Corrected evaluation of the breech presentation outcome based on etiology of this presentation in congenitally malformed uterus
- 1Department of Neurology, University Clinical Center of Vojvodina, Novi Sad, Serbia
- 2Faculty of Medicine, University of Novi Sad, Novi Sad, Serbia
- 3Department of Pharmacology, Toxicology and Clinical Pharmacology, Faculty of Medicine, University of Novi Sad, Novi Sad, Serbia
- 4Department of Obstetrics and Gynecology, University Clinical Center of Vojvodina, Novi Sad, Serbia
- 5Department of Psychology, Faculty of Medicine, University of Novi Sad, Novi Sad, Serbia
- 6Centrum Medical Center, Ottawa, ON, Canada
- 7Institute for Biological Research “Sinisa Stankovic“, National Institute of the Republic of Serbia, University of Belgrade, Belgrade, Serbia
Background: Breech presentation (BP) results from at random filling of the intrauterine cavity, with an equal probability for a BP or cephalic presentation (CP). Each fetus in BP has its “pair” in CP randomly assumed CP. Direct comparison of BP and CP makes bias to less expressed differences between these two groups. It is therefore necessary to subtract the number of fetuses/newborns from the CP set that are identical to the number of fetuses/newborns in the BP set, with identical characteristics, and add this group to the BP set before comparing them to the rest of the CP fetuses/newborns in the matching process.
Methods: The procedure encompasses nine variables in pregnancies with a congenitally malformed uterus (CMU) identified at the Department of Obstetrics (1985–2014): gestational age, birth mass, birth length, head circumference, shoulders circumference, umbilical length, placental weight, newborn mass/newborn length ratio, and newborn mass/placental mass ratio. Firstly, the probability of BP was determined and its relation to gestational age, physical characteristics, and previous presentations. Then direct comparison as well as case–control matching of the CP and BP were performed. Case–control matching was based on either a single specific variable (M1) or all combined variables (M2).
Findings: 462 deliveries were identified with CMU. In 81 cases of multiparity, a fetal presentation was found to be an independent event regardless of the previous presentation, gestational age, and newborn physical characteristics. In four types of CMU with 337 deliveries (Bicornuate, Didelphys, Unicornuate, Arcuate), 9 variables with 36 instances of comparison were observed. M1 in 10 instances and M2 in 6 instances showed a statistically significant lower value of breech/random presentation compared with CP. CP have lower value in 2 instances in M1 and 1 in M2. Statistically significant differences were absent without the matching process.
Interpretations: The study confirms the maximum probability for the BP is 50%. The case–control matching procedure shows that it is able to detect the difference between the breech/random presentation and CP, while the classic method of direct comparison was unable to detect any differences. The outcome of the breech/random presentation in CMU should be evaluated with the described case–control matching procedure.
Introduction
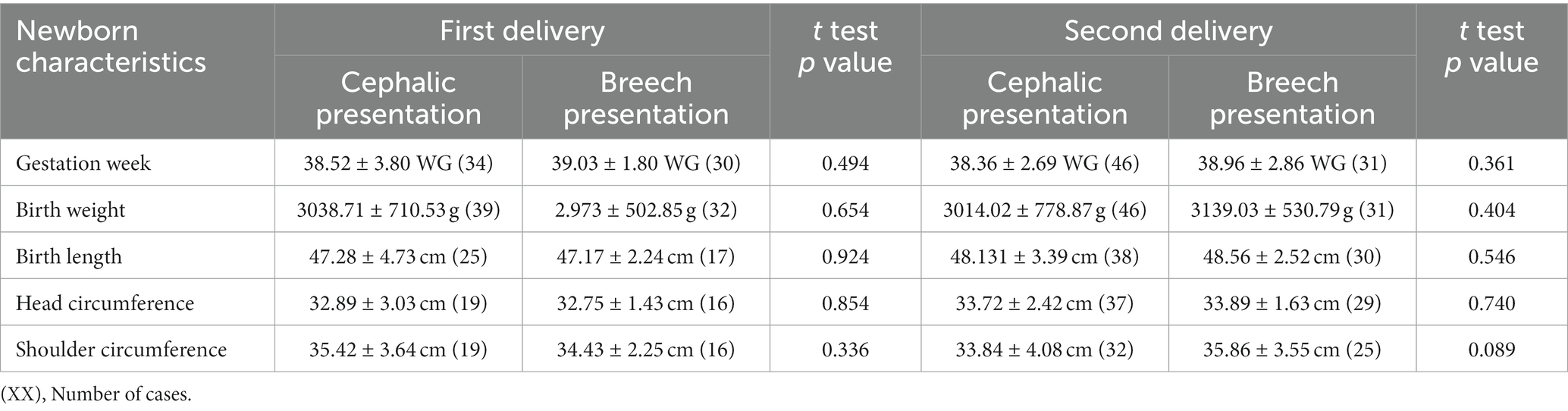
In a breech presentation, the fetus lies longitudinally with its buttocks, knees or feet positioned in the isthmic part of the uterus while its head is in the fundal region. Up to the 24th week of gestation, the fetus frequently changes its presentation, and incidences of breech and cephalic presentation are equal. From the 24th to the 36th week of gestation, there is an increase in cephalic presentation with a proportional decrease in breech presentation (1–4). The probability for definitive presentation appears and increases during this period (5–7). After the 36th week of gestation, the incidence of breech (3%) as well as cephalic (96%) presentation remains mainly unchanged (1–6) (Figure 1).
