- 1Department of Endoscopy, Affiliated Cancer Hospital and Institute of Guangzhou Medical University, Guangzhou, China
- 2Department of Nuclear Medicine, Affiliated Cancer Hospital and Institute of Guangzhou Medical University, Guangzhou, China
Objective: To evaluate the detection ability of 18F-FDG PET/CT for identifying high-risk lesions (high-risk adenomas and adenocarcinoma) from incidental focal colorectal 18F-FDG uptake foci combining maximum standard uptake value (SUVmax) and localized colonic wall thickening (CWT). The secondary objective was to investigate the factors of missed detection of high-risk adenomas by 18F-FDG PET/CT.
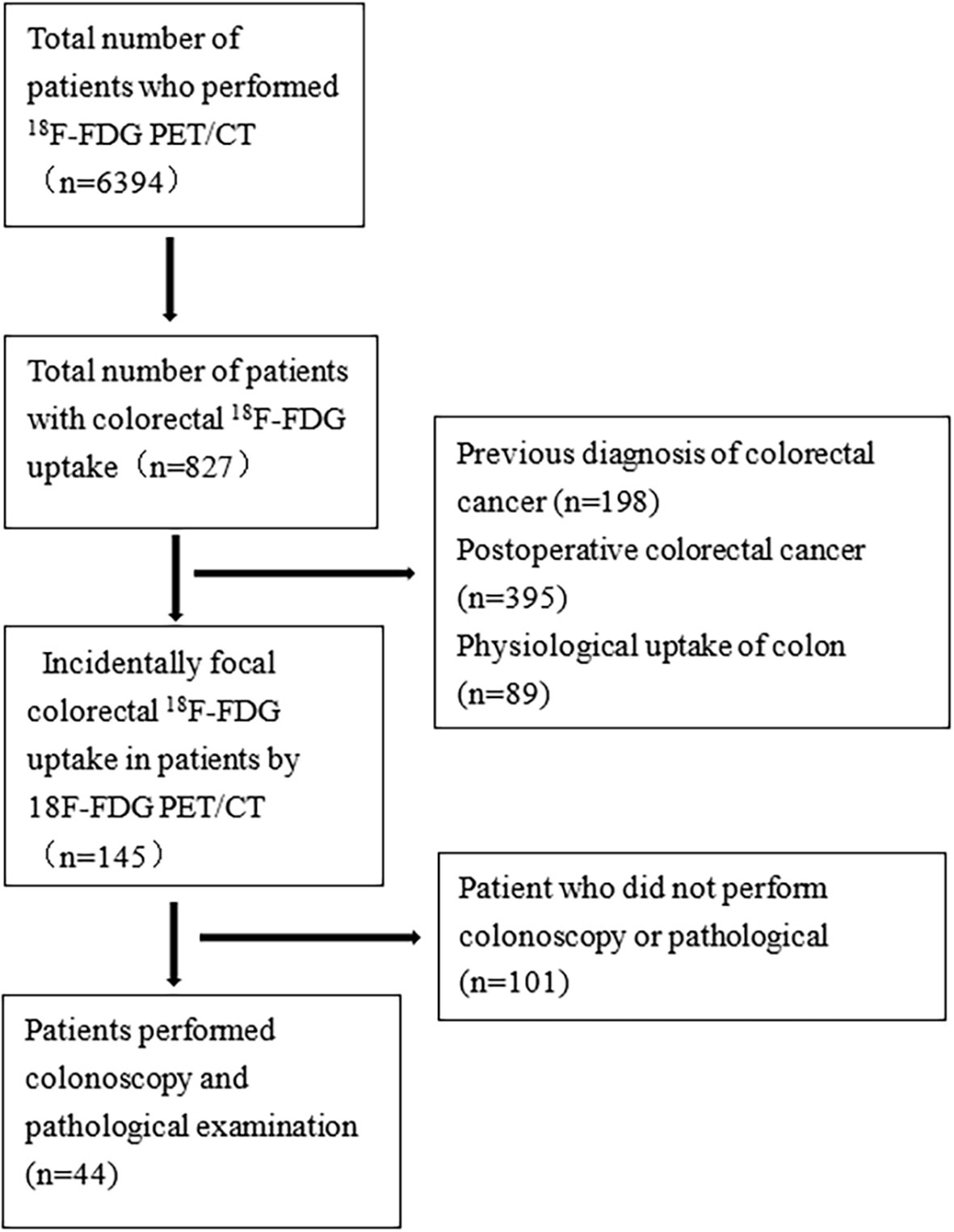
Patients and methods: A total of 6394 patients who underwent 18F-FDG PET/CT in our hospital from August 2019 to December 2021 were retrospectively analysed, and 145 patients with incidental focal colorectal 18F-FDG uptake foci were identified. The optimal cut-off value of SUVmax for 18F-FDG PET/CT diagnosis of high-risk lesions was determined by receiver operating characteristic (ROC) curves. SUVmax and localized CWT were combined to identify high-risk lesions from incidental focal colorectal 18F-FDG uptake foci. The characteristics of incidental adenomas detected and high-risk adenomas missed by 18F-FDG PET/CT were compared.
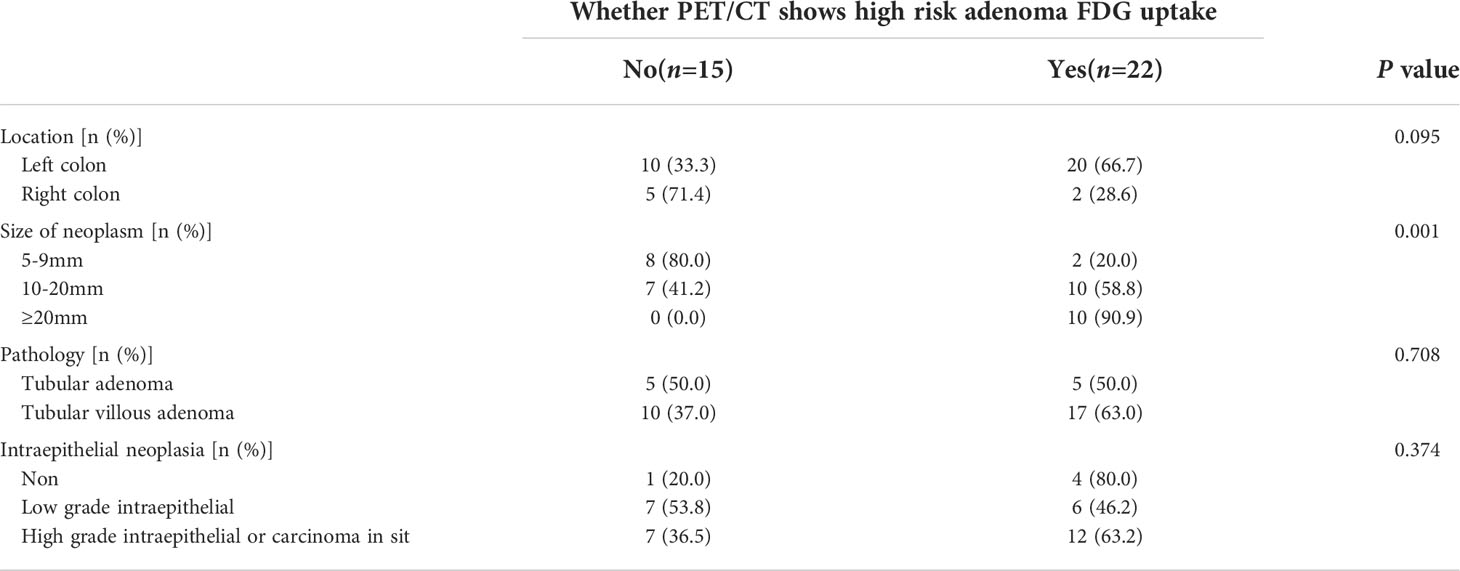
Results: Of the 6394 patients, 145 patients were found to have incidental focal colorectal FDG uptake foci (2.3%), and 44 patients underwent colonoscopy and pathological examination at the same time. In fact, 45 lesions, including 12 low-risk lesions and 33 high-risk lesions (22 high-risk adenomas, 11 adenocarcinoma), were found by colonoscopy. The area under the ROC curve of SUVmax for low-risk lesions and high-risk lesions was 0.737, and the optimal cut-off value was 6.45 (with a sensitivity of 87.9% and specificity of 58.3%). When SUVmax ≥6.45, the combination of localized CWT parameters has little influence on the sensitivity and specificity of detection; when SUVmax <6.45, the combination of localized CWT parameters can improve the specificity of detection of high-risk lesions, but the sensitivity has little change. In addition, the size of high-risk adenomas discovered incidentally by 18F-FDG PET/CT was larger than that of high-risk adenomas missed, but there was no significant difference in lesion location, pathological type or intraepithelial neoplasia between the two groups.
