- 1Department of Psychology, Brandenburg Medical School Theodor Fontane, Neuruppin, Germany
- 2Department of Hematology, Oncology, and Tumor Immunology, Charité – University Medicine Berlin, Berlin, Germany
- 3Agaplesion Bethanien Diakonie, Berlin, Germany
- 4Cardiology Department, Schlosspark-Klinik, Berlin, Germany
- 5Department of Pediatrics, Division of Oncology and Hematology, Charité – University Medicine Berlin, Berlin, Germany
- 6Department of Psychology, University of Cologne, Cologne, Germany
- 7Schloss Luetgenhof Hospital, Centre for Personal Medicine, Psychosomatics and Psychotherapy, Dassow, Germany
Objective: Although treatment adherence and lifestyle changes significantly improve the prognosis of cardiovascular disease, many patients do not comply with clinician recommendations. Personality functioning appears to be of importance and is hypothesized to be superior to symptom-based measures in explaining individual differences in non-adherence.
Methods: 194 cardiology inpatients (mean age = 70.6 years, 60% male) were assessed using self-report measures in a cross-sectional design. Patients were assessed using the short version of the Operationalized Psychodynamic Diagnosis Structure Questionnaire (OPD-SQS) to measure personality functioning, as well as the Childhood Trauma Screener (CTS), the Patient Health Questionnaire (PHQ-9) for symptoms of depression, and the Generalized Anxiety Disorder Scale-7 (GAD-7). To assess non-adherence we introduced a brief, novel scale.
Results: Non-adherence correlated significant with personality functioning (r = 0.325), childhood trauma (r = 0.204) and depressiveness (r = 0.225). In a stepwise multiple regression analysis with socio-demographic variables inputted into the model, higher deficits in personality functioning, higher levels of childhood trauma, and male gender were associated with non-adherence (adjusted R2 = 0.149, F(3,190) = 12.225, p < 0.01). Level of depressive symptoms, anxiety, age, education, and income showed no significant additional predictive value and were excluded from the model.
Conclusion: In cardiovascular disease, personality functioning, childhood trauma and male gender are associated with non-adherence and appear to be more important than symptom reports of depression and anxiety. This highlights the relevance of basic impairments in intra- and interpersonal functioning in chronic disease, where the patient’s adherence is central.
Introduction
Cardiovascular disease (CVD) is a major cause of premature death and disability throughout the world (Smith et al., 2012). Although the medical understanding of CVD and its treatment options have improved significantly in recent decades, secondary prevention has shown to be an indispensable factor in reducing the risk of CVD and its negative consequences (Bansilal et al., 2015). Secondary prevention involves consistently taking one’s medication on a daily basis, and substantial changes in lifestyle. The World Health Organization (WHO) recommends smoking cessation and dietary changes such as the following: Salt reduction, eating at least 400 g of fruits and vegetables and a range of whole grains and pulses daily, at least 30 min of moderate physical activity a day, loss of weight or obesity, and considerably reducing one’s alcohol intake. Recommendations also include medical treatment of hypertension, high levels of cholesterol, fasting blood glucose and risks of thrombosis (World Health Organization, 2007). A large meta-analysis revealed that only about 50% of cardiovascular patients adhered to the medication prescribed to prevent myocardial infarction (Naderi et al., 2012). Another study which examined lifestyle factors such as regular physical activity, healthy diet, non-smoking, and moderate alcohol consumption meanwhile found that only approximately one third of the patients were adherent to all their advised restrictions and lifestyle changes (Huy et al., 2010).
Such strikingly poor rates of adherence are concerning given the strong evidence that lifestyle and medication adherence is closely linked to the occurrence of cardiological diseases and their course. In a systematic review and meta-analysis of prospective epidemiological studies, poor adherence to vascular medication was found to be responsible for roughly 9% of all CVD events in Europe (Chowdhury et al., 2013). According to this meta-analysis, good adherence could lead to a 20% lower risk of CVD and a 35% reduction of all-cause mortality. Further, a healthy lifestyle seems to be associated with a 66% reduced risk for cardiovascular disease (Barbaresko et al., 2018). Although there is clear proof of the importance of adherence to lifestyle recommendations for patients with CVD, changing patients’ behavior seems to be very challenging (McAlister et al., 2001).
The reasons for poor adherence are complex and diverse (Bosworth et al., 2011). Many studies emphasized the role of mental health in adherence, mainly focusing on patients with depression and anxiety (Bane et al., 2006; Gentil et al., 2012; Dempe et al., 2013; Kretchy et al., 2014; Gathright et al., 2017; Penninx, 2017). However, the role of psychiatric disorders in cardiology patients’ adherence seems to be intricate. Several studies indicate the negative influence of depression on adherence in CVD patients (Carney et al., 1995; Rieckmann et al., 2006; Casey et al., 2008; Berntson et al., 2015; Goldstein et al., 2017; Okunrinboye et al., 2019), although one study has highlighted that milder forms of depression may not necessarily be related to decreased levels of medication adherence (Okunrinboye et al., 2019). A range of mediators of this process have been proposed (Gellad et al., 2009; Manning and Bettencourt, 2011; Osborn and Egede, 2012; Hilliard et al., 2015) [e.g., social support (Osborn and Egede, 2012)]. The relationship between anxiousness and the likelihood of adhering to treatment recommendations seems even more ambiguous (DiMatteo et al., 2000). While some studies highlighted a link between anxiety and non-adherence (Bautista et al., 2012), others only found minimal associations (Schweitzer et al., 2007). The regular occurrence of severe panic attacks might lower the ability to follow prescriptions, but there is good reason to assume that moderate levels of anxiety might also increase the likelihood of following medical recommendations. This might especially be the case if anxious beliefs involve health-related issues (Bellg, 2004). These inconsistencies may not just be explained by severity of anxiety or depression, but also by other factors that define heterogeneity within a given psychiatric diagnosis, such as personality functioning or personality disorders (e.g., Köhling et al., 2015). Specific personality disorders as well as dimensional measures of levels of personality are related to health-related outcomes (Dokucu and Cloninger, 2019; Sinnaeve et al., 2021). Deficits in personality functioning appear to have a negative impact on disease progression and adherence (Collier et al., 1999) in mental illness (bipolar disorder (Wagner-Skacel et al., 2020; Ortelbach et al., 2022); eating disorders (Rohde et al., 2019); personality disorders (Zimmermann et al., 2014); major depressive disorder (Zeeck et al., 2020) as well as cancer (Wynn, 2010; Di Mattei et al., 2018) and chronic physical illness (Leichter and Dreelin, 2005; Pollock-BarZiv and Davis, 2005; Moran et al., 2007; Lee et al., 2010). Only two studies have examined the influence of personality disorders on non-adherence in cardiovascular health to date (Suárez-Bagnasco et al., 2015; Hall et al., 2019), indeed despite knowledge that personality disorders are an important risk factor for health-related matters such as physical functioning, role limitations, fatigue, and pain (Powers and Oltmanns, 2012). Furthermore, personality disorders are linked to several variables concerning general health status (Soeteman et al., 2008; El-Gabalawy et al., 2010).
The paucity of research on personality disorders on CVD patients’ treatment adherence may be explained by the low occurrence rates of severe personality disorders in this population (Pérez-Piñar et al., 2016). However, there is good reason to assume that milder impairments of basic personality functions, such as difficulties with emotion regulation, impaired social functioning and interpersonal problems, are more prominent in this cohort and also lead to serious problems of physical well-being and health-related behaviors (Bach and Hutsebaut, 2018; Nelson et al., 2018). As suggested by the Alternative Model for the Assessment of Personality Disorders (AMPD) of the DSM-5 (Bender et al., 2011) or the upcoming model for ICD-11 (Tyrer et al., 2019), general personality functioning in terms of basic self- and other-related emotion processing and regulation allow for the inclusion of subclinical impairments.
In addition to the more recent developments from formal psychiatric diagnosis, the concept of personality functioning has a long tradition in for example psychodynamic or interpersonal theory (Hopwood, 2018; Ehrenthal and Benecke, 2019), and describes biographically evolved and persistent patterns of emotion, cognition, regulation, and behavior. These patterns are shaped by early relational experiences (Zimmermann et al., 2012). Conveniently, the psychodynamic concept of ego integration offers scope for examining even milder forms of impairment in basic personality functioning, which, as discussed, may serve to clarify fundamental and important mechanisms underpinning problems in patient adherence (e.g., medication refusal and refusal to adopt lifestyle recommendations). Its role in predicting the course and symptom severity of physical illness, as well as its processing, also seems significant (Ehrenthal et al., 2019) and may be especially important in chronic diseases that demand a particularly high level of compliance and lifestyle changes.
