Secondary outcomes of enhanced cognitive behavioral therapy (eCBT) for children and adolescents with obsessive-compulsive disorder
- 1Norwegian Centre for E-health Research, University Hospital of North Norway, Tromsø, Norway
- 2Faculty of Psychology, University of Iceland, Reykjavík, Iceland
- 3Department of Mental Health, Regional Centre for Child and Youth Mental Health and Child Welfare (RKBU Central Norway), Norwegian University of Science and Technology, Trondheim, Norway
- 4Department of Child and Adolescent Psychiatry, St. Olav’s University Hospital, Trondheim, Norway
- 5Accare Child Study Center, Groningen, Netherlands
Background: Obsessive-compulsive disorder (OCD) is a debilitating mental health condition usually presenting with a high degree of comorbid symptoms in the majority of cases. Although face-to-face cognitive-behavioral therapy (CBT) is considered the therapeutic golden standard for pediatric OCD, its accessibility, availability, and consistency in delivery are still limited. To address some of these challenges, an enhanced CBT (eCBT) package was created and introduced. This study explored eCBT’s broad-based impact on OCD-related comorbid symptoms, functional impairment, quality of life and family accommodation among youth with OCD.
Methods: This open trial involved 25 pediatric patients with OCD (7−17 years), assessed between January 2018 to February 2020. All patients received eCBT for 14 weeks. Secondary outcomes were assessed at baseline, post-treatment, and 3-, 6-, and 12-month follow-up co-occurring symptoms were evaluated using the Strengths and Difficulties Questionnaire (SDQ), Screen for Child Anxiety-Related Emotional Disorders (SCARED), and Mood and Feelings Questionnaire (MFQ). Quality of life was measured using the KINDL-R, functional impairment through the Child Obsessive-Compulsive Impact Scale Revised (COIS-R), and family accommodation by the Family Accommodation Scale (FAS). Linear mixed-effects models were applied to analyze treatment effects.
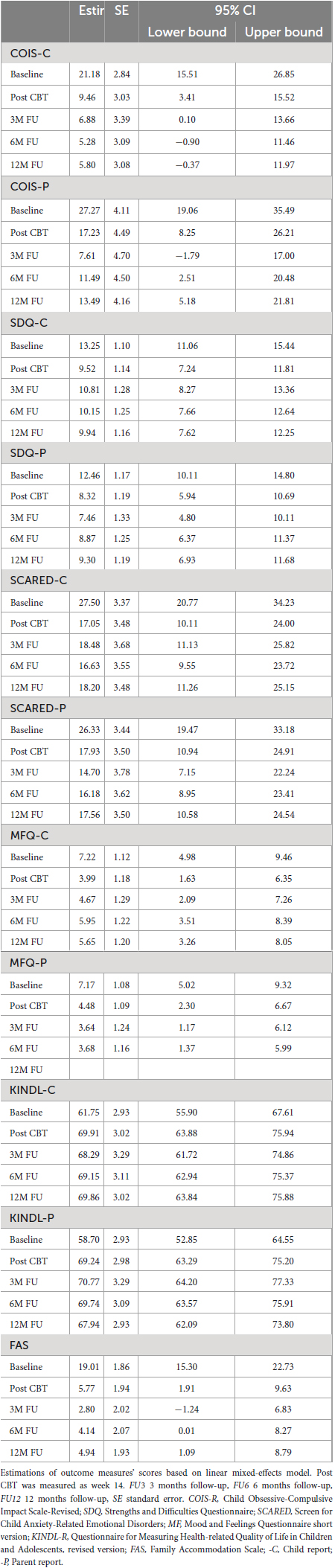
Results: Results indicated a significant decrease in OCD-related comorbid symptoms post-treatment, with SDQ mean reduce of 3.73 (SE = 1.10, child) and 4.14 (SE = 1.19, parent), SCARED mean reduce of 10.45 (SE = 2.52, child) and 8.40 (SE = 2.82, parent), MFQ mean reduce of 3.23 (SE = 1.11, child) and 2.69 (SE = 1.18, parent). Family accommodation declined with clinician scored FAS mean reduction of 13.25 (SE = 2.31). Quality-of-Life improved significantly post-treatment, with KINDL mean increase of 8.15 (SE = 2.87, children), and 10.54 (SE = 3.07, parents). These positive improvements were further amplified at the 3-month follow-up and remained consistent at the 12-month follow-up.
Conclusion: A significant reduction was observed in all secondary outcomes employed and OCD-related functional impairments from baseline to post-treatment, which was maintained through 12-month follow-up. These results imply that after receiving eCBT, children and adolescents experienced substantial decrease in the negative impacts of OCD-related symptoms on their daily life, including home, school, and social interactions.
Introduction
Obsessive-compulsive disorder (OCD) is a debilitating mental health disorder affecting 1−3% children and adolescents globally (Flament et al., 1988; Zohar et al., 1992; Valleni-Basile et al., 1994; Douglass et al., 1995; Stewart et al., 2004). Pediatric OCD is often accompanied by various comorbid conditions, including major depressive disorder, anxiety disorders, disruptive behavior disorders, and attention-deficit/hyperactivity disorder (Sharma et al., 2021). These comorbidities often exacerbate impairments in quality of life for affected children and adolescents (Geller et al., 1996, 2001, 2003; Masi et al., 2004, 2006; Sukhodolsky et al., 2005; Termine et al., 2006; Sharma et al., 2021).
Cognitive-behavioral therapy (CBT) with Exposure and Response Prevention (E/RP) is widely recognized as the first-line treatment for pediatric OCD (National Collaborating Centre for Mental Health [NCCMH], 2006). Previous research has consistently shown moderate to large effect sizes for CBT in treating OCD in children (McGuire et al., 2015; Skarphedinsson et al., 2015; Torp et al., 2015b). Moreover, CBT has demonstrated certain advantages over selective serotonin reuptake inhibitors (SSRIs) (Öst et al., 2016). Although limited, previous evidence suggests that CBT can reduce the impact of comorbid symptoms in pediatric OCD. For example, a meta-analysis (Sánchez-Meca et al., 2014) about the differential efficacy of CBT, pharmacological and combined treatment for pediatric OCD including 18 studies, concluded that all types of interventions were efficacious not only in reducing obsessive–compulsive symptoms, but also improved depression, anxiety, and other secondary responses, especially with CBT interventions.
