- 1Department of Psychiatry, The First Hospital of Hebei Medical University, Shijiazhuang, China
- 2Mental Health Institute of the Hebei Medical University, Shijiazhuang, China
- 3Department of Neurology, The First Hospital of Hebei Medical University, Shijiazhuang, China
Objective: To evaluate the correlation between clinical symptoms and cognitive impairment in elderly patients with depressive disorder.
Methods: In this retrospective study, a total of 123 elderly patients with depressive disorder admitted to our hospital from January 2020 to February 2021 were included. Patients' cognitive function was assessed by the Montreal Cognitive Assessment Scale (MoCA). According to the combination of cognitive impairment or not, patients were divided into the combined group (64 cases) and the depressive disorder group (59 cases). In addition, 70 healthy people who came to our hospital for physical examination during the same period were randomly selected as the healthy group.
Results: The incidence of severe cognitive impairment in the combined group (33, 51.56%) was significantly higher than that in the depression group (19, 32.20%), the difference was statistically significant (P = 0.003). The incidence of somatization symptoms, suicidal tendency, retardation of thinking, diminution of energy, anxiety and sleep disorder in the combined group were higher than that in the depressive disorder group with significant difference [30 (56.88%) vs. 16 (27.12%), P = 0.024; 12 (18.75%) vs. 3 (5.08%), P = 0.021; 33 (51.56%) vs. 14 (23.73%), P = 0.002; 37 (57.81%) vs. 23 (38.98%), P = 0.029; 42 (65.63) vs. 25 (42.37), P = 0.011; 50 (78.13) vs. 42 (71.19), P = 0.031, respectively]. Spearman rank correlation analysis suggested that somatic symptom, mood change, suicidal tendency, retardation of thinking, diminution of energy, anxiety, and sleep disorder were negatively correlated with cognitive impairment, respectively (r =-0.161, −0.672, −0.262, −0.871, −0.421, −0.571, −0.512, P < 0.001).
Conclusion: The clinical symptoms of depressive disorder were negatively correlated with cognitive impairment. Somatic symptoms, suicidal tendency, retardation of thinking, diminution of energy, anxiety, and sleep disorder were the risk factors for cognitive impairment.
Introduction
It was reported that China's aging population was about 18.1 percent at the end of 2019 and is expected to reach 28 percent by 2040 (1). With the increase of the elderly population, the psychological state of elderly patients has gradually received more attention (2). Geriatric depressive disorder refers to a mental disorder occurring after the age of 60 with persistent depressive mood as the main clinical phase, with a high incidence of 3.5–7.5% (3). The main characteristics of geriatric depressive disorder are high disability rate, high recurrence rate, and high suicide rate. It was reported that the disability rate was about 18%, the recurrence rate was about 80%, and the suicide rate was about 10–15%, as a result, geriatric depression disorder not only has a serious impact on the quality of life of patients but also increases the burden on patients and society (4). Previous studies have suggested that the incidence of depressive disorder accompanied by cognitive dysfunction is as high as 50–75%, if depressive disorder accompanied by cognitive dysfunction is temporary, it can be recovered with the relief of depressive mood, so it is also called pseudodementia (5).
The geriatric depressive disorder has a high prevalence, but low consultation rate, when developed into severe cognitive impairment, seriously affects the quality of life of the elderly and their spouses. The report suggested that more than 80 percent of older adults with depression in the United States seek care in primary care settings, often undiagnosed at the time of the visit (6). Therefore, it is of great clinical significance to timely distinguish elderly patients with depressive disorder and determine whether there is cognitive impairment for timely and effective symptomatic treatment and to avoid exacerbation of the condition (7). At present, there are few clinical studies on the clinical characteristics of elderly patients with depression disorder complicated with cognitive impairment. Based on this, this study aimed to evaluate the correlation between clinical symptoms and cognitive impairment and to explore the risk factors of cognitive impairment in elderly patients with depressive disorder.
