- 1College of Nursing, University of Utah, Salt Lake City, UT, United States
- 2Department of Health Outcomes and Behavior, Moffitt Cancer Center, Tampa, FL, United States
- 3Department of Epidemiology, Human Genetics and Environmental Sciences, School of Public Health, University of Texas Health Science Center at Houston, El Paso, TX, United States
- 4Larner College of Medicine, University of Vermont, Burlington, VT, United States
Purpose: The purpose of this study was to describe the social support networks and daily support interactions of cancer-affected individuals, including young adult (YA) and LGBTQIA+ survivors and care partners.
Methods: Participants were recruited at two United States cancer centers and via social media for a pilot study testing a novel online method for collecting prospective, daily social support interaction data (N=28). All participants were aged 18+; survivors had a current or recent cancer diagnosis and were engaged in treatment and/or services; care partners were identified by the survivors. Enrollment also purposefully targeted YA and LGBTQIA+ survivors. Social network data (up to 10 members) were assessed at baseline. Daily online surveys assessed support interactions between participants and specific network members over 14 days. Descriptive statistics summarized data and explored between-group (YA/non-YA, LGBTQIA+/non-LGBTQIA+) differences in social network characteristics (size, heterogeneity, density, centralization, cohesion) and support interactions (support source and type).
Results: There were no significant differences between YA and non-YA participants on any measures. LGBTQIA+ participants’ support networks were less dense (Mdn=0.69 vs. 0.82, p=.02), less cohesive (Mdn=0.85 vs. 0.91,.02), more centered on the participant (Mdn=0.40 vs. 0.24, p=.047), and included more LGBTQIA+ members (Mdn=0.35 vs. 0.00, p<.001). LGBTQIA+ participants reported having more interactions with LGBTQIA+ network members (Mdn=14.0 vs. Mdn=0.00, p<.001) and received significantly more of all types of support from LGBTQIA+ vs. non-LGBTQIA+ members. LGBTQIA+ participants also reported receiving more appraisal support than non-LGBTQIA+ (Mdn 21.64 vs. 9.12, p=.008) including more appraisal support from relatives (Mdn=11.73 vs 6.0, p+.037).
Conclusions: Important information related to support access, engagement, and needs is embedded within the everyday contexts of the social networks of cancer-affected people. Individualized, accessible, and prospective assessment could help illuminate how their “real world” support systems are working and identify specific strengths and unmet needs. These insights would inform the development of more culturally competent and tailored interventions to help people understand and leverage their unique support systems. This is particularly critical for groups like YA and LGBTQIA+ survivors and care partners that are underserved by formal support services and underrepresented in cancer, caregiving, and social support research.
Introduction
Social support, a social determinant of health that influences a range of outcomes (1), is a critical resource for people affected by cancer, including both cancer survivors and their care partners (2–4). Research has sought to explain how social support influences individuals’ cognitive and emotional appraisal of stress and, thereby, their psychosocial and physical health outcomes (5–7). Disparities in social support among diverse groups are also being more closely examined to determine how lack of access to culturally competent, relevant, and inclusive formal services and resources contributes to inequitable cancer outcomes (8–10).
Young adult (YA, aged 18-39) (11–13) and LGBTQIA+ (14–16) individuals are members of two underserved, yet growing subgroups within the cancer-affected population (17), and these groups will increasingly intersect as adolescents and YAs identify as LGBTQIA+ at higher rates than previous generations (18, 19). Younger demographics in the US also continue to grow more racially and ethnically diverse (20). Racial and ethnic minority cancer survivors in both YA and LGBTQIA+ groups experience even greater disparities in all-cause mortality, health outcomes, mental health, and quality of life (21–23).
Both YA and LGBTQIA+ groups also share characteristics that impact access to and engagement with formal support services such as lower income and financial stress, inadequacy of insurance, less traditional family and kinship systems, and lack of access to culturally competent care, increasing risk for unmet support needs. YA and LGBTQIA+ survivors have also reported feeling excluded from typical formal support services that have been largely developed with older, heterosexual, and cisgender patients living within traditional spousal relationships centered in nuclear, biological family structures; these services are not seen as relevant to their relationships and experiences (24, 25). YA and LGBTQIA+ survivors and care partners may therefore be even more reliant on informal sources of support, which may or may not be adequate to meet their needs, but this possibility has not been widely explored within either group.
Cancer-affected individuals, particularly those in underserved groups, rely on their informal social systems for support (4, 26). In the everyday lives of survivors and care partners, social support is accessed and activated within the real-time contexts of their actual personal networks through relationships and interactions that vary daily and over weeks, months and years (27). Social support networks are unique to each individual, and often include a mix of people who provide varying types of informal and formal support at different times (24). And while for many, support networks center on biological and legal relationships within nuclear family structures, this is changing as more YAs forgo marriage and traditional family structures and adopt more flexible kinship systems (28). The concept of chosen family, defined as kinship bonds formed outside of bio-legal family structures, has long been an important facet of LGBTQIA+ community (29).
Relatively little research, however, has examined the social support networks of YA and LGBTQIA+ cancer-affected individuals (30, 31). YAs rely on a mix of family, friends, and cancer peers for social support, and receive differing types of support from these sources depending on their changing needs over time and situation (32). LGBTQIA+ cancer survivors also receive support from diverse members of their networks and chosen family, which often includes friends and other LGBTQIA+ people, and they may be more likely to identify a close friend as a primary care partner (33, 34). Diverse social networks are associated with better aging and health outcomes and help buffer the stress of homophobia and transphobia (35), yet the social networks of older LGB adults may be less diverse and more tenuous than non-LGB peers (36, 37). The very few studies addressing the social support networks of transgender and gender diverse people also highlight the protective effects of adequate social support networks for buffering effects of discrimination and stress and improving health outcomes (38, 39)
The purpose of our study was to pilot an individualized, prospective, observational approach to assess characteristics of the personal social support networks and patterns within daily support interactions of a sample of cancer survivors and care partners focusing on YA and LGBTQIA+ individuals. To do so, we developed a novel online method combining social network assessment (structural factors) and prospective daily interaction diaries (functional factors) and we report on the development, feasibility, and acceptability of these methods elsewhere (40). Here we present the results of our descriptive analysis of participants’ personal social support networks and interactions with network members which included exploratory between-group comparisons (YA/non-YA and LGBTQIA+-non-LGBTQIA+.).
Methods
Study Design
We employed a prospective cohort design. All study activities were reviewed and approved by institutional review boards for the protection of human subjects at both study sites. This study was determined to be exempt by the University of Utah IRB (#00119352) and the Advarra IRB (Moffitt Cancer Center; Review #MCC20021).