Conclusions: The combination of SUVmax and localized CWT parameters of 18F-FDG PET/CT helped identify high-risk lesions from incidental focal colorectal 18F-FDG uptake foci, especially for lesions with SUVmax <6.45. Lesion size may be the only factor in 18F-FDG PET/CT missing high-risk adenomas.
Introduction
F-18 fluorodeoxyglucose (18F-FDG) positron emission tomography (PET/CT) has become one of the most commonly used positron emission radiography examinations for various oncology imaging, has been used for tumour diagnosis, staging and therapeutic effect prediction and evaluation (1–3), and has been applied to screen second primary cancer in cancer patients (4).
18F-FDG PET/CT examination incidentally shows unexpected abnormal areas while performing these functions for patients with noncolorectal indications. Segmental or diffuse uptake of colorectal tissue is often indicative of physiological uptake or inflammatory lesions, while focal FDG uptake is often more important and may indicate colorectal tumours (5–7). Incidental focal colorectal 18F-FDG uptake is a relatively rare event, and the incidence of incidental colorectal 18F-FDG uptake with PET/CT is approximately 2% (8). Colonoscopy is a powerful method to detect colorectal lesions, and endoscopic resection of adenomatous polyps can reduce the mortality of colorectal cancer (9). However, it is an invasive examination. There are risks of intestinal perforation, intestinal bleeding and anaesthesia (10, 11), and intestinal preparation is troublesome (12). Some frail cancer patients may not be able to tolerate colonoscopy. Whether cancer patients with incidental focal colorectal 18F-FDG uptake foci during 18F-FDG PET/CT examinations undergo further colonoscopy is still controversial. There is still no consensus on the best strategy. SUVmax represents the maximum standard uptake value of PET during scanning and the quantitative index of the radioactive uptake value of lesions. Increased SUVmax may indicate malignancy. Localized CWT is one of the appearances of the colonic wall on CT of the abdomen, which may also suggest the presence of an underlying neoplasia (13). These two parameters are available in 18F-FDG PET/CT. To our knowledge, however, few studies have combined these two parameters to assess whether incidental focal colorectal 18F-FDG uptake foci. In this study, we combined SUVmax with localized CWT to distinguish whether incidentally focal colorectal 18F-FDG uptake foci are high-risk lesions and should be recommended for further colonoscopy. The secondary objective of this study was to investigate the factors contributing to the missed detection of high-risk adenomas by 18F-FDG PET/CT.
Methods
Patients and methods
This study is a retrospective study and has been approved by the Institutional Ethics Committee of the Affiliated Cancer Hospital and Institute of Guangzhou Medical University, and the requirement to obtain written informed consent was waived. The information on the patients in our study was mainly obtained from the endoscopy, radiology, and pathology databases of our hospital. The data of patients who underwent 18F-FDG PET/CT and colonoscopy from August 2019 to December 2021 were reviewed. During the study, 6394 patients underwent 18F-FDG PET/CT at the Affiliated Cancer Hospital and Institute of Guangzhou Medical University. A total of 682 patients were found to have abnormal colorectal 18F-FDG uptake on 18F-FDG PET/CT examination. Among them, 198 patients diagnosed with colorectal cancer, 395 patients with postoperative colorectal cancer and 89 patients with physiological uptake were excluded. Finally, 145 patients with incidental colorectal 18F-FDG uptake foci were found by 18F-FDG PET/CT, of whom 44 patients underwent colonoscopy and pathological biopsy examination at the same time (Figure 1). High-risk adenomas were defined as those with a diameter greater than or equal to 10 mm, with villous composition (>25.0%) or with high-grade intraepithelial neoplasia or above (14).
18F-FDG PET/CT protocal
All eligible patients underwent PET/CT scanning (Discovery 710, GE healthcare, Milwaukee, WI, USA) after fasting for at least 6 hours to maintain venous blood glucose levels below 10 mmol/L before administration of 18F-FDG. Preexamination blood glucose levels were recorded. Then, patients were intravenously injected with 18F-FDG and quietly rested for 60 minutes. CT scan was performed from cranial top to plantar first, with a current of 80-250mA, a total voltage 120kV, a layer thickening of 5.0mm and rotation time of 0.5s; PET image was acquired from cranial top scan to planta for 60-70s per bed and was reconstructed by ordered subset maximum expected value method (OSEM) with 33 subset and 512×512 matrix. Coronal plane, sagittal plane, cross section and maximum density projection image were obtained by CT attenuation correction.
Image analysis
All data were transferred to the Advantage Workstation (version AW 4.7, GE Healthcare, Milwaukee, WI, USA) and reconstructed using the Bayesian penalized likelihood reconstruction algorithm (Q.clear, GE Healthcare, Milwaukee, WI, USA) with penalization factor (beta) of 500. The semi-automatic quantitative measurements began with manually placement of an oval frame that needed to be drawn to include primary lesions and adjusted to exclude organs with high physiological uptake. SUVmax would be calculated and generated automatically after work frame is placed.
18F-FDG PET/CT reports were recorded by junior physicians in the nuclear medicine department and reviewed by experienced 18F-FDG PET/CT nuclear medicine specialists. According to the location, shape, size, localized CWT, radioactivity distribution, and SUVmax of the lesions, the characteristic of suspicious colorectal lesions was diagnosed by specialists. Besides, ≥3mm for the colon and ≥5mm for the rectum were considered as increased wall thickness. Localized thickening was defined as CWT that was localized and present in only one of parts of the colon.