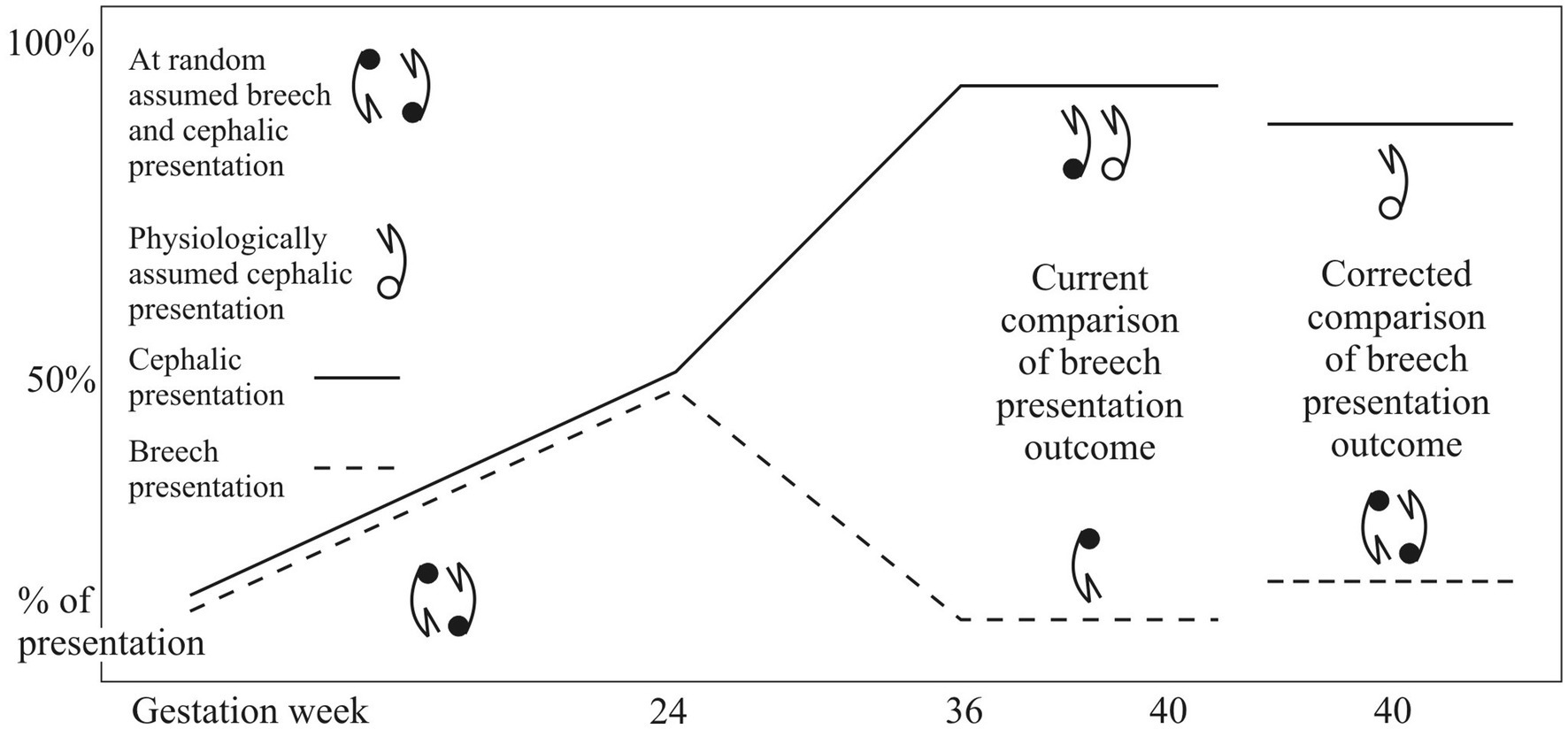
Figure 1. Incidences of fetal presentations during gestation in the general population, etiological mechanisms of the fetal presentations and outcome evaluations of the breech presentation.
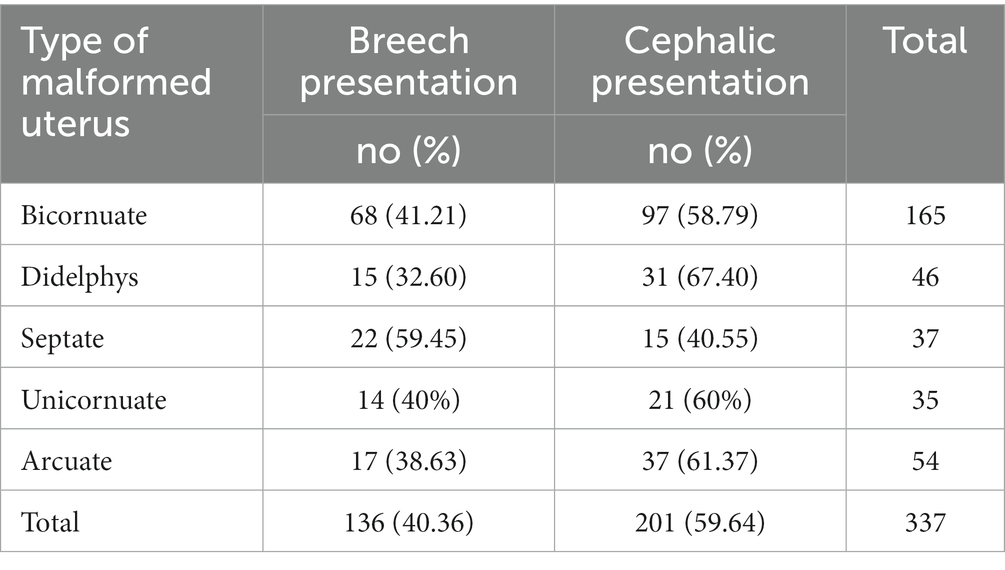
So far, the outcome of gestations with breech-presenting fetuses has been evaluated based on data obtained by directly comparing the breech and cephalic groups. This current method of comparison was introduced prior to the probability of breech presentation was determined. For example, a study of more than 50 known diseases and medical conditions with the incidence of breech presentation higher than the one which occurs in the general population, revealed that the probability of breech presentation is located within the interval between 3% and 50% (8, 9). The largest part of these medical entities is shown in Figure 2.
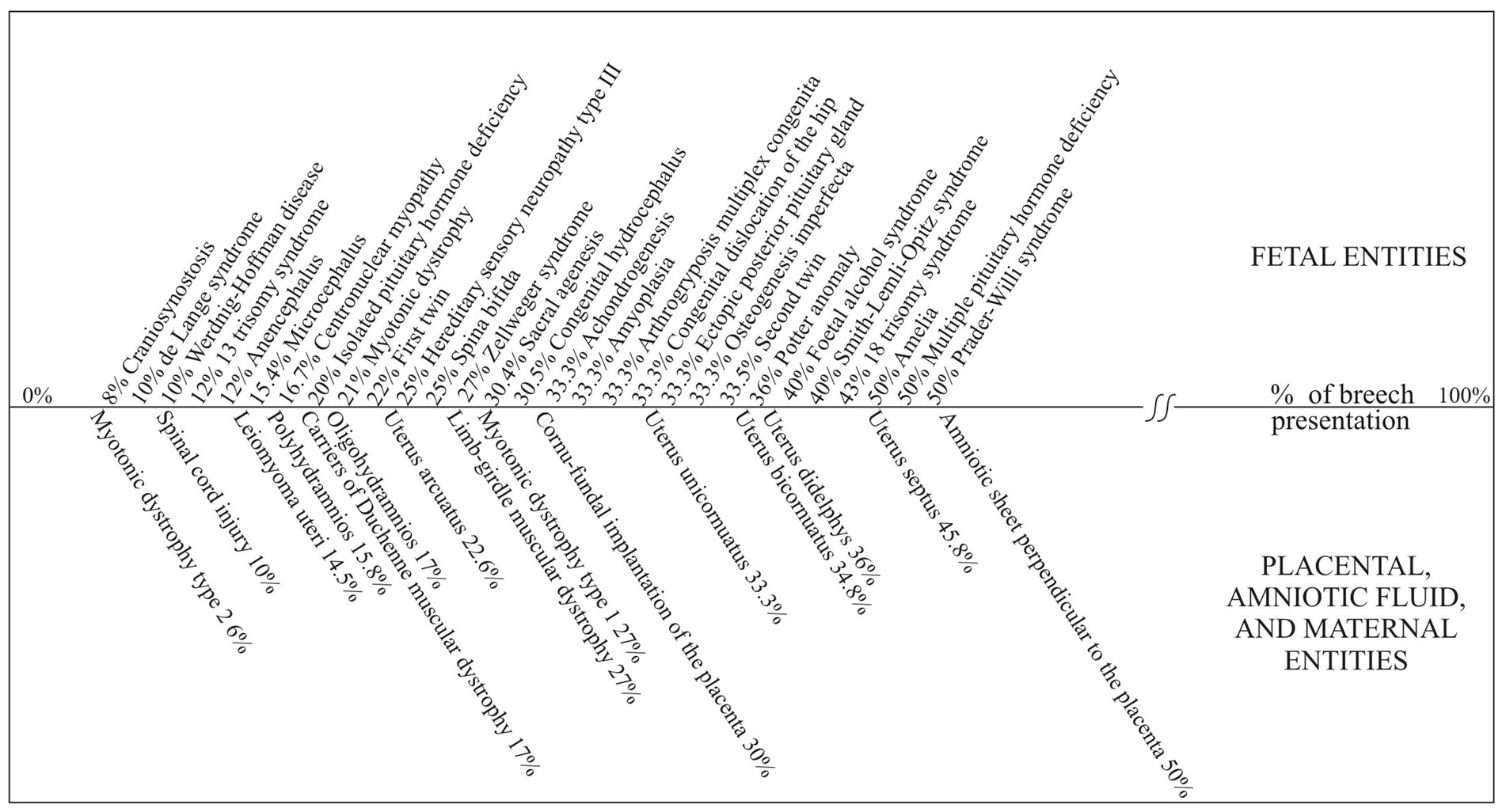
Figure 2. Incidence of breech presentation among various medical entities. Data in figure are from references (7–11).