Setting and Recruitment
A purposive, non-random sample of participants meeting study eligibility criteria were recruited from populations served by two comprehensive cancer centers in the Intermountain West and the Southeast regions of the United States and nationally via community partners’ social media channels. Rolling recruitment occurred between August 2019 and May 2020. As our primary aim was to pilot test the feasibility of our methods within hard-to-reach populations (i.e. YA, LGBTQIA, care partners) and provide proof of concept for prospective assessment of complex social network and support data, the small sample size and use of purposive sampling methods were acceptable strategies (41).
Participants
All eligible participants were 18 and older, able to speak and read English, and were either a cancer survivor (broadly defined according to the NCI definition of a person who is on a trajectory from cancer diagnosis to end of life) (42) or a care partner of a cancer survivor (a person who most often helps the survivor and is not paid to do so). Eligible survivors had at least one current or historical cancer diagnosis, were currently engaged in treatment, services, monitoring, or follow-up related to this diagnosis, and were able to identify a primary, informal care partner or support person who also consented to participate in the study. Additionally, they had to be either YA or self-identify as LGBTQIA+ or both. Eligibility criteria for care partners included a person who the survivor considers a main source of routine support who also consented to participate. We had originally intended to enroll eight YA survivor/care partner dyads and eight LGBTQIA+ survivor/care partner dyads for a target enrollment of N=32. This was complicated by the onset of the COVID-19 pandemic in the US, however, and we stopped enrollment before fully accruing as planned. Each participant was screened by research staff for inclusion criteria, participated in the informed consent process, and was compensated $100 on study completion.
Measures
At baseline, participants completed a demographic survey in REDCap (43) and an interview-based assessment in which ecomaps were constructed to assess characteristics of their personal (egocentric) social support networks. Interview responses and ecomaps were recorded and transferred by research staff into REDCap. Participants’ network member data were then used to personalize a daily electronic survey that was texted or emailed to participants for 14 consecutive days. These prospective daily surveys assessed characteristics of participants’ daily interactions with network members, described below. While participants included survivor and care partner dyads, individual participant data were not shared by study team members.
Demographics
Demographic data included cancer-related role (survivor or care partner), age, racial identity, Hispanic/Latinx ethnicity, sexual orientation, gender, cis- or transgender status, relationship status, highest level of education, and income.
Social Network Measures
Each participant completed an individual baseline interview with a researcher in which an eco- mapping technique was used to elicit egocentric social network information. Participants were asked to identify up to 10 people in their social network they considered to be important sources of support related to their cancer experience (e.g. spouses/partners, relatives, friends, neighbors, co-workers, spiritual advisors, case managers, therapists). For each person, participants provided the following data: First name or initials, age, gender, whether the member was LGBTQIA+, the participants’ primary relationship to the network member, length of time known, closeness of the relationship between the participant and each network member, and whether/how specific network members were connected with other network members.
Daily Interaction Surveys
Based on participant preference, first names or initials of network members were then incorporated into brief daily REDCap surveys assessing characteristics of participants’ interactions with the identified members (alters) of their support network. Each day for 14 days, participants received a link via text or email to an online survey presenting a list of their network members and were asked to select which members they had interacted with during the last 24 hours. For each network member selected, participants were then asked to focus on one interaction with that member during the past 24 hours and provide the following information about that focal interaction: the purpose of the interaction (free text response), whether the interaction was perceived as supportive (yes, no, not meant to be supportive), the type of support the interaction represented for the participant (instrumental, informational, emotional, appraisal, based on definitions and examples provided for participants), and perception of helpfulness of the interaction (5-point Likert rating, 0 = not at all helpful, 5 = very much helpful). Only interactions perceived as supportive (yes vs. no/not mean to be) and rated as at least somewhat helpful (≥ 2 Likert rating) were included in analysis.
Analysis
Study data from both sites were merged, and all study data were reviewed and checked for consistency and errors. Missing data analysis was conducted to assess the pattern of missingness for the baseline psychosocial measures; multiple imputation was used to impute missing data after missing completely at random was confirmed. Descriptive statistics were used to summarize baseline and daily interaction data using both SPSS (version 27) and R software. UCINET (44) software was used to calculate social network variables for density (the extent to which most or all participants’ network members know each other), degree centralization (the extent to which connections within one’s network are numerically dominated by one or few individuals, including the participant), and cohesion (the extent to which the network is more connected vs. disconnected, somewhat irrespective of density). Three network heterogeneity measures were also calculated: diversity of age of network members, the ratio of relatives to non-relatives, and the ratio of LGBTQIA+ to non-LGBTQIA+ members. Because of the small sample size and the nonnormality of psychosocial, network, and daily interaction data, Mann-Whitney U tests were used to compare between-group differences (i.e., YA vs. non-YA, LGBTQIA+, vs. non-LGBTQIA+). A significance level of p = 0.05 was set for all tests, and we report exact p values where possible.
