Impact of the SARS-CoV-2 infection in individuals with sickle cell disease: an integrative review
- Department of Medicine, Federal University of São Carlos (UFSCar), São Carlos, Brazil
Sickle cell disease is the most common hemoglobinopathy among humans. As the condition promotes susceptibility to infections, chronic inflammation, and hypercoagulability disorders, several international agencies have included individuals with this disease in the COVID-19 risk group for severe outcomes. However, available information about the subject is not properly systematized yet. This review aimed to understand and summarize the scientific knowledge about the impact of SARS-CoV-2 infection in patients with sickle cell disease. Searches were performed in the Medline, PubMed, and Virtual Health Library databases based on descriptors chosen according to the Medical Subject Headings. We analyzed studies published between 2020 and October 2022, developed with qualitative, quantitative, or mixed methodology, and written in English, Spanish, or Portuguese. The search resulted in 90 articles organized into six categories. There is disagreement in the literature about how different aspects related to sickle cell disease, such as chronic inflammation status, hypercoagulability, hemolytic anemia, use of hydroxyurea, and access to medical care interference with the clinical course of COVID-19. These topics deserve further investigation. It is evident, however, that the infection may manifest in an atypical way and act as a trigger for the development of sickle cell-specific complications, such as acute chest syndrome and vaso-occlusive crises, conditions that are associated with great morbidity and mortality. Therefore, healthcare professionals must be aware of the different forms of presentation of COVID-19 among these individuals. Specific guidelines and therapeutic protocols, as well as public policies for sickle cell individuals, must be considered.
Systematic review registration: This review (https://doi.org/10.17605/OSF.IO/NH4AS) and the review protocol (https://osf.io/3y649/) are registered in the Open Science Framework platform.
1. Introduction
Sickle cell disease is the most frequent hemoglobinopathy in humans (1). At least 300, 000 children are born with the condition each year (2, 3). It is an inherited hemolytic anemia caused by a genotype that determines the production of type S hemoglobin (HbS), a variant of adult hemoglobin (HbA), as the result of a single mutation (missense mutation) in the β-globin gene, which consists of a thymine nucleotide substitution for adenine. This event changes the codon of the sixth amino acid in the β-globin chain from glutamic acid to valine (3).
The homozygous form of the HbS gene characterizes sickle cell anemia, the most prevalent monogenic condition in the world. However, other genotypes causing sickle cell disease can be identified. Basically, they correspond to the uniparental inheritance of the βS allele in concomitance with mutations for other HbA variants, such as S/β°thalassemia, S/β+ thalassemia, and SC (1, 4). Although there may be some variation in the severity of the clinical phenotype for each of the genotypes associated with sickle cell disease, the pathophysiology of this entity is multisystemic and, regardless of the origin genotype, is fundamentally anchored in HbS polymerization, vaso-occlusion, and hemolytic anemia (3). A carrier of sickle cell, also known as having the sickle cell trait, is an individual who, despite being heterozygous for the HbS gene, can synthesize enough HbA to inhibit polymerization and, generally, does not exhibit relevant clinical manifestations (4).
It is possible to group the most relevant chronic complications of sickle cell disease into two categories: those related to large vessel vasculopathy, such as cerebrovascular disease, pulmonary hypertension, priapism, and retinopathy; and those that contribute to progressive ischemic organ damage, such as hyposplenia, renal failure, bone disease, and liver injury. Damage to the spleen, which can culminate in functional asplenia, confers an increased risk of infections, representing an additional factor in higher mortality, especially in children. As for acute complications, pain crises and acute chest syndrome, one of the main causes of death in this population, are the most frequent manifestations. Despite advances in medical care, the life expectancy of individuals with sickle cell disease is still reduced by about two to three decades compared to the general population. Child mortality in this group can reach 90% in low-income countries (2, 3, 5, 6).
In light of the high prevalence of sickle cell disease in different populations and the well-known susceptibility of these individuals to infections (2, 7), it is essential to understand the pathophysiology of COVID-19 in the context of sickle cell disease. The World Health Organization has recorded over 6 million deaths worldwide due to COVID-19 (8). Furthermore, the statistics reveal that the elderly, especially those over 60 years old, and people with underlying chronic diseases, such as hypertension, diabetes, cardiovascular disease, chronic kidney disease, cancer, obesity, and chronic obstructive pulmonary disease, are more susceptible to the severe forms of the disease, with increased mortality rates (9–12). Although several specialized agencies around the world, such as the Centers for Disease Control and Prevention (CDC), have included people with sickle cell disease as part of the risk group for poor outcomes of COVID-19 (13), the available information on the impact of infection on these individuals has not yet been properly systematized.
