- 1Unit of Clinical Psychology, Bambino Gesù Children's Hospital, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Rome, Italy
- 2Department of Neuroscience, Headache Center, Bambino Gesù Children's Hospital, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Rome, Italy
- 3Child Neurology and Psychiatry Unit, Tor Vergata University of Rome, Rome, Italy
- 4Center for Sensory-Motor Interaction, Aalborg University, Aalborg, Denmark
Primary headache is a very common and disabling disease. The burden of pain and recurrent attacks may lead to a poor quality of life, anxiety and depression. An increased risk of low functioning and curricular performances in young patients with primary headache has been described. The mechanisms underlying the relationship between migraine and poor school achievement may be various and could be a reflection of weak cognitive skills. Data concerning the cognitive functioning in the free pain interval in pediatric age are under-investigated and results are far from conclusive. The present review article suggests that, though considered a benign disease, pediatric migraine may be associated to altered neuropsychological functioning in the interictal phase. Although children and adolescents with migraine generally have a normal intelligence, they may show a not homogeneous cognitive profile, characterized by possible difficulties in verbal skills, in particular comprehension abilities. Pediatric primary headache may present altered neuropsychological functioning involving attentional resources, processing speed and memory, particularly verbal memory. Given the impact that this disease can have on school performance and the tendency to persist from childhood to adulthood, a cognitive screening in young patients affected by primary headache is pivotal. Additional neuropsychological research using more homogenous methods is needed.
Introduction
Primary headache is a very common and disabling disease (1, 2). Migraine is characterized by moderate to severe pulsating pain attacks lasting even 72 h and aggravated by routine physical activity (3). In pediatric age, pain is more often bilateral than in adults. Migraine pain is often associated with nausea and/or vomiting, phonophobia and photophobia. In migraine with aura, pain may be accompanied or preceded by reversible visual, sensory or motor symptoms (3). Bilateral and pressing/tightening attacks of moderate or mild intensity pain are the main features of tension-type headache (TTH) (3). The burden of pain and recurrent attacks may lead to a poor quality of life, social isolation, anxiety and depression. The impact of headache on academic achievement and school attendance has been described since'80. In an early study, Leviton et al. showed that, out of 150 elementary-school children with headache referred to his center, ~40% had academic difficulties (4). Over the time, several studies highlighted an increased risk of low functioning and curricular performances in young patients with migraine, even compared with patients with cardiomyopathy, cancer and diabetes (5–10). Some vulnerability factors, such as the frequency and intensity of pain and the presence of associated symptoms, have been identified as determinants in the association between migraine and academic failure (10). The mechanisms underlying the relationship between migraine and poor school achievement may be various and could also include: (1) absenteeism from school (11); (2) sleep deprivation as a consequence of pain (12); (3) emotional and behavioral symptoms associated with recurrent pain, affecting the learning process (13); (4) reduced attention in the classroom due to pain and unwellness (12).
Poor academic performance in children and adolescents with migraine may also be a reflection of weak cognitive skills (14). Although cognitive difficulties are not considered “core” symptoms of migraine, a low percentage of patients may experience transient and premonitory cognitive symptoms, such as speech or language impairment, as part of typical aura, but also color and face recognition difficulties, and memory abnormalities (3, 15). Transient neuropsychological problems, such as poor ability to concentrate and feeling of distraction, incapacity to think clearly and to deal with multiple tasks, are often described in the ictal phase of the migraine attacks and may contribute to the attack-related disability (16–18). These reversible neuropsychological disturbances have been attributed to the widespread and complex brain modifications and dysfunction underlying the development of the migraine attacks (16). Since transient cognitive symptoms may also persist after the resolution of pain (16, 19), they cannot be merely explained by pain (16). Electrophysiological and functional alterations in cortical functioning during the free pain interval have been reported in both children and adults (20–23), suggesting the presence of interictal cognitive dysfunctions in patients suffering from migraine. Neurophysiological data on adult and pediatric populations, have evidenced altered processing of stimuli in patients with migraine and TTH (17, 18, 24–26). Moreover, several neuro-imaging studies disclosed structural abnormalities of the brain, such as reduced cortical thickness (27–30) and decreased frontal and parietal lobe gray matter density (31), areas of hypoperfusion (32), and focal or generalized atrophies (i.e., temporal lobe) (33), that may represent the anatomical counterpart of the low performance in cognitive tests (34, 35).
Neuropsychological studies in adults found impaired cognitive functions, such as attention, processing speed (reaction time), executive functioning, verbal and visual memory, during the interictal phase of migraine (16, 35, 36). With regard to children and adolescents, data concerning the cognitive functioning in the free pain interval are under-investigated and results are far from conclusive (14). Considering that school functioning is one of the most important domains of children's life and that childhood and adolescence are critical periods for appropriate academic achievements and personal growth, an analysis of cognitive interictal impairment associated with migraine is essential for an appropriate management of children and adolescents with headache.
Aims
In the present review, we aimed to explore and summarize the current literature on neuropsychological difficulties in children and adolescents with migraine, attempting to describe patients' cognitive profile in the interictal phase of the migraine cycle. Moreover, in order to better understand patients' global needs, we investigated the literature data on the association between headache features, duration of disease and cognitive impairment.
Given the results issued from studies in adult patients with migraine, we hypothesized that: (1) neuropsychological difficulties, particularly those involving memory and attention, may be common also in pediatric migraine, and (2) impairment of cognitive abilities may depend on frequency of migraine attacks and duration of disease.
Methods
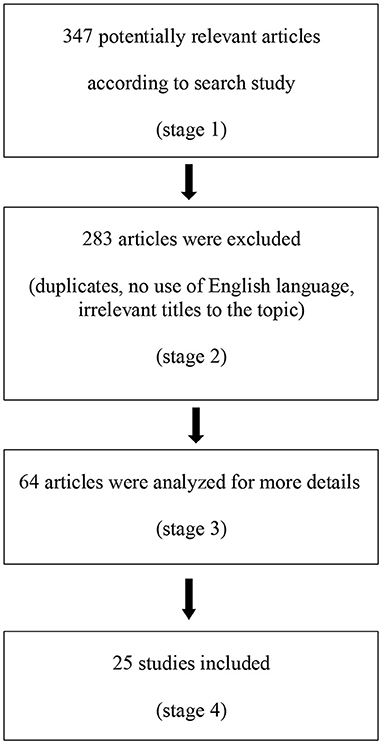
Suitable studies were identified using MEDLINE and Web of Science. Our research considered studies published up to December 2021. We considered only papers in the English language. Search terms included “Pediatric migraine” or “Pediatric headache” and “Cognitive performance,” “Cognitive impairment” or “Neuropsychology,” “Intelligence,” “Attention,” “ADHD,” “Memory,” “Language,” “Visuo-spatial,” “Coordination” and “Difficulties” or “Problems.” We considered papers involving subjects of an age ranging from 0 to 18 years. We considered also articles that, though focusing on adults, included subjects <18 years old. Prospective, observational and retrospective studies were considered as well as multicentric studies and clinical trials (Figure 1).
