- 1School of Post-Baccalaureate Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
- 2Department of Urology, Kaohsiung Municipal Siaogang Hospital, Kaohsiung, Taiwan
- 3Department of Urology, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
- 4Graduate Institute of Clinical Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
- 5Research Center for Environmental Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
- 6Department of Internal Medicine, Kaohsiung Municipal Siaogang Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
- 7Division of Nephrology, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
- 8Faculty of Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
- 9Graduate Institute of Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
- 10Department of Psychiatry, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
Background: Living alone has been linked to poor mental health, however large-scale epidemiological studies on the association between living alone and psychiatric morbidity including depression and anxiety are lacking. The aim of this study was to investigate this issue in a large Taiwanese cohort.
Methods: In this cross-sectional study, we enrolled 121,601 volunteers from 29 community recruitment stations in Taiwan and divided them into two groups based on whether or not they lived alone. Psychiatric morbidity was defined as a Generalized Anxiety Disorder 2-item score ≥ 3, Patient Health Questionnaire 2-item score ≥ 3, or self-reported depression. Logistic regression was used to explore the associations between living alone and psychiatric morbidity.
Results: The participants who lived alone had a higher prevalence of psychiatric morbidity [odds ratio (OR) = 1.608, 95% confidence interval (CI) = 1.473 to 1.755] after adjusting for potential confounders. In a subgroup analysis, married subjects who lived alone and divorce/separation (OR = 2.013, 95% CI = 1.763 to 2.299) or widowing (OR = 1.750, 95% CI = 1.373 to 2.229) were more likely to have psychiatric morbidity than those who were married and not living alone.
Conclusions: Our findings suggest that living alone is a risk factor for psychiatric morbidity, especially for married subjects who live alone in concordance with divorce, separation, or the death of a spouse.
Introduction
In recent years, the increase in unmarried, later marriage, and divorce rates has caused the pattern of marriage and family to change dramatically. A smaller family size has led to a growth in single-person households (1), and social isolation and a lack of contact has been associated with health issues such as mental disorders, dementia, poor nutrition, and cardiac disease (2–4). Worldwide, more than 300 million people are affected by depression, and more than 250 million live with anxiety disorders (5). According to a cross-sectional survey in Taiwan, the prevalence of potentially common mental diseases, including non-psychotic, depression, and anxiety disorders, doubled from 11.5% in 1990 to 23.8% in 2010 (6). Proper care and treatment for these patients can reduce mortality and extend life expectancy (7). Moreover, an increase in the prevalence of these common mental diseases would result in tremendous medical and social costs (8, 9), making it crucial to determine the risk factors and comorbidities associated with them.
Researchers have investigated the relationship between living alone and mental health, and found that social isolation increases the risk of common mental diseases (10). However, these studies mainly focused on the effects of depression on elderly populations, rather than on the general or young populations. In addition, only a few have mentioned the association between living alone and other psychiatric conditions, such as anxiety, and most only included a small number of subjects (11). Furthermore, as the number of single-person households increases, mental disorders could also affect younger people who are unmarried or divorced as well as elderly populations.
Psychiatric morbidity is a symptom-based medical term generally applied to those aware of their condition, including a variety of mental illnesses, such as depression, anxiety, schizophrenia, bipolar disorder, et cetera, which is well–suited for exploring the association between living alone and mental health (12). One advantage of using psychiatric morbidity to test our hypothesis is that it not only covers depression, but also other psychiatric disorders as well. Another advantage is that psychiatric morbidity often represents the symptomatic group, which makes our results more clinically meaningful (12). Because living alone has been associated with loneliness (13), social support (14), and substance use (15), which are risk factors for psychiatric morbidity, we hypothesize that living alone is associated with psychiatric morbidity. Previously, numerous studies have documented that education (16), smoking (17), drinking (18), chronic disorders (19), stressful life events (20) and obesity (21) are associated with psychiatric morbidity; however, only a few have mentioned the association between living alone and psychiatric morbidity, and most only included a small number of subjects (10). The goals of this study were to determine the association between living alone and psychiatric morbidity.
Materials and methods
Data source and study population
The data used in this study were from a population-based dataset derived from 29 community recruitment stations in Taiwan since 2008, details of which have been described in our previous publications (22–24). In brief, all subjects were enrolled as volunteers and completed several questionnaires including basic profile, habitus, past history, Generalized Anxiety Disorder 2-item (GAD-2) and Patient Health Questionnaire 2-item (PHQ-2). They also underwent physical examinations during which body weight and height were measured and blood tests were performed. Before enrollment, all subjects understood the purpose, interests, pros and cons of our research and signed a consent form. All researchers followed the Declaration of Helsinki throughout the study, which was approved by the Institutional Review Board of our institute (KMUHIRB-E(I)-20210058).
Variables
The variables used in this study came from the aforementioned questionnaires, physical examinations, and blood tests. Data on age, gender, smoking status, drinking status, exercise status, marital status, educational status, medical history, GAD-2 and PHQ-2 scores, were obtained from the questionnaires. Data on body mass index (BMI) and waist circumference were obtained from the physical examinations, and data on serum creatinine and chronic kidney disease (defined as an estimated glomerular filtration rate < 60 ml/min/1.73 m2) were obtained from the blood tests.
Living arrangements and marital status
Each subject would need to fill out a questionnaire about their living arrangements and marital status. Regarding living arrangements, there are two options in the questionnaire: (1) living alone and (2) living with family or others. Based on the subjects' responses, they were divided into living alone (+) and living alone (-). Regarding marital status, there are four options in the questionnaire: (1) unmarried (single/never married), (2) married, (3) divorced or separated, and (4) widowed. We further combined living arrangements with marital status, and subjects were subdivided into 6 groups: (1) living alone (+) and unmarried, (2) living alone (+) and married, (3) living alone (+) and divorce/separation, (4) living alone (+) and widowing, (5) living alone (-) and unmarried, (6) living alone (-) and married.
