- The Third Affiliated Hospital of Zhengzhou University, Zhengzhou, China
Background: Fear of childbirth (FOC) is one of the most common psychological symptoms among pregnant women and significantly relates to cesarean section, anxiety, and depression. However, it is not clear the prevalence and risk factors of FOC among Chinese pregnant women since the outbreak of the COVID-19 pandemic.
Aims: The objective of this study was to examine the associations between coping styles, intolerance of uncertainty, and FOC.
Method: From December 2021 to April 2022, a cross-sectional survey was conducted in two hospitals in China through convenient sampling. The cross-sectional survey was conducted among 969 pregnant women, which included the Childbirth Attitude Questionnaire (CAQ), Intolerance of Uncertainty Scale-12 (IUS-12), and Simplified Coping Style Questionnaire (SCSQ).
Results: The total prevalence of FOC was 67.8%. The percentages of women with mild (a score of 28–39), moderate (40–51), and severe FOC (52–64) were 43.6, 20.2, and 4.0%, respectively. The regression results indicated that primiparas, unplanned pregnancy, few spousal support, intolerance of uncertainty, and negative coping styles were significant risk factors of FOC. Women who adopt positive coping strategies experienced a lower level of childbirth fear.
Conclusion: These findings suggest that cultivating positive coping styles and obtaining sufficient childbirth information may be helpful for mothers' mental health. Regular screening assessment of perinatal psychological symptoms, such as the high level of intolerance of uncertainty and negative coping styles, should be adopted to reduce the risk of fear of childbirth.
Introduction
Fear of childbirth (FOC), a spectrum of anxious thoughts and feelings relating to woman's appraisal of labor and birth, was reported to be a prevalence of 14% around the world (1–4). Prior research has found that mild or high levels of FOC are correlated with prolonged labor, cesarean section, choice of epidural analgesia, prenatal and postpartum depression, and anxiety (5–9). The potential risk factors of FOC (e.g., young age, low educational level, anxiety, depression) have been identified in different countries or regions (8, 10–12). Additionally, Rondung et al. suggested that intolerance of uncertainty (IU) was one of the best predictors of FOC (13). However, the relationships among FOC, IU, and other variables are seldom investigated clearly in China during the COVID-19 pandemic.
Emerging evidence has shown that the COVID-19 outbreak had a significant psychological impact on pregnant women (14–16). Temporary closure of public places, strict quarantine policies, and other measures were taken in various countries to prevent the spread of the virus (14, 17–19). There was a lot of available negative news information about COVID-19 online, which may increase distress and fears for the users. A prior study revealed that users interested in suicide-related news are more likely to search it through various applications (20). Furthermore, it is confirmed that pregnant women have experienced more psychological symptoms since the outbreak (21). In addition, the extreme uncertainty caused by the COVID-19 pandemic elevated anxiety and fears among pregnant women (21–24). Baldessarini et al. also suggested that affective-temperament ratings, which were related to psychological distress and negative clinical outcomes, were higher in females (25). Thus, pregnant women may experience significant distress as they have continuously faced ambiguous circumstances during the pandemic.
Intolerance of uncertainty (IU) is defined as the tendency to react negatively to uncertainty, and it is a potential important transdiagnostic factor related to multiple psychological disorders in fear of childbirth (26–30). Previous studies have investigated that IU has robust associations with a range of disorder symptoms, including generalized anxiety disorder, social anxiety disorder, panic disorder, and agoraphobia (26, 27, 31). People with high levels of intolerance of uncertainty tend to experience greater physiological distress and avoidance of uncertainty (23, 32–36).
In addition, COVID-19 is an exemplar of a real-world uncertain and threatening situation related to uncertainty distress (37). Moreover, anxiety sensitivity significantly increased individuals' COVID-19 worries and behaviors, especially those with high IU (38). Emerging evidence suggests that individuals with high IU may take different threat reactivity strategies (e.g., internet searches and avoidance) to adjust to changing information about COVID-19 threats (39, 40). Meanwhile, pregnant women with high IU usually adopt avoidance strategies to cope with stress, which failed to improve the current situation (16, 26, 27). Consequently, an appropriate coping response (positive coping styles) toward uncertainty may protect pregnant women from the potentially detrimental impacts of the COVID-19 pandemic.
In Lazarus and Folkman's transactional coping theory (41), coping was defined as continuously altering cognitive and behavioral efforts to respond to stressors. The coping style included two widely known primary functions: emotion-focused coping (e.g., passive or active avoidance, escaping and positively reappraising the stressor) and problem-focused coping (e.g., seeking practical or informational support). It is of great significance to explore the relationships between psychological risk factors and coping styles of pregnant women during the pandemic to help them deal with stressors effectively. However, to the best of our knowledge, studies elucidating the relationships of IU, coping styles, and FOC in Chinese pregnant women are limited.
Given that intolerance of uncertainty and different coping styles have been well documented as predictors for individuals' mental health, it would be of great value to investigate the relationships among IU, FOC, and coping styles of pregnant women during the COVID-19 pandemic. In addition, the examination of risk factors related to FOC is essential for researchers to develop efficient interventions to improve pregnant women's mental health and ameliorate the erosion of the distress caused by the pandemic.
Therefore, the underlying hypothesis was that intolerance of uncertainty and negative coping styles would be positively related to fear of childbirth, but positive coping styles would be inversely correlated with IU and FOC in Chinese pregnant women. This study aims to investigate the prevalence and risk factors of FOC in Chinese pregnant women during the COVID-19 pandemic.
Materials and Methods
Design
From December 2021 to April 2022, a cross-sectional survey was conducted in two hospitals in China through convenient sampling. All participants were informed of the study's purpose and required to provide an informed consent form online before enrollment. The online platform of Wenjuanxing (https://www.wjx.cn/app/survey.aspx) was employed to distribute the electric questionnaires, which indicated to the participants when they had unanswered questions.
This survey included the sociodemographic characteristics questionnaire, the Childbirth Attitude Questionnaire (CAQ), the Intolerance of Uncertainty Scale-12 (IUS-12), and the Simplified Coping Style Questionnaire (SCSQ). Finally, there were 969 eligible samples in the data analyses.
Study Participants
Inclusion criteria comprised being over 20 years of age, pregnant at 12–40 weeks with no severe gestational complications, no history of severe physical illness, fluent in Mandarin, and access to a smartphone.
Women with diagnoses of threatened abortion and fetal anomaly were excluded. All pregnant women need to provide online written informed consent at the beginning of this survey.
Measurements
Sociodemographic and Obstetrical Characteristics Questionnaire
According to previous reviews and research (2, 10, 11, 42–44), we constructed the sociodemographic and obstetrical characteristics questionnaire to collect general information of pregnant women. It included age, employment status, educational level, monthly income (CNY), marital status, residence, medical insurance, gestational week, parity, planning of pregnancy, family's opinion of a childbirth mode, the preferred mode of childbirth, prenatal spousal support, access to childbirth information, and a regular prenatal visit. And the mode of previous birth and epidural analgesia during the last labor were added to it for the data collection of multiparous women.