Results
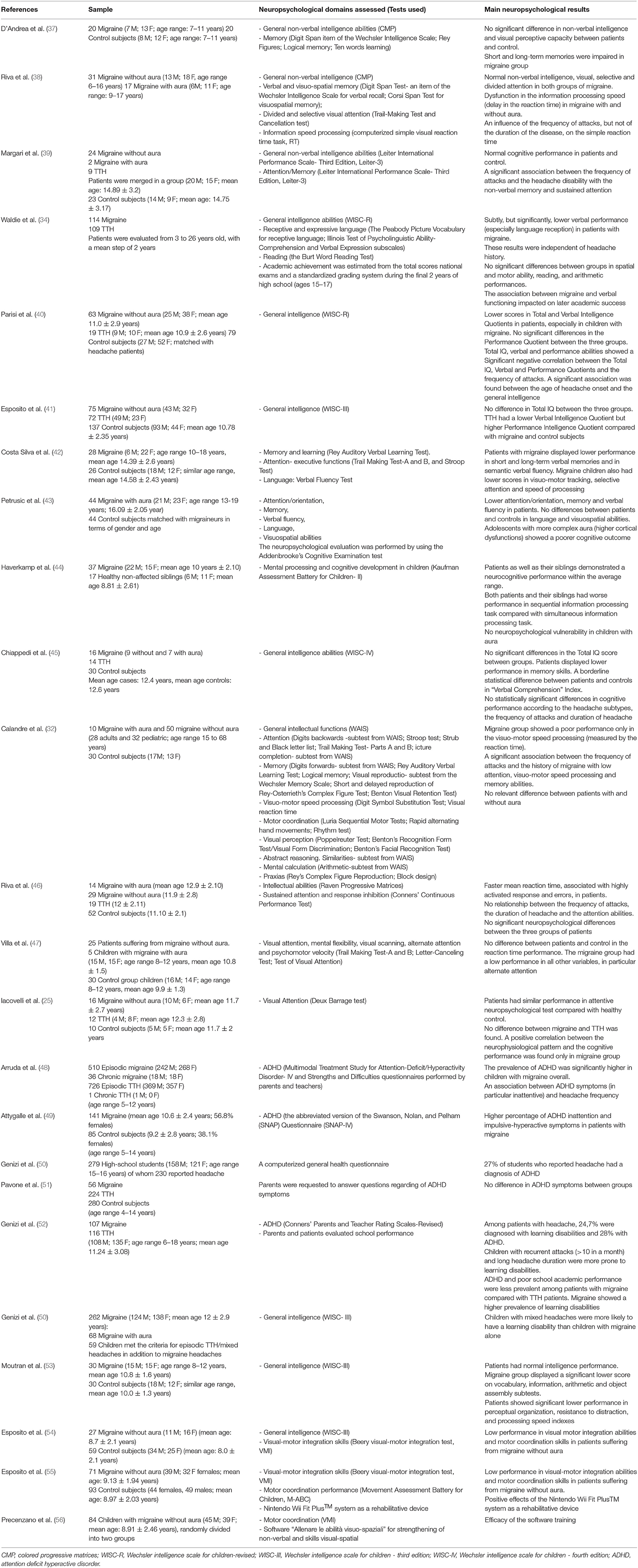
Using the above described strategy, we identified 25 articles concerning the neuropsychology in pediatric migraine. Among them, 1 was a research letter, 2 were retrospective study, 1a longitudinal research and 2 were population studies. As for multicentric studies, we identified 3 papers. One study evaluated neuropsychological performance in both adults and children. Several different tests were employed to measure neuropsychological abilities across studies.
General Intelligence and Language
Over the last decades, several authors aimed to study the general intelligence in children with migraine, reporting discrepancies depending on the nature of the tests administered (non-verbal vs. verbal) (Table 1). In 1989, D'Andrea et al. explored the general non-verbal intelligence and reasoning in a small cohort of 20 children with migraine (age range 7–11 years) (37). By using “Raven's Colored Progressive Matrices” (CMP), the authors demonstrated normal cognitive performances and the absence of difference in intelligence levels between patients with migraine and control subjects. Normal general non-verbal intelligence and reasoning were confirmed by Riva et al. (38). In particular, comparing the performance of children suffering from migraine with (n. 17) and without aura (n. 31), the authors did not identify significant differences in the distribution of Progressive Matrices scores between the groups of patients. In a more recent study, Margari et al. evaluated the non-verbal intelligence abilities, including fluid intelligence, attention skills and non-verbal memory, in pediatric patients with primary headache (39). Thirty-five children suffering from migraine (n. 26) or TTH (n. 9) and 23 healthy subjects were evaluated with the cognitive battery “Leiter-3” (57). In line with previous studies, the headache group did not show global cognitive deficits (the IQ mean value in patients was 97.6 ± 11.3). In particular, no statistical significant difference in the non-verbal IQ mean value was found between patients and control group. The study did not find a significant correlation between the attack frequency and duration of headache and Leiter-3 scores.
While results of studies evaluating non-verbal intelligence agree in showing normal values in children and adolescent with migraine, findings obtained from global intelligence tests show a peculiar profile characterized by subclinical difficulties in verbal skills (14, 34, 40, 45). Results, however, are largely heterogeneous (Table 1). Waldie et al. explored the cognitive performances of headache patients from the age of 3–26 years (34). To the best of our knowledge, the authors were the first to evaluate the general intellectual ability of children and adolescents with migraine and TTH, focusing on different and specific cognitive domains (verbal and performance abilities). Using the “Wechsler Intelligence Scale for Children-Revised” (WISC-R) (58) at ages of 7, 9, 11, and 13 years, the authors observed lower verbal skills (in particular verbal comprehension) in patients with migraine compared not only with free control subjects (Verbal-IQ mean score = 100.6 ± 11.4 and 105.7 ± 13.5, respectively), but also with patients with TTH (mean score = 104.4 ± 13.8). Low verbal receptive performances were also found in 3 years old migraine patients tested with “Peabody Picture Vocabulary test” (PPVT) (59), which evidenced a strong correlation with the mean WISC Verbal-IQ (p < 0.001). Data analysis showed that the verbal performance in patients with migraine did not decline with age and remained lower than other groups over the time. On the other hand, verbal expression measured by the “Illinois Test of Psycholinguistic Ability” (ITPA) (60) did not differ between the headache groups. The cognitive abilities were not related to duration of disease, use of medications or duration and severity of migraine attacks. These findings led the authors to suppose that the low verbal abilities evidenced in migraine group could not be imputable to a cause-effects relationship between history of migraine and cognitive performance, but was rather due to a “not-identified” common risk factor presumably occurring in a prenatal developmental phase. As alternative hypothesis, the authors suggested that the lower performances could be due to patients' attention and concentration difficulties (34).