Psychiatric morbidity
Psychiatric morbidity was defined as depression and anxiety in this study. We used the PHQ-2, GAD-2, and self-reported depression to assess the presence or absence of psychiatric morbidity. The PHQ-2 uses the following two questions to assess a subject's depressive condition in the last 2 weeks: “Do you feel little interest or pleasure in doing things? (0 = not at all; 1 = several days; 2 = more than half the days; 3 = nearly every day)” and “Do you feel down, depressed, or hopeless? (0 = not at all; 1 = several days; 2 = more than half the days; 3 = nearly every day)”. The GAD-2 also uses two questions to assess a subject's anxiety in the last 2 weeks as follows: "Do you feel nervous, anxious, or on edge? (0 = not at all; 1 = several days; 2 = more than half the days; 3 = nearly every day)” and “Do you feel unable to stop or control worrying? (0 = not at all; 1 = several days; 2 = more than half the days; 3 = nearly every day)”. Participants with a PHQ-2 score of 3 to 6 were considered to have depressive tendencies, and those with a GAD-2 score of 3 to 6 were considered to have anxiety tendencies. We further defined psychiatric morbidity as a GAD-2 score ≥ 3, PHQ-2 score ≥ 3, or self-reported depression.
Statistical analysis
We used descriptive statistics to describe the profiles of all subjects. Continuous variables are expressed as means and standard deviations, and categorical variables are expressed as numbers and percentages. We then divided the subjects into two groups according to whether or not they lived alone, and the differences between groups were measured using the independent t test and chi-square test. The possible confounders of the association between living alone and psychiatric morbidity were identified through literature reviews, including age (25), sex (25), obesity (21), educational status (16), smoking (17), drinking (18), physical activity (26), marital status (27) and chronic diseases (heart disease, asthma, chronic obstructive pulmonary disease, gastrointestinal problems, hypertension, diabetes mellitus, dyslipidemia, gout, osteoporosis, chronic kidney disease, neurological diseases and substance abuse) (19, 28–30). To further identify the risk factors, these possible confounders were entered into the feature selection process using the least absolute shrinkage and selection operator (LASSO) regression, by assigning each training observation to be subdivided randomly into 10 parts, then by a method of an automated 10-fold cross-validation (31). We further used univariable and multivariable logistic regression to test the association of each variable with psychiatric morbidity. Finally, we conducted a subgroup analysis to explore the association of marriage and dependency with psychiatric morbidity. In this study, a p value < 0.05 indicated a significant association. Our analysis was performed using R (version 3.6.2, R Foundation for Statistical Computing, Wien, Austria), SAS (version 9.4, SAS Institute Inc., Cary, NC, United States) and SPSS (version 20.0, IBM Corp, Armonk, NY, United States).
Results
Profiles of the participants
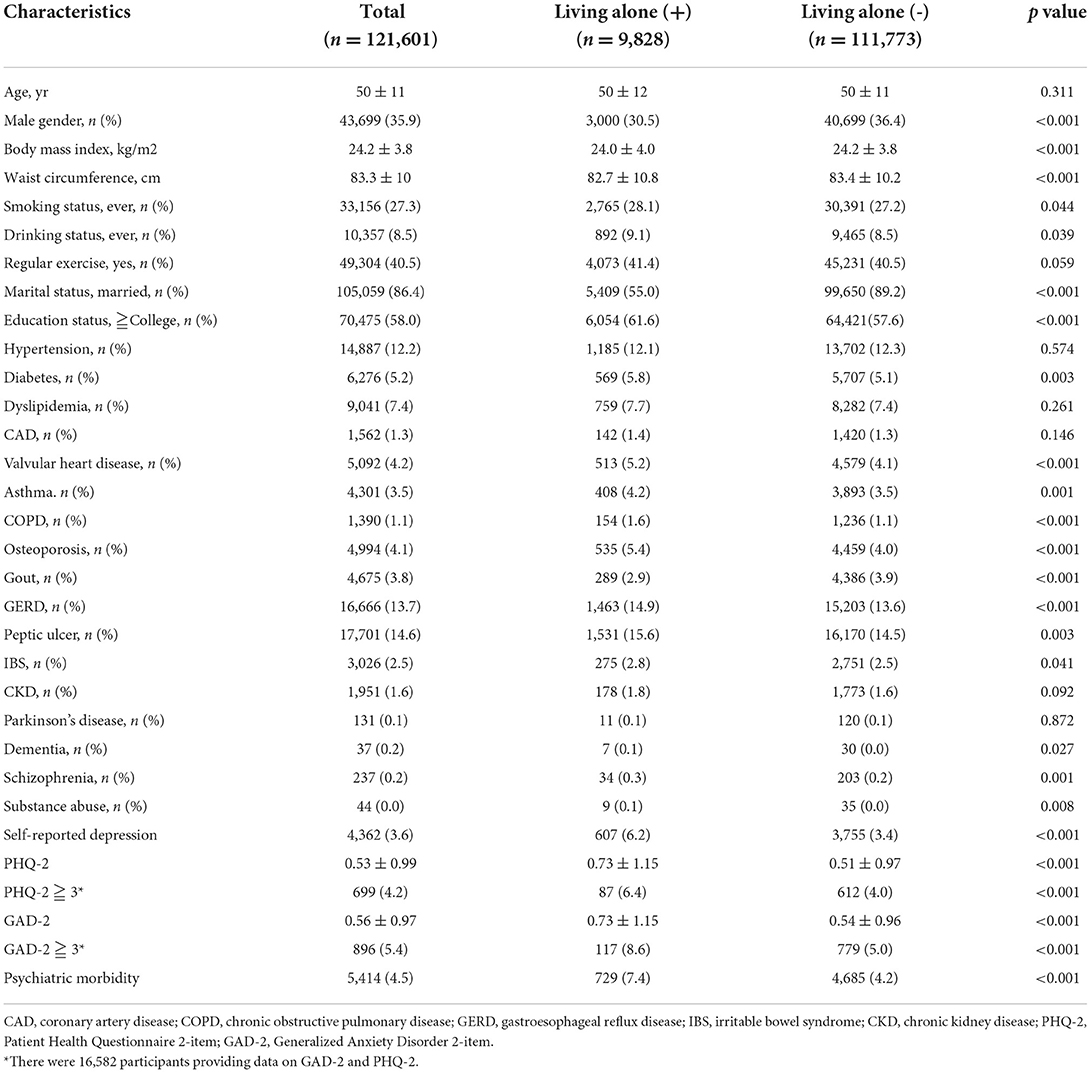
A total of 121,601 participants with sufficient data were included in our analysis. Their average age was 50 years, 27.3% smoked, 8.5% drank alcohol, 86.4% were married, 3.6% had self-reported diagnosed depression, 4.5% had psychiatric morbidity and 8.1% lived alone (Table 1). Among the 16,582 participants who completed the PHQ-2 and GAD-2, the average PHQ-2 score was 0.53, the GAD-2 score was 0.56, 4.2% had a PHQ-2 ≧ 3, and 5.4% had a GAD-2 ≧ 3. The subjects' past medical histories are also listed in Table 1. The subjects who lived alone (n = 9,828) had a lower BMI, lower waist circumference, higher proportion of smoking, drinking, PHQ-2 ≧ 3, GAD-2 ≧ 3, psychiatric morbidity, and more were unmarried than those who did not live alone. Concerning past medical history, the subjects who lived alone were more likely to have diabetes, respiratory diseases, gastrointestinal diseases, orthopedic diseases, neurological diseases and self-reported diagnosed depression than those who did not live alone (Table 1).