It seems that the clinical course of COVID-19 in this population is quite variable. Some studies point out, for example, that SARS-CoV-2 infection may act as a trigger for the occurrence of typical complications of sickle cell disease, in particular vaso-occlusive crises and acute chest syndrome, but the data on mortality and hospitalizations, in principle, do not exhibit significant differences compared with the general population (14–16).
Therefore, this review aimed to provide a detailed overview of the scientific production on sickle cell disease and COVID-19 in order to understand and systematize the knowledge produced on the subject. Ultimately, it intends to offer subsidies to guide decision-making in clinical practice, the formulation of guidelines and therapeutic protocols, and the development of public policies directed at this population.
2. Methods
This is an integrative review conducted according to the literature (17–19), based on PRISMA recommendations (20), and with a research protocol registered in the Open Science Framework (https://osf.io/3y649/). The intent of this review was to answer the following research question: “What is the impact of SARS-CoV-2 virus infection in people with sickle cell disease?” outlined in the PICO format (21, 22), as detailed in Table 1.
2.1. Search strategy
The searches were performed in three databases: Virtual Health Library (Biblioteca Virtual da Saúde, BVS), PubMed, and Web of Science. Using the BVS, we were able to access the LILACS (Latin American and Caribbean Literature on Health Sciences) database, which includes SciELO (Scientific Electronic Library Online), medRxiv, bioRxiv, and ColecionaSUS. In PubMed, we used the MEDLINE database. The Web of Science was searched by topics and all collections were accessed.
The following descriptors, extracted from the “Medical Subject Headings” platform (https://www.nlm.nih.gov/mesh/), were used in the search: [(HbS Disease) OR (Hemoglobin S Disease) OR (Sickle Cell Anemia) OR (Sickle Cell Disease) OR (Sickle Cell Disease) OR (Sickle Cell Disease due to Hemoglobin S)] AND [(SARS-CoV-2) OR (SARS-CoV-2 Virus) OR (SARS-CoV-2 Infection) OR (COVID- Virus 19) OR (COVID-19 Virus) OR (Pandemic COVID-19) OR (Pandemic COVID-19) OR (Pandemic COVID-19) OR (COVID-19 Virus) OR (COVID-19 Virus Disease) OR (COVID-19 Virus Infection) OR (2019 Novel Coronavirus) OR (2019 Novel Coronavirus Disease) OR (2019 Novel Coronavirus Infection) OR (2019-nCoV) OR (2019-nCoV Disease) OR (2019-Infection nCoV) OR (2019 Coronavirus Disease) OR (2019 Coronavirus Disease) OR (2019 Coronavirus Virus) OR (2019 Coronavirus Infection) OR (SARS Coronavirus 2) OR (SARS Coronavirus 2)] AND [(inflammation) OR (mediators of inflammation) OR (innate inflammatory response) OR (embolism and thrombosis) OR (thrombosis) OR (blood clot) OR (thrombus) OR (hypercoagulability) OR (thromboembolism) OR (physiology) OR (oxidative stress) OR (oxidative injury) OR (hemolysis)].
The research was conducted independently by two researchers with the help of a third collaborator, who was consulted to resolve any doubts. The concordance between the searches in the three databases was checked in terms of the date and quantitative characteristics of the data collected. After confirming the compatibility of the information, the identified publications were entered into the Rayyan software (https://www.rayyan.ai/), a tool specifically developed to assist in the primary selection of articles in systematic review projects (23).
Using Rayyan, duplicates were identified and excluded. Then, an initial analysis of the papers was performed by reading the title, abstract, and keywords. Articles that were not aligned with the research question were eliminated. In this first screening, the reading and selection of the documents were conducted by two researchers in a “blind” mode to avoid bias. Doubts and disagreements were discussed, solved together, and then, if necessary, triple-checked with the other researcher to reach a final decision.
The articles that remained under analysis were entirely read and submitted to a new selection stage after filling out an eligibility form (Form 1-Supplementary material) based on the inclusion and exclusion criteria. Additionally, the references of these articles were reviewed in a manual search for other manuscripts pertinent to the study. In this step, the selection was performed with the help of the Mendeley reference manager (https://www.mendeley.com/) (24).
