Ureteral dilation recovery after intravesical reimplantation in children with primary obstructive megaureter
- 1Department of Pediatric Surgery, Shandong Provincial Hospital, Shandong University, Jinan, China
- 2Department of Pediatric Surgery, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
Background: To observe the postoperative recovery following ureteral dilation in primary obstructive megaureter (POM) after ureteral implantation, and evaluate the risk factors affecting ureter diameter resolution.
Materials and Methods: A retrospective study was performed in patients with POM who underwent ureteral reimplantation using the Cohen procedure. Patient characteristics, perioperative parameters, and postoperative outcomes were also analysed. A widest ureteral diameter of <7 mm was defined as a normal shape and outcome. Survival time was defined as the time from surgery to ureteral dilation recovery or to the last follow-up.
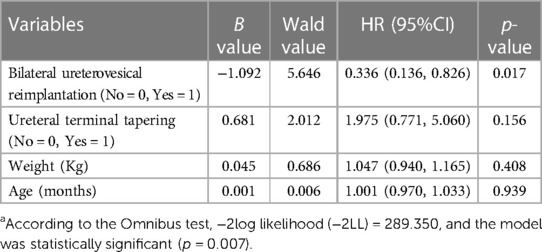
Results: A total of 49 patients (54 ureters) were included in the analysis. The survival time ranged from 1 to 53 months. The shapes of a total of 47 (87.04%) megaureters recovered, and most (29/47) resolutions happened within 6 months after surgery. In the univariate analysis, bilateral ureterovesical reimplantation (p = 0.015), ureteral terminal tapering (p = 0.019), weight (p = 0.036), and age (p = 0.015) were associated with the recovery time of ureteral dilation. A delayed recovery of ureteral diameter was noted in bilateral reimplantation (HR = 0.336, p = 0.017) using multivariate Cox regression.
Conclusions: Ureteral dilation in POM mostly returned to normal within six postoperative months. Moreover, bilateral ureterovesical reimplantation is a risk factor for delayed postoperative recovery of ureter dilation in POM.
1. Introduction
Primary obstructive megaureter (POM) mainly caused by vesicoureteral junction obstruction is a well-known disease in pediatric urology (1), with an incidence of approximately 1 in 1,500 and a male preponderance (2). For POM patients with worsening hydroureteronephrosis, frequent urinary tract infection, and decreasing kidney function, the primary therapy is surgical treatment in the form of ureteral reimplantation (3). Of the numerous published studies, the improvement in renal function and descent of the renal pelvis anteroposterior diameter are used to assess the surgical outcome of hydronephrosis (4–6). However, to date, few studies have examined the changes in megaureter shape after ureteral reimplantation. In our previous study, the postoperative recovery of ureteral dilation in these patients differed among individuals. Hence, this study aimed to investigate the recovery of ureteral dilation for POM after surgery and the predictors that affect the resolution of ureteral dilation.
2. Methods
2.1. Patients
We retrospectively analyzed the medical history of patients with POM who underwent ureteral reimplantation using the Cohen method at our institution between January 2011 and January 2021. Pneumovesical Cohen has been the main approach used for POM in the last 5 years. POM was confirmed by diuretic provocation with 99mTechnetium mercaptoacetyltriglycine-3 (MAG3). Preoperative evaluations were performed using ultrasonography, computed tomography urography (CTU), magnetic resonance urography (MRU) and voiding cystourethrography (VCUG). After excluding the vesicoureteral reflux (VUR) through VCUG, megaureters with an obstructive pattern on diuretic renogram and the beak-like appearance or spindle-shaped narrowing of the ureterovesical junction on MRU or CTU are identified as the POM. For cases included in the present study, intraoperative findings and postoperative pathological results confirmed the diagnosis of POM. Hydronephrosis and ureteral diameter were assessed using ultrasound measurements recorded pre-operatively and during the postoperative follow up. The ureteral diameter was measured as the largest transverse dimension of the distal ureter, as shown on ultrasonography. Patients with POM secondary to ureterocoele, posterior urethral valves, or neurogenic bladder or those with other urinary system abnormalities were not included in the study. Cases without complete follow-up data within 1 year after surgery were also excluded.
