Prevalence and factors associated with restless legs syndrome among pregnant women in middle-income countries: a systematic review and meta-analysis
- 1School of Midwifery, College of Health Science, Woldia University, Woldia, Ethiopia
- 2School of Public Health, College of Health Science, Woldia University, Woldia, Ethiopia
Introduction: Restless legs syndrome (RLS) is a debilitating condition characterized by uncomfortable sensations in the legs, typically occurring during periods of rest or sleep. It is more prevalent during pregnancy and is linked to sleep disturbances, diminished quality of life, and pregnancy complications. However, previous studies yielded inconsistent findings among pregnant women in middle-income countries. Consequently, this systematic review and meta-analysis sought to determine the pooled prevalence of restless legs syndrome and its associated factors in these populations.
Method: A systematic review and meta-analysis was conducted on published studies from middle-income countries until May 2023. The review strictly adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Relevant search terms were used to search for studies in PubMed, MEDLINE, EMBASE, and Google Scholar. Data extraction was performed using the Joanna Briggs Institute tool for prevalence studies. The meta-analysis was conducted using STATA 17 software, and heterogeneity was assessed using the I2 test, while publication bias was evaluated using Egger's test. Forest plots were also used to present the pooled prevalence and odds ratio (OR) with a 95% confidence interval (CI) using the random-effects model.
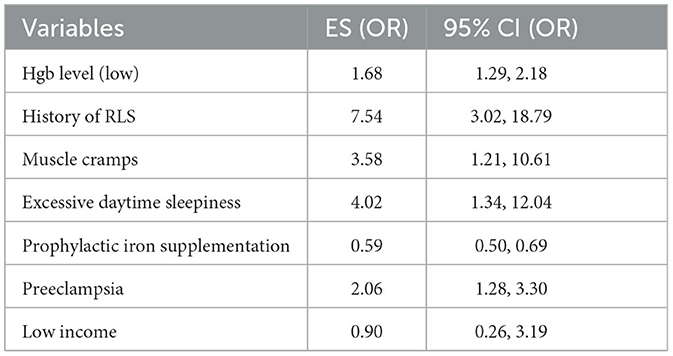
Result: This review included 22 studies from nine countries with a total of 17, 580 study participants. The overall pooled prevalence of RLS among pregnant women in middle-income countries was 13.82% (95% CI: 13.31, 14.32), and having low hemoglobin level (AOR: 1.68, 95% CI: 1.29, 2.18), history of RLS (AOR: 7.54, 95% CI: 3.02, 18.79), muscle cramps (AOR: 3.58, 95% CI: 1.21, 10.61), excessive day time sleepiness (AOR: 4.02, 95% CI: 1.34, 12.04), preeclampsia (AOR: 2.06, 95% CI: 1.28, 3.30), and taking prophylactic iron supplementation (AOR: 0.59, 95% CI: 0.50, 0.69) were the identified factors associated with it.
Conclusion: Generally, nearly one in every eight pregnant women in middle-income countries develop restless legs syndrome during pregnancy. Having low hemoglobin level, a history of RLS, muscle cramps, excessive daytime sleepiness, preeclampsia, and taking prophylactic iron supplementation were the identified factors associated with it. These findings underscore the importance of addressing the identified factors associated with RLS in order to effectively mitigate its occurrence among pregnant women.
Introduction
Restless legs syndrome (RLS) is a syndrome characterized by uncomfortable sensations in the legs, particularly during sleep or rest, leading to an urge to move the legs. Although patients often have difficulty articulating their symptoms comprehensively, restless legs syndrome (RLS) typically manifests in the thighs, legs, and feet. It can be accompanied by sensations such as tingling, chilling, itching, crushing, and burning in the lower extremities (1, 2). This debilitating condition has affected individuals throughout the history (3). The diagnosis of RLS is difficult as it relies on clinical history, and there are other conditions, such as nocturnal leg cramps and hypnic jerks, that can be mistakenly diagnosed as RLS. However, a comprehensive history and physical examination can help differentiate the condition (3–5).
It is important to recognize that RLS is not solely characterized by its symptoms and severity. RLS is associated with various pregnancy complications, including pregnancy-induced hypertension (6–8), cardiovascular disease (6–9), gestational diabetes (10, 11), sleep disorders (12, 13), poor quality of life, and depression (14–16). These issues can contribute to adverse pregnancy outcomes such as preterm birth (17, 18), miscarriage (19), low birth weight (8, 18), postpartum depression (20), and baby blues (9). Furthermore, RLS increases the risk of recurrence, chronicity, and cardiovascular disease (21, 22). Surprisingly, RLS also elevates the likelihood of anxiety disorders and learning disabilities in offspring (14, 20, 23–25).
The prevalence of RLS has been estimated to range from 3.9 to 15% (22, 26, 27), with 2.5% of adults experiencing symptoms severe enough to require medical intervention (26). Women are two to three times more likely to have RLS compared to men (27–30), and the prevalence may increase to 25% during pregnancy (31).
Factors associated with RLS include female gender, pregnancy, lower socioeconomic status, poor health, low iron levels, and advanced age, comorbidity with Parkinson's disease or psychiatric disorders, and family history of similar disorders (16, 32). During pregnancy, variables such as taking prophylactic iron supplementation (11, 33), a history of premenstrual syndrome (9), chronic diabetes mellitus (21), later gestational age (34), poor sleep quality, stressful life events, and excessive daytime sleepiness (7) have also been associated with RLS.
However, previous studies have yielded inconsistent findings among pregnant women in middle-income countries. Furthermore, restless legs syndrome (RLS) is influenced by various factors such as lifestyle, previous experiences, and the quality of healthcare services received, which can vary significantly among individuals in middle-income countries compared to others. Therefore, the purpose of this systematic review and meta-analysis was to determine the pooled prevalence of RLS and identify the associated factors among pregnant women in middle-income countries.
Methods
Study design and search strategy
This systematic review and meta-analysis utilized published studies to determine the prevalence of RLS and its associated factors among pregnant women in middle-income countries. Various databases including PubMed, EMBASE, Google Scholar, CINAHL, Medline, SCOPUS, and reference lists were searched for relevant articles. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and the Joanna Briggs Institute (JBI) Critical Appraisal Checklist were strictly followed in the review process to assess its quality.
The search for articles was performed with the following MeSH terms “((((((((((((prevalence) OR (magnitude)) OR (level)) AND (predictors)) OR (associated factors)) OR (determinant factors)) AND (restless leg syndrome)) OR (RLS)) OR (Willis-Ekbom disease)) OR (WED)) AND (antepartum)) OR (pregnancy)) OR (prenatal period)”. Boolean operators (AND/OR) were used to combine the different search terms and develop a search syntax. To boost the possibility of finding pertinent empirical research, additional sources (i.e., reference lists of included studies and systematic reviews of published articles) were manually searched. Moreover, the searches were made by combining the abovementioned MeSH term with the names of all countries in middle-income countries.