2.2. Inclusion and exclusion criteria
This review included theoretical or empirical studies, primary or secondary research, carried out with qualitative, quantitative, or mixed methodology, written in Portuguese, English, or Spanish, that portray the theme of interest and were published between January 2020 and the day of the last database search, performed on October 7, 2022.
2.3. Assessment of the level of evidence of the studies and data extraction
Selected papers were classified according to their levels of evidence, taking into consideration the type of study, according to criteria adapted from Melnyk and Fineout- Overholt (25) (Table 2). Their data were systematically extracted using a standardized form (Form 2-Supplementary material) that includes information about authorship, country of origin, type of study, year of publication, main outcomes, and conclusions, allowing the synthesis of the information found and the evaluation of the consistency and validity of the studies.
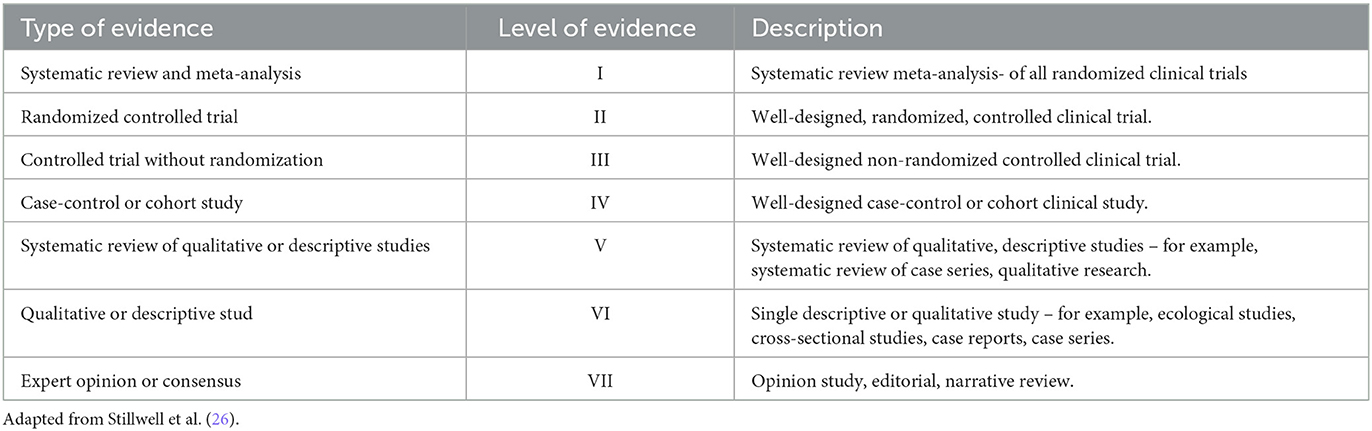
Table 2. Categorization of the level of evidence, according to the type of study of the scientific productions.
Once the data were extracted, the results were compared and problematized. The objective was to integrate the knowledge through a synthesis of the findings. Therefore, the similarities of the studies were explored by placing them into categories to organize the data clearly, allowing better visualization of the available evidence and gaps in scientific production. This process occurred through an inductive approach based on identifying patterns and a thematic analysis of the final set of information (27, 28).
3. Results
The database search initially identified 256 articles. Of this total, 172 were from the Web of Science, 80 were from PubMed, and only 4 were from the BVS. After the first screening, 38 duplicates and one article published in French were excluded. Another 148 articles were excluded after reading the title, abstract, and keywords. Thus, 69 articles were selected for a full reading. After this phase, 64 articles were included, along with another 26 studies collected from the references. Therefore, 90 articles were finally selected for this review. The selection process is summarized in Figure 1.
