Blood Glucose and Lactate Levels and Cerebral Oxygenation in Preterm and Term Neonates—A Systematic Qualitative Review of the Literature
- 1Division of Neonatology, Department of Paediatrics, Medical University of Graz, Graz, Austria
- 2Research Unit for Neonatal Micro- and Macrocirculation, Department of Paediatrics, Medical University of Graz, Graz, Austria
- 3Centre for the Studies of Asphyxia and Resuscitation, Royal Alexandra Hospital, Edmonton, AB, Canada
- 4Department of Pediatrics, University of Alberta, Edmonton, AB, Canada
Background: Cerebral oxygenation monitored non-invasively by near-infrared spectroscopy (NIRS) is of increasing interest in neonatal care. Cerebral oxygenation is determined by cerebral oxygen delivery and cerebral oxygen consumption. Oxygen delivery as well as oxygen consumption might be influenced by metabolic parameters like blood glucose and lactate.
Objective: The aim of the present systematic qualitative review is therefore to identify and summarize all studies, which describe cerebral oxygenation measured with NIRS and blood glucose and/or blood lactate levels in neonates.
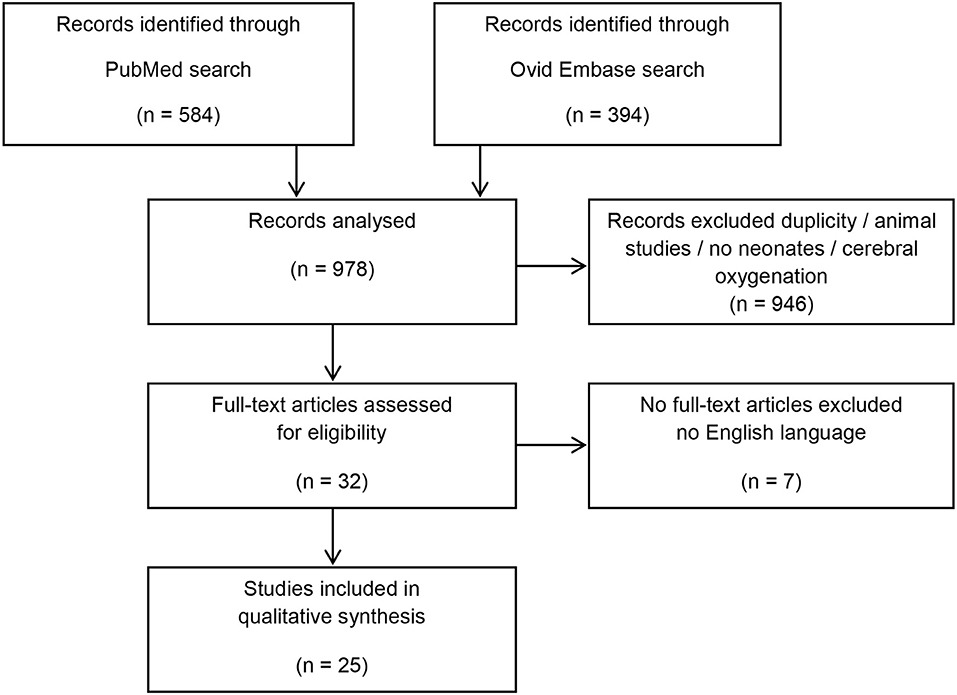
Data sources: A systematic search of Ovid Embase and PubMed was performed. Search terms included near-infrared spectroscopy, fractional tissue oxygen extraction, cerebral tissue oxygen saturation, regional cerebral tissue oxygen saturation, oxygenation, term, and preterm neonates, cesarean delivery, transition, after-birth, newborn, vaginal delivery, cesarean delivery, baby, neonatal transition, metabolism, lactate, glucose, and blood glucose level.
Study selection/data synthesis: Studies analyzing cerebral oxygenation and blood glucose and/or blood lactate levels in neonates were included. Animal studies, duplicates, or studies in non-English language were excluded.
Results: Twenty-five studies were identified that describe blood glucose and/or blood lactate levels as primary or secondary outcome parameters with additional measured cerebral oxygenation by NIRS in neonates. Twelve studies were included with blood glucose measurements: four described an association between blood glucose levels and cerebral oxygenation, two show no association, and six do not report on possible associations. Eighteen studies were included with lactate measurements: one describe an association between lactate levels and cerebral oxygenation, while three show no association and 14 do not report on possible associations.
Discussion: The influence of blood glucose and blood lactate levels on the cerebral oxygenation in neonates is still controversial. However, there seems to be an association between cerebral oxygenation and the metabolic parameter blood glucose and lactate, which need further investigation.