The absence of association between the intelligence profile and migraine features in children and adolescents was also confirmed in a more recent study (45). The authors described the risk of lower verbal performance in young patients with headache diagnosis (20 children with migraine and 10 with TTH, age ranging from 11 to 14 years) in comparison with healthy children. Patients' group showed a normal TIQ (mean = 112.80 ± 13.4), but exhibited a characteristic neuropsychological functioning regarding memory and verbal skills. The authors identified lower scores in the “Working memory” and, though not statistically significant, in “Verbal Comprehension” indexes of WISC-IV test (61). Duration of headache and frequency of the attacks did not influence the results. Moreover, patients with migraine and TTH had a similar cognitive profile.
In pediatric patients with headache, lower resources in verbal skills and in total intelligence were also reported by Parisi et al. (40) who compared the functioning of children diagnosed with migraine without aura (n. 63) and TTH (n.19) with that of a control healthy group (n. 79) by using the WISC-R edition (58). The authors found lower total quotient (TIQ) scores in children with migraine than in control subjects, although no difference between headache groups was found. Moreover, the study confirmed the lower performance in verbal quotient (VIQ), in particular comprehension subscale, in children with migraine and TTH, as compared to control group. On the other hand, no difference between groups was found in the performance scale (PIQ). In disagreement with the previous study by Waldie et al. (34) the authors showed a significant negative correlation between the frequency of attacks and total, verbal and performance intelligence quotients of WISC test and between the age of headache onset and the total intelligence quotient score. It was suggested that cognitive impairment in headache, particularly migraine, may be due to repeated hyperactivation of several cortical or subcortical neuronal networks during the attacks.
A different intelligence profile between migraine and TTH patients was described by Esposito et al. (41). The authors confirmed a normal intelligence development in patients with primary headache, although, in disagreement with previous literature, they showed weak perceptual organization competences in patients with migraine as compared with both TTH patients and healthy controls. Abnormalities in frontal lobe structure and impairment of executive functions have been suggested as causal mechanisms.
Studies focusing on receptive and expressive language in young patients with headache are sparse. To the best of our knowledge, in addition to the above mentioned study by Waldie et al. (34), only two other studies examined specific interictal language abilities in children/adolescents with migraine. In 2016, Costa Silva et al. evaluated semantic and phonological fluency (“Verbal Fluency test”) in migraine patients (n. 28) and healthy children (n. 26) (42). In patients with migraine, there were significant lower scores in semantic verbal fluency (“animals” subtest), but not in phonemic verbal fluency. Petrusic et al. (43) recruited 74 adolescents (age range 13–19 years) who suffered from migraine with aura. Compared with healthy subjects, performances in verbal fluency, but not in language, were lower in patients than in control subjects. The study did not show a significant association between the neuropsychological performance, including language and verbal fluency, and both higher cortical dysfunctions and aura frequency/duration.
Memory
Several studies investigated memory abilities in children and adolescents with migraine by using standardized test (Table 1). In an early study, D'Andrea et al. (37) described impaired short and long-term visuo-spatial (“Rey Memory test”) and verbal (“Logical Memory test,” the “t, and 10 word learning test”) memory. Several years later, by using the Kaufman Assessment Battery for Children (K-ABC) (62), Haverkamp et al. (44) found cognitive performance within the normal range in children with migraine (n. 37, mean age = 10 years) and in their siblings (n.17, mean age = 8.81 years). The authors, however, described lower performance in subtests requiring memory competences, as in sequential information processing tasks (SEQ). No neuropsychological vulnerability in patients with aura was revealed. Considering that similar scores were found in both migraine patients and their sibling, the authors hypothesized a sample artifact and concluded that no general risk for defective cognitive development exists in young patients with migraine. Using the structured test “Rey Auditory Verbal Learning test” (RAVLT) (63), deficits in verbal memory and learning were reported (42). Compared with healthy subjects, migraine patient performance was more influenced by distractors. Difficulties in verbal memory and, in particular, registration, consolidation, and recall of verbal stimuli were found. As discussed by the authors, since these functions are associated with the ability to use schemas to seek information and organize thoughts, their impairment may lead to poor school performance. The results of a study by Chiappedi et al. (45) provided confirmatory evidence that adolescents affected by headache (migraine and TTH) may have short-term memory difficulties. Although a specific structured evaluation of memory was not performed, cognitive test WISC-IV showed specific impairment in the “Working Memory” index, especially concerning the subtest “Digit Span,” which provides a measure of the ability to store, manage and manipulate information indispensable for language and learning. The study failed to find statistically significant differences in working memory abilities according to headache diagnosis, frequency of attacks, and duration of headache.
In disagreement with previous studies, Margari et al. (39) reported the absence of significant differences between patients with primary headache and controls in “Forward Memory,” “Reverse Memory” and “Non-verbal Memory” subtests scores, issued from the cognitive non-verbal test “Leiter-3” (57). However, the study described a significant association of frequency of the attacks and headache disability with non-verbal memory abilities, suggesting that higher headache disability may have a significant impact on specific cognitive domains, such as the non-verbal memory.
Focusing on migraine with aura, Petrusic et al. (43) showed significantly lower performance in memory skills in adolescents suffering from migraine with aura compared with healthy subjects. As for language, the authors did not evidence significant association between the presence of higher cortical dysfunctions, frequency and duration of aura and the memory skills (evaluated by the “ACE-R test”) (43, 64).