Study selection and eligibility criteria
Peer-reviewed published articles written in English before April 2023 were included. This review included cross-sectional and case–control studies on RLS among pregnant women. However, case reports, case series, editorials, and studies published as abstracts were excluded. The references of selected articles were also screened to retrieve any additional articles. There were no restrictions on participant characteristics (Figure 1).
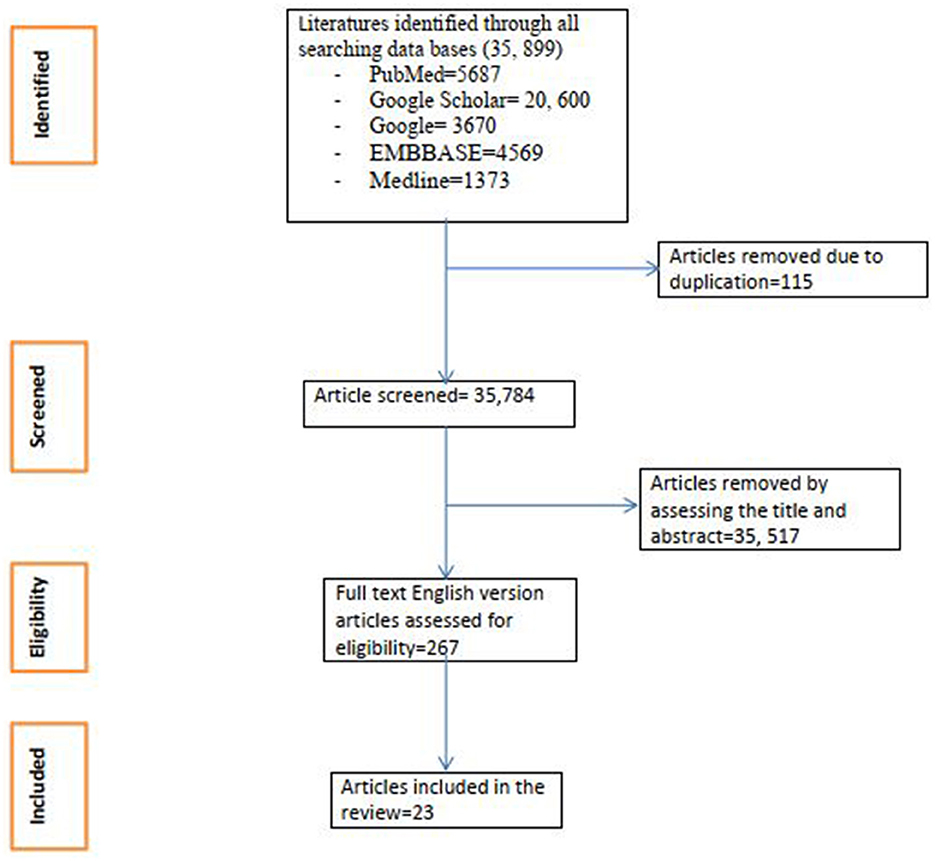
Figure 1. Flow chart of study selection for systematic review and meta-analysis of prevalence and associated factor for restless legs syndrome in middle income countries.
Study outcomes
Prevalence and factors associated with RLS.
Quality assessment
Articles were screened using their titles, abstracts, and full paper reviews prior to inclusion for meta-analysis. All authors assessed the quality of the included articles with the Joanna Briggs Institute (JBI) Critical Appraisal Checklist, which consists of eight total questions. Studies scoring five or more out of eight on the JBI criteria were considered of good quality and included in the review. Discrepancies in the critical appraisal process among authors were resolved through discussion. JBI result of the included studies is available in the Supplementary material.
Data extraction and management
The data extraction tool contained information regarding the author, year of publication, study area and region, study design, study population, sample size, response rate, outcome measured, prevalence, and factors associated with RLS among pregnant women. Furthermore, each author was independently examined, and an agreement was reached among all authors on the titles and abstracts to be incorporated into this review and meta-analysis.
Registration and protocol
This review did not undergo prior registration or protocol preparation. Therefore, no modifications or adjustments were made to the review process.
Heterogeneity and publication bias
The heterogeneity among included studies was assessed by using the I2 statistics, with a p-value < 0.05 indicating the presence of heterogeneity. Based on I2 test statistics findings, heterogeneity among the included studies was categorized as low (25%), moderate (50%), and high (75%). Moreover, publication bias was also assessed using the Egger regression asymmetry test, with a p-value < 0.05 suggesting the presence of publication bias. The Duval and Tweedie non-parametric trim-and-fill analysis was conducted to observe the presence of publication bias using the random-effects analysis.
Data processing and analysis
Data were entered into Microsoft Excel, and the meta-analysis was conducted using STATA 16 software. Forest plots were used to present the results of the meta-analysis. The random-effects model of analysis was used as a method of meta-analysis. Moreover, the meta-analysis regression was conducted to identify the sources of heterogeneity among studies. It was conducted in a classified study setting and region wise in the included studies. Predictors of restless legs syndrome were presented using odds ratios at a 95% confidence interval (CI).
Result
Characteristics of included studies
A total of 23 studies were included in this review. A single study was included from Nigeria (35), Thailand (36), Peru (37), and Brazil (38) each. Two studies were from India (39, 40), three were from Pakistan (41–43), four from Iran (17, 44–46), four from China (7, 8, 47, 48), and five from Turkey (49–53). According to WHO region classification studies included for this review, one was from the African region (35), three from the south-east region (36, 39, 40), five from the European region (49–53), four from the western pacific region (7, 8, 47, 48), two from the American region (37, 38), and eight from the Eastern Mediterranean (EM) region (17, 41–46). The World Bank's classification for lower- and upper-middle-income countries, which was based on the gross national income per capita of the countries (from $1,136 to 4,465, and $4,466 to 13,845, respectively), was utilized (54, 55). Twelve studies (7, 8, 36–38, 47–53) were from upper-middle-income countries, and ten studies were (17, 35, 39–46) from lower-middle-income countries. Except for a case–control study from Iran (56), all others were cross-sectional.
Prevalence of restless legs syndrome among pregnant women
The pooled prevalence of RLS in this review is 13.82 (95% CI: 13.31, 14.32). The I2 test was 96.2% with a p-value < 0.0001, which indicated significant heterogeneity. The forest plot showed the overall and individual effect size of the studies. Publication biases among the included studies were examined by using funnel plots and Egger's regression test. The results of funnel plots showed an asymmetric shape, which indicates the presence of publication bias among included studies. Supplementary Figure 1 contains the funnel plot.