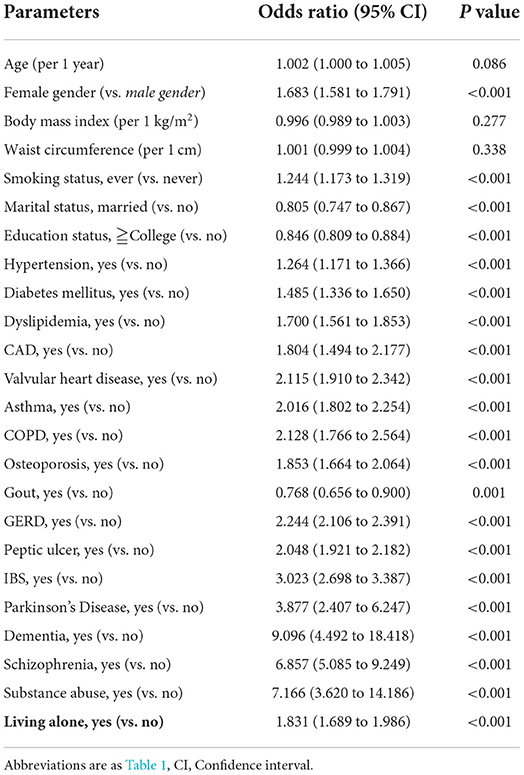
Parameters associated with psychiatric morbidity in univariable binary logistic analysis
By performing LASSO regression, we excluded three variables, including drinking status, exercise and chronic kidney disease, that had minimal effects on psychiatric morbidity (Supplementary Figure 1 and Supplementary Table 1). The remaining 24 variables were entered into further analysis. In univariable binary logistic analysis, female gender, smoking, diabetes mellitus, dyslipidemia, cardiovascular diseases, respiratory diseases, orthopedic diseases, gastrointestinal diseases, neurological diseases, and living alone were associated with a higher prevalence of psychiatric disorders (Table 2). The subjects who lived alone had a higher prevalence of psychiatric morbidity with an odds ratio (OR) of 1.831 [95% confidence interval (CI) = 1.689 to 1.986, p < 0.001]. Conversely, being married and having a high degree of education were associated with a lower prevalence of psychiatric disorders (Table 2).
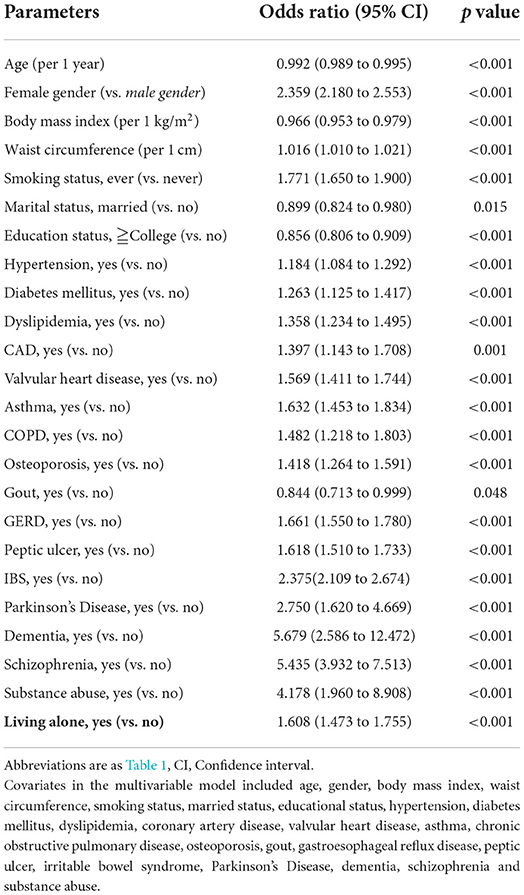
Parameters associated with psychiatric morbidity in multivariate binary logistic analysis
In multivariable binary logistic analysis, female gender, waist circumference, smoking, diabetes mellitus, dyslipidemia, cardiovascular diseases, respiratory diseases, orthopedic diseases, gastrointestinal diseases, neurological diseases, and living alone were associated with a higher prevalence of psychiatric disorders (Table 3). The subjects who lived alone had a higher prevalence of psychiatric morbidity with an OR of 1.608 (95% CI = 1.473 to 1.755, p < 0.001) after adjusting for potential confounders. In contrast, age, BMI, being married, and having a high degree of education were associated with a lower prevalence of psychiatric disorders (Table 3). We further analyzed males and females separately, and the results were similar to the results of the whole study population (Supplementary Table 2).