Childbirth Attitude Questionnaire
The Chinese version of the Childbirth Attitude Questionnaire (CAQ) (45) was employed in this study. It was first designed by Areskog (46) and developed by Lowe (47) and Tanglakmankhong (48). Then, Wei et al. (45) translated it into Chinese and found four dimensions of the CAQ: fear of baby safety (FBS), fear of labor pain (FLP), fear of losing control (FLC), and fear of environment (FE). The CAQ consisted of 16 items scored on a 4-point Likert scale (1 “never” to 4 “high”). Scores of 16–27, 28–39, 40–51, and 52–64 represent mild, moderate, and severe fear of childbirth. It was reported good internal consistency reliability (Cronbach's α = 0.910) (45). Internal consistency of CAQ in this survey also showed excellent (Cronbach's α = 0.942).
Intolerance of Uncertainty Scale−12
Freeston et al. (29) first proposed the term intolerance of uncertainty and constructed the Intolerance of Uncertainty Scale (IUS) in 1994. Then, Carleton et al. (49) simplified it into the IUS-12 in 2007. The IUS-12 scored on a 5-point Likert scale (1, “not at all characteristic of me” to 5, “entirely characteristic of me”). Wu et al. (50) translated the IUS-12 into Chinese and investigated the IUS-12 consists of three dimensions: prospective action (PA), inhibitory action (IA), and prospective emotion (PE). In the Chinese IUS-12, Cronbach's alpha reliability coefficient was reported to be 0.79 in 1,275 Chinese adolescents. The Cronbach's α of IUS-12 was 0.853 in this study.
Simplified Coping Style Questionnaire
Xie compiled the SCSQ in 1998 (51), and it was widely used to assess coping styles in China. Xie simplified the ways of coping questionnaire (WCQ), first designed by Folkman and Lazarus (41). The SCSQ is a universal self-rating scale with 20 items and includes two subscales: positive coping (SCSQ-P) and negative coping (SCSQ-N). It scored on a 4-point Likert scale (0, “do not use” to 3, “often use”). The higher the sum score of the positive coping dimension was, the more pronounced the participants' propensity to adopt it and vice versa. The SCSQ showed good internal consistency (Cronbach's α = 0.868) in this study, as well as its sub-scales: 0.900 (SCSQ-P) and 0.837 (SCSQ-N).
Data Collection
Trained midwives conducted the prenatal survey at the Perinatal Health Care Clinics of two tertiary hospitals in Henan Province, China. The online platform Wenjuanxing was employed to complete the survey. It will automatically generate a QR code or URL link for the manually entered questionnaire.
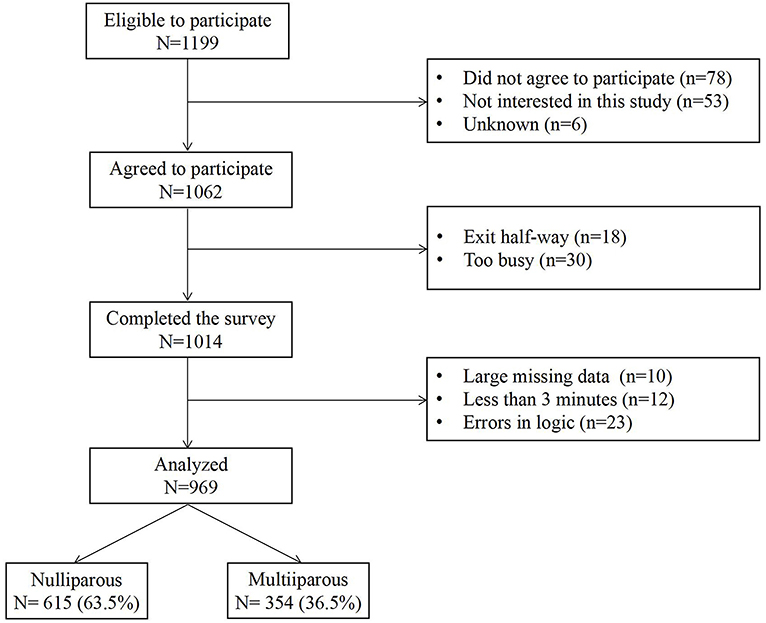
During the survey, the midwives showed pregnant women the printed picture of the questionnaires' QR code or sent the URL link using WeChat. Then the participants scanned the QR code or clicked on the link to fill in the questionnaire within 15 min. There were no missing data because the survey was conducted through Wenjuanxing, which indicates to the participants when they had unanswered questions. Furthermore, all the collected data were manually checked for the questionnaire answer time (<3 min was excluded) and whether the answer was logical and reasonable (e.g., answering regularly or choosing the same option was excluded). The flow chart of the participants is shown in Figure 1.
Data Analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS, version 25.0 for Windows). The participants' sociodemographic characteristics and the scores of CAQ, IUS-12, and SCSQ were presented with the frequencies, percentages, means (M), standard deviations (SD), and range of scores. Chi-square tests were used to explore the group differences in CAQ scores (CAQ < 28 and CAQ ≥ 28), as appropriate. Correlation analysis was performed to examine the relationships between FOC and independent variables, including demographic characteristics and the sum scores of CAQ, IUS-12, and SCSQ.
According to previous reviews and research (2, 10, 11, 42–44), age, parity, gestational weeks, and spousal support were associated with FOC. Thus, the exploratory analysis was first conducted to clarify the relationships between sociodemographic and obstetric factors and FOC. After these preliminary analyses, the multiple hierarchical linear regression for predicting FOC was conducted to investigate whether intolerance of uncertainty and coping style could significantly affect FOC. With the scores of SCSQ-P, SCSQ-N, and IUS-12 as independent variables and the score of CAQ as the dependent variable, the hierarchical linear regression analysis for predicting FOC was constructed by enter method.
The multiple linear regression analysis was established in three steps using the score of CAQ as the dependent variable, and the independent variables were entered in the following steps: (1) sociodemographic and obstetric factors (e.g., age, educational level, and parity); (2) the score of SCSQ-P; (3) the score of SCSQ-N; (4) the score of IUS-12.
In addition, we compared the mean differences across the scores of CAQ, SCSQ, and IUS-12 according to parity. The scores of the two groups were presented with means (M) and the range of scores. Mean differences of them were assessed using Pearson t-test. Then, linear regression analysis was employed to evaluate the predictors of FOC in nulliparous and multiparous women, respectively. The level of statistical significance was set at p < 0.05.
Results
Participant Characteristics
There were 969 valid questionnaires, including 615 (63.5%) nulliparas and 354 (36.5%) multiparas. The mean age of pregnant women was 30.1 (SD = 3.8). Most of the participants were pregnant at 12–28 weeks (n = 620), full-time workers (n = 638), middle-income households of China (n = 378), and with college or above educational background (n = 794). Of the 969 pregnant women, 67.1% (n = 650) were planned pregnancy, 27.5% (n = 266) were unplanned pregnancy, and 5.5% (n = 53) were assisted reproductive technology pregnancy. Most of the participants received full support from their spouses (87.2%), while 11.1% were general support and 1.7% had little support.
