- 1Department of Hand & Reconstructive Surgery, Center for Plastic & Reconstructive Surgery, Zhejiang Provincial People’s Hospital, Affiliated People’s Hospital, Hangzhou Medical College, Hangzhou, Zhejiang, China
- 2Department of Plastic and Aesthetic Center, First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, Zhejiang, China
- 3Department of Plastic Surgery, First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, Zhejiang, China
- 4Department of Orthopaedics, First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, Zhejiang, China
- 5Department of Gastrointestinal Surgery, The Second Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou, China
Although non-invasive and minimally invasive aesthetic procedures increasingly dominate the cosmetic market, traditional plastic surgery remains the most effective improvement method. One of the most common complications in plastic surgery, peripheral nerve injuries, though has a low incidence but intrigued plastic surgeons globally. In this article, a narrative review was conducted using several databases (PubMed, EMBASE, Scopus, and Web of Science) to identify peripheral nerve injuries following cosmetic surgeries such as blepharoplasty, rhinoplasty, rhytidectomy, breast surgeries, and abdominoplasty. Surgery-related nerve injuries were discussed, respectively. Despite the low incidence, cosmetic plastic surgeries can cause iatrogenic peripheral nerve injuries that require special attention. The postoperative algorithm approaches can be effective, but the waiting and treatment processes can be long and painful. Preventive measures are undoubtedly more effective than postoperative remedies. The best means of preventing disease is having a good understanding of anatomy and conducting a careful dissection.
Introduction
Plastic surgeons are cognizant that non-invasive and minimally invasive aesthetic procedures with limited complications and downtime are gradually capturing a significant share of the market (1). Traditional cosmetic plastic surgeries are still indispensable due to their high effectiveness (2). Despite the low occurrence, peripheral nerve injuries are one of the common complications that can be a complex problem with various causes (3, 4). Besides causing patients significant anxiety, they also frustrate practitioners. Chronic pain, hyperesthesia, hypoesthesia, and numbness are common symptoms of peripheral nerve injury that must be considered seriously to distinguish them from infectious, neoplastic, and wound-related causes that can be prevented with antibiotics and proper tissue handling (5, 6).
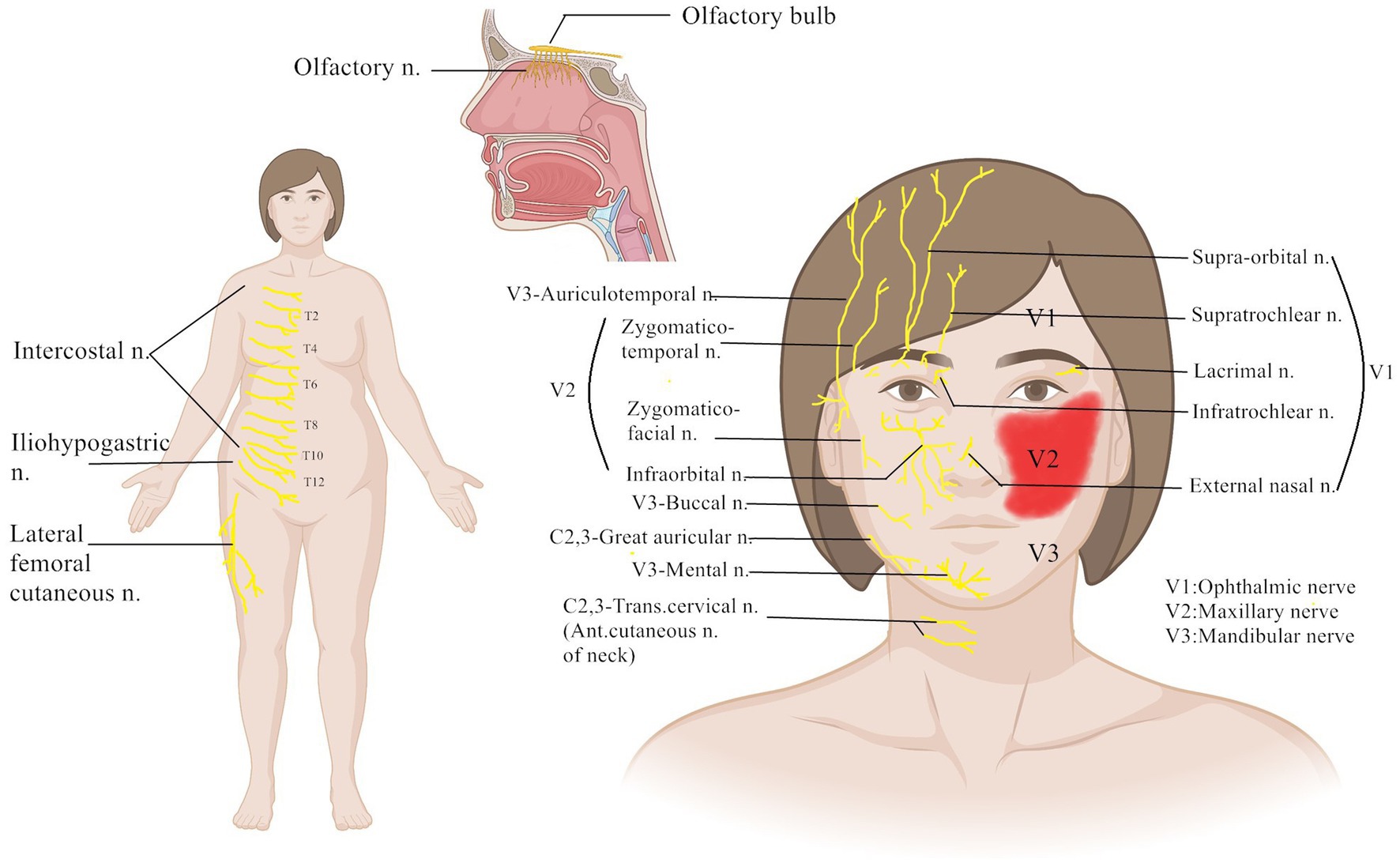
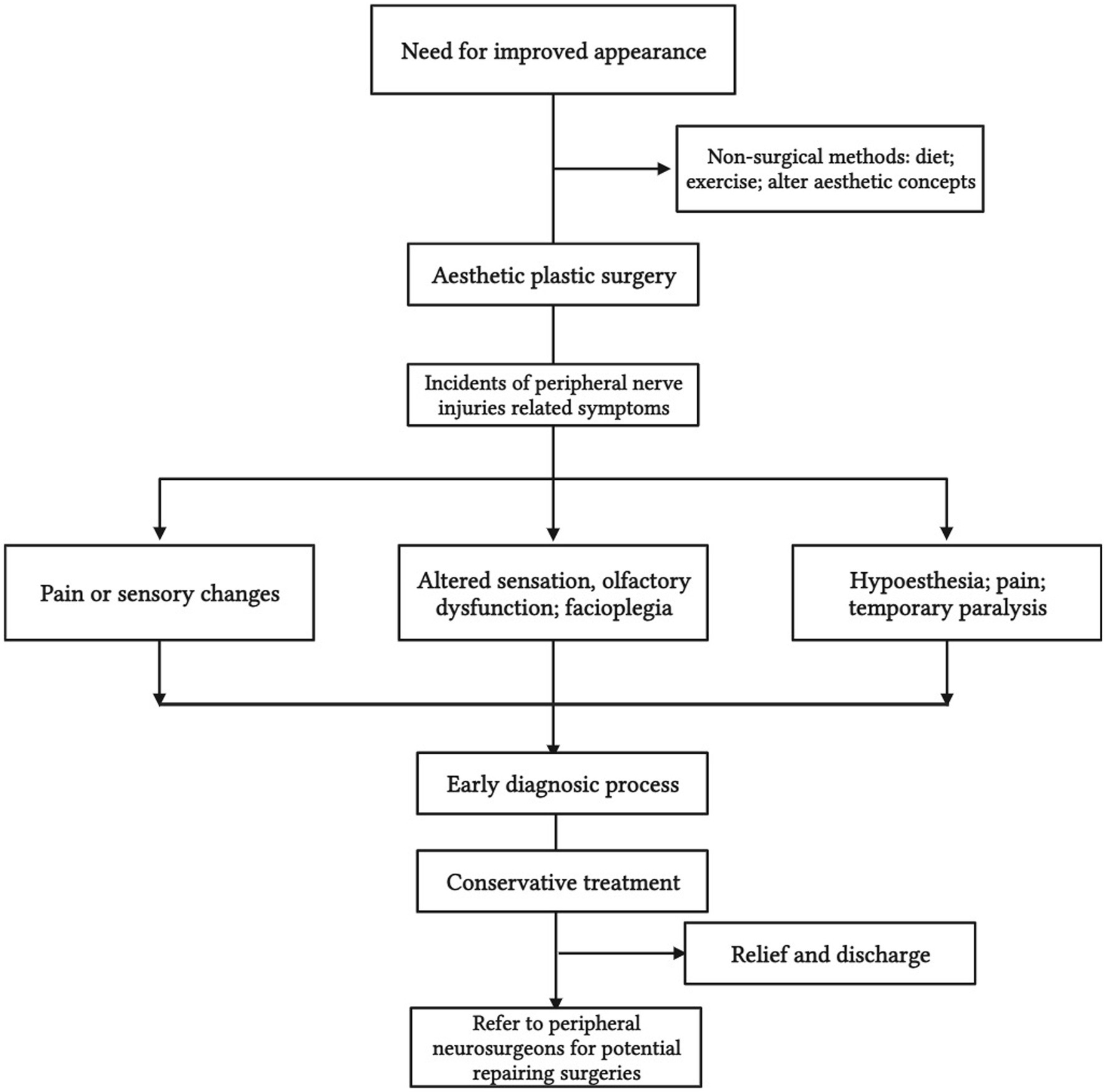
