- 1Department of Special Education, Faculty of Education, University of Haifa, Haifa, Israel
- 2The Edmond J. Safra Brain Research Center for the Study of Learning Disabilities, University of Haifa, Haifa, Israel
Depression is a serious psychiatric illness that negatively affects people’s feelings, thoughts, and actions. Providing emotion regulation support to others, also termed Extrinsic Emotion Regulation (EER), reduces depressive symptoms such as perseverative thinking and negative mood. In this conceptual review paper, we argue that EER may be especially beneficial for individuals with depression because it enhances the cognitive and affective processes known to be impaired in depression. Behavioral studies have shown that EER recruits processes related to cognitive empathy, intrinsic emotion regulation (IER), and reward, all impaired in depression. Neuroimaging data support these findings by showing that EER recruits brain regions related to these three processes, such as the ventrolateral prefrontal cortex which is associated with IER, the ventral striatum, which is associated with reward-related processes, and medial frontal regions related to cognitive empathy. This conceptual review paper sheds light on the mechanisms underlying the effectiveness of EER for individuals with depression and therefore offers novel avenues for treatment.
1. Introduction
Major Depressive Disorder (MDD) is a highly prevalent and often chronic disorder affecting more than 264 million people worldwide (Santomauro et al., 2021). Depression is therefore considered one of the most pressing health issues of our time (Fried et al., 2022). The increasing rates of depression impose substantial personal and societal costs. Unfortunately, there has been no significant change in the effectiveness of treatment for depression in the last few decades (Khan and Brown, 2015). Approximately half the patients remain depressed after undergoing psychological or pharmacological treatment (Khan and Brown, 2015; Cuijpers et al., 2018). Current treatments reduce the disease burden by only one-third (van Zoonen et al., 2014). In spite of considerable efforts and investment into understanding the biological underpinnings of depression, the mechanisms underlying it remain largely opaque (Kapur et al., 2012; Rogers, 2017). Identifying risk factors and the underlying mechanisms behind depression may assist in the development of effective prevention and treatment approaches (Joormann and Stanton, 2016).
A new approach suggests that individuals with depression can benefit from providing emotion regulation support to others, a process termed interpersonal emotion regulation (Zaki and Craig Williams, 2013) or extrinsic emotion regulation (EER; Nozaki and Mikolajczak, 2020). Based on a comprehensive literature review, we present evidence that EER may be especially helpful for individuals with depression as it enhances three main processes found impaired in depression: cognitive empathy, intrinsic emotion regulation, and reward (for reviews, see Singh and Gotlib, 2014; Cohen and Arbel, 2020).
1.1. Extrinsic emotion regulation
Emotion regulation (ER) is the set of processes responsible for monitoring, evaluating, and modifying emotional reactions in order to accomplish one’s goals (Gross and Thompson, 2007). It has recently been proposed that emotional health does not depend on the use of specific emotion regulation strategies but rather on the fit between the strategy used and the situation at hand (Cheng, 2001; Kashdan and Rottenberg, 2010; Bonanno and Burton, 2013; Cheng et al., 2014; Aldao et al., 2015). While most emotion regulation research has focused on intrinsic (or intrapersonal) emotion regulation, in which a person regulates their own emotions, recent studies have started to explore processes related to emotion regulation provided to others during social interactions. This social emotion regulation process, named Extrinsic Emotion Regulation (EER), is defined as “an action performed with the goal of influencing another person’s emotion trajectory; it can aim to decrease or increase either negative emotion or positive emotion.” (Nozaki and Mikolajczak, 2020).
EER has been largely studied as a way of reducing negative emotions and increasing positive ones (pro-hedonic motives; Zaki and Craig Williams, 2013). Nevertheless, a provider could also increase the negative emotions of the recipient or decrease the positive ones (contra-hedonic motives; Nozaki and Mikolajczak, 2020). In this manuscript, we discuss only pro-hedonic EER, which is the act of trying to make others feel better.
Relying on the process model of emotion (Gross, 1998), which presents four stages of emotion regulation, EER was also offered to consist of similar stages (Reeck et al., 2016). Namely, EER can be seen as a process consisting of the following stages; identification, selection, implementation and monitoring. In the identification stage, the emotion regulation support provider should infer the recipient’s emotional state, assign a value to that state and establish a regulation goal (Nozaki and Mikolajczak, 2020). In the selection stage, the provider should first perceive the available emotion regulation strategies, evaluate which ones are most valuable, and then choose which ones to use (Tanna and MacCann, 2022). In the implementation stage, the provider should consider how to implement the selected emotion regulation strategies into behavioral tactics, assess their capabilities, limitations and likely outcomes, as well as implement these tactics (Tanna and MacCann, 2022). The last stage is monitoring, in which the provider should identify whether to switch or stop the regulation strategy (Sheppes et al., 2015).
Providing help to others is associated with various beneficial outcomes such as lower mortality (Brown et al., 2003), better overall health (Piferi and Lawler, 2006), improved mood (Schacter and Margolin, 2019), reduced perceived stress (Raposa et al., 2016), greater happiness (Dunn et al., 2008), and an enhanced sense of personal worth (Klein, 2017). While these beneficial outcomes characterize providing support in general, recent studies have shown similar effects arising from specifically providing emotion regulation support to others (Zaki and Craig Williams, 2013; Nozaki, 2015; Reeck et al., 2016; Arbel et al., 2020; Cohen and Arbel, 2020; Nozaki and Mikolajczak, 2020; Arbel et al., 2022). These studies indicate both short- and long-term beneficial outcomes of EER for the provider’s emotional health (for review, see Cohen and Arbel, 2020). These beneficial outcomes among the general population include a reduction in depression symptoms and perseverative thinking (Morris et al., 2015), enhanced positive mood (Schacter and Margolin, 2019), and increased happiness (Morelli et al., 2015). For example, providing emotional support, such as empathy, to a same-sex friend improved the provider’s self-reported daily well-being, increased happiness, and decreased distress (Morelli et al., 2015). These effects carried over to the next day, albeit in a reduced form. Prisoners at a high-security prison reported a more positive mood one month after attempting to improve the feelings of others (Niven et al., 2012). Similarly, during the COVID-19 pandemic, psychological distress and daily negative mood of healthy young adults were reduced following a 3-week EER training that included providing support to others using cognitive reappraisal (Arbel et al., 2022). EER is also beneficial in reducing psychological distress during and following a stressful task (the Trier Social Stress Task; TSST; Kirschbaum et al., 1992, 1993). Providing EER by writing a supportive letter to a friend reduced physiological stress markers shortly afterwards (systolic blood pressure and alpha-amylase, but not cortisol or reported negative affect among healthy participants; Inagaki and Eisenberger, 2016). Although this research is still in its infancy, it suggests that EER may reduce physiological stress responses, especially sympathetic-related arousal (Inagaki and Eisenberger, 2016). A recent study that used text-based online communication has demonstrated that EER is most effective when people use emotion regulation strategies such as cognitive reappraisal and problem-solving, as well as when providing empathic responses (Nozaki and Mikolajczak, 2022).
Depression is characterized by impairments in social interactions (Teo et al., 2013), with better social relationships having a positive impact on mental health (Schön et al., 2009). The perception of support from others is commonly associated with a lower risk for depression and depressive symptoms (for review, see Gariépy et al., 2016). Throughout the life course, from childhood to old age, having a large social network is associated with a lower risk for depression (Santini et al., 2015; Loades et al., 2020). Individuals with depression may improve their social relationships by providing EER support to others. For example, providing support using cognitive reappraisal to individuals with high self-esteem who shared their failures was associated with increased positive affect, as well as higher relationship quality (Marigold et al., 2014). In emerging adulthood, EER was also found to improve relationship quality; a greater tendency to engage in taking perspective was associated with a higher quality of relationships and a greater well-being (Chan and Rawana, 2021). College students who favored EER strategies and perceived them to be useful were more well-adjusted, more connected socially, and developed stronger supportive relationships than their counterparts (Williams et al., 2018). Moreover, in new social contexts, EER can help a person become popular in both work and non-work interactions (Niven et al., 2015). Therefore, it is unsurprising that feelings of social connection increase when support is given (Inagaki and Ross, 2018).
Despite the evidence that EER may be a promising way to reduce depression symptoms, some findings suggest that under specific contexts EER may be maladaptive for depressed individuals. For example, providing tangible support to friends or listening to their disclosures led to higher levels of depression among young adults (Morelli et al., 2015). In addition, providing support to a stranger experiencing a negative event was found to be challenging and exhausting for providers (Gosnell and Gable, 2017). Furthermore, support providers who expressed high concerns about the effectiveness of their support displayed greater signs of depletion (Gosnell and Gable, 2017).
