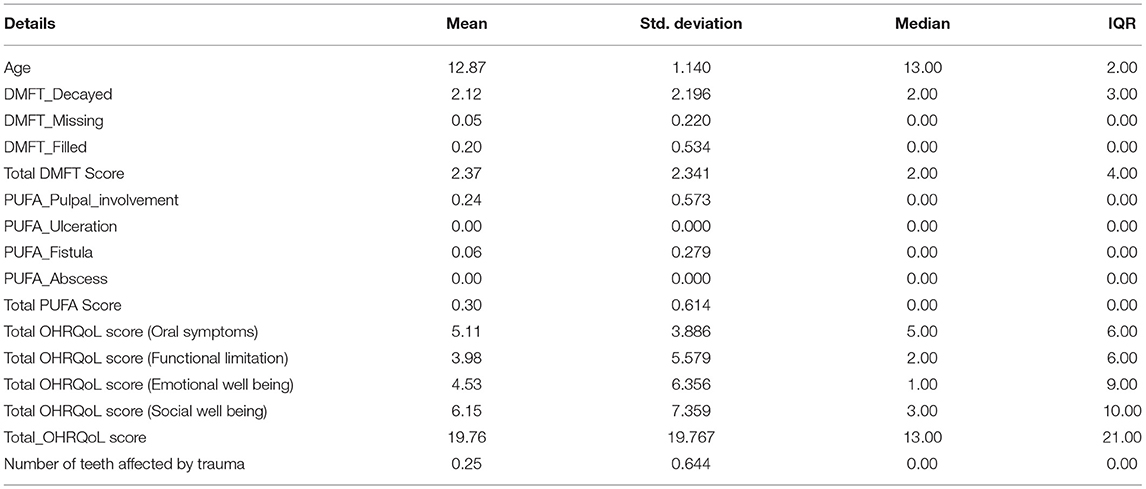
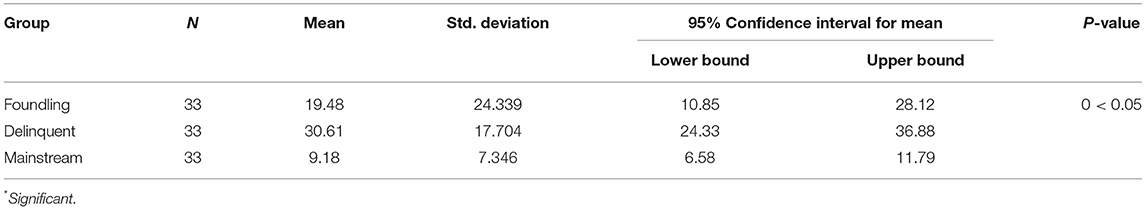
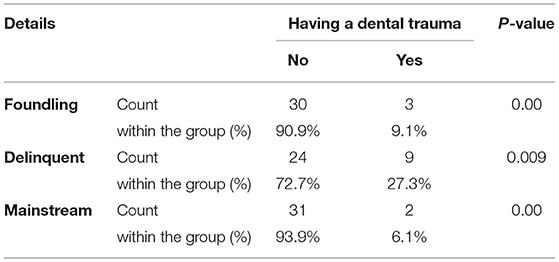
This study comprised a total of 99 children aged 11–14 years. There were 33 in each group, and the mean ages were foundling, 12.2; delinquent, 13.5; and mainstream, 12.8 years. In each group, the male-female percentage was 57.6 and 42.4 for foundling, 87.9 and 12.1 for delinquent, and 75.8 and 24.2 for the mainstream, respectively (Table 1). Overall scores of DMFT, PUFA, Number of teeth involved in trauma, and OHRQoL scores were summarized in Table 2. The mean total OHRQoL score was lowest in the mainstream and the highest in the delinquent group. Variation in the mean total OHRQoL score was statistically significant between the mainstream and delinquent groups, but no significant difference was observed between the mainstream and foundling or between the foundling and delinquent groups (Table 3). The mean DMFT score was found to be lowest in the mainstream and highest in the delinquent group. The results showed a significant difference in the mean DMFT score among all three. Similarly, the mean PUFA score was lowest in the mainstream and highest in the delinquent group. A statistically significant difference was observed in the mean PUFA score between foundling and delinquent groups and between mainstream and delinquent groups, while this difference was not significant between the foundling and mainstream groups (Table 4). In addition, a statistically significant difference was found in the occlusion status of children in the foundling and delinquent groups, whereas the mainstream group did not show any significant differences. No significant difference was observed in the occlusion status of children among all three groups (Table 5). The presence of TDI was significantly higher in the delinquent in comparison to the other two groups (Table 6). The Pearson correlation test showed that the DMFT, PUFA, and DAI (malocclusion) scores and the TDIs significantly impacted the total OHRQoL score in the foundling and delinquent groups. The DMFT, PUFA, and DAI (malocclusion) score significantly impacted the total OHRQoL score in the mainstream group, but there was no significant impact from TDIs on the total OHRQoL score (Table 7).