Despite its promise, access to CBT still remains limited due to various barriers, including a lack of experienced therapists, long waiting lists, geographical limitations, and high costs (Franklin et al., 2013). Technological innovations present a potential solution to these challenges (Storch et al., 2011; Farrell et al., 2016; Lenhard et al., 2017). In this context, we developed an enhanced CBT (eCBT) package aiming to improve both access and treatment outcomes (Wolters et al., 2020). The primary studies explored, respectively, feasibility and accessibility (Babiano-Espinosa et al., 2021), and efficacy (Babiano-Espinosa et al., 2022) of eCBT, demonstrating significant reduction in OCD symptom severity [as measured by the Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS)], with 76% of participants classified as responders (CY-BOCS total score ≤15) and mean reduction of 63.8% on the CY-BOCS at post-treatment. The primary study (Babiano-Espinosa et al., 2022) also reported further decreases in CY-BOCS scores at 3 and 6-month follow-ups.
Besides the importance of primary outcomes, the limited attention to secondary outcomes such as comorbid symptoms, quality of life (QoL), and family accommodation constitutes a significant gap in the literature (Ginsburg et al., 2008; Lack et al., 2009; Weidle et al., 2014; Torp et al., 2015a). Addressing secondary outcomes is not merely an academic exercise, they are frequently associated with poorer primary treatment outcomes and are key indicators of treatment’s broader impact. For instance, family accommodation, which occurs within the context of family dynamics, can be highly resistant to change. Previous studies have indicated that children may be more reluctant to participate in treatment and refrain from confronting their obsessional fears, making symptom attenuation less likely (Ginsburg et al., 2008; Peris et al., 2008; Merlo et al., 2009; Garcia et al., 2010). Furthermore, early reductions in family accommodation have been shown to correlate with treatment effects at post-treatment (Piacentini et al., 2011; Peris et al., 2017) and during long-term follow-up (Piacentini et al., 2011). Moreover, comorbid symptoms are frequently associated with poorer primary treatment outcomes (Ginsburg et al., 2008; Torp et al., 2015a), and children and adolescents with OCD tended to experience increased comorbidity and reduced QoL compared to those without OCD (Lack et al., 2009; Weidle et al., 2014; Storch et al., 2018; Zaboski et al., 2019; Jensen et al., 2022).
The current study aims to explore the impact of eCBT on secondary outcomes, i.e., comorbid symptoms, QoL, and family accommodation in children and adolescents with OCD. We hypothesize that eCBT for OCD will reduce OCD-related comorbid symptoms and family accommodation, as well as increase quality of life.
Materials and methods
Study design
The open trial study took place at Child and Adolescent Mental Health Services (CAMHS) in St. Olav’s University Hospital, Trondheim, Norway (n = 23) and CAMHS in Hospital of Aalesund, Norway (n = 2) from January 2018 to February 2020. Assessments were made at baseline (week 0), post-treatment (week 14), 3-month follow-up, 6-month follow-up, and 12-month follow-up.
Treatment and procedures
Enhanced cognitive-behavioral treatment (eCBT) is an innovative treatment package for children and adolescents with OCD. The treatment manual is derived from a NordLOTS manual (Jensen et al., 2022) and a Dutch treatment manual (Piacentini et al., 2007) for pediatric OCD. eCBT uniquely contains face-to-face sessions – covering psychoeducation, E/RP, cognitive interventions, and relapse prevention – with the flexibility of home-based videoconferencing sessions. The direct interaction in face-to-face sessions potentially strengthens the therapeutic alliance and provides comprehensive observational insights that webcam interactions may miss (Wolters et al., 2020). Videoconferencing, on the other hand, facilitates E/RP exercises in home environment or other natural settings. This approach aims to enhance the ecological validity of the treatment and encourage the application of CBT principles beyond the therapist’s office, directly into the settings where the problems naturally occur (Wolters et al., 2020). Compared to traditional CBT, eCBT offers more frequent therapist contact, overcoming geographical limitations. Additionally, eCBT incorporates an app to support psychoeducation and structured E/RP between sessions.
Enhanced cognitive-behavioral treatment (eCBT) covered a 14-weeks treatment period. The first part of the treatment (week 1−5) consists of weekly (45 min) face-to-face sessions, equivalent to traditional CBT. In the first week, psychoeducation videos and the eCBT concept (including the smartphone application system) are introduced to the patients and parents. From week 2, the E/RP exercises are modelled in the office followed by homework exercises based on an individualized OCD symptom inventory provided by children and parents. As soon as the child starts with E/RP homework (week 2), treatment is supplemented by a weekly videoconferencing (15 min) meeting, resulting in two appointments (one face-to-face session and one video conferencing session) with the therapists per week. During the additional webcam sessions, homework is reviewed and E/RP exercise at home or at another location can be performed. From week 6 onwards, the frequency of the face-to-face sessions is reduced to bi-weekly, while the frequency of webcam sessions (guided E/RP at home) is increased, resulting in one face-to-face session and two videoconferencing meetings in a two-week period. This default schedule provides the possibility to perform therapist assisted E/RP exercises in a natural environment. The frequency of sessions could be altered and personalized to patients’ needs but could not exceed the total number of sessions (a maximum of 10 face-to-face sessions and up to 12 shorter webcam sessions).
Treatment sessions are coordinated in a smartphone application (app) system. The app system consists of separate apps for children and parents, and a web-based application for therapists with a coordinating and monitoring function. All the apps are interconnected to synchronize the treatment outcome. The app provides information about OCD and CBT in the form of psychoeducation videos, supports, and structures E/RP at home, and closely monitors treatment progress. It can be used either in treatment sessions together with the therapists or independently at home. The app has been developed for the Android system, and children who had iPhone were given Android phones by the study staff.
Participants
Participants were eligible for the study based on these criteria: (a) aged between 7−17 years; (b) a primary Diagnostic and Statistical Manual of Mental Disorders (DSM)-5 diagnosis of OCD1 ; (c) CY-BOCS score ≥16.