Materials and methods
Study patients
This study retrospectively included 123 elderly patients with the depressive disorder who were admitted to our hospital from January 2020 to February 2021. The Montreal Cognitive Assessment Scale (MoCA) (8) was used to assess whether the patients with combined cognitive impairment were divided into the combined group, and the patients with single depressive disorder were divided into the depressive disorder group. Another seventy healthy people who were randomly selected to our hospital for physical examination at the same time were set as the healthy group for comparison.
Inclusion criteria
(1) The diagnosis of depressive disorder was in line with the diagnostic criteria for depression in the International Classification of Diseases (ICD-10) (9), the diagnosis was made by two psychiatrists with intermediate or higher professional titles; (2) Patients whose Geriatric Depression Scale (4) (GDS) score was ≥11; (3) No drugs such as escitalopram were used before admission; (4) Informed consent was signed by patients and their families.
Exclusion criteria
(1) Patients complicated with serious physical diseases, brain organic diseases, alcohol or drug dependence; (2) Patients complicated with mental retardation, Alzheimer's diseases, secondary depression, and bipolar disorder; (3) Patients complicated with heart, lung, kidney, and other organ diseases; (4) Depression caused by non-dependent substances; (5) Patients with systemic diseases and complications; (6) Patients with a history of alcohol or drug abuse or dependence within the past 2 years.
The study was approved by the Ethical Committee, and the informed consent forms were obtained from all patients.
General information collection
Age, sex, marital status, education level, family history of depression, and causes of depression were collected for all subjects. Clinical symptoms of depressive disorder were collected, including somatic symptoms, mood change, suicidal tendency, retardation of thinking, diminution of energy, anxiety, and sleep disorder. Medication history and chronic disease history were collected. Chronic diseases to be screened included chronic bronchitis, chronic obstructive pulmonary disease, emphysema, cholelithiasis, cataract, chronic renal insufficiency, prostate disease, musculoskeletal disease, cerebrovascular disease, diabetes, and hyperlipidemia.
Evaluation of depressive disorder
The severity of patients' depressive disorder was assessed by the GDS scale (4). The scale includes 30 subitems such as depressed mood, reduced activity, and irritability. Each item is given a score of 1 and the full score is 30. Depression is rated on three scales: 0–10 for normal, 11–20 for mild depression, and 21–30 for moderate to severe depression.
Assessment of cognitive impairment
Cognitive impairment was assessed by the MoCA (8). The scale consists of 11 items with a total score of 30 points. A score <25 is classified as cognitive dysfunction; A score of ≥26 is considered normal. The patients were evaluated by 2 doctors by talking and observing, and each event was assessed for about 20 min. The physician didn't know the patient's disease information when evaluating the patient.
Statistical analysis
Statistical analysis was performed using the SPSS software program (version 21.0; IBM Corp, Chicago, IL, USA). Normally distributed measurement data were expressed as mean ± standard deviation (SD). One-way ANOVA was used for comparison of measurement data between groups, and post-doc least significant difference (LSD) was used for comparison of data between and within groups. The enumeration data were expressed in frequency and percentage and were compared with the Chi-square test. Spearman rank correlation was used to analyze the relationship between clinical symptoms and cognitive impairment in patients with depressive disorder. Logistic regression was used to analyze the influencing factors of cognitive function in patients with depressive disorder. The test level α was 0.05 on both sides. P < 0.05 was considered statistically significant.