Introduction
Irreversible cerebral injury due to impaired cerebral oxygenation is a persisting problem in the neonatal period despite improved monitoring and intervention options. Standard non-invasive monitoring in neonatal care does not yet assess cerebral oxygenation, oxygen delivery to the brain, or cerebral oxygen consumption (1–3). However, cerebral near-infrared spectroscopy (NIRS) monitoring has the potential to detect impaired cerebral oxygenation in neonates while other vital parameters such as arterial oxygen saturation or heart rate remain within their normal range (4). NIRS is a continuous, non-invasive monitoring technique to measure the cerebral oxygenation in neonates and measures the cerebral regional oxygen saturation and fractional tissue oxygen extraction. A recently published multicenter trial using cerebral NIRS monitoring to reduce the burden of cerebral hypoxia in preterm neonates described beside cardiovascular and respiratory interventions also interventions based on blood glucose levels (5). Another recently published study describe an association between blood glucose level and cerebral oxygenation in preterm and term neonates immediately after birth (6). Further, lactate as a product of anaerobic metabolism might be associated with hypoxic conditions in the tissue. An association between the blood lactate level and the cerebral oxygenation has been described in extremely preterm neonates during the 1st days after birth (7).
The aim of the present systematic qualitative review is therefore to identify and summarize all studies, which describe cerebral oxygenation measured with NIRS and blood glucose and/or blood lactate levels in neonates.
Methods
Search Strategy and Selection Criteria
Studies were identified using the stepwise approach specified in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) Statement (8).
Eligibility Criteria
Studies had to address cerebral oxygenation measurements with NIRS as well as the metabolic parameters blood glucose and/or lactate in neonates.
Search Strategy
A systematic search of Ovid Embase and PubMed NCBI was performed to identify studies in English language published between 1974 and November 2019. Search terms included near-infrared spectroscopy, fractional tissue oxygen extraction, cerebral tissue oxygen saturation, regional cerebral tissue oxygen saturation, oxygenation, term, and preterm neonates, cesarean delivery, neonatal transition, after-birth, newborns, vaginal delivery, baby, after cesarean delivery, metabolism, lactate, glucose, and blood glucose level.
Inclusion and Exclusion Criteria—Population
To be eligible, studies had to investigate human neonates. Neonates were defined as infants with a postnatal age of <28 days. Studies that included neonates and infants or children were also included in our analysis, when the results were not separately analyzed for neonates. Animal studies were excluded.
Inclusion and Exclusion Criteria—Measurements (Exposure)
We included studies with different NIRS devices, if any additional measurements of either capillary, venous, or arterial blood glucose levels and/or lactate levels were included.
Inclusion and Exclusion Criteria—Types of Publication
We included clinical or observational studies published in English language. Non-original articles, such as comments, book chapters, editorials, reviews, and methods papers, were excluded. Duplications and publications in non-English languages were also excluded.
Study Selection
The articles identified in the literature review were evaluated independently by two authors (CM and GP) for inclusion using the titles and abstracts. Then, full texts were retrieved and were included based on the eligibility criteria. Any disagreement was resolved through discussion and consensus between two authors. If there was uncertainty regarding eligibility for inclusion on the basis of the abstract, the full text was assessed too. Data were analyzed qualitatively. Data extraction included the study design, characterization of type (preterm/term) and number of neonates included in the study, applied device, NIRS and metabolic values, age of neonates during NIRS and metabolic measurements, and the presence or absence of any association.
Risk of Bias in Individual Studies
A longer period between cerebral measurements and blood samples may originate a bias. Therefore, we included the exact time between cerebral measurements and blood samples in our qualitative analysis.
Results
After the initial search, 978 abstracts were identified, which were assessed for eligibility. After full text search, 25 studies remained to be included in the present review (Figure 1) (6, 7, 9–31).