We excluded individuals who met any of the following conditions: (a) the presence of psychiatric comorbidity that has a higher treatment priority than OCD or rendering participation clinically inappropriate (examples include primary anorexia nervosa, depression with suicidality, and psychosis); (b) current engagement in psychological treatment specifically for OCD; (c) significant developmental delays; (d) inadequate proficiency in the Norwegian language.
Concurrent medications except for OCD were allowed during the study (Babiano-Espinosa et al., 2021). Among the participants, five were on medication: two on Methylphenidate for Attention deficit/hyperactivity disorder (ADHD), one on Guanfacine for tics and ADHD, one on Risperidone for eating disorder, and one on Aripiprazole for bipolar disorder. None were using SSRIs or other medications for anxiety or depression (Babiano-Espinosa et al., 2021).
Measures
Comorbid symptoms and impairments
Child Obsessive-Compulsive Impact Scale-Revised (COIS-R) measures OCD-specific functional impairment of children and adolescents (Piacentini et al., 2007). There are separate child- and parent-rated questionnaires, each consisting of 33 items and a total score ranging from 0 to 99. A higher score indicates more severe functional impairment. The COIS-R demonstrated good internal consistency for both parent report (α = 0.83−0.91) and children report (α = 0.78−0.92) (Piacentini et al., 2007).
Strengths and Difficulties Questionnaire (SDQ) is a clinical tool to measure psychological adjustment in children and adolescents (Goodman, 1997). It is a broader measure of child’s mental health symptoms. The SDQ includes both a youth self-report and a parent-proxy version, each consisting of 25 items divided into five subscales. These subscales assess various aspects of a child’s emotional and behavioral functioning: emotional symptoms, conduct or behavior problems, hyperactivity-inattention, peer problems, and prosocial behavior. In our study, we use the Total Difficulties Score of SDQ (scoring from 0−40) to provide a measure of general psychological functioning from the perspectives of both the child and their parent. The Total Difficulties score includes the four problem-based subscales (emotional symptoms, conduct problems, hyperactivity-inattention, and peer problems). The Total Difficulties Score of the SDQ has shown satisfactory psychometric properties in children and adolescents (α = 0.74−0.80) as well as parents’ proxy samples (α = 0.76) (Van Roy et al., 2008).
Screen for Child Anxiety-Related Emotional Disorders (SCARED) is a 50-item child and parent self-support instrument (score 0−40) for child anxiety screening (Birmaher et al., 1997). A total score of ≥25 may indicate the presence of an anxiety disorder. Both the child and parent SCARED showed adequate internal consistency (α = 0.74−0.93) and good test-retest reliability (r = 0.70−0.90, intraclass correlation coefficient) (Birmaher et al., 1997).
Mood and Feelings Questionnaire, short version (MFQ) is a 13-item children and parent-rated measure assessing recent depressive symptomatology in children aged 6−17 years (Angold et al., 1995). Scores on the MFQ range between 0 to 26, with higher scores indicating greater depressive severity of a child. MFQ showed good internal consistency in both children (α = 0.76) and parent version (α = 0.87) (Sucupira et al., 2017).
Quality of life
Questionnaire for Measuring Health-related Quality of Life in Children and Adolescents, revised version (KINDL-R) is a well-established QoL questionnaire used in children and adolescents (Ravens-Sieberer et al., 2008). The present study employed both the self-reported questionnaire for children and adolescents and the parent proxy version. The KINDL-R questionnaire consists of 24 items which the participants were asked to rate on a five-point Likert scale (1 = never, 5 = always). The questionnaire is equally distributed into six subscales, representing the child’s well-being in physical, emotional, self-esteem, family, friends, and school over the past week. All subscale scores can be combined for a total QoL score, transformed to a scale ranging from 0−100. A higher score represents a better quality of life. In addition, the questionnaire provides an independent disorder-related subscale to produce information on the perceptions of OCD-related burden. Psychometric testing of the KINDL-R revealed good scale utilization (except for the family subscale showing ceiling effects of 17%) and sound scale fit (85%) (Bullinger et al., 2008). The internal consistencies for subscales ranged from α = 0.54 (friends and school) to α = 0.73 (family) and an α = 0.82 for the total score (Bullinger et al., 2008).
Family accommodation
Family Accommodation Scale (FAS) is a 12-item clinician-rated questionnaire with a total score ranging from 0−48 (Calvocoressi et al., 1999). It measures the extent to which the family members accommodate the child’s OCD symptoms as well as distress/impairment related to such accommodation. The FAS demonstrates satisfactory interrater reliability ranging from 0.72−1.0, as measured by intraclass correlation coefficients, and good internal consistency (α = 0.76) (Calvocoressi et al., 1999).
Analysis
COIS-R, SDQ, SCARED, MFQ, and KINDL was filled in by 25 children and 25 parents. FAS was filled by 25 parents. Statistical analyses on secondary outcome variables at Baseline, Post CBT, 3-month follow-up (FU3), 6-month follow-up (FU6), and 12-month follow-up (FU12) were conducted using linear mixed-effected (LME) models (Supplementary Table 1). The fixed effect was time (Baseline, Post CBT, FU3, FU6, and FU12) and was treated as a categorical variable. Random effects included intercept and linear slope terms. Missing data were handled with maximum likelihood estimation as part of the LME. For each variable, mean value and standard deviation were reported with p-value and 95% confidence interval. To understand whether the change in secondary outcomes was related to the change of time, the relationship between baseline and follow-up treatment change in each variable score were calculated and reported as correlation coefficients (see Supplementary Table 1). Analyses were conducted in Statistical Analysis System (SAS) and Statistical Package for the Social Sciences (SPSS).