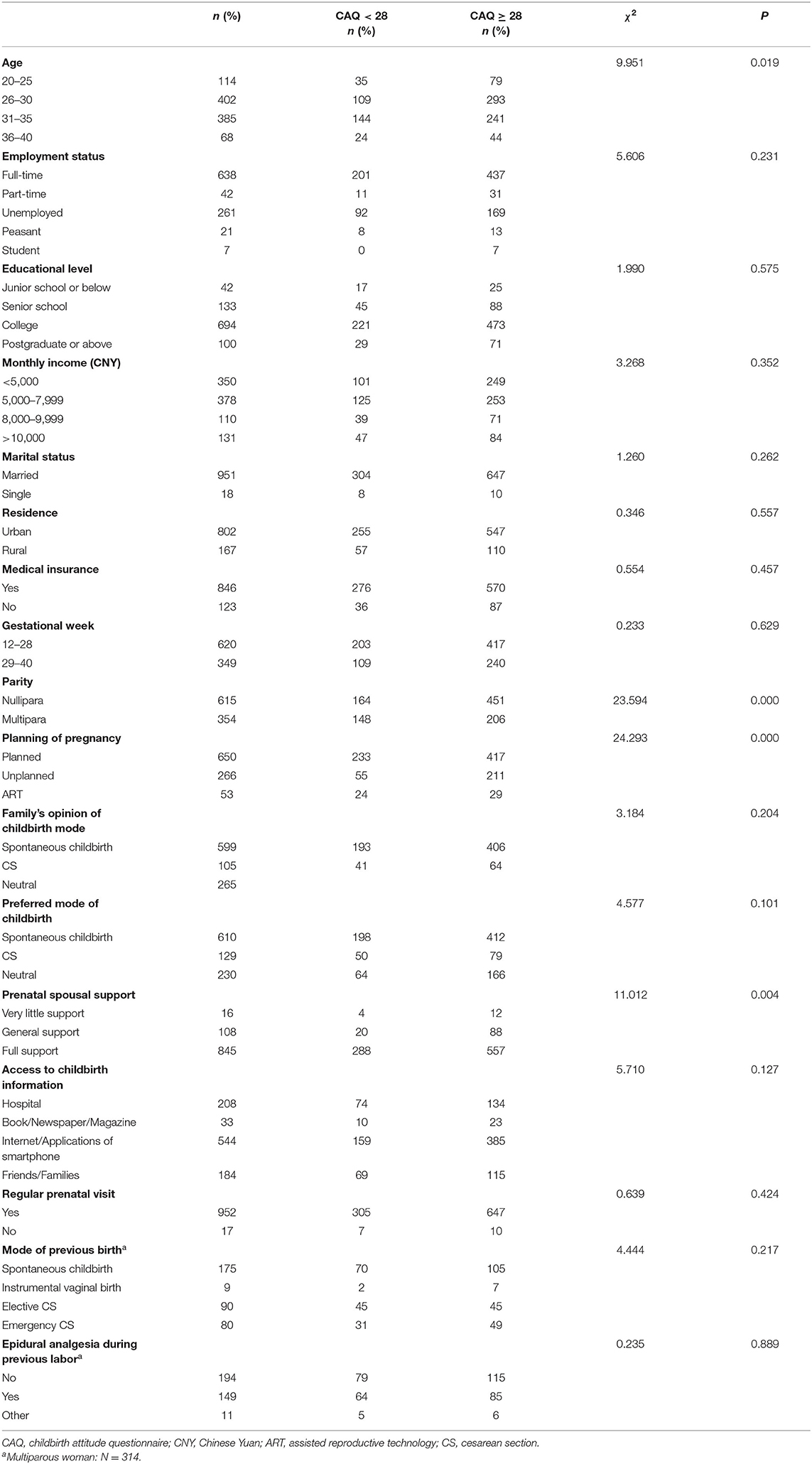
Furthermore, chi-square tests showed that there were significant differences between the fear of childbirth group (CAQ ≥ 28) and no fear of childbirth group (CAQ < 28) on the part of maternal age, parity, planning of pregnancy, and prenatal spousal support (all P-values < 0.05). Additional sociodemographic and obstetric variables are shown in Table 1.
Descriptive Statistics of Measurements
Total
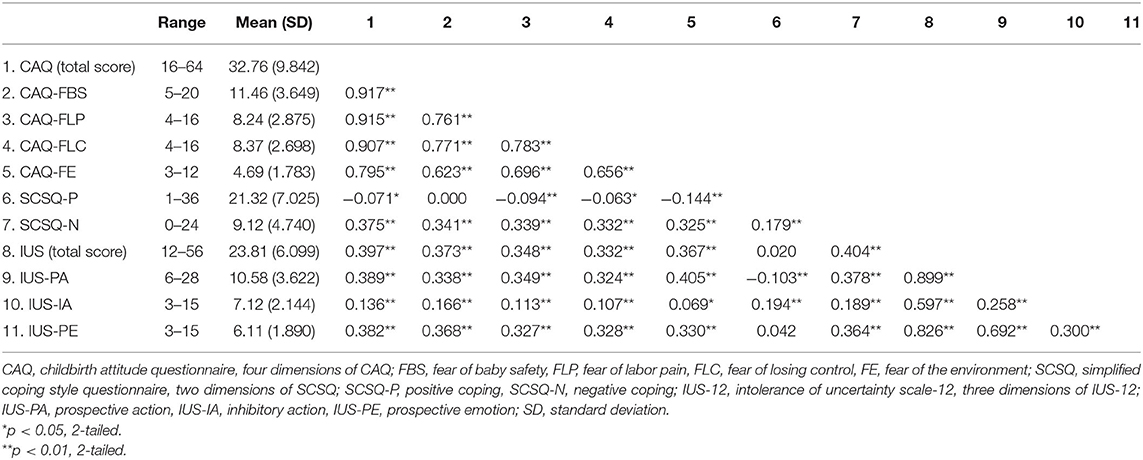
The results of the scores of the CAQ, SCSQ, and IUS-12 among 969 pregnant women are shown in Table 2. The mean score of the CAQ was 32.76 (SD = 9.842), and 67.8% (n = 657) of women had FOC symptoms with a CAQ score ≥ 28. The percentages of women with mild (score of 28–39), moderate (40–51), and severe FOC (52–64) were 43.6, 20.2, and 4.0%, respectively. The mean scores of the SCSQ-P and SCSQ-N were 21.32 (SD = 7.025) and 9.12 (SD = 4.740), respectively. The mean IUS-12 score was 23.81 (SD = 6.099), and 52.1% of women (n = 505) scored higher than average.
