- 1College of Pharmacy, Gulf Medical University, Ajman, United Arab Emirates
- 2Thumbay University Hospital, Ajman, United Arab Emirates
- 3ResponsePlus Medical, Abu Dhabi, United Arab Emirates
- 4Dubai Pharmacy College, Dubai, United Arab Emirates
- 5College of Pharmacy, Qatar University, Doha, Qatar
Background: This study was aimed to describe the choice of Surgical Antimicrobial Prophylaxis at a tertiary-level care hospital in United Arab Emirates. It also associated the choice between two leading antimicrobials for the SAP to the site of surgery.
Methods: A descriptive drug use evaluation was performed retrospectively to study choices of antimicrobials in surgical antibiotic prophylaxis. An analytical cross-sectional study design was used to develop a hypothesis regarding the choice of ceftriaxone. Data were collected from the medical records of Hospital from July 2020 to December 2020. Results were presented in numbers and percentages.
Results: SAP data were collected from 199 patients, of which 159 were clean or clean-contaminated. Dirty surgeries (18) needed a higher level of antimicrobials as there were infections to be treated. For other surgeries with no infection, overuse of antimicrobials was found regarding the choice of antimicrobials. Surgical antibiotic Prophylaxis was administered within the recommended time prior to surgeries. Ceftriaxone was preferred over cefuroxime in all types of surgeries based on the timing of Surgical Antibiotic Prophylaxis, wound classification, and the surgical site. A statistically significant association for choice of ceftriaxone over cefuroxime was found regarding surgical sites (p-value <0.05). About 99% of the patients were prescribed discharge antimicrobials when 158 (80%) surgeries were clean or clean-contaminated.
Conclusion: Overuse of antimicrobials was found in surgical antimicrobial prophylaxis. Ceftriaxone was preferred more than cefuroxime in all types of surgeries. No surgical site infections were reported. A follow-up comparative study is recommended to decrease antimicrobial use without increasing risk of surgical site infection.
Introduction
The surgical antimicrobial prophylaxis (SAP) often seems to have overuse of antimicrobials in the effort to prevent surgical site infections (SSI) (Barie, 2013). It is important to avoid overuse of antimicrobials, control the risk of microbial resistance and prevent SSIs by optimal use of antimicrobials in SAP. One of the most comprehensive SAP guidelines was developed jointly by the American Society of Health-System Pharmacists (ASHP), the Infectious Diseases Society of America (IDSA), the Surgical Infection Society (SIS), and the Society for Healthcare Epidemiology of America (SHEA). For convenience, this guideline is hereafter mentioned as ASHP guidelines. The ASHP guidelines of SAP provide comprehensive details in indication, selection, dosing, duration, and the timing of antimicrobials (Bratzler et al., 2013). The guideline-directed SAP has a beneficial effect (if properly implemented) to ensure that appropriate antimicrobials are chosen to cover the most likely pathogen at the correct dose. Evidence suggests that the administration of antimicrobials before surgery prevents infection after surgery, thus reducing SSI (Barie, 2013; Bratzler et al., 2013).
Antimicrobial stewardship program (ASP) plays a significant role in the empirical, prophylactic, and therapeutic use of antimicrobials (Bratzler et al., 2013). SSIs are associated with morbidity, mortality, increased healthcare costs, and hospital readmissions. A detailed understanding of factors and strategies is needed to optimize SAP and patient care (Alemkere, 2018). Prolonged use of antimicrobials can increase the risk of adverse events such as Clostridium difficile infections, antimicrobial resistance, acute kidney injury, and many other safety concerns. The SAP interventions should target before, while, and after surgery as needed (Abubakar et al., 2019). Several studies suggested that guideline compliance to SAP was compromised as there was a gap in awareness, availability of guidelines to health care professionals, acceptance of guidelines by surgeons, and lack of clarity about roles and responsibilities (Abubakar et al., 2019; Surgical Site Infection (SSI) Event, 2010). A well-implemented evidence-based (international/local) ASP program is essential to improve the appropriate use of SAP.
Surgical wound classication is categorized by the degree of gross contamination (clean, clean-contaminated, contaminated, and dirty) and is used in conjunction with American Society of Anesthesiology and procedure duration to find out the risk of SSIs (Surgical Site Infection, 2010). Many studies showed the use of different antimicrobial agents despite the guidelines recommendations, even not following the local/internal guidelines. Many factors could contribute to deviations from international guidelines or even local/internal guidelines that aremedication availability (shortage of medicine that need to be given as a prophylaxis as per the guidelines), less trust in local practice guidelines, healthcare delivery policies, personal experiences, and antimicrobial resistance in a particular setting (Cohen et al., 2017; Segala et al., 2020).
Researchers suggested in a study that around 55% of surgical site infections may be preventable with the help of evidence based strategies implementation appropriately (Umscheid et al., 2011). Therefore, evaluating multiple factors related to SAP is essential to reduce SSI rates and healthcare costs with better patient outcomes (Cheng et al., 2015).