Results
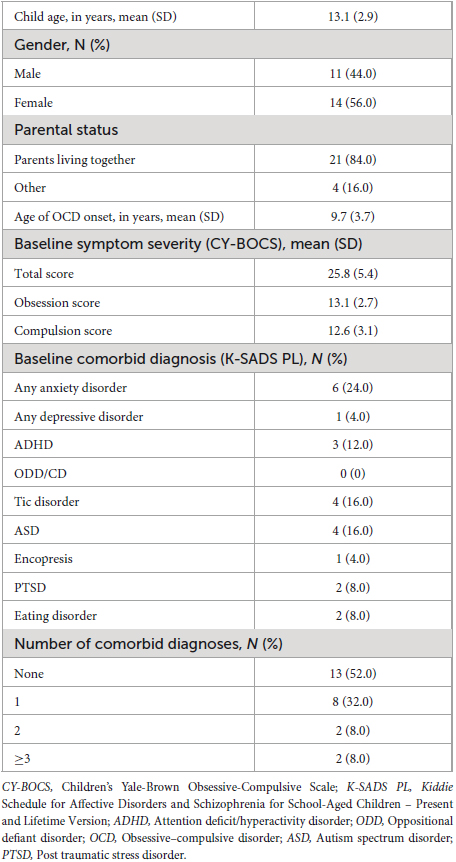
All 25 patients enrolled and completed eCBT treatment program (Table 1). Mean age of participants (N = 25) was 13.1 years (2.9) with slightly more girls (56%) than boys. Most of the participants (84%) lived with parents. Anxiety disorder (24%) was the most prevalent comorbid disorder among participants, followed by Tic disorder (16%) and autism spectrum disorder (ASD, 16%) (Table 1). Details regarding the administration and assessment of CY-BOCS and K-SADS PL have been described elsewhere (Wolters et al., 2020; Babiano-Espinosa et al., 2021).
Secondary outcomes
Comorbid symptoms and impairments
In the child-reported version of COIS (COIS-C), the baseline score for functional impairment was significantly higher (p < 0.001) than the score at all other subsequent assessment points, including the post-treatment evaluation (Tables 2, 3). This suggests that functional impairment reduces following the treatment and that improvement is maintained through FU12. Childrens’ post-treatment scores were not significantly different from those at the FU-points, suggesting that functional impairment reduces following treatment, and that improvement is maintained through the follow up period. In the parent-reported version of COIS (COIS-P), the scores also significantly decreased at all assessment points. The most rapid decrease was observed at the FU3 (p < 0.001), with a more gradual but still significant decline seen at post treatment evaluation (p < 0.05).
Child-reported SDQ (SDQ-C) scores improved from baseline to post-treatment (mean reduce = 3.73, SE = 1.10, p < 0.01). No significant change was observed between baseline and FU3 (p = 0.054) or in subsequent follow-ups, suggesting that improvement in child-reported emotional and behavioral functioning was maintained over time. In the parent reported version, a significant improvement was observed at post-treatment (p < 0.001) and at FU3 (p < 0.001). In addition, further improvements were observed at FU6 and FU12 (p < 0.01).
Compared to baseline, significant reductions were observed in the child-reported SCARED scores post-treatment (mean reduce = 10.45, SE = 1.10, p < 0.001) and at all subsequent FUs (FU3: mean reduce = 9.02, SE = 2.80, p < 0.01; FU6: mean reduce = 10.87, SE = 2.62, p < 0.001; FU12: mean reduce = 9.30, SE = 2.50, p < 0.001). Similar significant improvements were found in SCARED-P, also these were maintained throughout the FU period.
In both MFQ-C and MFQ-P, the baseline score was significantly higher than post-treatment and any subsequent assessment point (Tables 2, 3). This indicates that depressive symptoms reduced following treatment and this reduction was maintained up to the FU12.
Quality of life
Both child- and parent-rated KINDL-R scores have improved significantly from baseline to post-treatment, and from baseline to the FU3 (p < 0.001) (Table 3). Specifically, there was a mean increase of 3.73 points (SE = 1.57) from baseline to post treatment, and 6.93 points (SE = 2.92) from baseline to FU3 for children. For parents, the corresponding increase was 6.57 points (SE = 1.67) from baseline to post and a 12.20-point increase (SE = 3.09) from baseline to FU3.
Family accommodation
Family Accommodation Scale (FAS) scores showed a significant decrease at post-treatment compared to baseline (p < 0.001) (Table 3). Mean decrease was 8.65 points (SE = 1.21) from baseline to post-treatment, and 16.06 points (SE = 2.26) compared from baseline to FU3 for children’s scores.
Discussion
The present study investigated the impact of eCBT for pediatric OCD on comorbid symptoms, OCD-related functional impairment, quality of life, and family accommodations. Overall, we observed a statistically significant reduction in all secondary outcomes from baseline to post-treatment, which was maintained through the 12-month follow-up period. These results suggest that the participants experienced significant improvements in daily functioning across various domains, including home life, schooling, and social interactions. Our findings conveyed a positive message, suggesting that the treatment effects of pediatric OCD may extend beyond merely reducing OCD symptoms. This is in line with an early study by (Conelea et al., 2017), which observed improvement in non-OCD anxiety, inattention, hyperactivity, and overall quality of life following CBT for pediatric OCD. Furthermore, the decreased OCD-related functional impairment evidenced by our results resonate with previous research (Storch et al., 2011; Bonnert et al., 2014), reinforcing the idea that effects of treatment are broader than solely targeting OCD symptoms.
We observed a reduction in general psychological adjustment in children and adolescents, as reflected in the total score of the SDQ (both parents and the young people), from baseline to post-treatment and at three-month follow-up. This finding indicates that eCBT demonstrated an overall positive impact on youth with OCD in various domains – spanning child’s overall emotional well-being, behavior, attention, peer relations, and prosocial behavior – as rated by both children and parents. Particularly, the co-occurring emotional problems, such as depressive symptoms, witnessed a significant decline, as measured by the MFQ scores (both parents and the young people) from baseline to post-treatment and sustained through the 12-month follow up. This outcome supports our hypothesis that effectively treating OCD symptoms may enhance overall mood, particularly considering that many children with OCD often experience depression due to the restrictive nature of their disorder in social life (Griffiths et al., 2012). The reduction of OCD likely lessens this burden. During eCBT, pediatric patients learned techniques to manage obsessions and other intrusive thoughts that can also contribute to depression and anxiety. These techniques can also be beneficial for treating non-OCD anxiety symptoms, thereby improving comorbid symptoms. Our findings resonate with those from a large previous meta-analysis conducted by Sánchez-Meca et al. (2014), which reported improvements in depression, anxiety, and other secondary responses following treatment, irrespective of the modality (CBT, medication, or their combination), with CBT showing particular effectiveness.