Subgroup analysis
The subgroup analysis was performed based on WHO regions and the World Bank's classification of countries. Table 1 shows the pooled prevalence, and it was found to be the highest in the Eastern Mediterranean region at 22.91% (95% CI: 21.54, 24.27), and lowest in Africa, 4.16 % (95% CI: 2.03, 6.29), based on the WHO region classification. Moreover, subgroup analysis showed that the highest pooled prevalence of RLS was seen in lower-middle-income countries, 17.58 (95% CI: 16.49, 18.67), compared to upper-middle-income countries, 12.80% (95% CI: 12.24, 13.37) (Table 1) (Figure 2). Supplementary Figure 2 contains the forest plot for subgroup analysis based on the WHO region classification.
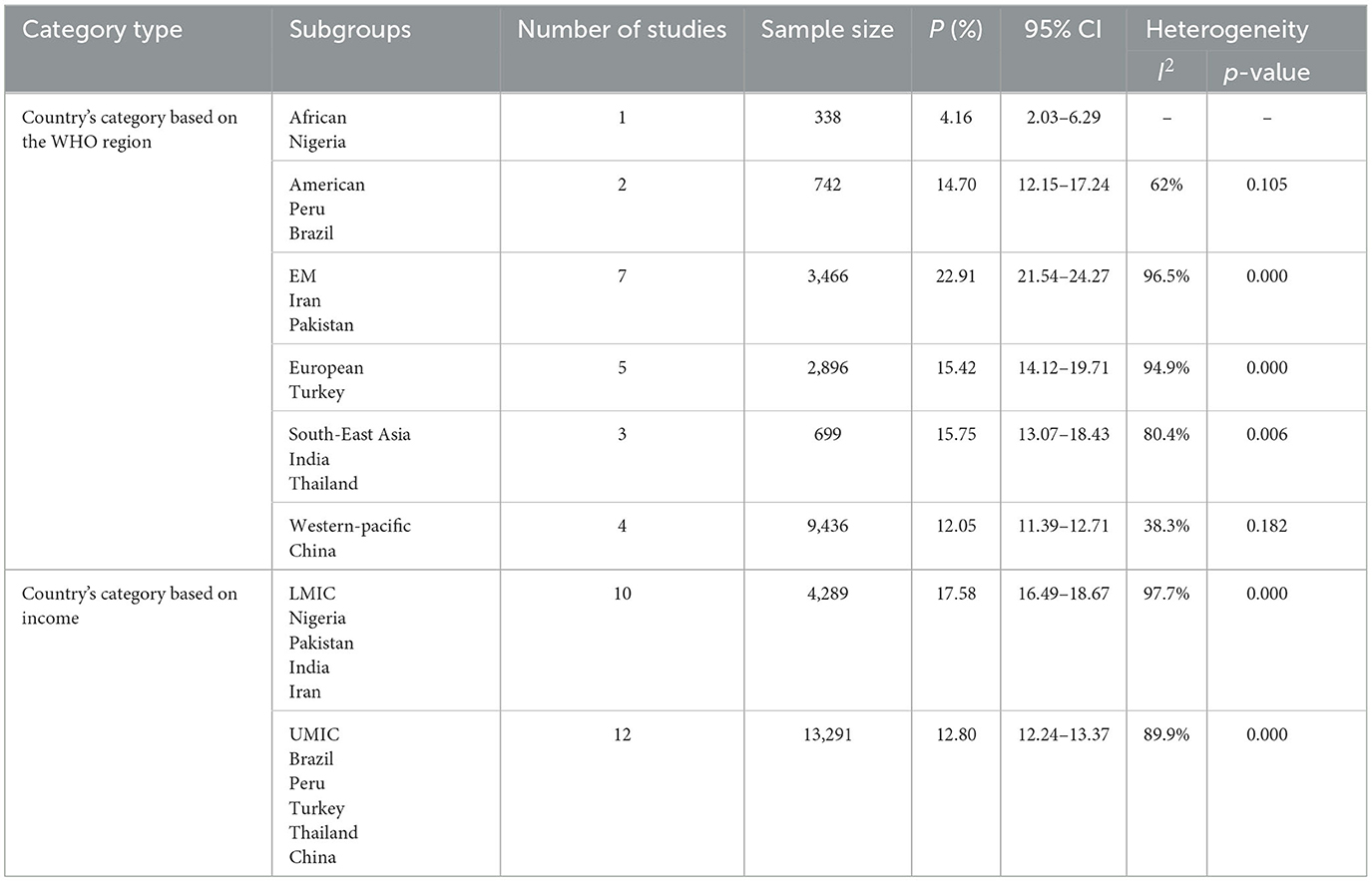
Table 1. Summary of subgroup analysis of the pooled prevalence of RLS among pregnant women in middle-income countries, 2023.