Colonoscopy examination
All eligible patients underwent dietary preparation on a half-flow diet 2 days in advance and then a liquid diet 1 day in advance. Polyethylene glycol electrolytes (PGE; 137.15g; Shenzhen Wanhe Pharmaceutical Co., Ltd, Shenzhen, Guangdong Province, China) dissolved with 2000mL water was administered for bowel preparation six hours before colonoscopy examinations. Complete colonoscopy (Olympus CV-290, Olympus Medical Systems Corp, Tokyo, Japan) from caecal insertion to withdrawal of the colonoscopy was perform using the LCI or WL in all patients. The bowel cleanliness score (Boston score) was ≥7 in all patients (15). If colorectal neoplasms were found during the inspection, their size and location in the colon were estimated by the endoscopic physicians. All data were transferred to the Annet Medical Image Workstation (AnnetWS, Shenzhen Annet Information System Co., Ltd, Shenzhen, Guangdong Province, China). Endoscopic biopsy or electric resection was performed for pathological analysis.
Data collection and analysis
The statistical description of numerical variable data is expressed as the mean (x ± s), and the statistical description of categorical variable data is expressed as the constituent ratio (%). T test or Mann–Whitney U test was used for statistical data, and Chi-square test or Fisher’s exact probability method was used for statistical data. We applied ROC curves, showing sensitivity and specificity, to evaluate the optimal cut-off value for SUVmax in differentiating colorectal high-risk lesions. P<0.05 was considered statistically significant. SPSS 16.0 software (Chicago, IL, United States) was used in the statistical process. GraphPad Prism 8.0.2 software was used for the mapping.
Results
Basic patient characteristics
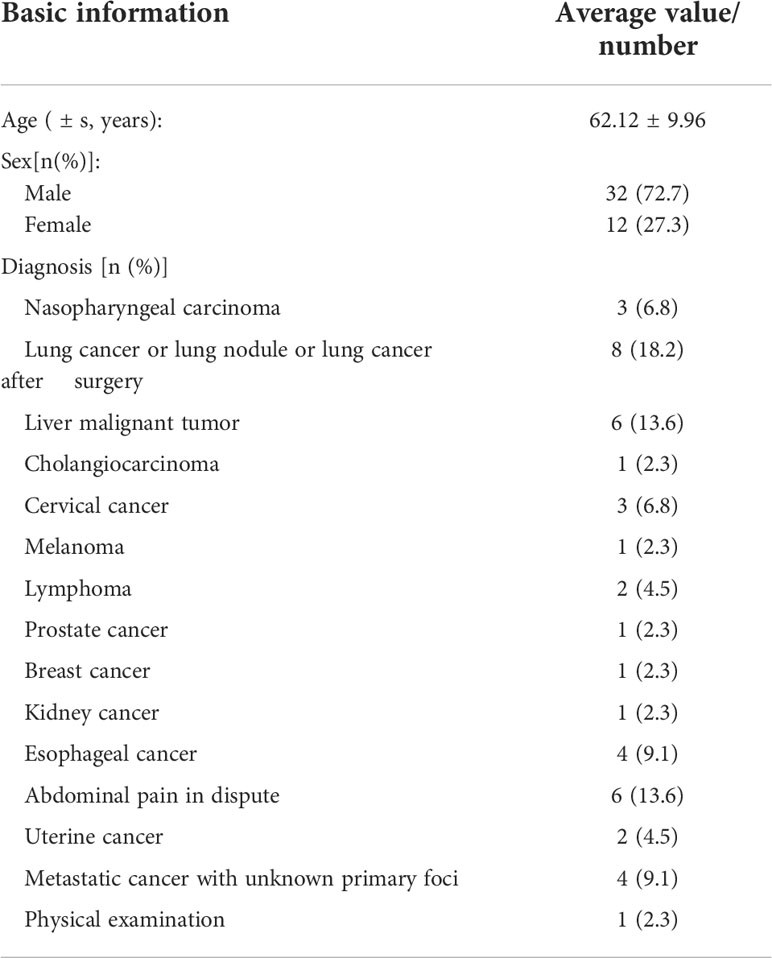
18F-FDG PET/CT found 44 patients with incidental focal colorectal FDG uptake foci (Figures 2, 3). Among the 44 patients with incidental focal colorectal 18F-FDG uptake, there were 32 males and 12 females, with an average age of 62.12 ± 9.96 years (37-78 years), and the top three indications of 18F-FDG PET/CT examination were lung cancer or lung nodule or lung cancer after surgery (18.2%), malignant liver tumour (13.6%) and metastatic cancer with unknown primary foci (9.1%). (Table 1).
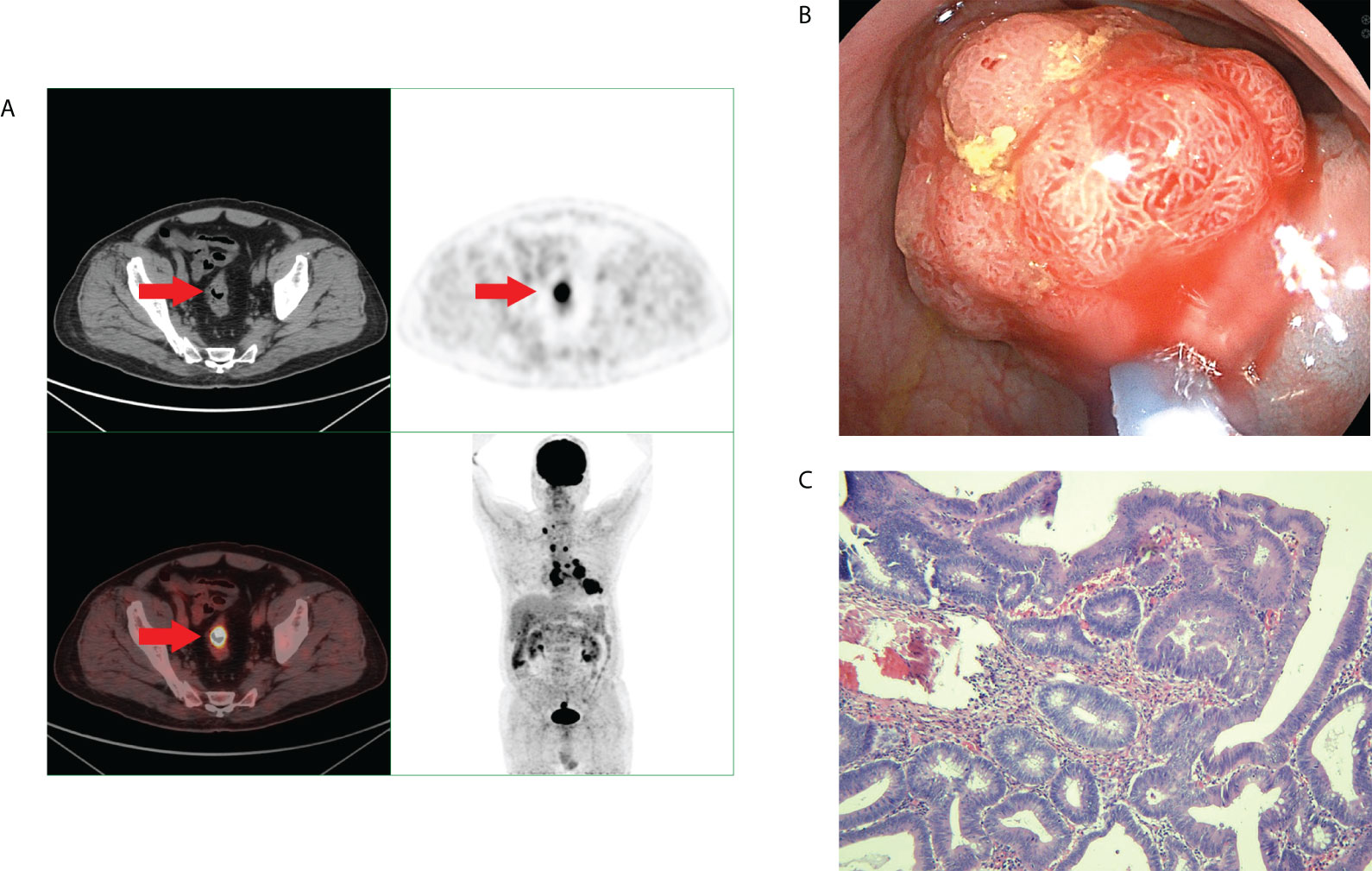
Figure 2 A middle-aged man underwent 18F-FDG PET/CT for left lung squamous cell carcinoma. Incidental focal 18F-FDG uptake was found in thesigmoid colon. The patient underwent colonoscopy and pathology examination. (A) Abnormal 18F-FDG PET/CT uptake in the sigmoid colon. (B) shows a sigmoid colonpolyp with a diameter of 2.5 cm. (C) shows the pathological pattern of villous tubular adenoma with high-grade intraepithelial neoplasia.