In a similar vein, childhood trauma – which, theoretically, is closely linked to personality functioning (de Carvalho et al., 2015) – has been proposed as an important risk factor in CVD (Rozanski et al., 2005). While there is some evidence that childhood trauma has an impact on medication adherence in HIV (Mugavero et al., 2006; Whetten et al., 2013; Willie et al., 2016), to our knowledge, no research is available to date for CVD. However, it seems likely that exposure to adverse experiences such as sexual, physical, or emotional abuse in childhood could lead to difficulties in self-care such as implementing complex behavioral changes (Prather and Golden, 2009), and perhaps also to negative interactions with healthcare providers (Green et al., 2012).
The current study aims to address the research question as to whether deficits in basic intrapersonal and social functioning, defined as personality functioning, and a history of childhood trauma are associated with a higher self-reported tendency of non-adherence to secondary prevention guideline recommendations in cardiology inpatients. Furthermore, we aim to investigate whether personality functioning and a history of childhood trauma are better at predicting non-adherence than (a) more symptom-based variables such as depression and anxiety, as well as (b) basic socio-economic characteristics.
Materials and Methods
Study Design and Recruitment
Between May 2019 and March 2020, we recruited participants on two wards in the cardiological inpatient unit of the Ruppiner Kliniken, a general hospital in northeast Germany. Due to the focus on secondary prevention, only patients with a history of cardiological disease were included in the study. These patients were informed about the study and after providing informed consent, they were asked to complete a self-report assessment. Demographic information was also collected (namely age, gender, education, relationship status, income). Medical parameters such as medical diagnoses, including coronary heart disease, arterial hypertension, hyperlipoproteinemia and diabetes, were extracted based on file review. Inclusion criteria were a history of cardiological disease, at least 18 years of age, and completion of the questionnaire battery.
Procedures
The local ethics committee of the Medical School Brandenburg – Theodor Fontane approved the study protocol.
Measurements
Patient Health Questionnaire
The Patient Health Questionnaire (PHQ-9) is a 9-question, self-report depression subscale of the PHQ (Kroenke et al., 2001). Each item is based on the DSM-IV criteria for depression and the questionnaire can be used to predict the severity of depression. Patients are required to assess depressive symptoms (e.g., “feeling down, depressed or hopeless”) over the last 2 weeks on a 4-point Likert scale (where 0 = not at all and 3 = nearly every day). A total score ranging between 0 and 27 is achieved by adding all item scores. Values from 0 to 4 indicate none/minimal symptoms, 5 to 9 is considered mild, 10 to 14 is moderate, 15 to 19 is moderately severe, and 20 to 27 represents severe symptoms. In general, a cutoff score of 11 is considered indicative of severe depressive symptoms. A recent study by Kroenke, Spitzer and Williams showed good internal consistency (Cronbach’s α = 0.89/0.86) and construct validity compared with the 20-Item Short Form Health Survey (SF-20) questionnaire as well as good criterion validity (Kroenke et al., 2010).
Generalized Anxiety Disorder Scale-7
In order to assess anxiety we used the Generalized Anxiety Disorder Scale-7 (GAD-7), a self-report questionnaire for screening and measurement of the severity of generalized anxiety disorder (Spitzer et al., 2006). It forms part of the PHQ-D and is reported to also measure other anxiety disorders including social phobia, post-traumatic stress disorder and panic disorder (Kroenke et al., 2007). The GAD-7 consists of seven items reflecting states over the past 2 weeks (e.g., “feeling afraid as if something awful might happen”). The instrument contains a 4-point Likert scale (where 0 = not at all and 3 = nearly every day). Total anxiety scores range from 0 to 21 (0–4 = minimal, 5–9 = mild, 10–14 = moderate, 15–21 = severe). The internal consistency is reported to be good (Cronbach’s α = 0.92) and validity has been proven (Löwe et al., 2008).
The Operationalized Psychodynamic Diagnosis Structure Questionnaire
Personality functioning was measured according to the Levels of Structural Integration Axis (LSIA) of the Operationalized Psychodynamic Diagnosis (OPD-2) (OPD Task Force, 2008), a multiaxial psychodynamic diagnosis system which has attained wide usage in Germany in the last 20 years for both diagnostic and treatment planning purposes (Cierpka et al., 2007). The OPD covers five axes: Illness experience and treatment assumptions, relationships, mental conflicts, and personality structure, i.e., levels of personality functioning. We used the short form of the OPD Structure Questionnaire (OPD-SQS) (Ehrenthal et al., 2012; Ehrenthal et al., 2015), a 12-item screening instrument where item scores range between 0 and 4, for example: “Sometimes my feelings are so intense that I get scared,” “I sometimes feel like a stranger to myself,” or “I sometimes misjudge how my behavior affects others.” A total score is computed and ranges from 0 (“indicating high levels of personality functioning”) to 48 (“indicating notable impairment of personality functioning”), whereby lower scores represent lower personality functioning. The internal consistency (α = 0.89) and validity have been confirmed (Ehrenthal et al., 2012; Obbarius et al., 2019), and the long version also correlated with the expert ratings of the personality functioning to r = 0.62 (Dinger et al., 2014).
Beyond the use of the overall scale, the developers propose three subscales for research questions that are highly correlated with one other: self-perception, contact formation and relationship model (Ehrenthal et al., 2012). While the self-perception subscale links structural aspects of the self with emotion regulation skills, the contact formation subscale links interactional skills with aspects of self-uncertainty. Thirdly, the relationship model subscale maps the representation of relationship experiences which, accordingly, are associated with expectations for new relationships (Obbarius et al., 2019).
Childhood Trauma Screener
The Childhood Trauma Screener (CTS, Grabe et al., 2012) is a brief version of the Childhood Trauma Questionnaire (CTQ) (Bernstein et al., 1997; Bernstein et al., 2003; Wingenfeld et al., 2010), an internationally used, short self-assessment procedure for the retrospective recording of various traumas in childhood, including emotional, physical and sexual abuse as well as emotional and physical neglect. The CTS consists of 5 items scaled from 1 (not at all) to 5 (very often), whereby every item corresponds to one scale of the larger CTQ. The total score is built by adding the values of all items leading to a score ranging from 5 to 25. Studies have found good psychometric properties of the instrument with an internal consistency of α = 0.76 and correlation of r = 0.88 between the total sum score of the CTS and the CTQ (Grabe et al., 2012).
Measuring Non-adherence
Due to the lack of existing questionnaires that cover the desired range of non-adherence, we created a three-item scale. It was operationalized as a self-assessed overall tendency not to start recommended treatments, to not implement recommended lifestyle changes, and to discontinue recommended treatment, using a single item for each, respectively. The participants could rate their tendency on a 4-point Likert scale ranging from 1 (not at all) to 4 (very much). We calculated the total score and found a rather low internal consistency of Cronbach’s α = 0.55.
Data Analysis
Statistical analysis and data preparation were carried out using IBM SPSS Statistics 27.
Results
Participants
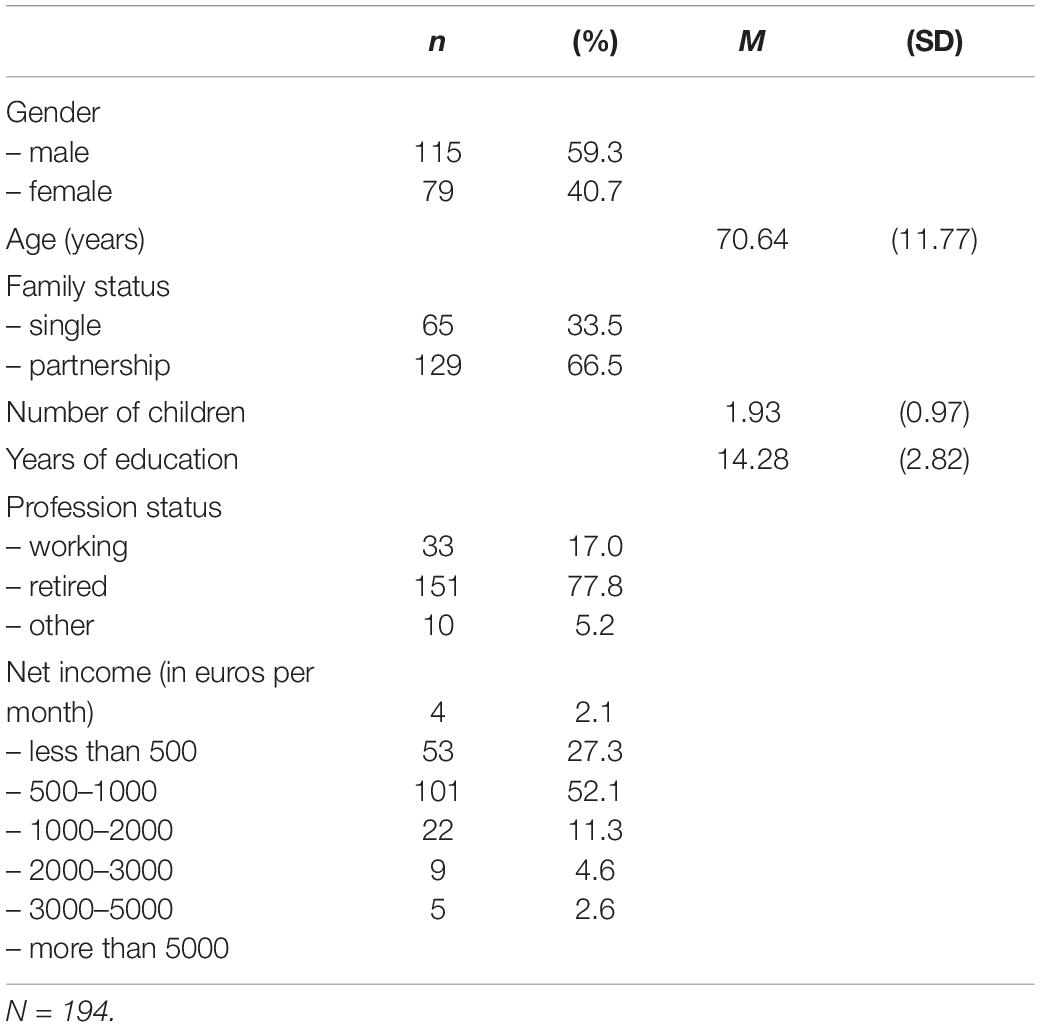
While data was collected for 218 patients, due to missing data the final analyses was based on 194 participants. Table 1 reports the sociodemographic variables.