As the choice of antimicrobials in SAP depends on many factors, describing the SAP practices at that hospitalis essential. Evaluating the choices of antimicrobials in SAP helps explore areas of improvement. Furthermore, it is helpful to compare good practices in other hospitals and optimize antimicrobial use as the threat of antimicrobial resistance is a global problem and achieving better patient outcomes is a local need. In this study, we aim to describe the choices of antimicrobials in SAP. It was also necessary to generate a hypothesis for further testing if ceftriaxone is preferred over cefuroxime in surgical antimicrobial prophylaxis. The objective of the study is to evaluate the choice of surgical antimicrobial prophylaxis at a tertiary-level care hospital in United Arab Emirates. Also, to find out the choice of SAP is ceftriaxone or cefuroxime.
Materials and Methods
Study Design
The study design was a retrospective, descriptive antimicrobial use evaluation among patients who underwent a surgical procedure in a tertiary-level care hospital in the UAE. It was basically an observational study. For exploring the significance of choosing ceftriaxone, an analytical cross-sectional design was used.
Study Population
Data of all the patients who underwent a surgical procedure at the hospital from July 2020 to December 2020 were collected considering inclusion and exclusion criteria. The clinical pharmacists at the hospital informed that over 100 surgeries being conducted in 6 months. Thus, data were collected for 6 months to get minimum sample of 100 surgeries.
Inclusion and Exclusion Criteria
Patients who are above 18 years and underwent any surgical procedures such as (ENT, Thyroid, orthopedic, gastrointestinal, urology, breast and miscellaneous surgeries) were included in the study. However, dental procedures and non-surgical medical procedures were excluded. Surgeries in special populations, pediatric, geriatric (patients above 85 years old), pregnant, cancer or transplant and immunocompromised patients were excluded from this study.
Study Settings
The study was conducted in a teriary-level care hospital in the UAE. The hospital treated patients in multiple specialties with inpatient and outpatient services and it have an operation theater complex. Main surgeries happening at the hospital included cesarean sessions, general surgeries, orthopedic, neurological, cardiac, and other surgeries. Transplant surgeries were not performed at the study site, but other surgeries are performed on patients who have a transplant.
Data Collection and Analysis
All patient data were collected from the medical records through electronic system. The research student collected the data. ASHP Antimicrobial Stewardship Program guidelines were used to compare the ASP use in our study (Bratzler et al., 2013) in addition to the Hospital ASP guidelines. In addition, socio-demographic characteristics of the patients, surgery-related information (site of surgery, duration of surgery, previous history of surgery, surgery type, hospital stay after surgery, wound class and occurrence of SSI after surgery within 30 days), and antimicrobials used (preoperative, postoperative and discharge) were collected.
Statistical Analysis
The statistical package of social sciences (SPSS version 26.0) was used to analyze the data. Pearson chi-square test was used to find an association between the timing of antimicrobial administration, or type of surgical site to the choice of ceftriaxone or cefuroxime. P-values less than 0.05 were considered statistically significant. The test was performed to generate a hypothesis, not to prove the hypothesis. Sample size needs to be calculated for analytical cross-sectional studies in the future.
Ethics Approval
The study was approved by the institutional review board (IRB). Permission from the Medical Director was obtained with a copy of IRB approval for data collection. Patient confidentiality has been maintained. While processing the data, patient identifiers were removed.
Results and Findings
Patient Demographics
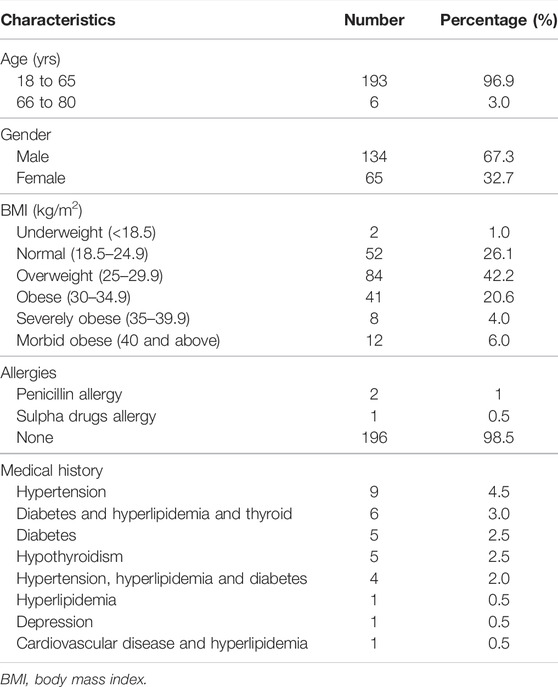
Data were collected from the electronic medical records of 199 patients after considering inclusion and exclusion criteria. There were no more than one surgery in single patient. Pregnancy-related surgeries were a major group of surgeries that were not included in this study. All the study population underwent surgery at Hospital. Their demographic details are shown in Table 1. The majority were adult males with a Body Mass Index (BMI) of normal or overweight categories.