Data on the role of migraine features on memory abilities in pediatric patients are sparse (Table 1). To the best of our knowledge, in addition to the above mentioned studies (39, 45), only Calandre et al. (32) explored this topic. In a sample of 28 adults and 32 pediatric patients with migraine, the authors described an impairment of short- and long-term visual memory, verbal memory, and working memory, related to frequency of the attacks and headache history. Multiple hypoperfusion areas demonstrated by Single Photon Emission Computed Tomography (SPECT) suggested an involvement of several cerebral areas in both hemispheres.
Attention and Attention Deficit Hyperactive Disorder
Research suggests difficulties in attention, processing speed and executive functions during the interictal period of migraine (14) (Table 1). Riva et al. (38) investigated the cognitive performances and behavioral problems in children and adolescents affected by migraine with and without aura (17 and 31 patients, respectively). Normal visual, selective and divided, attention was found in both groups of patients, evaluated with a paper-and-pencil test (“Trail making test,” TMT A and B) (65). However, slower information processing speed, assessed by a computerized simple reaction time to visual stimuli task, was found in migraine patients compared to controls. Frequency of the attacks, but not the duration of the disease, influenced the simple reaction time (38). Confirmatory evidence of altered reaction time in young headache patients was provided by a later study of the same authors (46). The “Conners' Continuous Performance test” (66), evaluating selective and sustained attention, was administered to 62 young patients with primary headache (14 with migraine with aura, 29 with migraine without aura and 19 with TTH) and 52 controls. Faster mean reaction time, associated with highly activated response and errors (more frequent false positive responses), was found in patients compared with controls, suggesting an impulsive response style. The role of emotional factors, such as anxiety, in attentive performance of patients was hypothesized. As in their previous study, no difference was found between the groups of patients, suggesting that migraine and TTH may represent a continuum and share the same pathophysiological mechanisms (22, 24). In a more recent study (42), low performance in attention and executive functions tests was described in children with migraine. In particular, a significant longer execution time (“Trail-Making test”) was found in migraine patients compared with healthy subjects. On the other hand, patients and controls exhibited similar performances in errors. Considering that reaction time explores mainly the speed in detecting and responding to a signal, the authors suggested that its abnormality can be considered as an early and subclinical sign of a neuropsychological impairment, associated with the frequency of headache attacks. In contrast with these findings, another study (44) described similar sequential and simultaneous information processing abilities (evaluated by Kaufman-Assessment Battery for Children) (62) in patients with migraine (with and without aura) and their healthy siblings. These results were replicated by Villa et al. (47), who found no differences between migraine patients (n. 30) and healthy children (n. 30) in a visual reaction time task (“Visual attention test”) (47, 67).
Peculiar attention mechanisms in young patients with migraine were suggested by psychophysiological research (22). Agessi et al. (68) showed impairment of auditory selective attention and physiologic mechanisms of temporal processing. In 2011, we explored both neuropsychological and neurophysiological components of attention in children with migraine (n. 16), TTH (n. 12), and healthy subjects (n. 10) (25). Although a paper and pencil attentive test (“Deux Barrage”) (25) did not evidence any significant impairments and differences in speed and errors between groups, the authors found abnormal neurophysiological mechanisms of spatial attention in patients with headache. Moreover, only in migraine patients, and not in those with TTH, the N140 amplitude increase showed a positive correlation with the neuropsychological performance. We hypothesized that in children with migraine normal attention achievement can be obtained involving a larger amount of “frontal lobe resources,” as compared to healthy children (25).
Though a causal association cannot be maintained, a high prevalence of ADHD symptoms has been described in children and adolescents suffering from migraine (48, 49, 69) (Table 1). Arruda et al. (48) showed a significant higher prevalence of ADHD in children with migraine compared with control subjects. In particular, since this comorbidity mostly involved children with chronic migraine, it was suggested that frequency of migraine attacks increased the risk of ADHD. These results were confirmed by Attygalle et al. (49). The authors described a higher percentage of inattention and impulsive-hyperactive symptoms in patients with migraine than in control subjects. Exploring the opposite association, a high prevalence of migraine (and other primary headache) was described in children with ADHD (70).
We must underline that the association between pediatric headache, in particular migraine, and ADHD is not generally accepted. In a cohort study conducted on 279 high-school students, ADHD prevalence was not different between students who reported headache and those who did not (50). These results were in accordance with a previous study of Pavone et al. (51). In order to explore the prevalence of ADHD and learning disabilities in pediatric patients with headache, a total of 243 medical records of patients (6–18 years) with migraine (n. 107) and TTH (n. 116) were retrospectively reviewed by Genizi et al. (52). Higher rates of ADHD, but also learning disabilities, were found in headache children than in the general population. However, the study did not confirm the relationship between ADHD symptoms and migraine. Supporting a previous study of Mazzone et al. (71), the research revealed a higher prevalence of ADHD symptoms and lower school achievements in children and adolescents with TTH compared to those with migraine.
Learning Disabilities
Learning disabilities are a heterogeneous group of disorders involving difficulties mainly in reading, writing, or mathematical abilities (Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition, DSM-5) (72). These disorders show very often a comorbidity with impairments in cognitive domains, such as memory, attention and processing speed. Few studies investigated the association between migraine and learning disabilities (Table 1). While some of them reported normal abilities in arithmetic and reading in children with migraine (34, 37), other authors described an association between learning disabilities and migraine. Genizi (52) found that about 25% of patients referred to a headache center reported learning disabilities. In particular, compared with children with TTH, those with migraine showed a higher prevalence of learning disabilities (respectively, 26.4 vs. 21.7%). Children with more than 10 attacks/month and long headache duration were more prone to show learning disabilities. Despite these results, children with migraine had good to excellent school achievement. The authors hypothesized that fear of failure and desire for successes, typical of children with headache, may lead to an approach to school characterized by over achievement. Some years later, the same authors (50) showed a higher prevalence of learning disabilities in children with mixed headache (migraine and TTH) compared to those with migraine alone. We have to underline that most studies did not provide a specific neuropsychological evaluation for learning disabilities.
Visuo-Motor and Visuo-Spatial Abilities
Data on visuo-motor and visuo-spatial abilities of children with migraine during the interictal phase are sparse (Table 1). In a study by Correa Moutran et al., a low perceptual organization (evidenced by WISC-III) was observed (53, 73). On the other hand, no difference in visuospatial skills between migraneurs with aura and controls was found in a later study using “Addenbrooke's Cognitive Examination” test (43). In 2012, Esposito et al. showed a lower performance in motor coordination and visual motor integration evaluation in children with migraine, as compared with controls (54). Using the “Beery Visual-motor integration” test (VMI) (74) and the “Movement Assessment Battery” for Children (M-ABC) (75), the same authors confirmed a low performance in visual motor integration abilities and motor coordination skills in patients suffering from migraine without aura (55). Effectiveness of the Nintendo Wii Fit Plus™ system as a rehabilitative device in these patients was suggested (55). Also, Precenzano et al. showed the efficacy of a specific software training (“Allenare le abilitsuo-spaziali”) for enhancing the visuospatial abilities (56).