The purpose of this article was to comprehensively review the literature on peripheral nerve injuries associated with cosmetic surgery (as shown in Figure 1). The specific nerve injuries that occur following cosmetic surgery, such as faciocervical, breast, and abdominal procedures, will be discussed, respectively. Injuries of this type are also subject to potential treatments.
Methods
Literature search strategy
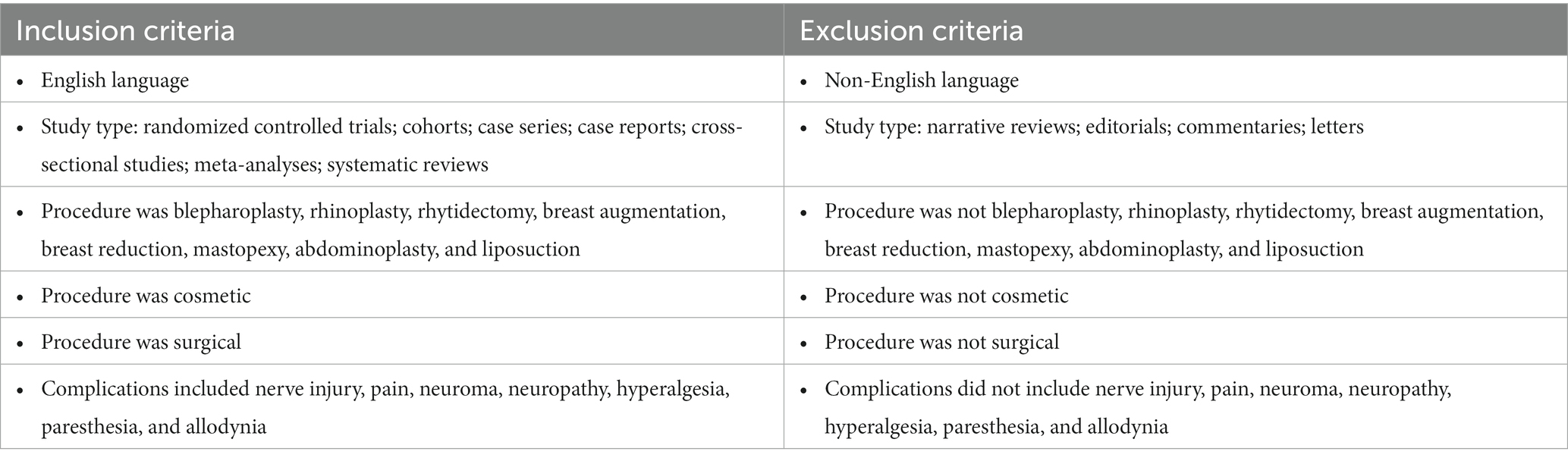
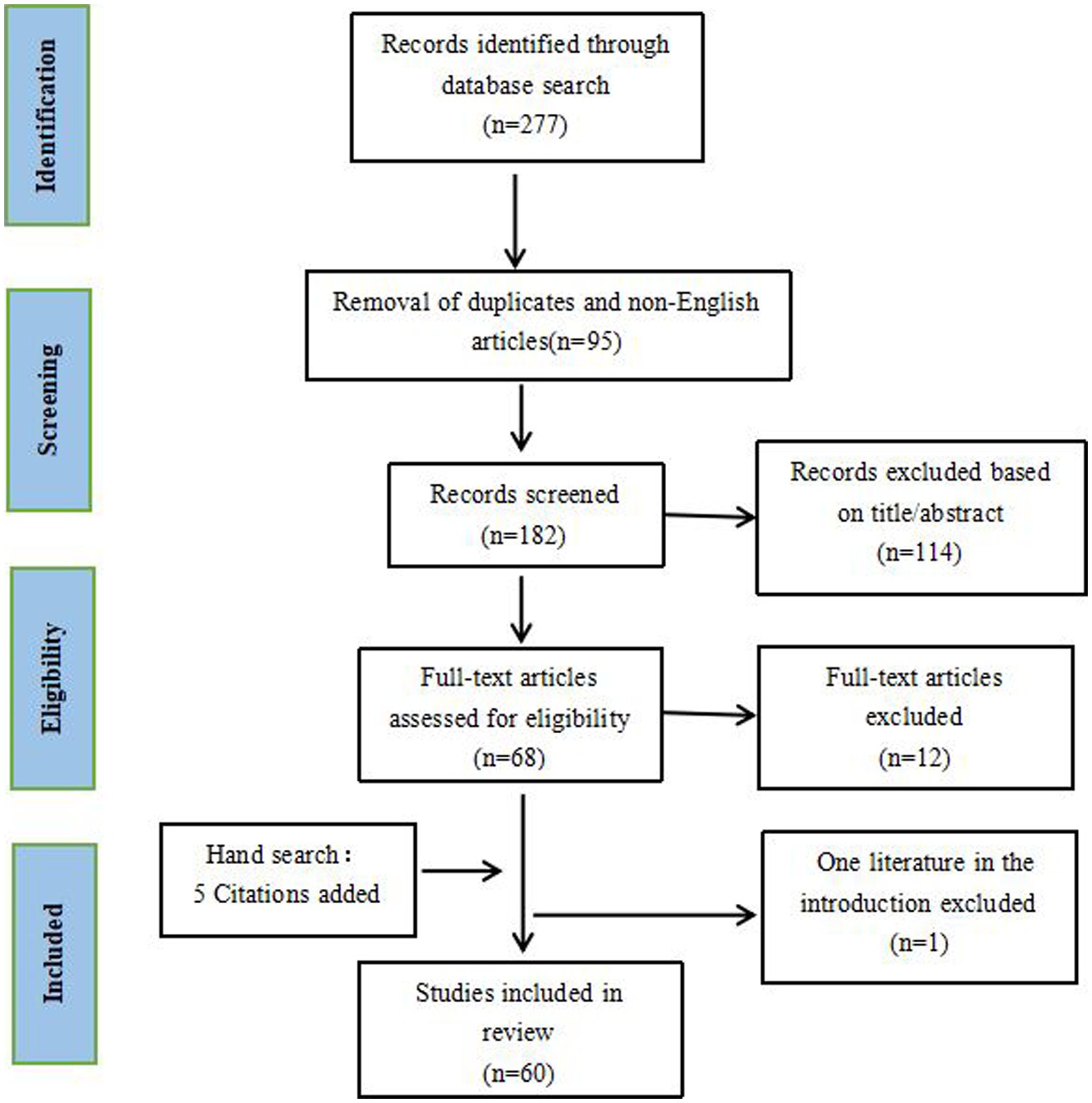
A literature search was performed in October 2022 using the PubMed, EMBASE, Scopus and Web of Science databases. Search strategies included blepharoplasty, rhinoplasty, rhytidectomy, breast augmentation, breast reduction, mastopexy, abdominoplasty, and liposuction, combined with key subject terms: nerve injury, pain, neuroma, neuropathy, hyperalgesia, paresthesia, and allodynia. Literature was restricted to aesthetic surgeries, ranged from January 1950 to October 2022, and all articles except narrative reviews, editorials, commentaries, and letters were considered. Additional studies were included by reviewing the reference lists of included literature and referencing relevant articles based on search results. Inclusion and exclusion criteria were established before conducting the search, as shown in Table 1. A total of 277 citations were initially identified, 95 of which were eliminated as duplicates or non-English. After evaluating the titles and abstracts according to the inclusion and exclusion criteria (Table 1), 114 articles were excluded as irrelevant studies. Literature screening and evaluation were independently done. Discrepancies were resolved by the two authors through discussion. Hand searching added 5 articles that met our criteria. Furthermore, 12 studies were excluded because the full text was unavailable. Ultimately, a total of 60 studies published between January 1976 and October 2022 were finally included in this review (Figure 2). The quality of the included studies was screened through assessing using the American Society of Plastic Surgeons, Scales for Rating Levels of Evidence (7). The search and screening were done independently by QC, PL, and QZ, and the discrepancies were resolved by communication and discussion.
Results
Blepharoplasty
Blepharoplasty is currently the most popular aesthetic procedure, which improves the appearance of one’s upper eyelids, lower eyelids, or both (8, 9). However, upper blepharoplasty can cause injury to the supraorbital nerve or supratrochlear nerve, while lower blepharoplasty may damage the infraorbital nerve (3). It was reported in several papers that the combination of an infra-brow and a supra-brow resulted in 1.8% (8/432) (10), and 0.8% (5/564) (11) incidence of transient forehead numbness, which gradually subsides within six months with no documented