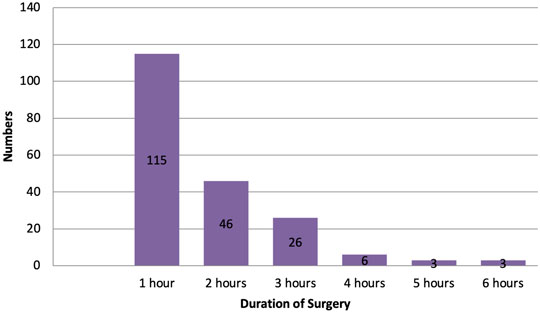
Antimicrobial Administration Timing Before Surgery
The majority of surgeries were performed within an hour, as shown in Figure 1. Only a few surgeries lasted more than 3 h. For surgeries happening more than 3 or 4 h, ASHP guidelines recommend an intraoperative dose of antimicrobials depending on the type of antimicrobials used. For example, cefuroxime provides prophylactic coverage for 4 h, but cefotaxime needs to be administered intraoperatively if surgery prolongs over 3 h. Unfortunately, data regarding the intraoperative administration of antimicrobials were not available to the research team. (Bratzler et al., 2013).
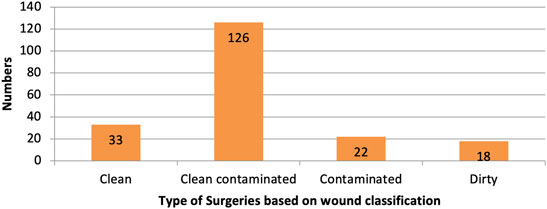
Depending on the site of surgery, as shown in Table 2, there were some differences when surgical antimicrobials were administered. On average, the timing of administration of antimicrobials prior to surgery was similar and within the recommended time. The ASHP guidelines recommend administering SAP 60–120 min prior to surgery, with some exceptions (Bratzler et al., 2013). There were two surgeries; calculous of kidney surgery (135 min) and anterior cervical discectomy and fusion (150 min) when an SAP was administered over 120 min prior to surgery (this is mentioned in miscellaneous surgeries in Table 2).
Ceftriaxone and cefuroxime were the most commonly used antimicrobials in the study population. Pre-surgical administration of ceftriaxone and cefuroxime were all within 2 h prior to surgery (Table 2).
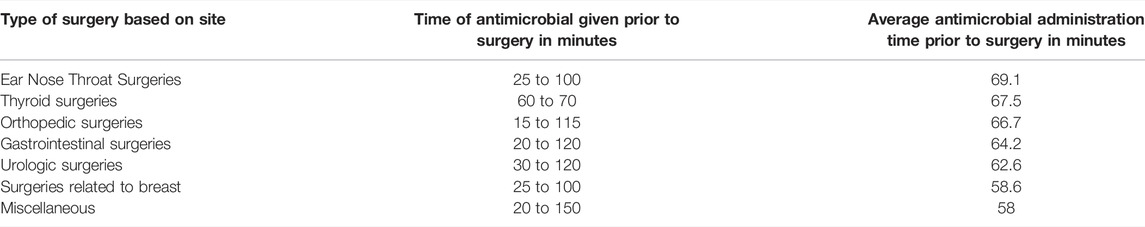
Surgeries Based on Wound Classification
The majority of surgeries were clean-contaminated, followed by clean, contaminated, and dirty, as shown in Figure 2.
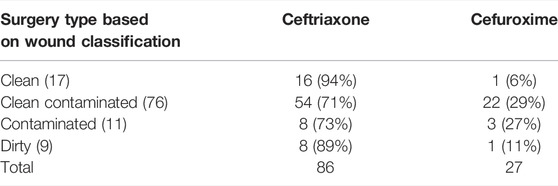
Dirty surgeries with infection needed antimicrobials for the treatment of existing infections and prevention of further infections. The use of higher antimicrobials was justified in dirty surgeries. There is a higher risk for SSIs in contaminated surgeries that might motivate surgeons to prescribe higher antimicrobials. Table 3 shows pre-surgical antimicrobials administered based on wound classification.
There were not enough data to run the Pearson Chi-Square or Fisher’s extract test to find an association between ceftriaxone or cefuroxime with the type of surgeries based on wound classification. However, the preference in numbers and percentages was for ceftriaxone, as shown in Table 4.