Another noteworthy improvement in emotional well-being in our study was the significant reduction in overall anxiety symptoms, as evidenced by the score of SCARED (both parents and the young people), from baseline to post-treatment, and consistently maintained at the three-month follow-up. These reductions encompass a range of anxiety symptoms, including generalized anxiety, panic symptoms, separation anxiety symptoms, social anxiety symptoms and anxiety related to school. Given the high prevalence of OCD and co-occurring anxiety symptoms (Banneyer et al., 2018), the observed reduction in anxiety symptom levels following CBT in pediatric OCD cases holds clinical importance. Our results mirror those of a recent study by Babiano-Espinosa et al. (2022), which underscored the effectiveness of eCBT in reducing anxiety symptoms and stress. Furthermore, our findings are in line with several previous research in this domain. For example, a study by (Cancilliere et al., 2018) found that children aged 5−8 years (n = 127) who underwent family-based CBT for OCD exhibited significantly reduced comorbid anxiety symptoms than those receiving family-based Relaxation Therapy. Similarly, Conelea et al. (2017) reported a reduction in comorbid anxiety and inattention symptoms among OCD patients treated with CBT in combination with medication.
Aligned with our hypothesis, we observed significant reductions in OCD-specific functional impairment, as measured by COIS scores (from both parents and the young people), at post-treatment. The gains were maintained through the 12-month follow-up. This pattern of improvements mirrors findings from the Nordic Long-term OCD treatment Study (NordLOTS) by Højgaard et al. (2017), where both patient- and parent-rated functioning in pediatric patients showed maintained enhancements one year post-CBT. Similarly, our results resonate with the study by Bolton et al. (2011), which also reported a significant reduction in the impact of pediatric OCD on level of functioning. Furthermore, we observed a significant overall decrease in family accommodation over time, which is in line with the trends observed in previous studies (Piacentini et al., 2011; Thompson-Hollands et al., 2015; Peris et al., 2017). This outcome holds clinical importance in treating pediatric OCD, as evidence reveals that higher levels of family accommodation (e.g., specific contamination/cleaning symptoms and behavioral manifestations) are often linked with increased severity of OCD symptoms (Skarphedinsson et al., 2023).
Both children and parents reported an improvement in quality of life (QoL) from baseline to post-treatment, aligning with findings from previous studies (Weidle et al., 2015; Storch et al., 2018). Interestingly, we observed further improvement from baseline to the three-month follow-up, which persisted throughout the follow-up period. This additional improvement during the first 3°months after treatment may be indicative of a phase where skills and gains acquired during therapy are integrated into daily life, leading to a continued improvement in QoL beyond mere symptom reduction. This observation is consistent with the understanding from earlier research by Weidle, 2015, which documented that alleviating OCD symptoms has a positive impact on children’s overall quality of life and well-being.
Strengths and limitations
The strength of our study is a comprehensive evaluation of outcome of OCD-related impairments beyond OCD symptom reduction after treatment in pediatric OCD employing reliable instruments and a multi-perspective approach, representing both children and parents. Another strength is the assessment of comorbid symptoms, OCD-related impairments quality of life, and family accommodation with follow-up points over a span of 12 months.
However, the main limitation for interpreting the results from our study is relatively small sample size, due to the pilot character of the intervention. This limits generalizability of the findings. However, our study sample comprises patients exhibiting moderate to severe OCD and a high prevalence of comorbid symptoms which seems to be demographic representative for patients usually referred for OCD treatment to child psychiatric services. In addition, we acknowledge the potential for type I error due to not correcting for multiple comparisons. Our methodology, using linear-mixed effects models, mitigates this risk by adjusting for correlations within repeated measures. Nonetheless, the exploratory nature of our study and the conventions of related research allow for this approach, though it may constrain the interpretability of our results. In addition, as an open-label trial study lacking a control group, the potential influence of other factors such attention, spontaneous remission, or regression to the mean, cannot be ruled out. Another limitation is that eCBT was facilitated through an app designed for the Android platform only. Hence, children with iPhones and no access to an Android device had to borrow one for the study’s duration, including the need to manage and maintain the function of two devices, potentially influencing their motivation and engagement for treatment.
Conclusion
Enhanced cognitive behavioral therapy (eCBT) for pediatric OCD decreased OCD-associated comorbid anxiety- and depressive symptoms, impairments of daily life functioning and improved quality of life beyond OCD symptom reduction. These improvements were sustained over a period of time.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Regional Committee for Medical and Health Research Ethics (No 2016/716/REK Nord) and registered with the ISRCTN (https://www.isrctn.com/) registry (trial ID: ISRCTN37530113). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
BoW: Conceptualization, Data curation, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. GS: Software, Supervision, Validation, Writing – review & editing. BeW: Resources, Writing – review & editing. LB-E: Writing – review & editing. LW: Writing – review & editing. JA: Writing – review & editing. NS: Funding acquisition, Project administration, Resources, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Liaison Committee for Education and Research and Innovation in Central Norway (Samarbeidsorganet mellom Helse Midt-Norge RHF og NTNU).
Acknowledgments
We thank the therapists involved in assessment or treatment of patients: Marit Synnøve Skrove, Marit Henriksen, Hanne Undheim Hoff, Lise Marie Rande Dahl, Henrik Nordahl, Ove Helset and JA. A special thank goes to all the participants and their parents.
Conflict of interest
LW receives royalties from Springer Media and Lannoo for a treatment protocol and a book on pediatric OCD.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnhum.2023.1330435/full#supplementary-material
Abbreviations
ADHD, Attention deficit/hyperactivity disorder; ASD, autism spectrum disorder; CAMHS, Child and adolescent mental health services; CBT, Cognitive-behavioral treatment; COIS-R, Child Obsessive-Compulsive Impact Scale-Revised; CY-BOCS, Children’s Yale-Brown Obsessive-Compulsive Scale; E/RP, Exposure and Response Prevention; eCBT, Enhanced cognitive-behavioral treatment; FAS, Family Accommodation Scale; KINDL-R, Questionnaire for Measuring Health-related Quality of Life in Children and Adolescents, revised version; K-SADS PL, The schedule for Affective Disorders and Schizophrenia for School-aged Children – Present and Lifetime Version; MFQ, Mood and Feelings Questionnaire, short version; OCD, Obsessive-compulsive disorder; ODD, oppositional defiant disorder; PTSD, Post traumatic disorder; QoL, Quality of life; SCARED, Screen for Child Anxiety-Related Emotional Disorders; SDQ, Strengths and Difficulties Questionnaire; SSRIs, selective serotonin reuptake inhibitors.