1.2. The mechanisms underlying the beneficial outcomes of EER in depression
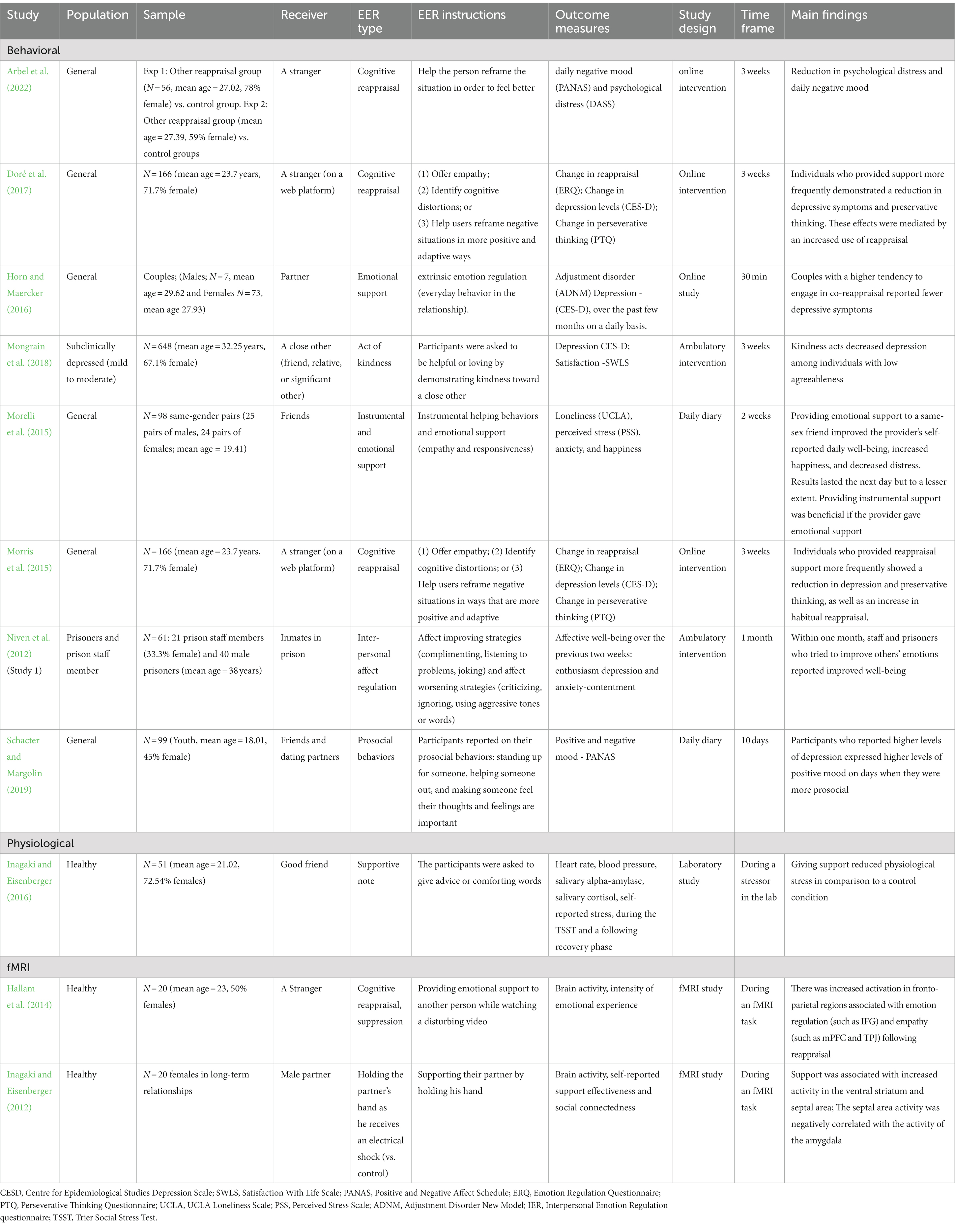
Although providing support to others may be difficult or exhausting (Morelli et al., 2015; Gosnell and Gable, 2017), recent findings indicate that providing emotion regulation support to others is mostly beneficial for individuals with depression (see Table 1). These findings received support both in studies assessing providing EER to a stranger and in studies in which EER was provided to an acquaintance or a family member. For example, helping strangers by using cognitive reappraisal in a three-week training study among healthy young adults reduced the providers’ depression symptoms and perseverative thinking (Morris et al., 2015; Doré et al., 2017). These reductions were mediated by increased use of habitual reappraisal (see also Arbel et al., 2022).
Providing EER to someone close also reduced depression symptoms among the support providers. For example, high-security prisoners, who helped other inmates improve their mood, reported more positive emotions one month later (Niven et al., 2012). In addition, performing acts of kindness to someone close during a three-week intervention reduced depression among individuals with low agreeableness (Mongrain et al., 2018). Healthy women who experienced a recent major life stressor and engaged more in co-reappraisal with their partner (i.e., helping one another to regulate their emotions using cognitive reappraisal) showed lower depressive symptoms (Horn and Maercker, 2016). This effect was not observed among the male partners. This may possibly be due to women’s tendency to verbalize stress more frequently than men, suggesting that they rely more on EER than men to regulate their emotions. Additionally, depressed adolescents showed higher positive mood following days on which they provided support for dating partners or peers (Schacter and Margolin, 2019).
While these studies show the beneficial effects of EER in reducing depression, there are very few data on the mechanisms underlying these effects. Our comprehensive literature review suggests that EER enhances three key functions known to be impaired in depression: (1) cognitive empathy, (2) intrinsic emotion regulation, and (3) reward. Below, we review behavioral and neuroimaging evidence for the role of each of these mechanisms in EER and discuss how the recruitment of these processes during EER can lead to a reduction in symptoms of depression.
1.2.1. Cognitive empathy
The first mechanism by which EER may reduce depression symptoms is empathy - the process of perceiving, understanding, experiencing, and responding to another’s emotional state (Barker, 2003). Researchers commonly distinguish between two types of empathy: cognitive empathy and emotional empathy (Davis, 1983). Cognitive empathy allows an individual to understand what someone else may think, adopt their psychological point of view, and predict their behavior (Frith and Singer, 2008). This ability may involve making inferences about the other’s affective and cognitive mental states (Shamay-Tsoory et al., 2009) and is related to cognitive flexibility (e.g., Eslinger, 1998; Shamay-Tsoory et al., 2004). Cognitive empathy, therefore, requires perspective-taking (Eslinger, 1998) and Theory of Mind (ToM; Shamay-Tsoory et al., 2004), which are the ability to understand another’s mental state and determine how the other will act (Decety and Jackson, 2004; Fan et al., 2011; Eres et al., 2015). Emotional empathy, on the other hand, enables individuals to tune into their feelings or experience affective reactions to the observed experiences of others (Shamay-Tsoory, 2011; Zaki, 2014). It is unconscious and requires lower-order cognitive abilities than cognitive empathy (Shamay-Tsoory, 2011; de Waal and Preston, 2017). High emotional empathy may be maladaptive due to the possibility of becoming overwhelmed by one’s distress and withdrawing from social interactions (Grynberg and Lopez-Perez, 2018). It has been suggested that the risk for depression and its severity may be associated with high emotional empathy levels and limited cognitive empathy (Schreiter et al., 2013).
Theoretical models suggest that EER requires the identification of the other person’s emotions (Reeck et al., 2016; Nozaki and Mikolajczak, 2020), making empathy a crucial antecedent of EER (Zaki, 2020). EER involves mostly cognitive empathy (Levy-Gigi and Shamay-Tsoory, 2017), as the individual needs to understand the other person’s perspective in order to choose which emotion regulation strategy can help that person (Gilead and Ochsner, 2021). Therefore, cognitive empathy is crucial during EER, as it enables the support provider to understand the other person’s perspective and to choose an emotion regulation strategy that fits the situation that the other is experiencing (Franklin-Gillette and Shamay-Tsoory, 2021). In line with this idea, in a study of dyadic interactions between romantic couples, the provider’s cognitive, but not emotional empathy, was linked to more successful EER for the support receiver (Levy-Gigi and Shamay-Tsoory, 2017). The importance of cognitive empathy in EER has also been highlighted in another study, which showed that cognitive empathy mediated the link between EER and higher couple satisfaction (Florean and Păsărelu, 2019). Together, these findings indicate the role of cognitive empathy in EER. Therefore, EER may be a good tool for elevating cognitive empathy among those characterized by deficits in cognitive empathy, such as individuals with depression. It is noteworthy, however, that the mentioned studies (Levy-Gigi and Shamay-Tsoory, 2017; Florean and Păsărelu, 2019) focused on the effects of support on the support receiver and not on the support provider. Therefore, more research is needed to understand the cognitive empathy’s role in EER in both healthy and clinical populations.
While the behavioral data on cognitive empathy in EER is limited, neuroimaging data support the role of cognitive empathy in EER. For example, Hallam et al. (2014) have found that providing EER increased activity in brain regions associated with empathy, such as the left tempero-parietal junction (TPJ), inferior temporal gyri, the medial prefrontal cortex (mPFC) and the temporal pole (TP). The mPFC and TPJ are likely to be engaged in the identification stage of EER (Reeck et al., 2016). Furthermore, the TPJ, mPFC, and TP are commonly associated with ToM (Gallagher and Frith, 2003; Saxe et al., 2006; Schurz et al., 2014). As EER is mainly associated with activations in the TPJ, mPFC and TP, it may depend more on cognitive empathy than on emotional empathy, which is mainly associated with activity in regions such as the insula, amygdala and anterior cingulate cortex (Dvash and Shamay-Tsoory, 2014).