Results
General data
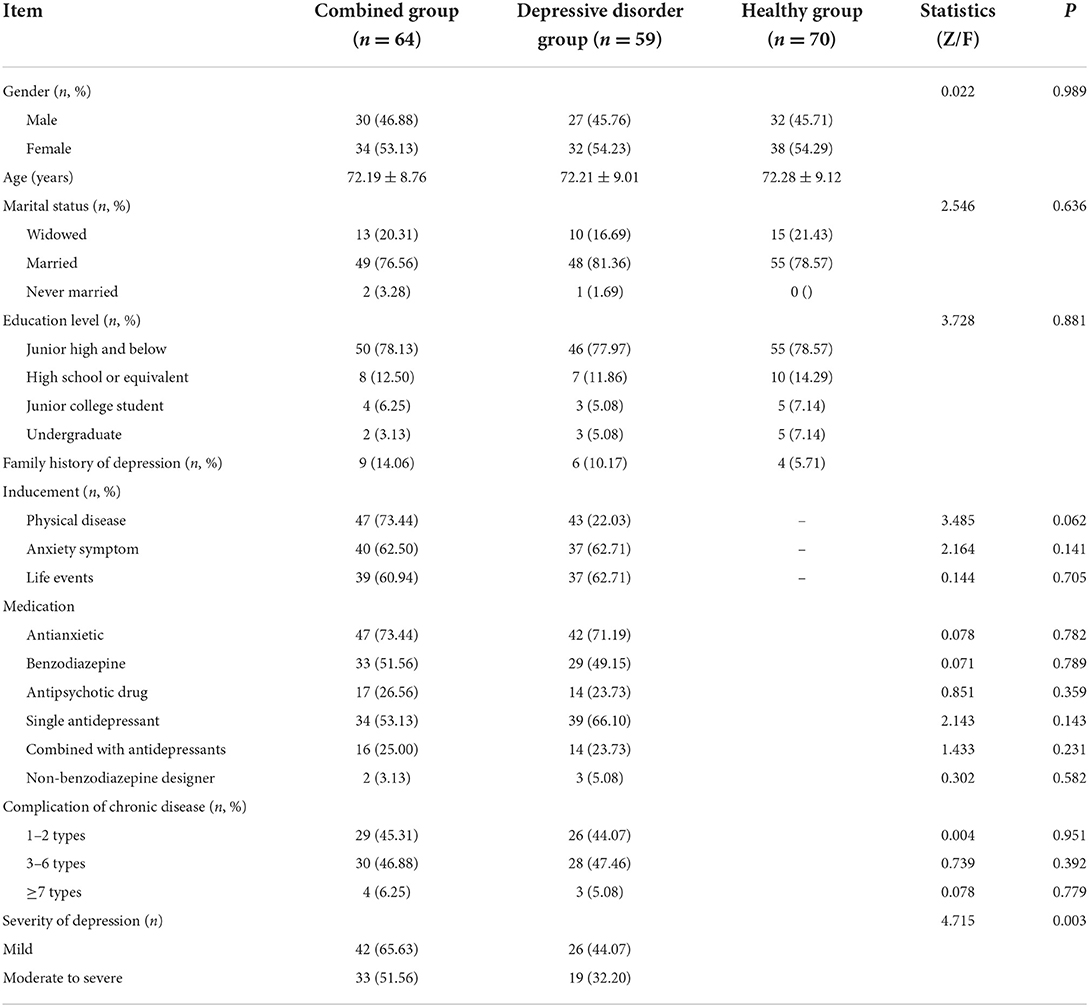
A total of 123 elderly patients, including 64 patients in the comorbid group and 59 patients in the depressive disorder group, and 70 healthy controls, were retrospectively included in this study (Figure 1). The incidence of depressive disorder combined with cognitive impairment was 52.03% (64/123). There were no significant differences in gender, age, marital status, education background, and smoking among the three groups (P > 0.05). The incidence of moderate to severe cognitive impairment in the combined group was significantly higher than that in the depressive group (P = 0.003; Table 1).
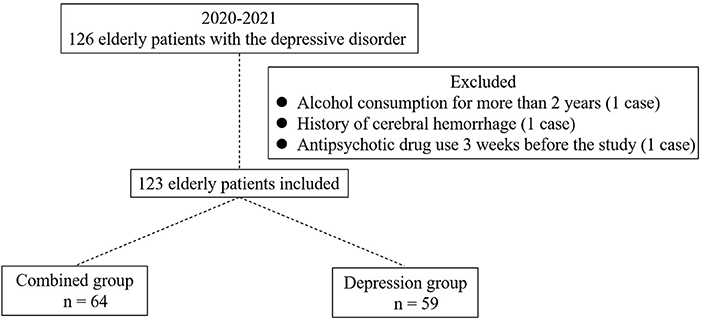
Figure 1. Enrollment of elderly patients with depressive disorder. A total of 126 elderly patients with depressive disorder were primarily enrolled. One case was excluded for alcohol consumption for more than 2 years, one case was excluded for history of cerebral hemorrhage, and one case was excluded for antipsychotic drug use 3 weeks before the study. A total of 123 patients were finally included, among which 64 patients were divided into the combined group, and the others were divided into the depression group.
