- Research Center Innovations in Care, Rotterdam University of Applied Sciences, Rotterdam, Netherlands
Introduction: Aging with a childhood-onset disability, such as cerebral palsy (CP), spina bifida (SB), and muscular diseases (MD), comes along with significant impairments and comorbidities. Despite the increasing evidence an overall picture is lacking. This study aimed to review the literature about adults with CP/SB/MD and impairments and comorbidities to perform a meta-analysis.
Materials and methods: Embase, PubMed, Cinahl, and Google Scholar were searched (2000–2020). Search terms included adults with one of the aforementioned disabilities combined with impairments and comorbidities. If specific impairments or comorbidities were reported by at least four studies, these were included in the study. Pooled prevalence (95% Confidence Interval) of impairments/comorbidities were calculated.
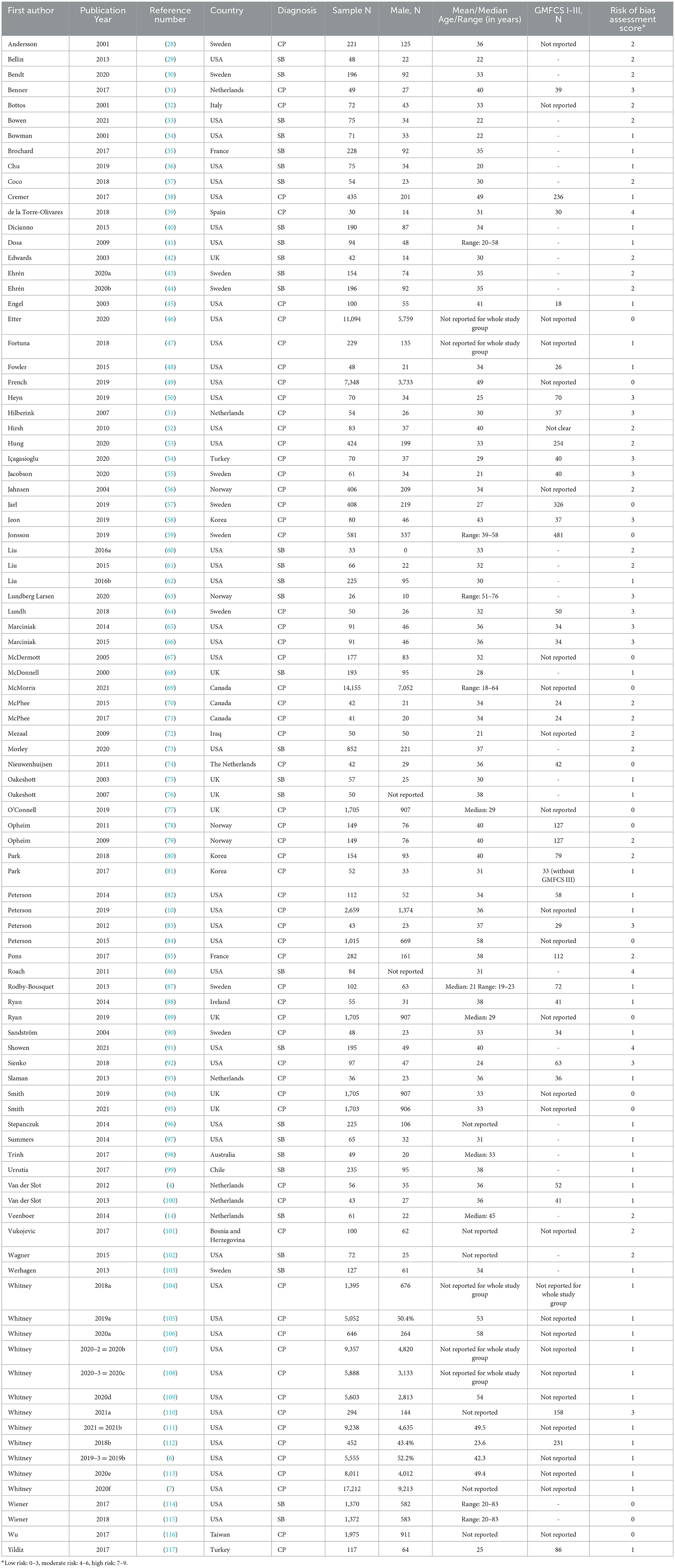
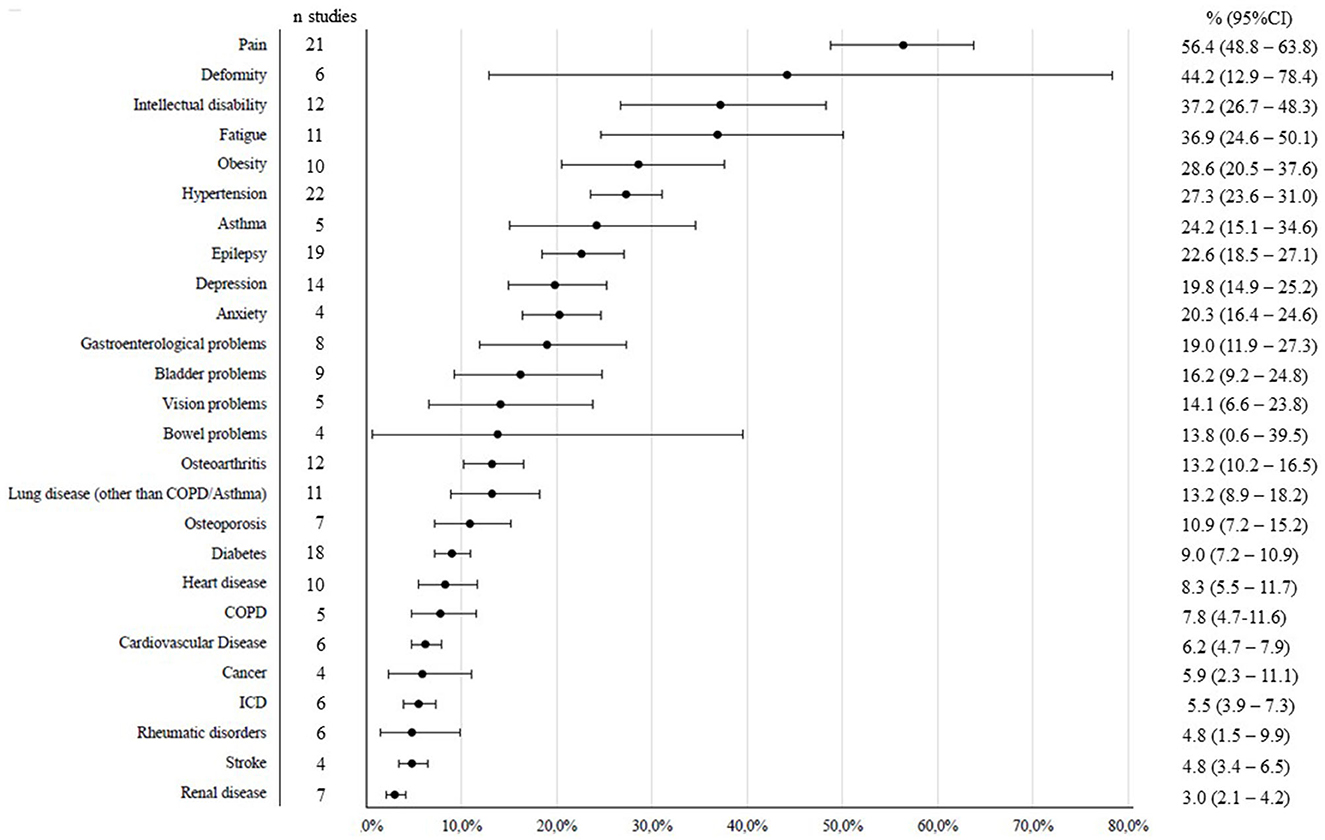
Results: The search yielded 7,054 studies of which 95 were included in the meta-analysis (64 CP, 31 SB, 0 MD). In total estimates were calculated for 26 (CP) and 11 (SB) outcomes. In adults with CP, pain [56.4% (95%CI 48.8–63.8)], deformities [44.2% (95%CI 12.9–78.4)], intellectual disability [37.2% (95%CI 26.7–48.3)], and fatigue [36.9% (95%CI 24.6–50.1)] were most prevalent; renal disease [3.0% (95%CI 2.1–4.2)] and stroke/rheumatic diseases {4.8% (95%CI 3.4–6.5; 4.8% (95%CI 1.5–9.9)] respectively} were least prevalent. For adults with SB, bladder incontinence [60.0% (95%CI 50.5–69.2)], bowel incontinence [49.2% (95%CI 34.5–64.0)], pain [44.1% (95%CI 27.4–61.5)], and sleeping problems [30.3% (95%CI 4.7–65.8)] were most prevalent; diabetes [4.8% (95%CI 2.8–7.3)] and renal disease [8.7% (95%CI 2.0–19.9)] were least prevalent. The included studies showed large heterogeneity.