Footnotes
- ^ The OCD clinical diagnoses were established based on CY-BOCS scores and ICD-10/DSM-5 criteria.
References
Angold, A., Costello, E. J., Messer, S. C., and Pickles, A. (1995). Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int. J. Methods Psychiatr. Res. 5, 251–262.
Babiano-Espinosa, L., Skarphedinsson, G., Weidle, B., Wolters, L. H., Compton, S., Ivarsson, T., et al. (2022). eCBT Versus standard individual CBT for paediatric obsessive–compulsive disorder. Child Psychiatry Hum. Dev. 54, 1567–1576.
Babiano-Espinosa, L., Wolters, L. H., Weidle, B., Compton, S. N., Lydersen, S., and Skokauskas, N. (2021). Acceptability and feasibility of enhanced cognitive behavioral therapy (eCBT) for children and adolescents with obsessive–compulsive disorder. Child Adolesc. Psychiatry Ment. Health 15:47.
Banneyer, K. N., Bonin, L., Price, K., Goodman, W. K., and Storch, E. A. (2018). Cognitive behavioral therapy for childhood anxiety disorders: A review of recent advances. Curr. Psychiatry Rep. 20:65.
Birmaher, B., Khetarpal, S., Brent, D., Cully, M., Balach, L., Kaufman, J., et al. (1997). The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. J. Am. Acad. Child Adolesc. Psychiatry36, 545–553.
Bolton, D., Williams, T., Perrin, S., Atkinson, L., Gallop, C., Waite, P., et al. (2011). Randomized controlled trial of full and brief cognitive-behaviour therapy and wait-list for paediatric obsessive-compulsive disorder. J. Child Psychol. Psychiatry 52, 1269–1278.
Bonnert, M., Ljótsson, B., Hedman, E., Andersson, J., Arnell, H., Benninga, M. A., et al. (2014). Internet-delivered cognitive behavior therapy for adolescents with functional gastrointestinal disorders—An open trial. Internet Interv. 1, 141–148.
Bullinger, M., Brütt, A. L., Erhart, M., Ravens-Sieberer, U., and Group, B. S. (2008). Psychometric properties of the KINDL-R questionnaire: Results of the BELLA study. Eur. Child Adolesc. Psychiatry 17, 125–132.
Calvocoressi, L., Mazure, C. M., Kasl, S. V., Skolnick, J., Fisk, D., Vegso, S. J., et al. (1999). Family accommodation of obsessive-compulsive symptoms: Instrument development and assessment of family behavior. J. Nerv. Ment. Dis. 187, 636–642.
Cancilliere, M. K., Freeman, J., Garcia, A., Benito, K., Sapyta, J., and Franklin, M. (2018). Assessing acute secondary treatment outcomes in early-onset obsessive–compulsive disorder. Child Psychiatry Hum. Dev. 49, 718–729.
Conelea, C. A., Selles, R. R., Benito, K. G., Walther, M. M., Machan, J. T., Garcia, A. M., et al. (2017). Secondary outcomes from the pediatric obsessive compulsive disorder treatment study II. J. Psychiatr. Res. 92, 94–100.
Douglass, H. M., Moffitt, T. E., Dar, R., McGee, R., and Silva, P. (1995). Obsessive-compulsive disorder in a birth cohort of 18-year-olds: Prevalence and predictors. J. Am. Acad. Child Adolesc. Psychiatry 34, 1424–1431.
Farrell, L. J., Oar, E. L., Waters, A. M., McConnell, H., Tiralongo, E., Garbharran, V., et al. (2016). Brief intensive CBT for pediatric OCD with E-therapy maintenance. J. Anxiety Disord. 42, 85–94.
Flament, M. F., Whitaker, A., Rapoport, J. L., Davies, M., Berg, C. Z., Kalikow, K., et al. (1988). Obsessive compulsive disorder in adolescence: An epidemiological study. J. Am. Acad. Child Adolesc. Psychiatry 27, 764–771.
Franklin, M. E., Dingfelder, H. E., Coogan, C. G., Garcia, A. M., Sapyta, J. J., and Freeman, J. L. (2013). Cognitive behavioral therapy for pediatric obsessive-compulsive disorder: Development of expert-level competence and implications for dissemination. J. Anxiety Disord. 27, 745–753.
Garcia, A. M., Sapyta, J. J., Moore, P. S., Freeman, J. B., Franklin, M. E., March, J. S., et al. (2010). Predictors and moderators of treatment outcome in the Pediatric Obsessive Compulsive Treatment Study (POTS I). J. Am. Acad. Child Adolesc. Psychiatry 49, 1024–1033.
Geller, D. A., Biederman, J., Griffin, S., Jones, J., and Lefkowitz, T. R. (1996). Comorbidity of juvenile obsessive-compulsive disorder with disruptive behavior disorders. J. Am. Acad. Child Adolesc. Psychiatry 35, 1637–1646.
Geller, D. A., Coffey, B., Faraone, S., Hagermoser, L., Zaman, N. K., Farrell, C. L., et al. (2003). Does comorbid attention-deficit/hyperactivity disorder impact the clinical expression of pediatric obsessive-compulsive disorder? CNS Spectr. 8, 259–264.
Geller, D. A., Hoog, S. L., Heiligenstein, J. H., Ricardi, R. K., Tamura, R., Kluszynski, S., et al. (2001). Fluoxetine treatment for obsessive-compulsive disorder in children and adolescents: A placebo-controlled clinical trial. J. Am. Acad. Child Adolesc. Psychiatry 40, 773–779.