Odds ratios for psychiatric morbidity by marital status
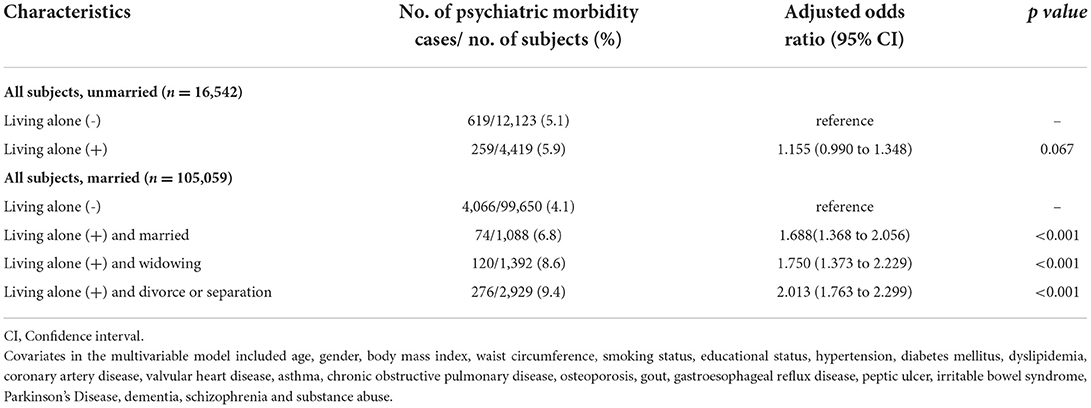
Because the presence or absence of living alone is related to marital status, we then performed a subgroup analysis, and divided the subjects into two groups according to marital status. As shown in Supplementary Table 3, the risk of psychiatric morbidity in the unmarried group was not affected by living alone (OR = 1.155, 95% CI = 0.990 to 1.348, p = 0.067), however the risk of psychiatric disorders in the married group was related to living alone (OR = 1.876, 95% CI = 1.692 to 2.081, p < 0.001). The results were similar when analyzing men and women separately (Supplementary Table 4). Moreover, married subjects who lived alone and divorce/separation (OR = 2.013, 95% CI = 1.763 to 2.299, p < 0.001) or widowing (OR = 1.750, 95% CI = 1.373 to 2.229, p < 0.001) were more likely to have psychiatric morbidity than those who were married and not living alone (Table 4 and Supplementary Table 5).
Discussion
This study is the largest population-based study to examine the association between living alone and psychiatric morbidity, and it showed a statistically significant association between them. We also found that this association was present in the subjects who were married, but not in those who were not married. In addition, married subjects who lived alone in concordance with divorce, separation, or the death of a spouse were associated with a higher risk of psychiatric morbidity.
Living alone has been associated with poor mental health conditions (32–36). Stahl, et al. (32) found that living alone was associated with elevated levels of depressive symptoms compared to living with a family member. Similar findings were also noted in the elderly population (34). In a qualitative meta-analysis, Hu, et al. found that older people living alone had a higher risk of depression than those not living alone (33). Consistent with our results, the relationship between living alone and anxiety has also been discussed in previous research; for example, Hunt, et al. (35) and Yu, et al. (36) found that people living alone had a significantly higher risk of generalized anxiety disorder than those living with their families.
An interesting finding of this study is that living alone increased the risk of psychiatric morbidity in married subjects, but not in unmarried subjects. A previous study reported that the psychological well-being of divorced and widowed people was poorer than those who never married (37). Marital relationships can provide a sense of well-being and emotional support, producing mutual obligations and reinforcements between the two parties (38, 39). These relationships reduce vulnerability to psychological disorders. However, a change in this connection has been shown to significantly increase depressive symptoms (40). Thus, this might explain a higher likelihood of married people but living alone suffering from psychiatric disorders.
We also found that married subjects who lived alone and widowed had a 1.76-fold risk of having psychiatric morbidity compared to those who were married and not living alone. Widowhood has been known for being a catastrophic event with a negative impact on both physical and emotional well-being (41, 42). Various factors have influenced the degree of emotional response to spouse loss such as age, gender, length of widowhood, health condition, economic status, and living arrangements (43, 44). Srivastava, et al. (45) reported that the interaction between marital status and living arrangements on depression showed that widowed and living alone elderly were more likely to suffer from depression than those currently married and co-residing. The rates of depression were highest in widowed and living alone, followed by widowed and co-residing, currently married and co-residing, currently married and living alone (45). The negative psychological well–being of widowhood could be explained by the poor emotional and financial support that comes with spouse loss (46, 47).
Meanwhile, the relationship between living alone and lack of social support was also reported in COVID-19 related studies that resulted in higher risk of depression and anxiety (48, 49). The addition of widowed and separated status was revealed to be related to depression and poor quality of life due to loneliness (50). Poor psychological well-being has been linked to objective social isolation (51) and subjectively perceived social support, such as loneliness (52). Moreover, in a large nationally longitudinal study, Domènech-Abella, et al. (53) reported that both loneliness and social isolation affected the probability of suffering from depression and anxiety.
This is an important public health issue, because people suffered from psychiatric disorders are at increased risk of suicide, self-harm, and mortality (54–56). Thus, proper care and treatment are crucial to reduce mortality and extend life expectancy. Stahl, et al. (32) suggested that adults living alone need to have a better perception of neighborhood social quality. Having a good relationship with neighbors has been shown to relieve loneliness and depression by increasing the availability of social activities, receiving practical help from others, and making older people feel safer and more secure (57–59). Another study showed that leisure activities may moderate poor mental health in older adults living alone (60). Older adults living alone may have reduced physical activity and social interaction, and encouraging them to participate in leisure activities could increase their level of physical activity and social connection with others and affect positive emotional outcomes (60–62). Thus, people living alone tend to have fewer social interactions and activities and feel lonely and insecure (36). Having a good relationship with neighbors or participating in leisure activities could reduce the risk of suicide, self-harm, and mortality.