Importantly, the cognitive empathy regions found activated during EER are considered key nodes of networks impaired in depression (Wen et al., 2021). For example, functional connectivity of the TPJ with the dorsolateral prefrontal cortex (dlPFC) and posterior cingulate cortex (PCC) is disrupted in depression (Penner et al., 2018). Patients with depression show abnormal large-scale functional coherence in the mPFC (Murrough et al., 2016). In addition, individuals with depression show less activity in the temporal pole than controls (Rodríguez-Cano et al., 2014), and this region appears to be reduced in size in this population (Rodríguez-Cano et al., 2014). Therefore, EER may be helpful for people with depression as it recruits the brain regions associated with cognitive empathy known to be impaired among these individuals (e.g., TPJ and mPFC; Shamay-Tsoory, 2011).
1.2.2. Intrinsic emotion regulation
The second mechanism that may reduce depression symptoms following EER is the enhancement of intrinsic emotion regulation (IER) processes. Individuals with depression show IER deficits, tending to use maladaptive IER strategies (e.g., rumination, suppression) with a reduced tendency to use adaptive IER strategies (distraction, reappraisal) (Joormann and Stanton, 2016). These individuals are also considered inflexible regulators, i.e., they find it difficult to assess contextual demands, to fit the IER strategies they use to the situation at hand, and lack the ability to monitor the effectiveness of a chosen strategy and make necessary modifications (Chen and Bonanno, 2021). Accordingly, difficulty switching between IER strategies is associated with more severe symptoms of depression (Kato, 2015, 2017). Thus, EER may be particularly beneficial for individuals with depression as it can enhance their use of adaptive IER strategies.
In support of this idea, in a three-week training study, supporting others using cognitive reappraise increased the supporter’s tendency to employ reappraisal on their own experiences. This increase in the use of cognitive reappraisal was associated with a reduction in depression and perseverative thinking. Thus, beyond reducing depressive symptoms, helping others provides an opportunity to practice and improve one’s regulatory skills (Morris et al., 2015; Doré et al., 2017). This may also have an impact on the quality of social interactions. For example, people who were better at regulating emotions were found to have better social interactions and were more inclined to engage in prosocial behaviors (Lopes et al., 2005). Namely, people who struggle with social interactions might be able to interact with others more effectively and have more positive social interactions if they are trained in emotion regulation abilities. One reason that EER may be a good tool for practicing one’s regulatory skills, especially among individuals with depression, is based on the idea that EER may require less cognitive effort than self-regulation (Cohen and Arbel, 2020). Most adaptive ways people use to regulate their emotions require a relatively high amount of cognitive resources (Ortner et al., 2016), which are not always available during a depressive episode (Zetsche et al., 2012).
The idea that EER may be less demanding than self-regulation is supported by findings showing that speaking in a third-person language (e.g., “Why is Lisa feeling this way?”) leads to a greater reduction in negative affect than using a first-person language (e.g., “Why am I feeling this way?”). Third-person thinking enhances people’s ability to control their thoughts, feelings, and behavior during stressful situations (Kross et al., 2014; Moser et al., 2017; Nook et al., 2017; Streamer et al., 2017). Similarly, considering other people’s problems entails psychological distance, making EER easier than regulating one’s emotions. This psychological distance may also help navigate stressful experiences in more objective, wise, and emotionally intelligent ways (Beck, 1970; Mischel and Rodriguez, 1993; Fujita et al., 2006; Trope and Liberman, 2010; Kross and Ayduk, 2011; Grossmann and Kross, 2014; Bernstein et al., 2015). Importantly, speaking to oneself in a third-person language facilitates IER relatively effortlessly without draining the cognitive control resources that are depleted during stressful situations (Moser et al., 2017). A third account for the relative effectiveness of EER as compared to IER comes from Coan’s social baseline theory (SBT; Beckes and Coan, 2011). According to this theory, the human brain acts as if it is in a social environment, so being near other people or groups is our baseline. Based on this assumption, humans experience fewer negative outcomes when embedded in social groups than when excluded or alone (Beckes and Coan, 2011; Coan and Maresh, 2014). In support to the social nature of emotion regulation, an individual’s dorsolateral prefrontal cortex (dlPFC), which is important for the self-regulation of emotions, is less active when they are around supportive others. Namely, the brain has to spend less attentional resources on IER when around others (Beckes and Coan, 2011; Coan and Maresh, 2014; for a review, see Ochsner and Gross, 2008). Consequently, Beckes and Coan (2011) and Coan and Maresh (2014) argue that the use of EER is not only beneficial but also more effective and efficient than self-regulation since less cognitive resources are needed to employ the regulation. In line with this idea, Levy-Gigi and Shamay-Tsoory (2017) observed that EER is more effective than IER in reducing distress. Therefore, EER can serve as an effective means for increasing self-regulatory skills in depression (Liu, 2022).
Neuroimaging data, mainly from healthy individuals, support the idea that EER recruits brain networks involved in IER, which are impaired in depression. For example, when healthy participants are asked to regulate other peoples’ emotions watching a disturbing video using cognitive reappraisal or expressive suppression was associated with increased activity in brain regions involved in IER, such as the left anterior cingulate cortex (ACC) and the rostral and medial prefrontal cortex (Hallam et al., 2014). The ventrolateral prefrontal systems may be involved in the selection stage of EER, while the lateral prefrontal and posterior medial prefrontal regions may be involved in the implementation stage of EER (Reeck et al., 2016). Activity in the ACC, and the connectivity between it and other regions, such as the striatum and the insula, are impaired in depression (Philippi et al., 2015). Also, the volume of the gray matter of the subgenual ACC is significantly reduced in patients with depression (Drevets et al., 2008). In addition, patients who failed to recover during a 12-week controlled treatment had a smaller volume of gray matter in the ACC than remitted patients (Gunning et al., 2009), suggesting a better clinical outcome for patients with larger ACC (Frodl et al., 2008). The rostral and medial prefrontal cortex also show altered activity in depression (Rodríguez-Cano et al., 2014; Murrough et al., 2016).
In addition to ACC and prefrontal regions, EER is also associated with activation in the septal area (SA). Among healthy participants, SA activation is increased when emotional support is given to another person (holding the partner’s arm when he received an electrical shock; Inagaki and Eisenberger, 2012). The SA also appears to be involved in caregiving behaviors (D’Anna and Gammie, 2009), such as parental care (Inagaki, 2018) and IER (Singewald et al., 2011). Increased activation of this region while giving support is associated with greater perceived effectiveness of the support, increased social connectedness, and reduced amygdala activity (Inagaki, 2018). Reduction in amygdala activity is often seen in IER tasks (Walter et al., 2009) but less among depressed individuals (Johnstone et al., 2007), who are characterized by hyperactivation of the amygdala (Sheline et al., 2001; Surguladze et al., 2004; Suslow et al., 2010; Victor et al., 2010).
Hallam et al. (2014) and Inagaki and Eisenberger (2012) studied the brain mechanisms of EER in healthy individuals; we assume that the same IER networks are activated when individuals with depression provide EER. Thus, asking individuals with depression to provide emotion regulation support to others may strengthen brain regions associated with IER, whose activity is commonly impaired among this population.
1.2.3. Reward
A third way in which EER may benefit individuals with depression is through the rewarding nature of this act. Reward represents the pleasure individuals typically experience when they receive or experience something positive (Wilson et al., 2018). Reduced reward function is a key diagnostic criterion for depression (Feighner et al., 1972). Individuals with depression show altered reward sensitivity (Pizzagalli et al., 2008). They are less responsive to social (e.g., positive feedback) and to non-social (e.g., monetary gains) rewards and are less motivated to seek rewards (Forbes et al., 2009, 2010; Pizzagalli et al., 2009; Olino et al., 2014, 2015). As a result, it may be difficult for a person with depression to avoid negative situations and to make new positive experiences to overcome a depressive mood. Individuals with depression may, therefore, especially benefit from rewarding experiences such as providing support to others (Morris et al., 2015; Horn and Maercker, 2016; Doré et al., 2017; Mongrain et al., 2018).
Extensive behavioral research has shown that prosocial behaviors enhance well-being (for reviews, see Anderson et al., 2014; Konrath, 2014; Aknin and Whillans, 2021). EER is mostly a prosocial act, suggesting that it can also serve as a rewarding experience (Aknin et al., 2018). And providing emotion regulation support to others does increase positive mood (Orth et al., 2016; Will et al., 2017) and boosts feelings of self-worth (Schacter and Margolin, 2019).