Ginsburg, G. S., Kingery, J. N., Drake, K. L., and Grados, M. A. (2008). Predictors of treatment response in pediatric obsessive-compulsive disorder. J. Am. Acad. Child Adolesc. Psychiatry 47, 868–878.
Goodman, R. (1997). The strengths and difficulties questionnaire: A research note. J. Child Psychol. Psychiatry 38, 581–586.
Griffiths, J., Norris, E., Stallard, P., and Matthews, S. (2012). Living with parents with obsessive–compulsive disorder: Children’s lives and experiences. Psychol. Psychother. Theory Res. Pract. 85, 68–82.
Højgaard, D., Hybel, K. A., Ivarsson, T., Skarphedinsson, G., Becker Nissen, J., Weidle, B., et al. (2017). One-year outcome for responders of cognitive-behavioral therapy for pediatric obsessive-compulsive disorder. J. Am. Acad. Child Adolesc. Psychiatry 56, 940–947.e1.
Jensen, S., Hybel, K. A., Højgaard, D. R., Nissen, J. B., Weidle, B., Ivarsson, T., et al. (2022). Quality of life in pediatric patients with obsessive–compulsive disorder during and 3 years after stepped-care treatment. Eur. Child Adolesc. Psychiatry 31, 1377–1389.
Lack, C. W., Storch, E. A., Keeley, M. L., Geffken, G. R., Ricketts, E. D., Murphy, T. K., et al. (2009). Quality of life in children and adolescents with obsessive-compulsive disorder: Base rates, parent–child agreement, and clinical correlates. Soc. Psychiatry Psychiatr. Epidemiol. 44, 935–942.
Lenhard, F., Andersson, E., Mataix-Cols, D., Rück, C., Vigerland, S., Högström, J., et al. (2017). Therapist-guided, internet-delivered cognitive-behavioral therapy for adolescents with obsessive-compulsive disorder: A randomized controlled trial. J. Am. Acad. Child Adolesc. Psychiatry 56, 10–19.e2.
Masi, G., Millepiedi, S., Mucci, M., Bertini, N., Pfanner, C., and Arcangeli, F. (2006). Comorbidity of obsessive-compulsive disorder and attention-deficit/hyperactivity disorder in referred children and adolescents. Compr. Psychiatry 47, 42–47.
Masi, G., Perugi, G., Toni, C., Millepiedi, S., Mucci, M., Bertini, N., et al. (2004). Obsessive-compulsive bipolar comorbidity: Focus on children and adolescents. J. Affect. Disord. 78, 175–183.
McGuire, J. F., Piacentini, J., Lewin, A. B., Brennan, E. A., Murphy, T. K., and Storch, E. A. (2015). A meta-analysis of cognitive behavior therapy and medication for child obsessive–compulsive disorder: Moderators of treatment efficacy, response, and remission. Depress. Anxiety 32, 580–593.
Merlo, L. J., Lehmkuhl, H. D., Geffken, G. R., and Storch, E. A. (2009). Decreased family accommodation associated with improved therapy outcome in pediatric obsessive–compulsive disorder. J. Consult. Clin. psychol. 77:355.
National Collaborating Centre for Mental Health [NCCMH] (2006). Obsessive-compulsive disorder: Core interventions in the treatment of obsessive-compulsive disorder and body dysmorphic disorder. London: National Collaborating Centre for Mental Health.
Öst, L.-G., Riise, E. N., Wergeland, G. J., Hansen, B., and Kvale, G. (2016). Cognitive behavioral and pharmacological treatments of OCD in children: A systematic review and meta-analysis. J. Anxiety Disord. 43, 58–69.
Peris, T. S., Bergman, R. L., Langley, A., Chang, S., McCracken, J. T., and Piacentini, J. (2008). Correlates of accommodation of pediatric obsessive-compulsive disorder: Parent, child, and family characteristics. J. Am. Acad. Child Adolesc. Psychiatry 47, 1173–1181.
Peris, T.S., Rozenman, M. S., Sugar, C. A., McCracken, J. T., and Piacentini, J. (2017). Targeted family intervention for complex cases of pediatric obsessive-compulsive disorder: A randomized controlled trial. J. Am. Acad. Child Adolesc. Psychiatry 56, 1034–1042.
Piacentini, J., Bergman, R. L., Chang, S., Langley, A., Peris, T., Wood, J. J., et al. (2011). Controlled comparison of family cognitive behavioral therapy and psychoeducation/relaxation training for child obsessive-compulsive disorder. J. Am. Acad. Child Adolesc. Psychiatry 50, 1149–1161.
Piacentini, J., Peris, T. S., Bergman, R. L., Chang, S., and Jaffer, M. (2007). BRIEF REPORT: Functional impairment in childhood OCD: Development and psychometrics properties of the child obsessive-compulsive impact scale-revised (COIS-R). J. Clin. Child Adolesc. Psychol. 36, 645–653.
Ravens-Sieberer, U., Erhart, M., Wille, N., Bullinger, M., and Group, B. S. (2008). Health-related quality of life in children and adolescents in Germany: Results of the BELLA study. Eur. Child Adolesc. Psychiatry 17, 148–156.
Sánchez-Meca, J., Rosa-Alcázar, A. I., Iniesta-Sepúlveda, M., and Rosa-Alcázar, Á (2014). Differential efficacy of cognitive-behavioral therapy and pharmacological treatments for pediatric obsessive–compulsive disorder: A meta-analysis. J. Anxiety Disord. 28, 31–44.
Sharma, E., Sharma, L., Balachander, S., Lin, B., Manohar, H., Khanna, P., et al. (2021). Comorbidities in obsessive-compulsive disorder across the lifespan: A systematic review and meta-analysis. Front. Psychiatry 12:703701. doi: 10.3389/fpsyt.2021.703701
Skarphedinsson, G., Hanssen-Bauer, K., Kornør, H., Heiervang, E. R., Landrø, N. I., Axelsdottir, B., et al. (2015). Standard individual cognitive behaviour therapy for paediatric obsessive–compulsive disorder: A systematic review of effect estimates across comparisons. Nordic J. Psychiatry 69, 81–92.