Besides living alone, other parameters are also associated with psychiatric morbidity. Our results revealed that the subjects with chronic diseases, such as diabetes mellitus, cardiovascular, respiratory, orthopedic, gastrointestinal, or neurological diseases had a higher likelihood of psychiatric morbidity (63–66). Chaudhry, et al. (67) reported a prevalence of psychiatric morbidity among insulin-dependent patients of 18%, and that people with diabetes mellitus were twice as likely as the general population to suffer from psychiatric morbidity. Psychiatric morbidity is common in patients with coronary heart disease, and a previous study reported that 16% of patients assessed seven days after myocardial infarction had symptoms consistent with a major depressive episode (68, 69). With regards to the relationship between respiratory diseases and psychiatric morbidity, a study in India found that 44.8% of patients with respiratory illnesses had a mental illness compared with 24.3% of controls (70).
The relationship between psychiatric morbidity and chronic diseases could be attributed to patients' panic, pessimism, and emotional imbalance after diagnosis. From the aspect of biology, the hypothalamic adrenocortical axis could be induced by both depression and diabetes (67). Devolving psychiatric morbidity, hypertension, and cardiovascular diseases could be attributed to a lack of the central neurotransmitter serotonin (68, 71, 72). Thus, people with chronic diseases have an increased risk of psychiatric morbidity.
Although our study is the most extensive population-based study examining the relationship between living alone and psychiatric morbidity to date, several limitations should be acknowledged. First, the design of this study was cross-sectional, and thus determining the duration of psychiatric morbidity in the people living alone is difficult. Further prospective studies are needed to elucidate the causal effects of living alone on psychopathology. Second, we used self-report questionnaires to assess psychiatric morbidity. As psychiatric disorders remain a social stigma, some people may have hesitated to answer truthfully, and thus we may have underestimated the prevalence of psychiatric morbidity. Furthermore, we may have underestimated the role of certain comorbid conditions due to a lack of information. Third, we defined psychiatric morbidity as a GAD-2 score ≧3, PHQ-2 score ≧3, or self-reported depression to include both depression and anxiety as the main focus of this study. However, we lacked data on self-reported anxiety. The initial questionnaire design of our study did not cover self-reported anxiety, so we used the GAD-2 score ≧3 to represent anxiety groups. Such an approach has been validated in other studies (73, 74). Fourth, we did not include some factors that may affect mental health, such as income, work, socioeconomic status, physical activity, and family support (75–77). This may have led to an underestimation of the risk of psychiatric morbidity and the association with living alone. Finally, only 16,582 participants completed the PHQ-2 and GAD-2, resulting in a lot of missing data. However, both PHQ-2 and GAD-2 are quantitative indicators which can represent the current status of participants, and by combining self-reported depression, PHQ-2 and GAD-2 can provide a holistic understanding of living alone and mental disorders.
Conclusion
Our findings suggest that living alone is a risk factor for psychiatric morbidity, especially in those who are married. This highlights the importance of improving the care system for married persons living alone in concordance with divorce, separation or the death of a spouse to protect their physical and mental health. Further well-designed prospective studies are needed to investigate the causal effects of living alone on psychopathology.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the data underlying this study is from the Taiwan Biobank. Due to restrictions placed on the data by the Personal Information Protection Act of Taiwan, the minimal data set cannot be made publicly available. Data may be available upon request to interested researchers. Requests to access these datasets should be directed to S-CC, scarchenone@yahoo.com.tw.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Board of Kaohsiung Medical University Hospital (KMUHIRB-E(I)-20210058). The patients/participants provided their written informed consent to participate in this study.
Author contributions
Conceptualization, methodology, formal analysis, investigation, data curation, writing—review and editing, and visualization: J-HG and J-IL. Software and project administration: J-HG. Validation, supervision, and funding acquisition: S-CC. Resources: J-HG and S-CC. Writing—original draft preparation: T-YC. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported partially by the Research Center for Environmental Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan, from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan and by Kaohsiung Medical University Research Center Grant (KMU-TC111A01-1 and KMUTC111IFSP01).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1054615/full#supplementary-material
References
1. Aldrich HE, Cliff JE. The pervasive effects of family on entrepreneurship: toward a family embeddedness perspective. J Busi Ventur. (2003) 18:573–96. doi: 10.1016/S0883-9026(03)00011-9
2. Hanna KL, Collins PF. Relationship between living alone and food and nutrient intake. Nutr Rev. (2015) 73:594–611. doi: 10.1093/nutrit/nuv024
3. Udell JA, Steg PG, Scirica BM, Smith SC, Ohman EM, Eagle KA, et al. Living alone and cardiovascular risk in outpatients at risk of or with atherothrombosis. Arch Intern Med. (2012) 172:1086–95. doi: 10.1001/archinternmed.2012.2782
4. Hughes M, Gove WR. Living alone, social integration, and mental health. Am J Sociol. (1981) 87:48–74. doi: 10.1086/227419