Blood Glucose Level and Cerebral Oxygenation
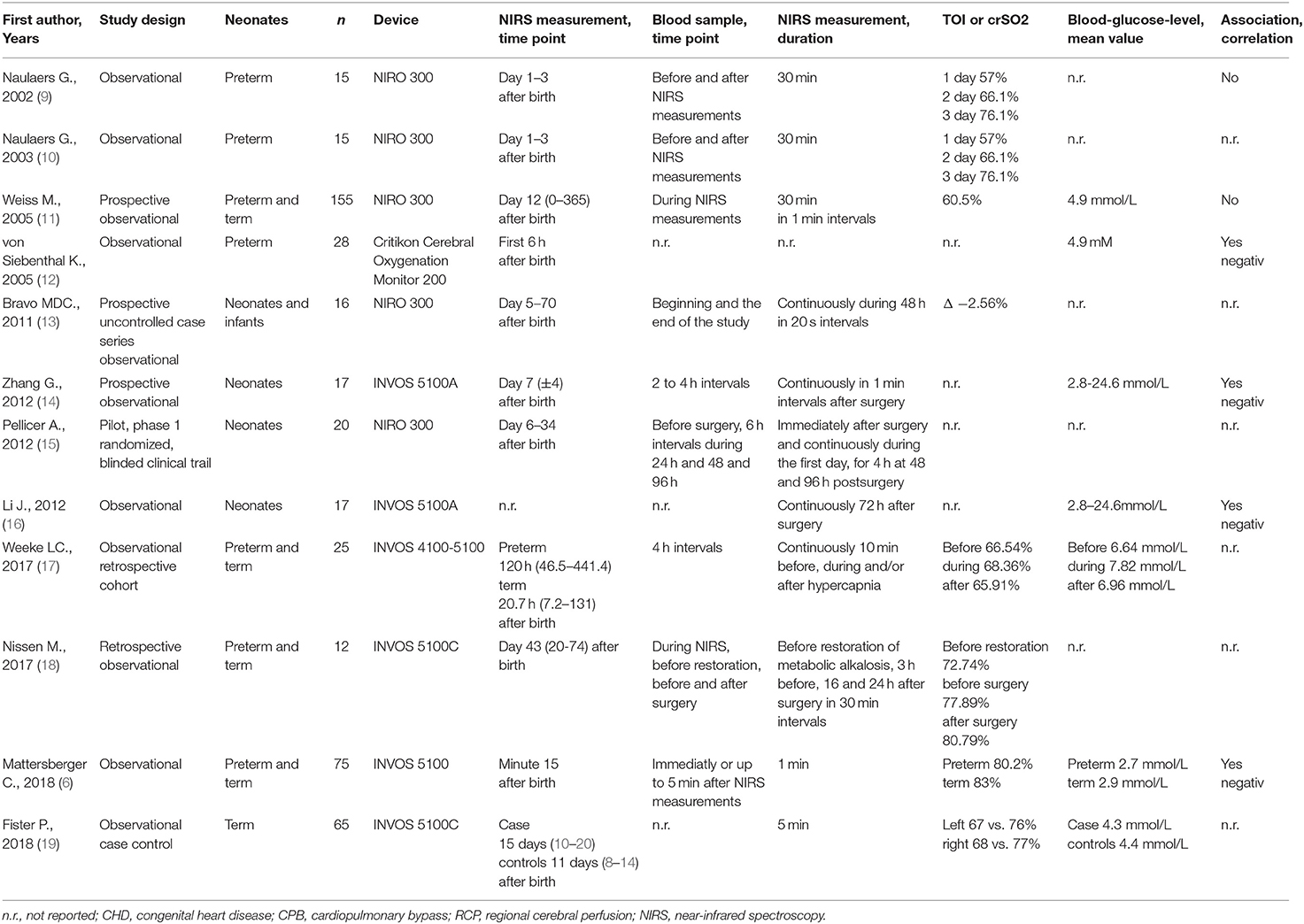
Twelve studies were identified, which describe blood glucose level measurements in combination with cerebral NIRS measurements (Table 1) (6, 9–19). Four studies describe an association (6, 12, 14, 16) between blood glucose levels and cerebral oxygenation. All studies demonstrate a negative correlation. Two studies show no association (9, 11) and six studies do not report on possible associations (10, 13, 15, 17–19).