The highest possible probability, which is 50% for a breech presentation, shows that it results from a random event, whether the fetus randomly changes between breech and cephalic presentation, or arranges its body parts in the space available. For example, a fetus could assume either a breech or a cephalic presentation in a longitudinally elongated uterus. Therefore, each fetus in a breech presentation has its ‘pair’, which has randomly assumed a cephalic presentation (8, 9). When the incidence of breech presentation is 50%, all fetuses in the breech and cephalic-presenting groups have assumed their presentation randomly. However, when the probability of breech presentation is less than 50%, then the group of cephalic-presenting fetuses is heterogeneous. Some fetuses from this group have assumed a cephalic presentation randomly, while others assume a cephalic presentation as a part of the physiological process, resulting in the majority of the fetuses assuming a cephalic presentation at delivery. The mechanism of this physiological process is still unknown (8, 9).
Compared to cephalic presenting newborns of the same gestational age, breech presenting newborns have: 1. Smaller body lengths (12, 13), 2. Lower body weights (12–14), and 3. Increased proportions of small for gestational age newborns (14, 15). In addition, there are reports of decreased placental weights (12, 13), lower fetal-to-placenta ratio (12), shorter umbilical cords (16), and an increased incidence of congenital malformations (12, 17) in the breech presenting group.
The heterogeneity of the cephalic-presenting group raises the question concerning the validity of the direct comparisons of breech- and cephalic-presenting fetuses/newborns. For example, in the group of fetuses that randomly assume a cephalic presentation, there is an increased incidence of the above-mentioned diseases and medical conditions for the same reason that applies to breech presentation. This makes the difference between the breech-presenting and the cephalic-presenting fetuses/newborns smaller than it should be. The mode of delivery does not influence the physical characteristics of the fetus or the placenta, nor on the inherited and acquired fetal diseases before delivery (8, 9).
Before making a comparison, bias should be eliminated by subtracting from the cephalic presenting group the number of fetuses/newborns with identical characteristics to the number of fetuses/newborns in the breech presentation. This subtracted group of cephalic presenting fetuses/newborns should be added to the breech presenting group before being compared with the rest of the cephalic presenting fetuses/newborns (Figure 1) (8, 9).
To test this new concept, we chose the pregnancies complicated with a congenitally malformed uterus in relation to the characteristics of the newborn and the placenta that are not affected by the delivery. Congenital malformations of the uterus allowed for testing the probability of a breech presentation in repeated pregnancies/deliveries under the same conditions.
The aims of this study were, first, to confirm that breech presentation is a consequence of the random filling of the intrauterine cavity with equal probability for breech and cephalic presentation in CMU. Second, to show that the classical method of direct comparison of the breech and cephalic group has bias towards the less expressed differences between these two groups.
The assumptions are as followed: 1. Maximum probability of breech presentation in CMU is 50%. 2. The new method of comparison for the outcome of breech and cephalic presentations will show a more expressed difference than the classic method for comparison. 3. Using the new method of comparison, there will be differences between the breech and cephalic groups that were not present with the classic method for comparison.
Materials and methods
Study population
The research was conducted at the Department of Gynecology and Obstetrics, University Clinical Center of Novi Sad. In accordance with the Helsinki declaration, the study was approved by the Ethical Committee of the Univesity Clinical Center of Vojvodina 00-5/299 – date of issue: May 7, 2015. This was a retrospective cohort study. It included the period from January 1, 1985 to December 31, 2014. The study consisted of all consecutive singleton pregnancies with the following congenital uterine anomalies: septate, unicornuate, bicornuate, didelphys, and arcuate uterus. Congenital uterine anomalies were diagnosed by: hysterosalpingography, ultrasonography, hysterosonography, hysteroscopy, laparoscopy, laparotomy, and magnetic resonance imaging. Each pregnancy was considered an individual case. Because of the study’s retrospective nature, informed consent from patients was unnecessary.
The exclusion criteria was absence of data on the type of the malformed uterus, absence of data on the presentation at delivery, previously performed uteroplastic intervention, presence of myoma uteri, intrauterine adhesions, twin pregnancies, and severe congenital fetal malformations.
The study did not include a control group of infants from noncomplicated cases of cephalic presentation. Regarding the absence of CMU in this group, the matching procedure is not justified.
Data collection
Data was acquired by reviewing the history of disease and birth protocols. Besides the patient’s full name, they were identified according to their unique personal number. This way, last name changes did not influence the patient’s identification. Data registered was related to the type of the malformed uterus; presentation at birth; gestational age; newborn mass, length, head circumference, shoulder circumference, umbilical length, and placental weight. From the obtained data, two new values were calculated: newborn mass/newborn length ratio and newborn mass/placental mass ratio. Five cohorts were formed. Each cohort represented a particular type of congenitally malformed uterus: uterus didelphis, uterus bicornis, uterus unicornis, uterus arcuatus, and uterus duplex.
Definitions
Classification of uterine anomalies was made according to the American Fertility Society classification (18). Gestational age at delivery was determined by the last menstrual period and was verified based on the newborn’s neural and physical maturity characteristics.
Statistical analysis
The IBM SPSS Statistics for Windows, version 23.0, was used for all the analyses (IBM Corp., Armonk, NY, United States). The data set was analysed for normality and outliers using normal plots, with tests and histograms. Samples with values greater than 3 standard deviations than the mean gestational age were removed from further analysis. Cases with extremely low gestational ages were excluded as they affected all other continuous variables of the fetus. They small number produce heterogeneity of the group. After the statistical analysis was done, the two-tailed Fisher’s exact probability or the Pearson Chi-Square test with Yates’s correction for continuity was used to compare the categorical variables between the two groups. McNemar’s test was performed to establish the relationship between the first and the second birth presentation. The Student’s t-test or the Mann–Whitney U test was employed to compare continuous variables. The case–control matching procedure was applied to randomly match cases in two different methods. The case–control matching procedure for both means encompassed the following variables: gestational age, birth mass, length, head circumference, shoulders circumference, umbilicus length, placental weight, newborn mass/newborn length ratio, and newborn mass/placental mass ratio. The difference was that in the first procedure, matching cases was based on a single specific variable (M1), and in the second, matching was based on all combined variables (M2). Furthermore, each variable had a tolerance factor (fuzz factor) of 1.5 SD. SPSS options “Give priority to exact matches” and “Maximize execution performance” were applied, while “Randomize case order when drawing matches” was not used. Afterwards, matched cases from the cephalic-presenting group were moved to the breech-presenting group where statistical analysis was completed once more.