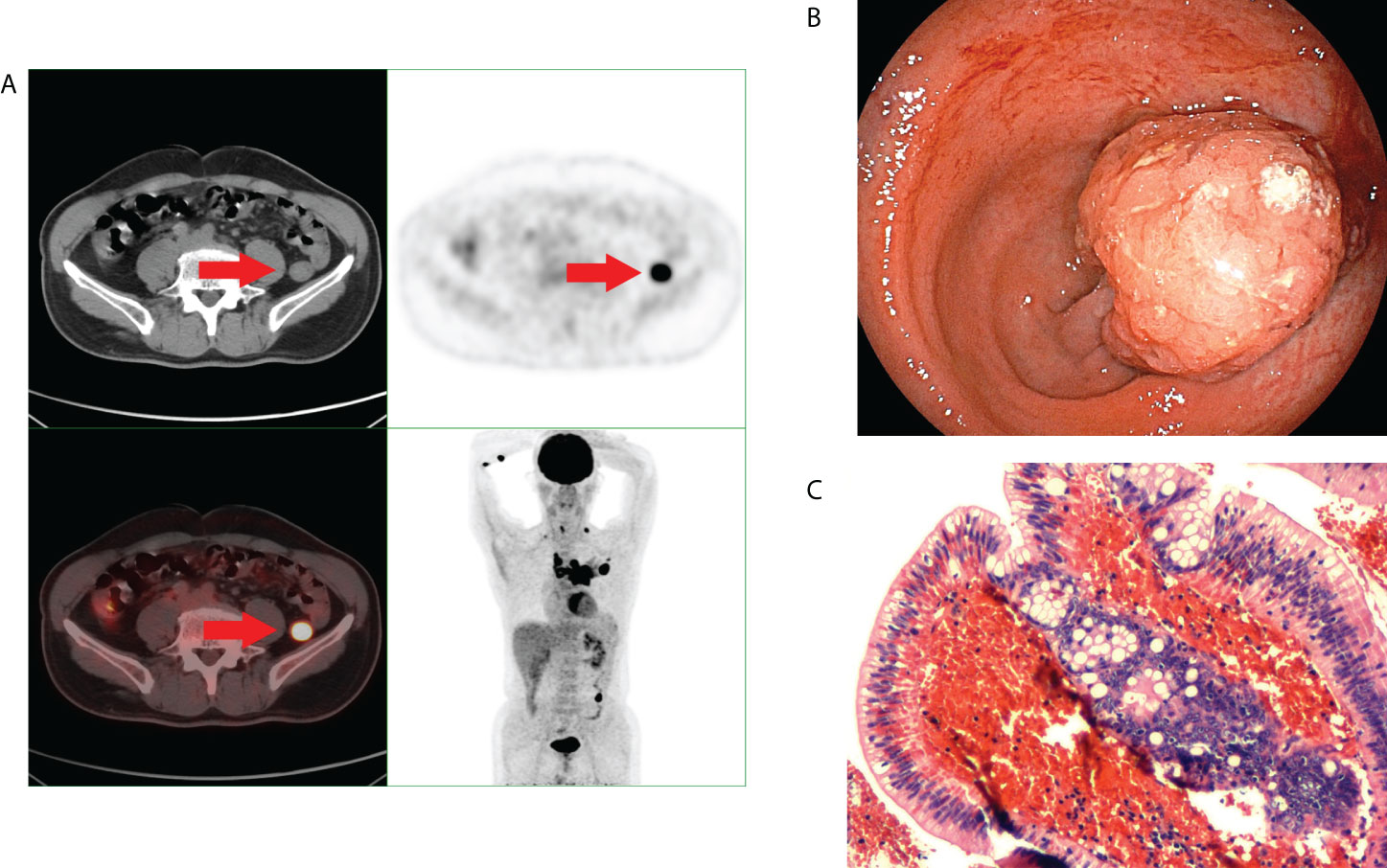
Figure 3 A middle-aged man underwent 18F-FDG PET/CT for left pulmonary nodules. Incidental focal uptake of 18F-FDG was found in the rectum. The patient underwent colonoscopy and pathology examination. (A) Abnormal uptake of 18F-FDG PET/CT in the rectum. (B) shows a colonoscopic pedicled polyp with a diameter of approximately 2.0 cm. (C) shows the pathological type of villous tubular adenoma.