Neuroimaging data support the behavioral findings that EER is a rewarding experience for the support provider. Providing EER increases activation in the striatum (Inagaki and Eisenberger, 2012; Hallam et al., 2014), a region implicated in reward processing (Delgado, 2007). Helping other people using cognitive reappraisal is associated with heightened activity in the caudate nucleus (part of the dorsal striatum; Hallam et al., 2014). Similarly, activation increased in the ventral striatum (VS) when women held their partner’s hand while he was experiencing physical pain (electric shock; Inagaki and Eisenberger, 2012). The reward system is likely to be involved in the monitoring stage (Sheppes et al., 2015).
A growing body of literature suggests that the dopaminergic mesolimbic regions involved in reward processing during EER are dysfunctional in depression (Dunlop and Nemeroff, 2007). The striatum shows reduced activation in depression (Robinson et al., 2012), especially during reward processing (Kelley, 2004; O’Doherty et al., 2006; Delgado, 2007). Depression is also known to be associated with altered intrinsic connectivity within the ventral striatum (Pan et al., 2017). The striatum also appears smaller among patients with depression compared to controls (Dombrovski et al., 2012). Patients with depression who committed suicide showed decreased gray matter in the VS (Dombrovski et al., 2012). Taken together, these results highlight the potential role of VS recruitment during EER in reducing depressive symptoms.
2. Conclusion
Depression is a serious mental illness that adversely affects the person’s mood, behaviors and thoughts. This leads to personal and societal costs. Only 50% of people with depression benefit from psychological treatment and medications (Khan and Brown, 2015; Cuijpers et al., 2018). This review has shown that EER appears promising as a non-pharmaceutical treatment for depression. Behavioral and neuroimaging evidence both suggest that EER reduces depression symptoms and promotes well-being among the healthy population. These effects appear to be due to EER affecting three key processes that are impaired in depression: cognitive empathy, IER, and reward. Individuals with depression show altered neural activity in the brain regions subserving these cognitive functions as well as behavioral deficits. Initial findings indicate that the benefits of EER for depressed individuals are achieved by the recruitment of these three cognitive functions, but there is a need for more empirical research (Cohen and Arbel, 2020).
Other mechanisms, such as increased social relationships and connectedness, may also underlie the beneficial effects of EER for depressed individuals (Marigold et al., 2014). Individuals with depression may find it difficult to engage in social connections due to their own distress and anxiety, which may lead them to withdraw or avoid social interactions (Kupferberg et al., 2016). Asking these people to provide EER to another person may help them engage in social interactions, increase their feeling of social connectedness and prevent withdrawal or avoidance behaviors (Brown et al., 2012; Satici et al., 2016). Furthermore, when people with depression provide EER support to others, the feeling that they helped another person may enhance their self-efficacy (Caprara and Steca, 2007), known to be low in individuals with depression (Volz et al., 2019) and to be important in preventing depressive symptoms (Blazer, 2002). As there are only a few studies on the role of EER in increasing social connectedness and self-efficacy (Marigold et al., 2014), more research is needed to test whether these mechanisms play a role in the beneficial effects of EER for individuals with depression.
It is noteworthy, however, that people with depression may find it difficult to provide emotional support. Indeed, there is evidence showing that providing support may be exhausting for the provider (Gosnell and Gable, 2017). Supporting others is challenging and potentially stressful since it requires emotional resources and the ability to identify, prioritize, and respond appropriately to the other person’s needs (Jayamaha et al., 2021). Depression is characterized by the depletion of cognitive resources, which may lead to a feeling of inability to deal with stressful situations and poor coping strategies, especially in interpersonal situations (Hammen, 1991). Namely, people with depression symptoms may perceive stressful situations, especially in interpersonal contexts, as something they can cope with effectively (Nezu and Ronan, 1988; Herzberg et al., 1998; Caldwell et al., 2004; Keser et al., 2020). The need to cope in these situations may lead to distress and burnout that, in turn, reduce the quality of the support (Given et al., 2011; Bastawrous, 2013; Liu et al., 2020). However, although people with depression report lower use of adaptive IER strategies during both self-regulation and EER (Joormann and Stanton, 2016), they manage to implement these strategies effectively (similarly to non-depressed individuals) when instructed to do so in laboratory and training studies (Ellis et al., 2013; Smoski et al., 2014; Millgram et al., 2015; Platt et al., 2015). These findings suggest that while people with depression are less prone to use adaptive emotion regulation strategies, they can implement these strategies when instructed to do so (Liu and Thompson, 2017).
Our review raises important suggestions for future research and clinical practice. Group therapy may be highly effective for individuals with depression as this therapy can encourage both the sharing of negative feelings and supporting others with their struggles (McDermut et al., 2001; Truax, 2001; Kösters et al., 2006; Cuijpers et al., 2008), what may increase cognitive empathy and self-regulatory skills, as well as serve as a rewarding experience. Namely, helping others may allow depressed individuals to practice IER strategies and cognitive empathy skills and to experience reward from their involvement in a prosocial act. Utilizing EER in therapy may thus help to decrease distress and improve well-being. However, it is important to consider the fact that individuals with depression may have difficulty providing support, which may adversely affect the effectiveness of their support (Given et al., 2011; Bastawrous, 2013; Liu et al., 2020). This should be taken into account when considering the effects of EER provided by individuals with depression on the support recipient, such as when applying EER in clinical settings (e.g., group therapy).
To conclude, the current paper suggests that depressed individuals may benefit from EER via three processes: cognitive empathy, intrinsic emotion regulation, and reward. As most prior studies on EER were done on the general population and only one study tested the effects of EER among depressed individuals (Mongrain et al., 2018), more research is needed to uncover the mechanisms underlying the benefits of EER in depression.
Author contributions
AM drafted the manuscript. NC provided critical revisions. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aknin, L. B., Van de Vondervoort, J. W., and Hamlin, J. K. (2018). Positive feelings reward and promote prosocial behavior. Curr. Opin. Psychol. 20, 55–59. doi: 10.1016/j.copsyc.2017.08.017
Aknin, L. B., and Whillans, A. V. (2021). Helping and happiness: a review and guide for public policy. Soc. Issues Policy Rev. 15, 3–34. doi: 10.1111/sipr.12069
Aldao, A., Sheppes, G., and Gross, J. J. (2015). Emotion regulation flexibility. Cogn. Ther. Res. 39, 263–278. doi: 10.1007/s10608-014-9662-4
Anderson, N. D., Damianakis, T., Kröger, E., Wagner, L. M., Dawson, D. R., Binns, M. A., et al. (2014). The benefits associated with volunteering among seniors: a critical review and recommendations for future research. Psychol. Bull. 140, 1505–1533. doi: 10.1037/a0037610
Arbel, R., Khuri, M., Sagi, J., and Cohen, N. (2020). Reappraising others’ negative emotions as a way to enhance coping during the COVID-19 outbreak. PsyArXiv 17. doi: 10.31234/osf.io/y25gx
Arbel, R., Szpiro, S. F. A., Sagi, J., Khuri, M., Berkovits, L., and Cohen, N. (2022). Reappraising negative emotions reduces distress during the COVID-19 outbreak. Curr. Psychol. 1–10, 1–10. doi: 10.1007/s12144-022-03642-6
Bastawrous, M. (2013). Caregiver burden—a critical discussion. Int. J. Nurs. Stud. 50, 431–441. doi: 10.1016/j.ijnurstu.2012.10.005
Beck, A. T. (1970). Cognitive therapy: nature and relation to behavior therapy. Behav. Ther. 1, 184–200. doi: 10.1016/S0005-7894(70)80030-2
Beckes, L., and Coan, J. A. (2011). Social baseline theory: the role of social proximity in emotion and economy of action. Soc. Personal. Psychol. Compass 5, 976–988. doi: 10.1111/j.1751-9004.2011.00400.x
Bernstein, A., Hadash, Y., Lichtash, Y., Tanay, G., Shepherd, K., and Fresco, D. M. (2015). Decentering and related constructs: a critical review and metacognitive processes model. Perspect. Psychol. Sci. 10, 599–617. doi: 10.1177/1745691615594577
Blazer, D. G. (2002). Self-efficacy and depression in late life: a primary prevention proposal. Aging Ment. Health 6, 315–324. doi: 10.1080/1360786021000006938
Bonanno, G. A., and Burton, C. L. (2013). Regulatory flexibility: an individual differences perspective on coping and emotion regulation. Perspect. Psychol. Sci. 8, 591–612. doi: 10.1177/1745691613504116
Brown, K. M., Hoye, R., and Nicholson, M. (2012). Self-esteem, self-efficacy, and social connectedness as mediators of the relationship between volunteering and well-being. J. Soc. Serv. Res. 38, 468–483. doi: 10.1080/01488376.2012.687706
Brown, S. L., Nesse, R. M., Vinokur, A. D., and Smith, D. M. (2003). Providing social support may be more beneficial than receiving it: results from a prospective study of mortality. Psychol. Sci. 14, 320–327. doi: 10.1111/1467-9280.14461
Caldwell, M. S., Rudolph, K. D., Troop-Gordon, W., and Kim, D.-Y. (2004). Reciprocal influences among relational self-views, social disengagement, and peer stress during early adolescence. Child Dev. 75, 1140–1154. doi: 10.1111/j.1467-8624.2004.00730.x
Caprara, G. V., and Steca, P. (2007). Prosocial agency: the contribution of values and self–efficacy beliefs to prosocial behavior across ages. J. Soc. Clin. Psychol. 26, 218–239. doi: 10.1521/jscp.2007.26.2.218
Chan, S., and Rawana, J. S. (2021). Examining the associations between interpersonal emotion regulation and psychosocial adjustment in emerging adulthood. Cogn. Ther. Res. 45, 652–662. doi: 10.1007/s10608-020-10185-2
Chen, S., and Bonanno, G. A. (2021). Components of emotion regulation flexibility: linking latent profiles to depressive and anxious symptoms. Clin. Psychol. Sci. 9, 236–251. doi: 10.1177/2167702620956972
Cheng, C. (2001). Assessing coping flexibility in real-life and laboratory settings: a multimethod approach. J. Pers. Soc. Psychol. 80, 814–833. doi: 10.1037/0022-3514.80.5.814
Cheng, C., Lau, H.-P. B., and Chan, M.-P. S. (2014). Coping flexibility and psychological adjustment to stressful life changes: a meta-analytic review. Psychol. Bull. 140, 1582–1607. doi: 10.1037/a0037913
Coan, J. A., and Maresh, E. L. (2014). “Social baseline theory and the social regulation of emotion” in Handbook of Emotion Regulation. ed. J. J. Gross (New York: The Guilford Press), 221–236.