Conclusions: More research is needed to study health issues in adults with MD. Adults with CP or SB deal with a variety of health issues. More attention for the mental health of these adults is needed. There also is a need for accessible and adequate screening, preventive measures and clinical follow-up.
1. Introduction
Healthcare for adults with life-long disabilities has gained attention in the literature in the last two decades. Ample research showed increased impairments and comorbidities (also referred to as health issues) in these adults as they age (1–3). Many studies target specific adult populations, such as cerebral palsy (CP), spina bifida (SB) or muscular diseases (MD) [i.e., spinal muscular disease (SMA) or Duchenne muscular disease (DMD)/Becker muscular disease (BMD)]. Of these, adults with CP have been studied most (4–10).
Pain, fatigue, epilepsy and asthma are prevalent in adults with CP (11). In addition, these adults are at risk of several health complaints, including hypertension, depressive symptoms, osteoarthritis, cardiovascular diseases, type 2 diabetes (6, 12, 13). Adults with SB often experience bladder and bowel problems and fatigue (14, 15); fecal incontinence is more often observed with increasing age. Moreover these adults are at risk of renal failure (16). Adult men with DMD/BMD report urine incontinence (17), as well as psychiatric problems such as depressive and stress symptoms (18) and cardiac and renal dysfunction (19). Pain and fatigue are also common (20).
Recently three systematic reviews were published on adults with CP (11, 21, 22). These studies focused on specific health issues (pain and hypertension) or aimed at the most studied outcomes (including participation). As shown, adults with SB or MD develop significant health issues. However, they experience many barriers to healthcare services and screening (23, 24), hampering timely detection and secondary preventive measures. To inform both healthcare professionals as well as adults with CP, SB, or MD, we aim to estimate the prevalence of a broader scope of impairments and comorbidities in these adults. The present study goes beyond focusing on one diagnosis group and had more strict criteria to include outcomes to have more robust estimates. As such, it provides a broader overview of comorbidities that people with CP, SB, or MD often have to deal with than current literature does.
2. Methods
2.1. Study design and participants
We conducted a systematic review of the literature including meta-analysis to estimate the prevalence of impairments and comorbidities in adults with CP, SB, or MD. No review protocol was prepared, and the review was not registered in any register.
2.2. Search strategy
A search strategy was formulated and used in four databases: Embase, Pubmed, Cinahl, and Google Scholar. Search terms included the conditions “cerebral palsy”, “spina bifida”, “spinal muscular atrophy”, and “Duchenne muscular dystrophy” in combination with possible impairments and comorbidities such as “fatigue”, “pain”, and “diabetes. Some impairments and comorbidities were not included as search terms, but were still picked up, because they were often included as one among other outcomes in studies. This was the case for osteoporosis, obesity (as reflected by BMI) and gastroenterological problems. The full search strategy for Pubmed is presented in Supplementary material 1. After removing duplicates, publications were screened on title and abstract to check for eligibility (by both reviewers). Subsequently, full texts were screened, and disagreements were discussed and resolved.
2.3. Selection criteria
Studies were included if they met the following criteria:
1. Published in the period January 1st 2000–December 31th 2020;
2. Including a study sample of n ≥ 25;
3. All participants ≥18 years of age;
4. Not a follow-up intervention study;
5. No selected samples (i.e., only dyskinetic CP).
Of longitudinal designs, the most recent follow-up study with the specific comorbidity or impairment as outcome was included.
2.4. Data extraction
Data extraction was done by both reviewers with a standardized data extraction form in Microsoft Excel. Study sample characteristics and number of cases reported to have an impairment or a comorbidity were recorded for every study. Sample characteristics included first author and publication year, country, sex, age (mean/median), sample size and for CP the GMFCS levels (25). All impairments or comorbidities reported in the studies were recorded, but if less than four studies reported on a specific impairment or comorbidity, we did not include this outcome in the analysis.
2.5. Data analysis
Overall mean proportions and 95% Confidence Interval (95%CI) were estimated for each comorbidity. Random-effects meta-analysis models were used (with DerSimonian and Laird estimator). Meta-analysis modeling was done using the proportion meta-analysis function in StatsDirect. The random-effects model takes the heterogeneity of samples into account. The I2 measure indicated heterogeneity and represents the variation attributed to heterogeneity rather than sampling error across samples.
3. Results
3.1. Study characteristics
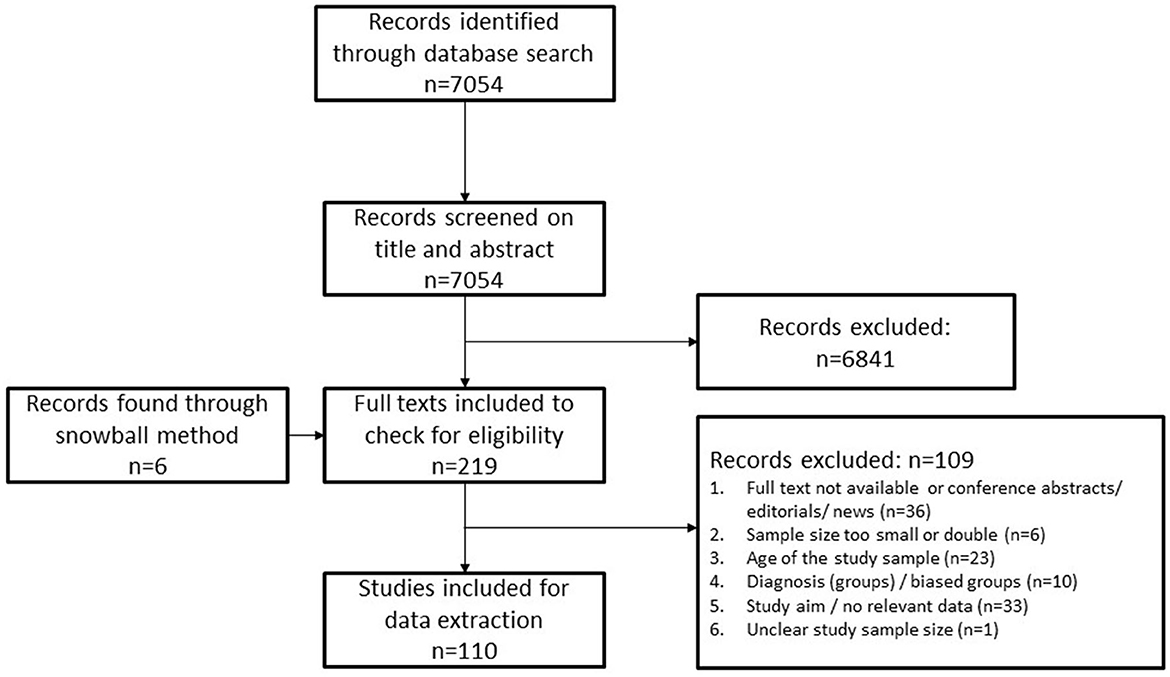
The full selection process is presented in Figure 1. In total 110 (of 7,054) studies met the inclusion criteria. Of these, 15 were excluded because these studies reported on impairments or comorbidities that were studied in less than three other studies. Of the 95 included studies, 64 reported on CP and 31 reported on SB. Regarding adults with MD, no outcome was reported more than three times, and therefore no results on health issues of these adults could be described. Risk of bias was assessed with a quality assessment checklist for prevalence studies that Nguyen and colleagues (26) adapted from Hoy and colleagues (27) and is presented in Table 1.