2.2. Surgical procedures
Surgical indications included obstruction, as evidenced by hydroureteronephrosis with either reduced split renal function (less than 40% on the affected side) or symptoms (pain, breakthrough febrile urinary tract infection). All patients underwent surgery using Cohen's cross-trigonal ureteral reimplantation by a paediatric urologist. The pneumovesical approach was used as described by Yeung et al. (7). During the surgical procedure, the distal narrow segment and grossly dilated proximal segment of the ureter were dissected, and ureteral folding was performed if the ureteral diameter was >15 mm.
2.3. Follow-up
All patients underwent repeat urinalysis and ultrasound to monitor for obstruction at 1, 2, 3, 6 and 12-months postoperatively and once a year thereafter. If persistent changes in the general urine test and ultrasound were identified, VCUG and diuretic renography were performed. In our study, a widest ureteral diameter <7 mm under ultrasound was defined as the normal shape (3, 8) and outcome event. Survival time was defined as the time from surgery to ureteral dilation recovery or the last follow-up if the ureteral diameter did not become normal.
2.4. Statistical analysis
Statistical analyses were performed using SPSS version 25. Numerical variables are described as medians and quartiles. We used univariate Cox regression analysis for numerical variables and the log-rank test in the Kaplan–Meier estimation for categorical variables. Variables with a significance level below 0.05 were included in a multivariate Cox regression analysis. In multivariate analysis, p < 0.05 was considered to be statistically significant.
3. Results
A total of 49 patients (37 males and 12 females) were included in the analysis. The median age was 21 months (1–42 months), and the median survival time was 6 months (1–53 months). 25 of the patients were diagnosed prenatally, 13 were symptomatically detected, and 11 were incidentally diagnosed. The majority (31/49) were left-sided, 13 were right-sided, and 5 were bilateral. Of the 54 ureters, forty were operated using a laparoscopic pneumovesical approach, and 14 were treated via open surgery. Eight ureters underwent terminal ureteral folding (Table 1).