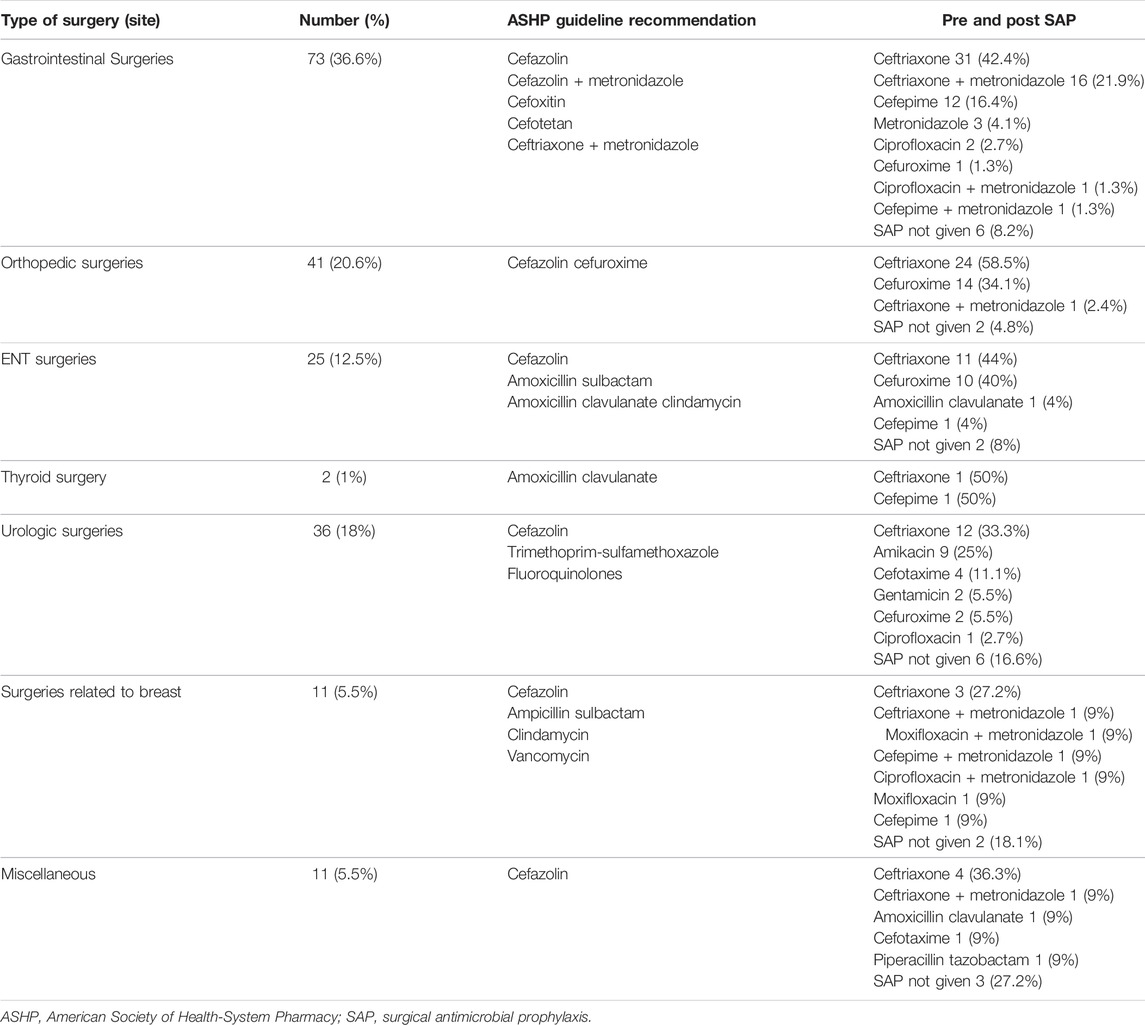
Surgeries Based on Surgical Site
Deviations were observed to SAP at the study site compared to the ASHP SAP guidelines. More information is provided in Table 5.
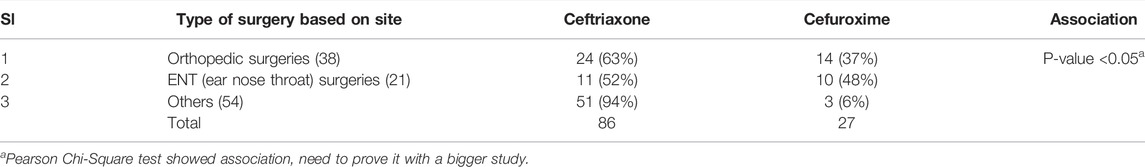
Other than orthopedic and ear, nose, throat (ENT), surgeries were combined to control expected frequencies of <5 in <25% cells. The Pearson Chi-Square test showed a statistically significant association (p-value < 0.05) of choice of ceftriaxone over cefuroxime in surgeries (orthopedic, ENT, and others) categorized based on surgical site. Though the preference in choice was ceftriaxone in all surgeries, as shown in Table 6, it needs to be further evaluated after calculating the appropriate sample size. Among cefuroxime use, orthopedic and ENT surgeries showed relatively higher prescribing. This shows that ASP programs shall initially focus on these two types of surgeries to improve the use of cefuroxime.
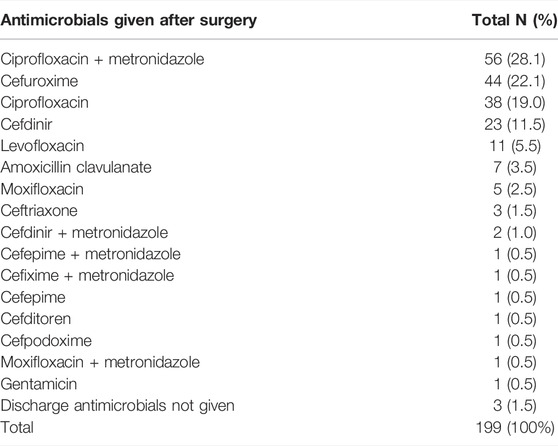
In the case of clean and clean-contaminated surgeries, it is recommended not to prescribe antimicrobials at discharge from the hospital. However, almost all patients received discharge antimicrobials (99%) when it might not be required for clean and clean-contaminated surgeries, 159 (80%). Ceftriaxone and gentamicin are parenteral antimicrobials prescribed at discharge, probably for patients who have access to nursing care on a daily basis. Cefuroxime was more commonly used at discharge compared to ceftriaxone. More details are provided in table 7.