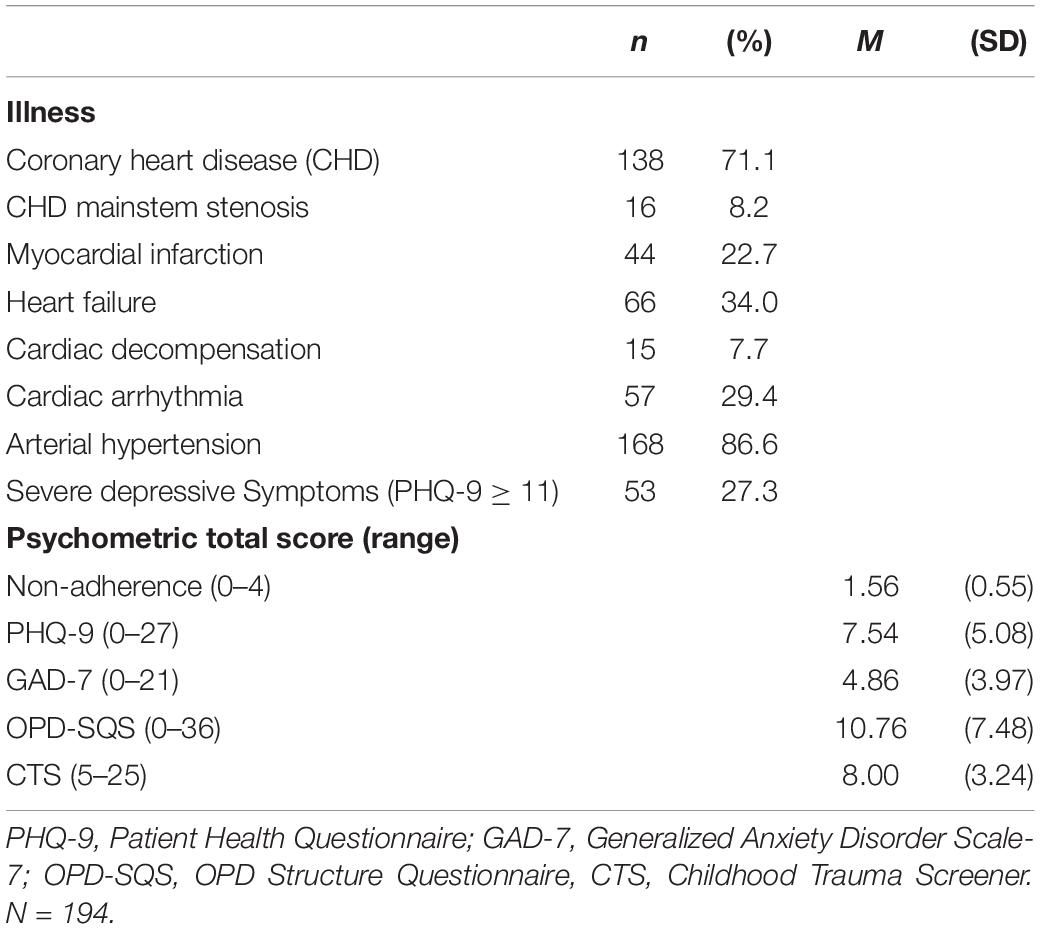
Table 2 presents the information regarding the participants’ somatic functioning and medical diagnoses. Limited information regarding mental illness was obtained from the file review. For this reason, we report the number of participants which had severe depressive symptoms based on the PHQ-9 [cut-off score of ≥11 as recommended by Gräfe et al. (2004)].
As summarized in Table 2, overall participants endorsed agreeing to implement recommendations. Overall, levels of depression and anxiety were mild in our participant group. Indeed, personality functioning as indicated by the OPD-SQS was generally in the low range indicating relatively high levels of personality functioning.
To examine whether the group of the 24 excluded participants differed significantly from the 194 included patients in the reported variables, t-tests and chi-square tests were conducted. Participants that were excluded due to missing data differed significantly in the frequency of CHD (94% in the excluded group vs 71% in the included group; p = 0.027). All other variables showed no significant differences.
Statistical Analysis
We hypothesized, and found evidence of, a statistically significant, positive relation between personality functioning (OPD-SQS) and non-adherence (r = 0.325, p < 0.001). Also, depressiveness and childhood trauma, respectively showed small but significant correlations with non-adherence (r = 0.225, p < 0.001); (r = 0.204, p < 0.001). According to conventional models of p-values, generalized anxiety was not significantly associated with self-reported non-adherence (r = 0.140, p < 0.051). To test for the influence of socio-demographic variables, we also included age, years of education and net monthly income, and found no connection to non-adherence. In addition, to control for possible gender differences, we conducted a t-test. The level of non-adherence differed statistically significant for men and women, t(192) = 2.095, p < 0.05.
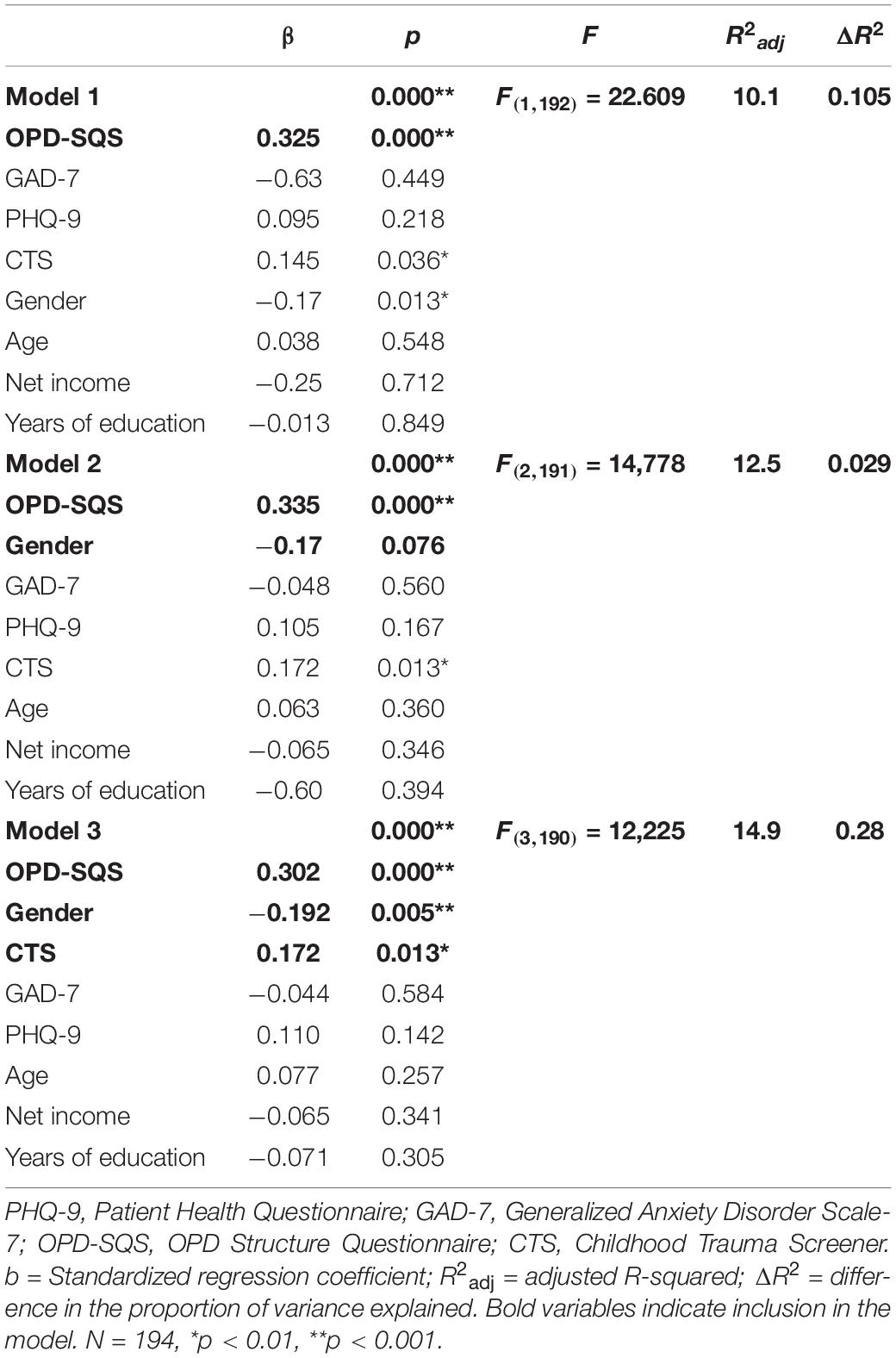
Stepwise multiple regression analysis was used to test if the reported variables significantly predict participants’ self-reported non-adherence. Table 3 shows the regression models with the three steps of variable inclusion. Model 3 indicates that the three predictors explained 14.9% of the variance (Adjusted R2 = 0.149, F(3,190) = 12.225, p < 0.01). It was found that levels of personality functioning (OPD-SQS) significantly predicted non-adherence (β = 0.33, p < 0.001), as did extent of childhood trauma (CTS) (β = 0.17, p < 0.05) and gender (β = −0.19, p < 0.05). Depressiveness (PHQ-9), generalized anxiety (GAD-7), age, years of education and net income showed no significant additional predictive value and were thus not considered any further for the model.