facial nerve injuries. Booth et al. (12) demonstrated the incidence of altered forehead sensation was 74% (32/43 brows), while Lee et al. (13) encountered no such case (14, 15). Turin et al. (16) reported two cases of temporary nerve palsy of the frontal branch of the facial nerve, which resolved completely without permanent nerve damage (150 cases). It is noteworthy that multiple studies (13, 14, 17) have demonstrated the need for careful surgical skills at the supraorbital nerve notch(SON) and glabellar area to avoid damaging the supratrochlear and supraorbital nerves. According to one study (18), the deep branch of the supraorbital nerve traverses the periosteum. It passes between the periosteum and the pericranium towards the top of the head, providing sensation to the frontoparietal scalp. Researchers (11) demonstrated that damage to the supraorbital nerve’s deep branch causes most distress, paresthesia, and numbness following brow lifts, while the superficial branch is more likely to be injured because it penetrates the frontalis muscle to provide sensation to the forehead and anterior region of the scalp. During dissection and fixation, care must be taken to prevent damage to the superficial branch.
Lower eyelid blepharoplasty has a complex anatomy that can lead to injury to the infraorbital nerve (19). In a previous study (20), six patients developed numbness (injury to the infraorbital nerve) following 34 lower eyelid blepharoplasties (17.65%). Five of them recovered within three months; the other recovered within six months after surgery. In another retrospective study (21), 184 consecutive patients received transconjunctival orbital fat grafts without any numbness or nerve injury noted. The levator labii superioris muscle, which overlies the infraorbital nerve, remains intact during surgery as a floor of the premaxillary space (22), so there should be no damage to the nerve. Consequently, to reduce the incidence of injury to the infraorbital nerve (21, 23), the authors suggested that the surrounding soft tissues should be dissected along the sides above the anterior periosteum near the infraorbital anterior portal. To reveal the inferior margin of the orbit, the soft tissues should be pulled away with a cold light retractor.
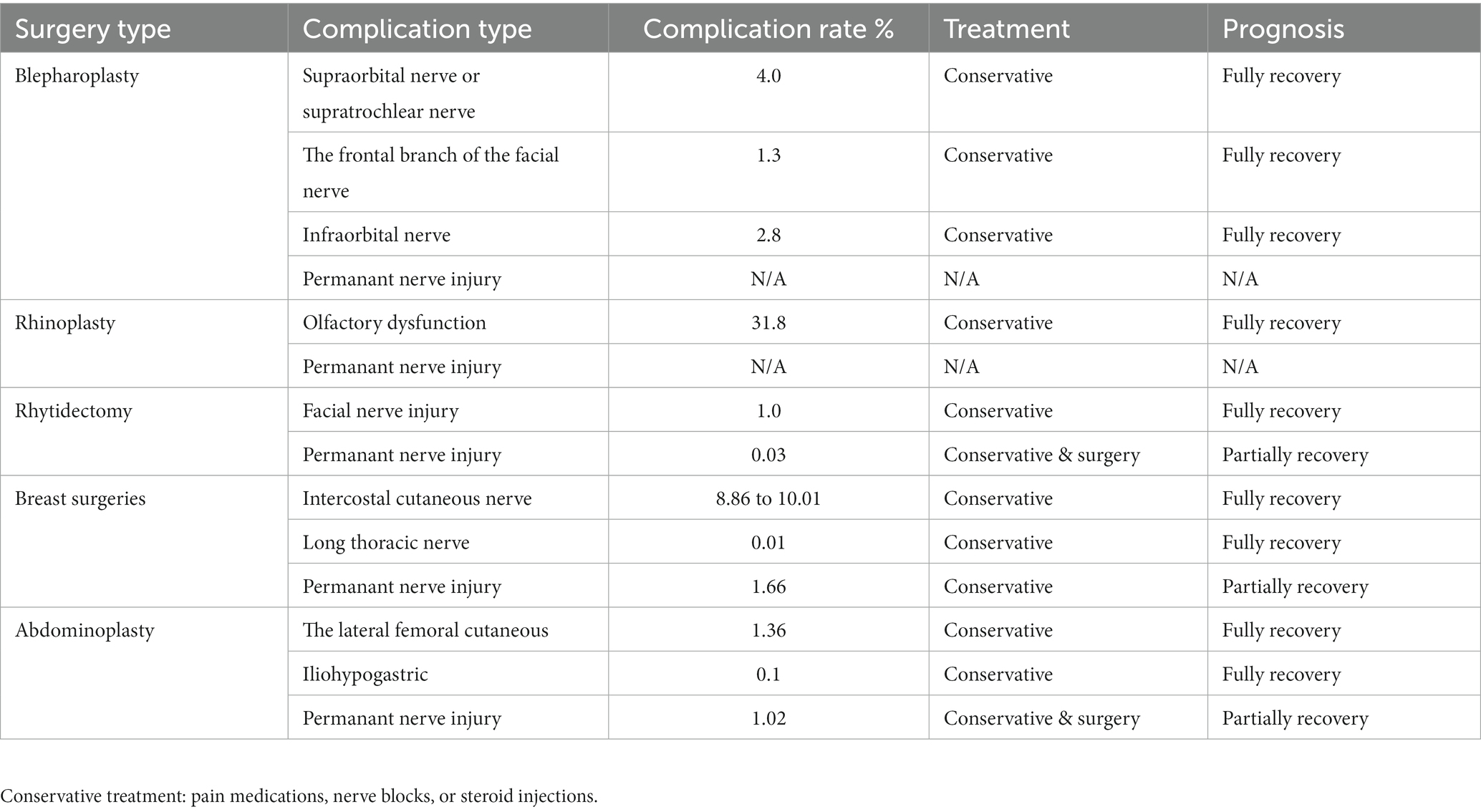
In the literature cited above, it has been reported that the transient injury incidence of the supraorbital nerve or supratrochlear nerve injury was, on average, 4.0% (45/1119), whereas the frontal branch of the facial nerve was 1.3% (2/150), and the infraorbital nerve was 2.8% (6/218), and no permanent nerve injury has been reported. Therefore, in blepharoplasty, the most frequently injured nerve was the supraorbital nerve or supratrochlear nerve injury.