No SSIs were reported to any of the study population during the study period July 2020 to December 2020. As per ASP data of the hospital, from January 2021 to May 2021, there were no reports of any SSIs in any surgeries conducted. There was an SSI case in a pediatric patient in June 2021.
Discussion
Our study population received SAP similar to some studies but different from the guidance of using first or second-generation cephalosporins (Umscheid et al., 2011; Cheng et al., 2015; Cohen et al., 2017; Halawi et al., 2018). The ASHP guidelines and SAP guidelines in the study setting were recommending first or second-generation cephalosporins. In all types of surgeries, ceftriaxone (third-generation cephalosporin) was used more than cefuroxime (second-generation cephalosporin).
In our study, the majority of the surgical procedures were clean-contaminated or clean based on wound classification. Similar findings were reported in other studies where clean-contaminated surgeries were higher, followed by clean surgeries. In addition, discharge from hospital antimicrobials was prescribed for most patients, including clean and clean-contaminated surgeries, when it was not necessary (Ozgun et al., 2010; Halawi et al., 2018).
In our study, antimicrobial administration time was reported <1 h in most surgeries, which was consistent with many studies. Some studies suggested no significant difference in SSI risk comparing 120–60 min versus 60–0 min before surgical procedure. Administration >120 min before incision shall increase SSIs risk (Alahmadi et al., 2020).
The SAP guidelines reported multifactorial contexts of SSIs, including drug selection, dose administration, time of administration, duration of surgery, patient-related factors like BMI. Several studies have linked antimicrobials’ pharmacokinetics, such as half-life, adequate tissue concentrations, to surgical site infections. Therefore, adherence to SAP guidelines varies considering multiple aspects (de Jonge et al., 2017; Siddiqi et al., 2019; Alahmadi et al., 2020). Further research is required to prove if there is any association exists.
Our results also show a difference in gender distribution who underwent surgeries. The duration of surgeries was significantly higher in females compared to males. As duration A similar finding was reported in many studies, but contrasting findings were reported in a study where males (51.2%) had a higher duration compared to females (48.8%) (Umscheid et al., 2011; Cheng et al., 2015; Halawi et al., 2018; Alahmadi et al., 2020). In our study number of males are significantly more than female that can impact the overall duration of antimicrobials.
For none of the surgeries, cefazolin was used. Cefazolin is recommended for SAP as per the guidelines. The use of narrow-spectrum antimicrobials needs to be avoided and to reduce or even stop in clean surgeries. Overuse of antimicrobials will increase resistance among microbes and may lead to the emergence of multi-drug resistant organisms (Mendelson and Matsoso, 2015; Mossanen et al., 2015; Hawn and Knowlton, 2019; Niraula et al., 2021). Several studies recommended monitoring hospital prescriptions that can help in guiding the antimicrobial use and resistance pattern among pathogens. (Lai et al., 2016; Tiri et al., 2020).
Antimicrobial administration time before surgical incision was as per the hospital guidelines (60–120 min). Therefore, it is essential to review the pattern of antimicrobial prophylaxis in relation to the duration of surgery (Mu et al., 2011; Argaw et al., 2017; Tiri et al., 2020). However, no data was found about intraoperative administration for the surgeries that took more than 3 h. As per the practitioners, intraoperative antimicrobial doses were administered when surgery was prolonged more than 3 h. The intraoperative dose depends on the type of antimicrobial, time of administration before surgery, duration of the surgical procedure, and surgical site (Mu et al., 2011; Argaw et al., 2017).
Studies show different choices of antimicrobials, e.g., in otolaryngological surgeries, cefazolin or ampicillin-sulbactam/amoxicillin-clavulanate or clindamycin were used (Ottoline et al., 2013). Most of the surgeries in our study population were clean-contaminated or clean; SAP might be unnecessary as per the ASHP guidelines for surgeries in some locations. However, the findings showed the overuse of antimicrobials. The results also reported no surgical site infection in any of the cases collected. In fact, from December 2020 to May 2021, no surgical site infection was reported to any patients treated at the study site. Many of the other studies were showing more SSIs from US (1.9%), Pakistan (9.29%), Ethiopia (20.6%), and as low as from 2.5 to 41.9% depending on hospital settings and the extent of implementation of sterilization and aseptic techniques. Limited resources at hospitals might also be factors contributing to SSIs (Linda, 2003; Mu et al., 2011; Tefera et al., 2020). It is understandable that choices of antimicrobials vary depending on multiple aspects. Studies related to the antimicrobials and stewardships are less evident in Asian countries.
Retrospective data collection on ASP is convenient and quick but will be affected by missing data issues. Some studies show missing data on intra-operative surgical antimicrobial prophylaxis. Deviation from ASP guidance is also reported in other studies. For example, in a study, more than 95% of surgeries received third generationcephalosporins such as ceftriaxone followed by second-generation cephalosporins such as cefuroxime (Haney et al., 2020). In our study also, ceftriaxone was more commonly used than cefuroxime. Wound classification, the timing of pre-surgical antimicrobials, or surgery sites were preferring ceftriaxone over cefuroxime or vice versa. In a study related to orthopedic surgeries, ceftriaxone and cefuroxime were their choices of antimicrobials (Dhammi et al., 2015). The antimicrobial choice for surgeries related to the breast was ampicillin/ampicillin-sulbactam and third generationcephalosporins (Bağhaki et al., 2014). From our study, within the use of cefuroxime, it was preferred more in orthopedic and ENT surgeries though less than ceftriaxone. ASP of the hospital shall focus first on these surgeries to improve the use of cefuroxime.