During the follow-up, three patients had febrile urinary tract infections within one month of the surgery and were treated with antibiotics, but they had no reflux according to a VCUG. One patient presented with mild urinary incontinence, and a VUR grade III was diagnosed using VCUG. Postoperative data, including parenchymal thickness (median 9.00 mm with IQR 7.00–12.00 mm vs. median 5.00 mm with IQR 3.00–6.75 mm), APD (median 6.50 mm with IQR 0.00–11.00 mm vs. median 16.00 mm with IQR 11.00–27.00 mm), widest ureteral diameter (median 3.00 mm with IQR 3.00–3.13 mm vs. median 15.00 mm with IQR 11.00–19.00 mm), were significantly improved (p < 0.001). No increase in ureteral dilation was observed during follow-up.
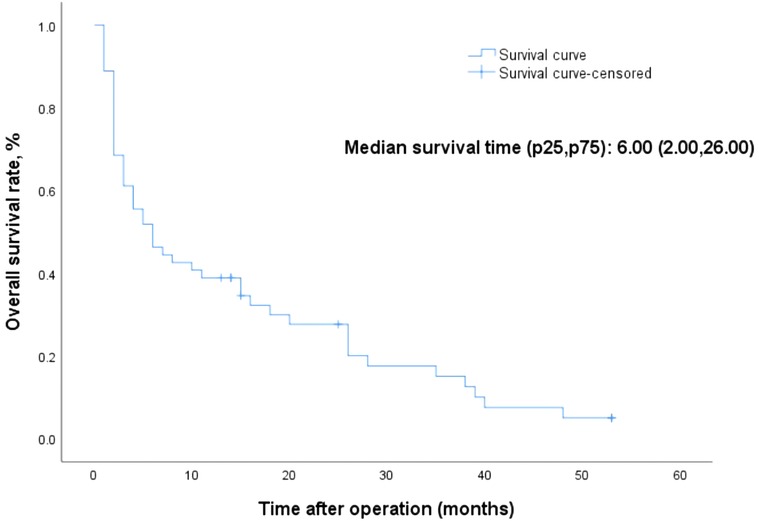
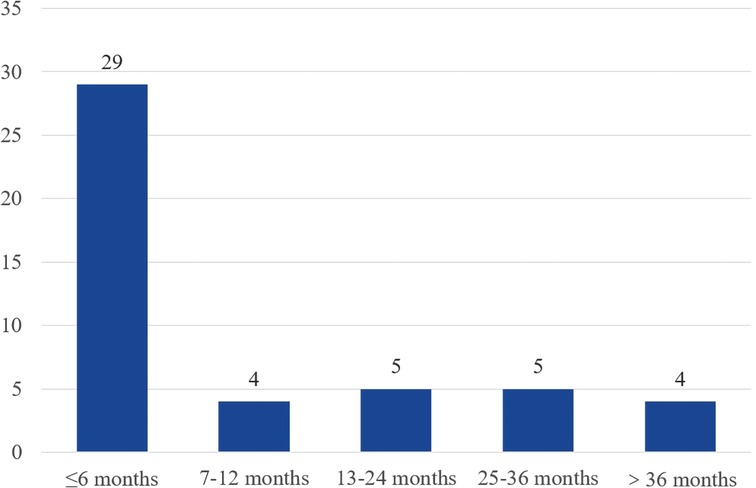
The Overall Kaplan-Meier survival curves are shown in Figure 1. The survival time ranged from 1 to 53 months, and the median survival time was 6 months. Forty-seven megaureter ureters progressively disappeared, and most resolution occurred within 6 months after surgery. Figure 2 shows the distribution of ureteral recovery time. There were seven censored events, and the median survival time for those cases was 15 months (range: 13–53 months). Except for two ureters without recovery to normal shape at the end of the study, five ureters were lost to follow-up. However, in those censored cases, the postoperative widest ureteral diameter was still reduced significantly (median 9.00 mm vs. median16.20 mm, p = 0.003).
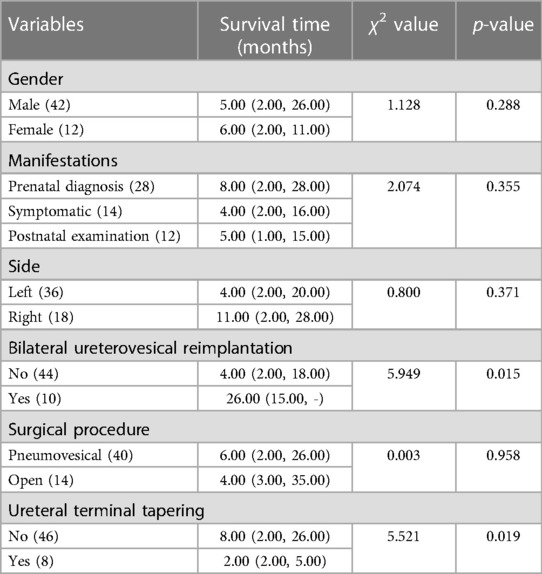
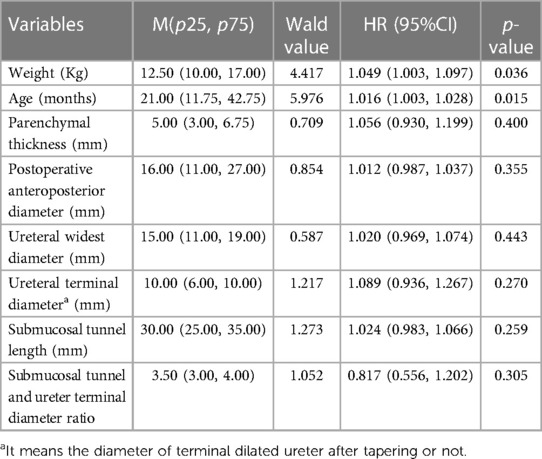
Tables 1, 2 show the univariate analysis results for clinical categorical variables and numerical variables related to the postoperative recovery time of ureteral dilation, respectively. Bilateral ureterovesical reimplantation (χ2 = 5.949, p = 0.015), ureteral terminal tapering (χ2 = 5.521, p = 0.019), weight (Wald = 4.417, p = 0.036), and age (Wald = 5.976, p = 0.015) were statistically significant. These factors were included in the multivariate analysis. Bilateral ureterovesical reimplantation (HR = 0.336, p = 0.017) was statistically significant in the multivariate Cox regression analysis (Table 3), and the Kaplan-Meier survival curves are shown in Figure 3. A slower decrease in dilatation of the megaureter to normal was noted in patients with bilateral ureterovesical reimplantation.