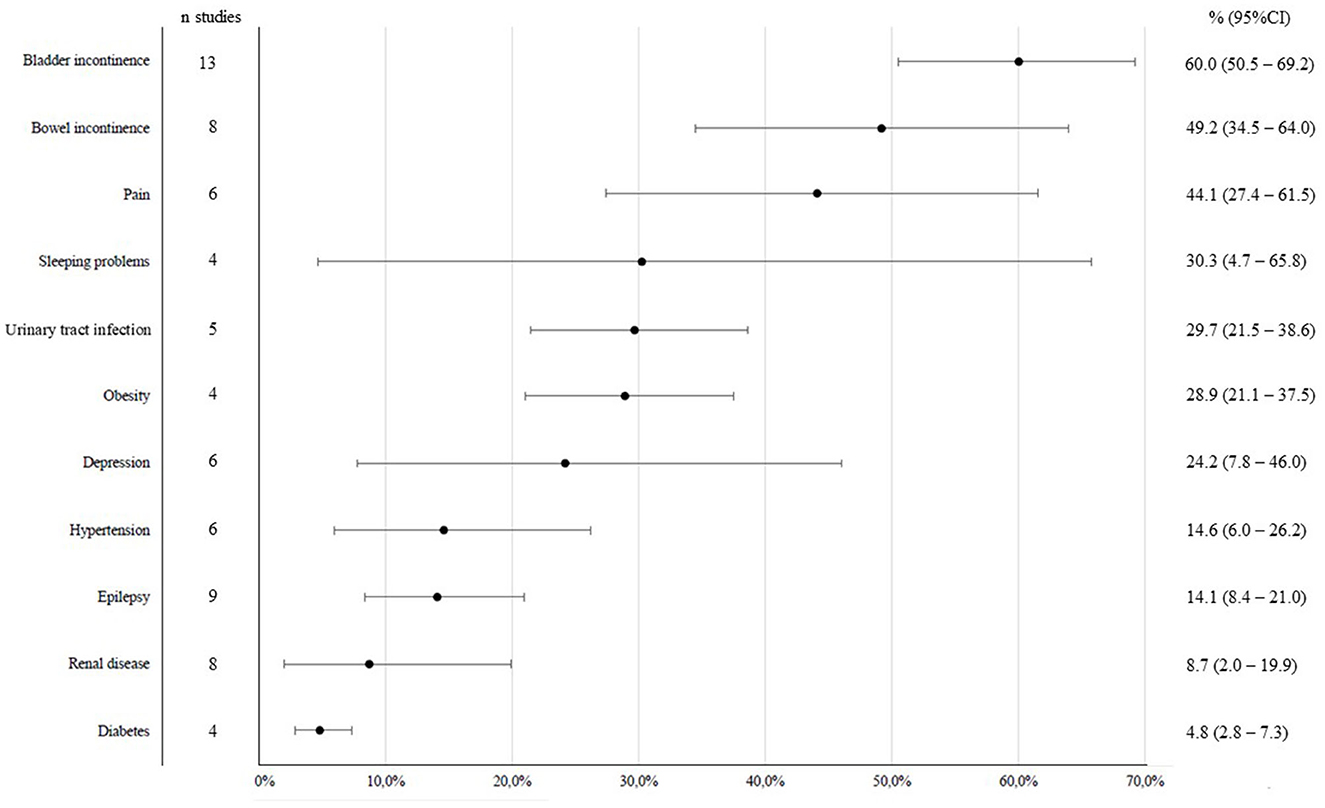
Almost half of all studies were conducted in the United States of America (USA) (ṇ = 47), followed by eleven studies from Sweden (12%), eight studies conducted in the United Kingdom (UK) (8%), and seven studies from The Netherlands (7%). Other studies were from different countries all over the world, but the number of studies for specific countries was small (range: 1–4). Sample size of the included studies varied from 26 to 17,212 people with CP or SB. One study only included females in the study population (Liu et al., 2016) and one study included only males (Mezaal et al., 2009). Other studies had mixed study populations in terms of sex, the proportion of males varied from 25 to 69%. Of these, 53 studies (57%) had a more or less equal distribution of males and females in the study population (between 45 and 55%). All study characteristics are presented in Table 1.
3.2. Health issues in adults with CP
Figure 2 shows the number of studies per impairment or comorbidity and the estimated prevalence (95%CI) of these in adults with CP. A total overview of the health issues, the studies that reported on them, and the number of cases included in the analyses is given in Supplementary material 2. For all analyses the level of heterogeneity (I2) was high (>70%), indicating substantial variation in results across the studies.
The health issue that was most often included in study designs was hypertension (n = 22), followed by pain (n = 21) and epilepsy (n = 19). Least studied were stroke (n = 4), cancer (n = 4), bowel problems (n = 4), and anxiety (n = 4). The most prevalent comorbidity in adults with CP was pain, the overall prevalence was 56%. Deformities were the second most prevalent (44%). Intellectual disability, fatigue, obesity and hypertension, asthma, epilepsy, depression and anxiety were prevalent in more than 20% of adults with CP. Least common were renal diseases (3%), stroke (5%), and rheumatic disorders (5%).
3.3. Health issues in adults with SB
Figure 3 shows the number of studies per impairment or comorbidity and the overall proportion of these in adults with SB. A total overview of the health issues, the studies that reported on them and the number of cases included in the analyses is given in Supplementary material 3. For almost all of the analyses the level of heterogeneity was also high (>70%) except for diabetes (I2 = 41%).
The health issue that was most often included in study designs was bladder incontinence (n = 13), followed by epilepsy (n = 9) and renal disease (n = 8) and bowel incontinence (n = 8). Least studied were diabetes (n = 4), obesity (n = 4), and sleeping problems (n = 4). Bladder incontinence was most prevalent (60%), followed by bowel incontinence (49%) and pain (44%). Urinary tract infection, obesity and depression were present in more than 20% of adults with SB. Least common was diabetes (5%).
4. Discussion
4.1. Main findings
This meta-analysis is the first to review a wide scope of impairments and comorbidities in adults with CP or SB. Impairments and comorbidities in adults with MD could not be assessed due to limited studies. The overall picture may inform health professionals and adults with CP or SB about the common prevalent health issues.