Rhinoplasty
Cosmetic rhinoplasty is a popular cosmetic procedure performed globally that encompasses several procedures (24), including alteration of the nasal dorsum, the radix, the nasal tip, and the nasal base, septoplasty, and premaxillary augmentation. Various grafts and allografts are available for cosmetic rhinoplasty, including cartilage, bone, expanded polytetrafluoroethylene, silicone, porous polyethylene, and calcium hydroxyapatite (25). Patients may experience some degree of postoperative olfactory dysfunction following nasal surgery (26). Therefore, any type of nasal surgery, including cosmetic rhinoplasty, may deteriorate olfactory function (27, 28), even without directly damaging the nasal mucosa or the olfactory nerve (29). It should be noted that patients who undertake rhinoplasty need to participate in the Smell Identification Test to evaluate their olfactory function (30–32). Anosmia is an olfactory deficiency diagnosed using the SIT score < 20. Normosmia was referred to as having a SIT score > 35. Hyposmia is termed a composite test score of 20–35.
Furthermore, Shemshadi et al. (33) demonstrated that some degrees of olfactory dysfunction could occur following rhinoplasty, 87.5% (57/65) at postoperative week one. As a result of several studies investigating the effect of open aesthetic rhinoplasty on olfaction, 10 patients (29.5%) (26), 8 patients (10.8%) (34), and 7 patients (10.2%) (35) developed olfaction dysfunction. In particular, Brinner et al. (36) reported that 24% of normal patients (a total of 184 subjects) believed they had impaired sense of smell due to surgery. Conversely, some patients already had an impaired sense of smell before surgery without being unaware of it (36).
The olfactory bulb is mostly vulnerable to damage in the cosmetic rhinoplasty (33, 35, 36). Studies above reported an average incidence of postoperative olfactory dysfunction of 31.8% (26, 27, 33, 34). The patients mostly recovered their baseline olfactory function within six weeks to six months despite initially reducing their function (33, 34, 36).
Rhytidectomy
A rhytidectomy or facelift consists of a forehead lift, a mid-face lift, and a lower facelift, and most patients undergo two or three procedures. Mitz and Peyronie’s description of the superficial musculoaponeurotic system (SMAS) (37) led to a new epoch in rhytidectomy. Injuries to the facial nerve are among the most severe complications of rhytidectomy. A retrospective study conducted by Baker et al. (38) demonstrated that in a summary of 7,068 cases, the incidence of facial nerve injury was reported to be 0.7% (range 0.4% to 2.6%), and the incidence of permanent injury was 0.1%.
In a recent meta-analysis of the incidence of complications with different facial slimming techniques (39), the permanent injury rate of the facial nerve was reported from 0% to 0.08% for all types of SMAS manipulation techniques. Furthermore, they found that temporary facial nerve injury was reported in SMASectomy/imbrication (0.84%, n = 3,454), SMAS flap (0.79%, n = 17,247), SMAS plication (0.69%, n = 5,081), deep plane (0.69%, n = 1,597), and composite (1.52%, n = 858), and high lateral SMAS (1.85%, n = 1,300). Permanent facial nerve damage occurred in the high lateral SMAS (0.08%, n = 1,300) and the SMAS flap (0.04%, n = 14,253), and no perpetual facial nerve injuries were covered for the deep plane (n = 1795), SMAS plication (n = 5,638), SMAS imbrication (n = 3,254), and composite (n = 727).
Researchers (40) found a provisional facial nerve injury rate of 7.1% (primary surgery) and 2.2% (secondary surgery), with both primary and secondary facelifts using lamellar SMAS techniques (41).
Multiple studies (40–42) have explained the reasons for facial nerve injury, including suture placement, transection, electrocauterization, excessive traction and stretching, crushing injuries caused by surgical instruments, distorted anatomy, and adhesion from a previous procedure. In some studies (43, 44), researchers have suggested that facial nerve function generally recovers three to six months after an injury due to multiple interconnections and intermingling of the facial nerve branches (45).
Anatomical studies (41, 44, 46, 47) have further confirmed that the frontal branches are separate from the SMAS and contained within a distinct layer.
Therefore, according to the studies mentioned above, the incidence of facial nerve injury is nearly 1.0% (temporary) and 0.03% (permanent). The marginal mandibular branch and the cervical branch are most vulnerable to be injured. It is also beneficial to have a good understanding of the location of facial nerve branches, the retaining ligaments, and the soft-tissue plane of the face to decrease the incidence of facial nerve injury.
Breast surgeries
Aesthetic breast surgeries usually include augmentation, mastopexy, and reduction mammaplasties, with breast augmentation being the most frequently performed procedure (48). As part of a retrospective study by Broyles et al., all cases of augmentation, mastopexy, and reduction who complained of postoperative chronic pain failed to respond to physical or drug therapy (49). Surgical repair was then projected. Anesthesia blockade of suspected injured nerves was found to be effective prior to surgery. One or more intercostal nerves were found to be injured and resected and implanted into adjacent muscles. Except for the patient who underwent augmentation, both mastopexy and reduction patients responded well to therapy (49).
Brown et al. conducted a prospective study to examine objective sensory changes using a Semmes Weinstein monofilament following subfascial breast augmentation (50). According to the study, the greater the initial breast volume, the greater the sensory loss at 12 weeks in the nipple-areolar complexes. The calculated ratio was 102% to 4%. Helmy et al.’s study examined nipple-areolar complex sensitivity changes, showing a low incidence, which rebounded one year later to 1.66% (51). A peri-areolar approach tends to have fewer sensation changes.