Results
Participant Demographics
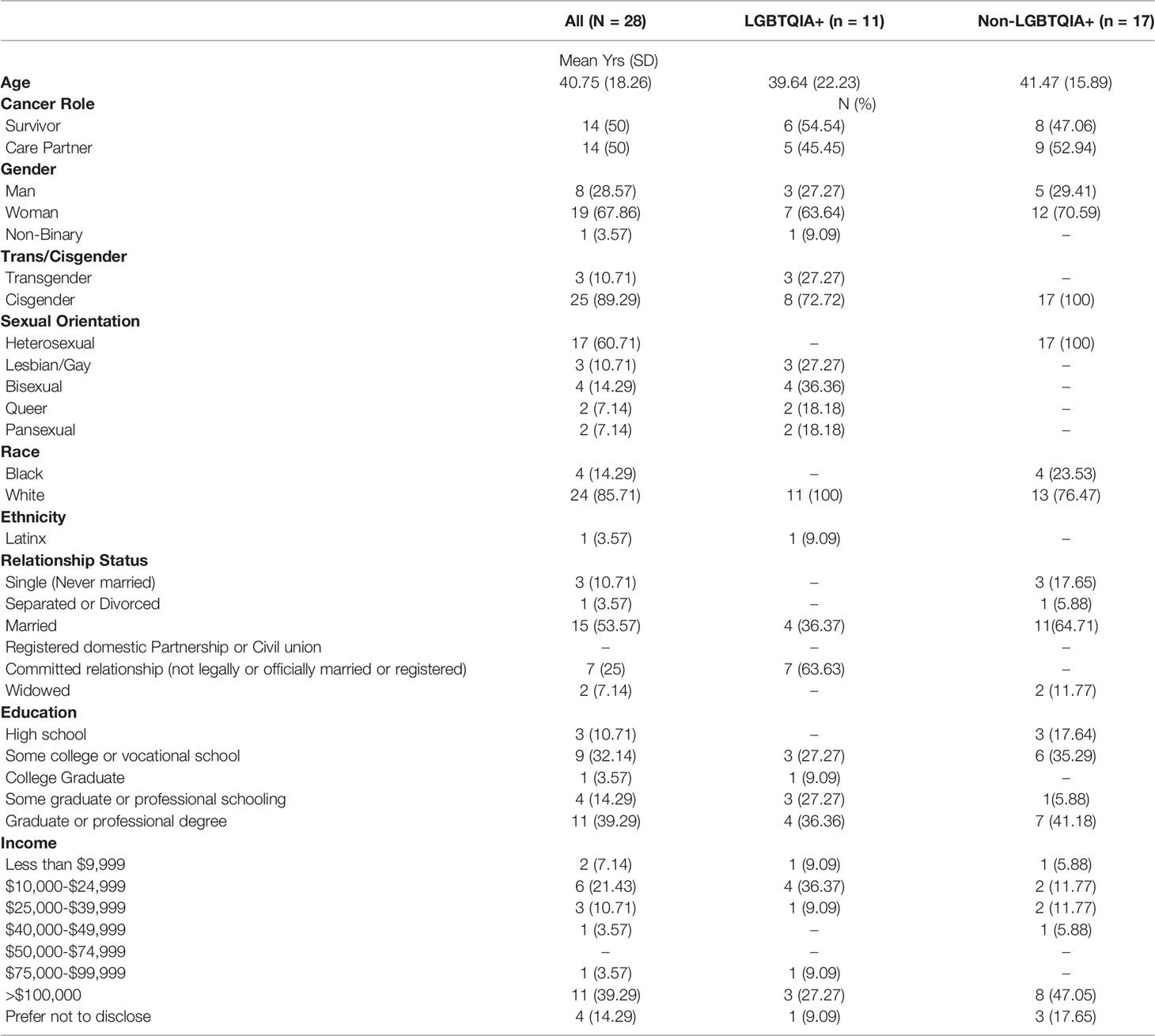
Table 1 presents participant demographics. Most participants were White (n=24, 86%), not Hispanic/Latinx (n=23, 96%), female (n=19, 67.9%), and cisgender (n=25, 89%). Seventeen participants were heterosexual (61%), and 11 were either lesbian, gay, bisexual, queer, or pansexual (39.3%). There were no significant between-group differences for demographics aside from non-heterosexual and transgender and nonbinary categories.
Social Network Characteristics
Participants’ support networks had a mean of six members (SD = 2.22, range 2-10) and represented a mix of relatives (e.g. sibling, in-law; M = 3.6, SD = 1.4, range 1-7) and non-relatives (e.g. friend, co-worker; M = 2.8, SD = 2.3, range 1-7). Between-group comparisons showed no significant differences in network size/number of network members.
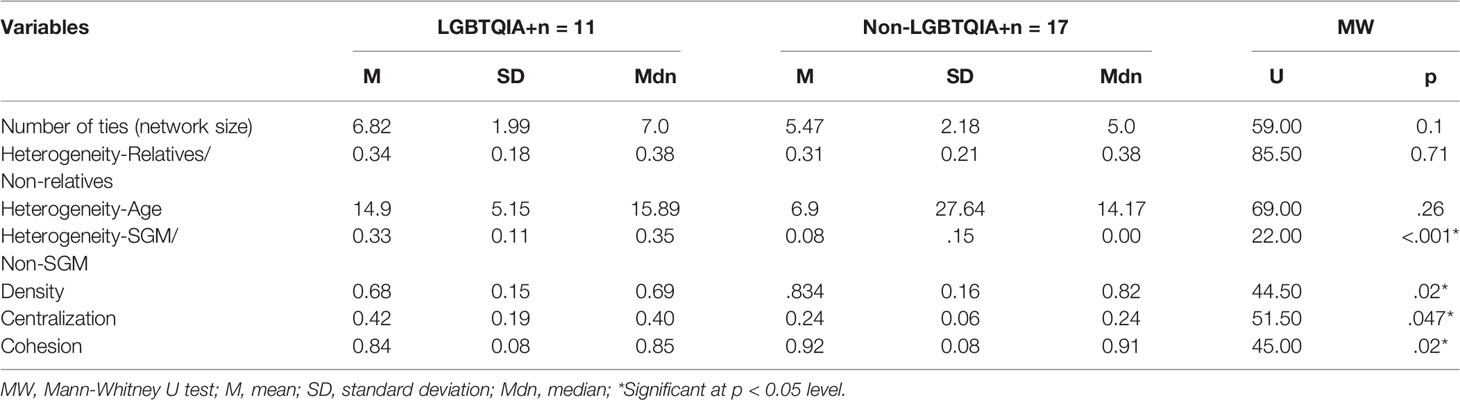
There were no significant differences between YA and non-YA support networks composition or structure. Table 2 presents a comparison of LGBTQIA+ and non-LGBTQIA+ social network characteristics. The support networks of LGBTQIA+ participants were significantly less dense (Mdn = 0.69 vs. 0.82, p = .02), less cohesive (Mdn = 0.85 vs. 0.91, p = .02) and more degree centralized (Mdn = 0.4 vs. 0.24, p = .047) than those of non-LGBTQIA+ participants. They also were significantly more heterogeneous in terms of having more LGBTQIA+ members than the networks of non-LGBTQIA+ participants (Mdn = 0.35 vs. 0.00, p <.001). While not significantly different, the support networks of LGBTQIA+ participants also tended to be more heterogenous for member age (Mdn = 15.89 vs. 14.7).
Daily Interactions and Perceived Support
We examined the total number of reported support interactions overall and with unique network members for each participant, focusing on relationship type (relatives vs. non-relatives), LGBTQIA+ status (LGBTQIA+ vs. non-LGBTQIA+ network members), and on the number of support interactions for each type of perceived support (emotional, informational, appraisal, instrumental).
Participants reported a mean of 41.79 support interactions overall during the two-week period (Mdn=39, SD=26.3, range=8-108) and a mean of 27.8 interactions with different network members (M= 27.75, Mdn=25.5, SD=15.6, range=4 - 58). There were no significant differences between YAs and non-YAs for number of interactions of any specific support type (instrumental, informational, emotional, appraisal, other) overall, or when examining support type by source (relative or non-relative.)