Prescribing post-surgical antimicrobials at discharge from the hospital were common at the study site. In many of these cases, ASHP guidelines recommend against the need for antimicrobials. Considering the environmental factors, the ability of patients for their self-care, misuse of antimicrobials shall be justified, but it is important to consider a decrease in the use of antimicrobials. In clean and clean-contaminated surgeries, hospital discharge antimicrobials shall be avoided if there is no specific indication in a particular patient. Misuse of antimicrobials is a global problem that needs to be addressed (Loozen et al., 2017; MondeloGarcía et al., 2018; Podda et al., 2019; Zaha et al., 2020). Health insurance not covering expenses of SSIs and patient preferences to take over precaution might be contributing to overuse of antimicrobials at the study site.
This tertiary-level care hospital has an established ASP. Which has a policy to prescribe the antibiotic as surgical prophylaxis to different classes of surgeries. This policy is supported by IDSA & SEHA guidelines and it promotes cefuroxime for clean & clean-contaminated cases. But the reason for not compliance to the policies being many like; 1) Change of surgeons, new surgeons need time and motivation to change old habits of prescribing. 2) the surgeons feel comfortable to start with ceftrixone as prophylactic and continue as therapeutic antibiotic until the patient gets discharge. 3) Non-availability of cefuroxime for some period of the year. 4) pressure from insurance companies for early discharge post-operative and surgeons feels ceftrixone is superior and broad spectrum antibiotic.
After this study, the Antibiotic Stewardship Committee shall discuss this presentation and highlights the significance & effectiveness of cefuroxime as pre-surgrical prophylaxis. After a period of 1 year, a comparative analysis can be presented showing that the number % of surgical site infections as remained to minimal so as when ceftriaxone was prescribing.
Limitations
The study has limitations regarding its retrospective design. Some data were missing, especially about intraoperative antimicrobial use. The accuracy of data might also be compromised compared to a prospective design. Still, a retrospective design was used, considering the feasibility of the study. For the data collected from medical records, there is the possibility that some of the antimicrobials were used for the treatment of infections instead of prophylaxis of SSIs. Health insurance not paying for the management of SSIs might add pressure to overuse antimicrobials.
Another limitation of the study is whether any patients had some level of immunosuppression that was not mentioned in the medical records. In such patients, more than the usual use of antimicrobials shall be justified. We did exclude patients who were having a transplant, cancer, or consuming any immunosuppressant drugs. Collecting data from cesarean sessions might be useful as a separate study as they were high in number. Though the current number of surgeries described a pattern in antimicrobial use, more data will help generate more hypotheses to be tested. The current analytical cross-sectional design was used to generate a hypothesis only, not to test it.
Clinical Hypothesis
The surgical site showed association to the choice of ceftriaxone. In all cases, ceftriaxone was preferred over cefuroxime based on descriptive data. The following hypothesis is generated to be tested with adequate sample size, “ceftriaxone is not preferred over cefuroxime in surgical antimicrobial prophylaxis of surgeries categorized based on sites of surgeries.” While discharging patients’ home after surgery, unnecessary use of antimicrobials was also observed.
Conclusion
The study showed the overuse of antimicrobials in surgical prophylaxis. In dirty surgeries, higher use of antimicrobials is essential as it treats the existing infection. In other cases, overuse of higher classes of antimicrobials is observed in SAP. No surgical site infection happened among any of the study population. In relation to ASHP SAP guidelines, overuse of antimicrobials was found before and after surgery and at the discharge of the patients. The selection of antimicrobials was also different compared to the ASHP guidelines and the guidelines at the study site. Instead of first or secondgeneration cephalosporins, ceftriaxone (third generation) was more commonly used. A comparative analysis is recommended after a period of 1 year to review the antibiotic prescribing and rate of surgical site infections.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Research Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abubakar, U., Syed Sulaiman, S. A., and Adesiyun, A. G. (2019). Impact of Pharmacist-Led Antimicrobial Stewardship Interventions on Compliance with Surgical Antimicrobial Prophylaxis in Obstetric and Gynecologic Surgeries in Nigeria. PLoS One 14 (3), e0213395. doi:10.1371/journal.pone.0213395