SUVmax in identifying high-risk lesions
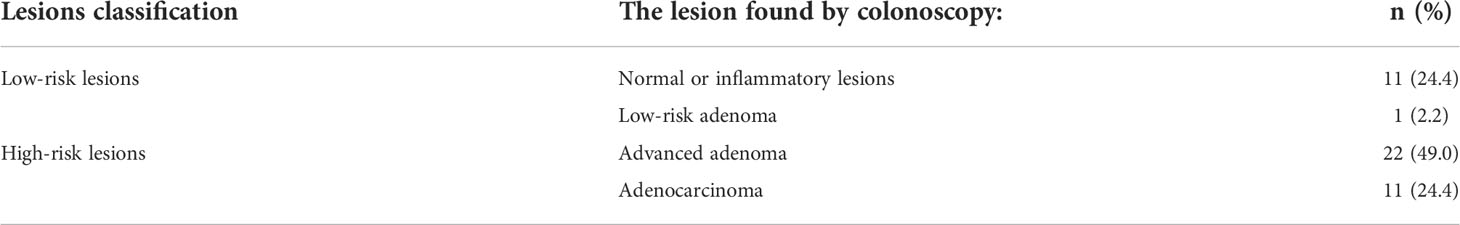
Among the 44 patients with focal incidental colorectal 18F-FDG uptake foci, 45 lesions were detected by 18F-FDG PET/CT, and 34 lesions were confirmed to be true positive by colonoscopy and pathological results, with a positive predictive value of 75.56%. Among them, low-risk adenoma was found in one patient (2.2%), high-risk adenomas in 22 patients (49.0%) and adenocarcinoma in 11 patients (24.4%). No lesions or inflammatory lesions were found in 11 patients (24.4%) (Table 2). We classified normal or inflammatory lesions and low-risk adenoma into one group (low-risk lesion group) and found that the SUVmax in the low-risk lesion group was lower than that in the high-risk adenoma group and adenocarcinoma group (P<0.05). However, there was no significant difference in SUVmax between the high-risk adenoma group and the adenocarcinoma group (P=0.774) (Figure 4A). From the perspective of clinical practice, both high-risk adenomas and adenocarcinoma need to be actively treated. High-risk adenomas and adenocarcinoma with no statistically significant difference in SUVmax were classified into another group (high-risk lesions group). The optimal cut-off point of SUVmax obtained by ROC to distinguish the high-risk lesion group from the low-risk lesion group was 6.45 (Figure 4B). When SUVmax=6.45, the sensitivity and specificity were 87.9% and 58.3%, respectively.
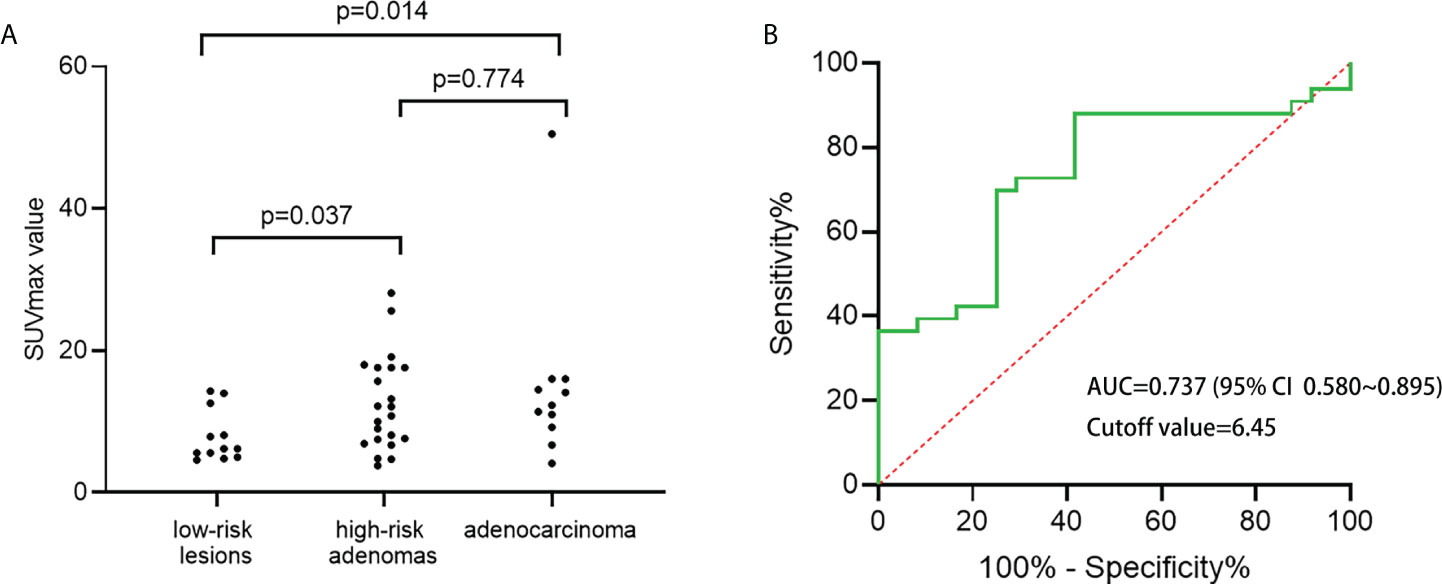
Figure 4 (A) SUVmax of low-risk, high-risk adenomas, adenocarcinoma were compared; (B) ROC curve of maximum standardized uptake value (SUVmax) for high-risk lesions.
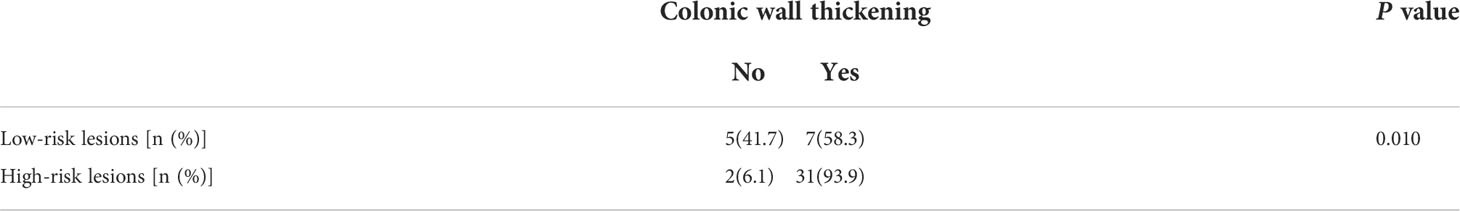
SUVmax and localized CWT in identifying high-risk lesions
Among the 45 lesions found by 18F-FDG PET/CT, 38 lesions were observed with localized CWT under 18F-FDG PET/CT scan, and 7 lesions were not. Localized CWT was observed on 18F-FDG PET/CT in 58.3% of low-risk lesions, 90.9% of high-risk adenomas and 100% of adenocarcinomas. There was a difference in the localized CWT between the low-risk lesion group and the high-risk lesion group (P=0.010). With localized CWT as the only judgement indicator, it was found that the sensitivity and specificity of the high-risk lesion group were 93.9% and 41.7%, respectively (Table 3). We found that when SUVmax ≥6.45 was combined with localized CWT to identify high-risk lesions, the sensitivity or specificity of high-risk lesions did not increase significantly. However, when SUVmax <6.45 was combined with CWT, the specificity of finding high-risk lesions could be improved, while the sensitivity showed little change (Table 4).