To investigate the relationship between personality functioning and self-reported non-adherence in more detail, we also calculated the subscales of the OPD-SQS. Internal consistency of all three subscales was acceptable with Cronbach’s α ranging from.685 to.699. Correlational analysis revealed small to moderate associations with non-adherence for all three subscales (self-perception, r = 0.213, p < 0.01); (contact formation, r = 0.267, p < 0.001); (relationship model, r = 0.305, p < 0.001).
Discussion
In our sample of 194 cardiology inpatients, stepwise multiple regression revealed personality functioning and childhood trauma as significant predictors of non-adherence. In contrast, levels of depression and anxiety were not predictive of non-adherence. 10% of the variance could be explained by levels of personality functioning alone (Adjusted R2 = 0.101, F(1,192) = 22.609, p < 0.001). When controlling for sociodemographic variables such as age, gender, net income, and years of education, only gender had a significant association with non-adherence with males identified as more likely not to comply with treatment recommendations. A lower level of personality functioning on the OPD-SQS, higher levels of childhood trauma, and male gender, were predictive of higher levels of non-adherence, explaining 15% of the variance in scores.
In addition, symptoms of depression and to a certain degree anxiety were observed to correlate with non-adherence, which is in line with previous studies (Ziegelstein et al., 2000; Kuhl et al., 2009). In our sample, anxiety showed a weaker, non-significant association with non-adherence compared with the results for depression. This could be explained by differences in prototypical psychopathology (World Health Organization, 2004). While anxiety is characterized by symptoms such as increased activation and agitation, depressive symptomatology is usually characterized by symptoms such as lack of motivation, low energy, limited ability to concentrate, and pessimistic beliefs about the future. As such, typical depressive symptoms are likely to be more related in content to non-adherence than those of anxiety. All the same, the clearest association occurred with personality functioning predicting non-adherence in the regression model. This finding is in support of our proposal that fundamental psychological features and abilities, as conceptualized in the framework of personality functioning (Ehrenthal et al., 2015), may play an essential role in adhering to lifestyle-related medical recommendations.
Which particular aspects of personality functioning are relevant in the context of non-adherence to chronic cardiac disease may be an important focus for future research. In our study, aspects of self-perception, contact formation, and relationship model had a significant positive correlation with non-adherence. The strongest correlation was shown with the relationship model subscale (r = 0.305), which points to the centrality of early shaped relational patterns in informing non-adherence; most likely played out in the clinician-patient relationship. Non-adherence most likely occurs against the backdrop of an interactional, relational event. On the OPD-SQS, the relationship dimension of personality functioning primarily maps the tendency of people to experience contact with others as threatening and uncontrollable (Ehrenthal et al., 2012). It is plausible therefore that such a personality effect could influence willingness or ability to make and uphold behavioral adaptations, whereby subclinical difficulties in experiencing the other person as trusting and helpful may lead to an increased tendency not to implement or to discontinue treatment recommendations. Accordingly, clinical implications of this may include scope for cardiologists to assess patient personality functioning earlier in treatment planning. This may enable clinicians to identify negative personality effects on adherence early and intervene appropriately, e.g., by lining up further multidisciplinary supports and liaising with psychology, psychosomatic medicine and psychiatry (Sudhir, 2017). In this vein, some possibilities may include providing training to clinicians on how to interact with such patients fruitfully, such as how to focus on problem behaviors without punishing; to involve mental health professionals at an early stage of treatment; to adopt regular staff meetings to liaise regarding patients; and to establish realistic expectations regarding patients’ capacity to implement their healthcare recommendations and indeed support them in achieving them (Peteet et al., 2011). In addition, several psychodynamic treatment approaches to enhance personality functioning have been developed (Kernberg et al., 2008; Bateman and Fonagy, 2013; Rudolf, 2020). Initial attempts have been made to implement such psychotherapy techniques to support adherence in the context of medical recommendations for chronic conditions by promoting a more accurate understanding of their mental state (Malberg, 2019). Further research is needed to derive more specific treatment recommendations from this.”
Our findings suggest that people who suffered trauma in childhood also have more difficulty adhering to medical recommendations. Several studies have shown that people with childhood trauma are more likely to develop insecure attachment styles, which are associated with difficulties in seeking help and maintaining stable relationships (Pearlman and Courtois, 2005; Clark et al., 2011; Millar et al., 2021) and other factors related to somatic medicine (Graetz et al., 2013; Graf et al., 2020; Graetz et al., 2021). Therapeutic alliance, a marker of a stable relationship, indeed appears to play an important role in adherence (Pringle and Fawcett, 2017). Individuals with a history of childhood trauma may be more likely to encounter challenges in trusting others, including their medical caregivers. Our findings point toward the value in identifying childhood trauma among CVD patients. In case of a trauma history, appropriate relational and rapport-based adjustments may be made to the clinical course, e.g., longer appointment durations during early treatment to facilitate trust, or the application of a greater focus on a person-centered approach.
Our results indicated that men tended to report higher levels of non-adherence than women. Interestingly, this contradicts other study findings on the role of gender in adherence (Vervloet et al., 2020), with several studies and reviews finding women to be more non-adherend to statins (Lewey et al., 2013; Ofori-Asenso et al., 2018; Ingersgaard et al., 2020), or indeed no such gender differences (Holmes et al., 2012; Holt et al., 2013). It seems likely that differences in medication adherence might be explained by variation in side effects, beliefs about drugs, and treatment recommendation by physicians (Vervloet et al., 2020). In contrast to medication adherence, women seem to be more willing to change their lifestyle (Jarbøl et al., 2017). This might explain why we found men to report higher levels of non-adherence, as we asked regarding the general tendency not to start recommended treatments, implement recommended lifestyle changes, and to discontinue recommended treatments. Our results highlight the general assumption in cardiology that gender differences in symptomatology, treatment options, adherence and perception by medical staff should be heeded and researched further (Möller-Leimkühler, 2007; Mosca et al., 2011; Goldstein et al., 2016).
In interpreting the findings of this study, we note several limitations. All variables were measured using self-report, and accordingly may be subject to recall bias or social desirability. All the same, in the case of non-adherence at least, the influence of social desirability on self-reported adherence has been proposed to be overestimated (Wagner and Miller, 2004). Several alternative approaches to measuring non-adherence have been developed (Vitolins et al., 2000), however, most are limited to assessing adherence to medication (e.g., electronic medication packaging (EMP) devices or medication counts) (Kronish et al., 2021). Other measurement methods directly capture clinical outcomes as an indicator of non-compliance, but are proposed to be confounded by various individual and disease-specific factors (Nguyen et al., 2014). As such, when it comes to identifying subjective burden of adhering to a large variety of different treatment recommendations, self-assessment appears to be a reliable and valid measurement approach, especially when it comes to identifying patient burden and their associated support needs. A reasonable approach for future research may therefore be to balance self-report scales with behavioral measures, such as nutrition or exercise diaries, that counteract possible recall biases (Nguyen et al., 2014; Anghel et al., 2019). The measurement of childhood trauma may also have been influenced by recall bias. Our sample is comparatively old (mean age = 70.6 years) and it is conceivable that memories of abusive experiences in childhood are biased due to cognitive impairment. We did not examine the patients for cognitive impairment ourselves but screened the patient files for clinical diagnosis and found no case of dementia or mild cognitive impairment in our sample. However, we acknowledge that it is possible that these diagnoses have been overlooked by cardiology colleagues. While we cannot completely rule out a possible recall bias, retrospective recording of ACEs seem comparatively reliable (Brewin et al., 1993; Hardt and Rutter, 2004) and has also been used in other studies with participants of advanced age (Felitti et al., 1998).