Results
At the Department for Obstetrics and Gynecology, University Clinical Centre of Vojvodina, during the period from the year 1985 until the year 2014, there were 125,240 deliveries. A total of 462 deliveries were identified with women giving birth with congenital uterus malformations, which makes an incidence of 0.37. There were 27 cases that were excluded due to a transverse lie, 11 were excluded due to a myoma uteri, and 5 were excluded due to uteroplastic interventions.
Eighty-one cases of multipara with two deliveries were identified. In cases of multiparty there was no data available for all nine variables except for the fetal presentation data (due to the delivery occuring in another institution and incomplete medical data).
The Chi-Square test 2 × 2 showed no difference in the distribution of cases with breech and cephalic presentation at the first and second delivery in multiparity (Table 1).
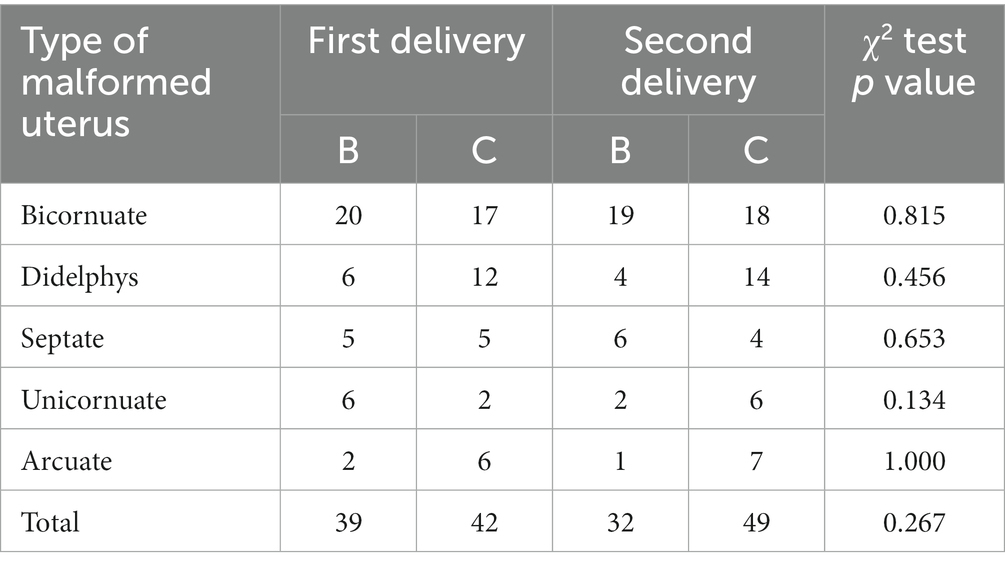
Table 1. Number of breech and cephalic presentation among different types of congenitally malformed uterus in multiparity at delivery.
In Table 2, variants of cases for pairs of presentations at the first and the second delivery were presented for different types of congenitally malformed uteri. There was no statistically significant difference in incidence determined for variants of pair presentations at the first and the second birth for any type of CMU. Among 39 cases which had a breech presentation at the first delivery, this presentation was repeated in 16 cases at the mother’s second delivery. From the rest of the 32 cases in breech presentation at second delivery, 16 of them had cephalic presentation at first delivery. The difference in nonrepeating breech presentation at second delivery compared to repeating breech presentation was statistically significant (Chi square test 2 × 2, 39:16 vs. 39:39 p value = 0.015 p < 0.05).
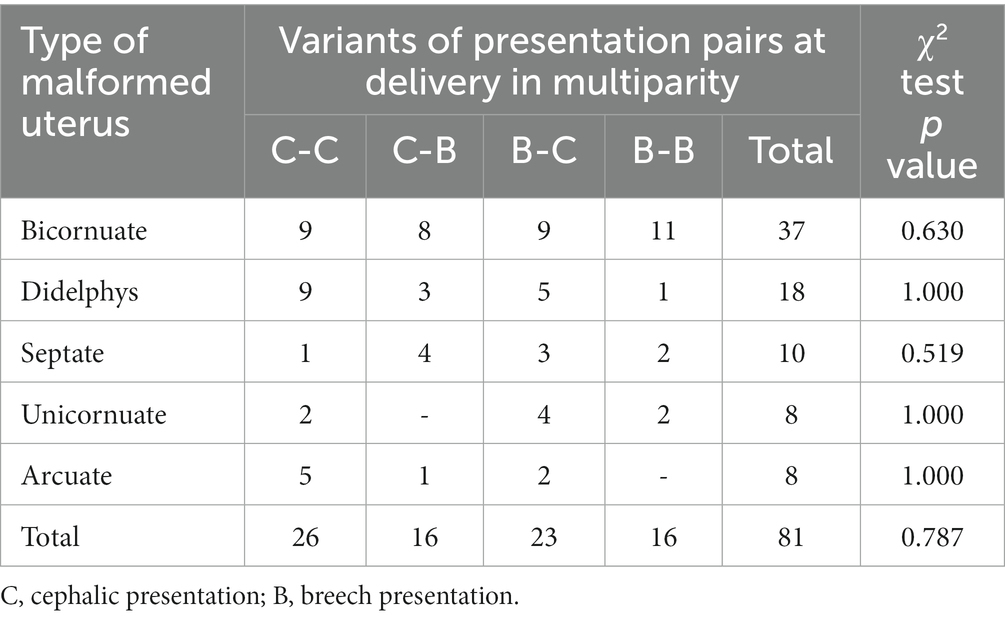
Table 2. Variants of presentation pairs at delivery in multiparity for various types of the congenitally malformed uterus.
Regarding the physical characteristics of the fetus, placenta and gestational age, there were no significant differences between breech and cephalic group at the first and the second deliveries (Table 3).
Regarding the fetal physical characteristics and gestational age, no statistically significant differences were found between the newborn group that repeated the same presentation from the previous delivery and the group that had a different presentation (Table 4).
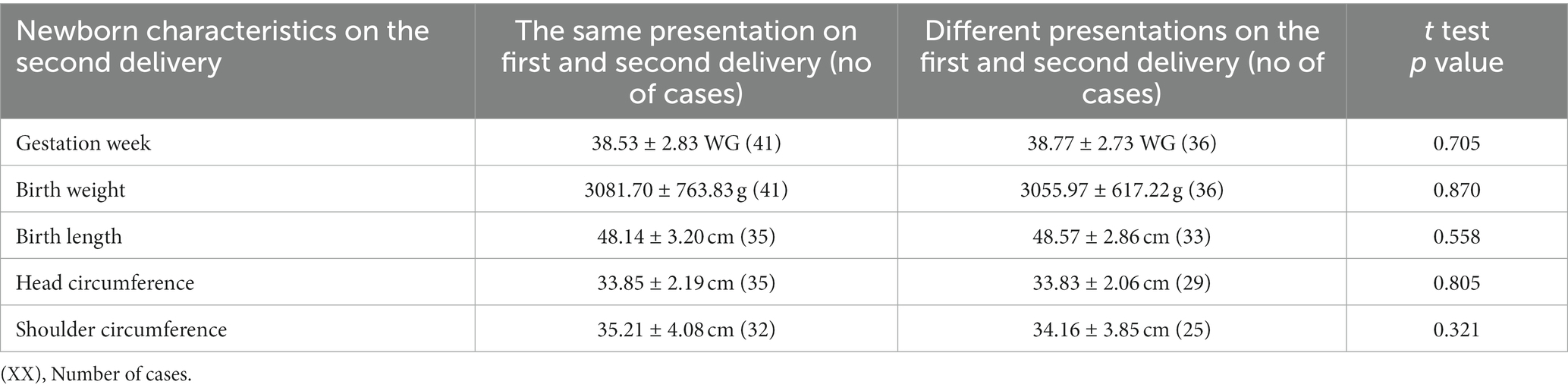
Table 4. Newborn characteristics at second delivery in case of the same or different presentation on first and second delivery.