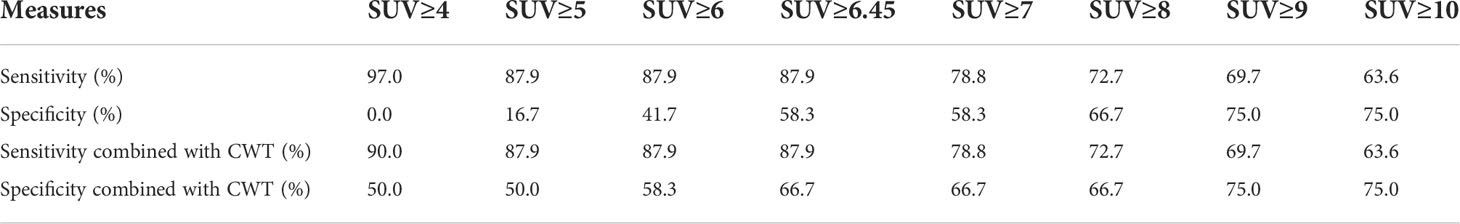
Table 4 Sensitivity and specificity of SUVmax and SUVmax combined with localized CWT in the identification of high-risk lesions from incidental focal colorectal 18F-FDG uptake foci.
Factors of missing high-risk adenomas by 18F-FDG PET/CT
In this study, 22 high-risk adenomas were incidentally found by 18F-FDG PET/CT. In addition, we searched and compared all patients who underwent 18F-FDG PET/CT and colonoscopy at the same time and found that 15 high-risk adenomas were missed by 18F-FDG PET/CT. We compared the characteristics of incidental high-risk adenomas and high-risk adenomas missed by 18F-FDG PET/CT. The volume of high-risk adenomas missed by 18F-FDG PET/CT was smaller than that of incidentally high-risk adenomas missed by 18F-FDG PET/CT (P=0.001), but there were no significant differences in lesion location, pathological type or intraepithelial neoplasia grade between the two groups (P>0.05) (Table 5).
Discussion
18F-FDG PET/CT has been widely used in radiation oncology. Incidental focal colorectal 18F-FDG uptake foci, although relatively rare, can alter the management and prognosis of some cancer patients (16). The incidence of incidental focal colorectal 18F-FDG uptake was 2.3% in our study, which was similar to previous studies (17, 18). Most studies have recommended further performance of colonoscopy in patients with incidental focal colorectal 18F-FDG uptake in 18F-FDG PET/CT examination, since a significant proportion of incidental lesions were confirmed to be cancerous or precancerous (17, 19). In our study, it was also confirmed by colonoscopy and pathology that 24.4% of incidental focal colorectal 18F-FDG uptake foci were adenocarcinoma and 48.9% were high-risk adenomas, but there were still a considerable proportion of normal or inflammatory lesions (24.4%) and low-risk adenomas (2.2%). Indiscriminate colonoscopy is not beneficial for cancer patients with limited survival or physical examination.
Advanced adenomas have a higher risk of developing into cancer than nonadvanced adenomas (20). A meta-analysis showed a significantly higher incidence of high-risk adenomas compared with patients without adenomas. In addition, colorectal cancer-related mortality was significantly higher in patients with high-risk adenomas than in patients with low-risk adenomas and those without adenomas (21). Therefore, advanced adenomas should also be treated promptly. We classified high-risk adenomas and adenocarcinoma into the high-risk lesion group and differentiated high-risk and low-risk lesions by relevant parameters of 18F-FDG PET/CT. Previous studies have suggested that optimal cut-off points for SUVmax can be used to distinguish malignant lesions or high-grade intraepithelial neoplasia (22) or that metabolic volume (MV) and SUVmax can be used to progressively distinguish malignant and atypical hyperplasia from benign colorectal 18F-FDG uptake lesions by 18F-FDG PET/CT (23). Some studies found that SUVmax could distinguish malignant lesions from other types of lesions but could not distinguish benign lesions from adenomas (24). Different from previous studies, our study evaluated the ability of 18F-FDG PET/CT to diagnose incidental high-risk lesions by using SUVmax and localized CWT parameters and found that SUVmax=6.45 was the optimal cut-off value, with a sensitivity of 87.9% and specificity of 58.3%. When lesion SUVmax <6.45 was combined with CWT parameters, the specificity of diagnosis of high-risk lesions was improved, and the sensitivity was not significantly decreased.
Localized CWT may be a predictor of colon cancer, which can be obtained directly from 18F-FDG PET/CT. In Bas et al.’s study, 132 patients were found to have CWT by CT and underwent colonoscopy. A total of 28.8% of the patients were found to have malignant tumours, and 22.7% were found to have colorectal polyps, indicating that CWT may indicate malignant tumours. However, a deficiency of this study is the lack of specific data on colonic wall thickening (25). Karacin et al. compensated for this limitation by retrospectively analysing 5300 colonoscopy reports, including 122 patients with CWT, and grading them according to the specific thickness of CWT. Multivariate analysis found that moderate to severe (≥12 mm), focal or asymmetric CWT was a risk factor for cancer (26). In this study, CWT was used as the evaluation parameter of benign and malignant lesions of incidental colorectal FDG uptake to improve the specificity of lesions with SUVmax <6.45. To our knowledge, this is the first time that a combination of SUVmax and localized CWT parameters has been used to evaluate lesions of incidental focal colorectal 18F-FDG uptake foci.
In addition, patients who underwent 18F-FDG PET/CT and colonoscopy during the same period were analysed, and 34 high-risk adenomas were missed. We compared the pathological characteristics of incidental and missed high-risk adenomas and found that there was a difference in size between the two groups (P=0.01). A total of 58.8% of high-risk adenomas with diameters ≥1 cm and 90.9% of high-risk adenomas with diameters ≥2 cm could be detected by 18F-FDG PET/CT, while there were no significant differences in lesion location, pathological type or grade of intraepithelial neoplasia between the two groups. The above data suggest that the lesion size may be a decisive factor affecting the detection of high-risk adenomas by 18F-FDG PET/CT. We believe that this may be due to the small size (small number of cells) of advanced adenomas and the relatively low degree of cell malignancy compared with malignant tumours, so it cannot be shown on 18F-FDG PET/CT. Our results are similar to those of earlier studies that indicated that size is the only variable affecting colorectal tumour detection (27, 28). However, in recent years, some studies have challenged this view. Through univariate and multivariate analysis, Ravizza et al. found that size >10 mm, villus content and a high degree of atypical hyperplasia were all factors affecting PET/CT detection of adenoma (29). In addition to pathological grade and lesion size, flat shape and lesions located near the colon were also correlated with low sensitivity of PET/CT for colorectal adenoma (30). In view of the relatively small number of patients in this study and retrospective study, further discussion and confirmation are still needed in the future.