Discussion
The reviewed literature suggests that, though considered a benign disease, pediatric primary headache may also be associated to altered neuropsychological functioning in the interictal phase. Available findings provide evidence of the role of cognitive difficulties in poor academic achievement in children with headache (34, 40).
Although migraine was especially investigated, literature data suggest that some cognitive abilities, such as memory and attention, may be impaired also in children with TTH. These results support the hypothesis that, in pediatric age, migraine and TTH are not distinct entities, but two aspects of the same spectrum of benign headache (22, 24, 46).
The interictal cognitive profile of pediatric patients with primary headache is characterized also by dysfunctions in selective, prolonged and alternate attention. It was shown that pediatric patients with migraine and TTH have altered processing speed and reaction time, suggesting an impulsive response style and impaired executive functioning. Although children and adolescents with migraine generally show a normal intelligence, they may have difficulties in verbal skills, in particular comprehension abilities. Some authors hypothesized that this may be related to a risk factor, common to migraine and language, occurring in an early developmental, even prenatal, phase (34).
Data on vulnerability factors leading to cognitive impairment in children with primary headache are sparse. The mechanisms underlying the relationship between migraine and interictal cognitive impairment are not completely known. Shared neurobiological factors, such as neurotransmitters, play a key role in both migraine and cognition (76). Noradrenaline and dopamine are involved in memory, learning and attention, as well in several components of executive functions. While noradrenaline keeps adequate levels of alternate, sustained, and selective attention, dopaminergic connections regulate cognitive functions associated with working memory and attention skills. Dysfunction of the hypothalamic-pituitary-adrenal axis (77) and dopamine networks (78) have been suggested as common factors underlying migraine and ADHD. Both noradrenaline and dopamine are involved also in migraine pathophysiology, pain generation as well as accompanying symptoms of migraine attacks (79, 80). Noradrenaline and dopamine act on the trigeminal system by modulating neuronal excitability (81, 82). Low levels of noradrenaline may predispose patients with migraine to syncope and headache attacks. On the other hand, several prodromal symptoms (mood changes, somnolence), accompanying symptoms (vomiting and nausea), and postdromal symptoms (tiredness, drowsiness, mood changes) of the migraine attack may be related to dopaminergic activation (80).
An increasing body of research explored the role of pediatric migraine severity on cognitive resources in the headache free period (32, 38–40, 45, 46, 82). There is evidence that early age of onset and high frequency of the attacks may represent factors favoring cognitive impairment (32, 40).
Though out of the purpose of the present review, the role of medications in causing cognitive difficulties in children with primary headache is not to be forgotten. A negative influence, as possible side-effects of drugs, has been described by Powers et al. (83), who reported memory impairment (17%) and a not specified “cognitive disorder” (16%) in subjects with migraine treated with topiramate. However, the relationship between pharmacological treatment may be bi-univocal. Villa demonstrated lower performance, although within the normal range, in a visual selective and alternate attention test in untreated migraine patients compared with both children assuming migraine prophylaxis and control subjects (84). The authors supposed a positive influence of prophylactic treatment in re-establishing the equilibrium of neurotransmitters and, as a consequence, a reinforcement of the attentive functions (84).
Reviewed literature shows several limitations and heterogeneity in the used methods. Firstly, most recruited patients are referred to neurologists or specialistic headache clinics, resulting unrepresentative of the general population. Second, included samples can be very small and do not consider the migraine phenotype, such as migraine with or without aura. Third, some studies lack a control group. Forth, the neuropsychological tools used for patient evaluation are extremely variable. Fifth, in some studies neuropsychological information are only issued from parents' and/or teachers' reports. Lastly, the possible role of psychological symptoms in explaining, at least in part, the association between pediatric migraine and cognitive difficulties has been scarcely investigated (38, 82).
Conclusions
Pediatric migraine may be associated with altered neuropsychological functioning involving language, attentional resources, processing speed and memory, particularly verbal memory. Given the impact that this disease can have on school performance and the tendency to persist from childhood to adulthood, a special attention should be paid to patients' cognitive development. Unfortunately, the heterogeneity of the results obtained by the different neurocognitive tests prevents statistical analysis of the published findings to be performed. Additional neuropsychological research evaluating larger samples and using more homogenous methods is needed.
Author Contributions
ST and MPC: conceptualization. ST and MV: writing—original draft preparation. MPC, LP, FU, MANF, RM, GS, and GM: writing—review and editing. MV, TGC, and FV: supervision. All authors have read and agreed to the published version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wöber-Bingöl C. Epidemiology of migraine and headache in children and adolescents. Curr Pain Headache Rep. (2013) 17:341. doi: 10.1007/s11916-013-0341-z
2. Krogh A-B, Larsson B, Linde M. Prevalence and disability of headache among Norwegian adolescents: a cross-sectional school-based study. Cephalalgia Int J Headache. (2015) 35:1181–91. doi: 10.1177/0333102415573512
3. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia Int J Headache. (2013) 33:629–808. doi: 10.1177/0333102413485658
4. Leviton A. Do learning handicaps and headache cluster? J Child Neurol. (1986) 1:372–7. doi: 10.1177/088307388600100411
5. Pawlowski C, Buckman C, Tumin D, Smith AW, Crotty J. National trends in pediatric headache and associated functional limitations. Clin Pediatr. (2019) 58:1502–8. doi: 10.1177/0009922819875560
6. Arruda MA, Bigal ME. Migraine and migraine subtypes in preadolescent children: association with school performance. Neurology. (2012) 79:1881–8. doi: 10.1212/WNL.0b013e318271f812
7. Rocha-Filho PAS, Santos PV. Headaches, quality of life, and academic performance in schoolchildren and adolescents. Headache. (2014) 54:1194–202. doi: 10.1111/head.12394
8. Powers SW, Patton SR, Hommel KA, Hershey AD. Quality of life in paediatric migraine: characterization of age-related effects using PedsQL 4.0. Cephalalgia Int J Headache. (2004) 24:120–7. doi: 10.1111/j.1468-2982.2004.00652.x
9. Varni JW, Limbers CA, Burwinkle TM. Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL 4.0 generic core scales. Health Qual Life Outcomes. (2007) 5:43. doi: 10.1186/1477-7525-5-43
10. Powers SW, Patton SR, Hommel KA, Hershey AD. Quality of life in childhood migraines: clinical impact and comparison to other chronic illnesses. Pediatrics. (2003) 112:e1–5. doi: 10.1542/peds.112.1.e1
11. Breuner CC, Smith MS, Womack WM. Factors related to school absenteeism in adolescents with recurrent headache. Headache. (2004) 44:217–22. doi: 10.1111/j.1526-4610.2004.04050.x
12. Gorodzinsky AY, Hainsworth KR, Weisman SJ. School functioning and chronic pain: a review of methods and measures. J Pediatr Psychol. (2011) 36:991–1002. doi: 10.1093/jpepsy/jsr038
13. Strine TW, Okoro CA, McGuire LC, Balluz LS. The associations among childhood headaches, emotional and behavioral difficulties, and health care use. Pediatrics. (2006) 117:1728–35. doi: 10.1542/peds.2005-1024
14. Termine C, Bartoli B, Agosti MA, Cavanna AE, Balottin U. Cognitive impairment in children and adolescents with migraine. Front Neurol. (2018) 9:667. doi: 10.3389/fneur.2018.00667
15. Vincent MB, Hadjikhani N. Migraine aura and related phenomena: beyond scotomata and scintillations. Cephalalgia Int J Headache. (2007) 27:1368–77. doi: 10.1111/j.1468-2982.2007.01388.x
16. Martins IP. Cognitive performance in chronic migraine. Arq Neuropsiquiatr. (2020) 78:131–2. doi: 10.1590/0004-282x20200024
17. Gil-Gouveia R, Oliveira AG, Martins IP. Subjective cognitive symptoms during a migraine attack: a prospective study of a clinic-based sample. Pain Physician. (2016) 19:E137–50.