For adults with CP, the results show a lower estimated prevalence of pain (56%) compared to a previous meta-analysis [70%; (21)]. This perhaps has to do with the difference in included studies and thus in other samples concerning sex, age, GMFCS levels, and subtypes. Nevertheless, pain is the most prevalent impairment reported, not only in our study but also in another recent study (11); it was also the second most studied health issue. Attention for pain as a health problem in adults with CP is important in clinical practice (118). This is also the case for adults with SB: They also have a high prevalence of pain (44%), but less often studied. Pain is found to be an important health issue for almost all people with childhood-onset disabilities, starting from a young age. Research also shows that pain can have a profound impact on quality of life and mental health (119).
There seems to be a lack of attention for mental health. While for both depressive symptoms and anxiety, the prevalence rates in adults with CP are around 20%, these outcomes belong to the less studied ones, and this is especially true for anxiety. On the contrary, epilepsy and hypertension are not much more prevalent, but far more often studied, with hypertension being the most studied outcome among adults with CP in this review. For adults with SB, the same pattern was found. While depressive symptoms were prevalent in almost 25% of the people with SB, these were studied in < 50% of the studies included. Other original studies also highlighted the risk of depression and anxiety in people with CP and SB and the need for more attention for mental health in these groups (94, 120, 121). Moreover, literature suggests that comprised mental health is associated with health issues such as pain and fatigue (4, 20). The results call for attention for mental health.
The overall results of this meta-analysis show profound health issues that people with CP and SB have to deal with. They have increased medical needs compared to the general population. Yet, screening of people with CP or SB on health issues is not common practice yet (122–124) and access to needed healthcare is not always self-evident (125). More attention is needed for this matter of how current healthcare practice can be tailored to these increased needs of people with CP or SB. The need for prevention and clinical follow-up of health issues (including mental health) has been emphasized before (120, 126). Moreover, comorbidities not only reflect medical challenges, preventive measures may positively impact social participation of adults with lifelong disabilities as well (125, 127).
4.2. Limitations
It is important to acknowledge the high levels of heterogeneity (I2) in our analyses, indicating substantial variation in results across studies. These levels show that there is no clear pattern of comorbidities or impairments across studies. Yet, we felt it appropriate to summarize the outcomes, because the level of heterogeneity can also be influenced by the fact that outcome measures were not measured in a uniform way across studies. Also, there are differences in sex, age, disability and subtypes of conditions in the study samples. A limitation of this study is also that, due to a small number of studies, other conditions than CP and SB (e.g., MD) could not be included in the analysis. Finally, it must be emphasized that most studies included in this meta-analysis were performed in high-income countries. Therefore, it is not representative for the whole world. More research in low- and middle-income countries is warranted.
4.3. Conclusions
Health issues in adults with MD are studied too less to perform a meta-analysis. Hence research on the impairments and comorbidities in this population is strongly recommended to inform health professionals and the adults themselves. Adults with CP or SB have to deal with a variety of health issues next to their main disability. Pain is found to be the most prevalent issue and can have profound impact on quality of life and mental health. Mental health of adults with CP or SB seems to be understudied and it is important to gain insight into useful interventions for mental wellbeing in these adults. There also is a need for accessible and adequate screening, preventive measures and clinical follow-up of health issues.
Author contributions
JS and SH contributed to the study conception and design, data collection, and interpretation of results. JS performed data analysis and drafted the manuscript. Both authors reviewed the results and approved the final version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1122061/full#supplementary-material
References
1. Kemp BJ. What the rehabilitation professional and the consumer need to know. Phys Med Rehabil Clin. (2005) 16:1–18. doi: 10.1016/j.pmr.2004.06.009
2. Klingbeil H, Baer HR, Wilson PE. Aging with a disability. Arch Phys Med Rehabil. (2004) 85:68–73. doi: 10.1016/j.apmr.2004.03.014
3. Hilberink SR, van der Slot WM, Klem M. Health and participation problems in older adults with long-term disability. Disabil Health J. (2017) 10:361–6. doi: 10.1016/j.dhjo.2016.12.004
4. Van Der Slot WM, Nieuwenhuijsen C, VAN DEN BERG-EMONS RJ, Bergen MP, Hilberink SR, Stam HJ, et al. Chronic pain, fatigue, and depressive symptoms in adults with spastic bilateral cerebral palsy. Dev Med Child Neurol. (2012) 54:836–42. doi: 10.1111/j.1469-8749.2012.04371.x
5. Benner JL, Hilberink SR, Veenis T, Stam HJ, van der Slot WM, Roebroeck ME. Long-term deterioration of perceived health and functioning in adults with cerebral palsy. Arch Phys Med Rehabil. (2017) 98:2196–205.e1. doi: 10.1016/j.apmr.2017.03.013
6. Whitney DG. Prevalence of high-burden medical conditions among young and middle-aged adults with pediatric-onset medical conditions: findings from US private and public administrative claims data. Int J Health Policy Manage. (2019) 8:629. doi: 10.15171/ijhpm.2019.62
7. Whitney DG, Warschausky SA, Whibley D, Kratz A, Murphy SL, Hurvitz EA, et al. Clinical factors associated with mood affective disorders among adults with cerebral palsy. Neurology. (2020) 10:206–13. doi: 10.1212/CPJ.0000000000000721
8. Whitney DG, Whitney RT, Kamdar NS, Hurvitz EA, Peterson MD. Early-onset noncommunicable disease and multimorbidity among adults with pediatric-onset disabilities. Mayo Clin Proc. (2020) 95:274–282. doi: 10.1016/j.mayocp.2019.07.010
9. Peterson MD, Haapala HJ, Kratz A. Pain Phenotypes in Adults Living With Cerebral Palsy. Neurology. (2021) 11:e848–e55. doi: 10.1097/j.pain.0000000000002240