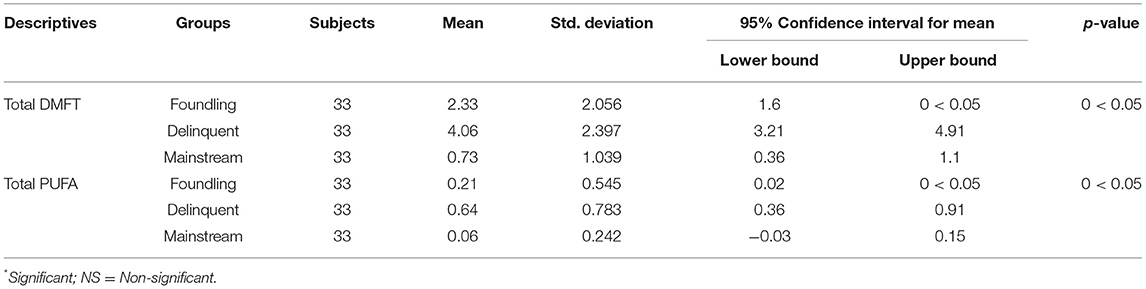
Table 4. The mean prevalence of DMFT and PUFA score in foundling, delinquent and mainstream children groups.
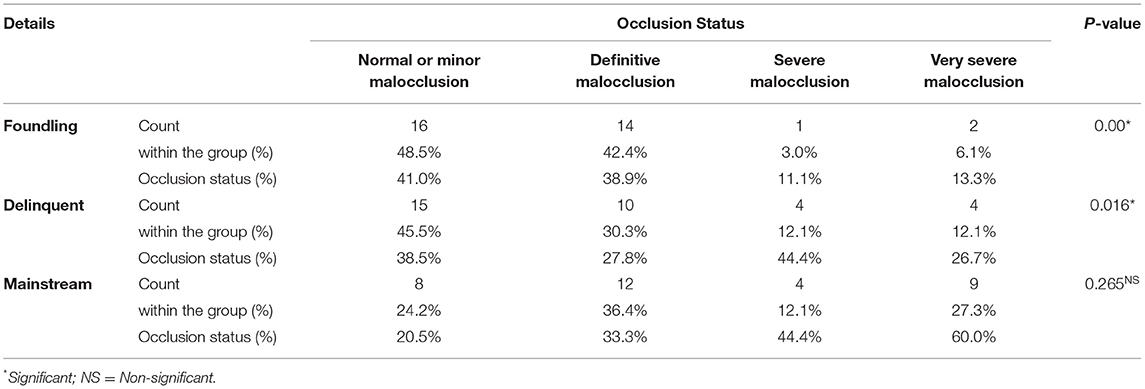
Table 5. The occlusion status in foundling, delinquent and mainstream children groups according to the Dental Aesthetic Index.
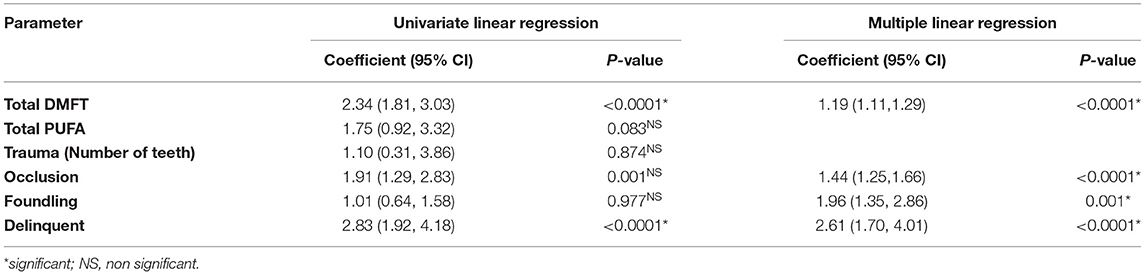
Table 7. Correlation between oral findings (DMFT score, PUFA score, occlusion status, dental trauma) and total OHRQoL scores of foundling and delinquent children groups with mainstream children.