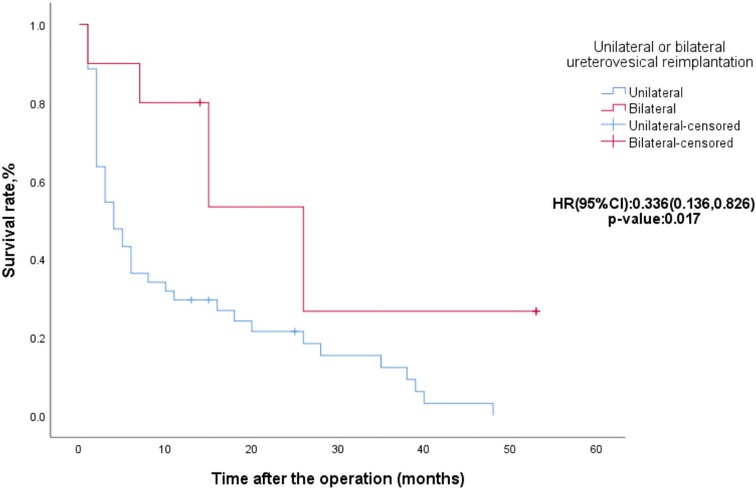
Figure 3. Kaplan-Meier survival curves for ureters with unilateral or bilateral ureterovesical reimplantation.
4. Discussion
Postoperative dilation recovery of the ureter and renal pelvis is a major concern in POM and hydronephrosis. Hydronephrosis after pyeloplasty has been reported to stabilise 6 to 8 months after the operation (9) and mostly resolves within 12 months (10). However, postoperative recovery of ureteral dilation in POM has rarely been reported. Cussen LJ has measured the ureteral shape of fetuses (>20 weeks) and children (<12 years), and then he concluded that the upper limit of normal ureteral diameters was 5.0–6.5 mm (11). In another study, after analyzing the radiological data of normal ureters from 194 children aged 0–16 years, Hellström M et al. defined the ureteral dilation as ureteral diameter >7 mm (12). On the basis of previous reports, in 2014, British Association of Paediatric Urologists confirmed that in fetuses after 30 weeks of gestation and children, a ureter can be thought of dilated if the diameter was larger than 7 mm (3). Furthermore, this criterion was also used in another study (8). In our study, ureteral diameter less than 7 mm was used as the cut-off value of the resolution of megaureter.
Ureterovesical reimplantation is currently the procedure of choice for POM (13). There have been many reports on the surgical procedure for ureterovesical reimplantation (14–16). Furthermore, in those articles, the degree of ureteral dilatation and hydronephrosis significantly improved after surgery. Similarly, we observed that the widest ureteral diameter recovered after surgery, and most megaureters (47/54) returned to a normal size. The resolution of the megaureter (29/47) mainly occurred within six months after surgery. What was striking was that we observed resolution even 36 months after the surgery. Therefore, long-term postoperative follow-up is necessary for children with persistent dilated ureters.
A multicentre international survey confirmed that bilaterality is a predictor of postoperative bladder dysfunction in extravesical ureteral reimplantation (17). In another study, bilateral primary obstructive megaureters appeared to have more postoperative vesicoureteral reflux after high-pressure balloon dilation (18). In our study, no postoperative bladder dysfunction or vesicoureteral reflux was observed in bilateral ureterovesical reimplantation. However, we found that ureters that underwent bilateral ureterovesical reimplantation had slower postoperative recovery of ureteral dilation. Therefore, leaving a stent in these cases would have contributed to ureteral recovery.
The role of ureteral tapering in the surgical repair of POM has been well documented and is controversial (19–21). Our clinical practice is to incorporate tapering when the distal ureteral diameter is greater than 1.5 cm to create an adequate anti-refluxing tunnel. Since the folding technique was judged to be better at maintaining the blood supply (22), we were more inclined to perform ureteral folding rather than tailoring. In this study, there was no significant risk effect of folding on the recovery of ureteral dilation, and there was no stenosis or reflux of the folding ureters during follow-up.
The relationship between age and postoperative recovery of the renal pelvis in patients with hydronephrosis has been previously reported. González Ruiz Y found that reduction of the postoperative renal pelvis anteroposterior diameter was more common in patients younger than one year (23). However, another study reported that early pyeloplasty (< 3 months) did not seem to contribute to the recovery of postoperative renal pelvis in children with prenatally diagnosed ureteropelvic junction obstruction (24). We incorporated age and weight into our analysis, but there was no significant association between age or weight and postoperative recovery of ureteral dilation.