We note that our sample reported good overall personality functioning, with low personality functioning presenting rarely. However, this finding may be considered representative of the cardiology patient group as a whole. In comparison with other studies the picture that emerges is that the degree of mental illness seems to be related to the level of personality functioning. For example, diabetic patients show better scores in personality functioning (Ehrenthal et al., 2019) than patients who were in outpatient treatment for mental illness (Ehrenthal et al., 2012) and these in turn show better scores than patients who were in inpatient treatment for mental illness (Obbarius et al., 2019). We caution that a conclusive evaluation of personality functioning on the OPD-SQS is best achieved when conducted by a trained clinician as opposed to by self-report. This was beyond the scope of this study. However, on the basis that sufficient agreement between self-assessment and expert rating has been demonstrated (Dinger et al., 2014), we consider this self-report measure to have had good and sufficient reliability and validity overall.
Finally, although the psychodynamic concept of personality functioning makes theoretical assumptions about the early childhood development of these traits (Dagnino et al., 2020; Krakau et al., 2021), due to the cross-sectional design of the study we cannot make a clear statement about the causality of the associations between personality functioning and non-adherence. However, we collected data from a large and well-characterized clinical sample which serves as an important and appropriate first step in investigating associations between these variables. Future research should attempt to unpick a potential causal relationship and adopt a longitudinal design: For example, in investigating to what extent the level of personality functioning at initial diagnosis of a cardiological disease can predict the implementation of recommended medical measures across the treatment and clinical course. Another interesting question would be how stable personality functioning is over time. To examine these temporal relationships more closely would be an intriguing line of inquiry. Indeed, there are initial findings that show that the OPD-SQS is also suitable for measuring change in the context of psychotherapeutic treatment (Lübke et al., 2021).
Conclusion
Our findings highlight the role of personality functioning and trauma as important predictors of treatment adherence in cardiovascular disease, indeed to a greater extent than psychopathology symptoms (depression, anxiety) and demographic factors. The relevance of discrete and fundamental personality features, and their role in intra- and interpersonal functioning as reflected in the patient and care provider relationship, may be important in informing cardiological care given the centrality of lifestyle changes in preventative medical care and management of cardiovascular disease.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Medical School Brandenburg Theodor Fontane. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
KH, SF, IK, and JE contributed to the conception or design of the work. KH, SF, IK, and TS contributed to the acquisition and analysis or interpretation of data for the work. KH and SF drafted the manuscript. GO’M, TS, and JE critically revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
We acknowledge funding by the MHB Open Access Publication Fund supported by the German Research Association (DFG).
Conflict of Interest
SF was employed by the company Agaplesion Bethanien Diakonie.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank Lena Dschietzig, Anja Hummel, Johanna Seiffert, Stephan Müller, and Orcun Cinel for their assistance with data collection.
References
Anghel, L. A., Farcas, A. M., and Oprean, R. N. (2019). An overview of the common methods used to measure treatment adherence. Med. Pharm. Rep. 92, 117–122. doi: 10.15386/mpr-1201
Bach, B., and Hutsebaut, J. (2018). Level of Personality Functioning Scale–Brief Form 2.0: utility in capturing personality problems in psychiatric outpatients and incarcerated addicts. J. Pers. Assess. 100, 660–670. doi: 10.1080/00223891.2018.1428984
Bane, C., Hughes, C. M., and McElnay, J. C. (2006). The impact of depressive symptoms and psychosocial factors on medication adherence in cardiovascular disease. Patient Educ. Couns. 60, 187–193. doi: 10.1016/j.pec.2005.01.003
Bansilal, S., Castellano, J. M., and Fuster, V. (2015). Global burden of CVD: focus on secondary prevention of cardiovascular disease. Int. J. Cardiol. 201(Suppl. 1), S1–S7. doi: 10.1016/s0167-5273(15)31026-3
Barbaresko, J., Rienks, J., and Nöthlings, U. (2018). Lifestyle indices and cardiovascular disease risk: a meta-analysis. Am. J. Prev. Med. 55, 555–564. doi: 10.1016/j.amepre.2018.04.046
Bateman, A., and Fonagy, P. (2013). Mentalization-based treatment. Psychoanal. Inq. 33, 595–613. doi: 10.1080/07351690.2013.835170
Bautista, L. E., Vera-Cala, L. M., Colombo, C., and Smith, P. (2012). Symptoms of depression and anxiety and adherence to antihypertensive medication. Am. J. Hypertens. 25, 505–511. doi: 10.1038/ajh.2011.256
Bellg, A. J. (2004). “Clinical cardiac psychology,” in Clinical Handbook of Health Psychology: A Practical Guide to Effective Interventions, eds P. M. Camic and S. J. Knight (Ashland, OH: Hogrefe & Huber Publishers), 29–57.
Bender, D. S., Morey, L. C., and Skodol, A. E. (2011). Toward a model for assessing level of personality functioning in DSM–5, part I: a review of theory and methods. J. Pers. Assess. 93, 332–346. doi: 10.1080/00223891.2011.583808
Bernstein, D. P., Ahluvalia, T., Pogge, D., and Handelsman, L. (1997). Validity of the childhood trauma questionnaire in an adolescent psychiatric population. J. Am. Acad. Child Adolesc. Psychiatry 36, 340–348. doi: 10.1097/00004583-199703000-00012
Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., Ahluvalia, T., et al. (2003). Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl. 27, 169–190. doi: 10.1016/S0145-2134(02)00541-0
Berntson, J., Stewart, K. R., Vrany, E., Khambaty, T., and Stewart, J. C. (2015). Depressive symptoms and self-reported adherence to medical recommendations to prevent cardiovascular disease: NHANES 2005-2010. Soc. Sci. Med. 138, 74–81. doi: 10.1016/j.socscimed.2015.05.041
Bosworth, H. B., Granger, B. B., Mendys, P., Brindis, R., Burkholder, R., Czajkowski, S. M., et al. (2011). Medication adherence: a call for action. Am. Heart J. 162, 412–424. doi: 10.1016/j.ahj.2011.06.007
Brewin, C. R., Andrews, B., and Gotlib, I. H. (1993). Psychopathology and early experience: a reappraisal of retrospective reports. Psychol. Bull. 113, 82–98. doi: 10.1037/0033-2909.113.1.82
Carney, R. M., Freedland, K. E., Eisen, S. A., Rich, M. W., and Jaffe, A. S. (1995). Major depression and medication adherence in elderly patients with coronary artery disease. Health Psychol. 14, 88–90. doi: 10.1037/0278-6133.14.1.88
Casey, E., Hughes, J. W., Waechter, D., Josephson, R., and Rosneck, J. (2008). Depression predicts failure to complete phase-II cardiac rehabilitation. J. Behav. Med. 31, 421–431. doi: 10.1007/s10865-008-9168-1
Chowdhury, R., Khan, H., Heydon, E., Shroufi, A., Fahimi, S., Moore, C., et al. (2013). Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur. Heart J. 34, 2940–2948. doi: 10.1093/eurheartj/eht295
Cierpka, M., Grande, T., Rudolf, G., von der Tann, M., and Staschf, M. (2007). The operationalized psychodynamic diagnostics system: clinical relevance, reliability and validity. Psychopathology 40, 209–220. doi: 10.1159/000101363
Clark, L., Beesley, H., Holcombe, C., and Salmon, P. (2011). The influence of childhood abuse and adult attachment style on clinical relationships in breast cancer care. Gen. Hosp. Psychiatry 33, 579–586. doi: 10.1016/j.genhosppsych.2011.07.007
Collier, J. A., Nathanson, J. W., and Anderson, C. A. (1999). Personality functioning in adolescent heart transplant recipients. Clin. Child Psychol. Psychiatry 4, 367–377.
Dagnino, P., Ugarte, M. J., Morales, F., González, S., Saralegui, D., and Ehrenthal, J. C. (2020). Risk factors for adult depression: adverse childhood experiences and personality functioning. Front. Psychol. 11:594698. doi: 10.3389/fpsyg.2020.594698
de Carvalho, H. W., Pereira, R., Frozi, J., Bisol, L. W., Ottoni, G. L., and Lara, D. R. (2015). Childhood trauma is associated with maladaptive personality traits. Child Abuse Negl. 44, 18–25. doi: 10.1016/j.chiabu.2014.10.013
Dempe, C., Jünger, J., Hoppe, S., Katzenberger, M.-L., Möltner, A., Ladwig, K.-H., et al. (2013). Association of anxious and depressive symptoms with medication nonadherence in patients with stable coronary artery disease. J. Psychosom. Res. 74, 122–127. doi: 10.1016/j.jpsychores.2012.12.003
Di Mattei, V. E., Mazzetti, M., Taranto, P., Bernardi, M., and Carnelli, L. (2018). Personality disorders: the missing diagnosis in psycho-oncology? Clin. Neuropsychiatry 15, 258–271.