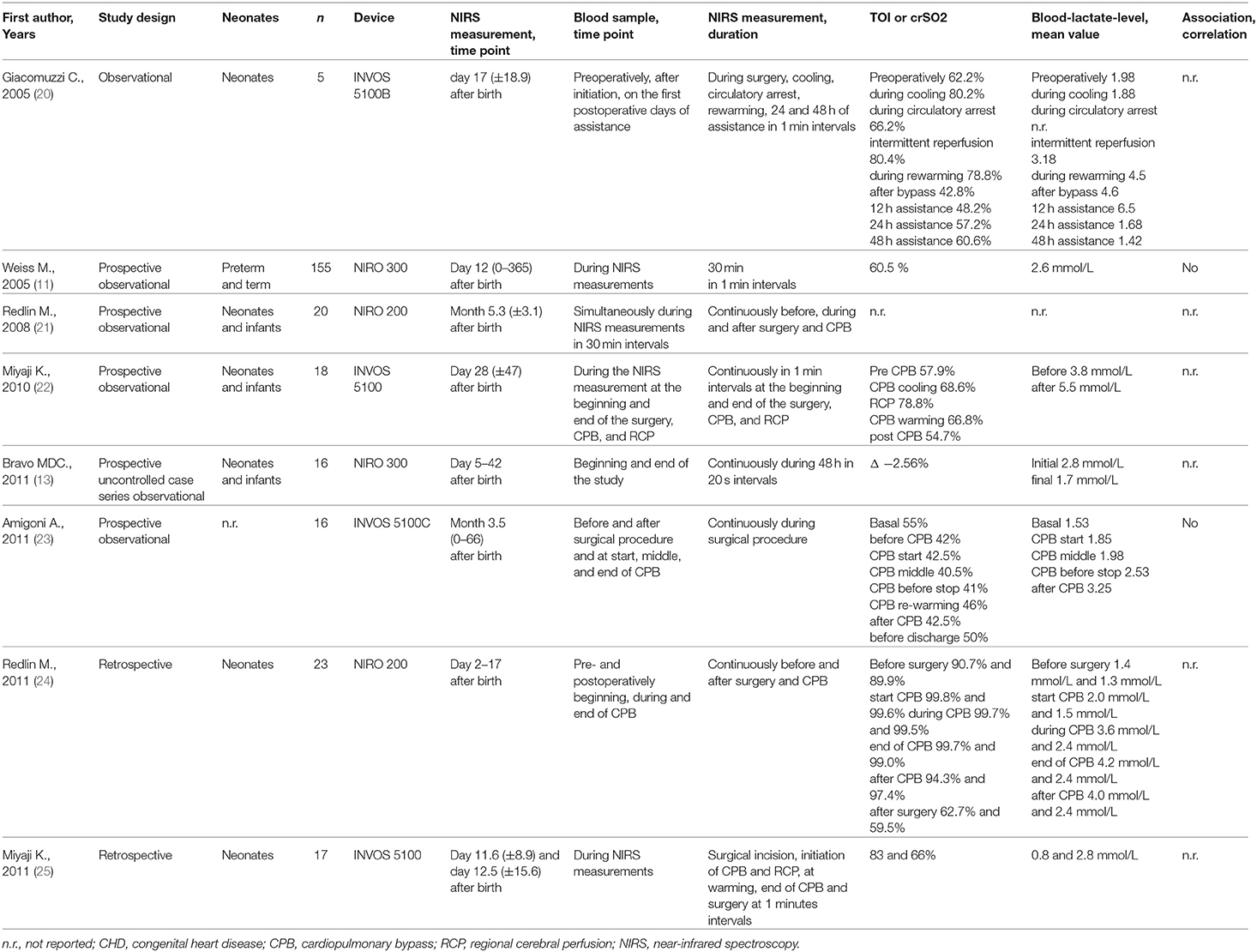
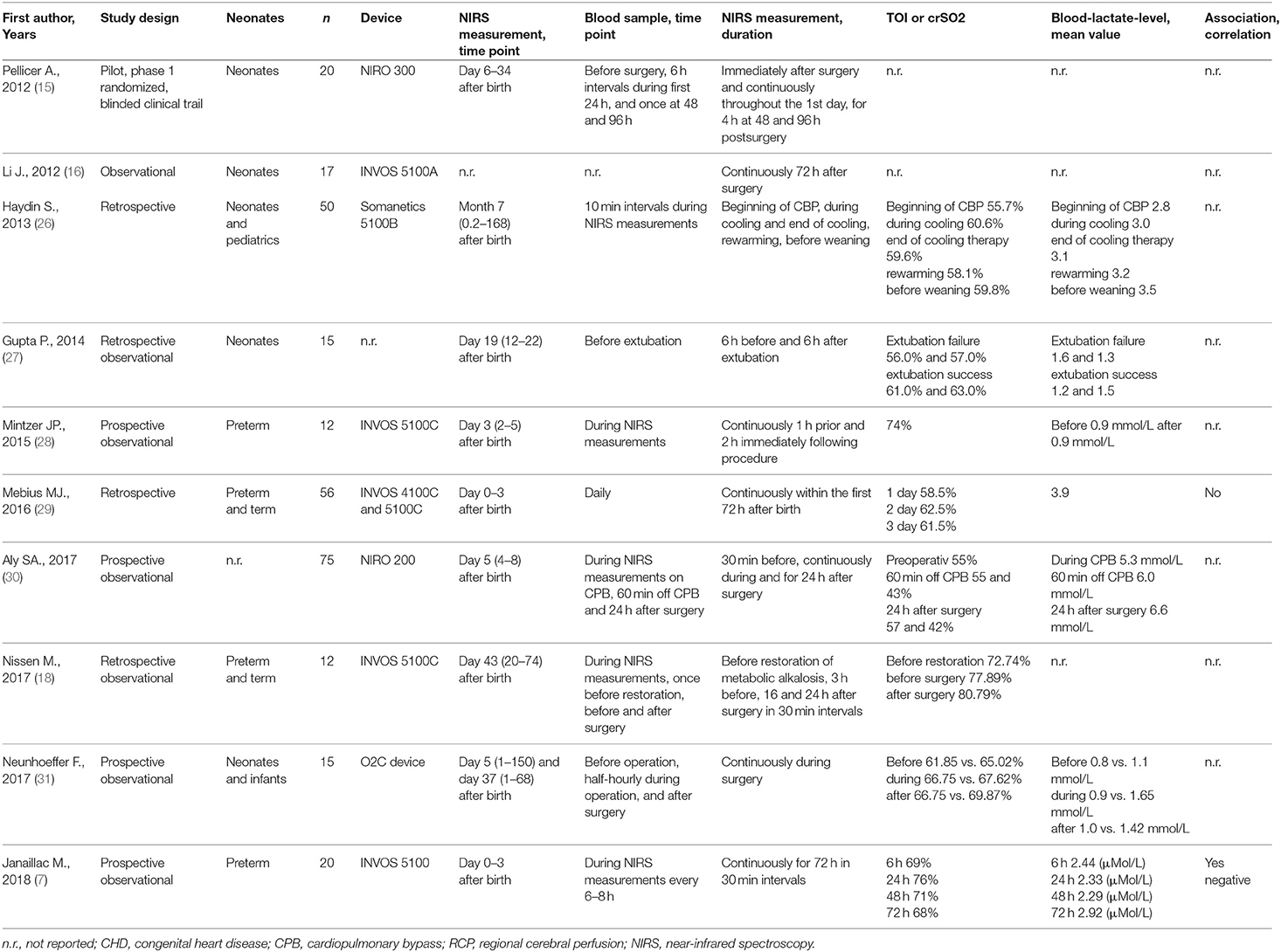
Blood Lactate Level and Cerebral Oxygenation
Eighteen studies were identified, which describe blood lactate level measurements in combination with cerebral NIRS measurements (Table 2) (7, 11, 13, 15, 16, 18, 20–31). Only one study demonstrated a negative correlation between blood lactate levels and cerebral oxygenation (7). Three studies demonstrate no association (11, 23, 29) and 14 do not report on possible associations (13, 15, 16, 18, 20–22, 24–28, 30, 31). Five studies include blood glucose level as well as blood lactate level (11, 13, 15, 16, 18).
Tables 1 and 2A,B give an overview of the data of the included studies.
None of the studies reported on possible simultaneous associations between both metabolic parameters (glucose and lactate) and cerebral oxygenation.
Discussion
In the last few years, interest into research of cerebral oxygenation and metabolic parameters during the neonatal period increased significantly. There are several studies describing results of possible or missing association between metabolic parameters and cerebral oxygenation measured with NIRS. These results are controversial.
Blood Glucose Level and Cerebral Oxygenation
Hyperglycemia has been identified as a risk factor for adverse outcome in critically ill patients (14, 16). The findings of the 12 identified studies (6, 9–19). with cerebral oxygenation measured with NIRS and blood glucose measurements are conflicting. Most studies described a negative association between cerebral oxygenation and blood glucose level (6, 12, 14, 16) with a decrease of cerebral oxygenation with increasing blood glucose levels. However, two studies described no association (9, 11). Naulears et al. (9) described an increase of cerebral oxygenation from day 1 to 3 after birth in