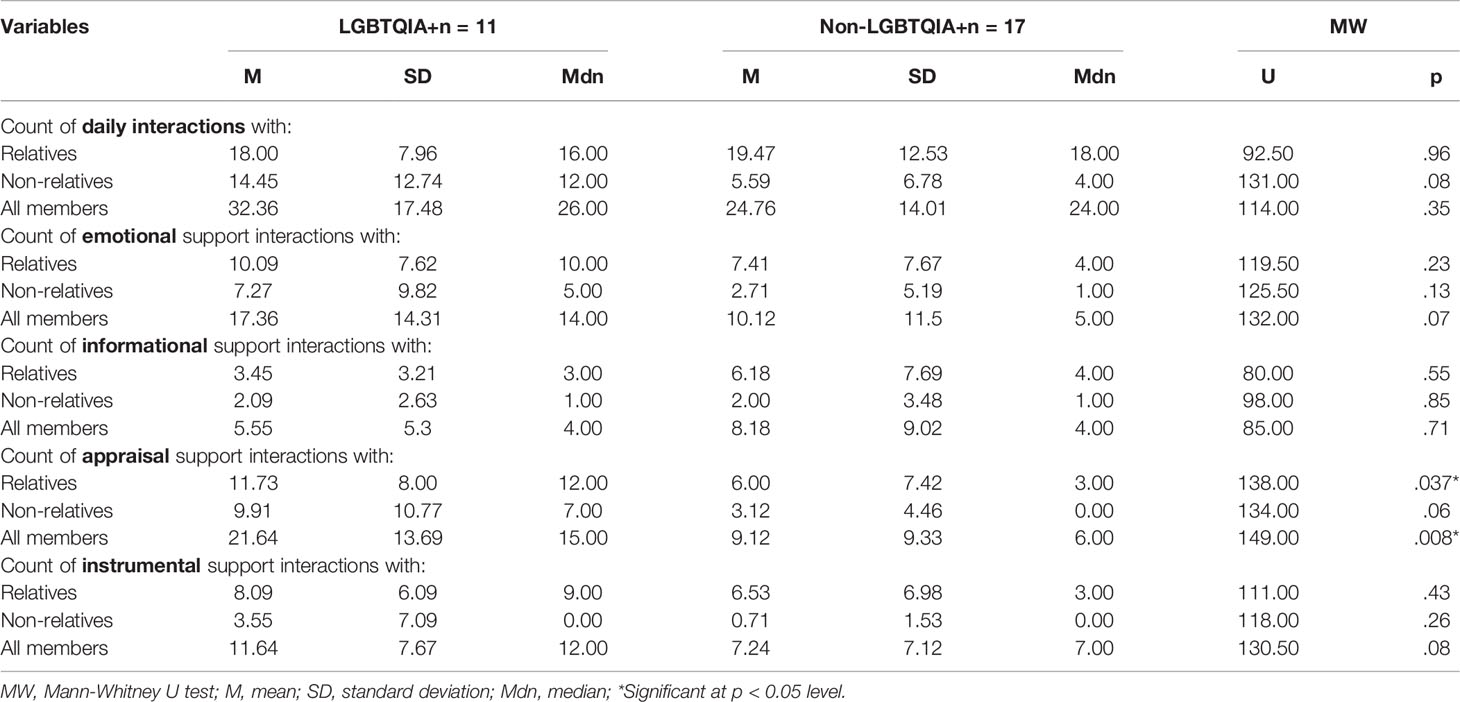
While not statistically significant, LGBTQIA+ participants reported more daily interactions with non-relatives than with relatives overall (Table 3, p = .08). LGBTQIA+ participants reported more appraisal support interactions with all members in their network (relatives and non-relatives) compared to non-LGBTQIA+ participants (p = .008), including more appraisal support interactions with relatives (p = .037).
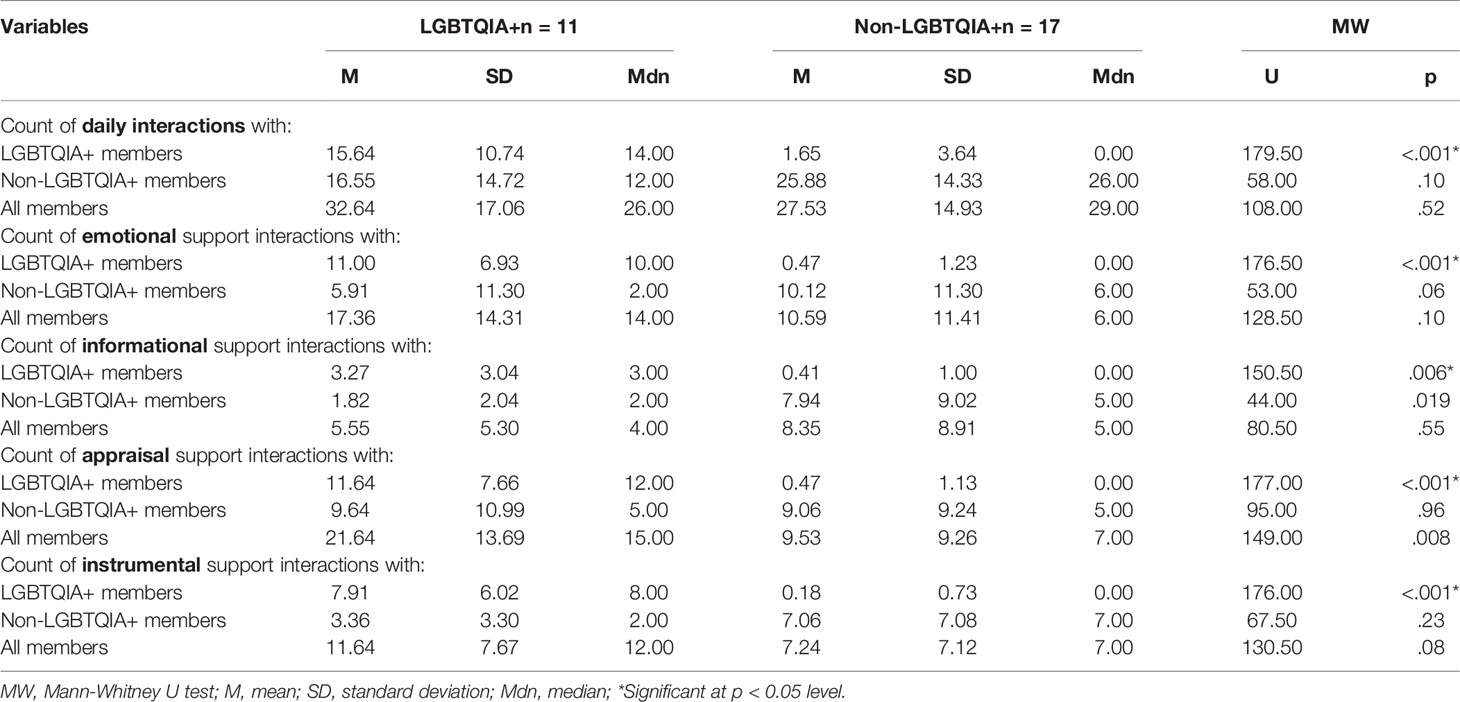
LGBTQIA+ participants reported more interactions with LGBTQIA+ members than with non-LGBTQIA+ members (Table 4, p <.001), and more emotional support (p <.001), appraisal support (p <.001), and instrumental support from LGBTQIA+ vs. non-LGBTQIA+ members (p <.001). LGBTQIA+ participants also reported more informational interactions with both LGBTQIA+ (p = .006) and non-LGBTQIA+ (p = .019) alters, and more appraisal support from all members (p = .008), than did non-LGBTQIA+ participants.