The data acquired in multiparity indicate that breech presentation is a consequence of the random filling of the intrauterine cavity with an equal probability for a breech or cephalic presentation. The results justify applying a matching procedure to evaluate the breech presentation outcome, which was done in the following part of the work.
Data for the statistical analysis of CMU with all nine variables was available for 350 deliveries. After stratification of the sample and excluding the cases of extreme prematurity, 337 deliveries remained (Table 5). Therefore, in examining the characteristics for each type of congenitally malformed uterus, all included cases had all the mentioned parameters that were being examined.
The comparison of before and after matching was not performed in the case of the septate uterus. Taking into consideration the incidence of the breech presentation of ≥50%, sampling bias towards less expressed differences between the breech and the cephalic group is absent according to the concept presented in the introduction. Fetuses/newborns in both groups were taken at random their presentation.
In four types of CMU (arcuate, bicornuate, didelphys, unicornuate), nine variables with 36 instances of comparison were observed before and after the matching (Tables 6–8). No statistically significant difference was present in any of the variables without the matching. When M1 matching was performed, in 10 instances, variables in the breech/random group compared to the cephalic group had statistically significant lower values, while in two instances, the cephalic group had lower values which were statistically significant. In the M matching procedure in 6 instances, variables in the breech/random group compared to the cephalic group had statistically significant lower values. In one instance statistically significant lower values were observed in the cephalic group.
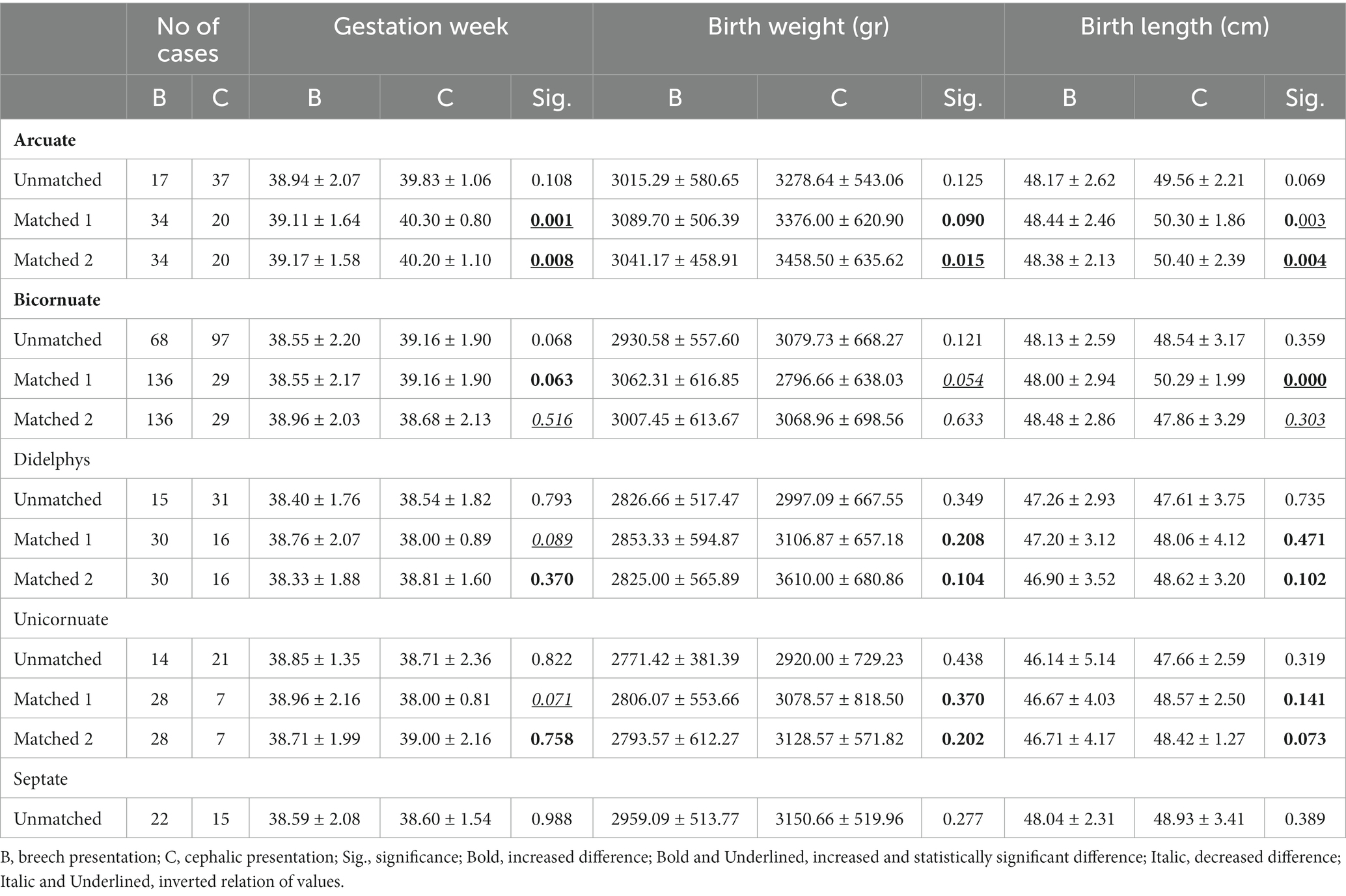
Table 6. The matched and unmatched outcome of breech presenting newborns in relation to gestational age, birth weight, and birth length.