Alahmadi, Y. M., Alharbi, R. H., Aljabri, A. K., Alofi, F. S., Alshaalani, O. A., and Alssdi, B. H. (2020). Adherence to the Guidelines for Surgical Antimicrobial Prophylaxis in a Saudi Tertiary Care Hospital. J. Taibah Univ. Med. Sci. 15 (2), 136–141. doi:10.1016/j.jtumed.2020.01.005
Alemkere, G. (2018). Antimicrobial Usage in Surgical Prophylaxis: A Prospective Observational Study in the Surgical ward of Nekemte Referral Hospital. PLoS One 13 (9), e0203523. doi:10.1371/journal.pone.0203523
Argaw, N. A., Shumbash, K. Z., Asfaw, A. A., and Hawaze, S. (2017). Assessment of Surgical Antimicrobial Prophylaxis in Orthopaedics and Traumatology Surgical Unit of a Tertiary Care Teaching Hospital in Addis Ababa. BMC Res. Notes 10 (1), 160. doi:10.1186/s13104-017-2475-2
Bağhaki, S., Soybir, G. R., and Soran, A. (2014). Guideline for Antimicrobial Prophylaxis in Breast Surgery. J. Breast Health 10 (2), 79–82. doi:10.5152/tjbh.2014.1959
Barie, P. S. (2013). Guidelines for Antimicrobial Prophylaxis in Surgery: a Must-Read, Must-Heed for Every Surgeon. Surg. Infect. (Larchmt) 14 (1), 5–7. doi:10.1089/sur.2013.9995
Bratzler, D. W., Dellinger, E. P., Olsen, K. M., Perl, T. M., Auwaerter, P. G., Bolon, M. K., et al. (2013). Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery. Am. J. Health Syst. Pharm. 70 (3), 195–283. doi:10.2146/ajhp120568
Cheng, K., Li, J., Kong, Q., Wang, C., Ye, N., and Xia, G. (2015). Risk Factors for Surgical Site Infection in a Teaching Hospital: a Prospective Study of 1,138 Patients. Patient Prefer Adherence 9, 1171–1177. doi:10.2147/PPA.S86153
Cohen, M. E., Salmasian, H., Li, J., Liu, J., Zachariah, P., Wright, J. D., et al. (2017). Surgical Antibiotic Prophylaxis and Risk for Postoperative Antibiotic-Resistant Infections. J. Am. Coll. Surg. 225 (5), 631–e3. doi:10.1016/j.jamcollsurg.2017.08.010
de Jonge, S. W., Gans, S. L., Atema, J. J., Solomkin, J. S., Dellinger, P. E., and Boermeester, M. A. (2017). Timing of Preoperative Antibiotic Prophylaxis in 54,552 Patients and the Risk of Surgical Site Infection. Medicine (Baltimore) 96 (29), e6903. doi:10.1097/md.0000000000006903
Dhammi, I. K., Haq, R. U., and Kumar, S. (2015). Prophylactic Antibiotics in Orthopedic Surgery. Ijoo 49 (4), 373–376. doi:10.4103/0019-5413.159556
Halawi, E., Assefa, T., and Hussen, S. (2018). Pattern of Antibiotics Use, Incidence and Predictors of Surgical Site Infections in a Tertiary Care Teaching Hospital. BMC Res. Notes 11 (1), 538. doi:10.1186/s13104-018-3643-8
Haney, V., Maman, S., Prozesky, J., Bezinover, D., and Karamchandani, K. (2020). Improving Intraoperative Administration of Surgical Antimicrobial Prophylaxis: a Quality Improvement Report. BMJ Open Qual. 9, e001042. doi:10.1136/bmjoq-2020-001042
Hawn, M. T., and Knowlton, L. M. (2019). Balancing the Risks and Benefits of Surgical Prophylaxis: Timing and Duration Do Matter. JAMA Surg. 154 (7), 598–599. doi:10.1001/jamasurg.2019.0570
Lai, C. C., Shi, Z. Y., Chen, Y. H., and Wang, F. D. (2016). Effects of Various Antimicrobial Stewardship Programs on Antimicrobial Usage and Resistance Among Common Gram-Negative Bacilli Causing Health Care-Associated Infections: A Multicenter Comparison. J. Microbiol. Immunol. Infect. 49, 74–82. doi:10.1016/j.jmii.2015.05.011
Linda, T. (2003). Infection Prevention Guidelines for Healthcare Facilities with Limited Resources. 5th ed. Berlin: Springer.
Loozen, C. S., van Santvoort, H. C., van Geloven, A. A. W., Nieuwenhuijzen, G. A. P., de Reuver, P. R., Besselink, M. H. G., et al. (2017). Perioperative Antibiotic Prophylaxis in the Treatment of Acute Cholecystitis (PEANUTS II Trial): Study Protocol for a Randomized Controlled Trial. Trials 18 (1), 390. doi:10.1186/s13063-017-2142-x
Mendelson, M., and Matsoso, M. P. (2015). The World Health Organization Global Action Plan for Antimicrobial Resistance. S. Afr. Med. J. 105 (5), 325. doi:10.7196/samj.9644
Mondelo García, C., Gutiérrez Urbón, J. M., Pérez Sanz, C., Martín HerranzAuditing, M. I., and Surgical, Improving. (2018). Auditing and Improving Surgical Antibiotic Prophylaxis. Surg. Infections 19 (7), 679–683. doi:10.1089/sur.2018.097
Mossanen, M., Calvert, J. K., Holt, S. K., James, A. C., Wright, J. L., Harper, J. D., et al. (2015). Overuse of Antimicrobial Prophylaxis in Community Practice Urology. J. Urol. 193 (2), 543–547. doi:10.1016/j.juro.2014.08.107
Mu, Y., Edwards, J. R., Horan, T. C., Berrios-Torres, S. I., and Fridkin, S. K. (2011). Improving Risk-Adjusted Measures of Surgical Site Infection for the National Healthcare Safely Network. Infect. Control. Hosp. Epidemiol. 32 (10), 970–986. doi:10.1086/662016
Niraula, R., Tambat, R. M., Gupta, R., and Devkota, A. (2021). A Hospital-Based Prospective Study on Surgical Antimicrobial Prophylaxis and Incidence of Surgical Site Infections in the Department of General Surgery. World J. Surg. Surg. Res. 4 (2021), 1274. doi:10.4172/2332-0877.1000e452
Ottoline, A. C., Tomita, S., Marques Mda, P., Felix, F., Ferraiolo, P. N., and Laurindo, R. S. (2013). Antimicrobial Prophylaxis in Otolaryngologic Surgery. Int. Arch. Otorhinolaryngol. 17 (1), 85–91.