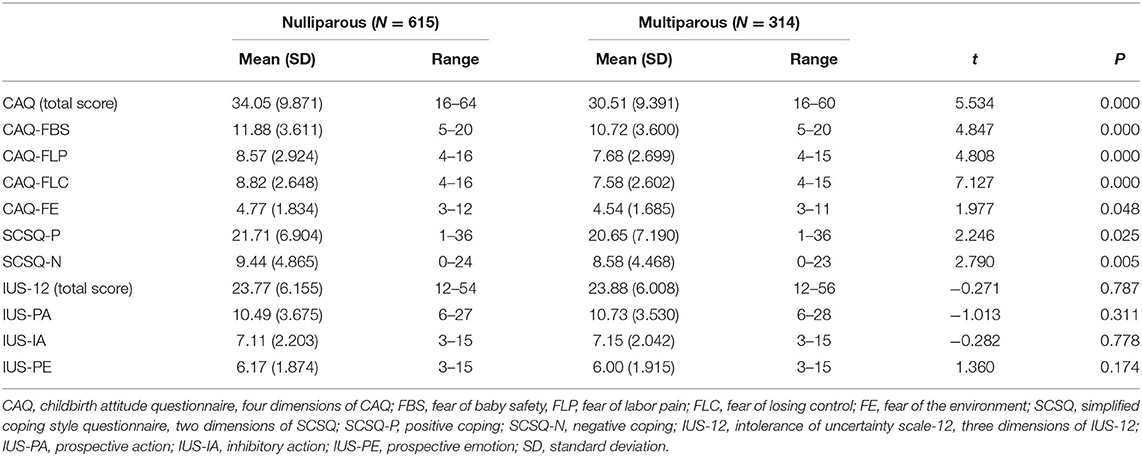
Mean Differences Across CAQ, SCSQ, and IUS-12 in Parity
The mean differences across CAQ, SCSQ, and IUS-12 between nulliparous and multiparous women are shown in Table 3. It was investigated that nulliparous and multiparous women differed significantly in the sum scores of the CAQ, the SCSQ-P, and SCSQ-N (all P-values < 0.05). There were no significant differences in the sum scores of IUS-12 between nulliparous and multiparous women.
Correlations Analyses
The results of correlational analyses are shown in Table 2. The sum scores of CAQ positively correlated with negative coping styles (r = 0.375, p < 0.01) and IU (r = 0.397, p < 0.01) while negatively related with positive coping styles (r = −0.071, p < 0.05). Furthermore, the sum scores of SCSQ-N correlated with IUS-12 significantly (r = 0.404, p < 0.01). However, there was no significant correlation between the sum scores of SCSQ-P and IUS-12.
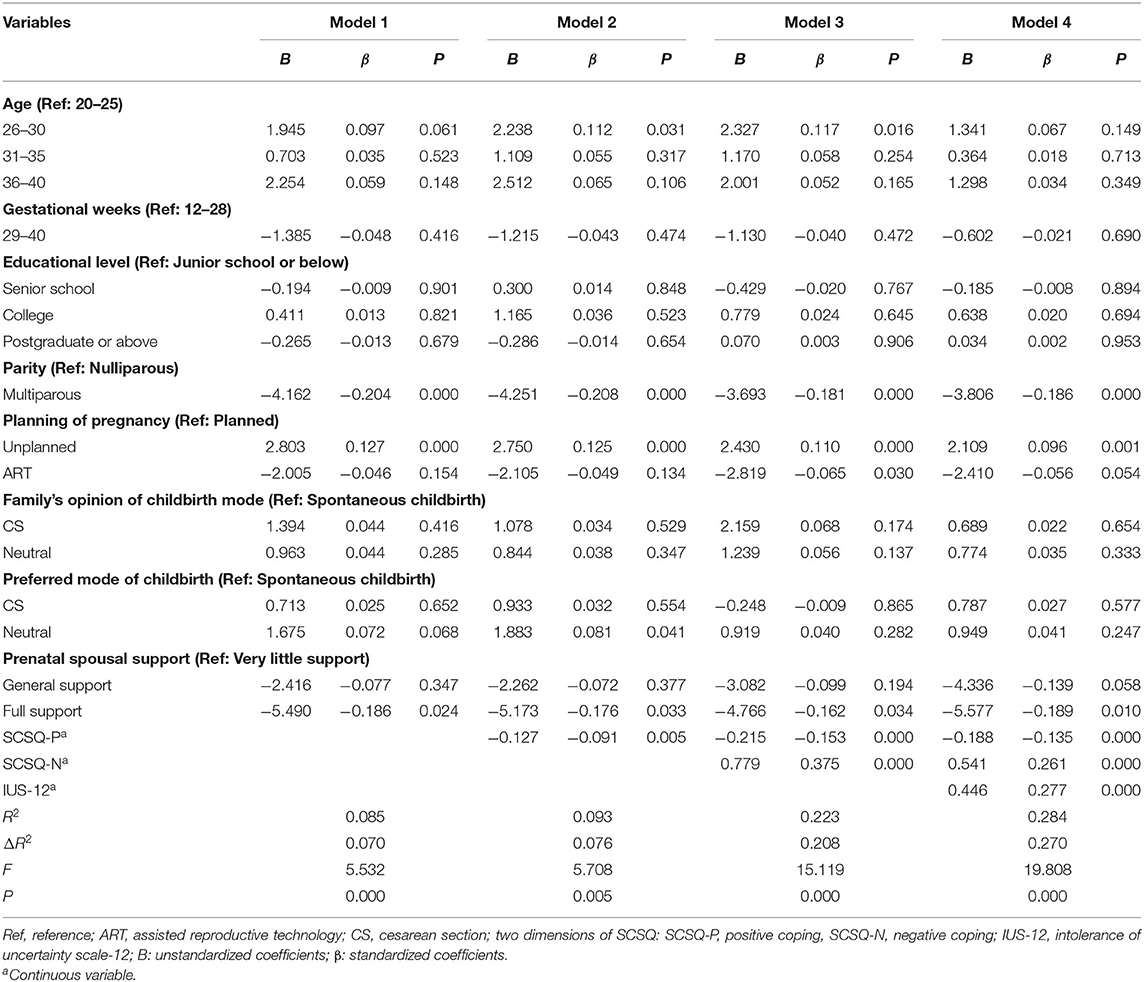
Hierarchical Linear Regression for Predicting FOC
The results are shown in Table 4. It was investigated that the sociodemographic and obstetric characteristics could explain 8.5% of the variation in FOC (Model 1: F = 5.532, R2 = 0.085, p = 0.000). Model 2 (F = 5.708, R2 = 0.093, p = 0.005) could explain 9.3% of the variation in FOC, of which 0.8% were explained by the sum score of SCSQ-P. In Model 3 (F = 15.119, R2 = 0.223, p = 0.000), all variables explained 22.3% of the variation in FOC. Additionally, SCSQ-P (β = −0.153, p < 0.000) and SCSQ- N (β = 0.375, p < 0.000) were significant risk factors of the FOC. In Model 4 (F = 19.808, R2 = 0.284, p = 0.000), all the included variables explained 28.4% of the variation in FOC, of which 6.1% were explained by the sum score of IUS-12. In addition, the influences of the score of SCSQ-P (β = −0.135, p < 0.000), SCSQ-N (β = 0.261, p < 0.000), and IUS-12 (β = 0.277, p < 0.000) were significant.