On the whole, there are several novelties could be highlighted in this study: Firstly, we attempted to provide clinicians with some help in evaluating whether the foci of incidental focal colorectal uptake are high-risk lesions and whether colonoscopy need to be performed actively by these two parameters (SUVmax and localized CWT) of 18F-FDG PET/CT. Previous studies have used SUVmax of 18F-FDG PET/CT to distinguish benign lesions from malignant lesions (31, 32). However, there may be some limitations to the studies: In Luboldt et al.’s and Putora et al.’s study, they concluded that SUVmax ≥ cut-off value, patients should be considered for colonoscopy, when SUVmax < cut-off value, they still requires individual evaluation or can’t rule out malignant lesion (33, 34). CWT is a condition encountered on computed tomography, which may be associated with colonic malignancy, inflammation or other benign lesions (13, 25). Further research found that localized CWT may be more associated with malignancy (26, 35). The results of our study showed that when SUVmax < 6.45 (cut-off value), the combination of localized CWT parameters could improve the specificity of the diagnosis of high-risk lesions, and the sensitivity was not significantly reduced. To our knowledge, few studies have used these two parameters to identify incidental focal colorectal 18F-FDG uptake foci as high-risk lesions; Secondly, different from previous study (24), adenomas in this study were subdivided into high-risk adenomas and low-risk adenomas, and high-risk adenomas and adenocarcinoma were included in high-risk lesions, which was more consistent with the necessity of colonoscopy for cancer patients. Thirdly, these two parameters can be easily obtained in 18F-FDG PET/CT without obtaining other results such as serological tests of the patient (36). Finally, the influence factor of high-risk adenomas missed by 18F-FDG PET/CT is still controversial. Our results found that size may be the main factor affecting missed diagnosis, which may provide a perspective for this controversial point.
The limitations of this study are as follows: it was a single-centre retrospective study, and some 18F-FDG PET/CT parameters and clinical information were lacking or difficult to trace. Due to incomplete data, 18F-FDG PET/CT only recorded the localized CWT and failed to obtain complete specific values and explore them. Due to the defect of description, no comparative analysis was performed on the morphology of colorectal adenomas when comparing incidental and missed high-risk adenomas.
In conclusion, the combination of SUVmax and localized CWT parameters of 18F-FDG PET/CT can help improve the specificity of identifying high-risk lesions from incidental focal colorectal 18F-FDG uptake foci, especially for lesions with SUVmax < 6.45. For whether patients with incidental focal colorectal 18F-FDG uptake foci need colonoscopy, these two easily available parameters may help clinicians make a strategy. In addition, clinicians should pay attention to the fact that high-risk adenomas may be missed by 18F-FDG PET/CT due to small size.
Data availability statement
The datasets generated for this study are available on reasonable request to the corresponding author.
Ethics statement
The current study was approved by the Institutional Ethics Committee of the Affiliated Cancer Hospital & Institute of Guangzhou Medical University (No.ZN2022-21), and the need of signed informed consent was waived.
Author contributions
WX and HL participated in the design of the study and drafted the manuscript. ZG and WX collected the patients’ data and performed analysis. LiZ and RZ offered advice and revised the manuscript. LoZ conceived the study and supervised the project. All authors contributed to the article and approved the submitted version.
Funding
The publication fees of this study will be funded by Affiliated Cancer Hospital and Institute of Guangzhou Medical University
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hohenstein NA, Chan JW, Wu SY, Tahir P, Yom SS. Diagnosis, staging, radiation treatment response assessment, and outcome prognostication of head and neck cancers using PET imaging: A systematic review. PET Clin (2020) 15:65–75. doi: 10.1016/j.cpet.2019.08.010
2. Seol HY, Kim YS, Kim SJ. Predictive value of 18F-fluorodeoxyglucose positron emission tomography/computed tomography for PD-L1 expression in non-small cell lung cancer: A systematic review and meta-analysis. Thorac Cancer (2020) 11:3260–8. doi: 10.1111/1759-7714.13664
3. Kim CG, Hwang SH, Kim KH, Yoon HI, Shim HS, Lee JH, et al. Predicting treatment outcomes using (18)F-FDG PET biomarkers in patients with non-small-cell lung cancer receiving chemoimmunotherapy. Ther Adv Med Oncol (2022) 14:17486532. doi: 10.1177/17588359211068732
4. Liu Y, Ma J, Liu Y. (18)F-fluorodeoxyglucose positron emission tomography-computed tomography as a screening tool for second primary cancers in cancer patients. Oncotarget (2017) 8:92555–60. doi: 10.18632/oncotarget.21444
5. Şimşek FS, İspiroğlu M, Taşdemir B, Köroğlu R, Ünal K, Özercan IH, et al. What approach should we take for the incidental finding of increased 18F-FDG uptake foci in the colon on PET/CT? Nucl Med Commun (2015) 36:1195–201. doi: 10.1097/MNM.0000000000000388
6. Roh SH, Jung SA, Kim SE, Kim HI, Lee MJ, Tae CH, et al. The clinical meaning of benign colon uptake in (18)F-FDG PET: Comparison with colonoscopic findings. Clin Endosc (2012) 45:145–50. doi: 10.5946/ce.2012.45.2.145
7. Tatlidil R, Jadvar H, Bading JR, Conti PS. Incidental colonic fluorodeoxyglucose uptake: Correlation with colonoscopic and histopathologic findings. Radiology (2002) 224:783–7. doi: 10.1148/radiol.2243011214
8. Kousgaard SJ, Thorlacius-Ussing O. Incidental colorectal FDG uptake on PET/CT scan and lesions observed during subsequent colonoscopy: A systematic review. Tech Coloproctol (2017) 21:521–9. doi: 10.1007/s10151-017-1652-6
9. Zauber AG, Winawer SJ, O'Brien MJ, Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med (2012) 366:687–96. doi: 10.1056/NEJMoa1100370
10. Kim SY, Kim HS, Park HJ. Adverse events related to colonoscopy: Global trends and future challenges. World J Gastroenterol (2019) 25:190–204. doi: 10.3748/wjg.v25.i2.190
11. Bielawska B, Hookey LC, Sutradhar R, Whitehead M, Xu J, Paszat LF, et al. Anesthesia assistance in outpatient colonoscopy and risk of aspiration pneumonia, bowel perforation, and splenic injury. Gastroenterology (2018) 154:77–85. doi: 10.1053/j.gastro.2017.08.043
12. Latos W, Aebisher D, Latos M, Krupka-Olek M, Dynarowicz K, Chodurek E, et al. Colonoscopy: Preparation and potential complications. Diagnostics (Basel) (2022) 12(3):747. doi: 10.3390/diagnostics12030747
13. Moraitis D, Singh P, Jayadevan R, Cayten CG. Colonic wall thickening on computed tomography scan and clinical correlation. does it suggest the presence of an underlying neoplasia? Am Surg (2006) 72:269–71.