5. Conclusions
Postoperative ureteral diameter in POM patients mostly returned to normal within 6 months. The resolution of ureteral dilation was slower in children with bilateral ureterovesical reimplantation, which is a risk factor for increased postoperative recovery time of ureteral dilation. The drawbacks of this study are its small size and the retrospective nature without renal function analysis. Long-term and large sample studies are needed for further exploration of ureteral dilation recovery after intravesical reimplantation.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Ethics Committee of Shandong Provincial Hospital. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
RW and WL conceived the research. YH, XW, YX, ZL and XW collected and reviewed subjects’ data. YH performed statistical analysis and drafted the manuscript. GD and WL contributed to its revision. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors thank the research personnel and the research volunteers involved with this project. And we would like to thank Editage (www.editage.com) for English language editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Shokeir AA, Nijman RJ. Primary megaureter: current trends in diagnosis and treatment. BJU Int. (2000) 86(7):861–8. doi: 10.1046/j.1464-410x.2000.00922.x
2. Ranawaka R, Hennayake S. Resolution of primary non-refluxing megaureter: an observational study. J Pediatr Surg. (2013) 48(2):380–3. doi: 10.1016/j.jpedsurg.2012.11.017
3. Farrugia MK, Hitchcock R, Radford A, Burki T, Robb A, Murphy F. British association of paediatric urologists consensus statement on the management of the primary obstructive megaureter. J Pediatr Urol. (2014) 10(1):26–33. doi: 10.1016/j.jpurol.2013.09.018
4. Sarica K, Tarhan F, Erdem K, Sevinc AH, Guzel R, Eryildirim B. Functional and morphological recovery of solitary kidneys after drainage. Double J stent placement vs emergency ureteroscopy: which one is reasonable? Urolithiasis. (2018) 46(5):479–84. doi: 10.1007/s00240-017-1005-y
5. Nayyar R, Yadav S, Singh P, Kumar R, Seth A, Dogra PN. Outcomes of pyeloplasty in very poorly functioning kidneys: examining the myths. Urology. (2016) 92:132–5. doi: 10.1016/j.urology.2016.02.045
6. Li M, Yang Y, Hou Y, Chen H, Niu Z. Functional and morphological outcome after pyeloplasty for children with unilateral hydronephrosis. Chinese Journal of Urology. (2016) 37(06):431–5. doi: 10.3760/cma.j.issn.1000-6702.2016.06.009
7. Yeung CK, Sihoe JD, Borzi PA. Endoscopic cross-trigonal ureteral reimplantation under carbon dioxide bladder insufflation: a novel technique. J Endourol. (2005) 19(3):295–9. doi: 10.1089/end.2005.19.295
8. Di Renzo D, Aguiar L, Cascini V, Di Nicola M, McCarten KM, Ellsworth PI, et al. Long-Term followup of primary nonrefluxing megaureter. J Urol. (2013) 190(3):1021–6. doi: 10.1016/j.juro.2013.03.008
9. Peng Q, Zhao Y, Zhao X, Yin P. Study on postoperative recovery of renal morphology and function in children with hydronephrosis caused by stenosis of ureteropelvic junction. Chin Pediatr Integr Tradit West Med. (2017) 9(05):404–7. doi: 10.3969/j.issn.1674-3865.2017.05.012
10. Värelä S, Omling E, Börjesson A, Salö M. Resolution of hydronephrosis after pyeloplasty in children. J Pediatr Urol. (2021) 17(1):102.e1–.e7. doi: 10.1016/j.jpurol.2020.10.031
11. Cussen LJ. Dimensions of the normal ureter in infancy and childhood. Invest Urol. (1967) 5(2):164–78.6052953
12. Hellström M, Hjälmås K, Jacobsson B, Jodal U, Odén A. Normal ureteral diameter in infancy and childhood. Acta Radiol Diagn (Stockh). (1985) 26(4):433–9. doi: 10.1177/028418518502600412
13. Doudt AD, Pusateri CR, Christman MS. Endoscopic management of primary obstructive megaureter: a systematic review. J Endourol. (2018) 32(6):482–7. doi: 10.1089/end.2017.0434