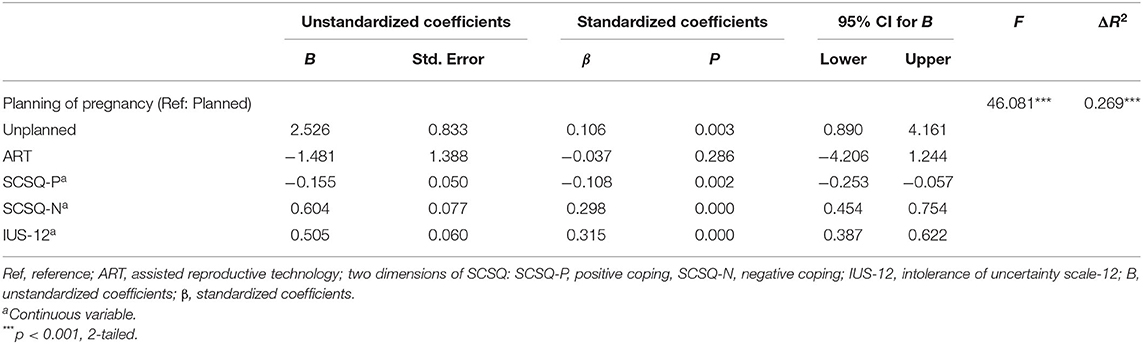
Table 5 shows the results of linear regression for predicting FOC among nulliparous women (F = 46.081, adjusted R2 = 0.269). It was worth noting that higher scores of CAQ were significantly associated with unplanned pregnancy (β = 0.106, p = 0.003), a lower score of SCSQ-P (β = −0.108, p = 0.002), a higher score of SCSQ-N (β = 0.298, p = 0.000) and IUS-12 (β = 0.315, p = 0.000).
Table 6 reveals that part-time workers (β = 0.141, p = 0.004), unplanned pregnancy (β = 0.119, p = 0.014), the score of SCSQ-P (β = −0.187, p = 0.000), SCSQ-N (β = 0.192, p = 0.001), and IUS-12 (β = 0.273, p = 0.000) were risk factors of FOC among multiparous women.
Discussion
Fear of childbirth has become one of the most common psychological symptoms. It is confirmed that FOC leads to significant anxiety, depression, and loneliness (1, 2, 4, 52). We found that the prevalence of FOC was 67.8% (Childbirth Attitude Questionnaire, CAQ ≥ 28) in the present study, which is consistent with one research in Chongqing, China (67.1%) (32) and a survey in Guangdong, China (79.4%) (53). However, there were lower incidences of FOC reported in Sweden (24.6%) and Italy (8.2%) before the outbreak of the COVID-19 pandemic (13, 54). Moreover, approximately 24.2% of the sample reported high or severe FOC in this study. In addition, IU and negative coping styles were positively correlated with the sum score of CAQ. However, it is investigated that the positive coping style of pregnant women was inversely related to fear of childbirth. According to the results, it may be helpful for pregnant women with FOC symptoms to adopt positive coping styles and decrease the level of intolerance of uncertainty.
Since the COVID-19 pandemic was declared by the World Health Organization (WHO) (55), a growing body of evidence has shown that pregnant women have experienced more psychological symptoms (14, 16, 21). Because of the heterogeneity of measurement tools of FOC, several studies reported lower rates of moderate FOC among pregnant women during the pandemic: 10.% in Portugal and 31.% in Iran (2, 56). Therefore, a multicenter cross-sectional survey and a larger sample are necessary to explore the incidence and predictors of FOC during the COVID-19 pandemic. Although the potential risk factors of FOC are widely demonstrated and reported in previous studies from various countries, there is a lack of research validating the relationships between intolerance of uncertainty, coping styles, and FOC in China.
Our study identified that primiparas, unplanned pregnancy, and little spousal support were significant risk factors in FOC. In line with previous research (2, 44, 57), primiparity was one of the significant predictors of severe FOC. In contrast, one Finland population-based analysis suggested that multiparous women also tended to have fear of childbirth for previous cesarean section, preterm birth, and unspecified socioeconomic status (58). Given that parity was the strong predictor of FOC, we compared different risk factors of FOC between nulliparous and multiparous. According to the results, unplanned pregnancy, negative coping style, and IU were predictors of FOC in both nulliparous and multiparous. Of note, unplanned pregnant women tend to score higher on FOC (59, 60). They may consider this pregnancy unintended or unwanted, which is associated with a sense of being unprepared to be a mother (44, 59). At the same time, part-time work was significantly related to FOC in multiparous. The uncertain income and poor financial status of pregnant women may contribute to life stress. Similar to the present study, a lack of spousal support relates to an increased probability of FOC (44, 61). However, Bilgin et al. argued that there is no significant relationship between spousal support and FOC (62). Because the samples and measurement tools are different, various studies have inconsistent results. Therefore, further research is warranted in different countries and regions to specify these associations in the present study.
According to the results, 26.5% of women adopt negative coping styles (Simplified Coping Style Questionnaire-Negative coping styles, SCSQ-N ≥ 12). A similar result was obtained in a cross-sectional survey during the pandemic (16). In addition, it is confirmed that passive coping strategies of pregnant women are correlated with depression, anxiety, and psychological distress (63). Daglar et al. also suggested that optimistic coping styles with stress were correlated with pregnant women's self-confidence (64). Interestingly, our study investigated that negative coping styles were risk factors in FOC, while positive coping styles were protective factors. Therefore, positive coping styles may be associated with better mental resiliency and helpful for women to face distress during pregnancy.
In addition, the present study confirmed that IU was positively related to FOC, consistent with the survey conducted by Rondung et al. (13). The uncertainty caused by the pandemic may increase pregnant women's fear of childbirth and worry about being infected with the virus. The unpredictability caused by pandemic restrictions may increase pregnant women's fears and worries about childbirth. Pregnant women with high IU would experience significant distress and anxiety and take different coping strategies when faced with ambiguous circumstances (22, 24, 65).
A recent review has suggested that non-pharmacological treatments may reduce the fear of childbirth and cesarean section births (66). In light of the evidence about alleviating the FOC of pregnant women, psychoeducation intervention based on Human Caring Theory, online cognitive behavior therapy, mindfulness training, art therapy, and haptotherapy effectively decrease the level of FOC (3, 30, 67–70). Furthermore, access to childbirth information was associated with a decreased likelihood of fear of birth and cesarean delivery (71). It is investigated that sufficient information about childbirth and positive coping strategies (e.g., mindfulness training, psychoeducation training, art therapy) may decrease the IU and FOC of pregnant women.
To some extent, the present study further highlights the impact and risk factors of FOC among pregnant women. It may provide a new perspective to construct the targeted interventions of FOC. The current findings have important implications for the assessment and treatment of fear of childbirth among pregnant women. It is indicated that primiparas, unplanned pregnancy, few spousal support, intolerance of uncertainty, and negative coping styles were significant risk factors in FOC. Women who adopt positive coping strategies experience a lower level of childbirth fear. It is suggested that more attention should be paid to identifying pregnant women with the high level of IU, especially for nulliparous. For instance, knowing that pregnant women with high IU tend to adopt negative coping styles, clinicians could make more empirically informed decisions to intervene in psychological treatment.