Another retrospective study conducted by Ducic et al. (5, 52) demonstrated that 74% of the patients that presented with pain in the surgical scar had concomitant injuries of intercostal nerves (2nd to 7th) due to mechanical trauma of sharp dissection or compressive scar entrapment. As a result of blunt tissue dissection, 7% suffered from traction-stretch neuropathy. Furthermore, the lateral zone could be the most damaged area (79%). Specifically, augmentations through peri-areolar incisions tended to injure intercostal nerves (3rd to 4th) in the central zone, whereas the inframammary approach mostly affected intercostal nerves (5th to 6th) in the inferior zone, and for transaxillary incisions, the second intercostal nerve in the lateral zone was the most injured. Intercostal nerves (3rd to 5th) in the central, inferior, and lateral zones were involved in breast reduction, and intercostal nerves (3rd to 4th), usually in the central zone, were affected by mastopexy. Their recommendations included physical therapy, avoiding compressive garments, and corresponding oral medications in the initial stages of injured nerve symptoms. If the symptoms persist beyond three to six months, surgical treatment with selective neuroma excision and proximal end implantation is advised. The effectiveness of the recommended treatment has not been systematically tested.
During cosmetic breast surgeries, the intercostal cutaneous nerves are most vulnerable to damage (8.86% to 10.01%). It is estimated that 13.57% of total injuries and 1.66% of permanent injuries occur on average during cosmetic breast surgeries (5, 51). It is interesting to note that the injury not only results from sharp or blunt dissection but is also determined by the volume of prosthesis implanted in augmentation mammaplasties.
Abdominoplasty
Aesthetic abdominoplasty is a cosmetic surgery that removes excess skin and fat, tightening the muscles and fascia to make the abdomen thinner and firmer (53, 54). A retrospective study by Chatel et al. evaluated persistent postsurgical pain in 67 patients who underwent abdominoplasty using a visual analog pain scale (VAS) with the Douleur Neuropathique 4 (DN4) questionnaire (55), of these patients, 19.4% (13) reported neuropathic pain accompanied by hypoesthesia or hyperesthesia. The identified risk factors were acute postoperative pain, history of bariatric surgery, prolonged hospitalization, depressive status, substantial stress, and significant postoperative complications. Though specific nerve injuries were not discussed, the authors emphasized the importance of preemptive approaches and early postoperative diagnosis.
Another retrospective study done by Uchelen et al. (56) reviewed 86 patients who had underwent abdominoplasty found that 9 patients (10.5%) were documented with nerve injuries. Among which, 8 patients (9.3%) experienced sensibility disorder of the thigh. Special attention to preserve the lateral cutaneous nerves of the thigh was emphasized by the authors.
Pechter et al. described a case of right femoral nerve damage that manifested as the patient being unable to extend her right knee immediately following the performance of abdominoplasty. Her right patellar reflex and sensibility in the anteromedial thigh and medial leg were diminished (57). Two days after surgery, the patient was subjectively better and fully recovered without any surgical complications or neurologic deficits. Considering her rapid recovery, it is likely that she suffered a mild neuropraxic injury or a possible side effect of local anesthetic. Another case reported by Ege et al. (58), who underwent abdominoplasty 3 weeks ago, sustained the anterior abdominal skin burnt resulted from sensory loss. The case reminded us the importance to inform our patients of possible skin injury due to the loss of sensation.
An anatomical study by Chowdhry et al. conducted a surgical recommendation to prevent lateral femoral cutaneous nerve injury in abdominoplasty (59). Based on their dissection of 23 fresh cadaver abdomens, careful dissection in about 4 cm anterior superior iliac spine and preservation of the scarpa fascia near the inguinal ligament can provide a safe strategy to avoid lateral femoral cutaneous nerve injury in abdominoplasty.
According to a review by Ducic et al., specific nerve injury rates were 1.94%, and permanent injury rates were 1.02% after abdominoplasty (6). Among all the patients, the rates of hypoesthesia, chronic pain, and temporary weakness or paralysis were 7.67%, 1.07%, and 0.44%, respectively. The nerves directly injured were the lateral femoral cutaneous nerves (1.36%) and iliohypogastric nerves (0.10%) (60–62). The authors recommended a timely, multidisciplinary treatment to optimize symptoms related to nerve injury, including a rigorous diagnostic examination followed by initial conservative treatment. Medication treatment with painkillers, nerve blocks, or steroid injections are also recommended in the short term. A peripheral nerve surgeon should be consulted if the symptoms persist for over three months.
Based on the studies, the most injured nerve in cosmetic abdominoplasty is the lateral femoral cutaneous nerve. A permanent nerve injury occurs in 1.02% of cases. In abdominoplasty, nerve injuries may be reduced by carefully handling the anterior superior iliac spine and area near the inguinal ligament.
Discussion
Although cosmetic surgery is on the rise, plastic procedures remain the most impregnable in comparison with burgeoning non-invasive or minimally invasive procedures due to their radical improvements. However, radical changes caused by these invasive operations are the source of iatrogenic complications (63). Although peripheral nerve injuries are rare, they continue to be a serious concern for affected patients and plastic surgeons. Thus, all plastic surgeons should be familiar with the vulnerable nerves for specific surgeries, respectively, to reduce the possible damage as much as possible. This review, though not complete, lists the vulnerable nerves and their symptoms following commonly performed plastic surgeries. The complication was discussed in relation to preventing, diagnosing, and treating it to provide some information for plastic surgeons (Table 2). Raising concerns in a timely manner is essential.
Treatment algorithm
There are several challenges associated with nerve injuries, both in terms of diagnosis and therapy. Based on the opinions of the authors of included studies, we developed a recommended treatment algorithm to assist fellow surgeons with various problems (Figure 3).
Before surgeries, patients should be informed of the potential symptoms of nerve injuries, including chronic pain, hyperesthesia, hypoesthesia, and possible numbness. Mastering the related anatomy and careful dissection are necessary for a better outcome at surgery. Prevention is better than treating injuries after they have occurred.
Although some pain and paresthesia are expected to be normal in the early postoperative period, symptoms over three months can indicate nerve injuries. Early diagnosis and treatment are crucial (64) because postponed or improper treatment can result in irreversible consequences or even additional morbidities (65, 66). In addition to a comprehensive physical examination, common complications such as infection, seroma, hematoma, or fluid collection, together with other probable causes, for example, hernia, endometriosis, or abdominal visceral diseases, should be excluded. A Tinel’s sign or relief of tenderness after the targeted injection of anesthetic nerve blocks proximal to the focal point is a strong indication of nerve injury (3). Providing the diagnosis to patients validates the cause of their symptoms and reduces their emotional stress (67).
Initially, conservative modalities, such as scar massage, desensitization, and sensory reeducation, are advised for symptoms associated with some nerve injuries that can self-resolve over time. Furthermore, medication treatment that includes pain relievers, tricyclic antidepressants, anticonvulsants, steroid injections, or nerve blocks may also be helpful (6). Besides, standardized diet, nutrition, and supplementation recommendations and protocols may be of great importance for better nerve regeneration and functional recovery (68). If no improvement is seen over the first three months, referring to a peripheral nerve surgeon for possible surgical treatment, which involves exploring the suspected injured nerves with corresponding management, such as neurolysis, neurectomy, and implantation, is necessary (69, 70). This algorithmic approach generally eliminates most symptoms, but prevention remains the best treatment.