10. Peterson MD, Kamdar N, Hurvitz EA. Age-related trends in cardiometabolic disease among adults with cerebral palsy. Dev Med Child Neurol. (2019) 61:484–9. doi: 10.1111/dmcn.13777
11. van Gorp M, Hilberink SR, Noten S, Benner JL, Stam HJ, van der Slot WM, et al. Epidemiology of cerebral palsy in adulthood: a systematic review and meta-analysis of the most frequently studied outcomes. Arch Phys Med Rehabil. (2020) 101:1041–52. doi: 10.1016/j.apmr.2020.01.009
12. French ZP, Caird MS, Whitney DG. Osteoporosis epidemiology among adults with cerebral palsy: findings from private and public administrative claims data. JBMR plus. (2019) 3:e10231. doi: 10.1002/jbm4.10231
13. Whitney DG, Kamdar NS, Ng S, Hurvitz EA, Peterson MD. Prevalence of high-burden medical conditions and health care resource utilization and costs among adults with cerebral palsy. Clin Epidemiol. (2019) 11:469. doi: 10.2147/CLEP.S205839
14. Veenboer PW, Procee AI, Verheijden JM, Bosch JR, van Asbeck FW, de Kort LM. Medical and psychosocial problems in middle-aged spina bifida patients: survey among members of the Dutch patients' association. Disabil Rehabil. (2014) 36:539–45. doi: 10.3109/09638288.2013.801522
15. de Wild N, Herrmann F, Bos G, Brouwer O, Trzpis M, Broens P. Anorectal dysfunction in adults with spina bifida and associated socio-emotional factors—a retrospective, cross-sectional cohort study. Spinal Cord. (2022) 60:679–686. doi: 10.1038/s41393-022-00754-5
16. Whitney DG, Pruente J, Schmidt M. Risk of advanced chronic kidney disease among adults with spina bifida. Ann Epidemiol. (2020) 43:71–4.e1. doi: 10.1016/j.annepidem.2020.01.003
17. Morse CI, Higham K, Bostock EL, Jacques MF. Urinary incontinence in men with Duchenne and Becker muscular dystrophy. PLoS ONE. (2020) 15:e0233527. doi: 10.1371/journal.pone.0233527
18. Mori-Yoshimura M, Mizuno Y, Yoshida S, Ishihara N, Minami N, Morimoto E, et al. Psychiatric and neurodevelopmental aspects of Becker muscular dystrophy. Neuromusc Disor. (2019) 29:930–9. doi: 10.1016/j.nmd.2019.09.006
19. Motoki T, Shimizu-Motohashi Y, Saito I, Komaki H, Ishiyama A, Aibara K, et al. Renal dysfunction can occur in advanced-stage Duchenne muscular dystrophy. Muscle Nerve. (2020) 61:192–7. doi: 10.1002/mus.26757
20. Pangalila RF, Van Den Bos GA, Bartels B, Bergen M, Stam HJ, Roebroeck ME. Prevalence of fatigue, pain, and affective disorders in adults with Duchenne muscular dystrophy and their associations with quality of life. Arch Phys Med Rehabil. (2015) 96:1242–7. doi: 10.1016/j.apmr.2015.02.012
21. van der Slot WM, Benner JL, Brunton L, Engel JM, Gallien P, Hilberink SR, et al. Pain in adults with cerebral palsy: a systematic review and meta-analysis of individual participant data. Ann Phys Rehabil Med. (2021) 64:101359. doi: 10.1016/j.rehab.2019.12.011
22. Noten S, van den Berg-emons RJ, Thorpe DE, Heyn PC, Marciniak CM, McPhee PG, et al. Blood pressure in adults with cerebral palsy: a systematic review and meta-analysis of individual participant data. J Hyper. (2021) 39:1942. doi: 10.1097/HJH.0000000000002912
23. Merten JW, Pomeranz JL, King JL, Moorhouse M, Wynn RD. Barriers to cancer screening for people with disabilities: a literature review. Disabil Health J. (2015) 8:9–16. doi: 10.1016/j.dhjo.2014.06.004
24. Peterson-Besse JJ, O'Brien MS, Walsh ES, Monroe-Gulick A, White G, Drum CE. Clinical preventive service use disparities among subgroups of people with disabilities: A scoping review. Disabil Health J. (2014) 7:373–93. doi: 10.1016/j.dhjo.2014.04.005
25. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. (1997) 39:214–23. doi: 10.1111/j.1469-8749.1997.tb07414.x
26. Nguyen KA, Peer N, Mills EJ, Kengne AP, A. meta-analysis of the metabolic syndrome prevalence in the global HIV-infected population. PLoS ONE. (2016) 11:e0150970. doi: 10.1371/journal.pone.0150970
27. Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. (2012) 65:934–9. doi: 10.1016/j.jclinepi.2011.11.014
28. Andersson C, Mattsson E. Adults with cerebral palsy: a survey describing problems, needs, and resources, with special emphasis on locomotion. Dev Med Child Neurol. (2001) 43:76–82. doi: 10.1017/S0012162201
29. Bellin MH, Dicianno BE, Osteen P, Dosa N, Aparicio E, Braun P, et al. Family satisfaction, pain, and quality-of-life in emerging adults with spina bifida: a longitudinal analysis. Am J Phys Med Rehabil. (2013) 92:641–55. doi: 10.1097/PHM.0b013e31829b4bc1
30. Bendt M, Gabrielsson H, Riedel D, Hagman G, Hultling C, Franzén E, et al. Adults with spina bifida: A cross-sectional study of health issues and living conditions. Brain Behav. (2020) 10:e01736. doi: 10.1002/brb3.1736
31. Benner JL, Hilberink SR. Long-term deterioration of perceived health and functioning in adults with cerebral palsy. Dev Med Child Neurol. (2017) 59:14. doi: 10.1111/dmcn.13423
32. Bottos M, Feliciangeli A, Sciuto L, Gericke C, Vianello A. Functional status of adults with cerebral palsy and implications for treatment of children. Dev Med Child Neurol. (2001) 43:516–28. doi: 10.1017/S0012162201000950
33. Bowen DK, Balmert LC, Meyer T, Rosoklija I, Hodgkins KS, Ghossein C, et al. Variability in kidney function estimates in emerging adults with spina bifida: implications for transitioning from pediatric to adult care. Urology. (2021) 148:306–13. doi: 10.1016/j.urology.2020.10.050
34. Bowman RM, McLone DG, Grant JA, Tomita T, Ito JA. Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg. (2001) 34:114–20. doi: 10.1159/000056005
35. Brochard C, Peyronnet B, Dariel A, Ménard H, Manunta A, Ropert A, et al. Bowel dysfunction related to spina bifida: keep it simple. Dis Colon Rectum. (2017) 60:1209–14. doi: 10.1097/DCR.0000000000000892
36. Chu DI, Balmert LC, Arkin CM, Meyer T, Rosoklija I, Li B, et al. Estimated kidney function in children and young adults with spina bifida: A retrospective cohort study. Neurourol Urodyn. (2019) 38:1907–14. doi: 10.1002/nau.24092
37. Coco CT, Meenakshi-Sundaram B, Eldefrawy A, Henry ML, Watts T, Aston CE, et al. A cross sectional single institution study of quality of life in adult patients with spina bifida. Neurourol Urodyn. (2018) 37:1757–63. doi: 10.1002/nau.23511
38. Cremer N, Hurvitz EA, Peterson MD. Multimorbidity in middle-aged adults with cerebral palsy. Am J Med. (2017) 130:744.e9–e15. doi: 10.1016/j.amjmed.2016.11.044