However, as a cross-sectional study, the universality of the results was limited, and the long-term effects of COVID-19 on pregnant women may not be inferred using the current results. Thus, there are several limitations of our study that should be noted. First, the convenient sampling method may lead to certain methodological limitations. The small number of participants in some subgroups may induce sample selection bias. Future studies need a larger sample to establish and confirm causal relationships among FOC, IU, and coping styles. Second, the data were self-report without external observation. Therefore, FOC, IU, and coping styles of pregnant women cannot be considered the diagnosis of psychopathology. In addition, the cut-off scores of measurements in this study should be investigated in the future. Third, although most of the differences in background variables were controlled, some variables (e.g., personality, pregnancy status) cannot be controlled. Fourth, because the level of fear of COVID-19 in pregnant women was not measured in this study, it is difficult to infer how the pandemic affected the main variables in the study. Furthermore, the survey did not include other negative emotionality variables (e.g., trait anxiety, neuroticism, depression). Thus, these results may not be specific to IU and negative coping styles. As such, our results should be replicated in a larger sample to verify the relations between IU, the coping styles, and FOC of pregnant women. Therefore, future research should pay more attention to prenatal psychological symptoms screening and the construction of targeted interventions for FOC.
Conclusion
In summary, the results revealed that the prevalence of FOC was 67.8% among 969 Chinese pregnant women. It is identified that primiparas, unplanned pregnancy, few spousal support, intolerance of uncertainty, and negative coping styles were significant risk factors in FOC. Thus, more attention should be paid to screening perinatal psychological symptoms, such as the high level of intolerance of uncertainty and negative coping styles. Future research should be conducted to verify our findings within a large and cross-regional sample, and a longitudinal study is necessary.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The research was conducted in accordance with the Declaration of Helsinki. The study was supported by the Ethics Committee of the Third Affiliated Hospital of Zhengzhou University and the Chinese Health Department (No. 2021-169-01). Written consent was obtained from the participants, and they voluntarily participated in this study.
Author Contributions
LH contributed to the design of the study, acquisition of data, and revision of the manuscript. HB critically reviewed the manuscript and provided English edits. BL contributed to the acquisition of data and revision of the manuscript. YL and YW contributed to the acquisition and interpretation of data. All the authors read and approved the final manuscript.
Funding
This research was supported by the Joint Construction Project of Henan Province's Medical Science and Technology Research Plan (No. SBGJ2018049).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to express our appreciation for the great cooperation of the participants of this study and the staff at the two hospitals.
References
1. Wijma K. Why focus on ‘fear of childbirth'? J Psychosom Obstet Gynaecol. (2003) 24:141–3. doi: 10.3109/01674820309039667
2. Mortazavi F, Mehrabadi M. Predictors of fear of childbirth and normal vaginal birth among Iranian postpartum women: a cross-sectional study. BMC Pregnancy Childbirth. (2021) 21:316–29. doi: 10.1186/s12884-021-03790-w
3. Wahlbeck H, Kvist LJ, Landgren K. Art therapy and counseling for fear of childbirth: a randomized controlled trial. Art Therapy. (2020) 37:123–30. doi: 10.1080/07421656.2020.1721399
4. O'Connell MA, Leahy-Warren P, Khashan AS, Kenny LC, O'Neill SM. Worldwide prevalence of tocophobia in pregnant women: systematic review and meta-analysis. Acta Obstet Gynecol Scand. (2017) 96:907–20. doi: 10.1111/aogs.13138
5. Dencker A, Nilsson C, Begley C, Jangsten E, Mollberg M, Patel H, et al. Causes and outcomes in studies of fear of childbirth: a systematic review. Women Birth. (2019) 32:99–111. doi: 10.1016/j.wombi.2018.07.004
6. Sheen K, Slade P. Examining the content and moderators of women's fears for giving birth: A meta-synthesis. J Clin Nurs. (2018) 27:2523–35. doi: 10.1111/jocn.14219
7. Lara-Cinisomo S, Zhu K, Fei K, Bu Y, Weston AP, Ravat U. Traumatic events: exploring associations with maternal depression, infant bonding, and oxytocin in latina mothers. BMC Womens Health. (2018) 18:31–9. doi: 10.1186/s12905-018-0520-5
8. Lukasse M, Schroll AM, Karro H, Schei B, Steingrimsdottir T, Van Parys AS, et al. Prevalence of experienced abuse in healthcare and associated obstetric characteristics in six European countries. Acta Obstet Gynecol Scand. (2015) 94:508–17. doi: 10.1111/aogs.12593
9. Sitras V, ŠaltyteBenth J, Eberhard-Gran M. Obstetric and psychological characteristics of women choosing epidural analgesia during labour: a cohort study. PLoS ONE. (2017) 12:e0186564. doi: 10.1371/journal.pone.0186564
10. Gao LL, Liu XJ, Fu BL, Xie W. Predictors of childbirth fear among pregnant Chinese women: a cross-sectional questionnaire survey. Midwifery. (2015) 31:865–70. doi: 10.1016/j.midw.2015.05.003
11. Fairbrother N, Thordarson DS, Stoll K. Fine tuning fear of childbirth: the relationship between childbirth fear questionnaire subscales and demographic and reproductive variables. J Reprod Infant Psychol. (2018) 36:15–29. doi: 10.1080/02646838.2017.1396300
12. Zhou X, Liu H, Li X, Zhang S. Fear of childbirth and associated risk factors in healthy pregnant women in northwest of China: a cross-sectional study. Psychol Res Behav Manag. (2021) 14:731–41. doi: 10.2147/PRBM.S309889
13. Elisabet Rondung E, Ekdahl J, Sundin Ö. Potential mechanisms in fear of birth: The role of pain catastrophizing and intolerance of uncertainty. Birth. (2019) 46:61–8. doi: 10.1111/birt.12368