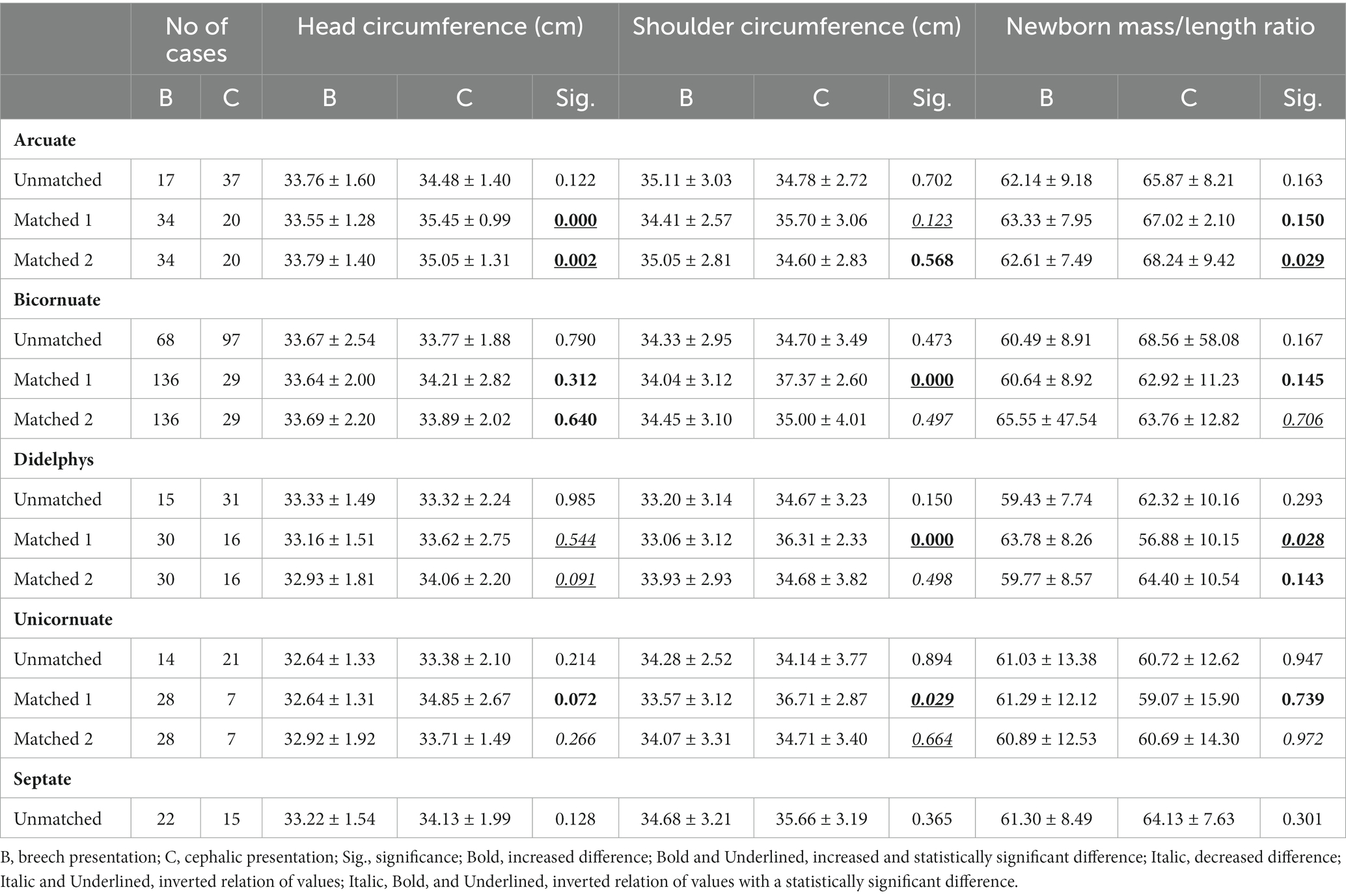
Table 7. The matched and unmatched outcome of breech presenting newborns in relation to head circumference, shoulder circumference and newborn mass/length ratio.
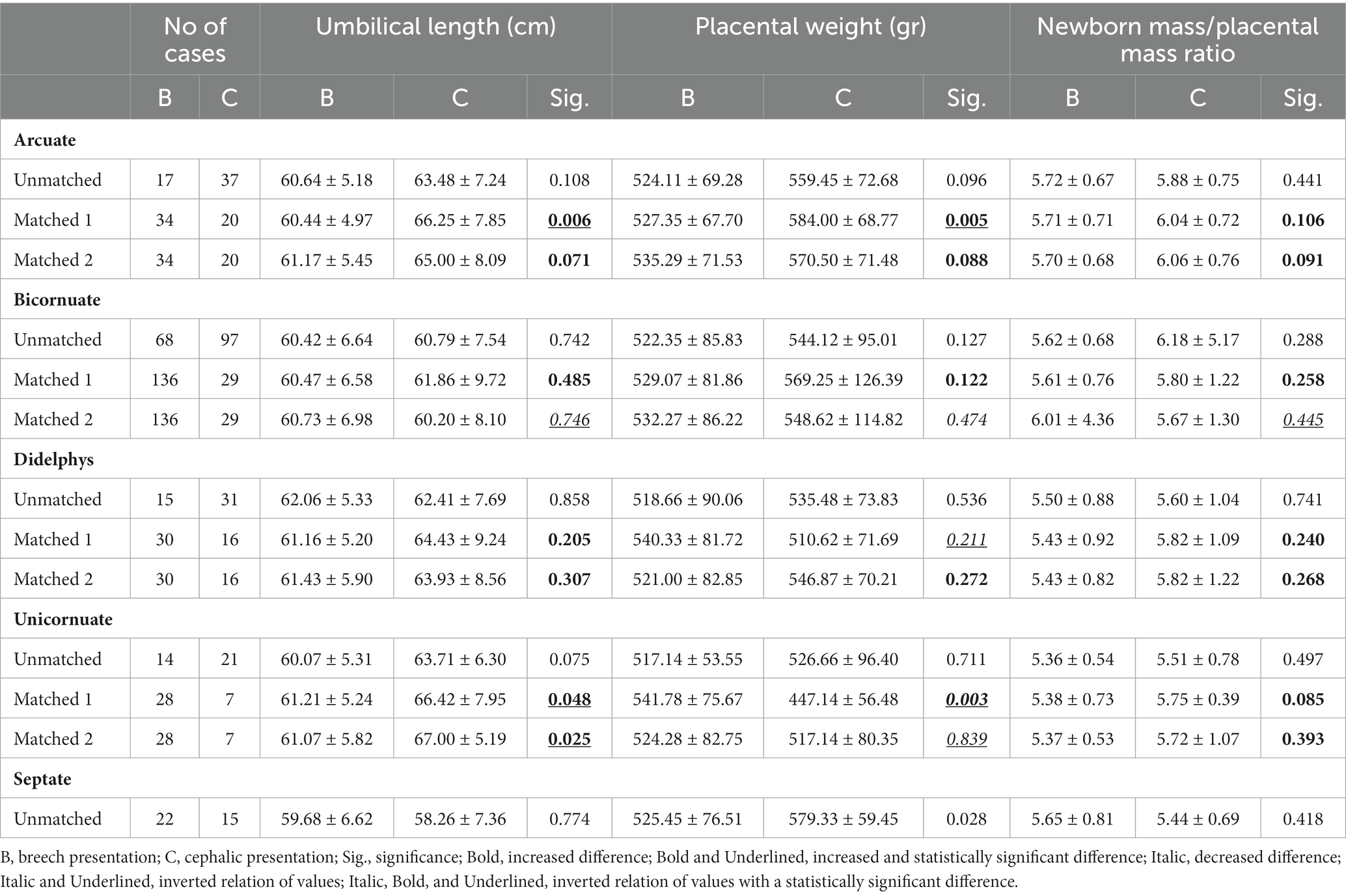
Table 8. The matched and unmatched outcome of breech presenting group in relation to umbilical length, placental weight, newborn mass/placental mass ratio.
Regarding the types of CMU, the arcuate uterus showed that the characteristics of the fetuses were significantly worse after the comparison. There was a statistically significant worsening of characteristics with regards to the physical characteristics of the fetus and placenta that were also present in the other three types of congenital malformations, but to a lesser degree.