Ozgun, H., Ertugrul, B. M., Soyder, A., Ozturk, B., and Aydemir, M. (2010). Peri-operative Antibiotic Prophylaxis: Adherence to Guidelines and Effects of Educational Intervention. Int. J. Surg. 8 (2), 159–163. doi:10.1016/j.ijsu.2009.12.005
Podda, M., Gerardi, C., Cillara, N., Fearnhead, N., Gomes, C. A., Birindelli, A., et al. (2019). Antibiotic Treatment and Appendectomy for Uncomplicated Acute Appendicitis in Adults and Children. Ann. Surg. 270 (6), 1028–1040. doi:10.1097/sla.0000000000003225
Segala, F. V., Murri, R., Taddei, E., Giovannenze, F., Del Vecchio, P., Birocchi, E., et al. (2020). Antibiotic Appropriateness and Adherence to Local Guidelines in Perioperative Prophylaxis: Results from an Antimicrobial Stewardship Intervention. Antimicrob. Resist. Infect. Control. 9 (1), 164–166. doi:10.1186/s13756-020-00814-6
Siddiqi, A., Forte, S. A., Docter, S., Bryant, D., Sheth, N. P., and Chen, A. F. (2019). Perioperative Antibiotic Prophylaxis in Total Joint Arthroplasty. J. Bone Jt. Surg. 101 (9), 828–842. doi:10.2106/jbjs.18.00990
Surgical Site Infection (SSI) Event (2010). Center for Disease Control. Available at: http://www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf?agree=yes&next=Accept. Updated January 2015 (Accessed March 3, 2015).
Tefera, G. M., Feyisa, B. B., Taye, G. M., Tesfaye Umeta, G., Negash Bereded, F., Dinsa Ayeno, H., et al. (2020). The Association between Incorrect Use of Antibiotic Prophylaxis and In-Hospital Surgical Site Infections - A Prospective Observational Study. Infect. Drug Resist. 13, 3063–3072. doi:10.2147/IDR.S260238
Tiri, B., Bruzzone, P., Priante, G., Sensi, E., Costantini, M., Vernelli, C., et al. (2020). Impact of Antimicrobial Stewardship Interventions on Appropriateness of Surgical Antibiotic Prophylaxis: How to Improve. Antibiotics (Basel) 9 (4), 168. doi:10.3390/antibiotics9040168
Umscheid, C. A., Mitchell, M. D., Doshi, J. A., Agarwal, R., Williams, K., and Brennan, P. J. (2011). Estimating the Proportion of Healthcare-Associated Infections that Are Reasonably Preventable and the Related Mortality and Costs. Infect. Control. Hosp. Epidemiol. 32, 101–114. doi:10.1086/657912
Keywords: surgical antimicrobial prophylaxis, ceftriaxone, cefotaxime, surgeries, surgical site infections, antimicrobial stewardship
Citation: Vippadapu P, Gillani SW, Thomas D, Ahmed F, Gulam SM, Mahmood RK, Menon V, Abdi S and Rathore HA (2022) Choice of Antimicrobials in Surgical Prophylaxis - Overuse and Surgical Site Infection Outcomes from a Tertiary-Level Care Hospital. Front. Pharmacol. 13:849044. doi: 10.3389/fphar.2022.849044
Received: 05 January 2022; Accepted: 14 February 2022;
Published: 11 April 2022.
Edited by:
Anthony Attama, University of Nigeria, NigeriaReviewed by:
Faiz Ullah Khan, Xi’an Jiaotong University, ChinaAmer Hayat Khan, Universiti Sains Malaysia (USM), Malaysia
Copyright © 2022 Vippadapu, Gillani, Thomas, Ahmed, Gulam, Mahmood, Menon, Abdi and Rathore. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Syed Wasif Gillani, wasifgillani@gmail.com, dr.syedwasif@gmu.ac.ae
 Prasanna Vippadapu
Prasanna Vippadapu Syed Wasif Gillani
Syed Wasif Gillani Dixon Thomas1
Dixon Thomas1 Shabaz Mohiuddin Gulam
Shabaz Mohiuddin Gulam Rana Kamran Mahmood
Rana Kamran Mahmood Vineetha Menon
Vineetha Menon Semira Abdi
Semira Abdi Hassaan Anwer Rathore
Hassaan Anwer Rathore