neonates with postmenstrual age of 28 weeks. In this cohort, the multiple regression analysis showed no correlation between tissue oxygenation index and glycemia. In the largest cohort of neonates described by Weiss et al. (11) no association between blood glucose and cerebral oxygenation was observed. Interestingly, there was a negative association of blood glucose level with cerebral oxygenation observed in neonates after a Norwood procedure (14). Jia et al. (16) described a negative association between hyperglycemia and oxygen delivery. Further, she described a positive association between hyperglycemia and oxygen extraction ratio in neonates 72 h after Norwood procedure. Mattersberger et al. (6) demonstrated that blood glucose levels have a negative correlation to the cerebral oxygen saturation and a positive correlation to the cerebral fractional tissue oxygen extraction in preterm and term neonates 15 min after birth. Cerebral hemoglobin concentration that influences cerebral oxygenation, measured with NIRS, was investigated by Von Siebental K in neonates in the first 6 h of life. (12) He described different parameters influencing the cerebral hemoglobin concentration of neonates, whereby blood glucose had a negative correlation with cerebral hemoglobin concentration. The changes in cerebral hemoglobin concentration are in accordance with the above-described negative association between cerebral oxygenation and blood glucose levels when taking into account an auto-regulatory mechanism to maintain glucose supply to the brain. With decreasing blood glucose levels, there might be an increase in cerebral hemoglobin volume/concentration by increase of cerebral blood flow due to vasodilatation. This causes an increase in oxygen delivery with increase in cerebral oxygenation in case of a consistent cerebral oxygen consumption.