Comparison of clinical symptoms of depression between the combined group and the depressive disorder group
The incidence of somatic symptoms, suicidal tendency, retardation of thinking, diminution of energy, anxiety, and sleep disorder in the combined group was significantly higher than that in the depressive disorder group, and the difference was statistically significant (P < 0.05; Table 2).
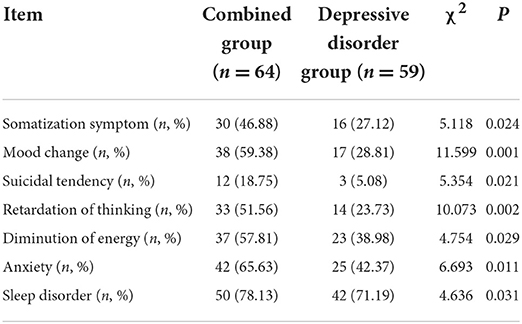
Table 2. Comparison of clinical symptoms between the combined group and the depressive disorder group.
Clinical symptoms of depression and its relationship with cognitive impairment in patients with depressive disorder
Spearman rank correlation analysis suggested that somatic symptom, mood change, suicidal tendency, retardation of thinking, diminution of energy, anxiety, and sleep disorder were negatively correlated with cognitive impairment, respectively (r = −0.161, −0.672, −0.262, −0.871, −0.421, −0.571, −0.512, P < 0.001).
Logistic regression was used to evaluate the influencing factors of cognitive function in patients with depressive disorder
Logistic regression analysis indicated that the influencing factors of cognitive dysfunction in patients with depressive disorder were somatic symptom [odds ratio (OR) = 0.532, 95% confidence interval (CI): 0.298–0.893, P = 0.013], suicidal ideation (OR = 0.927, 95% CI: 0.701–1.212, P < 0.001), retardation of thinking (OR = 2.217, 95% CI: 0.053–0.786, P < 0.001), diminution of energy (OR = 0.111, 95% CI: 0.041–0.231, P < 0.001), anxiety (OR = 0.072, 95% CI: 0.029–0.254, P < 0.001), and sleep disorder (OR = 0.871, 95% CI: 0.783–0.973, P = 0.014; Table 3).
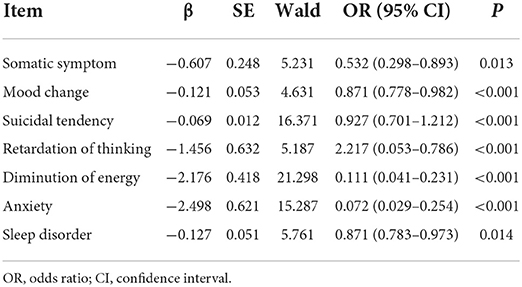
Table 3. Logistic regression analysis of influencing factors of cognitive function in patients with depressive disorder.
Discussion
Depressive disorder is a chronic mental disease, with significant and persistent low mood as the main clinical symptoms. It was reported that the incidence of depressive disorder in China was increasing year by year (10). In elderly patients, depressive disorder is not only accompanied by physical symptoms but also interwoven with depressive mood. This state has a huge negative impact on patients' physical and mental health and quality of life (10). Cognitive function is the function of the brain to perform higher-level activities including thinking, imagination, memory, and executive functions (11). Cognitive impairment could affect patients' quality of life in the long term. Elderly patients with depression disorder with cognitive dysfunction, visual-spatial ability, executive function, information processing speed, episodic memory, and other disorders. Therefore, the treatment goal of elderly depressive disorder not only includes the improvement of their depression symptoms, improves cognitive function, and then restores the patient's social function (11). Studies have pointed out that it is of great significance to analyze the relationship between clinical symptoms and cognitive impairment in elderly patients with the depressive disorder for early diagnosis and timely treatment intervention (12).