5. World Health O. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization en. (2017).
6. Fu TS, Lee CS, Gunnell D, Lee WC, Cheng AT. Changing trends in the prevalence of common mental disorders in Taiwan: a 20-year repeated cross-sectional survey. Lancet (London, England). (2013) 381:235–41. doi: 10.1016/S0140-6736(12)61264-1
7. Liu NH, Daumit GL, Dua T, Aquila R, Charlson F, Cuijpers P, et al. Excess mortality in persons with severe mental disorders: a multilevel intervention framework and priorities for clinical practice, policy and research agendas. World Psychiatry. (2017) 16:30–40. doi: 10.1002/wps.20384
8. Trautmann S, Rehm J, Wittchen HU. The economic costs of mental disorders: Do our societies react appropriately to the burden of mental disorders? EMBO Rep. (2016) 17:1245–9. doi: 10.15252/embr.201642951
9. Rice DP, Kelman S, Miller LS. The economic burden of mental illness. Hosp Community Psychiatry. (1992) 43:1227–32. doi: 10.1176/ps.43.12.1227
10. Jacob L, Haro JM, Koyanagi A. Relationship between living alone and common mental disorders in the 1993, 2000 and 2007 national psychiatric morbidity surveys. PLoS ONE. (2019) 14:e0215182. doi: 10.1371/journal.pone.0215182
11. Ansseau M, Fischler B, Dierick M, Albert A, Leyman S, Mignon A. Socioeconomic correlates of generalized anxiety disorder and major depression in primary care: the GADIS II study (Generalized Anxiety and Depression Impact Survey II). Dep Anxiety. (2008) 25:506–13. doi: 10.1002/da.20306
12. Lee JI, Burdick KE, Ko CH, Liu TL, Lin YC, Lee MB. Prevalence and factors associated with suicide ideation and psychiatric morbidity among inpatients of a general hospital: A consecutive three-year study. Kaohsiung J Med Sci. (2021) 37:427–33. doi: 10.1002/kjm2.12336
13. Russell D. Living arrangements, social integration, and loneliness in later life: the case of physical disability. J Health Soc Behav. (2009) 50:460–75. doi: 10.1177/002214650905000406
14. Grav S, Hellzèn O, Romild U, Stordal E. Association between social support and depression in the general population: the HUNT study, a cross-sectional survey. J Clin Nurs. (2012) 21:111–20. doi: 10.1111/j.1365-2702.2011.03868.x
15. Heydari ST, Izedi S, Sarikhani Y, Kalani N, Akbary A, Miri A, et al. The prevalence of substance use and associated risk factors among university students in the City of Jahrom, Southern Iran. Int J High Risk Behav Addic. (2015) 4:e22381. doi: 10.5812/ijhrba.4(2)2015.22381
16. Dutta S, Kar N, Thirthalli J, Nair S. Prevalence and risk factors of psychiatric disorders in an industrial population in India. Indian J Psychiatry. (2007) 49:103–8. doi: 10.4103/0019-5545.33256
17. Asharani PV, Ling Seet VA, Abdin E, Siva Kumar FD, Wang P, Roystonn K, et al. Smoking and mental illness: prevalence, patterns and correlates of smoking and smoking cessation among psychiatric patients. Int J Environ Res Public Health. (2020) 17:5571. doi: 10.3390/ijerph17155571
18. Raghuraman P, Balasundaram S, Sarkar S, Subramaniam E, A. cross-sectional study of psychiatric morbidity and quality of life among participants utilizing the preventive health-care services of a tertiary hospital. Indian J Psychiatry. (2019) 61:192–7. doi: 10.4103/psychiatry.IndianJPsychiatry_159_18
19. Daré LO, Bruand PE, Gérard D, Marin B, Lameyre V, Boumédiène F, et al. Co-morbidities of mental disorders and chronic physical diseases in developing and emerging countries: a meta-analysis. BMC Public Health. (2019) 19:304. doi: 10.1186/s12889-019-6623-6
20. Su TP, Lien TC, Yang CY, Su YL, Wang JH, Tsai SL, et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res. (2007) 41:119–30. doi: 10.1016/j.jpsychires.2005.12.006
21. Lee JI, Busler JN, Millett CE, Principe JL, Levin LL, Corrigan A, et al. Association between visceral adipose tissue and major depressive disorder across the lifespan: a scoping review. Bipolar Disord. (2022) 24:375–91. doi: 10.1111/bdi.13130
22. Li JY, Lee JI, Lu CC, Su YD, Chiu CT, Chen SC, et al. Hyperuricemia and its association with osteoporosis in a large Asian Cohort. Nutrients. (2022) 14:2206. doi: 10.3390/nu14112206
23. Chang CW, Ke HL, Lee JI, Lee YC, Jhan JH, Wang HS, et al. Metabolic syndrome increases the risk of kidney stone disease: a cross-sectional and longitudinal cohort study. J Personal Med. (2021) 11:1154. doi: 10.3390/jpm11111154
24. Lee MR, Ke HL, Huang JC, Huang SP, Geng JH. Obesity-related indices and its association with kidney stone disease: a cross-sectional and longitudinal cohort study. Urolithiasis. (2022) 50:55–63. doi: 10.1007/s00240-021-01288-w
25. Bebbington P, Dunn G, Jenkins R, Lewis G, Brugha T, Farrell M, et al. The influence of age and sex on the prevalence of depressive conditions: report from the national survey of psychiatric morbidity. Int Rev Psychiatry. (2003) 15:74–83. doi: 10.1080/0954026021000045976
26. Schuch FB, Vancampfort D. Physical activity, exercise, and mental disorders: it is time to move on. Trends Psychiatry Psychother. (2021) 43:177–84. doi: 10.47626/2237-6089-2021-0237
27. Olaya B, Bobak M, Haro JM, Demakakos P. Trajectories of verbal episodic memory in middle-aged and older adults: evidence from the english longitudinal study of ageing. J Am Geriatr Soc. (2017) 65:1274–81. doi: 10.1111/jgs.14789
28. Sporinova B, Manns B, Tonelli M, Hemmelgarn B, MacMaster F, Mitchell N, et al. Association of mental health disorders with health care utilization and costs among adults with chronic disease. JAMA Network Open. (2019) 2:e199910. doi: 10.1001/jamanetworkopen.2019.9910