14. Saccone G, Florio A, Aiello F, Venturella R, De Angelis MC, Locci M, et al. Psychological impact of coronavirus disease 2019 in pregnant women. Am J Obstet Gynecol. (2020) 223:293–5. doi: 10.1016/j.ajog.2020.05.003
15. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
16. Firouzbakht M, Rahmani N, Sharif Nia H, Omidvar S. Coping strategies and depression during the COVID-19 pandemic in pregnant women: a cross sectional study. BMC Psychiatry. (2022) 22:153. doi: 10.1186/s12888-022-03792-8
17. Inozu M, Gök BG, Tuzun D, Haciomeroglu AB. Does cognitive flexibility change the nature of the relationship between intolerance of uncertainty and psychological symptoms during the COVID-19 outbreak in Turkey? Cur Psychol. (2022) 4:1–12. doi: 10.1007/s12144-021-02450-8
18. de Sousa AR, Teixeira JRB, Palma EMS, Moreira WC, Santos MB, de Carvalho HEF, et al. Psychological distress in men during the COVID-19 pandemic in Brazil: the role of the sociodemographic variables, uncertainty, and social support. Int J Environ Res Public Health. (2021) 19:350. doi: 10.3390/ijerph19010350
19. Zhao J, Ye B, Ma T. Positive information of COVID-19 and anxiety: a moderated mediation model of risk perception and intolerance of uncertainty. Front Psychiatry. (2021) 12:715929. doi: 10.3389/fpsyt.2021.715929
20. Solano P, Ustulin M, Pizzorno E, Vichi M, Pompili M, Serafini G, et al. A Google-based approach for monitoring suicide risk. Psychiatry Res. (2016) 246:581–6. doi: 10.1016/j.psychres.2016.10.030
21. Schaal NK, Hagenbeck C, Helbig M, Wulff V, Märthesheimer S, Fehm T, et al. The influence of being pregnant during the COVID-19 pandemic on birth expectations and antenatal bonding. J Reprod Infant Psychol. (2021) 18:1–11. doi: 10.1080/02646838.2021.1962825
22. Ilska M, Kołodziej-Zaleska A, Brandt-Salmeri A, Preis H, Lobel M. Pandemic-related pregnancy stress assessment-psychometric properties of the polish PREPS and its relationship with childbirth fear. Midwifery. (2021) 96:102940. doi: 10.1016/j.midw.2021.102940
23. Li Q, Luo R, Zhang X, Meng G, Dai B, Liu X. Intolerance of COVID-19-related uncertainty and negative emotions among Chinese adolescents: a moderated mediation model of risk perception, social exclusion and perceived efficacy. Int J Environ Res Public Health. (2021) 18:2864. doi: 10.3390/ijerph18062864
24. Aksoy Derya Y, Altiparmak S, AkÇa E, GÖkbulut N, Yilmaz AN. Pregnancy and birth planning during COVID-19: the effects of tele-education offered to pregnant women on prenatal distress and pregnancy-related anxiety. Midwifery. (2021) 92:102877. doi: 10.1016/j.midw.2020.102877
25. Baldessarini RJ, Innamorati M, Erbuto D, Serafini G, Fiorillo A, Amore M, et al. Differential associations of affective temperaments and diagnosis of major affective disorders with suicidal behavior. J Affect Disord. (2017) 210:19–21. doi: 10.1016/j.jad.2016.12.003
26. Dugas MJ, Gagnon F, Ladouceur R, Freeston MH. Generalized anxiety disorder: a preliminary test of a conceptual model. Behav Res Ther. (1998) 36:215–26. doi: 10.1016/S0005-7967(97)00070-3
27. Dugas MJ, Laugesen N, Bukowski WM. Intolerance of uncertainty, fear of anxiety, and adolescent worry. J Abnorm Child Psychol. (2012) 40:863–70. doi: 10.1007/s10802-012-9611-1
28. Carleton RN. Fear of the unknown: One fear to rule them all? J Anxiety Disord. (2016) 41:5–21. doi: 10.1016/j.janxdis.2016.03.011
29. Freeston MH, Rheaume J, Letarte H, Dugas MJ, Ladouceur R. Why do people worry. Pers Individ Differ. (1994) 17:791–802. doi: 10.1016/0191-8869(94)90048-5
30. Rondung E, Thomtén J, Sundin Ö. Psychological perspectives on fear of childbirth. J Anxiety Disord. (2016) 44:80–91. doi: 10.1016/j.janxdis.2016.10.007
31. McEvoy PM, Hyett MP, Shihata S, Price JE, Strachan L. The impact of methodological and measurement factors on transdiagnostic associations with intolerance of uncertainty: a meta-analysis. Clin Psychol Rev. (2019) 73:101778. doi: 10.1016/j.cpr.2019.101778
32. Osmanagaoglu N, Creswell C, Dodd HF. Intolerance of uncertainty, anxiety, and worry in children and adolescents: a meta-analysis. J Affective Disorders. (2018) 225:80–90. doi: 10.1016/j.jad.2017.07.035
33. Kendall PC, Norris LA, Rabner JC, Crane ME, Rifkin LS. Intolerance of uncertainty and parental accommodation: promising targets for personalized intervention for youth anxiety. Curr Psychiatry Rep. (2020) 22:49. doi: 10.1007/s11920-020-01170-3
34. Morriss J, Zuj DV, Mertens G. The role of intolerance of uncertainty in classical threat conditioning: recent developments and directions for future research. Int J Psychophysiol. (2021) 166:116–26. doi: 10.1016/j.ijpsycho.2021.05.011
35. Morriss J, Wake S, Elizabeth C, van Reekum CM. I doubt it is safe: a meta-analysis of self-reported intolerance of uncertainty and threat extinction training. Biol Psychiatry Glob Open Sci. (2021) 1:171–9. doi: 10.1016/j.bpsgos.2021.05.011
36. Tanovic E, Gee DG, Joormann J. Intolerance of uncertainty: neural and psychophysiological correlates of the perception of uncertainty as threatening. Clin Psychol Rev. (2018) 60:87–99. doi: 10.1016/j.cpr.2018.01.001
37. Freeston M, Tiplady A, Mawn L, Bottesi G, Thwaites S. Towards a model of uncertainty distress in the context of coronavirus (COVID-19). Cogn Behav Therap. (2020) 13:e31. doi: 10.1017/S1754470X2000029X
38. Saulnier KG, Koscinski B, Volarov M, Accorso C, Austin MJ, Suhr JA, et al. Anxiety sensitivity and intolerance of uncertainty are unique and interactive risk factors for COVID-19 safety behaviors and worries. Cogn Behav Therap. (2022) 51:217–28. doi: 10.1080/16506073.2021.1976819
39. Baerg L, Bruchmann K. COVID-19 information overload: intolerance of uncertainty moderates the relationship between frequency of internet searching and fear of COVID-19. Acta Psychol. (2022) 224:103534. doi: 10.1016/j.actpsy.2022.103534
40. Funkhouser CJ, Klemballa DM, Shankman SA. Using what we know about threat reactivity models to understand mental health during the COVID-19 pandemic. Behav Res Ther. (2022) 153:104082. doi: 10.1016/j.brat.2022.104082
41. Richard S, Lazarus Folkman S. Stress, Appraisal, and Coping. New York, NY: Springer Publishing Company (1984). p. 456–60.