Lactate Level and Cerebral Oxygenation
High lactate levels might be associated with an adverse neurologic outcome and can be a predictor for short-term neonatal adverse outcomes with similar predictive value as the pH value (32). Since lactate is a product of anaerobic metabolism, an increased level of lactate might represent hypoxic conditions in the tissue. Therefore, the interest in lactate in relation to the cerebral oxygenation in the neonatal period increased in the last years. Eighteen studies were identified, which investigated cerebral oxygenation and blood lactate level in neonates (7, 11, 13, 15, 16, 18, 20–31). However, only one of these publications demonstrated a negative association between cerebral oxygenation and lactate (7), and three studies found no association (11, 23, 29) between these factors.
Weiss et al. (11) described, in the largest cohort of critically ill neonates, no significant correlation between cerebral oxygenation and lactate. Amigoni et al. (23) also did not find an association between serum lactate and cerebral oxygenation. However, they described a correlation between pH value and cerebral oxygenation. Mebius et al. assessed the course of cerebral regional oxygen saturation and clinical factors in neonates born with duct-dependent congenital heart disease and found no correlation during the first 72 h after birth (29). In extremely preterm infants, it has been demonstrated that the crSO2 and preductal perfusion index were weakly correlated with lactate and blood gas (7).
Limitation
The identified publications show many differences in methods: (e.g., study population, number of included neonates, NIRS devices, time point, and frequency of NIRS measurements). Important limitations are also the differences in frequencies of blood samples and differences in time periods between taking blood samples and NIRS measurements, ranging from 5 min (6) to 24 h (29). Several studies even provide no or inaccurate information on frequencies and time points of taking blood samples (11, 12, 16, 19, 27). This review identified only observational studies, where associations between cerebral oxygenation and blood glucose and/or lactate levels are described. No interventional study was identified elucidating any causality. Furthermore, there were several studies just describing cerebral oxygenation and blood glucose or lactate in neonates without analyzing any possible associations between these parameters.
Conclusion
The influence of blood glucose level and blood lactate level on the cerebral oxygenation in neonates is still controversial. However, there is some evidence that there is an association between cerebral oxygenation and the metabolic parameters, blood glucose, and blood lactate, whereby causal relationship needs further investigation.
Author Contributions
CM, GP, and BU: conception and design. CM and GP: literature search and drafting of the article. CM, GS, BU, and GP: analyses and interpretation of data, critical revision, editing, and final approval of the article. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. O'Donnell CPF, Kamlin COF, Davis PG, Morley CJ. Feasibility of and delay in obtaining pulse oximetry during neonatal resuscitation. J Pediatr. (2005) 147:698–9. doi: 10.1016/j.jpeds.2005.07.025
2. Finer N, Leone T. Oxygen saturation monitoring for the preterm infant: the evidence basis for current practice. Pediatr Res. (2009) 65:375–80. doi: 10.1203/PDR.0b013e318199386a
3. Dawson JA, Morley CJ. Monitoring oxygen saturation and heart rate in the early neonatal period. Semin Fetal Neonatal Med. (2010) 15:203–7. doi: 10.1016/j.siny.2010.03.004
4. Baik N, Urlesberger B, Schwaberger B, Schmölzer GM, Avian A, Pichler G. Cerebral haemorrhage in preterm neonates: does cerebral regional oxygen saturation during the immediate transition matter? Arch Dis Child Fetal Neonatal Ed. (2015) 100:F422–7. doi: 10.1136/archdischild-2014-307590