Depression disorder combined with cognitive dysfunction has a high incidence in the elderly population. Depression is associated with increased risk for cognitive function (13). Bellou et al. (14) reported that up to 60% of patients with the depressive disorder also met the diagnosis of cognitive dysfunction. In this study, the incidence of depressive disorder with cognitive impairment was 52.03% (64/123), indicating a high incidence of depressive disorder with cognitive impairment. The incidence of somatic diseases in the elderly is significantly higher than that in the young and middle-aged, which may be due to the increase in age, the incidence of somatic disease-induced depression also increases (15). Studies (16) have shown that the cognitive impairment of patients with the depressive disorder was mainly related to the impairment of the frontal-parietal lobe cognitive control network. Of these, executive function, memory, and attention were reported to be the most commonly affected areas. Previous research reported that cognitive impairment was a secondary symptom caused by depression, mental retardation, and other depressive disorders (17, 18). The study of Liu et al. (19) suggested that attention and delayed recall were negatively correlated with clinical symptoms in elderly patients with amnestic mild cognitive impairment. This current study also suggested that the clinical symptoms of patients with the depressive disorder were negatively correlated with cognitive impairment, suggesting that the more severe the depression disorder was in the elderly, the worse the cognitive function would be.
Cognitive dysfunction in patients with depressive disorder is affected by many factors. Studies have shown that sleep factors play an important role in the formation and development of cognitive impairment (20). Lack of sleep time is easy to leads to words can only appear as directional power disorder, if it is easy to wake up at night, nightmares and other sleep disturbances, will affect the patient's memory, language expression ability. Aging is associated with changes in sleep structure, decreased sleep efficiency, and increased risk of cognitive impairment. Anxiety is a common symptom in people with depressive disorders. Fang (21) reported that the somatic symptoms of elderly patients with a depressive disorder are mainly anxiety and suicidal consciousness. Brain imaging studies indicated that anxiety symptoms in patients with depressive disorders were associated with abnormal activity of local neurons in brain regions (22). Liu et al. (23) found that depression and anxiety were independent risk factors for cognitive dysfunction. The results of this study suggested that the influencing factors of cognitive function in patients with depressive disorder were somatization symptoms, suicidal ideation, thought retardation, energy loss, anxiety, and sleep disorder. At the same time, cognitive dysfunction had an impact on depressive disorders. Peng et al. (24) pointed out that cognitive dysfunction can aggravate a depressive mood. Li et al. (25) pointed out that cognitive function has an impact on suicidal ideation in depressed patients. According to clinical experience, the author thinks that depression disorder combined with cognitive dysfunction can be prevented from the following aspects: (1) Actively adopting symptomatic drug treatment and timely adjusting medication regimen according to the specific situation of patients to reduce the impact of depression on sleep disorders and cognitive impairment; (2) Strengthen health education. Combined with the education level of patients, the health knowledge education was strengthened in the form of pictures and interesting videos, and the influencing factors of depression disorder, sleep disorder, and cognitive impairment were informed to patients as well as daily self-management methods; (3) We should pay more attention to the elderly and education, comprehensively evaluate the individual's actual situation, and adopt memory games to ensure the continuous progress of cognitive impairment; (4) Targeted psychological intervention, guide patients to take a walk, listen to music, do manual work, embroidery and other ways to divert attention, relieve their depression, reduce the severity of the primary symptoms; (5) Patients should be informed to make a sleep schedule based on their actual situation, take regular rest in strict accordance with the schedule, reduce the noise of the sleep environment, and keep the sleep environment quiet. During the day or 30 min before falling asleep at night, they can properly take a walk, do exercises, and other sports to keep the balance of rest and movement.
This study also had the following limitations: The first is the limited sample size of the study Secondly, the cases included in this study were from a single-center, so there may be some bias in the selection of patients. Thirdly, the follow-up period is relatively short. Therefore, a more scientific sample size and more comprehensive design are still needed to improve the quality of research results.