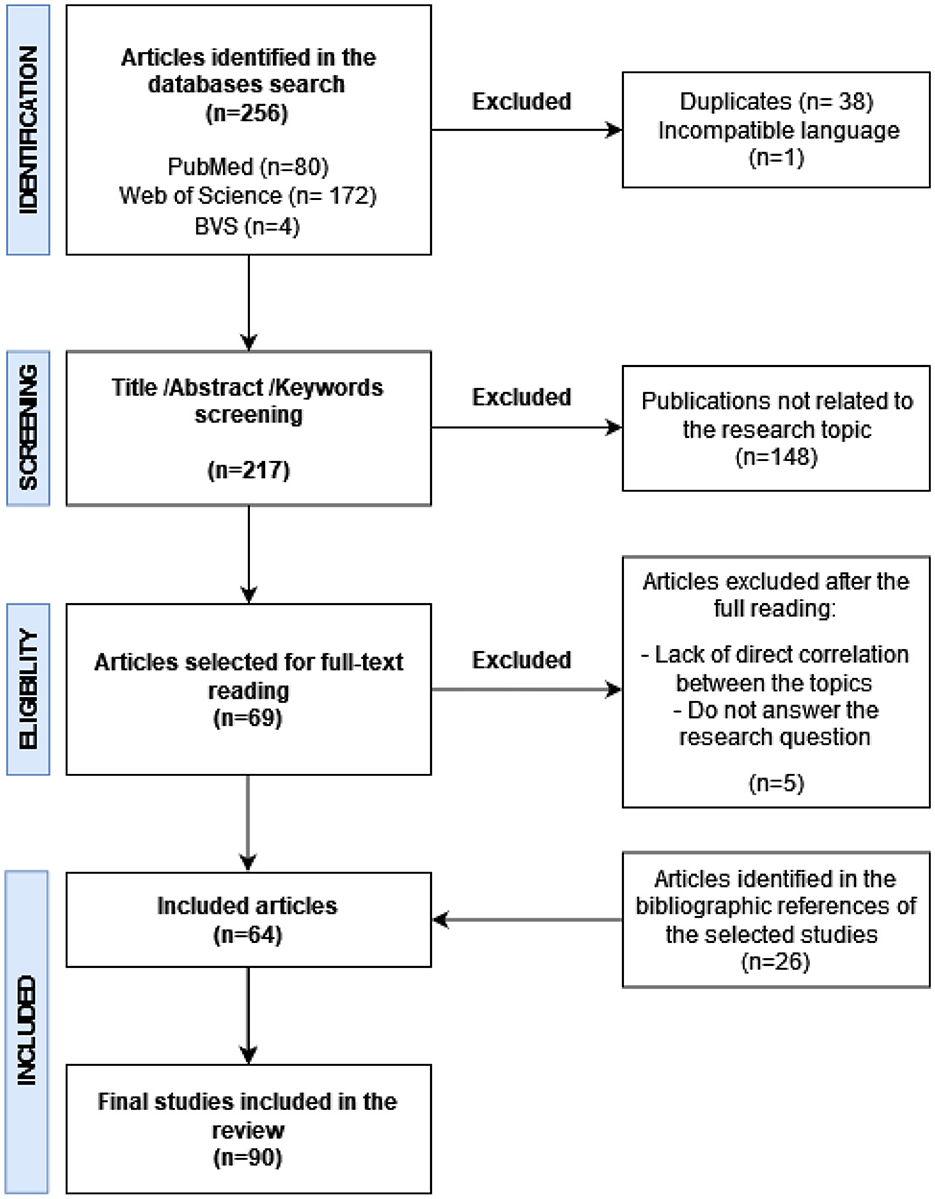
Figure 1. Flowchart summarizing the article selection process adopted in this review. Elaborated by the authors.
Most of the articles included were written in English [88], and only two were published in Portuguese. As for their origin, 38 studies were from the United States of America, 10 from the United Kingdom, 7 were from France, 6 were from Brazil, 4 were from Qatar, 4 were from Italy, 3 were from India, 2 from Ghana, 2 from Oman, and 2 were from Saudi Arabia; Bahrain, Belgium, the Democratic Republic of the Congo, Greece, Iran, Lebanon, Malaysia, the Netherlands, Nigeria, Tanzania, Turkey, and the United Arab Emirates contributed with one article each. Forty-two articles were published in 2020, 31 in 2021, and 17 in 2022.
Regarding methodology, most of the selected studies are case series (31 articles) and case reports (24 articles). Nevertheless, cohort studies (12 articles), case-control type studies (3 articles), cross-sectional studies (2 articles), and ecological studies (4 articles) were also present, as well as narrative reviews (6 articles), opinion articles/editorials (3 articles), systematic literature reviews (4 articles), and one meta-analysis. The selected articles were named A1 to A90, and their main characteristics are summarized in Table 3. An extended version of this table has been included in the Supplementary Table 1 and can be checked for more information about the sample features of each paper.