5. Pellicer A, Greisen G, Benders M, Claris O, Dempsey E, Fumagalli M, et al. The SafeBoosC phase II randomised clinical trial: a treatment guideline for targeted near-infrared-derived cerebral tissue oxygenation versus standard treatment in extremely preterm infants. Neonatology. (2013) 104:171–8. doi: 10.1159/000351346
6. Mattersberger C, Baik-Schneditz N, Schwaberger B, Schmölzer GM, Mileder L, Pichler-Stachl E, et al. Blood glucose and cerebral tissue oxygenation immediately after birth—an observational study. J Pediatr. (2018) 200:19–23. doi: 10.1016/j.jpeds.2018.05.008
7. Janaillac M, Beausoleil TP, Barrington KJ, Raboisson M-J, Karam O, Dehaes M, et al. Correlations between near-infrared spectroscopy, perfusion index, and cardiac outputs in extremely preterm infants in the first 72 h of life. Eur J Pediatr. (2018) 177:541–50. doi: 10.1007/s00431-018-3096-z
8. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Loannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. (2009) 339:b2700. doi: 10.1136/bmj.b2700
9. Naulaers G, Morren G, van Huffel S, Casaer P, Devlieger H. Cerebral tissue oxygenation index in very premature infants. Arch Dis Child Fetal Neonatal Ed. (2002) 1053:189–92. doi: 10.1136/fn.87.3.F189
10. Naulaers G, Morren G, van Huffel S, Casaer P, Devlieger H. Measurement of tissue oxygenation index during the first three days in premature born infants. Adv Exp Med Biol. (2003) 510:379–83. doi: 10.1007/978-1-4615-0205-0_63
11. Weiss M, Dullenkopf A, Kolarova A, Schulz G, Frey B, Baenziger O. Near-infrared spectroscopic cerebral oxygenation reading in neonates and infants is associated with central venous oxygen saturation. Paediatr Anaesth. (2005) 15:102–9. doi: 10.1111/j.1460-9592.2005.01404.x
12. von Siebenthal K, Keel M, Fauchère J-C, Dietz V, Haensse D, Wolf U, et al. Variability of cerebral hemoglobin concentration in very preterm infants during the first 6 h of life. Adv Exp Med Biol. (2005) 566:91–7. doi: 10.1007/0-387-26206-7_13
13. Bravo MDC, López P, Cabañas F, Pérez-Rodríguez J, Pérez-Fernández E, Pellicer A. Acute effects of levosimendan on cerebral and systemic perfusion and oxygenation in newborns: an observational study. Neonatology. (2011) 99:217–23. doi: 10.1159/000314955
14. Zhang G, Cai S, Li J. Hyperglycaemia is negatively associated with systemic and cerebral oxygen transport in neonates after the Norwood procedure. Cardiol Young. (2012) 22:49–56. doi: 10.1017/S1047951111000904
15. Pellicer A, Riera J, Lopez-Ortego P, Bravo MC, Madero R, Perez-Rodriguez J, et al. Phase 1 study of two inodilators in neonates undergoing cardiovascular surgery. Pediatr Res. (2013) 73:95–103. doi: 10.1038/pr.2012.154
16. Li J. Systemic oxygen transport derived by using continuous measured oxygen consumption after the Norwood procedure? an interim review. Interact Cardiovasc Thorac Surg. (2012) 15:93–101. doi: 10.1093/icvts/ivs089
17. Weeke LC, Dix LML, Groenendaal F, Lemmers PMA, Dijkman KP, Andriessen P, et al. Severe hypercapnia causes reversible depression of aEEG background activity in neonates: an observational study. Arch Dis Child Fetal Neonatal Ed. (2017) 102:F383–8. doi: 10.1136/archdischild-2016-311770
18. Nissen M, Cernaianu G, Thränhardt R, Vahdad MR, Barenberg K, Tröbs R-B. Does metabolic alkalosis influence cerebral oxygenation in infantile hypertrophic pyloric stenosis. J Surg Res. (2017) 212:229–37. doi: 10.1016/j.jss.2017.01.019
19. Fister P, Robek D, Paro-Panjan D, Mazić U, Lenasi H. Decreased tissue oxygenation in newborns with congenital heart defects: a case-control study. Croat Med J. (2018) 59:71–9. doi: 10.3325/cmj.2018.59.71
20. Giacomuzzi C, Heller E, Mejak B, You J, Ungerleider R, Silberbach M. Assessing the brain using near-infrared spectroscopy during postoperative ventricular circulatory support. Cardiol Young. (2005) 15:154–8. doi: 10.1017/s1047951105001204