Skarphedinsson, G., Torp, N. C., Weidle, B., Jensen, S., Ivarsson, T., Hybel, K. A., et al. (2023). Family accommodation in pediatric obsessive-compulsive disorder: Investigating prevalence and clinical correlates in the NordLOTS study. Child Psychiatry Hum. Dev. [Epub ahead of print].
Stewart, S., Geller, D., Jenike, M., Pauls, D., Shaw, D., Mullin, B., et al. (2004). Long-term outcome of pediatric obsessive–compulsive disorder: A meta-analysis and qualitative review of the literature. Acta Psychiatr. Scand. 110, 4–13.
Storch, E. A., Caporino, N. E., Morgan, J. R., Lewin, A. B., Rojas, A., Brauer, L., et al. (2011). Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Res. 189, 407–412.
Storch, E. A., Small, B. J., McGuire, J. F., Murphy, T. K., Wilhelm, S., and Geller, D. A. (2018). Quality of life in children and youth with obsessive-compulsive disorder. J. Child Adolesc. Psychopharmacol. 28, 104–110.
Sucupira, E., Sabino, M., Lima, E. L., Dini, G. M., Brito, M. J., and Ferreira, L. M. (2017). Short mood and feelings questionnaire for screening children and adolescents for plastic surgery: Cross-cultural validation study. Sao Paulo Med. J. 135, 518–528.
Sukhodolsky, D. G., do Rosario-Campos, M. C., Scahill, L., Katsovich, L., Pauls, D. L., Peterson, B. S., et al. (2005). Adaptive, emotional, and family functioning of children with obsessive-compulsive disorder and comorbid attention deficit hyperactivity disorder. Am. J. Psychiatry 162, 1125–1132.
Termine, C., Balottin, U., Rossi, G., Maisano, F., Salini, S., Di Nardo, R., et al. (2006). Psychopathology in children and adolescents with Tourette’s syndrome: A controlled study. Brain Dev. 28, 69–75.
Thompson-Hollands, J., Abramovitch, A., Tompson, M. C., and Barlow, D. H. (2015). A randomized clinical trial of a brief family intervention to reduce accommodation in obsessive-compulsive disorder: A preliminary study. Behav. Ther. 46, 218–229.
Torp, N. C., Dahl, K., Skarphedinsson, G., Compton, S., Thomsen, P. H., Weidle, B., et al. (2015a). Predictors associated with improved cognitive-behavioral therapy outcome in pediatric obsessive-compulsive disorder. J. Am. Acad. Child Adolesc. Psychiatry 54, 200–207.e1.
Torp, N. C., Dahl, K., Skarphedinsson, G., Thomsen, P. H., Valderhaug, R., Weidle, B., et al. (2015b). Effectiveness of cognitive behavior treatment for pediatric obsessive-compulsive disorder: Acute outcomes from the Nordic Long-term OCD Treatment Study (NordLOTS). Behav. Res. Ther64, 15–23.
Valleni-Basile, L. A., Garrison, C. Z., Jackson, K. L., Waller, J. L., McKEOWN, R. E., Addy, C. L., et al. (1994). Frequency of obsessive-compulsive disorder in a community sample of young adolescents. J. Am. Acad. Child Adolesc. Psychiatry 33, 782–791.
Van Roy, B., Veenstra, M., and Clench-Aas, J. (2008). Construct validity of the five-factor Strengths and Difficulties Questionnaire (SDQ) in pre-, early, and late adolescence. J. Child Psychol. Psychiatry 49, 1304–1312.
Weidle, B. (2015). Children and Adolescents with Obsessive-Compulsive Disorder: Comorbidity and Quality of Life. Ph. D Thesis. Trondheim: Norwegian University of Science and Technology.
Weidle, B., Ivarsson, T., Thomsen, P. H., Lydersen, S., and Jozefiak, T. (2015). Quality of life in children with OCD before and after treatment. Eur. Child Adolesc. Psychiatry 24, 1061–1074.
Weidle, B., Jozefiak, T., Ivarsson, T., and Thomsen, P. H. (2014). Quality of life in children with OCD with and without comorbidity. Health Qual. Life Outcomes 12:152.
Wolters, L. H., Weidle, B., Babiano-Espinosa, L., and Skokauskas, N. (2020). Feasibility, acceptability, and effectiveness of enhanced cognitive behavioral therapy (eCBT) for children and adolescents with obsessive-compulsive disorder: Protocol for an open trial and therapeutic intervention. JMIR Res. Protocols 9: e24057.
Zaboski, B. A., Gilbert, A., Hamblin, R., Andrews, J., Ramos, A., Nadeau, J. M., et al. (2019). Quality of life in children and adolescents with obsessive-compulsive disorder: The Pediatric Quality of Life Enjoyment and Satisfaction Questionnaire (PQ-LES-Q). Bull. Menninger Clin. 83, 377–397.
Keywords: cognitive-behavioral therapy (CBT), enhanced cognitive behavioral therapy (eCBT), obsessive-compulsive disorder (OCD), pediatric, children, adolescents, secondary outcomes
Citation: Wang B, Skarphedinsson G, Weidle B, Babiano-Espinosa L, Wolters L, Arntzen J and Skokauskas N (2024) Secondary outcomes of enhanced cognitive behavioral therapy (eCBT) for children and adolescents with obsessive-compulsive disorder. Front. Hum. Neurosci. 17:1330435. doi: 10.3389/fnhum.2023.1330435
Received: 30 October 2023; Accepted: 15 December 2023;
Published: 08 January 2024.
Edited by:
Leonardo F. Fontenelle, D’Or Institute for Research and Education (IDOR), BrazilReviewed by:
Maria Eduarda Moreira-de-Oliveira, Federal University of Rio de Janeiro, BrazilShyam Sundar Arumugham, National Institute of Mental Health and Neurosciences (NIMHANS), India
Copyright © 2024 Wang, Skarphedinsson, Weidle, Babiano-Espinosa, Wolters, Arntzen and Skokauskas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Norbert Skokauskas, norbert.skokauskas@ntnu.no
 Bo Wang
Bo Wang Gudmundur Skarphedinsson
Gudmundur Skarphedinsson Bernhard Weidle3,4
Bernhard Weidle3,4  Norbert Skokauskas
Norbert Skokauskas