18. Gil-Gouveia R, Martins IP. Clinical description of attack-related cognitive symptoms in migraine: a systematic review. Cephalalgia Int J Headache. (2018) 38:1335–50. doi: 10.1177/0333102417728250
19. Quintela E, Castillo J, Muñoz P, Pascual J. Premonitory and resolution symptoms in migraine: a prospective study in 100 unselected patients. Cephalalgia Int J Headache. (2006) 26:1051–60. doi: 10.1111/j.1468-2982.2006.01157.x
20. Evers S, Quibeldey F, Grotemeyer KH, Suhr B, Husstedt IW. Dynamic changes of cognitive habituation and serotonin metabolism during the migraine interval. Cephalalgia Int J Headache. (1999) 19:485–91. doi: 10.1046/j.1468-2982.1999.019005485.x
21. Cavestri R, Arreghini M, Longhini M, Ferrarini F, Gori D, Ubbiali A, et al. Interictal abnormalities of regional cerebral blood flow in migraine with and without aura. Minerva Med. (1995) 86:257–64.
22. Pro S, Tarantino S, Capuano A, Vigevano F, Valeriani M. Primary headache pathophysiology in children: the contribution of clinical neurophysiology. Clin Neurophysiol Off J Int Fed Clin Neurophysiol. (2014) 125:6–12. doi: 10.1016/j.clinph.2013.04.335
23. Schoenen J. Neurophysiological features of the migrainous brain. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol. (2006) 27(Suppl. 2):S77–81. doi: 10.1007/s10072-006-0575-1
24. Valeriani M, Galli F, Tarantino S, Graceffa D, Pignata E, Miliucci R, et al. Correlation between abnormal brain excitability and emotional symptomatology in paediatric migraine. Cephalalgia Int J Headache. (2009) 29:204–13. doi: 10.1111/j.1468-2982.2008.01708.x
25. Iacovelli E, Tarantino S, De Ranieri C, Vollono C, Galli F, De Luca M, et al. Psychophysiological mechanisms underlying spatial attention in children with primary headache. Brain Dev. (2012) 34:640–7. doi: 10.1016/j.braindev.2011.10.005
26. De Tommaso M, Valeriani M, Guido M, Libro G, Specchio LM, Tonali P, et al. Abnormal brain processing of cutaneous pain in patients with chronic migraine. Pain. (2003) 101:25–32. doi: 10.1016/s0304-3959(02)00299-3
27. Rocca MA, Messina R, Colombo B, Falini A, Comi G, Filippi M. Structural brain MRI abnormalities in pediatric patients with migraine. J Neurol. (2014) 261:350–7. doi: 10.1007/s00415-013-7201-y
28. Humbertclaude V, Riant F, Krams B, Zimmermann V, Nagot N, Annequin D, et al. Cognitive impairment in children with CACNA1A mutations. Dev Med Child Neurol. (2020) 62:330–7. doi: 10.1111/dmcn.14261
29. Messina R, Rocca MA, Colombo B, Valsasina P, Horsfield MA, Copetti M, et al. Cortical abnormalities in patients with migraine: a surface-based analysis. Radiology. (2013) 268:170–80. doi: 10.1148/radiol.13122004
30. Guarnera A, Bottino F, Napolitano A, Sforza G, Cappa M, Chioma L, et al. Early alterations of cortical thickness and gyrification in migraine without aura: a retrospective MRI study in pediatric patients. J Headache Pain. (2021) 22:79. doi: 10.1186/s10194-021-01290-y
31. Schmitz N, Arkink EB, Mulder M, Rubia K, Admiraal-Behloul F, Schoonman GG, et al. Frontal lobe structure and executive function in migraine patients. Neurosci Lett. (2008) 440:92–6. doi: 10.1016/j.neulet.2008.05.033
32. Calandre EP, Bembibre J, Arnedo ML, Becerra D. Cognitive disturbances and regional cerebral blood flow abnormalities in migraine patients: their relationship with the clinical manifestations of the illness. Cephalalgia Int J Headache. (2002) 22:291–302. doi: 10.1046/j.1468-2982.2002.00370.x
33. Mathew NT, Meyer JS, Welsch KM, Neblett CR. Abnormal CT-Scans in migraine. Headache. (1977) 16:272–9. doi: 10.1111/j.1526-4610.1976.hed1606272.x
34. Waldie KE, Hausmann M, Milne BJ, Poulton R. Migraine and cognitive function: a life-course study. Neurology. (2002) 59:904–8. doi: 10.1212/wnl.59.6.904
35. Foti M, Lo Buono V, Corallo F, Palmeri R, Bramanti P, Marino S. Neuropsychological assessment in migraine patients: a descriptive review on cognitive implications. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol. (2017) 38:553–62. doi: 10.1007/s10072-017-2814-z
36. De Araújo CM, Barbosa IG, Lemos SMA, Domingues RB, Teixeira AL. Cognitive impairment in migraine: a systematic review. Dement Neuropsychol. (2012) 6:74–9. doi: 10.1590/S1980-57642012DN06020002
37. D'Andrea G, Nertempi P, Ferro Milone F, Joseph R, Cananzi AR. Personality and memory in childhood migraine. Cephalalgia Int J Headache. (1989) 9:25–8.