Conclusion
The clinical symptoms of depressive disorder were negatively correlated with cognitive impairment. Somatic symptoms, suicidal tendency, retardation of thinking, diminution of energy, anxiety, and sleep disorder were the risk factors for cognitive impairment.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by the First Hospital of Hebei Medical University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
ZW and BX contributed to the conception and design of the study. GS and WL performed the experiments, collected, and analyzed data. LL, ZZ, ZW, and BX wrote the manuscript. GS, ZW, and BX revised the manuscript. All authors reviewed and approved the final version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
GDS, Geriatric Depression Scale; ICD-10, International Classification of Diseases; LSD, least significant difference; MoCA, Montreal Cognitive Assessment Scale; SD, standard deviation.
References
1. Wang XB, Li M, Yang ZZ. The clinical efficacy of repetitive rTMS combined with duloxetine in elderly patients with depressive disorder accompanied by somatic symptoms. J Hebei Med J. (2022) 44:578–80. doi: 10.3969/j.issn.1002-7386.2022.04.025
2. Forbes MP, O'Neil A, Lane M, Agustini B, Myles N, Berk M. Major depressive disorder in older patients as an inflammatory disorder: implications for the pharmacological management of geriatric depression. Drugs Aging. (2021) 38:451–67. doi: 10.1007/s40266-021-00858-2
3. Shoib S, Islam SMS, Arafat SY, Hakak SA. Depression and suicidal ideation among the geriatric population of Kashmir, India. Int J Soc Psychiatry. (2021) 67:651–5. doi: 10.1177/0020764020968592
4. Shin C, Park MH, Lee SH, Ko YH, Kim YK, Han KM, et al. Usefulness of the 15-item geriatric depression scale (GDS-15) for classifying minor and major depressive disorders among community-dwelling elders. J Affect Disord. (2019) 259:370–5. doi: 10.1016/j.jad.2019.08.053
5. Chakrabarty T, McInerney SJ, Torres IJ, Frey BN, Milev RV, Müller DJ, et al. Cognitive outcomes with sequential escitalopram monotherapy and adjunctive aripiprazole treatment in major depressive disorder: a Canadian biomarker integration network in depression (CAN-BIND-1) report. CNS Drugs. (2021) 35:291–304. doi: 10.1007/s40263-021-00793-1
6. Taylor WD. Clinical practice. Depression in the elderly. N Engl J Med. (2014) 371:1228–36. doi: 10.1056/NEJMcp1402180
7. Zainal NZ, Kalita P, Herr KJ. Cognitive dysfunction in Malaysian patients with major depressive disorder: a subgroup analysis of a multicountry, cross-sectional study. Asia Pac Psychiatry. (2019) 11:e12346. doi: 10.1111/appy.12346
8. Yang Q, Diwu YC, Wang W. A preliminary study of the montreal cognitive assessment scale for the screening of mild cognitive impairment in the community. J Apoplexy Nervous Dis. (2022) 39:139–42. doi: 10.19845/j.cnki.zfysjjbzz.2021.0033
9. Implementation Implementation of the international statistical classification of diseases and related health problems, tenth revision (ICD-10). Epidemiol Bull. (1997) 18:1–4.
10. Liu MC, Pan WG, Mao PX, Ma X. Magnetic resonance imaging markers of senile depression. Chin J Geriatr. (2021) 40:1498–503. doi: 10.3760/cma.j.issn.0254-9026.2021.12.005
11. Huang LP, Li B, Zuo XW, Jiang LF, Gao HY, Li HL. Changes of serum Hcy, BDNF and NRG-1 and their relationship with cognitive impairment in elderly patients with depression. J Neurosci Ment Health. (2020) 20:419–24. doi: 10.3969/j.issn.1009-6574.2020.06.009
12. Rajtar-Zembaty A, Sałakowski A, Rajtar-Zembaty J, Starowicz-Filip A. Executive dysfunction in late-life depression. Psychiatr Pol. (2017) 51:705–18. doi: 10.12740/PP/OnlineFirst/63765
13. Pitts BL, Wen V, Whealin JM, Fogle BM, Southwick SM, Esterlis I, et al. Depression and cognitive dysfunction in older U.S. military veterans: moderating effects of BDNF Val66Met polymorphism and physical exercise. Am J Geriatr Psychiatry. (2020) 28:959–67. doi: 10.1016/j.jagp.2020.02.001
14. Bellou V, Belbasis L, Tzoulaki I, Middleton LT, Ioannidis JP, Evangelou E. Systematic evaluation of the associations between environmental risk factors and dementia: an umbrella review of systematic reviews and meta-analyses. Alzheimers Dement. (2017) 13:406–18. doi: 10.1016/j.jalz.2016.07.152
15. Li YC, Gao J, Wu CX, Tang N, Yi X, Yang J. Effect of group reminiscence therapy for depression in the elderly: a systematic review. Chin J Geriatr. (2015) 34:1021–5. doi: 10.3760/cma.j.issn.0254-9026.2015.09.026
16. Hao WS, Wei M, Liu JH, Song PH, Wang J, Wang YP. New advances in cognitive impairment associated with depressive disorder and its evaluation. China Med Herald. (2021) 18:40–4.