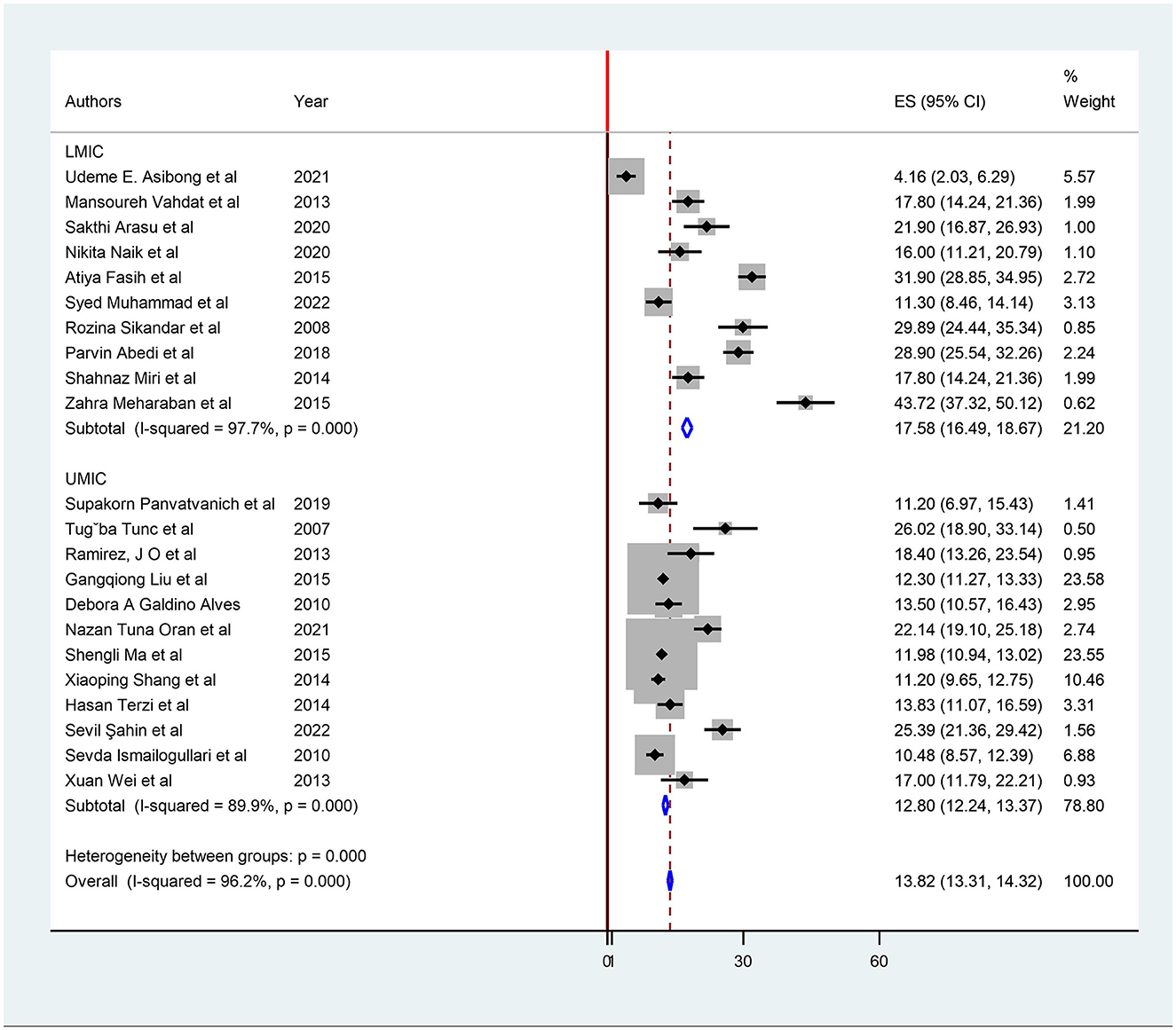
Figure 2. Subgroup analysis based on lower vs. upper middle-income countries for restless legs syndrome prevalence.
Factors associated with restless legs syndrome among pregnant women
In this meta-analysis, pregnant women with low hemoglobin level were 1.68 times (AOR: 1.68, 95% CI: 1.29, 2.18) more likely to have RLS as compared to those with normal hemoglobin level. Similarly, women with history of RLS had 7.54 times (AOR: 7.54, 95% CI: 3.02, 18.79); women with muscle cramps had 3.58 times (AOR: 3.58, 95% CI: 1.21, 10.61); women with excessive daytime sleepiness had 4.02 times (AOR: 4.02, 95% CI: 1.34, 12.04); and women with preeclampsia had 2.06 (AOR: 2.06, 95% CI: 1.28, 3.30) times higher odds of developing RLS as compared to their counterparts. On the contrary, pregnant women who took prophylactic iron supplementation were 41% (AOR: 0.59, 95% CI: 0.50, 0.69) less likely to develop RLS as compared to those who did not take prophylactic iron supplementation (Table 2).
Discussion
The current meta-analysis revealed several factors that were highly and positively associated with RLS during pregnancy. These include having low hemoglobin levels, a history of RLS, muscle cramps, excessive daytime sleepiness, and preeclampsia. However, pregnant women who took prophylactic iron supplementation had a 41% reduced likelihood of developing RLS compared to those who did not take prophylactic iron supplementation.
The pooled prevalence of RLS during pregnancy was found to be 13.82%. This indicates a significantly higher prevalence of RLS among pregnant women compared to the global general population (3%) and among all women (4.7%) (57). The higher prevalence rate can be attributed to various factors such as hormonal differences, pressure on adjacent blood vessels and nerves by the fetus, psychological stressors, lifestyle changes during pregnancy, and physiological changes such as vascular changes and nutrient deficiencies (iron, calcium, and magnesium) (31, 58, 59).
However, the current pooled prevalence of RLS during pregnancy (13.82%) is lower than that reported in a meta-analysis conducted in Iran (32.9%) (60). This difference could be due to variations in the included studies. The Iran meta-analysis included studies conducted on both sexes and different health problems, including patients on hemodialysis (60). Additionally, the prevalence of RLS in middle-income countries is lower than the global prevalence among all trimesters (21%) (61) and the third trimester (22.9%) of pregnancy (34). This difference could be attributed to the difference in the study population as most of the studies included in the worldwide meta-analysis were from high-income countries. This could result in a higher likelihood of diagnosis among affluent women compared to those with comparatively limited access to healthcare, higher stress levels associated with certain lifestyles or occupations, and sedentary lifestyles. Additionally, advanced gestational age among third-trimester pregnant women might have contributed to higher RLS prevalence (45).
This systematic review and meta-analysis identified a significant association between RLS among pregnant women in middle-income countries and hemoglobin levels. Women with low hemoglobin levels were 1.68 times more likely to develop RLS as compared to those with normal hemoglobin levels. Similarly, pregnant women who took prophylactic iron supplementation were 41% less likely to develop RLS compared to those who did not. These findings are consistent with previous studies conducted on RLS and its association with iron and dopamine in mice, pregnant or non-pregnant women, and older adults (31, 58, 62–64).
Furthermore, studies have shown that RLS is related to dysfunction of the dopamine system, particularly in the brain regions that control body movement. Iron also plays a crucial role in the production of dopamine, a neurotransmitter involved in regulating movement and sensations in the body (62–64). Therefore, a lack of iron can impair the production and regulation of dopamine, contributing to the development or worsening of RLS (31, 58). Iron deficiency further exacerbates dysfunction leading to symptoms of RLS like the urge to move the legs, discomfort, and disturbed sleep (64–67). Increasing hemoglobin levels through prophylactic iron supplementation is advisable to restore normal dopamine levels and alleviate the symptoms of RLS in pregnant women (58, 64).
The current study also found that women with a history of RLS were 7.54 times more likely to have RLS in their current pregnancy. This could be due to hormonal fluctuations, especially estrogen and progesterone (31, 58, 68), iron deficiency, increased blood volume, and pressure of the gravid uterus on nerves. These factors might contribute to the recurrence of RLS (68).
Additionally, pregnant woman who experienced muscle cramps had 3.58 times higher odds of having RLS as compared to their counterparts. Although muscle cramps and RLS are two distinct conditions (69–71), they may share some similarities in terms of leg sensations (70, 71). Muscle cramps can occur because of muscle fatigue, dehydration, electrolyte imbalances, or overuse. The association between RLS and muscle cramps could be attributed to abnormal nerve activity, issues with circulation and blood flow, and electrolyte imbalances (low levels of potassium, magnesium, or calcium) (70).