38. Riva D, Aggio F, Vago C, Nichelli F, Andreucci E, Paruta N, et al. Cognitive and behavioural effects of migraine in childhood and adolescence. Cephalalgia Int J Headache. (2006) 26:596–603. doi: 10.1111/j.1468-2982.2006.01072.x
39. Margari L, Palumbi R, Lecce PA, Craig F, Simone M, Margari M, et al. Non-verbal cognitive abilities in children and adolescents affected by migraine and tension-type headache: an observational study using the leiter-3. Front Neurol. (2018) 9:78. doi: 10.3389/fneur.2018.00078
40. Parisi P, Verrotti A, Paolino MC, Urbano A, Bernabucci M, Castaldo R, et al. Headache and cognitive profile in children: a cross-sectional controlled study. J Headache Pain. (2010) 11:45–51. doi: 10.1007/s10194-009-0165-8
41. Esposito M, Pascotto A, Gallai B, Parisi L, Roccella M, Marotta R, et al. Can headache impair intellectual abilities in children? An observational study. Neuropsychiatr Dis Treat. (2012) 8:509–13. doi: 10.2147/NDT.S36863
42. Costa-Silva MA, Prado AC de A, de Souza LC, Gomez RS, Teixeira AL. Cognitive functioning in adolescents with migraine. Dement Neuropsychol. (2016) 10:47–51. doi: 10.1590/S1980-57642016DN10100009
43. Petrusic I, Pavlovski V, Savkovic Z, Vucinic D, Filipovic B, Jancic J. Addenbrooke's cognitive examination test for brief cognitive assessment of adolescents suffering from migraine with aura. Acta Neurol Belg. (2017) 117:97–102. doi: 10.1007/s13760-016-0655-9
44. Haverkamp F, Hönscheid A, Müller-Sinik K. Cognitive development in children with migraine and their healthy unaffected siblings. Headache. (2002) 42:776–9. doi: 10.1046/j.1526-4610.2002.02179.x
45. Chiappedi M, Mensi M, Antonaci E, Zavani E, Tronconi L, Termine C, et al. Intellectual profile of adolescents with headache: a case-control study using the WISC-IV. Front Neurol. (2018) 9:128. doi: 10.3389/fneur.2018.00128
46. Riva D, Usilla A, Aggio F, Vago C, Treccani C, Bulgheroni S. Attention in children and adolescents with headache. Headache. (2012) 52:374–84. doi: 10.1111/j.1526-4610.2011.02033.x
47. Villa TR, Correa Moutran AR, Sobirai Diaz LA, Pereira Pinto MM, Carvalho FA, Gabbai AA, et al. Visual attention in children with migraine: a controlled comparative study. Cephalalgia Int J Headache. (2009) 29:631–4. doi: 10.1111/j.1468-2982.2008.01767.x
48. Arruda MA, Arruda R, Guidetti V, Bigal ME. ADHD is comorbid to migraine in childhood: a population-based study. J Atten Disord. (2020) 24:990–1001. doi: 10.1177/1087054717710767
49. Attygalle UR, Hewawitharana G, Wijesinghe CJ. Migraine, attention deficit hyperactivity disorder and screen time in children attending a Sri Lankan tertiary care facility: are they associated? BMC Neurol. (2020) 20:275. doi: 10.1186/s12883-020-01855-5
50. Genizi J, Khourieh Matar A, Schertz M, Zelnik N, Srugo I. Pediatric mixed headache -The relationship between migraine, tension-type headache and learning disabilities - in a clinic-based sample. J Headache Pain. (2016) 17:42. doi: 10.1186/s10194-016-0625-x
51. Pavone P, Rizzo R, Conti I, Verrotti A, Mistretta A, Falsaperla R, et al. Primary headaches in children: clinical findings on the association with other conditions. Int J Immunopathol Pharmacol. (2012) 25:1083–91. doi: 10.1177/039463201202500425
52. Genizi J, Gordon S, Kerem NC, Srugo I, Shahar E, Ravid S. Primary headaches, attention deficit disorder and learning disabilities in children and adolescents. J Headache Pain. (2013) 14:54. doi: 10.1186/1129-2377-14-54
53. Moutran ARC, Villa TR, Diaz LAS, Noffs MH da S, Pinto MMP, Gabbai AA, et al. Migraine and cognition in children: a controlled study. Arq Neuropsiquiatr. (2011) 69:192–5. doi: 10.1590/s0004-282x2011000200010
54. Esposito M, Verrotti A, Gimigliano F, Ruberto M, Agostinelli S, Scuccimarra G, et al. Motor coordination impairment and migraine in children: a new comorbidity? Eur J Pediatr. (2012) 171:1599–604. doi: 10.1007/s00431-012-1759-8
55. Esposito M, Ruberto M, Gimigliano F, Marotta R, Gallai B, Parisi L, et al. Effectiveness and safety of Nintendo Wii Fit PlusTM training in children with migraine without aura: a preliminary study. Neuropsychiatr Dis Treat. (2013) 9:1803–10. doi: 10.2147/NDT.S53853
56. Precenzano F, Ruberto M, Parisi L, Salerno M, Maltese A, Gallai B, et al. Visual-spatial training efficacy in children affected by migraine without aura: a multicenter study. Neuropsychiatr Dis Treat. (2017) 13:253–8. doi: 10.2147/NDT.S119648
57. Cornoldi C, Giofrè D, Bellacchi C. Procedure di Somministrazione E Scoring Dei Subtest. Leiter-3 Leiter International Scale. Firenze: Giunti OS Organizzazioni Speciali srl Adattamento italiano (2016).
58. Petrosko J. Wechsler intelligence scale for children—revised, 1974. David Wechsler. Meas Eval Guid. (1975) 7:265–7.
59. Taylor Lorne J. The peabody picture vocabulary test: what does it measure? Perceptual and Motor Skills. (1975) 41:777–8.