DiMatteo, M. R., Lepper, H. S., and Croghan, T. W. (2000). Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch. Intern. Med. 160, 2101–2107. doi: 10.1001/archinte.160.14.2101
Dinger, U., Schauenburg, H., Hörz, S., Rentrop, M., Komo-Lang, M., Klinkerfuß, M., et al. (2014). Self-report and observer ratings of personality functioning: a study of the OPD system. J. Pers. Assess. 96, 220–225. doi: 10.1080/00223891.2013.828065
Dokucu, M. E., and Cloninger, C. R. (2019). Personality disorders and physical comorbidities: a complex relationship. Curr. Opin. Psychiatry 32, 435–441. doi: 10.1097/yco.0000000000000536
Ehrenthal, J. C., and Benecke, C. (2019). “Chapter 15 – Tailored treatment planning for individuals with personality disorders: the Operationalized Psychodynamic Diagnosis (OPD) approach,” in Case Formulation for Personality Disorders, ed. U. Kramer (Cambridge, MA: Academic Press), 291–314.
Ehrenthal, J. C., Dinger, U., Horsch, L., Komo-Lang, M., Klinkerfuss, M., Grande, T., et al. (2012). [The OPD Structure Questionnaire (OPD-SQ): first results on reliability and validity]. Psychother. Psychosom. Med. Psychol. 62, 25–32. doi: 10.1055/s-0031-1295481
Ehrenthal, J. C., Dinger, U., Schauenburg, H., Horsch, L., Dahlbender, R. W., and Gierk, B. (2015). Development of a 12-item version of the OPD-Structure Questionnaire (OPD-SQS). Z. Psychosom. Med. Psychother. 61, 262–274. doi: 10.13109/zptm.2015.61.3.262
Ehrenthal, J. C., Düx, A., Baie, L., and Burgmer, M. (2019). Levels of personality functioning and not depression predict decline of plasma glucose concentration in patients with type 2 diabetes mellitus. Diabetes Res. Clin. Pract. 151, 106–113. doi: 10.1016/j.diabres.2019.04.011
El-Gabalawy, R., Katz, L. Y., and Sareen, J. (2010). Comorbidity and associated severity of borderline personality disorder and physical health conditions in a nationally representative sample. Psychosom. Med. 72, 641–647. doi: 10.1097/PSY.0b013e3181e10c7b
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) study. Am. J. Prev. Med. 14, 245–258. doi: 10.1016/s0749-3797(98)00017-8
Gathright, E. C., Dolansky, M. A., Gunstad, J., Redle, J. D., Josephson, R. A., Moore, S. M., et al. (2017). The impact of medication nonadherence on the relationship between mortality risk and depression in heart failure. Health Psychol. 36, 839–847. doi: 10.1037/hea0000529
Gellad, W. F., Grenard, J., and McGlynn, E. A. (2009). A Review of Barriers to Medication Adherence: a Framework for Driving Policy Options. Santa Monica, CA: RAND.
Gentil, L., Vasiliadis, H. M., Préville, M., Bossé, C., and Berbiche, D. (2012). Association between depressive and anxiety disorders and adherence to antihypertensive medication in community-living elderly adults. J. Am. Geriatr. Soc. 60, 2297–2301. doi: 10.1111/j.1532-5415.2012.04239.x
Goldstein, C. M., Gathright, E. C., and Garcia, S. (2017). Relationship between depression and medication adherence in cardiovascular disease: the perfect challenge for the integrated care team. Patient Prefer. Adherence 11, 547–559. doi: 10.2147/PPA.S127277
Goldstein, K. M., Zullig, L. L., Bastian, L. A., and Bosworth, H. B. (2016). Statin adherence: does gender matter? Curr. Atheroscler. Rep. 18:63. doi: 10.1007/s11883-016-0619-9
Grabe, H. J., Schulz, A., Schmidt, C. O., Appel, K., Driessen, M., Wingenfeld, K., et al. (2012). [A brief instrument for the assessment of childhood abuse and neglect: the childhood trauma screener (CTS)]. Psychiatr. Prax. 39, 109–115. doi: 10.1055/s-0031-1298984
Graetz, C., Ehrenthal, J. C., Senf, D., Semar, K., Herzog, W., and Dörfer, C. E. (2013). Influence of psychological attachment patterns on periodontal disease – a pilot study with 310 compliant patients. J. Clin. Periodontol. 40, 1087–1094. doi: 10.1111/jcpe.12159
Graetz, C., Woeste, S., Mrowietz, U., and Ehrenthal, J. C. (2021). The impact of psychological attachment on the relationship between periodontal health and dental fear in patients with versus without psoriasis: a questionnaire-based, cross-sectional study. BMC Oral Health 21:95. doi: 10.1186/s12903-021-01457-8
Graf, J., Junne, F., Ehrenthal, J. C., Schäffeler, N., Schwille-Kiuntke, J., Stengel, A., et al. (2020). Unmet supportive care needs among women with breast and gynecological cancer: relevance of attachment anxiety and psychological distress. Front. Psychol. 11:558190. doi: 10.3389/fpsyg.2020.558190
Gräfe, K., Zipfel, S., Herzog, W., and Löwe, B. (2004). Screening psychischer Störungen mit dem “Gesundheitsfragebogen für Patienten (PHQ-D)”. Diagnostica 50, 171–181. doi: 10.1026/0012-1924.50.4.171
Green, B. L., Kaltman, S. I., Chung, J. Y., Holt, M. P., Jackson, S., and Dozier, M. (2012). Attachment and health care relationships in low-income women with trauma histories: a qualitative study. J. Trauma Dissoc. 13, 190–208. doi: 10.1080/15299732.2012.642761
Hall, K., Barnicot, K., Crawford, M., and Moran, P. (2019). A systematic review of interventions aimed at improving the cardiovascular health of people diagnosed with personality disorders. Soc. Psychiatry Psychiatr. Epidemiol. 54, 897–904. doi: 10.1007/s00127-019-01705-x
Hardt, J., and Rutter, M. (2004). Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J. Child Psychol. Psychiatry 45, 260–273. doi: 10.1111/j.1469-7610.2004.00218.x
Hilliard, M. E., Eakin, M. N., Borrelli, B., Green, A., and Riekert, K. A. (2015). Medication beliefs mediate between depressive symptoms and medication adherence in cystic fibrosis. Health Psychol. 34, 496–504. doi: 10.1037/hea0000136
Holmes, H. M., Luo, R., Hanlon, J. T., Elting, L. S., Suarez-Almazor, M., and Goodwin, J. S. (2012). Ethnic disparities in adherence to antihypertensive medications of medicare part D beneficiaries. J. Am. Geriatr. Soc. 60, 1298–1303. doi: 10.1111/j.1532-5415.2012.04037.x
Holt, E., Joyce, C., Dornelles, A., Morisky, D., Webber, L. S., Muntner, P., et al. (2013). Sex differences in barriers to antihypertensive medication adherence: findings from the cohort study of medication adherence among older adults. J. Am. Geriatr. Soc. 61, 558–564. doi: 10.1111/jgs.12171
Hopwood, C. J. (2018). Interpersonal dynamics in personality and personality disorders. Eur. J. Pers. 32, 499–524. doi: 10.1002/per.2155
Huy, C., Thiel, A., Diehm, C., and Schneider, S. (2010). [Deficits in adherence on all levels. Current need of interventions in primary, secondary, and tertiary prevention of cardiovascular diseases]. Dtsch. Med. Wochenschr. 135, 2119–2124. doi: 10.1055/s-0030-1267489
Ingersgaard, M. V., Andersen, T. H., Norgaard, O., Grabowski, D., and Olesen, K. (2020). Reasons for nonadherence to statins–a systematic review of reviews. Patient Prefer. Adherence 14, 675–691. doi: 10.2147/PPA.S245365