RLS was found to be 4.02 times higher among pregnant women with excessive daytime sleepiness compared to those with normal sleeping patterns. This finding is supported by previous studies, which suggests that women with RLS may have poor sleep quality (72, 73), short duration of sleep at night (73–75), depression, and excessive daytime sleepiness for compensation (72, 76, 77).
Furthermore, pregnant woman with preeclampsia were 2.06 times more likely to develop RLS compared to their counterparts. This could be due to vascular changes and reduced blood flow associated with preeclampsia, which may contribute to the development or worsening of RLS symptoms (78–80). On the other hand, RLS, which is associated with obstructive sleep apnea, can result in the occurrence of preeclampsia by causing apneas or hypopneas, inducing sympathetic activation, endothelial dysfunction, and abnormal placental physiology (50, 81–85). This can be decreased by increasing ventilation and ensuring an open airway through lifestyle modifications, constant positive airway pressure, or other mechanisms based on individual needs (86, 87).
Additionally, a single study reported associations between RLS among pregnant women and various conditions, including poor sleep quality (40), higher Epworth sleep scale scores (7, 8, 36, 37), higher gestational age (45), caffeine consumption (45), smoking (8), hypertension (8), diabetes mellitus (8), gestational hypertension (45), increased wakefulness (48), increased number of children (52), menstrual irregularity before pregnancy (49), history of gynecologic surgery (49), thyroid disease (47), arthritis (47), varicose vein (47), and cesarean section (44).
It is important to acknowledge and consider certain limitations in these findings before generalizing the results. First, there was significant heterogeneity among the included studies, and this heterogeneity was not adequately addressed through subgroup analysis. Even though all studies were done among pregnant women, there was a difference in gestational age and obstetric complications. Additionally, it should be noted that only published articles were considered in this review, which might introduce publication bias. Future studies that explore the relationship between RLS and other factors such as hormonal levels, social functioning, and substance and alcohol use could provide valuable insights for a more comprehensive understanding of the topic.
Conclusion
During pregnancy, approximately one out of every eight women in middle-income countries experience restless legs syndrome (RLS), a higher prevalence compared to the general population. This puts pregnant women at a greater risk for RLS. Various factors have been associated with RLS, such as low hemoglobin levels, a previous history of RLS, muscle cramps, excessive daytime sleepiness, and preeclampsia. However, taking prophylactic iron supplementation has been shown to reduce the likelihood of developing RLS. Therefore, it is crucial to take measures to prevent pre-eclampsia, address muscle cramps, provide prophylactic iron supplementation to prevent anemia, and promote sufficient sleep, thereby decreasing the risk of pregnant women developing RLS. Additionally, it is important to conduct further research and review follow-up studies to determine the prevalence and associated factors of RLS among women in low-income countries.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
EM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. BA: Data curation, Investigation, Methodology, Resources, Writing – original draft. MA: Data curation, Investigation, Methodology, Resources, Visualization, Writing – original draft. FC: Data curation, Investigation, Methodology, Resources, Validation, Writing – original draft. TH: Data curation, Investigation, Methodology, Resources, Supervision, Writing – original draft, Writing – review & editing. LT: Data curation, Formal analysis, Investigation, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. AK: Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. HK: Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1326337/full#supplementary-material
Abbreviations
CI, Confidence interval; RLS, restless legs syndrome; WHO, World Health Organization.
References
1. Sateia MJ. International classification of sleep disorders. Chest. (2014) 146:1387–94. doi: 10.1378/chest.14-0970
2. Jankovic J. International classification of diseases, tenth revison: neurological adaptation (ICD-10 NA): extrapyramidal and movement disorders. Mov Disord. (1995) 10:533–40. doi: 10.1002/mds.870100502
3. Grover A, Clark-Bilodeau C, D'Ambrosio CM. Restless leg syndrome in pregnancy. Obstetr Med. (2015) 8:121–5. doi: 10.1177/1753495X15587452
4. Rana AQ, Khan F, Mosabbir A, Ondo W. Differentiating nocturnal leg cramps and restless legs syndrome. Expert Rev Neurother. (2014) 14:813–8. doi: 10.1586/14737175.2014.927734
5. Sharon D. Restless Legs Syndrome and Movement Disorders, an Issue of Sleep Medicine Clinics. Philadelphia, PA: Elsevier Health Sciences (2015).
6. Innes KE, Kandati S, Flack KL, Agarwal P, Selfe TK. The relationship of restless legs syndrome to history of pregnancy-induced hypertension. J Womens Health. (2016) 25:397–408. doi: 10.1089/jwh.2015.5484
7. Ma S, Shang X, Guo Y, Liu G, Yang J, Xue R. Restless legs syndrome and hypertension in Chinese pregnant women. Neurol Sci. (2015) 36:877–81. doi: 10.1007/s10072-015-2094-4
8. Liu G, Li L, Zhang J, Xue R, Zhao X, Zhu K, et al. Restless legs syndrome and pregnancy or delivery complications in China: a representative survey. Sleep Med. (2015) 17:158–62. doi: 10.1016/j.sleep.2015.02.541
9. Goecke TW, Schnakenberg P, Frensch M, Chechko N. restless legs syndrome during pregnancy and 12 weeks postpartum and its links to cardiovascular diseases, stressful life events, and psychiatric history. J Clin Med. (2020) 9:3046. doi: 10.3390/jcm9093046
10. Innes KE, Kandati S, Flack KL, Agarwal P, Selfe TK. The association of restless legs syndrome to history of gestational diabetes in an Appalachian primary care population. J Clin Sleep Med. (2015) 11:1121–30. doi: 10.5664/jcsm.5084