Cohen, N., and Arbel, R. (2020). On the benefits and costs of extrinsic emotion regulation to the provider: toward a neurobehavioral model. Cortex 130, 1–15. doi: 10.1016/j.cortex.2020.05.011
Cuijpers, P., Karyotaki, E., Reijnders, M., and Huibers, M. J. H. (2018). Who benefits from psychotherapies for adult depression? A meta-analytic update of the evidence meta-analytic update of the evidence. Cogn. Behav. Ther. 47, 91–106. doi: 10.1080/16506073.2017.1420098
Cuijpers, P., van Straten, A., Andersson, G., and van Oppen, P. (2008). Psychotherapy for depression in adults: a meta-analysis of comparative outcome studies. J. Consult. Clin. Psychol. 76, 909–922. doi: 10.1037/a0013075
D’Anna, K. L., and Gammie, S. C. (2009). Activation of corticotropin-releasing factor receptor 2 in lateral septum negatively regulates maternal defense. Behav. Neurosci. 123, 356–368. doi: 10.1037/a0014987
Davis, M. H. (1983). The effects of dispositional empathy on emotional reactions and helping: A multidimensional approach. Journal of Personality 51, 167–184.
de Waal, F. B. M., and Preston, S. D. (2017). Mammalian empathy: Behavioural manifestations and neural basis. Nature Reviews Neuroscience 18, 498–509. doi: 10.1038/nrn.2017.72
Decety, J., and Jackson, P. L. (2004). The functional architecture of human empathy. Behav. Cogn. Neurosci. Rev. 3, 71–100. doi: 10.1177/1534582304267187
Delgado, M. R. (2007). Reward-related responses in the human striatum. Ann. N. Y. Acad. Sci. 1104, 70–88. doi: 10.1196/annals.1390.002
Dombrovski, A. Y., Siegle, G. J., Szanto, K., Clark, L., Reynolds, C. F., and Aizenstein, H. (2012). The temptation of suicide: striatal gray matter, discounting of delayed rewards, and suicide attempts in late-life depression. Psychol. Med. 42, 1203–1215. doi: 10.1017/S0033291711002133
Doré, B. P., Morris, R. R., Burr, D. A., Picard, R. W., and Ochsner, K. N. (2017). Helping others regulate emotion predicts increased regulation of one’s own emotions and decreased symptoms of depression. Personal. Soc. Psychol. Bull. 43, 729–739. doi: 10.1177/0146167217695558
Drevets, W. C., Savitz, J., and Trimble, M. (2008). The subgenual anterior cingulate cortex in mood disorders. CNS Spectr. 13, 663–681. doi: 10.1017/S1092852900013754
Dunlop, B. W., and Nemeroff, C. B. (2007). The role of dopamine in the pathophysiology of depression. Arch. Gen. Psychiatry 64:327. doi: 10.1001/archpsyc.64.3.327
Dunn, E. W., Aknin, L. B., and Norton, M. I. (2008). Spending money on others promotes happiness. Science 319, 1687–1688. doi: 10.1126/science.1150952
Dvash, J., and Shamay-Tsoory, S. G. (2014). Theory of mind and empathy as multidimensional constructs: neurological foundations. Top. Lang. Disord. 34, 282–295. doi: 10.1097/TLD.0000000000000040
Ellis, A. J., Vanderlind, W. M., and Beevers, C. G. (2013). Enhanced anger reactivity and reduced distress tolerance in major depressive disorder. Cogn. Ther. Res. 37, 498–509. doi: 10.1007/s10608-012-9494-z
Eres, R., Decety, J., Louis, W. R., and Molenberghs, P. (2015). Individual differences in local gray matter density are associated with differences in affective and cognitive empathy. NeuroImage 117, 305–310. doi: 10.1016/j.neuroimage.2015.05.038
Eslinger, P. J. (1998). Neurological and neuropsychological bases of empathy. Eur. Neurol. 39, 193–199. doi: 10.1159/000007933
Fan, Y., Duncan, N. W., de Greck, M., and Northoff, G. (2011). Is there a core neural network in empathy? An fMRI based quantitative meta-analysis. Neurosci. Biobehav. Rev. 35, 903–911. doi: 10.1016/j.neubiorev.2010.10.009
Feighner, J. P., Robins, E., and Guze, S. B. (1972). Diagnostic criteria for use in psychiatric research. Arch. Gen. Psychiatry 26, 57–63. doi: 10.1001/archpsyc.1972.01750190059011
Florean, I.-S., and Păsărelu, C.-R. (2019). Interpersonal emotion regulation and cognitive empathy as mediators between intrapersonal emotion regulation difficulties and couple satisfaction. J. Evid. Based Psychother. 19, 119–134. doi: 10.24193/jebp.2019.2.17
Forbes, E. E., Hariri, A. R., Martin, S. L., Silk, J. S., Moyles, D. L., Fisher, P. M., et al. (2009). Altered striatal activation predicting real-world positive affect in adolescent major depressive disorder. Am. J. Psychiatr. 166, 64–73. doi: 10.1176/appi.ajp.2008.07081336
Forbes, E. E., Ryan, N. D., Phillips, M. L., Manuck, S. B., Worthman, C. M., Moyles, D. L., et al. (2010). Healthy adolescents’ neural response to reward: associations with puberty, positive affect, and depressive symptoms. J. Am. Acad. Child Adolesc. Psychiatry 49, 162–172.e5. doi: 10.1016/j.jaac.2009.11.006
Franklin-Gillette, S., and Shamay-Tsoory, S. G. (2021). “An interbrain approach for understanding empathy: the contribution of empathy to interpersonal emotion regulation” in The Neural Basis of Mentalizing eds. M. Gilead and K. N. Ochsner (Springer), 567–578.
Fried, E. I., Rieble, C., and Proppert, R. K. K. (2022). Building an early warning system for depression: rationale, objectives, and methods of the WARN-D study [preprint]. PsyArXiv. doi: 10.31234/osf.io/9qcvs
Frith, C. D., and Singer, T. (2008). The role of social cognition in decision making. Philosophical Transactions of the Royal Society B: Biological Sciences 363, 3875–3886.
Frodl, T., Jäger, M., Born, C., Ritter, S., Kraft, E., Zetzsche, T., et al. (2008). Anterior cingulate cortex does not differ between patients with major depression and healthy controls, but relatively large anterior cingulate cortex predicts a good clinical course. Psychiatry Res. Neuroimag. 163, 76–83. doi: 10.1016/j.pscychresns.2007.04.012
Fujita, K., Trope, Y., Liberman, N., and Levin-Sagi, M. (2006). Construal levels and self-control. J. Pers. Soc. Psychol. 90, 351–367. doi: 10.1037/0022-3514.90.3.351
Gallagher, H. L., and Frith, C. D. (2003). Functional imaging of ‘theory of mind.’. Trends Cogn. Sci. 7, 77–83. doi: 10.1016/S1364-6613(02)00025-6
Gariépy, G., Honkaniemi, H., and Quesnel-Vallée, A. (2016). Social support and protection from depression: systematic review of current findings in Western countries. Br. J. Psychiatry 209, 284–293. doi: 10.1192/bjp.bp.115.169094
Gilead, M., and Ochsner, K. N. (Eds.). (2021). The Neural Basis of Mentalizing. New York: Springer International Publishing.