29. Raghupathi W, Raghupathi V. An empirical study of chronic diseases in the United States: a visual analytics approach. Int J Environ Res Public Health. (2018) 15:431. doi: 10.3390/ijerph15030431
30. Bridges KW, Goldberg DP. Psychiatric illness in inpatients with neurological disorders: patients' views on discussion of emotional problems with neurologists. Br Med J. (1984) 289:656–8. doi: 10.1136/bmj.289.6446.656
31. Wang XY, Lin JJ, Lu MK, Jang FL, Tseng HH, Chen PS, et al. Development and validation of a web-based prediction tool on minor physical anomalies for schizophrenia. Schizophrenia. (2022) 8:4. doi: 10.1038/s41537-021-00198-5
32. Stahl ST, Beach SR, Musa D, Schulz R. Living alone and depression: the modifying role of the perceived neighborhood environment. Aging Mental Health. (2017) 21:1065–71. doi: 10.1080/13607863.2016.1191060
33. Xiu-Ying H, Qian C, Xiao-Dong P, Xue-Mei Z, Chang-Quan H. Living arrangements and risk for late life depression: a meta-analysis of published literature. Int J Psychiatry Med. (2012) 43:19–34. doi: 10.2190/PM.43.1.b
34. Dean A, Kolody B, Wood P, Matt GE. The influence of living alone on depression in elderly persons. J Aging Health. (1992) 4:3–18. doi: 10.1177/089826439200400101
35. Hunt C, Issakidis C, Andrews G, DSM-IV. generalized anxiety disorder in the Australian national survey of mental health and well-being. Psychol Med. (2002) 32:649–59. doi: 10.1017/S0033291702005512
36. Yu J, Choe K, Kang Y. Anxiety of older persons living alone in the community. Healthcare. (2020) 8:287. doi: 10.3390/healthcare8030287
37. Tucker JS. Health-related social control within older adults' relationships. J Gerontol Series B. (2002) 57:P387–95. doi: 10.1093/geronb/57.5.P387
38. Gove WR, Style CB, Hughes M. The effect of marriage on the well-being of adults:a theoretical analysis. J Family Issues. (1990) 11:4–35. doi: 10.1177/019251390011001002
39. Ren XS. Marital status and quality of relationships: the impact on health perception. Soc Sci Med. (1982) 44:241–9. doi: 10.1016/S0277-9536(96)00158-X
40. Kim HK, McKenry PC. The relationship between marriage and psychological well-being:a longitudinal analysis. J Family Issues. (2002) 23:885–911. doi: 10.1177/019251302237296
41. Schneider DS, Sledge PA, Shuchter SR, Zisook S. Dating and remarriage over the first two years of widowhood. Ann Clin Psychiatry. (1996) 8:51–7. doi: 10.3109/10401239609148802
42. Wilcox S, Evenson KR, Aragaki A, Wassertheil-Smoller S, Mouton CP, Loevinger BL. The effects of widowhood on physical and mental health, health behaviors, and health outcomes: the women's health initiative. Health Psychol. (2003) 22:513–22. doi: 10.1037/0278-6133.22.5.513
43. Krochalk PC Li Y, Chi I. Widowhood and self-rated health among Chinese elders: the effect of economic condition. Aust J Ageing. (2008) 27:26–32. doi: 10.1111/j.1741-6612.2007.00269.x
44. Moon JR, Kondo N, Glymour MM, Subramanian SV. Widowhood and mortality: a meta-analysis. PLoS One. (2011) 6:e23465. doi: 10.1371/journal.pone.0023465
45. Srivastava S, Debnath P, Shri N, Muhammad T. The association of widowhood and living alone with depression among older adults in India. Scient Rep. (2021) 11:21641. doi: 10.1038/s41598-021-01238-x
46. Ansari S, Muhammad T, Dhar M. How does multi-morbidity relate to feeling of loneliness among older adults? Evidence from a population-based survey in India. J Popul Ageing. (2021). doi: 10.1007/s12062-021-09343-5
47. Srivastava S, Shaw S, Chaurasia H, Purkayastha N, Muhammad T. Feeling about living arrangements and associated health outcomes among older adults in India: a cross-sectional study. BMC Public Health. (2021) 21:1322. doi: 10.1186/s12889-021-11342-2
48. Wang S, Quan L, Chavarro JE, Slopen N, Kubzansky LD, Koenen KC, et al. Associations of depression, anxiety, worry, perceived stress, and loneliness prior to infection with risk of post-COVID-19 conditions. JAMA Psychiatry. (2022) 79:1081–91. doi: 10.1001/jamapsychiatry.2022.2640
49. Qi T, Hu T, Ge QQ, Zhou XN Li JM, Jiang CL, et al. COVID-19 pandemic related long-term chronic stress on the prevalence of depression and anxiety in the general population. BMC Psychiatry. (2021) 21:380. doi: 10.1186/s12888-021-03385-x
50. Wongprommate D, Wongpakaran T, Pinyopornpanish M, Lerttrakarnnon P, Jiraniramai S, Satthapisit S, et al. Predictors for quality of life among older adults with depressive disorders: A prospective 3-month follow-up cohort study. Perspect Psychiatr Care. (2022) 58:1029–36. doi: 10.1111/ppc.12895
51. Levula A, Wilson A, Harré M. The association between social network factors and mental health at different life stages. Quality of Life Res. (2016) 25:1725–33. doi: 10.1007/s11136-015-1200-7
52. Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. (2018) 18:156. doi: 10.1186/s12888-018-1736-5
53. Domènech-Abella J, Mundó J, Haro JM, Rubio-Valera M. Anxiety, depression, loneliness and social network in the elderly: Longitudinal associations from The Irish longitudinal study on ageing (TILDA). J Affect Disord. (2019) 246:82–8. doi: 10.1016/j.jad.2018.12.043
54. Shaw RJ, Cullen B, Graham N, Lyall DM, Mack, et al. Living alone, loneliness and lack of emotional support as predictors of suicide and self-harm: a nine-year follow up of the UK Biobank cohort. J Affect Disord. (2021) 279:316–23. doi: 10.1016/j.jad.2020.10.026
55. Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. (2016) 387:1227–39. doi: 10.1016/S0140-6736(15)00234-2