Discussion
For an increasingly diverse population of cancer-affected people, there remain challenges to assessment and inclusion in survivorship, social support, and social network research that may limit the impact of this knowledge and its implementation in real-world contexts (45). Despite how many cancer survivors rely on informal support systems, little social support research accounts for the unique social context of the individual—this is a critical gap in achieving equity for groups whose support systems may look or work differently from the norms that currently inform assessment and intervention. Many of the influential findings related to social support in cancer and caregiving populations draw from research conducted with mostly white, heterosexual, cisgender, middle-aged, and older adults (8, 46). And while dyadic social support and cancer research expands beyond the individual perspective, it still largely ignores the possibility that other kinds of social relationships may be just as critical to supporting survivors and care partners as traditional spousal and kin relationships (47). Existing research also ignores the reality that for many groups, social support and caregiving are not centered in spouse/partner or biological parent/child dyads, but distributed across social networks comprising an array of members who may be more or less demographically and developmentally diverse (48). This pilot study uses novel methodology to address gaps in previous research and assess structural and functional aspects of personal social support networks of underserved YA and LGBTQIA+ cancer patients.
Though our analyses revealed no significant differences between social network characteristics of YA and non-YA participants, contrary to expectation (49), we did note significant differences in network characteristics based on LGBTQIA+ status (50, 51). LGBTQIA+ participants’ networks were less dense and less cohesive, suggesting that LGBTQIA+ participants’ connections to social support may be more diffused across network members. The higher degree centralization of LGBTQIA+ participants in their social networks (i.e., members are generally connected to the participant but less with each other) suggests that these individuals were playing a more central role in holding their own networks together. LGBTQIA+ participants’ networks were also more diverse in that they included more LGBTQIA+ members, plus LGBTQIA+ participants also had more support-related interactions overall, including more with non-relatives.
These network characteristics may be strengths, offering participants a wide reach of network members with frequent contact (52, 53). Diffuse and heterogeneous networks have been shown to have benefits, including brokering diverse information and access to an array of resources (54). Further, higher levels of perceived support may mitigate negative health effects related to less cohesive and more diffuse networks (55, 56). However, a combination of higher heterogeneity and degree centralization with less density and cohesion may also be associated with a diffusion of social support and overall weaker connections among network relationships, which may also put LGBTQIA+ participants in a more precarious position in more volatile and high need situations, such as when participants are ill or burdened. For example, if a support network is dependent on a cancer survivor or care partner as a stabilizing node of connection, with few strong, well-resourced ties, their inability to fulfill the connecting role due to illness, lack of resources to mobilize the network, or competing demands can lead to a lack of coordinated support. This network profile may create problems for accessing or leveraging social support resources and could lead to unmet support needs. This premise should also be tested in a larger study over a longer period of time.
Emotional and appraisal support appeared to be an important type of support for LGBTQIA+ participants, as they reported more of these interactions with all network members compared with non-LGBTQIA+ participants. Appraisal support provides individuals with a sense of context that supports self-evaluation, reflection on one’s situation and standing, and a sense of connection to others who know and understand you well enough to afford this perspective (57). For individuals who are also LQBTQIA+ who experience minority stress–a combination of proximal and distal stressors related to minority status that span intrapersonal, interpersonal, and structural factors, the role of appraisal-oriented support may be particularly relevant to perceptions of support and mental health outcomes (58). LGBTQIA+ individuals, including younger people, are likely to have more experience with minority stress than are their non-minority counterparts and may have more practice and facility with accessing appraisal and emotional support within their networks, which may be protective. The flip side of this dynamic, however, is the compounded risk associated with LGBTQIA+ cancer survivors and care partners not having stable connections to people who provide this support within their personal networks and/or not knowing how to ask for and generate this support among members.
Implications for Intervention
Future work should examine how formal sources of support (e.g. oncologists, therapists, counselors) are integrated within survivors’ and care partners’ existing social networks (or not), including interactions between timing and types of support, service use, and wellbeing. The social support systems of cancer-affected people are inherently unique and—for YAs and people in minoritized populations like LGBTQIA+–may not be well-reflected in the expectations and operations of established formal services. For example, routine clinical care may hold implicit expectations of a hetero-normative network more traditionally seen in research on older adults, in which a spouse or adult child is available to provide outpatient care to patients. Those whose networks do not conform to this standard may not only experience feelings of alienation, but may be missing critical support for their care.
Developing a working understanding of more diverse social support landscapes is therefore important for clinicians as well as researchers. Clinicians can be mindful of expectations for support required for patients and caregivers to participate effectively in treatment and facilitate connections to inclusive formal resources when additional support is needed. Across healthcare systems, more tailored, less generic patient-centered clinical and support services would be particularly impactful for groups like YA and LGBTQIA+ who report feeling alienated by normative care models that do not acknowledge their individual contexts and experiences.
Researchers should focus on developing personalized interventions that boost cancer survivors’ and cancer care partners’ self-efficacy in accessing and leveraging social support to meet everyday challenges. This is especially critical for underserved populations, including people who are YA and LGBTQIA+ cancer survivors or care partners, who may be even more reliant on their personal social networks who feel disconnected from typical, formal support resources, and whose support systems may look different than those represented in the cancer literature. Finding ways to better coordinate holistic, high-quality cancer care is a national priority (59). Conducting more inclusive survivorship research will be important to ensure health care policy remedies, rather than reinforces, health care disparities.
Limitations
There were a number of limitations to this study. The descriptive and exploratory nature of our analyses limits the generalizability of our findings. A small sample size and purposive, non-probability sampling may have increased the risk of selection bias. There was a wide age range within the LGBTQIA+ group which may be contributing to the differences we found, although we verified that groups did not significantly differ by age. While grouping individuals of diverse sexual orientations and gender identities together in a single LGBTQIA+ group is often necessary due to small numbers of participants in these groups, it confounds important between-group differences that are relevant to understanding cancer- and minority-stress related support needs; this is compounded by the lack of representation of transgender and gender diverse participants in most studies, including this one. Finally, our data collection period spanned August 2019-May 2020 and the onset of the COVID-19 pandemic in the US slowed our study enrollment considerably, leading us to close recruitment before enrolling an equal number of LGBTQIA+ and non-LGBTQIA+ participants.