Jarbøl, D. E., Larsen, P. V., Gyrd-Hansen, D., Søndergaard, J., Brandt, C., Leppin, A., et al. (2017). Determinants of preferences for lifestyle changes versus medication and beliefs in ability to maintain lifestyle changes. A population-based survey. Prev. Med. Rep. 6, 66–73. doi: 10.1016/j.pmedr.2017.02.010
Kernberg, O. F., Yeomans, F. E., Clarkin, J. F., and Levy, K. N. (2008). Transference focused psychotherapy: overview and update. Int. J. Psychoanal. 89, 601–620. doi: 10.1111/j.1745-8315.2008.00046.x
Köhling, J., Ehrenthal, J. C., Levy, K. N., Schauenburg, H., and Dinger, U. (2015). Quality and severity of depression in borderline personality disorder: a systematic review and meta-analysis. Clin. Psychol. Rev. 37, 13–25. doi: 10.1016/j.cpr.2015.02.002
Krakau, L., Tibubos, A. N., Beutel, M. E., Ehrenthal, J. C., Gieler, U., and Brähler, E. (2021). Personality functioning as a mediator of adult mental health following child maltreatment. J. Affect. Disord. 291, 126–134. doi: 10.1016/j.jad.2021.05.006
Kretchy, I. A., Owusu-Daaku, F. T., and Danquah, S. A. (2014). Mental health in hypertension: assessing symptoms of anxiety, depression and stress on anti-hypertensive medication adherence. Int. J. Ment. Health Syst. 8:25. doi: 10.1186/1752-4458-8-25
Kroenke, K., Spitzer, R. L., and Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x
Kroenke, K., Spitzer, R. L., Williams, J. B., and Löwe, B. (2010). The Patient Health Questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen. Hosp. Psychiatry 32, 345–359. doi: 10.1016/j.genhosppsych.2010.03.006
Kroenke, K., Spitzer, R. L., Williams, J. B., Monahan, P. O., and Löwe, B. (2007). Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 146, 317–325. doi: 10.7326/0003-4819-146-5-200703060-00004
Kronish, I. M., Thorpe, C. T., and Voils, C. I. (2021). Measuring the multiple domains of medication nonadherence: findings from a Delphi survey of adherence experts. Transl. Behav. Med. 11, 104–113. doi: 10.1093/tbm/ibz133
Kuhl, E. A., Fauerbach, J. A., Bush, D. E., and Ziegelstein, R. C. (2009). Relation of anxiety and adherence to risk-reducing recommendations following myocardial infarction. Am. J. Cardiol. 103, 1629–1634. doi: 10.1016/j.amjcard.2009.02.014
Lee, H. B., Bienvenu, O. J., Cho, S.-J., Ramsey, C. M., Bandeen-Roche, K., Eaton, W. W., et al. (2010). Personality disorders and traits as predictors of incident cardiovascular disease: findings from the 23-year follow-up of the Baltimore ECA study. Psychosomatics 51, 289–296. doi: 10.1016/S0033-3182(10)70699-X
Leichter, S. B., and Dreelin, E. (2005). Borderline personality disorder and diabetes: a potentially ominous mix. Clin. Diabetes 23, 101–103. doi: 10.2337/diaclin.23.3.101
Lewey, J., Shrank, W. H., Bowry, A. D., Kilabuk, E., Brennan, T. A., and Choudhry, N. K. (2013). Gender and racial disparities in adherence to statin therapy: a meta-analysis. Am. Heart J. 165, 665–678.e1. doi: 10.1016/j.ahj.2013.02.011
Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., et al. (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care 46, 266–274. doi: 10.1097/MLR.0b013e318160d093
Lübke, L., Flemming, E., Mestel, R., Masuhr, O., Jaeger, U., and Spitzer, C. (2021). [Measurement of change with the short form of the OPD Structure Questionnaire (OPD-SQS)]. Psychother. Psychosom. Med. Psychol. 71, 456–463. doi: 10.1055/a-1425-7618
Malberg, N. T. (2019). “Psychodynamic intervention in an inpatient medical setting,” in Contemporary Psychodynamic Psychotherapy, eds J. Ogrodniczuk and D. Kealy (New York, NY: Elsevier), 395–407.
Manning, M., and Bettencourt, B. A. (2011). Depression and medication adherence among breast cancer survivors: bridging the gap with the theory of planned behaviour. Psychol. Health 26, 1173–1187. doi: 10.1080/08870446.2010.542815
McAlister, F. A., Lawson, F. M., Teo, K. K., and Armstrong, P. W. (2001). Randomised trials of secondary prevention programmes in coronary heart disease: systematic review. BMJ 323, 957–962. doi: 10.1136/bmj.323.7319.957
Millar, H. C., Lorber, S., Vandermorris, A., Thompson, G., Thompson, M., Allen, L., et al. (2021). “No, you need to explain what you are doing”: obstetric care experiences and preferences of adolescent mothers with a history of childhood trauma. J. Pediatr. Adolesc. Gynecol. 34, 538–545. doi: 10.1016/j.jpag.2021.01.006
Möller-Leimkühler, A. M. (2007). Gender differences in cardiovascular disease and comorbid depression. Dialogues Clin. Neurosci. 9, 71–83. doi: 10.31887/DCNS.2007.9.1/ammoeller
Moran, P., Stewart, R., Brugha, T., Bebbington, P., Bhugra, D., Jenkins, R., et al. (2007). Personality disorder and cardiovascular disease: results from a national household survey. J. Clin. Psychiatry 68, 69–74. doi: 10.4088/JCP.v68n0109
Mosca, L., Barrett-Connor, E., and Kass Wenger, N. (2011). Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation 124, 2145–2154. doi: 10.1161/CIRCULATIONAHA.110.968792
Mugavero, M., Ostermann, J., Whetten, K., Leserman, J., Swartz, M., Stangl, D., et al. (2006). Barriers to antiretroviral adherence: the importance of depression, abuse, and other traumatic events. AIDS Patient Care STDS 20, 418–428. doi: 10.1089/apc.2006.20.418
Naderi, S. H., Bestwick, J. P., and Wald, D. S. (2012). Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am. J. Med. 125, 882–887.e1. doi: 10.1016/j.amjmed.2011.12.013
Nelson, S. M., Huprich, S. K., Meehan, K. B., Siefert, C., Haggerty, G., Sexton, J., et al. (2018). Convergent and discriminant validity and utility of the DSM-5 Levels of Personality Functioning Questionnaire (DLOPFQ): associations with medical health care provider ratings and measures of physical health. J. Pers. Assess. 100, 671–679. doi: 10.1080/00223891.2018.1492415
Nguyen, T. M. U., Caze, A. L., and Cottrell, N. (2014). What are validated self-report adherence scales really measuring?: A systematic review. Br. J. Clin. Pharmacol. 77, 427–445. doi: 10.1111/bcp.12194
Obbarius, A., Obbarius, N., Fischer, F., Liegl, G., and Rose, M. (2019). [Evaluation of factor structure and construct validity of the 12-item short version of the OPD Structure Questionnaire (OPD-SQS) in psychosomatic patients]. Psychother. Psychosom. Med. Psychol. 69, 38–48. doi: 10.1055/s-0043-125394
Ofori-Asenso, R., Jakhu, A., Curtis, A. J., Zomer, E., Gambhir, M., Jaana Korhonen, M., et al. (2018). A systematic review and meta-analysis of the factors associated with nonadherence and discontinuation of statins among people aged≥ 65 years. J. Gerontol. Ser. A 73, 798–805. doi: 10.1093/gerona/glx256
Okunrinboye, H. I., Otakpor, A. N., and Ilesanmi, O. S. (2019). Depression and medication-adherence in patients with hypertension attending a tertiary health facility in South-West Nigeria. Pan Afr. Med. J. 33:27. doi: 10.11604/pamj.2019.33.27.12941
OPD Task Force (2008). Operationalized Psychodynamic Diagnosis OPD-2: Manual of Diagnosis and Treatment Planning. Göttingen: Hogrefe Publishing.