Discussion
There are specific scales specifically designed for the quantitative evaluation of OHRQoL in children and young adults (4, 7) of which CPQ11-14 has been established as a reliable predictor of QoL among children and adolescents (23). Hence, in this study, CPQ11-14 was used to evaluate OHRQoL in children in all groups. Various authors studied the prevalence of dental caries, and a systematic review published in 2017 suggested that in the primary dentition of children in Gulf Cooperation Council Countries, it was 80% (24).
The mean DMFT score for Saudi citizens was found to be 5.38 in primary and 3.34 in permanent dentition in a meta-analysis (25). A systematic review reported a mean DMFT of 5.0 in primary and 3.5 in permanent dentition was observed in Saudi children (8). This study found mean DMFT scores of 2.33, 4.06, and 0.73 for the foundling, delinquent and mainstream groups, respectively, while the mean PUFA scores were 0.21, 0.64, and 0.06, respectively. The mean DMFT and PUFA scores were significantly higher in the delinquent group compared to the mainstream group, suggesting a higher prevalence of dental caries in delinquent compared to mainstream children (26). Pakkhesal et al. (27) concluded that the higher the DMFT score in preschool children, the more negatively impacted OHRQoL. Similar results were reported by Bukhari in working adults (28) and results were not comparable. The results of this study are in accordance with these studies. However, no other studies have mentioned the details of PUFA score assessment and its impact on OHRQoL.
Alongside dental caries and periodontal diseases, malocclusion has also been considered a dental problem (9). Majid (29) suggested that since malocclusion is often accompanied by more significant levels of discontent with appearance, it possibly has a higher negative impact on the OHRQoL. Similar observations were made by Bhatia et al. (30) who found that malocclusion affects boys' emotional well-being, whereas, in girls, it affects the both emotional and social well-being. A similar study on Malay adolescents suggested that the severity of malocclusion is directly proportional to the negative impact on OHRQoL (31). They observed that females manifested a higher negative impact and that the psychological component was predominantly affected. Similar observations were made in this study for all three groups. There was also significant variation in the prevalence of occlusion status of children within the foundling and delinquent groups but no significant difference within the mainstream group.
The PUFA score per person is calculated in the same cumulative way as for the DMFT and represents the number of teeth that meet the PUFA diagnostic criteria. There is no evident association between PUFA and OHRQoL scores found in the present study. These findings are not in agreement with an Indian study where the authors found a positive association between PUFA and OHRQoL (32). It has been well-documented in the literature about the detrimental impact of the presence of dentures, tooth mobility, and edentulism on the oral health-related quality of life (32). Considering the fact that dental caries is a major public health problem among a vast majority of the population, surprisingly there are conflicting results on the impact of the carious lesions on the quality of life of the subjects. Anyhow, these results must be carefully weighed as the study population belonged to different subsets of populations (33–35). This stimulated the investigators of the present study to look into the objective assessment of the complications of untreated carious lesions (PUFA index) on the oral health-related quality of life, especially among a general non-patientt adult rural population in our country. Due to its high psychosocial impact, TDI holds a special position among the causes of a negative OHRQoL (34, 35). Bagchi et al. confirmed that TDI affects a child's school performance and personal relations (36). In this study, TDI was significantly higher in the delinquent group than in the other two but significantly impacted the OHRQoL in all three. Similar observations were made in a 2019 study that found a negative impact of complicated TDI on the OHRQoL on children and their families (37). The impact of DMFT and PUFA on OHRQoL was established among school children with a positive association (38, 39). A Pakistani study conducted among 753 orphan school children reported that 50% of the study population had pulpal involved untreated teeth and also suggested regular visits and initiation of preventive services. Furthermore, recent cross-sectional surveys (40–43) from Saudi Arabia found that parental oral health literacy is critical to maintaining proper oral hygiene and preventive practices (44). The caries burden will be minimized among the children. Based on the present study findings and previous studies' recommendations from Saudi Arabia, the authors opined that it is mandatory to provide regular visits to homes where foundling and delinquent children reside. This will help in minimizing DMFT and eventually the OHRQoL could be improved.