Conclusion
Every cancer-affected individual’s social support system is unique. Both structural and functional aspects of social support networks–network characteristics and patterns of interactions within these networks—are likely to influence survivors’ perceptions of support, appraisal of stress, capacity to cope, and ultimately their well-being. These influences may differ from person to person and by groups affected by differing social determinants of health (60). Relationship types and quality, the closeness of member connections, modality of interactions, patterns of interaction over time, and survivors’ changing preferences, needs, and perceptions of helpfulness are also likely to shape how social support affects survivors’ appraisal and coping (61). Examining these complexities for diverse groups of cancer survivors and their care partners should, therefore, be a priority for developing and implementing culturally-relevant interventions.
We sought to examine the personal social support networks of cancer survivors and their care partners in two groups—YA and LGBTQIA+ cancer survivors—that have been under-represented in survivorship, caregiving, and social support research and who subsequently report unmet support needs. We further sought to contextualize this by studying the survivor-care partner dyads in relation to their personal support networks. This study provides proof of concept for this strategy, and suggests that there may be important aspects of YA and LGBTQIA+ survivor cohorts in the structure and function of their personal support networks. Next steps include adapting all data collection methods for online access, repeating the protocol with a larger sample over a longer period of time, and modeling how social network characteristics and daily interaction patterns predict changes in perceived stress, support, and mental health outcomes.
Data Availability Statement
A limited de-identified data set is available on request. Requests to access the datasets should be directed to kristin.cloyes@nurs.utah.edu.
Ethics Statement
The studies involving human participants were reviewed and approved by University of Utah IRB, and the Advarra IRB Moffitt Cancer Center. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
KGC and MR conceptualized this study and acquired project funding. KGC developed the methodology for data collection. KET, REM, and KJM coordinated project administration. J-WG developed the plan for formal analysis. KGC, J-WG, EJC, SCC, and SEW performed data analysis. KGC wrote the original draft. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by a Dick and Timmy Burton Foundation Pilot Grant Award, University of Utah College of Nursing, Moffitt Cancer Center Adolescent and Young Adult Program with support from Swim Across America and the Bay Area Advisors, K01NR016948 (J-WG’s effort), T32NR013456 (KJM’s effort), NINR F31NR018987 (SEW’s effort). The REDCap application reported in this publication was supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR001067 for period 5/1/13–3/30/18 and UL1TR002538 for period 4/1/18-2/28/23.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors wish to thank the participants for their time and invaluable feedback.
References
1. Office of Disease Prevention and Health Promotion. (n.d.) Healthy People 2030. U.S. Department of Health and Human Services. https://health.gov/healthypeople/objectives-and-data/browse-objectives/cancer.
2. García-Torres F, Jacek Jabłoński M, Gómez Solís Á, Moriana JA, Jaén-Moreno MJ, Moreno-Díaz MJ, et al. Social Support as Predictor of Anxiety and Depression in Cancer Caregivers Six Months After Cancer Diagnosis: A Longitudinal Study. J Clin Nurs (2020) 29(5-6):996–1002. doi: 10.1111/jocn.15123
3. Warner EL, Kent EE, Trevino KM, Parsons HM, Zebrack BJ, Kirchhoff AC. Social Well-Being Among Adolescents and Young Adults With Cancer: A Systematic Review. Cancer (2016) 122(7):1029–37. doi: 10.1002/cncr.29866
4. Coughlin SS. Social Determinants of Health and Cancer Survivorship. J Environ Health Sci (2021) 7(1):11–5.
5. Chen J-J, Wang Q-L, Li H-P, Zhang T, Zhang S-S, Zhou M-K. Family Resilience, Perceived Social Support, and Individual Resilience in Cancer Couples: Analysis Using the Actor-Partner Interdependence Mediation Model. Eur J Oncol Nurs (2021) 52:101932. doi: 10.1016/j.ejon.2021.101932
6. Luo R-Z, Zhang S, Liu Y-H. Short Report: Relationships Among Resilience, Social Support, Coping Style and Posttraumatic Growth in Hematopoietic Stem Cell Transplantation Caregivers. Psychol Health Med (2020) 25(4):389–95. doi: 10.1080/13548506.2019.1659985
7. Zamanian H, Amini-Tehrani M, Jalali Z, Daryaafzoon M, Ala S, Tabrizian S, et al. Perceived Social Support, Coping Strategies, Anxiety and Depression Among Women With Breast Cancer: Evaluation of a Mediation Model. Eur J Oncol Nurs (2021) 50:101892. doi: 10.1016/j.ejon.2020.101892
8. Diversity and Inclusion in Cancer Research and Oncology. Trends Cancer (2020) 6(9):719–23. doi: 10.1016/j.trecan.2020.07.003
9. Tucker-Seeley RD. Social Determinants of Health and Disparities in Cancer Care for Black People in the United States. JCO Oncol Pract (2021) 17(5):261–3. doi: 10.1200/OP.21.00229
10. Coughlin SS. Social Determinants of Breast Cancer Risk, Stage, and Survival. Breast Cancer Res Treat (2019) 177(3):537–48. doi: 10.1007/s10549-019-05340-7
11. Adolescent and Young Adult Oncology Progress Review Group. Closing the Gap: Research and Care Imperatives for Adolescent and Young Adults With Cancer. (2006).