17. Zou CJ, Zhang YZ, Liu ZW, Tao CL. Study on extent and correlated influencing factors of cognitive function injury of depressed elderly patients. Chin J Hosp Stat. (2017) 24:34–6. doi: 10.3969/j.issn.1006-5253.2017.01.010
18. Melloni EMT, Poletti S, Vai B, Bollettini I, Colombo C, Benedetti F. Effects of illness duration on cognitive performances in bipolar depression are mediated by white matter microstructure. J Affect Disord. (2019) 249:175–82. doi: 10.1016/j.jad.2019.02.015
19. Liu Y, Huang XB, Chen WQ, Wang NQ, Chen YJ. Relationship of cognitive function and depression in elderly patients with amnestic mild cognitive impairment. China Med Herald. (2018) 15:66–70.
20. Zhou WQ, Wang YQ, Cao J, Zeng WX, Zhai SZ, Li Q. Characteristics and influencing factors of cognitive impairment in first-episode depression patients with sleep disturbance. Contemp Med. (2021) 27:178–80. doi: 10.3969/j.issn.1009-4393.2021.32.071
21. Fang LJ. Status analysis on clinical features and drug treatment of the geriatric depression. Chin J Geriatr. (2018) 37:1143–5. doi: 10.3760/cma.j.issn.0254-9026.2018.10.020
22. Xin LM, Chen L, Ji ZP, Zhang S, Wang J, Liu Y, et al. Risk factors of suicidality in major depressive disorder patients with and without anxious characteristics. Chin Ment Health J. (2015) 11:812–6. doi: 10.3969/j.issn.1000-6729.2015.11.003
23. Liu RP, Li YH, Zhang YY, Wu SH, Li YC, Ma WL. Comparison of neuropsychiatric symptoms in patients with different degrees of cognitive impairment. J Tongji Univer. (2022) 43:113–9. doi: 10.12289/j.issn.1008-0392.21392
24. Peng D, Li W, Zhou DM, Song YJ. The correlation of anxiety, depression and cognitive impairment in type 2 diabetic patients with acute multiple cerebral infarction. Chin J Gerontol. (2016) 36:3711–2. doi: 10.3969/j.issn.1005-9202.2016.15.047
Keywords: geriatric depression disorder, cognitive impairment, correlation analysis, risk factors, cognitive
Citation: Wu Z, Su G, Lu W, Liu L, Zhou Z and Xie B (2022) Clinical symptoms and their relationship with cognitive impairment in elderly patients with depressive disorder. Front. Psychiatry 13:1009653. doi: 10.3389/fpsyt.2022.1009653
Received: 02 August 2022; Accepted: 22 September 2022;
Published: 10 October 2022.
Edited by:
Çiçek Hocaoǧlu, Recep Tayyip Erdogan University, TurkeyReviewed by:
Bo Jin, The First Affiliated Hospital of China Medical University, ChinaShuang Li, Capital Medical University, China
Copyright © 2022 Wu, Su, Lu, Liu, Zhou and Xie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bingchuan Xie, xbc150908@gmail.com
†These authors have contributed equally to this work
 Zhenguo Wu1,2†
Zhenguo Wu1,2† Bingchuan Xie
Bingchuan Xie