Strengths and Limitations
This is one of the first studies that explored DMFT, PUFA, TDI, occlusion, and OHRQoL among foundling and delinquent children who resided in Riyadh city, Saudi Arabia to the best of the authors' knowledge. Moreover, these findings could use as a reference for further studies. The small sample size was a limitation of the study, so we recommend a larger sample for future studies. The key variables such as socioeconomic status, social capital, and other structural factors of neighborhoods, and parental education of all groups were not included in the study. These children do not have any of these details, hence were not used in the study. This is also a potential limitation of the study. However, these are the only sample available the Riyadh city, Saudi Arabia. The results of the study may not be generalized due to its limitations.
Conclusion
With in the study limitations a significant impact on oral health status (DMFT and PUFA indices, malocclusion, and TDI) on the OHRQoL for both foundling and delinquent children compared to mainstream children. However, in the mainstream children, the DMFT and PUFA indices and malocclusion significantly impacted OHRQoL, whereas no significant impact forms TDI was observed. Further studies are waarrent to establish OHRQoL among foundling and delinquent children in Saudi Arabia.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the College of Dentistry, King Saud University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
AAA, TA, and AHA involved in the study design, performed the study, written and proof reading of the manuscript, and approved for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank the College of Dentistry Research Center and Deanship of Scientific Research at King Saud University for supporting this research project.
References
1. World Health Organisation. Constitution of WHO: Principles. Available online at: https://www.who.int/about/governance/constitution/ (accessed June 25, 2018)
2. Oleribe OO, Ukwedeh O, Burstow NJ, Gomaa AI, Sonderup MW, Cook N et al. Health: redefined. Pan Afr Med J. (2018) 30:292. doi: 10.11604/pamj.2018.30.292.15436
3. Benjamin RM. Oral health: the silent epidemic. Public Health Rep. (2010) 125:158–9. doi: 10.1177/003335491012500202
4. Drachev SN, Brenn T, Trovik TA. Oral health-related quality of life in young adults: a survey of russian undergraduate students. Int J Environ Res Public Health. (2018) 15:719. doi: 10.3390/ijerph15040719
5. Lin F, Ye Y, Ye S, Wang L, Du W, Yao L, et al. Effect of personality on oral health-related quality of life in undergraduates. Angle Orthod. (2018) 88:215–20. doi: 10.2319/051017-322.1
6. Llanos AH, Silva CGB, Ichimura KT, Rebeis ES, Giudicissi M, Romano MM, et al. Impact of aggressive periodontitis and chronic periodontitis on oral health-related quality of life. Braz Oral Res. (2018) 32:e006. doi: 10.1590/1807-3107bor-2018.vol32.0006
7. Chandra Pani S, AlEidan SF, AlMutairi RN, AlAbsi AA, Nasser AlMuhaidib D, Faisal AlSulaiman H, et al. The impact of gross motor function on the oral health-related quality of life in young adults with cerebral palsy in Saudi Arabia. Int J Dent. (2020) 2020:4590509. doi: 10.1155/2020/4590509
8. Al Agili DE. A systematic review of population-based dental caries studies among children in Saudi Arabia. Saudi Dent J. (2013) 25:3–11. doi: 10.1016/j.sdentj.2012.10.002
9. Yewe-Dyer M. The definition of oral health. Br Dent J. (1993) 174:224–25. doi: 10.1038/sj.bdj.4808131
10. Dolan T. Identification of appropriate outcomes for an aging population. Spec Care Dentist. (1993) 13:35–9. doi: 10.1111/j.1754-4505.1993.tb01451.x
12. Oliveira DC, Ferreira FM, Morosini IA, Torres-Pereira CC, Martins Paiva S, Fraiz FC. Impact of oral health status on the oral health-related quality of life of Brazilian male incarcerated adolescents. Oral Health Prev Dent. (2015) 13:417–25. doi: 10.3290/j.ohpd.a33922
13. Hu Z, Yan X, Song Y, Ma S, Ma J, Zhu G. Trends of dental caries in permanent teeth among 12-year-old Chinese children: evidence from five consecutive national surveys between 1995 and 2014. BMC Oral Health. (2021) 21:467. doi: 10.1186/s12903-021-01814-7
14. Monse B, Heinrich-Weltzien R, Benzian H, Holmgren C, van Palenstein Helderman W. PUFA—an index of clinical consequences of untreated dental caries. Community Dent Oral Epidemiol. (2010) 38:77–82. doi: 10.1111/j.1600-0528.2009.00514.x
15. Jenny J, Cons NC. Establishing malocclusion severity levels on the Dental Aesthetic Index (DAI) scale. Aust Dent J. (1996) 41:43–6. doi: 10.1111/j.1834-7819.1996.tb05654.x
16. Addo ME. Textbook and color atlas of traumatic injuries to the teeth (4th edition). Br Dent J. (2007) 203:615 doi: 10.1038/bdj.2007.1053
18. Raphael D, Brown I, Renwick R, Rootman I. Quality of Life Theory and Assessment: What are the Implications for Health Promotion. University of Toronto, Centre for Health Promotion (1994).