Given, B. A., Sherwood, P., and Given, C. W. (2011). Support for caregivers of cancer patients: transition after active treatment. Cancer Epidemiol. Biomark. Prev. 20, 2015–2021. doi: 10.1158/1055-9965.EPI-11-0611
Gosnell, C. L., and Gable, S. L. (2017). You deplete me: impacts of providing positive and negative event support on self-control. Pers. Relat. 24, 598–622. doi: 10.1111/pere.12200
Gross, J. J. (1998). The emerging field of emotion regulation: an integrative review. Rev. Gen. Psychol. 2, 271–299. doi: 10.1037/1089-2680.2.3.271
Gross, J. J., and Thompson, R. (2007). “Emotion regulation: conceptual foundations” in Handbook of Emotion Regulation. ed. J. J. Gross (New York, NY: Guilford Press), 3–26.
Grossmann, I., and Kross, E. (2014). Exploring Solomon’s paradox: Self-distancing eliminates the self-other asymmetry in wise reasoning about close relationships in younger and older adults. Psychological science 25, 1571–1580. doi: 10.1177/0956797614535400
Grynberg, D., and López-Pérez, B. (2018). Facing others’ misfortune: Personal distress mediates the association between maladaptive emotion regulation and social avoidance. PLoS ONE 13, 1–14. doi: 10.1371/journal.pone.0194248
Gunning, F. M., Cheng, J., Murphy, C. F., Kanellopoulos, D., Acuna, J., Hoptman, M. J., et al. (2009). Anterior cingulate cortical volumes and treatment remission of geriatric depression. Int. J. Geriatr. Psychiatry 24, 829–836. doi: 10.1002/gps.2290
Hallam, G. P., Webb, T. L., Sheeran, P., Miles, E., Niven, K., Wilkinson, I. D., et al. (2014). The neural correlates of regulating another person’s emotions: an exploratory fMRI study. Front. Hum. Neurosci. 8:376. doi: 10.3389/fnhum.2014.00376
Hammen, C. (1991). Generation of stress in the course of unipolar depression. J. Abnorm. Psychol. 100, 555–561. doi: 10.1037/0021-843X.100.4.555
Herzberg, D. S., Hammen, C., Burge, D., Daley, S. E., Davila, J., and Lindberg, N. (1998). Social competence as a predictor of chronic interpersonal stress. Pers. Relat. 5, 207–218. doi: 10.1111/j.1475-6811.1998.tb00168.x
Horn, A. B., and Maercker, A. (2016). Intra- and interpersonal emotion regulation and adjustment symptoms in couples: the role of co-brooding and co-reappraisal. BMC Psychol. 4:51. doi: 10.1186/s40359-016-0159-7
Inagaki, T. K. (2018). Neural mechanisms of the link between giving social support and health. Ann. N. Y. Acad. Sci. 1428, 33–50. doi: 10.1111/nyas.13703
Inagaki, T. K., and Eisenberger, N. I. (2012). Neural correlates of giving support to a loved one. Psychosomatic Medicine 74, 3–7. doi: 10.1097/PSY.0b013e3182359335
Inagaki, T. K., and Eisenberger, N. I. (2016). Giving support to others reduces sympathetic nervous system-related responses to stress. Psychophysiology 53, 427–435. doi: 10.1111/psyp.12578
Inagaki, T. K., and Ross, L. P. (2018). Neural correlates of giving social support: differences between giving targeted versus untargeted support. Psychosom. Med. 80, 724–732. doi: 10.1097/PSY.0000000000000623
Jayamaha, S. D., Overall, N. C., Girme, Y. U., Hammond, M. D., and Fletcher, G. J. O. (2021). Depressive symptoms, stress, and poorer emotional support when needed by intimate partners. Emotion 21, 1160–1176. doi: 10.1037/emo0001000
Johnstone, T., van Reekum, C. M., Urry, H. L., Kalin, N. H., and Davidson, R. J. (2007). Failure to regulate: counterproductive recruitment of top-down prefrontal-subcortical circuitry in major depression. J. Neurosci. 27, 8877–8884. doi: 10.1523/JNEUROSCI.2063-07.2007
Joormann, J., and Stanton, C. H. (2016). Examining emotion regulation in depression: a review and future directions. Behav. Res. Ther. 86, 35–49. doi: 10.1016/j.brat.2016.07.007
Kapur, S., Phillips, A. G., and Insel, T. (2012). Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Mol. Psychiatry 17, 1174–1179. doi: 10.1038/mp.2012.105
Kashdan, T. B., and Rottenberg, J. (2010). Psychological flexibility as a fundamental aspect of health. Clin. Psychol. Rev. 30, 865–878. doi: 10.1016/j.cpr.2010.03.001
Kato, T. (2015). The impact of coping flexibility on the risk of depressive symptoms. PLoS One 10:e0128307. doi: 10.1371/journal.pone.0128307
Kato, T. (2017). Effects of flexibility in coping with menstrual pain on depressive symptoms. Pain Pract. 17, 70–77. doi: 10.1111/papr.12412
Kelley, A. E. (2004). Ventral striatal control of appetitive motivation: role in ingestive behavior and reward-related learning. Neurosci. Biobehav. Rev. 27, 765–776. doi: 10.1016/j.neubiorev.2003.11.015
Keser, E., Kahya, Y., and Akın, B. (2020). Stress generation hypothesis of depressive symptoms in interpersonal stressful life events: the roles of cognitive triad and coping styles via structural equation modeling. Curr. Psychol. 39, 174–182. doi: 10.1007/s12144-017-9744-z
Khan, A., and Brown, W. A. (2015). Antidepressants versus placebo in major depression: an overview. World Psychiatry 14, 294–300. doi: 10.1002/wps.20241
Kirschbaum, C., Pirke, K.-M., and Hellhammer, D. H. (1993). The ‘Trier social stress test’ – a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology 28, 76–81. doi: 10.1159/000119004
Kirschbaum, C., Wüst, S., and Hellhammer, D. (1992). Consistent sex differences in cortisol responses to psychological stress. Psychosom. Med. 54, 648–657. doi: 10.1097/00006842-199211000-00004
Klein, N. (2017). Prosocial behavior increases perceptions of meaning in life. J. Posit. Psychol. 12, 354–361. doi: 10.1080/17439760.2016.1209541
Konrath, S. (2014). “The power of philanthropy and volunteering” in Interventions and Policies to Enhance Wellbeing. eds. F. A. Huppert and C. L. Cooper (London, UK: Wiley-Blackwell), 387–427.
Kösters, M., Burlingame, G. M., Nachtigall, C., and Strauss, B. (2006). A meta-analytic review of the effectiveness of inpatient group psychotherapy. Group Dyn. Theory Res. Pract. 10, 146–163. doi: 10.1037/1089-2699.10.2.146
Kross, E., and Ayduk, O. (2011). Making meaning out of negative experiences by self-distancing. Curr. Dir. Psychol. Sci. 20, 187–191. doi: 10.1177/0963721411408883
Kross, E., Bruehlman-Senecal, E., Park, J., Burson, A., Dougherty, A., Shablack, H., et al. (2014). Self-talk as a regulatory mechanism: how you do it matters. J. Pers. Soc. Psychol. 106, 304–324. doi: 10.1037/a0035173
Kupferberg, A., Bicks, L., and Hasler, G. (2016). Social functioning in major depressive disorder. Neurosci. Biobehav. Rev. 69, 313–332. doi: 10.1016/j.neubiorev.2016.07.002
Levy-Gigi, E., and Shamay-Tsoory, S. G. (2017). Help me if you can: evaluating the effectiveness of interpersonal compared to intrapersonal emotion regulation in reducing distress. J. Behav. Ther. Exp. Psychiatry 55, 33–40. doi: 10.1016/j.jbtep.2016.11.008
Liu, T. (2022). “Subjective well-being across one year of living through the COVID-19 pandemic: A 3-wave longitudinal study” in Master of Science thesis, University of Houston (University of Huston Repository) https://hdl.handle.net/10657/13166
Liu, Z., Heffernan, C., and Tan, J. (2020). Caregiver burden: a concept analysis. Int. J. Nurs. Sci. 7, 438–445. doi: 10.1016/j.ijnss.2020.07.012
Liu, D. Y., and Thompson, R. J. (2017). Selection and implementation of emotion regulation strategies in major depressive disorder: an integrative review. Clin. Psychol. Rev. 57, 183–194. doi: 10.1016/j.cpr.2017.07.004
Loades, M. E., Chatburn, E., Higson-Sweeney, N., Reynolds, S., Shafran, R., Brigden, A., et al. (2020). Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 59, 1218–1239.e3. doi: 10.1016/j.jaac.2020.05.009
Lopes, P. N., Salovey, P., Côté, S., and Beers, M. (2005). Emotion regulation abilities and the quality of social interaction. Emotion 5, 113–118. doi: 10.1037/1528-3542.5.1.113
Marigold, D. C., Cavallo, J. V., Holmes, J. G., and Wood, J. V. (2014). You can’t always give what you want: the challenge of providing social support to low self-esteem individuals. J. Pers. Soc. Psychol. 107, 56–80. doi: 10.1037/a0036554
McDermut, W., Miller, I. W., and Brown, R. A. (2001). The efficacy of group psychotherapy for depression: a meta-analysis and review of the empirical research. Clin. Psychol. Sci. Pract. 8, 98–116. doi: 10.1093/clipsy.8.1.98
Millgram, Y., Joormann, J., Huppert, J. D., and Tamir, M. (2015). Sad as a matter of choice? Emotion-regulation goals in depression. Psychol. Sci. 26, 1216–1228. doi: 10.1177/0956797615583295
Mischel, W., and Rodriguez, M. L. (1993). “Psychological distance in self-imposed delay of gratification” in The Development and Meaning of Psychological Distance. eds. R. R. Cocking and K. A. Renninger (Hillsdale, NJ: Erlbaum), 109–121.