11. Chechko N, Lefort-Besnard J, Goecke TW, Frensch M, Schnakenberg P, Stickel S, et al. Phenotypical predictors of pregnancy-related restless legs syndrome and their association with basal ganglia and the limbic circuits. Sci Rep. (2021) 11:9996. doi: 10.1038/s41598-021-89360-8
12. Pinheiro T, Thomas T, Devaraj U, Ramachandran P, Krishnaswamy UM. Prevalence of restless legs syndrome and quality of sleep in type 2 diabetics. J Diabetes Comp. (2020) 34:107727. doi: 10.1016/j.jdiacomp.2020.107727
13. Dunietz GL, Lisabeth LD, Shedden K, Shamim-Uzzaman QA, Bullough AS, Chames MC, et al. Restless legs syndrome and sleep-wake disturbances in pregnancy. J Clin Sleep Med. (2017) 13:863–70. doi: 10.5664/jcsm.6654
14. Bogan RK. Effects of restless legs syndrome (RLS) on sleep. Neuropsychiatr Dis Treat. (2006) 2:513–9. doi: 10.2147/nedt.2006.2.4.513
15. Sönmez A, Aksoy Derya Y. Effects of sleep hygiene training given to pregnant women with restless leg syndrome on their sleep quality. Sleep Breath. (2018) 22:527–35. doi: 10.1007/s11325-018-1619-5
16. Yeh P, Walters AS, Tsuang JW. Restless legs syndrome: a comprehensive overview on its epidemiology, risk factors, and treatment. Sleep Breath. (2012) 16:987–1007. doi: 10.1007/s11325-011-0606-x
17. Meharaban Z, Yahya S, Sadegniiat K. Restless legs syndrome during pregnancy and preterm birth in women referred to health centers of Ardabil. Iran Red Crescent Med J. (2015) 17:e24438. doi: 10.5812/ircmj.24438
18. Oyieng'o DO, Kirwa K, Tong I, Martin S, Antonio Rojas-suarez J, Bourjeily G. Restless legs symptoms and pregnancy and neonatal outcomes. Clin Ther. (2016) 38:256–64. doi: 10.1016/j.clinthera.2015.11.021
19. Yildirim E, Apaydin H. Zinc and magnesium levels of pregnant women with restless leg syndrome and their relationship with anxiety: a case-control study. Biol Trace Elem Res. (2021) 199:1674–85. doi: 10.1007/s12011-020-02287-5
20. Sarberg M, Bladh M, Svanborg E, Josefsson A. Postpartum depressive symptoms and its association to daytime sleepiness and restless legs during pregnancy. BMC Pregn Childbirth. (2016) 16:137. doi: 10.1186/s12884-016-0917-9
21. Ning P, Mu X, Yang X, Li T, Xu Y. Prevalence of restless legs syndrome in people with diabetes mellitus: a pooling analysis of observational studies. EClinicalMedicine. (2022) 46:101357. doi: 10.1016/j.eclinm.2022.101357
22. Joseph N, Suresh S, Prasad S, Malwee S, Brittas A, Gupta V. Study on restless leg syndrome and its relationship with quality of sleep among the general population of Mangalore, India. Egypt J Neurol Psychiatr Neurosurg. (2022) 58:109. doi: 10.1186/s41983-022-00544-z
23. Emmanuel EN, Sun J. Health related quality of life across the perinatal period among Australian women. J Clin Nurs. (2014) 23:1611–9. doi: 10.1111/jocn.12265
24. Jemere T, Getahun B, Tadele F, Kefale B, Walle G. Poor sleep quality and its associated factors among pregnant women in Northern Ethiopia, 2020: a cross sectional study. PLoS ONE. (2021) 16:e0250985. doi: 10.1371/journal.pone.0250985
25. Silvestri R, Aricò I. Sleep disorders in pregnancy. Sleep Sci. (2019) 12:232. doi: 10.5935/1984-0063.20190098
26. Maurice M, Ohayon A, Ruth O. Epidemiology of restless legs syndrome: a synthesis of the literature. Sleep Med Rev. (2012) 16:283–95. doi: 10.1016/j.smrv.2011.05.002
27. Allen RP, Walters AS, Montplaisir J, Hening W, Myers A, Bell TJ, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med. (2005) 165:1286–92. doi: 10.1001/archinte.165.11.1286
28. Berger K, Luedemann J, Trenkwalder C, John U, Kessler C. Sex and the risk of restless legs syndrome in the general population. Arch Intern Med. (2004) 164:196–202. doi: 10.1001/archinte.164.2.196
29. Bjorvatn B, Leissner L, Ulfberg J, Gyring J, Karlsborg M, Regeur L, et al. Prevalence, severity and risk factors of restless legs syndrome in the general adult population in two Scandinavian countries. Sleep Med. (2005) 6:307–12. doi: 10.1016/j.sleep.2005.03.008
30. Didriksen M, Rigas AS, Allen RP, Burchell BJ, Di Angelantonio E, Nielsen MH, et al. Prevalence of restless legs syndrome and associated factors in an otherwise healthy population: results from the Danish Blood Donor Study. Sleep Med. (2017) 36:55–61. doi: 10.1016/j.sleep.2017.04.014
31. Srivanitchapoom P, Pandey S, Hallett M. Restless legs syndrome and pregnancy: a review. Parkinsonism Relat Disord. (2014) 20:716–22. doi: 10.1016/j.parkreldis.2014.03.027
32. Weber FC, Danker-Hopfe H, Dogan-Sander E, Frase L, Hansel A, Mauche N, et al. Restless legs syndrome prevalence and clinical correlates among psychiatric inpatients: a multicenter study. Front Psychiatry. (2022) 13:846165. doi: 10.3389/fpsyt.2022.846165
33. Benson AE, Shatzel JJ. The incidence, complications, and treatment of iron deficiency in pregnancy. Eur J Haematol. (2022) 109:633–42. doi: 10.1111/ejh.13870
34. Darvishi N, Daneshkhah A, Khaledi-Paveh B, Vaisi-Raygani A, Mohammadi M, Salari N, et al. The prevalence of Restless Legs Syndrome/Willis-ekbom disease (RLS/WED) in the third trimester of pregnancy: a systematic review. BMC Neurol. (2020) 20:1–7. doi: 10.1186/s12883-020-01709-0
35. Asibong UE, Akpan UB, Chidi O, Ekpenyong E, Asibong I, Etuk S. The prevalence, pattern, and predictors of sleep disorders among pregnant women attending antenatal clinic in a Southern Nigerian City. Niger J Med. (2021) 30:687–92. doi: 10.4103/NJM.NJM_60_21
36. Panvatvanich S, Lolekha P. Restless legs syndrome in pregnant Thai women: prevalence, predictive factors, and natural course. J Clin Neurol. (2019) 15:97–101. doi: 10.3988/jcn.2019.15.1.97
37. Ramirez J, Cabrera S, Hidalgo H, Cabrera S, Linnebank M, Bassetti C, et al. Is preeclampsia associated with restless legs syndrome? Sleep Med. (2013) 14:894–6. doi: 10.1016/j.sleep.2013.03.013
38. Alves DAG, de Carvalho LBC, de Morais JF, do Prado GF. Restless legs syndrome during pregnancy in Brazilian women. Sleep Med. (2010) 11:1049–54. doi: 10.1016/j.sleep.2010.06.006