19. Locker Locker D: Concepts of oral health disease disease and the quality of life. In: Slade GD, editors. Measuring Oral Health and Quality of Life. Chapel Hill: University of North Carolina. p. 11–24.
20. Geffen DH. The founding hospital child welfare scheme. Br Med J. (1947) 2:23. doi: 10.1136/bmj.2.4513.23
21. Ennedy A, Scott PD. Juvenile delinquency with special reference to remand homes. Proc R Soc Med. (1948) 41:197–208. doi: 10.1177/003591574804100404
22. El Tantawi M, Folayan MO, Mehaina M, Vukovic A, Castillo JL, Gaffar BO, et al. Prevalence and data availability of early childhood caries in 193 united nations countries, 2007–2017. Am J Public Health. (2018) 108:1066–72. doi: 10.2105/AJPH.2018.304466
23. Kotha SB, Terkawi SA, Mubaraki SA, Saffan ADA, Kotha SL, Mallineni SK. Association between Body Mass Index (BMI) and dental caries among 6–12-year-old school children. Children. (2022) 9:608. doi: 10.3390/children9050608
24. Alayyan W, Al Halabi M, Hussein I, Khamis A, Kowash M. A systematic review and meta-analysis of school children's caries studies in Gulf cooperation council states. J Int Soc Prev Community Dent. (2017) 7:234–41.
25. Khan SQ, Khan NB, Arrejaie AS. Dental caries. A meta analysis on a Saudi population. Saudi Med J. (2013) 34:744–9.
26. Alsaif AA, Alkhadra TA, AlJameel AH. Oral health-related quality of life among groups of foundling and delinquent children in comparison with mainstream children. J Popul Ther Clin Pharmacol. (2021) 28:e7–e16. doi: 10.47750/jptcp.2021.859
27. Pakkhesal M, Riyahi E, Alhosseini AN, Amdjadi P, Nasser Behnampour N. Impact of dental caries on oral health related quality of life among preschool children: perceptions of parents. BMC Oral Health. (2021) 21:68. doi: 10.1186/s12903-021-01396-4
28. Bukhari OM. Dental caries experience and oral health related quality of life in working adults. Saudi Dent J. (2020) 32:382–9. doi: 10.1016/j.sdentj.2019.11.003
29. Majid ZSA. Effects of malocclusion on Oral Health Related Quality of Life (OHRQoL): a critical review. Eur Sci J. (2015) 11:386–400. Available online at: https://eujournal.org/index.php/esj/article/view/6007
30. Bhatia R, Winnier JJ, Mehta N. Impact of malocclusion on oral health-related quality of life in 10–14-year-old children of Mumbai, India. Contemp Clin Dent. (2016) 7:445–50. doi: 10.4103/0976-237X.194105
31. Elyaskhil M, Shafai NAA, Mokhtar N. Effect of malocclusion severity on oral health related quality of life in Malay adolescents. Health Qual Life Outcomes. (2021) 19:71. doi: 10.1186/s12955-021-01710-2
32. Praveen BH, Prathibha B, Reddy PP, Monica M, Samba A, Rajesh R. Co relation between PUFA index and oral health related quality of life of a rural population in India: a cross-sectional study. J Clin Diagn Res. (2015) 9:ZC39–42. doi: 10.7860/JCDR/2015/11427.5489
33. Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. (2005) 83:661–9.