Limitations and future
While this narrative review has provided insights into peripheral nerve injuries following cosmetic surgeries, there are several limitations to consider: 1. Limited Sample Size: the rarity of peripheral nerve injuries in the context of cosmetic surgeries makes it challenging to gather a large sample size for systematic analysis. 2. Potential Bias: the existing literature on peripheral nerve injuries may exhibit a bias towards highlighting severe or exceptional cases. Moreover, it appears that the majority of documented peripheral nerve injuries have a sensory component. This bias could be attributed to the influence of personal emotions, potentially impacting the objectivity of the reported results. 3. Heterogeneity of Data: the studies included in this review vary in terms of study design, patient demographics, surgical techniques, and follow-up periods. This heterogeneity can make it difficult to draw uniform conclusions and may introduce confounding variables. 4. Lack of Long-term Follow-up: many of the studies reviewed primarily focus on the immediate postoperative period and short-term outcomes. Long-term follow-up data on the persistence of nerve injuries and their impact on patients’ quality of life are often lacking. 5. Variable Reporting Standards: the reporting of peripheral nerve injuries across different studies may lack uniformity, making it challenging to compare and compile data accurately.
To address these limitations and further advance our understanding of peripheral nerve injuries following cosmetic surgeries, future research should consider the following aspects: 1. Prospective Studies: conducting large-scale, multicenter prospective studies specifically focused on peripheral nerve injuries in cosmetic surgeries would provide more robust data and reduce selection bias. 2. Standardized Reporting: the development of standardized criteria for reporting peripheral nerve injuries and their outcomes is essential. This would facilitate better comparisons between studies and enhance the accuracy of meta-analyses. 3. Long-term Follow-up: longitudinal studies with extended follow-up periods are necessary to assess the long-term consequences of peripheral nerve injuries and the effectiveness of various treatment modalities on patients’ quality of life. 4. Advancements in Preventative Techniques: research should continue to explore innovative techniques and technologies aimed at reducing the occurrence of iatrogenic peripheral nerve injuries during cosmetic surgeries. This may include the use of advanced imaging, surgical tools, and training methodologies. 5. Patient Education: emphasizing patient education about the potential risks and complications associated with cosmetic surgeries, including peripheral nerve injuries, can help patients recognize early symptoms and contribute to better prognosis. 6. Collaboration: collaboration between plastic surgeons, neurologists, and other medical specialties can lead to a more comprehensive understanding of peripheral nerve injuries, improved prevention strategies, and better treatment options.
In the realm of cosmetic surgeries, it is paramount that we emphasize the utmost care and precision to safeguard against possible nerve injuries. To minimize the risk of such injuries, practitioners should carefully assess the patient’s anatomy, taking into consideration any potential variations or anomalies. During surgery, gentle tissue handling and a thorough understanding of the nerves’ pathways are important to avoid inadvertent damage. Adequate lighting, magnification, and proper instruments can aid in preventing unintended injuries. Vigilance and meticulous attention to detail are essential. Moreover, post-operative monitoring and communication with patients are equally crucial to promptly identify and address any signs of nerve impairment. By adhering to these principles and prioritizing nerve preservation, we can improve the overall safety of cosmetic surgical procedures.
Conclusion
Peripheral nerve injuries are rare but deserves special attention. Albeit the postoperative algorithm approaches prove effective, the waiting and treating processes can be lengthy and painful. Preventive measures are always preferable to postoperative remedies. Good mastery of surgical anatomy and meticulous dissection are the best weapons of prevention.
Author contributions
QC: Conceptualization, Formal analysis, Methodology, Funding acquisition, Software, Writing - original draft. PL: Data curation, Formal analysis, Investigation, Methodology, Writing - original draft, review & editing. QZ: Project administration, Resources, Visualization, Writing - original draft. TT: Methodology, Supervision, Validation, Writing – review & editing. HL: Conceptualization, Formal analysis, Funding acquisition, Supervision, Writing – review & editing. WZ: Formal analysis, Funding acquisition, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study received funding from the National Natural Science Foundation of China (grant number 81702135), Zhejiang Provincial Natural Science Foundation (grant numbers LY20H060007 and LS21H060001), Alibaba Youth Studio Project (grant number ZJU-032), Zhejiang Provincial Continuing Education Program (grant number 2022-04-07-001), and the Key projects by the province of Zhejiang Medical and Health Science and Technology Project (WKJ-ZJ-2101).
Acknowledgments
First, I’d like to show my sincere gratitude to my colleagues who provided me with invaluable help and support in carrying out the study. Also, I really appreciate all the funding programs for sponsoring our research. Last but not least, I want to thank all my families and friends, especially my mother who backed me all the way to where I am.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
SON, supraorbital nerve notch; SIT, smell identification test; SMAS, superficial musculoaponeurotic system; VAS, visual analog pain scale; DN4, Douleur Neuropathique 4
References
1. Wang, JV, Akintilo, L, and Geronemus, RG. Growth of cosmetic procedures in millennials: a 4.5-year clinical review. J Cosmet Dermatol. (2020) 19:3210–2. doi: 10.1111/jocd.13768
2. Dominguez, S, Moshrefi, S, and Dobke, M. Treatment protocol for acute arterial occlusion secondary to facial Revolumization procedures artificial injectable dermal fillers offer minimally invasive and cost-effective alternatives to traditional cosmetic surgical procedures, but are associated with complications and adverse events. Emergency Med. (2017) 49:221–9. doi: 10.12788/emed.2017.0030
3. Chopra, K, Kokosis, G, Slavin, B, Williams, E, and Dellon, AL. Painful complications after cosmetic surgery: management of peripheral nerve injury. Aesthet Surg J. (2019) 39:1427–35. doi: 10.1093/asj/sjy284