39. de la Torre-Olivares R, Moreno-Lorenzo C, Pérez-Mármol JM, Cabrera-Martos I, Villaverde-Gutierrez C, Sánchez AMC, et al. Evaluation of functional status associated with overweight in adults with cerebral palsy. Rehabil Nurs. (2018) 43:88–94. doi: 10.1002/rnj.293
40. Dicianno BE, Kinback N, Bellin MH, Chaikind L, Buhari AM, Holmbeck GN, et al. Depressive symptoms in adults with spina bifida. Rehabil Psychol. (2015) 60:246–53. doi: 10.1037/rep0000044
41. Dosa NP, Foley JT, Eckrich M, Woodall-Ruff D, Liptak GS. Obesity across the lifespan among persons with spina bifida. Disabil Rehabil. (2009) 31:914–20. doi: 10.1080/09638280802356476
42. Edwards RJ, Witchell C, Pople IK. Chronic headaches in adults with spina bifida and associated hydrocephalus. Eur J Pediatr Surg. (2003) 13:S13–7. doi: 10.1055/s-2003-44751
43. Ehrén I, Hagman G, Lindbo L, Gabrielsson H, Bendt M, Seiger Å. Cognitive challenges in persons with spina bifida: Bearing on urological dysfunctions? Neurourol Urodyn. (2020) 39:2139–45. doi: 10.1002/nau.24515
44. Ehrén I, Lindbo L, Gabrielsson H, Bendt M, Seiger Å. Voiding conditions, renal and bowel function in a cohort of adults with spina bifida. Neurourol Urodyn. (2020) 39:1796–802. doi: 10.1002/nau.24422
45. Engel JM, Jensen MP, Hoffman AJ, Kartin D. Pain in persons with cerebral palsy: extension and cross validation. Arch Phys Med Rehabil. (2003) 84:1125–8. doi: 10.1016/S0003-9993(03)00263-6
46. Etter JP, Kannikeswaran S, Hurvitz EA, Caird MS, Jepsen K, Whitney D. The respiratory disease burden of non-traumatic fractures for adults with cerebral palsy. Bone Rep. (2020) 13:100730. doi: 10.1016/j.bonr.2020.100730
47. Fortuna RJ, Holub A, Turk MA, Meccarello J, Davidson PW. Health conditions, functional status and health care utilization in adults with cerebral palsy. Fam Pract. (2018) 35:661–70. doi: 10.1093/fampra/cmy027
48. Fowler EG, Rao S, Nattiv A, Heberer K, Oppenheim WL. Bone density in premenopausal women and men under 50 years of age with cerebral palsy. Arch Phys Med Rehabil. (2015) 96:1304–9. doi: 10.1016/j.apmr.2015.03.012
49. French ZP, Torres RV, Whitney DG. Elevated prevalence of osteoarthritis among adults with cerebral palsy. J Rehabil Med. (2019) 51:575–81. doi: 10.2340/16501977-2582
50. Heyn PC, Tagawa A, Pan Z, Thomas S, Carollo JJ. Prevalence of metabolic syndrome and cardiovascular disease risk factors in adults with cerebral palsy. Dev Med Child Neurol. (2019) 61:477–83. doi: 10.1111/dmcn.14148
51. Hilberink SR, Roebroeck ME, Nieuwstraten W, Jalink L, Verheijden JMA, Stam HJ. Health issues in young adults with cerebral palsy: Towards a life-span perspective. J Rehabil Med. (2007) 39:605–11. doi: 10.2340/16501977-0103
52. Hirsh AT, Gallegos JC, Gertz KJ, Engel JM, Jensen MP. Symptom burden in individuals with cerebral palsy. J Rehabil Res Dev. (2010) 47:863–76. doi: 10.1682/JRRD.2010.03.0024
53. Hung CW, Matsumoto H, Ball JR, Plachta S, Dutkowsky JP, Kim H, et al. Symptomatic cervical spinal stenosis in spastic cerebral palsy. Dev Med Child Neurol. (2020) 62:1147–53. doi: 10.1111/dmcn.14607
54. Içagasioglu A, Dogruoz Karatekin B, Mesci E, Yumusakhuylu Y, Murat S, Yasin S. Assessment of adult patients with cerebral palsy. Turk J Phys Med Rehabil. (2020) 66:429–35. doi: 10.5606/tftrd.2020.5614
55. Jacobson DNO, Löwing K, Tedroff K. Health-related quality of life, pain, and fatigue in young adults with cerebral palsy. Dev Med Child Neurol. (2020) 62:372–8. doi: 10.1111/dmcn.14413
56. Jahnsen R, Villien L, Aamodt G, Stanghelle JK, Holm I. Musculoskeletal pain in adults with cerebral palsy compared with the general population. J Rehabil Med. (2004) 36:78–84. doi: 10.1080/16501970310018305
57. Jarl J, Alriksson-Schmidt A, Rodby-Bousquet E. Health-related quality of life in adults with cerebral palsy living in Sweden and relation to demographic and disability-specific factors. Disabil Health J. (2019) 12:460–6. doi: 10.1016/j.dhjo.2019.02.002
58. Jeon I, Bang MS, Lim JY, Shin HI, Leigh JH, Kim K, et al. Sarcopenia among Adults with Cerebral Palsy in South Korea. PM R. (2019) 11:1296–301. doi: 10.1002/pmrj.12134
59. Jonsson U, Eek MN, Sunnerhagen KS, Himmelmann K. Cerebral palsy prevalence, subtypes, and associated impairments: a population-based comparison study of adults and children. Dev Med Child Neurol. (2019) 61:1162–7. doi: 10.1111/dmcn.14229
60. Liu JS, Vo AX, Doolittle J, Hamoui N, Lewicky-Gaupp C, Kielb SJ. Characterizing pelvic organ prolapse in adult spina bifida patients. Urology. (2016) 97:273–6. doi: 10.1016/j.urology.2016.06.026
61. Liu JS, Dong C, Casey JT, Greiman A, Mukherjee S, Kielb SJ. Quality of life related to urinary continence in adult spina bifida patients. Cent Eur J Urol. (2015) 68:61–7. doi: 10.5173/ceju.2015.01.494
62. Liu JS, Greiman A, Casey JT, Mukherjee S, Kielb SJ, A. snapshot of the adult spina bifida patient - high incidence of urologic procedures. Cent Eur J Urol. (2016) 69:72–7. doi: 10.5173/ceju.2016.596
63. Lundberg Larsen K, Maalen-Johansen IK, Rennie L, Lidal IB. Gait Function in Adults Aged 50 Years and Older With Spina Bifida. Arch Phys Med Rehabil. (2020). doi: 10.1016/j.apmr.2020.10.118
64. Lundh S, Nasic S, Riad J. Fatigue, quality of life and walking ability in adults with cerebral palsy. Gait Posture. (2018) 61:1–6. doi: 10.1016/j.gaitpost.2017.12.017
65. Marciniak C, O'Shea SA, Lee J, Jesselson M, Dudas-Sheehan D, Beltran E, et al. Urinary incontinence in adults with cerebral palsy: prevalence, type, and effects on participation. PM R. (2014) 6:110–20. doi: 10.1016/j.pmrj.2013.07.012
66. Marciniak CM, Lee J, Jesselson M, Gaebler-Spira D. Cross-sectional study of bowel symptoms in adults with cerebral palsy: prevalence and impact on quality of life. Arch Phys Med Rehabil. (2015) 96:2176–83. doi: 10.1016/j.apmr.2015.08.411
67. McDermott S, Moran R, Platt T, Issac T, Wood H, Dasari S. Depression in adults with disabilities, in primary care. Disabil Rehabil. (2005) 27:117–23. doi: 10.1080/09638280400007380
68. McDonnell GV, McCann JP. Issues of medical management in adults with spina bifida. Childs Nerv Syst. (2000) 16:222–7. doi: 10.1007/s003810050502
69. McMorris CA, Lake J, Dobranowski K, McGarry C, Lin E, Wilton D, et al. Psychiatric disorders in adults with cerebral palsy. Res Dev Disabil. (2021) 111:103859. doi: 10.1016/j.ridd.2021.103859
70. McPhee PG, Gorter JW, Cotie LM, Timmons BW, Bentley T, MacDonald MJ. Descriptive data on cardiovascular and metabolic risk factors in ambulatory and non-ambulatory adults with cerebral palsy. Data Brief. (2015) 5:967–70. doi: 10.1016/j.dib.2015.10.045