14. Fang JY, Zheng S, Jiang B, Lai MD, Fang DC, Han Y, et al. Consensus on the prevention, screening, early diagnosis and treatment of colorectal tumors in China: Chinese society of gastroenterology, October 14-15, 2011, shanghai, China. Gastrointest Tumors (2014) 1:53–75. doi: 10.1159/000362585
15. Digestive Endoscopy Special Committee of Endoscopic Physicians Branch of Chinese Medical Association and Cancer The Endoscopy Committee of China Anti-Cancer Association. Zhonghua Nei Ke Za Zhi (2019) 58:485–95. doi: 10.3760/cma.j.issn.0578-1426.2019.07.002
16. Young CJ, Zahid A, Choy I, Thompson JF, Saw R. Incidental detection of colorectal lesions by FDG PET/CT scans in melanoma patients. Eur J Surg Oncol (2017) 43:2163–9. doi: 10.1016/j.ejso.2017.09.012
17. Kousgaard SJ, Gade M, Petersen LJ, Thorlacius-Ussing O. Incidental detection of colorectal lesions on (18) f-FDG-PET/CT is associated with high proportion of malignancy: A study in 549 patients. Endosc Int Open (2020) 8:E1725–31. doi: 10.1055/a-1266-3308
18. Treglia G, Bertagna F, Sadeghi R, Muoio B, Giovanella L. Prevalence and risk of malignancy of focal incidental uptake detected by fluorine-18-fluorodeoxyglucose positron emission tomography in the parotid gland: A meta-analysis. Eur Arch Otorhinolaryngol (2015) 272:3617–26. doi: 10.1007/s00405-014-3308-8
19. Albertsen LN, Jaensch C, Tornbjerg SM, Teil J, Madsen AH. Correlation between incidental focal colorectal FDG uptake on PET/CT and colonoscopic and histopathological results. Scand J Gastroenterol (2022) 57:246–52. doi: 10.1080/00365521.2021.1998602
20. Click B, Pinsky PF, Hickey T, Doroudi M, Schoen RE. Association of colonoscopy adenoma findings with long-term colorectal cancer incidence. JAMA (2018) 319:2021–31. doi: 10.1001/jama.2018.5809
21. Duvvuri A, Chandrasekar VT, Srinivasan S, Narimiti A, Dasari C, Nutalapati V, et al. Risk of colorectal cancer and cancer related mortality after detection of low-risk or high-risk adenomas, compared with no adenoma, at index colonoscopy: A systematic review and meta-analysis. Gastroenterology (2021) 160:1986–96. doi: 10.1053/j.gastro.2021.01.214
22. Na SY, Kim KJ, Han S, Jin S, Kim JS, Yang DH, et al. Who should undergo a colonoscopy among patients with incidental colon uptake on PET-CT? Scand J Gastroenterol (2015) 50:1045–53. doi: 10.3109/00365521.2014.992363
23. Oh JR, Min JJ, Song HC, Chong A, Kim GE, Choi C, et al. A stepwise approach using metabolic volume and SUVmax to differentiate malignancy and dysplasia from benign colonic uptakes on 18F-FDG PET/CT. Clin Nucl Med (2012) 37:e134–40. doi: 10.1097/RLU.0b013e318239245d
24. van Hoeij FB, Keijsers RG, Loffeld BC, Dun G, Stadhouders PH, Weusten BL. Incidental colonic focal FDG uptake on PET/CT: Can the maximum standardized uptake value (SUVmax) guide us in the timing of colonoscopy? Eur J Nucl Med Mol Imaging (2015) 42:66–71. doi: 10.1007/s00259-014-2887-3
25. Bas BO, Pakoz ZB. Endoscopic evaluation of patients with colonic wall thickening detected ON computed tomography. Acta Clin Croat (2020) 59:463–8. doi: 10.20471/acc.2020.59.03.10
26. Karacin C, Türker S, Eren T, Imamoglu GI, Yılmaz K, Coskun Y, et al. Predictors of neoplasia in colonic wall thickening detected via computerized tomography. Cureus (2020) 12:e10553. doi: 10.7759/cureus.10553
27. Friedland S, Soetikno R, Carlisle M, Taur A, Kaltenbach T, Segall G. 18-fluorodeoxyglucose positron emission tomography has limited sensitivity for colonic adenoma and early stage colon cancer. Gastrointest Endosc (2005) 61:395–400. doi: 10.1016/s0016-5107(04)02775-0
28. van Kouwen MC, Nagengast FM, Jansen JB, Oyen WJ, Drenth JP. 2-(18F)-fluoro-2-deoxy-D-glucose positron emission tomography detects clinical relevant adenomas of the colon: A prospective study. J Clin Oncol (2005) 23:3713–7. doi: 10.1200/JCO.2005.02.401
29. Ravizza D, Bartolomei M, Santoro L, Tamayo D, Fiori G, Trovato C, et al. Positron emission tomography for the detection of colorectal adenomas. Dig Liver Dis (2010) 42:185–90. doi: 10.1016/j.dld.2009.06.018
30. Sekiguchi M, Kakugawa Y, Terauchi T, Matsumoto M, Saito H, Muramatsu Y, et al. Sensitivity of 2-[(18)F]fluoro-2-deoxyglucose positron emission tomography for advanced colorectal neoplasms: A large-scale analysis of 7505 asymptomatic screening individuals. J Gastroenterol (2016) 51:1122–32. doi: 10.1007/s00535-016-1201-5
31. Garrido DC, Payeras CM, García CC, Giménez GM, Daumal DJ. Clinical-endoscopic relevance of incidental colorectal lesions detected by PET-CT. Rev Esp Enferm Dig (2018) 110:434–9. doi: 10.17235/reed.2018.4719/2016
32. Fuertes J, Montagut C, Bullich S, Coma MI, Mestre-Fusco A, Suárez-Piñera M, et al. Incidental focal uptake in colorectal location on oncologic 1 8FDG PET and PET/CT studies: Histopathological findings and clinical significances. Rev Esp Med Nucl Imagen Mol (2015) 34:95–101. doi: 10.1016/j.remn.2014.07.008
33. Luboldt W, Wiedemann B, Fischer S, Bodelle B, Luboldt HJ, Grünwald F, et al. Focal colorectal uptake in (18)FDG-PET/CT: Maximum standard uptake value as a trigger in a semi-automated screening setting. Eur J Med Res (2016) 21:2. doi: 10.1186/s40001-016-0195-z
34. Putora PM, Müller J, Borovicka J, Plasswilm L, Schmidt F. Relevance of incidental colorectal FDG-PET/CT-enhanced lesions. Onkologie (2013) 36:200–4. doi: 10.1159/000350302
35. Pothoulakis I, Wikholm C, Verma V, Ahmad AI, Vangimalla SS, Patel H, et al. Predictors of colorectal carcinoma and inflammatory bowel disease in patients with colonic wall thickening. JGH Open (2022) 6:159–65. doi: 10.1002/jgh3.12708
Keywords: PET/CT, incidental focal colorectal 18F-FDG uptake, SUVmax, CWT, high-risk lesions
Citation: Xu W, Li H, Guo Z, Zhang L, Zhang R and Zhang L (2022) Combined SUVmax and localized colonic wall thickening parameters to identify high-risk lesions from incidental focal colorectal 18F-FDG uptake foci. Front. Oncol. 12:972096. doi: 10.3389/fonc.2022.972096
Received: 17 June 2022; Accepted: 25 July 2022;
Published: 12 August 2022.
Edited by:
Domenico Albano, University of Brescia, ItalyReviewed by:
Francesco Dondi, Università degli Studi di Brescia, ItalySalvatore Annunziata, Fondazione Policlinico Universitario A. Gemelli IRCCS, Italy
Copyright © 2022 Xu, Li, Guo, Zhang, Zhang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Long Zhang, 2012690541@gzhmu.edu.cn
†These authors have contributed equally to this work
 Wenmin Xu
Wenmin Xu Hansen Li
Hansen Li Ziqian Guo
Ziqian Guo Linqi Zhang
Linqi Zhang Rusen Zhang
Rusen Zhang Long Zhang
Long Zhang