39. Naik N, Polen Z. Prevalence of restless leg syndrome in pregnancy. Int J Health Sci Res. (2020) 10:50–4.
40. Arasu S, Angeline N, Steephan S, Shekhar V, Sebastian S, Ramesh N. Sleep quality and restless leg syndrome among antenatal women attending government healthcare facilities in urban bangalore. J Fam Med Prim Care. (2020) 9:3630. doi: 10.4103/jfmpc.jfmpc_81_20
41. Fasih A, Abdullah KN, Iqbal S. Obstetric restless legs syndrome in industrialized area of Pakistan. J Bahria Univ Med Dental College. (2015) 5:69–72. Retrieved from: https://jbumdc.bahria.edu.pk/index.php/ojs/article/view/114
42. Mubeen SM, Ahsan MD. Prevalence and associated factors of restless leg syndrome (RLS) in Pakistani women during pregnancy. J Obstet Gynaecol. (2022) 42:1829–34. doi: 10.1080/01443615.2022.2040963
43. Sikandar R, Khealani BA, Wasay M. Predictors of restless legs syndrome in pregnancy: a hospital based cross sectional survey from Pakistan. Sleep Med. (2009) 10:676–8. doi: 10.1016/j.sleep.2008.06.011
44. Vahdat M, Sariri E, Miri S, Rohani M, Kashanian M, Sabet A, et al. Prevalence and associated features of restless legs syndrome in a population of Iranian women during pregnancy. Int J Gynecol Obstetr. (2013) 123:46–9. doi: 10.1016/j.ijgo.2013.04.023
45. Abedi P, Bagheri R, Qorbani M, Ansari S. Is there a relationship between restless legs syndrome and medical problems in pregnant women? A cross-sectional study in Iran. Acta Neurologica Belgica. (2020) 120:1091–6. doi: 10.1007/s13760-018-01062-7
46. Miri S, Rohani M, Vahdat M, Kashanian M, Sariri E, Zamani B, et al. Presenting features of idiopathic versus secondary restless legs syndrome in pregnancy. Iran J Neurol. (2014) 13:241–4.
47. Shang X, Yang J, Guo Y, Ma S, Jia Z, Xue R. Restless legs syndrome among pregnant women in China: prevalence and risk factors. Sleep Breath. (2015) 19:1093–9. doi: 10.1007/s11325-014-1089-3
48. Wei X, Yang L, Tang X. Survey on restless legs syndrome in pregnant Chinese women. Sleep Biol Rhythms. (2013) 11:286–7. doi: 10.1111/sbr.12035
49. Sahin S, Guler D, Özdemir K, Unsal A. An assessment of restless legs syndrome and sleep quality in pregnant women. Cyprus J Med Sci. (2022) 7:2800. doi: 10.4274/cjms.2020.2800
50. Terzi H, Terzi R, Zeybek B, Ergenoglu M, Hacivelioglu S, Akdemir A, et al. Restless legs syndrome is related to obstructive sleep apnea symptoms during pregnancy. Sleep Breath. (2015) 19:73–8. doi: 10.1007/s11325-014-0964-2
51. Tunç T, Karadag YS, Dogulu F, Inan LE. Predisposing factors of restless legs syndrome in pregnancy. Mov Disord. (2007) 22:627–31. doi: 10.1002/mds.21291
52. Ismailogullari S, Ozturk A, Mazicioglu MM, Serin S, Gultekin M, Aksu M. Restless legs syndrome and pregnancy in Kayseri, Turkey: a hospital based survey. Sleep Biol Rhythms. (2010) 8:137–43. doi: 10.1111/j.1479-8425.2010.00437.x
53. Tuna Oran N, Yuksel E, Ruzgar S. Prevalence of restless leg syndrome and effects on quality of life during pregnancy. Sleep Breath. (2021) 25:2127–34. doi: 10.1007/s11325-021-02311-5
56. Vahed A, Kordi M, Rezaeitalab F, Mazlom R, Lotfalizadeh M, Asgharipour N. Relationship between pre-eclampsia and restless legs syndrome: a case-control study. J Mazandaran Univ Med Sci. (2016) 26:26–35.
57. Broström A, Alimoradi Z, Lind J, Ulander M. Worldwide estimation of restless legs syndrome: a systematic review and meta-analysis of prevalence in the general adult population. J Sleep Res. (2023) 32:e13783. doi: 10.1111/jsr.13783
58. Khan FH, Ahlberg CD, Chow CA, Shah DR, Koo BB. Iron, dopamine, genetics, and hormones in the pathophysiology of restless legs syndrome. J Neurol. (2017) 264:1634–41. doi: 10.1007/s00415-017-8431-1
59. Mendes A, Silva V. Possible etiologies of restless legs syndrome in pregnancy: a narrative review. Sleep Sci. (2022) 15:471–9. doi: 10.5935/1984-0063.20220080
60. Sorbi MH, Issazadegan A, Soleimani E, Mirhosseini H. Prevalence of restless legs syndrome in Iran: a systematic review and meta-analysis. J Commun Health Res. (2020) 9:191–202. doi: 10.18502/jchr.v9i3.4262
61. Chen S-J, Shi L, Bao Y-P, Sun Y-K, Lin X, Que J-Y, et al. Prevalence of restless legs syndrome during pregnancy: a systematic review and meta-analysis. Sleep Med Rev. (2018) 40:43–54. doi: 10.1016/j.smrv.2017.10.003
62. Pino JMV, da Luz MHM, Antunes HKM, Giampá SQC, Martins VR, Lee KS. Iron-restricted diet affects brain ferritin levels, dopamine metabolism and cellular prion protein in a region-specific manner. Front Mol Neurosci. (2017) 10:145. doi: 10.3389/fnmol.2017.00145
63. Matak P, Matak A, Moustafa S, Aryal DK, Benner EJ, Wetsel W, et al. Disrupted iron homeostasis causes dopaminergic neurodegeneration in mice. Proc Nat Acad Sci USA. (2016) 113:3428–35. doi: 10.1073/pnas.1519473113
64. Guo S, Huang J, Jiang H, Han C, Li J, Xu X, et al. Restless legs syndrome: from pathophysiology to clinical diagnosis and management. Front Aging Neurosci. (2017) 9:171. doi: 10.3389/fnagi.2017.00171
65. Salminen A. Peripheral hypoxia and autonomic responses in restless legs syndrome. (2015). Available online at: https://trepo.tuni.fi/handle/10024/96762
66. Louis EKS, Ulfberg J. Putting the legs back into restless legs syndrome. New Evid Microvasc Hypothesis. (2014) 82:1850–1. doi: 10.1212/WNL.0000000000000462