42. Badaoui A, Kassm SA, Naja W. Fear and anxiety disorders related to childbirth: epidemiological and therapeutic issues. Curr Psychiatry Rep. (2019) 21:27–40. doi: 10.1007/s11920-019-1010-7
43. Okumus F, Sahin N. Fear of childbirth in urban and rural regions of Turkey: Comparison of two resident populations. North Clin Istanb. (2017) 4:247–56. doi: 10.14744/nci.2017.46693
44. Huang J, Huang J, Li Y, Liao B. The prevalence and predictors of fear of childbirth among pregnant Chinese women: a hierarchical regression analysis. BMC Pregnancy Childbirth. (2021) 21:643. doi: 10.1186/s12884-021-04123-7
45. Wei J, Liu JY, Zhang LF, Wu YP, Fu CF. Reliability and validity of the Chinese version of childbirth attitudes questionnaire. J Nurs Sci. (2016) 31:81–3. doi: 10.3870/j.issn.1001-4152.2016.02.081
46. Areskog B, Kjessler B, Uddenberg N. Identification of women with significant fear of childbirth during late pregnancy. Gynecol Obstet Invest. (1982) 13:98–107. doi: 10.1159/000299490
47. Lowe NK. Self-efficacy for labor and childbirth fears in nulliparous pregnant women. J Psychosom Obstet Gynaecol. (2000) 21:219–24. doi: 10.3109/01674820009085591
48. Tanglakmankhong K, Perrin NA, Lowe NK. Childbirth self-efficacy inventory and childbirth attitudes questionnaire: psychometric properties of Thai language versions. J Adv Nurs. (2011) 67:193–203. doi: 10.1111/j.1365-2648.2010.05479.x
49. Carleton RN, Norton MA, Asmundson GJ. Fearing the unknown: a short version of the Intolerance of Uncertainty Scale. J Anxiety Disord. (2007) 21:105–17. doi: 10.1016/j.janxdis.2006.03.014
50. Wu LJ, Wang JN, Qi XD. Validity and reliability of the intolerance of uncertainty scale-12 in middle school students. Chin Ment Health J. (2016) 30:700–5. doi: 10.3969/j.issn.1000-6729.2016.09.012
51. Xie Y. Preliminary study on the reliability and validity of the simplified coping style questionnaire. Chin J Clin Psychol. (1998) 6:114–5. doi: 10.16128/j.cnki.1005-3611.1998.02.018
52. Challacombe FL, Nath S, Trevillion K, Pawlby S, Howard LM. Fear of childbirth during pregnancy: associations with observed mother-infant interactions and perceived bonding. Arch Womens Ment Health. (2021) 24:483–92. doi: 10.1007/s00737-020-01098-w
53. Deng Y, Lin Y, Yang L, Liang Q, Fu B, Li H, et al. A comparison of maternal fear of childbirth, labor pain intensity and intrapartum analgesic consumption between primiparas and multiparas: a cross-sectional study. Int J Nurs Sci. (2021) 8:380–7. doi: 10.1016/j.ijnss.2021.09.003
54. Molgora S, Fenaroli V, Prino LE, Rollè L, Sechi C, Trovato A, et al. Fear of childbirth in primiparous Italian pregnant women: the role of anxiety, depression, and couple adjustment. Women Birth. (2018) 31:117–23. doi: 10.1016/j.wombi.2017.06.022
55. World Health Organization. COVID-19 Outbreak a Pandemic. (2020). Available online at: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-c ovid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (accessed March 28, 2022).
56. do Souto SPA, Prata AP, de Albuquerque RS, Almeida S. Prevalence and predictive factors for fear of childbirth in pregnant Portuguese women: a cross-sectional study. Sex Reprod Healthc. (2021) 31:100687. doi: 10.1016/j.srhc.2021.100687
57. Zengin H, Bafali IO, Caka SY, Tiryaki O, Cinar N. Childbirth and postpartum period fear and the related factors in pregnancy. J Coll Physicians Surg Pak. (2020) 30:144–8. doi: 10.29271/jcpsp.2020.02.144
58. Räisänen S, Lehto SM, Nielsen HS, Gissler M, Kramer MR, Heinonen S. Fear of childbirth in nulliparous and multiparous women: a population-based analysis of all singleton births in Finland in 1997-2010. B J O G. (2014) 121:965–70. doi: 10.1111/1471-0528.12599
59. Ilska M, Brandt-Salmeri A, Kołodziej-Zaleska A, Banaś E, Gelner H, Cnota W. Factors associated with fear of childbirth among polish pregnant women. Sci Rep. (2021) 11:4397. doi: 10.1038/s41598-021-83915-5
60. Phunyammalee M, Buayaem T, Boriboonhirunsarn D. Fear of childbirth and associated factors among low-risk pregnant women. J Obstet Gynaecol. (2019) 39:763–7. doi: 10.1080/01443615.2019.1584885
61. Naanyu V, Wade TJ, Ngetich A, Mulama K, Nyaga L, Pell R, et al. A qualitative exploration of barriers to health-facility-based delivery in Bomachoge-Borabu and Kaloleni, Kenya. Int J Gynaecol Obstet. (2021) 153:273–9. doi: 10.1002/ijgo.13450
62. Çitak Bilgin N, Coşkun H, CoşkunerPotur D, IbarAydin E, Uca E. Psychosocial predictors of the fear of childbirth in Turkish pregnant women. J Psychosom Obstet Gynaecol. (2021) 42:123–31. doi: 10.1080/0167482X.2020.1734791
63. Werchan DM, Hendrix CL, Ablow JC, Amstadter AB, Austin AC, Babineau V, et al. Behavioral coping phenotypes and associatedpsychosocial outcomes of pregnant and postpartum women during the COVID-19 pandemic. Sci Rep. (2022) 12:1209. doi: 10.1038/s41598-022-05299-4
64. Daglar G, Bilgic D, Cakir D. The correlation between levels of prenatal attachment and styles coping with stress in pregnant women. J Reprod Infant Psychol. (2021) 1–12. doi: 10.1080/02646838.2021.2001795
65. McDonald AJ, Wickens CM. Bondy SJ, Elton-Marshall T, Wells S, Nigatu YT, et al. Age differences in the association between loneliness and anxiety symptoms during the COVID-19 pandemic. Psychiatry Res. (2022) 310:114446. doi: 10.1016/j.psychres.2022.114446
66. O'Connell MA, Khashan AS, Leahy-Warren P, Stewart F, O'Neill SM. Interventions for fear of childbirth including tocophobia. Cochrane Database Syst Rev. (2021) 7:Cd013321. doi: 10.1002/14651858.CD013321.pub2
67. Boz I, Akgün M, Duman F. A feasibility study of a psychoeducation intervention based on human caring theory in nulliparous women with fear of childbirth. J Psychosom Obstet Gynaecol. (2020) 22:1–13. doi: 10.1080/0167482X.2020.1752173
68. Duncan LG, Cohn MA, Chao MT, Cook JG, Riccobono J, Bardacke N. Benefits of preparing for childbirth with mindfulness training: a randomized controlled trial with active comparison. BMC Pregnancy Childbirth. (2017) 17:140–50. doi: 10.1186/s12884-017-1319-3
69. Klabbers GA, Wijma K, Paarlberg KM, EmonsWH, Vingerhoets AJ. Treatment of severe fear of childbirth with haptotherapy: design of a multicenter randomized controlled trial. BMC Complement Altern Med. (2014) 14:385–94. doi: 10.1186/1472-6882-14-385
70. Rondung E, Ternström E, Hildingsson I, Haines HM, Sundin Ö, Ekdahl J, et al. Comparing internet-based cognitive behavioral therapy with standard care for women with fear of birth: randomized controlled trial. JMIR Mental Health. (2018) 5:1–16. doi: 10.2196/10420
Keywords: childbirth fear, intolerance of uncertainty, coping styles, COVID-19, pregnant women
Citation: Han L, Bai H, Lun B, Li Y, Wang Y and Ni Q (2022) The Prevalence of Fear of Childbirth and Its Association With Intolerance of Uncertainty and Coping Styles Among Pregnant Chinese Women During the COVID-19 Pandemic. Front. Psychiatry 13:935760. doi: 10.3389/fpsyt.2022.935760
Received: 04 May 2022; Accepted: 27 May 2022;
Published: 27 June 2022.
Edited by:
Sara Molgora, Catholic University of the Sacred Heart, ItalyReviewed by:
Gianluca Serafini, San Martino Hospital (IRCCS), ItalyJayne Morriss, University of Reading, United Kingdom
Copyright © 2022 Han, Bai, Lun, Li, Wang and Ni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hua Bai, sfyhlb3726@zzu.edu.cn
 Lingli Han
Lingli Han Hua Bai
Hua Bai