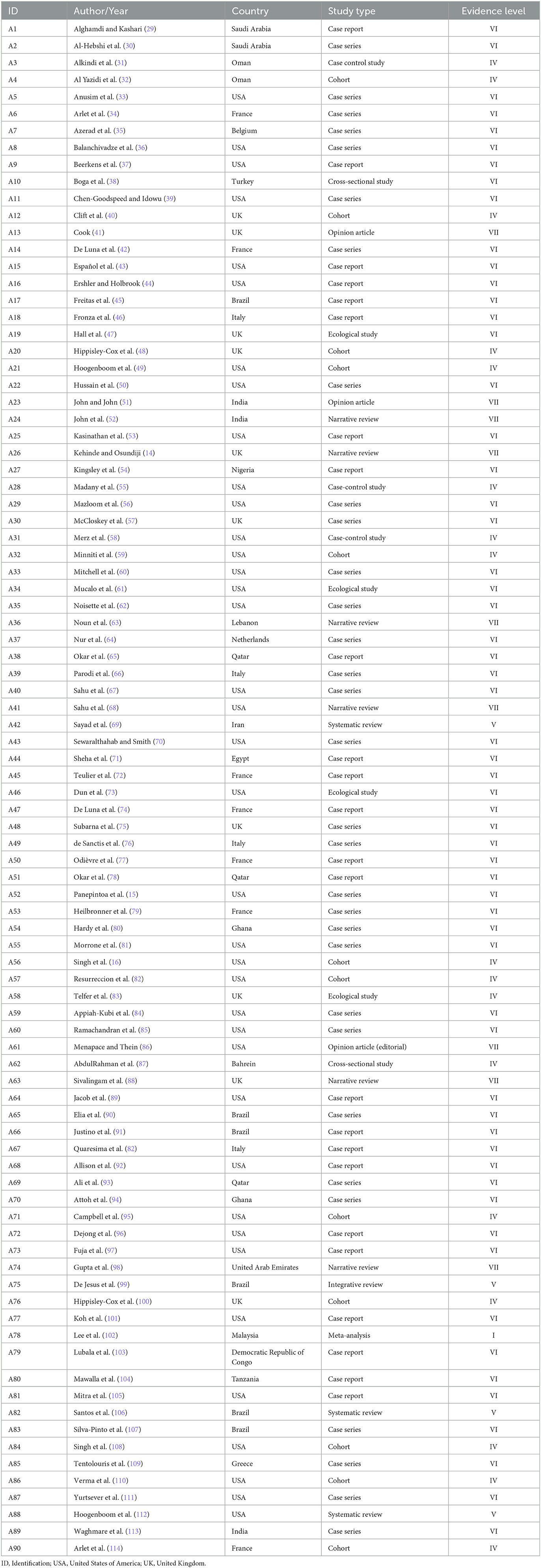
Table 3. Characterization of the 90 articles included in this integrative literature review, according to author/year of publication, origin country, type of study, level of evidence.
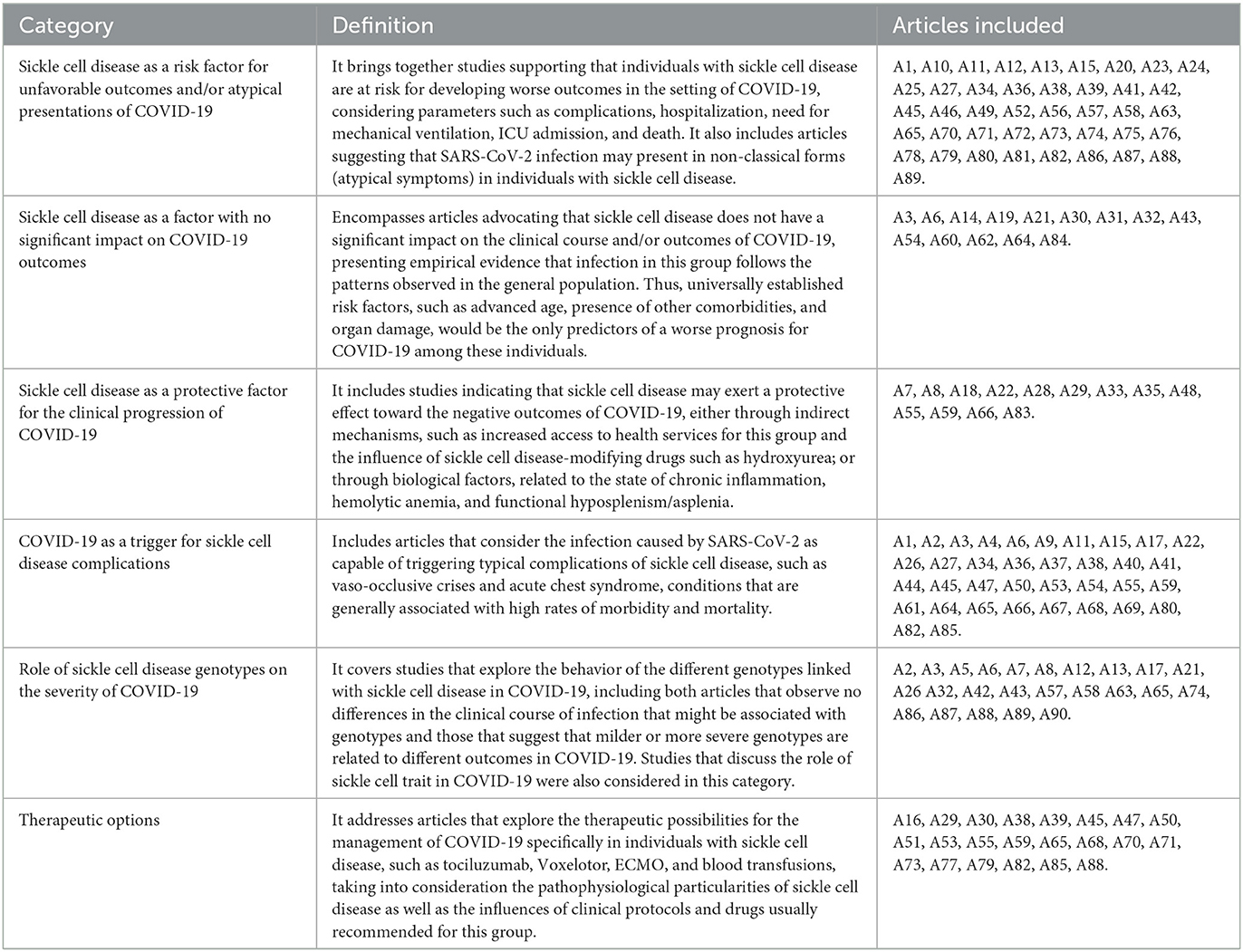
In the data extraction and analysis process, the articles were organized into six categories, as presented in Table 4: (1) sickle cell disease as a risk factor for unfavorable outcomes and/or atypical presentations of COVID-19; (2) sickle cell disease as a factor with no significant impact on COVID-19 outcomes; (3) sickle cell disease as a protective factor for the clinical progression of COVID-19; (4) COVID-19 as a trigger for sickle cell disease complications; (5) the role of sickle cell disease genotypes on the severity of COVID-19; and (6) therapeutic options. Category 1 encompasses 42 studies that, when considering parameters such as complications, hospitalization, need for mechanical ventilation, ICU admission, and death, suggest that individuals with sickle cell disease are at higher risk for worse outcomes in COVID-19 or demonstrate that the infection may present with unusual clinical patterns in this population. Fourteen articles are included in category 2; they gather empirical evidence supporting the idea that sickle cell disease has no crucial influence on the clinical course of COVID-19, and therefore the risk factors for those patients would be the same as those universally observed in the general population. As for the third category, 13 studies indicate that sickle cell disease may act as a protective feature against SAR-CoV-2 infection, either indirectly or biologically. Thirty-six articles pointing out that COVID-19 can trigger typical complications of sickle cell disease, such as vaso-occlusive crises and acute chest syndrome, are grouped in category 4. Category 5 comprises 24 papers that address the possible implications of the different sickle-cell disease-causing genotypes, as well as of the sickle-cell trait, on the clinical progression of SARS-CoV-2 infection. Finally, category 6 includes 22 studies that discuss the therapeutic management of COVID-19 in the sickle cell population, considering medical protocols and the use of certain drugs in these patients. Furthermore, it is worth noting that some articles are framed in more than one category.
4. Discussion
The results reveal a decrease in scientific production on the subject between 2020 and 2022. The data also indicate that, although a reasonable number of publications met the inclusion criteria, most of them have a low level of evidence, i.e., they are mainly observational studies with reduced samples, retrospective data collection, and a lack of adequate control groups.
4.1. The impact of sickle cell disease on COVID-19: a risk factor, a protective factor, or a factor without significance?