Mongrain, M., Barnes, C., Barnhart, R., and Zalan, L. B. (2018). Acts of kindness reduce depression in individuals low on agreeableness. Transl. Issues Psychol. Sci. 4, 323–334. doi: 10.1037/tps0000168
Morelli, S. A., Lee, I. A., Arnn, M. E., and Zaki, J. (2015). Emotional and instrumental support provision interact to predict well-being. Emotion 15, 484–493. doi: 10.1037/emo0000084
Morris, R. R., Schueller, S. M., and Picard, R. W. (2015). Efficacy of a web-based, crowdsourced peer-to-peer cognitive reappraisal platform for depression: randomized controlled trial. J. Med. Internet Res. 17:e72. doi: 10.2196/jmir.4167
Moser, J. S., Dougherty, A., Mattson, W. I., Katz, B., Moran, T. P., Guevarra, D., et al. (2017). Third-person self-talk facilitates emotion regulation without engaging cognitive control: converging evidence from ERP and fMRI. Sci. Rep. 7:4519. doi: 10.1038/s41598-017-04047-3
Murrough, J. W., Abdallah, C. G., Anticevic, A., Collins, K. A., Geha, P., Averill, L. A., et al. (2016). Reduced global functional connectivity of the medial prefrontal cortex in major depressive disorder. Hum. Brain Mapp. 37, 3214–3223. doi: 10.1002/hbm.23235
Nezu, A. M., and Ronan, G. F. (1988). Social problem solving as a moderator of stress-related depressive symptoms: a prospective analysis. J. Couns. Psychol. 35, 134–138. doi: 10.1037/0022-0167.35.2.134
Niven, K., Garcia, D., van der Löwe, I., Holman, D., and Mansell, W. (2015). Becoming popular: interpersonal emotion regulation predicts relationship formation in real life social networks. Front. Psychol. 6:1452. doi: 10.3389/fpsyg.2015.01452
Niven, K., Totterdell, P., Holman, D., and Headley, T. (2012). Does regulating others’ feelings influence people’s own affective well-being? J. Soc. Psychol. 152, 246–260. doi: 10.1080/00224545.2011.599823
Nook, E. C., Schleider, J. L., and Somerville, L. H. (2017). A linguistic signature of psychological distancing in emotion regulation. J. Exp. Psychol. Gen. 146, 337–346. doi: 10.1037/xge0000263
Nozaki, Y. (2015). Emotional competence and extrinsic emotion regulation directed toward an ostracized person. Emotion 15, 763–774. doi: 10.1037/emo0000081
Nozaki, Y., and Mikolajczak, M. (2020). Extrinsic emotion regulation. Emotion 20, 10–15. doi: 10.1037/emo0000636
Nozaki, Y., and Mikolajczak, M. (2022). Effectiveness of extrinsic emotion regulation strategies in text-based online communication. Emotion, Online ahead of print. doi: 10.1037/emo0001186
O’Doherty, J. P., Buchanan, T. W., Seymour, B., and Dolan, R. J. (2006). Predictive neural coding of reward preference involves dissociable responses in human ventral midbrain and ventral striatum. Neuron 49, 157–166. doi: 10.1016/j.neuron.2005.11.014
Ochsner, K. N., and Gross, J. J. (2008). Cognitive emotion regulation: insights from social cognitive and affective neuroscience. Curr. Dir. Psychol. Sci. 17, 153–158. doi: 10.1111/j.1467-8721.2008.00566.x
Olino, T. M., McMakin, D. L., Morgan, J. K., Silk, J. S., Birmaher, B., Axelson, D. A., et al. (2014). Reduced reward anticipation in youth at high-risk for unipolar depression: a preliminary study. Dev. Cogn. Neurosci. 8, 55–64. doi: 10.1016/j.dcn.2013.11.005
Olino, T. M., Silk, J. S., Osterritter, C., and Forbes, E. E. (2015). Social reward in youth at risk for depression: a preliminary investigation of subjective and neural differences. J. Child Adolesc. Psychopharmacol. 25, 711–721. doi: 10.1089/cap.2014.0165
Orth, U., Robins, R. W., Meier, L. L., and Conger, R. D. (2016). Refining the vulnerability model of low self-esteem and depression: disentangling the effects of genuine self-esteem and narcissism. J. Pers. Soc. Psychol. 110, 133–149. doi: 10.1037/pspp0000038
Ortner, C. N. M., Marie, M. S., and Corno, D. (2016). Cognitive costs of reappraisal depend on both emotional stimulus intensity and individual differences in habitual reappraisal. PLoS One 11, 1–19. doi: 10.1371/journal.pone.0167253
Pan, P. M., Sato, J. R., Salum, G. A., Rohde, L. A., Gadelha, A., Zugman, A., et al. (2017). Ventral striatum functional connectivity as a predictor of adolescent depressive disorder in a longitudinal community-based sample. Am. J. Psychiatr. 174, 1112–1119. doi: 10.1176/appi.ajp.2017.17040430
Penner, J., Osuch, E. A., Schaefer, B., Théberge, J., Neufeld, R. W. J., Menon, R. S., et al. (2018). Temporoparietal junction functional connectivity in early schizophrenia and major depressive disorder. Chronic Stress 2:247054701881523. doi: 10.1177/2470547018815232
Philippi, C. L., Motzkin, J. C., Pujara, M. S., and Koenigs, M. (2015). Subclinical depression severity is associated with distinct patterns of functional connectivity for subregions of anterior cingulate cortex. J. Psychiatr. Res. 71, 103–111. doi: 10.1016/j.jpsychires.2015.10.005
Piferi, R. L., and Lawler, K. A. (2006). Social support and ambulatory blood pressure: an examination of both receiving and giving. Int. J. Psychophysiol. 62, 328–336. doi: 10.1016/j.ijpsycho.2006.06.002
Pizzagalli, D. A., Holmes, A. J., Dillon, D. G., Goetz, E. L., Birk, J. L., Bogdan, R., et al. (2009). Reduced caudate and nucleus accumbens response to rewards in unmedicated individuals with major depressive disorder. Am. J. Psychiatr. 166, 702–710. doi: 10.1176/appi.ajp.2008.08081201
Pizzagalli, D. A., Iosifescu, D., Hallett, L. A., Ratner, K. G., and Fava, M. (2008). Reduced hedonic capacity in major depressive disorder: evidence from a probabilistic reward task. J. Psychiatr. Res. 43, 76–87. doi: 10.1016/j.jpsychires.2008.03.001
Platt, B., Campbell, C. A., James, A. C., Murphy, S. E., Cooper, M. J., and Lau, J. Y. F. (2015). Cognitive reappraisal of peer rejection in depressed versus non-depressed adolescents: functional connectivity differences. J. Psychiatr. Res. 61, 73–80. doi: 10.1016/j.jpsychires.2014.11.016
Raposa, E. B., Laws, H. B., and Ansell, E. B. (2016). Prosocial behavior mitigates the negative effects of stress in everyday life. Clin. Psychol. Sci. 4, 691–698. doi: 10.1177/2167702615611073
Reeck, C., Ames, D. R., and Ochsner, K. N. (2016). The social regulation of emotion: an integrative, cross-disciplinary model. Trends Cogn. Sci. 20, 47–63. doi: 10.1016/j.tics.2015.09.003
Robinson, O. J., Cools, R., Carlisi, C. O., Sahakian, B. J., and Drevets, W. C. (2012). Ventral striatum response during reward and punishment reversal learning in unmedicated major depressive disorder. Am. J. Psychiatr. 169, 152–159. doi: 10.1176/appi.ajp.2011.11010137
Rodríguez-Cano, E., Sarró, S., Monté, G. C., Maristany, T., Salvador, R., McKenna, P. J., et al. (2014). Evidence for structural and functional abnormality in the subgenual anterior cingulate cortex in major depressive disorder. Psychological Medicine 44, 3263–3273. doi: 10.1017/S0033291714000841
Rogers, A. (2017). Star neuroscientist tom Insel leaves the Google-spawned verily for… a startup? Wired. Science 5, 11–17. Available at: https://www.wired.com/2017/05/star-neuroscientist-tom-insel-leaves-google-spawned-verily-startup
Santini, Z. I., Koyanagi, A., Tyrovolas, S., Mason, C., and Haro, J. M. (2015). The association between social relationships and depression: a systematic review. J. Affect. Disord. 175, 53–65. doi: 10.1016/j.jad.2014.12.049
Santomauro, D. F., Mantilla Herrera, A. M., Shadid, J., Zheng, P., Ashbaugh, C., Pigott, D. M., et al. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet 398, 1700–1712. doi: 10.1016/S0140-6736(21)02143-7
Satici, S. A., Uysal, R., and Deniz, M. E. (2016). Linking social connectedness to loneliness: the mediating role of subjective happiness. Personal. Individ. Differ. 97, 306–310. doi: 10.1016/j.paid.2015.11.035
Saxe, R., Moran, J. M., Scholz, J., and Gabrieli, J. (2006). Overlapping and non-overlapping brain regions for theory of mind and self reflection in individual subjects. Soc. Cogn. Affect. Neurosci. 1, 229–234. doi: 10.1093/scan/nsl034
Schacter, H. L., and Margolin, G. (2019). When it feels good to give: depressive symptoms, daily prosocial behavior, and adolescent mood. Emotion 19, 923–927. doi: 10.1037/emo0000494
Schön, U.-K., Denhov, A., and Topor, A. (2009). Social relationships as a decisive factor in recovering from severe mental illness. Int. J. Soc. Psychiatry 55, 336–347. doi: 10.1177/0020764008093686
Schreiter, S., Pijnenborg, G. H. M., and aan het Rot, M. (2013). Empathy in adults with clinical or subclinical depressive symptoms. J. Affect. Disord. 150, 1–16. doi: 10.1016/j.jad.2013.03.009
Schurz, M., Radua, J., Aichhorn, M., Richlan, F., and Perner, J. (2014). Fractionating theory of mind: a meta-analysis of functional brain imaging studies. Neurosci. Biobehav. Rev. 42, 9–34. doi: 10.1016/j.neubiorev.2014.01.009
Shamay-Tsoory, S. G. (2011). The neural bases for empathy. Neuroscientist 17, 18–24. doi: 10.1177/1073858410379268
Shamay-Tsoory, S. G., Aharon-Peretz, J., and Perry, D. (2009). Two systems for empathy: A double dissociation between emotional and cognitive empathy in inferior frontal gyrus versus ventromedial prefrontal lesions. Brain 132, 617–627.