34. Hamilton FA, Hill FJ, Holloway PJ. An investigation of dento-alveolar trauma and its treatment in an adolescent population. Part 1: the prevalence and incidence of injuries and the extent and adequacy of treatment received. Br Dent J. (1997) 182:91–5. doi: 10.1038/sj.bdj.4809313
35. Cortes MI, Marcenes W, Sheiham A. Impact of traumatic injuries to the permanent teeth on the oral health-related quality of life in 12–14-year-old children. Community Dent Oral Epidemiol. (2002) 30:193–8. doi: 10.1034/j.1600-0528.2002.300305.x
36. Milani AJ, Fonseca Alves N, Martins do Espiroto-Santo T, Gonçalves Ribeiro L, Ammari MM, Antunes LS et al. Impact of traumatic dental injuries on oral health-related quality of life of preschool children and their families attending a dental trauma care program port. J Public Health. (2019) 37:19–25. doi: 10.1159/000501525
37. Bagchi S, Saha S, Reddy VK, Sinha P. Impact of dental trauma on oral health-related quality of life among 12 years Lucknow school children: a cross-sectional survey. J Indian Asso Public Health Dent. (2015) 13:239–43. doi: 10.4103/2319-5932.165225
38. Kamran R, Farooq W, Faisal MR, Jahangir F. Clinical consequences of untreated dental caries assessed using PUFA index and its covariates in children residing in orphanages of Pakistan. BMC Oral Health. (2017) 17:108. doi: 10.1186/s12903-017-0399-9
39. Habib F, Chaly PE, Junaid M, Musthafa HM. Caries experience, clinical consequences of untreated dental caries and associated factors among school going children—a cross-sectional study. Indian J Dent Res. (2020) 31:180–5. doi: 10.4103/ijdr.IJDR_120_19
40. Alyousef AM, Almehrej BA, Alshahrani MA, Almutairi KM, Muhannad Abdulrahman Alqasir MA, Alassaf A, et al. Arabian parents' knowledge, attitude, and practice towards their children's oral health and early childhood caries resided in Riyadh Province: an online-based cross-sectional survey. Ann Med Health Sci Res. (2021) 11:73–81.
41. Alshloul MN. Oral health knowledge, attitude, and practice among school children in Abha-Saudi Arabia. J Sch Nurs. (2021). doi: 10.1177/10598405211012981. [Epub ahead of print].
42. AlBlehed AK, AlThumairy AF, AlTurayri WS, Alassaf A, Almulhim B, Alghamdi S, et al. Assessment of knowledge, attitude and practices regarding oral hygiene among the parents of pre-school children: a cross-sectional study. Ann Med Health Sci Res. (2021) 11:82–6.
43. Al-Qahtani SM, Razak PA, Khan SD. Knowledge and practice of preventive measures for oral health care among male intermediate school children in Abha, Saudi Arabia. Int J Environ Res Public Health. (2020) 17:703. doi: 10.3390/ijerph17030703
Keywords: dental health surveys, health-related quality of life, oral health, quality of life, children
Citation: Alsaif AA, Alkhadra TA and AlJameel AH (2022) Impact of DMFT, PUFA, DAI, and TDIs on Oral Health-Related Quality of Life (OHRQoL) Among Foundling, Delinquent, and Mainstream School Children: A Prilimenary Study. Front. Public Health 10:894638. doi: 10.3389/fpubh.2022.894638
Received: 12 March 2022; Accepted: 13 June 2022;
Published: 08 July 2022.
Edited by:
Jayakumar Jayaraman, Virginia Commonwealth University, United StatesReviewed by:
Srinivasulu Sakamuri, Narayana Dental College and Hospital, IndiaAhmad Faisal Ismail, International Islamic University Malaysia, Malaysia
Ami Angela Harahap, University of North Sumatra, Indonesia
Daniel Carreno, Pontificia Universidad Católica de Chile, Chile
Copyright © 2022 Alsaif, Alkhadra and AlJameel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abdulaziz Abdullah Alsaif, drbinsaif@yahoo.com
 Abdulaziz Abdullah Alsaif
Abdulaziz Abdullah Alsaif Thamer Adel Alkhadra1
Thamer Adel Alkhadra1