4. Rasulić, L, Savić, A, Vitošević, F, Samardžić, M, Živković, B, Mićović, M, et al. Iatrogenic peripheral nerve injuries—surgical treatment and outcome: 10 years’ experience. World Neurosurg. (2017) 103:e6:841–851.e6. doi: 10.1016/j.wneu.2017.04.099
5. Ducic, I, Zakaria, HM, Felder, JM, and Fantus, S. Nerve injuries in aesthetic breast surgery: systematic review and treatment options. Aesthet Surg J. (2014) 34:841–56. doi: 10.1177/1090820X14536726
6. Ducic, I, Zakaria, HM, Felder, JM III, and Arnspiger, S. Abdominoplasty-related nerve injuries: systematic review and treatment options. Aesthet Surg J. (2014) 34:284–97. doi: 10.1177/1090820X13516341
7. Sullivan, D, Chung, KC, Eaves, FF, Rohrich, RJJP, and Surgery, R. The level of evidence pyramid: indicating levels of evidence in plastic and reconstructive Surgery articles. Plast Reconstr Surg. (2011) 128:311–4. doi: 10.1097/PRS.0b013e3182195826
8. Bhattacharjee, K, Misra, DK, and Deori, N. Updates on upper eyelid blepharoplasty. Indian J Ophthalmol. (2017) 65:551–8. doi: 10.4103/ijo.IJO_540_17
9. Bhattacharjee, K, Ghosh, S, Ugradar, S, and Azhdam, AM. Lower eyelid blepharoplasty: an overview. Indian. J Ophthalmol. (2020) 68:2075. doi: 10.4103/ijo.IJO_2265_19
10. Shu, M, He, L, Su, Y, Shi, J, Zhang, X, Liu, X, et al. A novel supra-brow combined with infra-brow lift approach for Asian women. Aesthet Plast Surg. (2016) 40:343–8. doi: 10.1007/s00266-016-0632-y
11. Kim, HS, and Kim, KK. Subbrow lift using frontalis sling to correct lateral orbital laxity. Aesthet Plast Surg. (2020) 44:2119–26. doi: 10.1007/s00266-020-01879-9
12. Booth, AJ, Murray, A, and Tyers, AG. The direct brow lift: efficacy, complications, and patient satisfaction. Br J Ophthalmol. (2004) 88:688–91. doi: 10.1136/bjo.2003.019232
13. Lee, JW, Cho, BC, and Lee, KY. Direct brow lift combined with suspension of the orbicularis oculi muscle. Arch Plast Surg. (2013) 40:603–9. doi: 10.5999/aps.2013.40.5.603
14. Griffin, GR, and Kim, JC. Ideal female brow aesthetics. Clin Plast Surg. (2013) 40:147–55. doi: 10.1016/j.cps.2012.07.003
15. Kim, YS. Subbrow blepharoplasty using supraorbital rim periosteal fixation. Aesthet Plast Surg. (2014) 38:27–31. doi: 10.1007/s00266-013-0189-y
16. Turin, SY, Vaca, EE, Cheesborough, JE, Sinno, S, and Mustoe, TA. Simplified lateral brow lift under local anesthesia for correction of lateral hooding. Plast Reconstr Surg Glob Open. (2019) 7:e2098. doi: 10.1097/GOX.0000000000002098
17. Hampton, T, and Nduka, C. Comments on “the role of gravity in periorbital and Midfacial aging”. Aesthet Surg J. (2015) 35:NP127. doi: 10.1093/asj/sju112
18. Kim, JB, Kim, JC, Jin, HB, Kim, SO, and Chung, JH. Sub-brow blepharoplasty for simultaneous correction of dermatochalasis with upper eyelid hooding and sunken eyelids. Arch Aesthet Plast Surg. (2019) 25:27–31. doi: 10.14730/aaps.2019.25.1.27
19. Schwarcz, RM, and Kotlus, B. Compllications of lower blepharoplasty and midface lifting. Clin Plast Surg. (2015) 42:63–71. doi: 10.1016/j.cps.2014.08.008
20. Zhang, H, Liu, C, Peng, C, Zhu, K, Bu, R, and Liu, H. Blending of the eyelid-cheek junction and removal of protruding fat: an intraoral approach to blepharoplasty of the lower eyelid. Br J Oral Maxillofac Surg. (2009) 47:541–4. doi: 10.1016/j.bjoms.2009.02.014
21. Jin, Y, Gao, W, Teo, HMT, and Lin, X. Transconjunctival lower blepharoplasty using Midcheek spaces for orbital fat transposition (S.O.F.T.). Ann Plast Surg. (2021) 86:620–6. doi: 10.1097/SAP.0000000000002864
22. Wong, CH, and Mendelson, B. Facial soft-tissue spaces and retaining ligaments of the midcheek: defining the premaxillary space. Plast Reconstr Surg. (2013) 132:49–56. doi: 10.1097/PRS.0b013e3182910a57
23. Hwang, K, Nam, YS, Choi, HG, Han, SH, and Hwang, SH. Cutaneous innervation of lower eyelid. J Craniofac Surg. (2008) 19:1675–7. doi: 10.1097/SCS.0b013e31818c0495
24. Schatz, CJ, and Ginat, DT. Imaging features of rhinoplasty. AJNR Am J Neuroradiol. (2014) 35:216–22. doi: 10.3174/ajnr.A3443
25. Sajjadian, A, Rubinstein, R, and Naghshineh, N. Current status of grafts and implants in rhinoplasty: part I. Autologous grafts. Plast Reconstr Surg. (2010) 125:40e–9e. doi: 10.1097/PRS.0b013e3181c82f12
26. Kokubo, LCP, Carvalho, TBO, Fornazieri, MA, Gomes, EMC, Alves, CMF, and Sampaio, ALL. Effects of septorhinoplasty on smell perception. Eur Arch Otorhinolaryngol. (2019) 276:1247–50. doi: 10.1007/s00405-019-05356-1
27. Kimmelman, CP. The risk to olfaction from nasal surgery. Laryngoscope. (1994) 104:981–8. doi: 10.1288/00005537-199408000-00012
28. Durr, J, Lindemann, J, and Keck, T. Sense of smell before and after functional esthetic rhinoplasty. HNO. (2002) 50:626–9. doi: 10.1007/s00106-001-0586-4
29. Kern, RC, Quinn, B, Rosseau, G, and Farbman, AI. Post-traumatic olfactory dysfunction. Laryngoscope. (2000) 110:2106–9. doi: 10.1097/00005537-200012000-00025
30. Hashimoto, Y, Fukazawa, K, Fujii, M, Takayasu, S, Muto, T, Saito, S, et al. Usefulness of the odor stick identification test for Japanese patients with olfactory dysfunction. Chem Senses. (2004) 29:565–71. doi: 10.1093/chemse/bjh061
31. Kobayashi, M, Saito, S, Kobayakawa, T, Deguchi, Y, and Costanzo, RM. Cross-cultural comparison of data using the odor stick identification test for Japanese (OSIT-J). Chem Senses. (2006) 31:335–42. doi: 10.1093/chemse/bjj037
32. Frank, RA, Gesteland, RC, Bailie, J, Rybalsky, K, Seiden, A, and Dulay, MF. Characterization of the sniff magnitude test. Arch Otolaryngol Head Neck Surg. (2006) 132:532–6. doi: 10.1001/archotol.132.5.532
33. Shemshadi, H, Azimian, M, Onsori, MA, and Azizabadi, FM. Olfactory function following open rhinoplasty: a 6-month follow-up study. BMC Ear Nose Throat Disord. (2008) 8:6. doi: 10.1186/1472-6815-8-6
34. Tutar, B, Ekincioglu, E, Karaketir, S, Berkiten, G, Salturk, Z, Arkan, ME, et al. The impact of platelet-rich fibrin (PRF) on olfactory function and pain after septoplasty operations. Eur Arch Otorhinolaryngol. (2020) 277:1115–20. doi: 10.1007/s00405-020-05839-6
35. Ulusoy, S, Dinc, ME, Dalgic, A, Dizdar, D, Avincsal, MO, and Kulekci, M. Effects of spreader grafts on olfactory function in Septorhinoplasty. Aesthet Plast Surg. (2016) 40:106–13. doi: 10.1007/s00266-015-0597-2
36. Briner, HR, Simmen, D, and Jones, N. Impaired sense of smell in patients with nasal surgery. Clin Otolaryngol Allied Sci. (2003) 28:417–9. doi: 10.1046/j.1365-2273.2003.00735.x
37. Mitz, V, and Peyronie, M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg. (1976) 58:80–8. doi: 10.1097/00006534-197607000-00013
38. Baker, DC. Complications of cervicofacial rhytidectomy. Clin Plast Surg. (1983) 10:543–62. doi: 10.1016/S0094-1298(20)31873-3
39. Jacono, AA, Alemi, AS, and Russell, JL. A Meta-analysis of complication rates among different SMAS facelift techniques. Aesthet Surg J. (2019) 39:927–42. doi: 10.1093/asj/sjz045