67. Salminen AV, Rimpilä V, Polo O. Peripheral hypoxia in restless legs syndrome (Willis-Ekbom disease). Neurology. (2014) 82:1856–61. doi: 10.1212/WNL.0000000000000454
68. Gupta R, Dhyani M, Kendzerska T, Pandi-Perumal SR, BaHammam AS, Srivanitchapoom P, et al. Restless legs syndrome and pregnancy: prevalence, possible pathophysiological mechanisms and treatment. Acta Neurol Scand. (2016) 133:320–9. doi: 10.1111/ane.12520
69. Tipton PW, Wszołek ZK. Restless legs syndrome and nocturnal leg cramps: a review and guide to diagnosis and treatment. Pol Arch Intern Med. (2017) 127:865–72. doi: 10.20452/pamw.4148
70. Hensley JG. Leg cramps and restless legs syndrome during pregnancy. J Midwif Womens Health. (2009) 54:211–8. doi: 10.1016/j.jmwh.2009.01.003
71. Allen RP, Picchietti DL, Garcia-Borreguero D, Ondo WG, Walters AS, Winkelman JW, et al. Restless legs syndrome/Willis–Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria–history, rationale, description, and significance. Sleep Med. (2014) 15:860–73. doi: 10.1016/j.sleep.2014.03.025
72. Cederberg KL, Brinkley EB, Belotserkovkaya N, Memon RA, Motl RW, Amara AW. Does restless legs syndrome impact cognitive function via sleep quality in adults with Parkinson's disease? Int J Neurosci. (2020) 130:322–9. doi: 10.1080/00207454.2019.1681423
73. Say B, Hamamci M, Ergün U. Assessment of sleep quality in spouses of patients with restless legs syndrome; are they also restless at night? Sleep Biol Rhythms. (2021) 19:113–9. doi: 10.1007/s41105-020-00294-6
74. Allen RP, Stillman P, Myers AJ. Physician-diagnosed restless legs syndrome in a large sample of primary medical care patients in western Europe: prevalence and characteristics. Sleep Med. (2010) 11:31–7. doi: 10.1016/j.sleep.2009.03.007
75. Shamekh AH, Hassan NZ, Rashwan ZI, Fathalla NF. Effect of stretching exercises versus thermotherapy on restless legs syndrome symptoms, pain, and quality of sleep among pregnant women. Int J Health Sci. (2022) 6:11204–20. doi: 10.53730/ijhs.v6nS6.13109
76. Sun S, Qiu J, Ren J, Zhao X, Jiang Y, Wang R, et al. Association between leg motor restlessness and depression among Chinese males living at high-altitude: the mediating role of insomnia. Sleep Breath. (2021) 25:979–87. doi: 10.1007/s11325-020-02156-4
77. Akmaz O, Koskderelioglu A, Eskut N, Sahan B, Kusbeci T. Restless legs syndrome in multiple sclerosis is related to retinal thinning. Photodiagnosis Photodyn Ther. (2022) 40:103169. doi: 10.1016/j.pdpdt.2022.103169
78. Koh SY, Kim MS, Lee SM, Hong JM, Yoon JH. Impaired vascular endothelial function in patients with restless legs syndrome: a new aspect of the vascular pathophysiology. J Neurol Sci. (2015) 359:207–10. doi: 10.1016/j.jns.2015.10.041
79. Kim MS, Park DG, Yoon JH. Impaired endothelial function may predict treatment response in restless legs syndrome. J Neural Transm. (2019) 126:1051–9. doi: 10.1007/s00702-019-02031-x
80. Oskarsson E, Wåhlin-Larsson B, Ulfberg J. Reduced daytime intramuscular blood flow in patients with restless legs syndrome/W illis–E kbom disease. Psychiatry Clin Neurosci. (2014) 68:640–3. doi: 10.1111/pcn.12170
81. Tantrakul V, Ingsathit A, Liamsombut S, Rattanasiri S, Kittivoravitkul P, Imsom-Somboon N, et al. Treatment of obstructive sleep apnea in high risk pregnancy: a multicenter randomized controlled trial. Respir Res. (2023) 24:171. doi: 10.1186/s12931-023-02445-y
82. Jaimchariyatam N, Na-Rungsri K, Tungsanga S, Lertmaharit S, Lohsoonthorn V, Totienchai S. Obstructive sleep apnea as a risk factor for preeclampsia-eclampsia. Sleep Breath. (2019) 23:687–93. doi: 10.1007/s11325-018-1758-8
83. Ryu G, Kim YM, Lee KE, Choi SJ, Hong SD, Jung YG, et al. Obstructive sleep apnea is associated with late-onset preeclampsia in overweight pregnant women in Korea. J Korean Med Sci. (2023) 38:e8. doi: 10.3346/jkms.2023.38.e8
84. Bazalakova M. Sleep disorders in pregnancy. Semin Neurol. (2017) 37:661–8. doi: 10.1055/s-0037-1608843
85. Almeneessier AS, Alangari M, Aldubayan A, Alsharidah A, Altaki A, Olaish AH, et al. Prevalence of symptoms and risk of obstructive sleep apnea in Saudi pregnant women. Ann Thorac Med. (2020) 15:163–70. doi: 10.4103/atm.ATM_59_20
86. Gordon P, Sanders MH. Sleep 7: positive airway pressure therapy for obstructive sleep apnoea/hypopnoea syndrome. Thorax. (2005) 60:68. doi: 10.1136/thx.2003.007195
Keywords: restless legs syndrome, systematic review, meta-analysis, sleep quality, RLS
Citation: Mislu E, Assalfew B, Arage MW, Chane F, Hailu T, Tenaw LA, Kidie AA and Kumsa H (2023) Prevalence and factors associated with restless legs syndrome among pregnant women in middle-income countries: a systematic review and meta-analysis. Front. Med. 10:1326337. doi: 10.3389/fmed.2023.1326337
Received: 23 October 2023; Accepted: 28 November 2023;
Published: 21 December 2023.
Edited by:
Félix Javier Jiménez-Jiménez, Hospital Universitario del Sureste, SpainReviewed by:
Abdulghani Sankari, Wayne State University, United StatesLucia Muntean, Paracelsus Elena Klinik Kassel, Germany
Copyright © 2023 Mislu, Assalfew, Arage, Chane, Hailu, Tenaw, Kidie and Kumsa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Esuyawkal Mislu, esuyawkalmislu@gmail.com
 Esuyawkal Mislu
Esuyawkal Mislu Betel Assalfew1
Betel Assalfew1  Mulugeta Wodaje Arage
Mulugeta Wodaje Arage Tilahun Hailu
Tilahun Hailu Lebeza Alemu Tenaw
Lebeza Alemu Tenaw Atitegeb Abera Kidie
Atitegeb Abera Kidie