Discussion
The incidence of CMU in this study, 0.37% is on the lower end of the scale when compared to other studies: 0.5%, 3.2%, and 5.4% (19–21). The incidence of a breech presentation among various types of the congenitally malformed uterus presented in this study (Table 5) were in accordance with the data presented in other studies. Studies with more than 20 cases for a particular type of malformed uterus showed that incidences of breech presentation were: 1. Uterus bicornuate 34.78%, 35%, 41.7%, and 46.47% (8, 22–24); 2. Uterus didelphys 36.4% and 41.17% (8, 23); 3. Uterus unicornuate 34% and 55.6% (23, 24); 4. Uterus arcuate 13, 22.58, and 40% (8, 22, 24); and 5. Uterus septate is an exception where the value in this study of 59.45% was higher than in other studies 35%, 38.33%, 45.71%, and 47.4% (8, 22–24).
In multiparity with CMU, the difference between the incidence of breech and cephalic presentations between the first and the second delivery were not statistically significant. This result was achieved despite the fact that subsequent deliveries did not repeat the same fetal presentation as on the first delivery. Pairs of presentations in multiparity were the result of independent events, during which the first and second birth had the same probability for a breech or a cephalic presentation independent of fetal physical characteristics and gestational age.
The results of this study confirm the findings of earlier studies, that the maximum probability for a breech presentation is 50% (8, 9).
Binomial distribution allows for values over 50% in individual series when the probability for the breech is close to or exactly 50%, similar to the probability of tossing a coin. For example, when considering a series with fewer tries in tossing the coin, the probability of a tail can be over or under 50%. When there is an infinite number of coin tosses, the incidence will be reaching a value that is closest to the ideal distribution 50:50 (25). We have identified only one study with a significant number of cases in which there was an incidence of breech presentation that was significantly higher than 50% (26). The authors of that study stated that not all the cases had had a routine examination in regard to CMU. However, detailed diagnostic searches were performed only when there were complications at birth, which included breech presentation. This resulted in bias regarding a higher frequency of breech presentation. In accordance with this, there was a low incidence of CMU, 0.13% in that specific study (26).
The fetus changes its presentation/lie from breech to cephalic and vice versa using a variety of movements, including kicking, locomotion, body twisting, and trunk and lower extremity stretching (27). The cephalic version of breech fetuses in cases of the congenitally malformed uterus is not recommended. A published study shows that the external version of breech to cephalic presentation was successful in one of 12 attempts (21). Furthermore, congenital malformations of the uterus present a contraindication for the fetus’s external or internal version because of insufficient intrauterine space volume (28). A likely explanation for the etiology of breech presentation in the case of CMU is that in the period up to 24 weeks of gestation, when the fetuses have randomly assumed a presentation (Figure 1), they have outgrown the malformed uteruses. The fetuses remained compressed in the uterine cavity before or at the beginning of the gestational period, characterized by the exclusive increase in the incidence of cephalic presentation from 24–36 WG (Figure 1). This could explain why the fetuses assume a breech presentation at random and why the probability of breech presentation in CMU is no higher than 50%. Thus, it would be interesting to further explore the incidence of presentation during gestation for each type of CMU.
To our knowledge, there were no studies available that examined the differences between breech and cephalic presenting newborns in CMU (22–24, 26). As a rule, the outcomes of CMU were examined regardless of the presentation.
The case–control matching procedure randomly matched cases and controls based on specific criteria. In other words, matching is used to balance the distributions of observed (and possibly confounding) covariates. Ideally, one would match each experimental subject with a control subject that was an exact match on each of the observed covariates. As the number of covariates increases or the ratio of the number of control subjects to examined subjects decreases, which was the case in our study, it becomes less likely that an exact match would be found for each examined subject. When the matching procedure was based on a single variable, it was easier to find a corresponding case. This was reflected in a larger number of statistically significant differences in M1 matching than in M2.
The case–control matching procedure showed that it is able to detect the difference between the breech/random and the cephalic group of newborns, while the classic method of direct comparison was unable to detect any differences. Some authors consider the arcuate uterus a minimal deviation in the anatomy of the uterus and do not consider it in the outcome of the pregnancy along with the other types of CMU (23, 29). The presented data from the matching procedure for the arcuate uteri, clearly showed that the physical characteristics of the newborn in a breech presentation, were significantly worse than those in the cephalic presentation. It should be noted that in arcuate uteri metroplasty leads to improvement of uterine artery Doppler velocimetry indices, i.e., better uterine perfusion (30). Our data suggest that it is necessary to reconsider the clinical approach in the prognosis, outcome, and management of breech/random presentation in case of CMU. Newborns from breech/random group compared to cephalic group, showed poorer values of body development parameters. In CMU it is necessary to investigate trophic factors such as diminished uterine blood flow, insufficient placental function, in relation to fetal presentation using matching process.
CMU are associated with increased incidence of: missed abortion, prematurity, intrauterine growth retardation, still birth, preterm premature rupture of membranes, postural deformation of the fetus (23, 31). Incomplete data in this study prevented investigation of mentioned entities regarding fetal presentation.
Conclusion
The study confirms that breech presentation in CMU is a consequence of the random filling of the intrauterine cavity with an equal probability for a breech or cephalic presentation. The case–control matching procedure shows that it is able to detect the difference between the breech/random presentation and CP, while the classic method of direct comparison was unable to detect any differences. The outcome of the breech/random presentation in CMU should be evaluated with the described case–control matching procedure. Applying the matching procedure to evaluate breech presentation outcome in any medical entity with increased incidence of breech presentation than in general population, would shed new light on the deviation from physiological norm and validity of current management of breech presentation.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by University Clinical Center of Vojvodina. Written informed consent was not provided because retrospective study.
Author contributions
SS, NS, ZN, BP, and VP: concept and design of the study. SS, BB, AK, IT, DP, and AV: gathering data from the hospital archive, search of literature. NS and ZN: statistical analysis. SS, BB, AK, IT, AV, BP, VP, and AM: interpretation of relevant literature. SS and AM: translation to English language. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Ministry of Science, Technological Development and Innovation of the Republic of Serbia, grant numbers 451-03-47/2003-01 and 451-03-47/2023-01/200007.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sørensen, T, Hasch, E, and Lange, AP. Fetal presentation during pregnancy. Lancet. (1979) 2:477. doi: 10.1016/S0140-6736(79)91536-8
2. Miller, EC, and Kouam, L. Frequency of breech presentation during pregnancy and on full term. Zentralbl Gynakol. (1981) 103:105–9.