Shamay-Tsoory, S. G., Tomer, R., Goldsher, D., Berger, B. D., and Aharon-Peretz, J. (2004). Impairment in Cognitive and Affective Empathy in Patients with Brain Lesions: Anatomical and Cognitive Correlates. Journal of Clinical and Experimental Neuropsychology 26, 1113–1127. doi: 10.1080/13803390490515531
Sheline, Y. I., Barch, D. M., Donnelly, J. M., Ollinger, J. M., Snyder, A. Z., and Mintun, M. A. (2001). Increased amygdala response to masked emotional faces in depressed subjects resolves with antidepressant treatment: an fMRI study. Biol. Psychiatry 50, 651–658. doi: 10.1016/S0006-3223(01)01263-X
Sheppes, G., Suri, G., and Gross, J. J. (2015). Emotion regulation and psychopathology. Annu. Rev. Clin. Psychol. 11, 379–405. doi: 10.1146/annurev-clinpsy-032814-112739
Singewald, G. M., Rjabokon, A., Singewald, N., and Ebner, K. (2011). The modulatory role of the lateral septum on neuroendocrine and behavioral stress responses. Neuropsychopharmacology 36, 793–804. doi: 10.1038/npp.2010.213
Singh, M. K., and Gotlib, I. H. (2014). The neuroscience of depression: Implications for assessment and intervention. Behaviour Research and Therapy 62, 60–73. doi: 10.1016/j.brat.2014.08.008
Smoski, M. J., Labar, K. S., and Steffens, D. C. (2014). Relative effectiveness of reappraisal and distraction in regulating emotion in late-life depression. Am. J. Geriatr. Psychiatr. 22, 898–907. doi: 10.1016/j.jagp.2013.01.070
Streamer, L., Seery, M. D., Kondrak, C. L., Lamarche, V. M., and Saltsman, T. L. (2017). Not I, but she: the beneficial effects of self-distancing on challenge/threat cardiovascular responses. J. Exp. Soc. Psychol. 70, 235–241. doi: 10.1016/j.jesp.2016.11.008
Surguladze, S. A., Young, A. W., Senior, C., Brébion, G., Travis, M. J., and Phillips, M. L. (2004). Recognition accuracy and response bias to happy and sad facial expressions in patients with major depression. Neuropsychology 18, 212–218. doi: 10.1037/0894-4105.18.2.212
Suslow, T., Konrad, C., Kugel, H., Rumstadt, D., Zwitserlood, P., Schöning, S., et al. (2010). Automatic mood-congruent amygdala responses to masked facial expressions in major depression. Biol. Psychiatry 67, 155–160. doi: 10.1016/j.biopsych.2009.07.023
Tanna, V. J., and MacCann, C. (2022). I know you so I will regulate you: closeness but not target’s emotion type affects all stages of extrinsic emotion regulation. Emotion, Online ahead of print. doi: 10.1037/emo0001073
Teo, A. R., Choi, H., and Valenstein, M. (2013). Social relationships and depression: ten-year follow-up from a nationally representative study. PLoS One 8:e62396. doi: 10.1371/journal.pone.0062396
Trope, Y., and Liberman, N. (2010). Construal-level theory of psychological distance. Psychol. Rev. 117, 440–463. doi: 10.1037/a0018963
Truax, P. (2001). Review: group psychotherapy is effective for depression. Evid. Based Ment. Health 4:82. doi: 10.1136/ebmh.4.3.82
van Zoonen, K., Buntrock, C., Ebert, D. D., Smit, F., Reynolds, C. F., Beekman, A. T. F., et al. (2014). Preventing the onset of major depressive disorder: a meta-analytic review of psychological interventions. Int. J. Epidemiol. 43, 318–329. doi: 10.1093/ije/dyt175
Victor, T. A., Furey, M. L., Fromm, S. J., Öhman, A., and Drevets, W. C. (2010). Relationship between amygdala responses to masked faces and mood state and treatment in major depressive disorder. Arch. Gen. Psychiatry 67, 1128–1138. doi: 10.1001/archgenpsychiatry.2010.144
Volz, M., Voelkle, M. C., and Werheid, K. (2019). General self-efficacy as a driving factor of post-stroke depression: a longitudinal study. Neuropsychol. Rehabil. 29, 1426–1438. doi: 10.1080/09602011.2017.1418392
Walter, H., von Kalckreuth, A., Schardt, D., Stephan, A., Goschke, T., and Erk, S. (2009). The temporal dynamics of voluntary emotion regulation. PLoS One 4:e6726. doi: 10.1371/journal.pone.0006726
Wen, X., Liu, Y., Zhao, P., Liu, Z., Li, H., Li, W., et al. (2021). Disrupted communication of the temporoparietal junction in patients with major depressive disorder. Cogn. Affect. Behav. Neurosci. 21, 1276–1296. doi: 10.3758/s13415-021-00918-5
Will, G.-J., Rutledge, R. B., Moutoussis, M., and Dolan, R. J. (2017). Neural and computational processes underlying dynamic changes in self-esteem. elife 6:e28098. doi: 10.7554/eLife.28098
Williams, W. C., Morelli, S. A., Ong, D. C., and Zaki, J. (2018). Interpersonal emotion regulation: implications for affiliation, perceived support, relationships, and well-being. J. Pers. Soc. Psychol. 115, 224–254. doi: 10.1037/pspi0000132
Wilson, R. P., Colizzi, M., Bossong, M. G., Allen, P., Kempton, M., and Bhattacharyya, S. (2018). The neural substrate of reward anticipation in health: a meta-analysis of fMRI findings in the monetary incentive delay task. Neuropsychol. Rev. 28, 496–506. doi: 10.1007/s11065-018-9385-5
Zaki, J. (2020). Integrating empathy and interpersonal emotion regulation. Annu. Rev. Psychol. 71, 517–540. doi: 10.1146/annurev-psych-010419-050830
Zaki, J., and Craig Williams, W. (2013). Interpersonal emotion regulation. Emotion 13, 803–810. doi: 10.1037/a0033839
Keywords: extrinsic emotion regulation, depression, intrinsic emotion regulation, reward, empathy, neuroimaging
Citation: Massarwe A and Cohen N (2023) Understanding the benefits of extrinsic emotion regulation in depression. Front. Psychol. 14:1120653. doi: 10.3389/fpsyg.2023.1120653
Edited by:
Lu Hua Chen, Hong Kong Polytechnic University, Hong Kong SAR, ChinaReviewed by:
Carolyn MacCann, The University of Sydney, AustraliaYuki Nozaki, Konan University, Japan
Copyright © 2023 Massarwe and Cohen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Atheer Massarwe, m.atheer1996@gmail.com
 Atheer Massarwe
Atheer Massarwe Noga Cohen
Noga Cohen