71. McPhee PG, Brunton LK, Timmons BW, Bentley T, Gorter JW. Fatigue and its relationship with physical activity, age, and body composition in adults with cerebral palsy. Dev Med Child Neurol. (2017) 59:367–73. doi: 10.1111/dmcn.13306
72. Mezaal MA, Nouri KA, Abdool S, Safar KA, Nadeem AS. Cerebral palsy in adults consequences of non progressive pathology. Open Neurol J. (2009) 3:24–6. doi: 10.2174/1874205X00903010024
73. Morley CP, Struwe S, Pratte MA, Clayton GH, Wilson PE, Dicianno BE, et al. Survey of U.S. adults with spina bifida. Disabil Health J. (2020) 13:100833. doi: 10.1016/j.dhjo.2019.100833
74. Nieuwenhuijsen C, van der Slot WMA, Dallmeijer AJ, Janssens PJ, Stam HJ, Roebroeck ME, et al. Physical fitness, everyday physical activity, and fatigue in ambulatory adults with bilateral spastic cerebral palsy. Scand J Med Sci Sports. (2011) 21:535–42. doi: 10.1111/j.1600-0838.2009.01086.x
76. Oakeshott P, Hunt GM, Whitaker RH, Kerry S. Perineal sensation: an important predictor of long-term outcome in open spina bifida. Arch Dis Child. (2007) 92:67–70. doi: 10.1136/adc.2006.102079
77. O'Connell NE, Smith KJ, Peterson MD, Ryan N, Liverani S, Anokye N, et al. Incidence of osteoarthritis, osteoporosis and inflammatory musculoskeletal diseases in adults with cerebral palsy: A population-based cohort study. Bone. (2019) 125:30–5. doi: 10.1016/j.bone.2019.05.007
78. Opheim A, Jahnsen R, Olsson E, Stanghelle JK. Physical and mental components of health-related quality of life and musculoskeletal pain sites over seven years in adults with spastic cerebral palsy. J Rehabil Med. (2011) 43:382–7. doi: 10.2340/16501977-0787
79. Opheim A, Jahnsen R, Olsson E, Stanghelle JK. Walking function, pain, and fatigue in adults with cerebral palsy: a 7-year follow-up study. Dev Med Child Neurol. (2009) 51:381–8. doi: 10.1111/j.1469-8749.2008.03250.x
80. Park MW, Kim WS, Bang MS, Lim JY, Shin HI, Leigh JH, et al. Needs for medical and rehabilitation services in adults with cerebral palsy in Korea. Ann Rehabil Med. (2018) 42:465–72. doi: 10.5535/arm.2018.42.3.465
81. Park EY, Kim WH. Prevalence of secondary impairments of adults with cerebral palsy according to gross motor function classification system. J Phys Ther Sci. (2017) 29:266–9. doi: 10.1589/jpts.29.266
82. Peterson MD, Haapala HJ, Chaddha A, Hurvitz EA. Abdominal obesity is an independent predictor of serum 25-hydroxyvitamin D deficiency in adults with cerebral palsy. Nutr Metab (Lond). (2014) 11:22. doi: 10.1186/1743-7075-11-22
83. Peterson MD, Haapala HJ, Hurvitz EA. Predictors of cardiometabolic risk among adults with cerebral palsy. Arch Phys Med Rehabil. (2012) 93:816–21. doi: 10.1016/j.apmr.2011.12.024
84. Peterson MD, Ryan JM, Hurvitz EA, Mahmoudi E. Chronic conditions in adults with cerebral palsy. JAMA. (2015) 314:2303–5. doi: 10.1001/jama.2015.11025
85. Pons C, Brochard S, Gallien P, Nicolas B, Duruflé A, Roquet M, et al. Medication, rehabilitation and health care consumption in adults with cerebral palsy: a population based study. Clin Rehabil. (2017) 31:957–65. doi: 10.1177/0269215516663286
86. Roach JW, Short BF, Saltzman HM. Adult consequences of spina bifida: a cohort study. Clin Orthop Relat Res. (2011) 469:1246–52. doi: 10.1007/s11999-010-1594-z
87. Rodby-Bousquet E, Czuba T, Hägglund G, Westbom L. Postural asymmetries in young adults with cerebral palsy. Dev Med Child Neurol. (2013) 55:1009–15. doi: 10.1111/dmcn.12199
88. Ryan JM, Crowley VE, Hensey O, McGahey A, Gormley J. Waist circumference provides an indication of numerous cardiometabolic risk factors in adults with cerebral palsy. Arch Phys Med Rehabil. (2014) 95:1540–6. doi: 10.1016/j.apmr.2014.03.029
89. Ryan JM, Peterson MD, Matthews A, Ryan N, Smith KJ, O'Connell NE, et al. Noncommunicable disease among adults with cerebral palsy: A matched cohort study. Neurology. (2019) 93:e1385–e96. doi: 10.1212/WNL.0000000000008199
90. Sandström K, Alinder J, Oberg B. Descriptions of functioning and health and relations to a gross motor classification in adults with cerebral palsy. Disabil Rehabil. (2004) 26:1023–31. doi: 10.1080/09638280410001703503
91. Showen A, Copp HL, Allen IE, Baradaran N, Liaw A, Hampson LA. Characteristics associated with depression, anxiety, and social isolation in adults with Spina Bifida. Urology. (2021) 149:255–62. doi: 10.1016/j.urology.2020.11.016
92. Sienko SE. An exploratory study investigating the multidimensional factors impacting the health and well-being of young adults with cerebral palsy. Disabil Rehabil. (2018) 40:660–6. doi: 10.1080/09638288.2016.1274340
93. Slaman J, Bussmann J, van der Slot WM, Stam HJ, Roebroeck ME, van den Berg-Emons RJ. Physical strain of walking relates to activity level in adults with cerebral palsy. Arch Phys Med Rehabil. (2013) 94:896–901. doi: 10.1016/j.apmr.2012.11.005
94. Smith KJ, Peterson MD, O'Connell NE, Victor C, Liverani S, Anokye N, et al. Risk of depression and anxiety in adults with cerebral palsy. JAMA Neurol. (2019) 76:294–300. doi: 10.1001/jamaneurol.2018.4147
95. Smith KJ, Peterson MD, Victor C, Ryan JM. Risk of dementia in adults with cerebral palsy: a matched cohort study using general practice data. BMJ Open. (2021) 11:e042652. doi: 10.1136/bmjopen-2020-042652
96. Stepanczuk BC, Dicianno BE, Webb TS. Young adults with spina bifida may have higher occurrence of prehypertension and hypertension. Am J Phys Med Rehabil. (2014) 93:200–6. doi: 10.1097/PHM.0b013e3182a92b03
97. Summers SJ, Elliott S, McAdams S, Oottamasathien S, Brant WO, Presson AP, et al. Urologic problems in spina bifida patients transitioning to adult care. Urology. (2014) 84:440–4. doi: 10.1016/j.urology.2014.03.041
98. Trinh A, Wong P, Sakthivel A, Fahey MC, Hennel S, Brown J, et al. Fat-bone interactions in adults with spina bifida. J Endocr Soc. (2017) 1:1301–11. doi: 10.1210/js.2017-00258
99. Urrutia J, Zamora T, Cuellar J. Does the prevalence of spondylolysis and spina bifida occulta observed in pediatric patients remain stable in adults? Clin Spine Surg. (2017) 30:E1117–e21. doi: 10.1097/BSD.0000000000000209
100. van der Slot WM, Roebroeck ME, Nieuwenhuijsen C, Bergen MP, Stam HJ, Burdorf A, et al. Cardiovascular disease risk in adults with spastic bilateral cerebral palsy. J Rehabil Med. (2013) 45:866–72. doi: 10.2340/16501977-1185
101. Vukojević M, Cvitković T, Splavski B, Ostojić Z, Šumanović-Glamuzina D, Šimić J. Prevalence of Intellectual Disabilities and Epilepsy in Different Forms of Spastic Cerebral Palsy in Adults. Psychiatr Danub. (2017) 29:111–7.