3. Hughey, MJ. Fetal position during pregnancy. Am J Obstet Gynecol. (1985) 153:885–6. doi: 10.1016/S0002-9378(85)80276-3
4. Ferreira, JCP, Borowski, D, Czuba, B, Cnota, W, Wloch, A, Sodowski, K, et al. The evolution of fetal presentation during pregnancy: a retrospective, descriptive cross-sectional study. Acta Obstet Ginecol Scand. (2015) 94:660–3. doi: 10.1111/aogs.12626
5. Tadmor, OP, Rabinowitz, R, Alon, L, Mostoslavky, V, and Aboulafia, Y. Can breech presentation at birth be predicted from ultrasound examination during the second or third trimester? Int J Gynaecol Obstet. (1994) 46:11–4. doi: 10.1016/0020-7292(94)90302-6
6. Boos, R, Hendrik, HJ, and Schmidt, W. Behavior of fetal position in the second half of pregnancy in labor with breech and vertex presentations. Geburtshilfe Frauenheilkd. (1987) 47:341–5. doi: 10.1055/s-2008-1035833
7. Kato, K, Nagamatsu, T, Yamaguchi, S, Ichinose, M, Sayama, S, Toshimitsu, M, et al. Changes in fetal presentation in the preterm period and the prediction of non-cephalic delivery. J Matern Fetal Mater Neonatal Med. (2023) 36:2141564. doi: 10.1080/14767058.2022.2141564
8. Sekulic, S, Vuleta, DP, and Vuleta, PD. Breech presentation and tossing a coin: heads or tails. Med Hypotheses. (2003) 60:218–24. doi: 10.1016/S0306-9877(02)00362-6
9. Sekulic, S, Mikov, A, and Petrovic, D. Probability of breech presentation and its significance. J Matern Fetal Neonatal Med. (2010) 23:1160–4. doi: 10.3109/14767051003677996
10. Awater, C, Zerres, K, and Rudnik-Schoneborn, S. Pregnancy course and outcome in women with hereditary neuromuscular disorders: comparison of obstetric risks in 178 patients. Eur J Obstet Gynecol Reprod Biol. (2012) 162:153–9. doi: 10.1016/j.ejogrb.2012.02.020
11. Renshaw, TS. Sacral agenesis. J Bone Joint Surg Am. (1978) 60:373–83. doi: 10.2106/00004623-197860030-00020
12. Brenner, WE, Bruce, RD, and Hendricks, CH. The characteristics and perils of breech presentation. Am J Obstet Gynecol. (1974) 118:700–12. doi: 10.1016/S0002-9378(16)33744-9
13. Sekulic, S, Zarkov, M, Slankamenac, P, Bozic, K, Vejnovic, T, and Novakov-Mikic, A. Decreased expression of righting reflex and locomotor movements in breech-presenting newborns in first days of life. Early Hum Dev. (2009) 85:263–6. doi: 10.1016/j.earlhumdev.2008.11.001
14. Zhang, J, and Schwingl, PJ. Breech presentation and fetal growth retardation. J Reprod Med. (1993) 38:193–6.
15. Macharey, G, Gissler, M, Rahkonen, L, Ulander, VM, Väisänen-Tommiska, M, Nuutila, M, et al. Breech presentation at term and associated obstetric risks factors-a nationwide population based cohort study. Arch Gynecol Obstet. (2017) 295:833–8. doi: 10.1007/s00404-016-4283-7
16. Westgren, M, Edvall, H, Nordström, L, Svalenius, E, and Ranstam, J. Spontaneous cephalic version of breech presentation in the last trimester. Br J Obstet Gynaecol. (1985) 92:19–22. doi: 10.1111/j.1471-0528.1985.tb01043.x
17. Mostello, D, Chang, JJ, Bai, F, Wang, J, Guild, C, Stamps, K, et al. Breech presentation at delivery: a marker for congenital anomaly? J Perinatol. (2014) 34:11–5. doi: 10.1038/jp.2013.132
18. American Fertility Society. The American fertility Sociaty classifications of adnexal adhesions, distal tubal pregnancies, Mullerian anomalies and intrauterine adhesions. Fertil Steril. (1988) 49:944–55. doi: 10.1016/S0015-0282(16)59942-7
19. Nahum, GG. Uterine anomalies. How common are they, and what is their distribution among subtypes? J Reprod Med. (1998) 43:877–87.
20. Simón, C, Martinez, L, Pardo, F, Tortajada, M, and Pellicer, A. Müllerian defects in women with normal reproductive outcome. Fertil Steril. (1991) 56:1192–3. doi: 10.1016/S0015-0282(16)54741-4
21. Jurkovic, D, Gruboeck, K, Tailor, A, and Nicolaides, KH. Ultrasound screening for congenital uterine anomalies. Br J Obstet Gynaecol. (1997) 104:1320–1. doi: 10.1111/j.1471-0528.1997.tb10982.x
22. Heinonen, PK, Saarikoski, S, and Pystynen, P. Reproductive performance of women with uterine anomalies. Acta Obstet Gynecol Scand. (1982) 61:157–62. doi: 10.3109/00016348209156548
23. Hiersch, L, Yeoshoua, E, Miremberg, H, Krissi, H, Aviram, A, Yogev, Y, et al. The association between Mullerian anomalies and short-term pregnancy outcome. J Matern Fetal Neonatal Med. (2016) 29:2573–8. doi: 10.3109/14767058.2015.1098613
24. Acien, P. Reproductive performance of women with uterine malformations. Hum Reprod. (1993) 8:122–6. doi: 10.1093/oxfordjournals.humrep.a137860
26. Stein, AL, and March, CM. Pregnancy outcome in women with müllerian duct anomalies. J Reprod Med. (1990) 35:411–4.
27. Suzuki, S, and Yamamuro, T. Fetal movement and fetal presentation. Early Hum Dev. (1985) 11:255–63. doi: 10.1016/0378-3782(85)90079-9
28. Rosman, AN, Guijt, A, Vlemmix, F, Rijnders, M, Mol, BW, and Kok, M. Contraindications for external cephalic version in breech position at term: a systematic review. Acta Obstet Gynecol Scand. (2013) 92:137–42. doi: 10.1111/aogs.12011
29. Naeh, A, Sigal, E, Barda, S, Hallak, M, and Gabbaz-Benziv, R. The association between congenital uterine anomalies and perinatal outcomes – does type of defects matters? J Matern Fetal Neonatal Med. (2022) 35:7406–11. doi: 10.1080/14767058.2021.1949446
30. Pace, S, Cerekja, A, Stentella, P, Frega, A, Pace, G, La, TR, et al. Improvement of uterine artery Doppler velocimetry indices after metroplasty in arcuate uteri. Eur J Obstet Gynecol Reprod Biol. (2007) 131:81–4. doi: 10.1016/j.ejogrb.2006.02.011
Keywords: breech presentation, congenitally malformed uterus, outcome, bias, birth
Citation: Sekulic S, Stilinovic N, Baturan B, Krsman A, Tesic I, Vejnovic A, Petrovic D, Nikolasevic Z, Mijavec A, Pesic V and Petkovic B (2023) Corrected evaluation of the breech presentation outcome based on etiology of this presentation in congenitally malformed uterus. Front. Med. 10:1160229. doi: 10.3389/fmed.2023.1160229
Edited by:
Simcha Yagel, Hadassah Medical Center, IsraelReviewed by:
Zhen Xiao, Dalian Medical University, ChinaCristian Furau, Vasile Goldiș Western University of Arad, Romania
Copyright © 2023 Sekulic, Stilinovic, Baturan, Krsman, Tesic, Vejnovic, Petrovic, Nikolasevic, Mijavec, Pesic and Petkovic. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Slobodan Sekulic, slobodan.sekulic@mf.uns.ac.rs
 Slobodan Sekulic
Slobodan Sekulic Nebojsa Stilinovic
Nebojsa Stilinovic Branislava Baturan2,4
Branislava Baturan2,4  Zeljka Nikolasevic
Zeljka Nikolasevic Vesna Pesic
Vesna Pesic Branka Petkovic
Branka Petkovic