14. Baek M, Han DH. Transvesicoscopic politano-leadbetter ureteral reimplantation in children with vesicoureteral reflux: a novel surgical technique. Invest Clin Urol. (2019) 60(5):405–11. doi: 10.4111/icu.2019.60.5.405
15. Nghiem DD. A new approach to the Hostile bladder in transplantation. Transplant Proc. (2021) 53(3):825–7. doi: 10.1016/j.transproceed.2020.10.029
16. Choi H, Park JY, Bae JH. Initial experiences of laparoscopic intravesical detrusorraphy using the politano-leadbetter technique. J Pediatr Urol. (2016) 12(2):110.e1–7. doi: 10.1016/j.jpurol.2015.07.014
17. Esposito C, Varlet F, Riquelme MA, Fourcade L, Valla JS, Ballouhey Q, et al. Postoperative bladder dysfunction and outcomes after minimally invasive extravesical ureteric reimplantation in children using a laparoscopic and a robot-assisted approach: results of a multicentre international survey. BJU Int. (2019) 124(5):820–7. doi: 10.1111/bju.14785
18. García-Aparicio L, Blázquez-Gómez E, de Haro I, Garcia-Smith N, Bejarano M, Martin O, et al. Postoperative vesicoureteral reflux after high-pressure balloon dilation of the ureterovesical junction in primary obstructive megaureter. Incidence, management and predisposing factors. World J Urol. (2015) 33(12):2103–6. doi: 10.1007/s00345-015-1565-9
19. Rudin YE, Marukhnenko DV, Galitskaya DA, Aliev JK, Lagutin GV, Vardak AB. Pneumovesicoscopic ureteral reimplantation with intravesical tailoring of obstructive megaureter in pediatric patient. J Pediatr Urol. (2022) 18(2):224.e1–.e8. doi: 10.1016/j.jpurol.2021.12.004
20. Lopez M, Gander R, Royo G, Varlet F, Asensio M. Laparoscopic-Assisted extravesical ureteral reimplantation and extracorporeal ureteral tapering repair for primary obstructive megaureter in children. J Laparoendosc Adv Surg Tech Part A. (2017) 27(8):851–7. doi: 10.1089/lap.2016.0456
21. Neheman A, Shumaker A, Gal J, Haifler M, Kord E, Rappaport YH, et al. Robot-Assisted laparoscopic extravesical cross-trigonal ureteral reimplantation with tailoring for primary obstructive megaureter. Urology. (2019) 134:243–5. doi: 10.1016/j.urology.2019.09.003
22. Bakker HH, Scholtmeijer RJ, Klopper PJ. Comparison of 2 different tapering techniques in megaureters. J Urol. (1988) 140(5 Pt 2):1237–9. doi: 10.1016/s0022-5347(17)42011-8
23. González Ruiz Y, Bragagnini Rodríguez P, Siles Hinojosa A, Álvarez García N, Delgado Alvira MR, Rihuete Heras MA, et al. Is there a difference in the postoperative follow up of ureteropelvic junction obstruction according to age? Cir Pediatr. (2018) 31(2):99–103.
24. Jiang D, Tang B, Xu M, Lin H, Jin L, He L, et al. Functional and morphological outcomes of pyeloplasty at different ages in prenatally diagnosed society of fetal urology grades 3-4 ureteropelvic junction obstruction: is it safe to wait? Urology. (2017) 101:45–9. doi: 10.1016/j.urology.2016.10.004
Keywords: primary obstructive megaureter, intravesical reimplantation, Cohen, pneumovesicum, ureteral dilation
Citation: He Y, Wu X, Xu Y, Liu Z, Du G, Wu X, Liu W and Wu R (2023) Ureteral dilation recovery after intravesical reimplantation in children with primary obstructive megaureter. Front. Pediatr. 11:1164474. doi: 10.3389/fped.2023.1164474
Received: 12 February 2023; Accepted: 14 June 2023;
Published: 23 June 2023.
Edited by:
Pierluigi Marzuillo, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Gilvydas Verkauskas, Vilnius University, LithuaniaMohamed Wishahi, Theodor Bilharz Research Institute, Egypt
© 2023 He, Wu, Xu, Liu, Du, Wu, Liu and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Liu lemontree1119@126.com Rongde Wu wrd2190@163.com
 Yan He
Yan He Xuemin Wu1
Xuemin Wu1