60. Kirk SA, Winifred D, Kirk James J. Illinois Test of Psycholinguistic Abilities. McCarthy: University of illinois press (1968).
61. Wechsler D. Wechsler Intelligence Scale For Children–Fourth Edition (WISC-IV). San Antonio, TX: The Psychological Corporation (2003).
62. Melchers P, Ulrich P. Kaufman Assessment Battery for Children: K-ABC; Deutschsprachige Fassung. Amsterdam: Swets und Zeitlinger (1994).
63. Rey A. L'examen psychologique dans les cas d'encéphalopathie traumatique. Arch Psychol. (1941) 28:286–340.
64. Mioshi E, Dawson K, Mitchell J, Arnold R, Hodges JR. The addenbrooke's cognitive examination revised (ACE-R): a brief cognitive test battery for dementia screening. Int J Geriatr Psychiatry. (2006) 21:1078–85. doi: 10.1002/gps.1610
65. Reitan RM. Trail making test results for normal and brain-damaged children. Percept Mot Skills. (1971) 33:575–81. doi: 10.2466/pms.1971.33.2.575
66. Conners CK. Manual for the Conners1 Continuous Performance Test-II Tonawanda. Now York, NY: Multi-Heath Systems (2002).
67. Duchesne M, Mattos P. Normalization of a computerized visual attention test (TAVIS). Arq Neuropsiquiatr. (1997) 55:62–9.
68. Agessi LM, Villa TR, Carvalho D de S, Pereira LD. Auditory processing in children with migraine: a controlled study. Neuropediatrics. (2017) 48:123–6. doi: 10.1055/s-0037-1598046
69. Salem H, Vivas D, Cao F, Kazimi IF, Teixeira AL, Zeni CP. ADHD is associated with migraine: a systematic review and meta-analysis. Eur Child Adolesc Psychiatry. (2018) 27:267–77. doi: 10.1007/s00787-017-1045-4
70. Langdon R, DiSabella M, Strelzik J, Fletcher A. Pediatric migraine and academics. Curr Pain Headache Rep. (2020) 24:40. doi: 10.1007/s11916-020-00869-5
71. Mazzone L, Vitiello B, Incorpora G, Mazzone D. Behavioural and temperamental characteristics of children and adolescents suffering from primary headache. Cephalalgia Int J Headache. (2006) 26:194–201. doi: 10.1111/j.1468-2982.2005.01015.x
72. First MB. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. Washington, DC: American Psychiatric Publishing (1994).
73. Woolger C. Wechsler Intelligence Scale for Children-(WISC-III). In: Understanding Psychological Assessment. Boston, MA: Springer (2001). p. 219–33.
74. Beery KE. Beery VMI: The Beery-Buktenica Developmental Test of Visual-Motor Integration. Minneapolis, MN: Pearson (2004).
76. Parisi P, Verrotti A, Paolino MC, Ferretti A, Raucci U, Moavero R, et al. Headache and attention deficit and hyperactivity disorder in children: common condition with complex relation and disabling consequences. Epilepsy Behav EB. (2014) 32:72–5. doi: 10.1016/j.yebeh.2013.12.028
77. Scherder EJA, Rommelse NNJ, Bröring T, Faraone SV, Sergeant JA. Somatosensory functioning and experienced pain in ADHD-families: a pilot study. Eur J Paediatr Neurol EJPN Off J Eur Paediatr Neurol Soc. (2008) 12:461–9. doi: 10.1016/j.ejpn.2007.11.004
78. Treister R, Eisenberg E, Demeter N, Pud D. Alterations in pain response are partially reversed by methylphenidate (Ritalin) in adults with attention deficit hyperactivity disorder (ADHD). Pain Pract Off J World Inst Pain. (2015) 15:4–11. doi: 10.1111/papr.12129
79. Goadsby PJ, Lipton RB, Ferrari MD. Migraine–current understanding and treatment. N Engl J Med. (2002) 346:257–70. doi: 10.1056/NEJMra010917
80. Akerman S, Goadsby PJ. Dopamine and migraine: biology and clinical implications. Cephalalgia Int J Headache. (2007) 27:1308–14. doi: 10.1111/j.1468-2982.2007.01478.x
81. Matsutani K, Tsuruoka M, Shinya A, Furuya R, Kawawa T. Stimulation of the locus coeruleus suppresses trigeminal sensorimotor function in the rat. Brain Res Bull. (2000) 53:827–32. doi: 10.1016/s0361-9230(00)00426-3
82. Araujo GC, Dodd JN, Mar S. Cognitive and emotional functioning in pediatric migraine relative to healthy control subjects. Pediatr Neurol. (2020) 111:35–6. doi: 10.1016/j.pediatrneurol.2020.06.003
83. Powers SW, Coffey CS, Chamberlin LA, Ecklund DJ, Klingner EA, Yankey JW, et al. Trial of amitriptyline, topiramate, and placebo for pediatric migraine. N Engl J Med. (2017) 376:115–24. doi: 10.1056/NEJMoa1610384
Keywords: headache, children, neuropsychology, cognitive performance, intelligence, memory, attention
Citation: Tarantino S, Proietti Checchi M, Papetti L, Ursitti F, Sforza G, Ferilli MAN, Moavero R, Monte G, Capitello TG, Vigevano F and Valeriani M (2022) Interictal Cognitive Performance in Children and Adolescents With Primary Headache: A Narrative Review. Front. Neurol. 13:898626. doi: 10.3389/fneur.2022.898626
Received: 17 March 2022; Accepted: 21 June 2022;
Published: 13 July 2022.
Edited by:
Simona Sacco, University of L'Aquila, ItalyReviewed by:
Umberto Balottin, University of Pavia, ItalyRoberto Palumbi, University of Bari Aldo Moro, Italy
Copyright © 2022 Tarantino, Proietti Checchi, Papetti, Ursitti, Sforza, Ferilli, Moavero, Monte, Capitello, Vigevano and Valeriani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Samuela Tarantino, samuela.tarantino@opbg.net
 Samuela Tarantino
Samuela Tarantino Martina Proietti Checchi
Martina Proietti Checchi Laura Papetti
Laura Papetti Fabiana Ursitti
Fabiana Ursitti Giorgia Sforza
Giorgia Sforza Michela Ada Noris Ferilli
Michela Ada Noris Ferilli Romina Moavero
Romina Moavero Gabriele Monte
Gabriele Monte Teresa Grimaldi Capitello
Teresa Grimaldi Capitello Federico Vigevano
Federico Vigevano Massimiliano Valeriani
Massimiliano Valeriani