102. Wagner R, Linroth R, Gangl C, Mitchell N, Hall M, Cady R, et al. Perception of secondary conditions in adults with spina bifida and impact on daily life. Disabil Health J. (2015) 8:492–8. doi: 10.1016/j.dhjo.2015.03.012
103. Werhagen L, Gabrielsson H, Westgren N, Borg K. Medical complication in adults with spina bifida. Clin Neurol Neurosurg. (2013) 115:1226–9. doi: 10.1016/j.clineuro.2012.11.014
104. Whitney D, Hurvitz E, Devlin M, Caird M, French Z, Ellenberg E, et al. Ageing trajectories of musculoskeletal morbidities in adults with cerebral palsy. Dev Med Child Neurol. (2018) 60:72. doi: 10.1111/dmcn.112_14017
105. Whitney DG, Warschausky SA, Ng S, Hurvitz EA, Kamdar NS, Peterson MD. Prevalence of mental health disorders among adults with cerebral palsy: a cross-sectional analysis. Ann Intern Med. (2019) 171:328–33. doi: 10.7326/M18-3420
106. Whitney DG. Nontrauma fracture increases risk for respiratory disease among adults with cerebral palsy. J Orthop Res. (2020) 38:2551–8. doi: 10.1002/jor.24675
107. Whitney DG, Bell S, Etter JP, Prisby RD. The cardiovascular disease burden of non-traumatic fractures for adults with and without cerebral palsy. Bone. (2020) 136:115376. doi: 10.1016/j.bone.2020.115376
108. Whitney DG, Bell S, Whibley D, Van der Slot WMA, Hurvitz EA, Haapala HJ, et al. Effect of pain on mood affective disorders in adults with cerebral palsy. Dev Med Child Neurol. (2020) 62:926–32. doi: 10.1111/dmcn.14559
109. Whitney DG, Schmidt M, Peterson MD, Haapala H. Polypharmacy Among Privately Insured Adults with Cerebral Palsy: A Retrospective Cohort Study. J Manag Care Spec Pharm. (2020) 26:1153–61. doi: 10.18553/jmcp.2020.26.9.1153
110. Whitney DG, Wolgat EM, Ellenberg EC, Hurvitz EA, Schmidt M. The paradoxical relationship between severity of cerebral palsy and renal function in middle-aged adults: better renal function or inappropriate clinical assessment? Disabil Rehabil. (2021) 44:3853–3859. doi: 10.1080/09638288.2021.1890841
111. Whitney DG, Schmidt M, Haapala H. Polypharmacy is a risk factor for mortality, severe chronic kidney disease, and liver disease among privately insured adults with cerebral palsy. J Manag Care Spec Pharm. (2021) 27:51–63. doi: 10.18553/jmcp.2021.27.1.051
112. Whitney DG, Hurvitz EA, Ryan JM, Devlin MJ, Caird MS, French ZP, et al. Noncommunicable disease and multimorbidity in young adults with cerebral palsy. Clin Epidemiol. (2018) 10:511–9. doi: 10.2147/CLEP.S159405
113. Whitney DG, Oliverio AL, Kamdar NS, Viglianti BL, Naik A, Schmidt M. Advanced CKD among adults with cerebral palsy: incidence and risk factors. Kidney Med. (2020) 2:569–77.e1. doi: 10.1016/j.xkme.2020.05.012
114. Wiener JS, Suson KD, Castillo J, Routh JC, Tanaka S, Liu T, et al. Bowel management and continence in adults with spina bifida: Results from the National Spina Bifida Patient Registry 2009–15. J Pediatr Rehabil Med. (2017) 10:335–43. doi: 10.3233/PRM-170466
115. Wiener JS, Suson KD, Castillo J, Routh JC, Tanaka ST, Liu T, et al. Bladder management and continence outcomes in adults with spina bifida: results from the national spina bifida patient registry, 2009 to 2015. J Urol. (2018) 200:187–94. doi: 10.1016/j.juro.2018.02.3101
116. Wu CW, Huang SW, Lin JW, Liou TH, Chou LC, Lin HW. Risk of stroke among patients with cerebral palsy: a population-based cohort study. Dev Med Child Neurol. (2017) 59:52–6. doi: 10.1111/dmcn.13180
117. Yildiz N, Akkoç Y, Ersöz M, Gündüz B, Erhan B, Yesil H, et al. Cross-sectional study of urinary problems in adults with cerebral palsy: awareness and impact on the quality of life. Neurol Sci. (2017) 38:1193–203. doi: 10.1007/s10072-017-2948-z
118. Shearer HM, Verville L, Côté P, Hogg-Johnson S, Fehlings DL. Clinical course of pain intensity in individuals with cerebral palsy: A prognostic systematic review. Dev Med Child Neurol. (2022). doi: 10.1111/dmcn.15358
119. Schmidt S, Markwart H, Rapp M, Guyard A, Arnaud C, Fauconnier J, et al. Quality of life and mental health in emerging adults with cerebral palsy compared to the general population. Health Qual Life Outc. (2022) 20:1–13. doi: 10.1186/s12955-022-01961-7
120. McMorris C, Lake J, Lunsky Y, Dobranowski K, Fehlings D, Bayley M, et al. Adults with cerebral palsy: physical and mental health issues and health service use patterns. Int Rev Res Dev Disabil. (2015) 48:115–49. doi: 10.1016/bs.irrdd.2015.03.003
121. Peterson MD, Lin P, Kamdar N, Mahmoudi E, Marsack-Topolewski CN, Haapala H, et al. Psychological morbidity among adults with cerebral palsy and spina bifida. Psychol Med. (2021) 51:694–701. doi: 10.1017/S0033291720001981
122. Turk MA. Health, mortality, and wellness issues in adults with cerebral palsy. Dev Med Child Neurol. (2009) 51:24–9. doi: 10.1111/j.1469-8749.2009.03429.x
123. Hilberink SR. The Whitney Comorbidity Index for adults with cerebral palsy: a challenge for practice. Dev Med Child Neurol. (2021) 63:767. doi: 10.1111/dmcn.14890
124. Mirkin K, Casey JT, Mukherjee S, Kielb SJ. Risk of bladder cancer in patients with spina bifida: case reports and review of the literature. J Pediatr Rehabil Med. (2013) 6:155–62. doi: 10.3233/PRM-130254
125. van Heijningen VG, Cardol M, van Heijningen-Tousain HJ, Oosterveer DM, van Markus-Doornbosch F, Sattoe JN, et al. Aging with cerebral palsy: a photovoice study into citizenship. Front Neurol. (2021) 12:729509. doi: 10.3389/fneur.2021.729509
126. Lidal IB, Lundberg Larsen K, Hoff M. 50 Years and older–born with spina bifida: participation, health issues and physical function. Disabil Rehabil. (2021) 43:241–50. doi: 10.1080/09638288.2019.1621953
Keywords: cerebral palsy, spina bifida, muscular disease, comorbidity, impairment, prevalence, meta-analysis, epidemiology
Citation: Sattoe JNT and Hilberink SR (2023) Impairments and comorbidities in adults with cerebral palsy and spina bifida: a meta-analysis. Front. Neurol. 14:1122061. doi: 10.3389/fneur.2023.1122061
Received: 12 December 2022; Accepted: 30 June 2023;
Published: 18 July 2023.
Edited by:
Ross D. Zafonte, Harvard Medical School, United StatesReviewed by:
Daniel Graham Whitney, University of Michigan, United StatesJennifer Lehmann, University of Regensburg, Germany
Copyright © 2023 Sattoe and Hilberink. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jane N. T. Sattoe, j.n.t.sattoe@hr.nl
 Jane N. T. Sattoe
Jane N. T. Sattoe Sander R. Hilberink
Sander R. Hilberink