56. Tabue Teguo M, Simo-Tabue N, Stoykova R, Meillon C, Cogne M, Amiéva H, et al. Feelings of loneliness and living alone as predictors of mortality in the elderly: the PAQUID study. Psychosomat Med. (2016) 78:904–9. doi: 10.1097/PSY.0000000000000386
57. Robinette JW, Charles ST, Mogle JA, Almeida DM. Neighborhood cohesion and daily well-being: results from a diary study. Soc Sci Med. (1982) 96:174–82. doi: 10.1016/j.socscimed.2013.07.027
58. Arrieta H, Rezola-Pardo C, Echeverria I, Iturburu M, Gil SM, Yanguas JJ, et al. Physical activity and fitness are associated with verbal memory, quality of life and depression among nursing home residents: preliminary data of a randomized controlled trial. BMC Geriatr. (2018) 18:80. doi: 10.1186/s12877-018-0770-y
59. Elliott J, Gale CR, Parsons S, Kuh D. Neighbourhood cohesion and mental wellbeing among older adults: a mixed methods approach. Soc Sci Med. (1982) 107:44–51. doi: 10.1016/j.socscimed.2014.02.027
60. Yoshida Y, Iwasa H, Ishioka Y, Suzukamo Y. Leisure activity moderates the relationship between living alone and mental health among Japanese older adults. Geriatr Gerontol Int. (2021) 21:421–5. doi: 10.1111/ggi.14151
61. Yoshida Y, Iwasa H, Kumagai S, Suzuki T, Awata S, Yoshida H. Longitudinal association between habitual physical activity and depressive symptoms in older people. Psychiatry Clin Neurosci. (2015) 69:686–92. doi: 10.1111/pcn.12324
62. Chao SF. Changes in leisure activities and dimensions of depressive symptoms in later life: a 12-year follow-up. Gerontologist. (2016) 56:397–407. doi: 10.1093/geront/gnu052
63. Yellowlees PM, Alpers JH, Bowden JJ, Bryant GD, Ruffin RE. Psychiatric morbidity in patients with chronic airflow obstruction. Med J Aust. (1987) 146:305–7. doi: 10.5694/j.1326-5377.1987.tb120267.x
64. Bergquist H, Ruth M, Hammerlid E. Psychiatric morbidity among patients with cancer of the esophagus or the gastro-esophageal junction: a prospective, longitudinal evaluation. Dis Esoph. (2007) 20:523–9. doi: 10.1111/j.1442-2050.2007.00741.x
65. Wong WS, Chen PP, Yap J, Mak KH, Tam BK, Fielding R. Chronic pain and psychiatric morbidity: a comparison between patients attending specialist orthopedics clinic and multidisciplinary pain clinic. Pain Med. (2011) 12:246–59. doi: 10.1111/j.1526-4637.2010.01044.x
66. Ron MA, Logsdail SJ. Psychiatric morbidity in multiple sclerosis: a clinical and MRI study. Psychol Med. (1989) 19:887–95. doi: 10.1017/S0033291700005602
67. Chaudhry R, Mishra P, Mishra J, Parminder S, Mishra BP. Psychiatric morbidity among diabetic patients: a hospital-based study. Indust Psychiatry J. (2010) 19:47–9. doi: 10.4103/0972-6748.77637
68. Davies SJ, Jackson PR, Potokar J, Nutt DJ. Treatment of anxiety and depressive disorders in patients with cardiovascular disease. BMJ. (2004) 328:939–43. doi: 10.1136/bmj.328.7445.939
69. Frasure-Smith N, Lespérance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. (1995) 91:999–1005. doi: 10.1161/01.CIR.91.4.999
70. Sharma BB, Singh S, Sharma VK, Choudhary M, Singh V, Lane S, et al. Psychiatric morbidity in chronic respiratory disorders in an Indian service using GMHAT/PC. Gen Hosp Psychiatry. (2013) 35:39–44. doi: 10.1016/j.genhosppsych.2012.09.009
71. Serebruany VL, Glassman AH, Malinin AI, Nemeroff CB, Musselman DL, van Zyl LT, et al. Platelet/endothelial biomarkers in depressed patients treated with the selective serotonin reuptake inhibitor sertraline after acute coronary events: the sertraline antidepressant heart attack randomized trial (SADHART) platelet substudy. Circulation. (2003) 108:939–44. doi: 10.1161/01.CIR.0000085163.21752.0A
72. Sauer WH, Berlin JA, Kimmel SE. Effect of antidepressants and their relative affinity for the serotonin transporter on the risk of myocardial infarction. Circulation. (2003) 108:32–6. doi: 10.1161/01.CIR.0000079172.43229.CD
73. Zhang C, Wang T, Zeng P, Zhao M, Zhang G, Zhai S, et al. Reliability, validity, and measurement invariance of the general anxiety disorder scale among Chinese medical university students. Front Psychiatry. (2021) 12:648755. doi: 10.3389/fpsyt.2021.648755
74. Silva MT, Caicedo Roa M, Martins SS, da Silva ATC, Galvao TF. Generalized anxiety disorder and associated factors in adults in the Amazon, Brazil: a population-based study. J Affect Disord. (2018) 236:180–6. doi: 10.1016/j.jad.2018.04.079
75. Araya R, Lewis G, Rojas G, Fritsch R. Education and income: which is more important for mental health? J Epidemiol Commun Health. (2003) 57:501–5. doi: 10.1136/jech.57.7.501
76. Yu Y, Williams DR. Socioeconomic status and mental health. In:Aneshensel CS, Phelan JC, , editors. Handbook of the Sociology of Mental Health. Boston, MA: Springer US (1999). p. 151–166.
Keywords: dependence, depression, anxiety, Psychiatric disorders, psychiatric distress, psychiatric morbidities, living alone
Citation: Chen T-Y, Geng J-H, Chen S-C and Lee J-I (2022) Living alone is associated with a higher prevalence of psychiatric morbidity in a population-based cross-sectional study. Front. Public Health 10:1054615. doi: 10.3389/fpubh.2022.1054615
Received: 27 September 2022; Accepted: 03 November 2022;
Published: 17 November 2022.
Edited by:
Maha Atout, Philadelphia University, JordanCopyright © 2022 Chen, Geng, Chen and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jia-In Lee, u9400039@gmail.com
 Te-Yu Chen
Te-Yu Chen Jiun-Hung Geng
Jiun-Hung Geng Szu-Chia Chen
Szu-Chia Chen Jia-In Lee9,10*
Jia-In Lee9,10*