12. Patterson P, McDonald FE, Zebrack B, Medlow S. Emerging Issues Among Adolescent and Young Adult Cancer Survivors. Semin Oncol Nurs (2015) 31(1):53–9. doi: 10.1016/j.soncn.2014.11.006
13. Warner EL, Kirchhoff AC, Ellington L, Waters AR, Sun Y, Wilson A, et al. Young Adult Cancer Caregivers’ Use of Social Media for Social Support. Psycho-Oncology (2020) 29(7):1185–92. doi: 10.1002/pon.5402
14. Griggs J, Maingi S, Blinder V, Denduluri N, Khorana AA, Norton L, et al. American Society of Clinical Oncology Position Statement: Strategies for Reducing Cancer Health Disparities Among Sexual and Gender Minority Populations. J Clin Oncol (2017) 35(19):2203–8. doi: 10.1200/JCO.2016.72.0441
15. Brown MT, McElroy JA. Unmet Support Needs of Sexual and Gender Minority Breast Cancer Survivors. Support Care Cancer (2018) 26(4):1189–96. doi: 10.1007/s00520-017-3941-z
16. Kent EE, Wheldon CW, Smith AW, Srinivasan S, Geiger AM. Care Delivery, Patient Experiences, and Health Outcomes Among Sexual and Gender Minority Patients With Cancer and Survivors: A Scoping Review. Cancer (2019) 125(24):4371–9. doi: 10.1002/cncr.32388
17. Scott AR, Stoltzfus KC, Tchelebi LT, Trifiletti DM, Lehrer EJ, Rao P, et al. Trends in Cancer Incidence in US Adolescents and Young Adults, 1973-2015. JAMA Netw Open (2020) 3(12):e2027738. doi: 10.1001/jamanetworkopen.2020.27738
18. Gates GJ. LGBT Data Collection Amid Social and Demographic Shifts of the US LGBT Community. Am J Public Health (2017) 107(8):1220–2. doi: 10.2105/AJPH.2017.303927
19. Briefing TGP. LGBT Identification Rises to 5.65 Ni Latest U.S. Estimate. Washington, DC: The Gallup Organization (2021).
20. Frey WH. Analysis of 2000 US Census and Census Population Estimates. Washington, DC: Brookings Institute (2020).
21. Matthews AK, Breen E, Kittiteerasack P. Social Determinants of LGBT Cancer Health Inequities. Semin Oncol Nurs (2018) 34(1):12–20. doi: 10.1016/j.soncn.2017.11.001
22. Murphy CC, Lupo PJ, Roth ME, Winick NJ, Pruitt SL. Disparities in Cancer Survival Among Adolescents and Young Adults: A Population-Based Study of 88 000 Patients. JNCI: J Natl Cancer Institute (2021) 113(8):1074–83. doi: 10.1093/jnci/djab006
23. Kirchhoff AC, Spraker-Perlman HL, McFadden M, Warner EL, Oeffinger KC, Wright J, et al. Sociodemographic Disparities in Quality of Life for Survivors of Adolescent and Young Adult Cancers in the Behavioral Risk Factor Surveillance System. J Adolesc Young Adult Oncol (2014) 3(2):66–74. doi: 10.1089/jayao.2013.0035
24. Feuz C. Are Current Care Models Meeting the Psychosocial Needs of Adolescent and Young Adult Cancer Survivors? A Literature Review. J Med Imaging Radiat Sci (2014) 45(2):119–30. doi: 10.1016/j.jmir.2013.09.002
25. Webster R, Drury-Smith H. How Can We Meet the Support Needs of LGBT Cancer Patients in Oncology? A Systematic Review. Radiography (2020) 27(2):633–44. doi: 10.1016/j.radi.2020.07.009
26. Snapp SD, Watson RJ, Russell ST, Diaz RM, Ryan C. Social Support Networks for LGBT Young Adults: Low Cost Strategies for Positive Adjustment. Family Relations (2015) 64(3):420–30. doi: 10.1111/fare.12124
27. Jones EC, Storksdieck M. Recent Research on the Social Network Concept and Cancer. Curr Opin Support Palliative Care (2019) 13(3):225–37. doi: 10.1097/SPC.0000000000000442
28. Pew Research Center. As Millenials Near 40, They’re Approaching Family Life Differently Than Previous Generations. (2020).
29. Jackson Levin N, Kattari SK, Piellusch EK, Watson E. “We Just Take Care of Each Other”: Navigating ‘Chosen Family’ in the Context of Health, Illness, and the Mutual Provision of Care Amongst Queer and Transgender Young Adults. Int J Environ Res Public Health (2020) 17(19):7346. doi: 10.3390/ijerph17197346
30. Huang IC, Jones CM, Brinkman TM, Hudson MM, Srivastava DK, Li Y, et al. Development of the Functional Social Network Index for Adolescent and Young Adult Cancer Survivors. Cancer (2018) 124(10):2220–7. doi: 10.1002/cncr.31278
31. Kamen C. Lesbian, Gay, Bisexual, and Transgender (LGBT) Survivorship. Semin Oncol Nurs (2018) 34(1):52–9. doi: 10.1016/j.soncn.2017.12.002
32. Kaluarachchi T, McDonald F, Patterson P, Newton-John TRO. Being a Teenager and Cancer Patient: What do Adolescents and Young Adults With Cancer Find Valuable and Challenging With Their Friends and Cancer Peers? J Psychosocial Oncol (2020) 38(2):195–209. doi: 10.1080/07347332.2019.1672847
33. Capistrant BD, Lesher L, Kohli N, Merengwa EN, Konety B, Mitteldorf D, et al. Social Support and Health-Related Quality of Life Among Gay and Bisexual Men With Prostate Cancer. Oncol Nurs Forum (2018) 45(4):439–55. doi: 10.1188/18.ONF.439-455
34. Capistrant BD, Torres B, Merengwa E, West WG, Mitteldorf D, Rosser BRS. Caregiving and Social Support for Gay and Bisexual Men With Prostate Cancer. Psycho-Oncology (2016) 25(11):1329–36. doi: 10.1002/pon.4249
35. Dakin EK, Williams KA, MacNamara MA. Social Support and Social Networks Among LGBT Older Adults in Rural Southern Appalachia. J Gerontol Soc Work (2020) 63(8):768–89. doi: 10.1080/01634372.2020.1774028
36. Hsieh N, Wong JS. Social Networks in Later Life: Similarities and Differences Between Sexual-Minority and Heterosexual Older Adults. Socius (2020) 6:2378023120977731. doi: 10.1177/2378023120977731
37. Breder K, Bockting W. Social Networks of LGBT Older Adults: An Integrative Review. Psychol Sexual Orientation Gender Diversity (2022). Advance online publication. doi: 10.1037/sgd0000552
38. Trujillo MA, Perrin PB, Sutter M, Tabaac A, Benotsch EG. The Buffering Role of Social Support on the Associations Among Discrimination, Mental Health, and Suicidality in a Transgender Sample. Int J Transgenderism (2017) 18(1):39–52. doi: 10.1080/15532739.2016.1247405
39. Budge SL, Adelson JL, Howard KA. Anxiety and Depression in Transgender Individuals: The Roles of Transition Status, Loss, Social Support, and Coping. J Consult Clin Psychol (2013) 81(3):545–57. doi: 10.1037/a0031774
40. Reblin M, McCormick R, Mansfield KJ, Wawrzynski SE, Ketcher D, Tennant KE, et al. Feasibility, Usability, and Acceptability of Personalized Web-Based Assessment of Social Network and Daily Social Support Interactions Over Time. J Cancer Survivorship (2022) 1–9. doi: 10.1007/s11764-021-01083-x
41. Etikan I. Comparison of Convenience Sampling and Purposive Sampling. Am J Theor Appl Stat (2016) 5(1):1–4. doi: 10.11648/j.ajtas.20160501.11
42. Denlinger CS, Carlson RW, Are M, Baker KS, Davis E, Edge SB, et al. Survivorship: Introduction and Definition. Clin Pract Guidelines Oncol J Natl Compr Canc Netw (2014) 12(1):34–45. doi: 10.6004/jnccn.2014.0001
43. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap Consortium: Building an International Community of Software Platform Partners. J Biomed Inf (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208
44. Borgatti SP, Everett MG, Freeman LC. Ucinet for Windows: Software for Social Network Analysis. Havard, MA: Analytic Technologies (2002).