21. Redlin M, Koster A, Huebler M, Boettcher W, Nagdyman N, Hetzer R, et al. Regional differences in tissue oxygenation during cardiopulmonary bypass for correction of congenital heart disease in neonates and small infants: relevance of near-infrared spectroscopy. J Thorac Cardiovasc Surg. (2008) 136:962–7. doi: 10.1016/j.jtcvs.2007.12.058
22. Miyaji K, Miyamoto T, Kohira S, Itatani K, Tomoyasu T, Inoue N, et al. Regional high-flow cerebral perfusion improves both cerebral and somatic tissue oxygenation in Aortic arch repair. Ann Thorac Surg. (2010) 90:593–9. doi: 10.1016/j.athoracsur.2010.03.113
23. Amigoni A, Mozzo E, Brugnaro L, Tiberio I, Pittarello D, Stellin G, et al. Four-side near-infrared spectroscopy measured in a paediatric population during surgery for congenital heart disease. Interact Cardiovasc Thorac Surg. (2011) 12:707–12. doi: 10.1510/icvts.2010.253328
24. Redlin M, Huebler M, Boettcher W, Kukucka M, Schoenfeld H, Hetzer R, et al. Minimizing intraoperative hemodilution by use of a very low priming volume cardiopulmonary bypass in neonates with transposition of the great arteries. J Thorac Cardiovasc Surg. (2011) 142:875–81. doi: 10.1016/j.jtcvs.2011.01.068
25. Miyaji K, Miyamoto T, Kohira S, Yoshii T, Itatani K-I, Sato H, et al. The effectiveness of high-flow regional cerebral perfusion in Norwood stage I palliation. Eur J Cardio Thoracic Surg. (2011) 40:1215–20. doi: 10.1016/j.ejcts.2011.02.040
26. Haydin S, Onan B, Onan IS, Ozturk E, Iyigun M, Yeniterzi M. Cerebral perfusion during cardiopulmonary bypass in children: correlations between near-infrared spectroscopy, temperature, lactate, pump flow, and blood pressure. Artif Organs. (2013) 37:87–91. doi: 10.1111/j.1525-1594.2012.01554.x
27. Gupta P, McDonald R, Goyal S, Gossett JM, Imamura M, Agarwal A, et al. Extubation failure in infants with shunt-dependent pulmonary blood flow and univentricular physiology. Cardiol Young. (2014) 24:64–72. doi: 10.1017/S1047951112002181
28. Mintzer JP, Parvez B, Alpan G, LaGamma EF. Effects of sodium bicarbonate correction of metabolic acidosis on regional tissue oxygenation in very low birth weight neonates. J Perinatol. (2015) 35:601–6. doi: 10.1038/jp.2015.37
29. Mebius MJ, van der Laan ME, Verhagen EA, Roofthooft MT, Bos AF, Kooi EM. Cerebral oxygen saturation during the first 72 h after birth in infants diagnosed prenatally with congenital heart disease. Early Hum Dev. (2016) 103:199–203. doi: 10.1016/j.earlhumdev.2016.10.001
30. Aly SA, Zurakowski D, Glass P, Skurow-Todd K, Jonas RA, Donofrio MT. Cerebral tissue oxygenation index and lactate at 24 hours postoperative predict survival and neurodevelopmental outcome after neonatal cardiac surgery. Congenit Heart Dis. (2017) 12:188–95. doi: 10.1111/chd.12426
31. Neunhoeffer F, Warmann SW, Hofbeck M, Müller A, Fideler F, Seitz G, et al. Elevated intrathoracic CO2 pressure during thoracoscopic surgery decreases regional cerebral oxygen saturation in neonates and infants-A pilot study. Paediatr Anaesth. (2017) 27:752–9. doi: 10.1111/pan.13161
Keywords: neonates, blood glucose, lactate, near-infrared spectroscopy, cerebral oxygenation
Citation: Mattersberger C, Schmölzer GM, Urlesberger B and Pichler G (2020) Blood Glucose and Lactate Levels and Cerebral Oxygenation in Preterm and Term Neonates—A Systematic Qualitative Review of the Literature. Front. Pediatr. 8:361. doi: 10.3389/fped.2020.00361
Received: 11 March 2020; Accepted: 29 May 2020;
Published: 29 July 2020.
Edited by:
Elisabeth M. W. Kooi, University Medical Center Groningen, NetherlandsReviewed by:
Anne Elisabeth Richter, University Medical Center Groningen, NetherlandsLizelle Van Wyk, Stellenbosch University, South Africa
Copyright © 2020 Mattersberger, Schmölzer, Urlesberger and Pichler. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gerhard Pichler, gerhard.pichler@medunigraz.at
†ORCID: Gerhard Pichler orcid.org/0000-0003-2405-7143
 Christian Mattersberger
Christian Mattersberger Georg M. Schmölzer
Georg M. Schmölzer Berndt Urlesberger
Berndt Urlesberger Gerhard Pichler
Gerhard Pichler