40. Chang, KN. Analysis of the outcome of Reoperative face lifts using sub-SMAS techniques. Plast Reconstr Surg. (2022) 150:47–56. doi: 10.1097/PRS.0000000000009199
41. Agarwal, CA, Mendenhall, SD 3rd, Foreman, KB, and Owsley, JQ. The course of the frontal branch of the facial nerve in relation to fascial planes: an anatomic study. Plast Reconstr Surg. (2010) 125:532–7. doi: 10.1097/PRS.0b013e3181c82e9d
42. Tzafetta, K, and Terzis, JK. Essays on the facial nerve: part I. Microanatomy. Plast Reconstr Surg. (2010) 125:879–89. doi: 10.1097/PRS.0b013e3181ccdc78
43. Roostaeian, J, Rohrich, RJ, and Stuzin, JM. Anatomical considerations to prevent facial nerve injury. Plast Reconstr Surg. (2015) 135:1318–27. doi: 10.1097/PRS.0000000000001244
44. Trussler, AP, Stephan, P, Hatef, D, Schaverien, M, Meade, R, and Barton, FE. The frontal branch of the facial nerve across the zygomatic arch: anatomical relevance of the high-SMAS technique. Plast Reconstr Surg. (2010) 125:1221–9. doi: 10.1097/PRS.0b013e3181d18136
45. Yang, SH, Park, H, Yoo, DS, Joo, W, and Rhoton, A. Microsurgical anatomy of the facial nerve. Clin Anat. (2021) 34:90–102. doi: 10.1002/ca.23652
46. O’Brien, JX, Ashton, MW, Rozen, WM, Ross, R, and Mendelson, BC. New perspectives on the surgical anatomy and nomenclature of the temporal region: literature review and dissection study. Plast Reconstr Surg. (2013) 131:510–22. doi: 10.1097/PRS.0b013e31827c6ed6
47. Visconti, G, and Salgarello, M. Anatomical considerations to prevent facial nerve injury: insights on frontal branch and Cervicofacial trunk nerve anatomy in SMAS face lifts. Plast Reconstr Surg. (2016) 137:751e–2e. doi: 10.1097/PRS.0000000000002166
48. Hardwicke, JT, Bechar, J, and Skillman, JM. Are systemic antibiotics indicated in aesthetic breast surgery? A systematic review of the literature. Plast Reconstr Surg. (2013) 131:1395–403. doi: 10.1097/PRS.0b013e31828bd752
49. Broyles, JM, Tuffaha, SH, Williams, EH, Glickman, L, George, TA, and Lee, DA. Pain after breast surgery: etiology, diagnosis, and definitive management. Microsurgery. (2016) 36:535–8. doi: 10.1002/micr.30055
50. Brown, T. Objective sensory changes following subfascial breast augmentation. Aesthet Surg J. (2016) 36:784–9. doi: 10.1093/asj/sjw005
51. Helmy, Y. Nipple and areola complex sensitivity changes after Peri-areolar and inframammary incisions for augmentation mammoplasty (a comparative study). Plastic Surgery Mod Tech. (2017) 3:118. doi: 10.29011/2577-1701.100018
52. Ducic, I, and Larson, EE. Outcomes of surgical treatment for chronic postoperative breast and abdominal pain attributed to the intercostal nerve. J Am Coll Surg. (2006) 203:304–10. doi: 10.1016/j.jamcollsurg.2006.05.018
53. Buck, DW, and Mustoe, TA. An evidence-based approach to abdominoplasty. Plast Reconstr Surg. (2010) 126:2189–95. doi: 10.1097/PRS.0b013e3181f83115
54. Staalesen, T, Elander, A, Strandell, A, and Bergh, C. A systematic review of outcomes of abdominoplasty. J Plast Surg Hand Surg. (2012) 46:139–44. doi: 10.3109/2000656X.2012.683794
55. Chatel, H, Madar, Y, Leyder, P, Bonneau, C, Barrat, C, and Quilichini, J. Prevalence and factors associated with persistent pain following body contouring surgery. J Plast Reconstr Aesthet Surg. (2016) 69:700–5. doi: 10.1016/j.bjps.2016.01.008
56. van Uchelen, JH, Werker, PM, Kon, MJP, and Surgery, R. Complications of abdominoplasty in 86 patients. Plast Reconstr Surg. (2001) 107:1869–73. doi: 10.1097/00006534-200106000-00037
57. Pechter, EA, and Smith, PB. Transient femoral neuropathy after abdominoplasty. Ann Plast Surg. (2008) 61:492–3. doi: 10.1097/SAP.0b013e31816c5cbe
58. Ege, GÖ, and MJBjops, Ö. Heating-pad burn as a complication of abdominoplasty. Br J Plast Surg. (2003) 56:52–3. doi: 10.1016/S0007-1226(03)00014-6
59. Chowdhry, S, Davis, J, Boyd, T, Choo, J, Brooks, R, Kelishadi, S, et al. Safe tummy tuck: anatomy and strategy to avoid injury to the lateral femoral cutaneous nerve during abdominoplasty. Eplasty. (2015) 15:e22.
60. Staalesen, T, Olsén, MF, and Elander, A. Complications of abdominoplasty after weight loss as a result of bariatric surgery or dieting/postpregnancy. J Plast Surg Hand Surg. (2012) 46:416–20. doi: 10.3109/2000656X.2012.717898
61. Zuelzer, HB, Ratliff, CR, and Drake, DB. Complications of abdominal contouring surgery in obese patients: current status. Ann Plast Surg. (2010) 64:598–604. doi: 10.1097/SAP.0b013e3181cf9f9e
62. Rawlani, V, Lee, MJ, and Dumanian, GA. Bilateral sciatic neurapraxia following combined abdominoplasty and mastopexy. Plast Reconstr Surg. (2010) 125:31e–2e. doi: 10.1097/PRS.0b013e3181c2a367
63. Yang, H, Dong, Y, Wang, Z, Lai, J, Yao, C, Zhou, H, et al. Traumatic neuromas of peripheral nerves: Diagnosis, management and future perspectives. Front. Neurol. (2023) 13:1039529. doi: 10.3389/fneur.2022.1039529
64. Lee, CH, and Dellon, AL. Surgical management of groin pain of neural origin. J Am Coll Surg. (2000) 191:137–42. doi: 10.1016/S1072-7515(00)00319-7
65. Liszka, TG, Dellon, AL, and Manson, PN. Iliohypogastric nerve entrapment following abdominoplasty. Plast Reconstr Surg. (1994) 93:181–4. doi: 10.1097/00006534-199401000-00030
66. Nahabedian, MY, and Dellon, AL. Outcome of the operative management of nerve injuries in the ilioinguinal region. J Am Coll Surg. (1997) 184:265–8.
67. Dong, Y, Alhaskawi, A, Zhou, H, Zou, X, Liu, Z, Ezzi, SHA, et al. Imaging diagnosis in peripheral nerve injury. Front. Neurol. (2023) 14:1250808. doi: 10.3389/fneur.2023.1250808
68. Lepic, S, Lepic, M, Banjanin, N, Mandic-Rajcevic, S, and Rasulic, L. A review of the diet, nutrients, and supplementation potential for the outcome augmentation in surgical treatment of peripheral nerve injuries. Front Surg. (2022) 9:942739. doi: 10.3389/fsurg.2022.942739
69. Dellon, AL. Surgical treatment of upper extremity pain. Hand Clin. (2016) 32:71–80. doi: 10.1016/j.hcl.2015.08.008
Keywords: nerve injuries, peripheral nerves, plastic surgeries, cosmetic surgeries, treatment algorithm, occurrence
Citation: Chen Q, Li P, Zhao Q, Tu T, Lu H and Zhang W (2023) Occurrence and treatment of peripheral nerve injuries after cosmetic surgeries. Front. Neurol. 14:1258759. doi: 10.3389/fneur.2023.1258759
Edited by:
Jian-Quan Shi, Nanjing Medical University, ChinaReviewed by:
Veronica Alexandra Antipova, Medical University of Graz, AustriaA. Emre Öge, Istanbul University, Türkiye
Shimon Rochkind, Tel Aviv University, Israel
Copyright © 2023 Chen, Li, Zhao, Tu, Lu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Zhang, zhangweils1968@163.com; Hui Lu, huilu@zju.edu.cn
†These authors have contributed equally to this work
 Qiang Chen1†
Qiang Chen1† Tian Tu
Tian Tu Hui Lu
Hui Lu