Ortelbach, N., Rote, J., Dingelstadt, A. M. L., Stolzenburg, A., Koenig, C., O’Malley, G., et al. (2022). The big five model in bipolar disorder: a latent profile analysis and its impact on longterm illness severity. Int. J. Bipolar Disord. 10, 1–10. doi: 10.1186/s40345-021-00248-y
Osborn, C. Y., and Egede, L. E. (2012). The relationship between depressive symptoms and medication nonadherence in type 2 diabetes: the role of social support. Gen. Hosp. Psychiatry 34, 249–253. doi: 10.1016/j.genhosppsych.2012.01.015
Pearlman, L. A., and Courtois, C. A. (2005). Clinical applications of the attachment framework: relational treatment of complex trauma. J. Traum. Stress 18, 449–459. doi: 10.1002/jts.20052
Penninx, B. W. (2017). Depression and cardiovascular disease: epidemiological evidence on their linking mechanisms. Neurosci. Biobehav. Rev. 74(Pt B), 277–286. doi: 10.1016/j.neubiorev.2016.07.003
Pérez-Piñar, M., Mathur, R., Foguet, Q., Ayis, S., Robson, J., and Ayerbe, L. (2016). Cardiovascular risk factors among patients with schizophrenia, bipolar, depressive, anxiety, and personality disorders. Eur. Psychiatry 35, 8–15. doi: 10.1016/j.eurpsy.2016.02.004
Peteet, J. R., Meyer, F. L., and Miovic, M. K. (2011). Possibly impossible patients: management of difficult behavior in oncology outpatients. J. Oncol. Pract. 7, 242–246. doi: 10.1200/JOP.2010.000122
Pollock-BarZiv, S. M., and Davis, C. (2005). Personality factors and disordered eating in young women with type 1 diabetes mellitus. Psychosomatics 46, 11–18. doi: 10.1176/appi.psy.46.1.11
Powers, A. D., and Oltmanns, T. F. (2012). Personality disorders and physical health: a longitudinal examination of physical functioning, healthcare utilization, and health-related behaviors in middle-aged adults. J. Pers. Disord. 26, 524–538. doi: 10.1521/pedi.2012.26.4.524
Prather, W., and Golden, J. A. (2009). A behavioral perspective of childhood trauma and attachment issues: toward alternative treatment approaches for children with a history of abuse. Int. J. Behav. Consult. Ther. 5, 56–74. doi: 10.1037/h0100872
Pringle, J., and Fawcett, J. (2017). “Facilitating the therapeutic alliance between pharmacists and patients to improve medication adherence,” in Feedback-Informed Treatment in Clinical Practice: Reaching for Excellence, eds D. S. Prescott, C. L. Maeschalck, and S. D. Miller (Washington, DC: American Psychological Association), 299–320. doi: 10.1017/S0033291709991553
Rieckmann, N., Kronish, I. M., Haas, D., Gerin, W., Chaplin, W. F., Burg, M. M., et al. (2006). Persistent depressive symptoms lower aspirin adherence after acute coronary syndromes. Am. Heart J. 152, 922–927. doi: 10.1016/j.ahj.2006.05.014
Rohde, J., Hofmann, T., Voigt, B., Rose, M., and Obbarius, A. (2019). Measurement of personality structure by the OPD structure questionnaire can help to discriminate between subtypes of eating-disorders. Front. Psychol. 10:2326. doi: 10.3389/fpsyg.2019.02326
Rozanski, A., Blumenthal, J. A., Davidson, K. W., Saab, P. G., and Kubzansky, L. (2005). The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J. Am. Coll. Cardiol. 45, 637–651. doi: 10.1016/j.jacc.2004.12.005
Rudolf, G. (2020). Strukturbezogene Psychotherapie: Leitfaden zur Psychodynamischen Therapie Struktureller Störungen. Stuttgart: Schattauer Verlag.
Schweitzer, R. D., Head, K., and Dwyer, J. W. (2007). Psychological factors and treatment adherence behavior in patients with chronic heart failure. J. Cardiovasc. Nurs. 22, 76–83. doi: 10.1097/00005082-200701000-00012
Sinnaeve, R., Vaessen, T., van Diest, I., Myin-Germeys, I., van den Bosch, L. M. C., Vrieze, E., et al. (2021). Investigating the stress-related fluctuations of level of personality functioning: a critical review and agenda for future research. Clin. Psychol. Psychother. 28, 1181–1193. doi: 10.1002/cpp.2566
Smith, S. C. Jr., Collins, A., Ferrari, R., Holmes, D. R. Jr., Logstrup, S., McGhie, D. V., et al. (2012). Our time: a call to save preventable death from cardiovascular disease (heart disease and stroke). Glob. Heart 7, 297–305. doi: 10.1016/j.gheart.2012.08.002
Soeteman, D. I., Verheul, R., and Busschbach, J. J. (2008). The burden of disease in personality disorders: diagnosis-specific quality of life. J. Pers. Disord. 22, 259–268. doi: 10.1521/pedi.2008.22.3.259
Spitzer, R. L., Kroenke, K., Williams, J. B., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166, 1092–1097. doi: 10.1001/archinte.166.10.1092
Suárez-Bagnasco, M., Brandani, M., Lobo, M., Masson, W., Peressotti, B., Jorge, N., et al. (2015). Psychosocial risk factors and personality disorders in outpatient cardiology setting. Int. Cardiovasc. Forum J. 3, 26–31. doi: 10.17987/icfj.v3i0.91
Sudhir, P. M. (2017). Advances in psychological interventions for lifestyle disorders: overview of interventions in cardiovascular disorder and type 2 diabetes mellitus. Curr. Opin. Psychiatry 30, 346–351. doi: 10.1097/YCO.0000000000000348
Tyrer, P., Mulder, R., Kim, Y.-R., and Crawford, M. J. (2019). The development of the ICD-11 classification of personality disorders: an amalgam of science, pragmatism, and politics. Annu. Rev. Clin. Psychol. 15, 481–502. doi: 10.1146/annurev-clinpsy-050718-095736
Vervloet, M., Korevaar, J. C., Leemrijse, C. J., Paget, J., Zullig, L. L., and van Dijk, L. (2020). Interventions to improve adherence to cardiovascular medication: what about gender differences? A systematic literature review. Patient Prefer. Adherence 14, 2055–2070. doi: 10.2147/PPA.S260562
Vitolins, M. Z., Rand, C. S., Rapp, S. R., Ribisl, P. M., and Sevick, M. A. (2000). Measuring adherence to behavioral and medical interventions. Control. Clin. Trials 21(Suppl. 5), S188–S194. doi: 10.1016/s0197-2456(00)00077-5
Wagner, G., and Miller, L. G. (2004). Is the influence of social desirability on patients’ self-reported adherence overrated? J. Acquir. Immune Defic. Syndr. 35, 203–204. doi: 10.1097/00126334-200402010-00016
Wagner-Skacel, J., Bengesser, S., Dalkner, N., Mörkl, S., Painold, A., Hamm, C., et al. (2020). Personality structure and attachment in bipolar disorder. Front. Psychiatry 11:410. doi: 10.3389/fpsyt.2020.00410
Whetten, K., Shirey, K., Pence, B. W., Yao, J., Thielman, N., Whetten, R., et al. (2013). Trauma history and depression predict incomplete adherence to antiretroviral therapies in a low income country. PLoS One 8:e74771. doi: 10.1371/journal.pone.0074771
Willie, T. C., Overstreet, N. M., Sullivan, T. P., Sikkema, K. J., and Hansen, N. B. (2016). Barriers to HIV medication adherence: examining distinct anxiety and depression symptoms among women living with HIV who experienced childhood sexual abuse. Behav. Med. 42, 120–127. doi: 10.1080/08964289.2015.1045823
Wingenfeld, K., Spitzer, C., Mensebach, C., Grabe, H. J., Hill, A., Gast, U., et al. (2010). The German version of the Childhood Trauma Questionnaire (CTQ): preliminary psychometric properties. Psychother. Psychosom. Med. Psychol. 60, 442–450. doi: 10.1055/s-0030-1247564
World Health Organization (2004). The International Statistical Classification of Diseases and Health Related Problems ICD-10: Tenth Revision. Geneva: World Health Organization.
World Health Organization (2007). Prevention of Cardiovascular Disease: Guideline for Assessment and Management of Cardiovascular Risk. Geneva: World Health Organization.
Wynn, J. D. (2010). “Difficult personality traits and disorders in oncology,” in Psycho-Oncology, eds J. C. Holland, W. S. Breitbart, P. B. Jacobsen, M. S. Lederberg, M. J. Loscalzo, and R. McCorkle (Oxford: Oxford University Press), 369–377. doi: 10.1093/med/9780199363315.003.0045
Zeeck, A., von Wietersheim, J., Weiss, H., Hermann, S., Endorf, K., Lau, I., et al. (2020). Self-criticism and personality functioning predict patterns of symptom change in major depressive disorder. Front. Psychiatry 11:147. doi: 10.3389/fpsyt.2020.00147
Ziegelstein, R. C., Fauerbach, J. A., Stevens, S. S., Romanelli, J., Richter, D. P., and Bush, D. E. (2000). Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Arch. Intern. Med. 160, 1818–1823. doi: 10.1001/archinte.160.12.1818
Zimmermann, J., Dahlbender, R. W., Herbold, W., Krasnow, K., Turrion, C. M., Zika, M., et al. (2014). The OPD structure questionnaire captures the general features of personality disorder. Psychother. Psychosom. Med. Psychol. 65, 81–83. doi: 10.1055/s-0034-1395626
Keywords: adherence, cardiology, childhood trauma, personality functioning, psychodynamic, secondary prevention
Citation: Haller K, Fritzsche S, Kruse I, O’Malley G, Ehrenthal JC and Stamm T (2022) Associations Between Personality Functioning, Childhood Trauma and Non-adherence in Cardiovascular Disease: A Psychodynamically-Informed Cross-Sectional Study. Front. Psychol. 13:913081. doi: 10.3389/fpsyg.2022.913081
Received: 05 April 2022; Accepted: 06 June 2022;
Published: 23 June 2022.
Edited by:
M. Graça Pereira, University of Minho, PortugalReviewed by:
Mattia Giuliani, San Raffaele Hospital (IRCCS), ItalyZaiquan Dong, Sichuan University, China
Copyright © 2022 Haller, Fritzsche, Kruse, O’Malley, Ehrenthal and Stamm. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Karl Haller, karl.haller@mhb-fontane.de, karl.haller@charite.de
 Karl Haller
Karl Haller Stefan Fritzsche3
Stefan Fritzsche3 Grace O’Malley
Grace O’Malley Johannes C. Ehrenthal
Johannes C. Ehrenthal Thomas Stamm
Thomas Stamm