45. Bavik YL, Shaw JD, Wang X-H. Social Support: Multidisciplinary Review, Synthesis, and Future Agenda. Acad Manage Ann (2020) 14(2):726–58. doi: 10.5465/annals.2016.0148
46. Burkhalter JE, Margolies L, Sigurdsson HO, Walland J, Radix A, Rice D, et al. The National LGBT Cancer Action Plan: A White Paper of the 2014 National Summit on Cancer in the LGBT Communities. LGBT Health (2016) 3(1):19–31. doi: 10.1089/lgbt.2015.0118
47. Thompson T, Heiden-Rootes K, Joseph M, Gilmore LA, Johnson L, Proulx CM, et al. The Support That Partners or Caregivers Provide Sexual Minority Women Who Have Cancer: A Systematic Review. Soc Sci Med (2020) 261:113214. doi: 10.1016/j.socscimed.2020.113214
48. AARP and National Alliance for Caregiving. Caregiving in the United States 2020. Washington, D.C (2020).
49. Child ST, Lawton L. Loneliness and Social Isolation Among Young and Late Middle-Age Adults: Associations With Personal Networks and Social Participation. Aging Ment Health (2019) 23(2):196–204. doi: 10.1080/13607863.2017.1399345
50. Erosheva EA, Kim H-J, Emlet C, Fredriksen-Goldsen KI. Social Networks of Lesbian, Gay, Bisexual, and Transgender Older Adults. Res Aging (2016) 38(1):98–123. doi: 10.1177/0164027515581859
51. Kim H-J, Fredriksen-Goldsen KI, Bryan AEB, Muraco A. Social Network Types and Mental Health Among LGBT Older Adults. Gerontologist (2017) 57(suppl_1):S84–94. doi: 10.1093/geront/gnw169
52. Farrell AK, Stanton SCE, Masrhall E. Social Network Strucure and Combating Social Disconnection: Implications for Physical Health. Curr Opin Psychol (2022) 45:101313. doi: 10.1016/j.copsyc.2022.101313
53. Trieu P, Bayer JB, Ellison NB, Schoenebeck S, Falk E. Who Likes to be Reachable? Availability Preferences, Weak Ties, and Bridging Social Capital. Information Commun Soc (2019) 22(8):1096–111. doi: 10.1080/1369118X.2017.1405060
54. Schröders J, Dewi FST, Nilsson M, Nichter M, Sebastian MS. Effects of Social Network Diversity in the Disablement Process: A Comparison of Causal Inference Methods and an Outcome-Wide Approach to the Indonesian Family Life Surveys, 2007–2015. Int J Equity Health (2020) 19(1):128. doi: 10.1186/s12939-020-01238-9
55. Heerde JA, Hemphill SA. Examination of Associations Between Informal Help-Seeking Behavior, Social Support, and Adolescent Psychosocial Outcomes: A Meta-Analysis. Dev Rev (2018) 47:44–62. doi: 10.1016/j.dr.2017.10.001
56. Uchino BN, Trettevik R, Kent de Grey RG, Cronan S, Hogan J, Baucom BRW. Social Support, Social Integration, and Inflammatory Cytokines: A Meta-Analysis. Health Psychol (2018) 37(5):462–71. doi: 10.1037/hea0000594
57. Toledo G, Ochoa CY, Farias AJ. Exploring the Role of Social Support and Adjuvant Endocrine Therapy Use Among Breast Cancer Survivors. Support Care Cancer (2020) 28(1):271–8. doi: 10.1007/s00520-019-04814-0
58. Kamen C, Jabson JM, Mustian KM, Boehmer U. Minority Stress, Psychosocial Resources, and Psychological Distress Among Sexual Minority Breast Cancer Survivors. Health Psychol (2017) 36(6):529–37. doi: 10.1037/hea0000465
59. Winckworth-Prejsnar K, McCanney J, Schatz AA, Smedley W, Platanias LC, Benitez CM, et al. Policy Challenges and Opportunities to Address Changing Paradigms in Cancer Care Delivery. J Natl Compr Cancer Netw J Natl Compr Canc Netw (2019) 17(5):424–31. doi: 10.6004/jnccn.2019.7299
60. Koltai K, Walsh C, Jones B, Berkelaar BL. Applying Social Network Analysis to Identify the Social Support Needs of Adolescent and Young Adult Cancer Patients and Survivors. J Adolesc Young Adult Oncol (2018) 7(2):181–6. doi: 10.1089/jayao.2017.0058
Keywords: LGBTQIA+, cancer survivor, care partner, young adult, sexual and gender minority, social network, social support
Citation: Cloyes KG, Guo J-W, Tennant KE, McCormick R, Mansfield KJ, Wawrzynski SE, Classen SC, Jones EC and Reblin M (2022) Exploring Social Support Networks and Interactions of Young Adult and LGBTQIA+ Cancer Survivors and Care Partners. Front. Oncol. 12:852267. doi: 10.3389/fonc.2022.852267
Received: 11 January 2022; Accepted: 14 March 2022;
Published: 08 April 2022.
Edited by:
Gwendolyn P. Quinn, New York University, United StatesReviewed by:
Kimberley Allison, Canteen Australia, AustraliaBenjamin Margolis, Albany Medical College, United States
Copyright © 2022 Cloyes, Guo, Tennant, McCormick, Mansfield, Wawrzynski, Classen, Jones and Reblin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kristin G. Cloyes, Kristin.cloyes@nurs.utah.edu
 Kristin G. Cloyes
Kristin G. Cloyes Jia-Wen Guo
Jia-Wen Guo Karrin E. Tennant
Karrin E. Tennant Rachael McCormick
Rachael McCormick Kelly J. Mansfield
Kelly J. Mansfield Sarah E. Wawrzynski
Sarah E. Wawrzynski Sarah C. Classen
Sarah C. Classen Eric C. Jones
Eric C. Jones Maija Reblin
Maija Reblin