Considering the pathophysiological aspects of sickle cell disease and the clinical observations made during the H1N1 epidemic, most experts prepared for a potential catastrophe regarding this group when the COVID-19 pandemic first became established. However, a fair number of case reports and case series have revealed surprisingly positive clinical courses and outcomes in this population (35, 36, 46, 50, 56, 60, 62, 75, 81, 84, 91).
In this regard, some authors argue that sickle cell disease may act as an indirect protective factor against severe forms of SARS-CoV-2 infection. As hypothesized by Sivalingam et al. (88), closer proximity to health care services and routines may have a beneficial influence by improving or speeding up access to medical monitoring and proper therapeutic regimens. In addition, organizations such as the CDC have recommended more meticulous clinical approaches for high-risk groups (13), and some countries have adopted protocols in this direction that included sickle cell patients. Thus, prior knowledge about the hematologic condition by health care professionals could also be associated with earlier diagnosis and the more aggressive administration of antivirals, anti-inflammatory drugs, anticoagulants, and blood transfusions, with a direct impact on the clinical course of COVID-19 (36, 56, 84).
Furthermore, the chronic use of sickle cell disease-modifying therapies, such as hydroxyurea, has been implicated as one of the possible causes of the positive outcomes of COVID-19 among sickle cell patients (59, 69, 75, 81, 90, 102, 111). By increasing fetal hemoglobin levels, hydroxyurea can reduce vaso-occlusive events (3, 115), but its role in viral infections is unclear. While some studies correlate continued use of the substance with better outcomes in COVID-19 (36, 59, 69, 75, 90) – Yurtsever et al. (111), for example, associate hydroxyurea use with a 17% reduction in the risk of ICU admission – others have found no significant difference between patients using or not using this drug (34, 61, 114). The mechanisms by which hydroxyurea possibly modulates the clinical course of COVID-19 are not fully elucidated, but it is postulated that the substance diminishes levels of inflammatory cytokines and lowers activation of neutrophils and endothelial adhesion molecules, also reducing the inflammatory cascade (59, 81). Due to its apparent anti-inflammatory and immunomodulatory effects, whether directly or indirectly (by fetal hemoglobin synthesis), some experts even argue that the drug can be repurposed to treat COVID-19 in people without sickle cell disease (116, 117), thereby supporting the hypothesis that it has protective effects on sickle cell patients.
Some authors argue that sickle cell disease may offer an actual biological advantage against SARS-CoV-2 infection. The characteristic state of chronic inflammation and hemolytic anemia associated with the condition would somehow protect individuals from severe presentations of COVID-19 (35, 46, 50, 91, 107), in a similar way to what occurs with sickle cell carriers in malaria. It is hypothesized that people with sickle cell disease have elevated levels of IFNα/β, which would contribute to the peculiar basal inflammatory activity in sickle cell status and could play a protective role regarding viral diseases, including SARS-CoV-2 infection (55). Chakravorty et al. (75), in contrast, suggests that hyposplenism would be able to inhibit the cytokine storm of COVID-19, preventing the severe outcomes of the infection.
Contrary to this, some authors advocate that sickle cell disease confers an increased risk for severe COVID-19 (41, 43, 51, 52, 54, 61, 63, 65, 66, 68, 69, 88, 94, 95, 98, 111, 112). More than one algorithm conceived to calculate the risk of different populations developing complications from COVID-19 pointed to sickle cell disease as a risk factor (48, 73, 88, 100) supporting, for example, the indication of the prophylactic use of anticoagulants for this group (53, 56, 65, 84). In fact, the hypercoagulability state typical of sickle cell disease and the capacity of COVID-19 to promote thromboembolic events are listed as reasons that could explain the possibly higher risk of adverse outcomes of the infection (52, 72, 99). Some studies suggest an elevated incidence of pulmonary embolism in people with sickle cell disease and COVID-19 (16, 43, 53, 72, 79, 103). However, case series, such as those conducted by Mitchell et al. (60) and Noisette et al. (62), present divergent data in this regard. Even more recently, in their cohort of 281 patients with sickle cell disease and COVID-19, Singh et al. (108) found no significant differences in rates of venous thromboembolism compared to the group of patients with sickle cell disease hospitalized for other reasons than SARS-CoV-2 infection. Therefore, we do not have clear evidence of the specific occurrences of thromboembolic complications among people with sickle cell disease in the context of COVID-19, and this is a topic that deserves future investigation.
Several studies describe severe presentations, increased rates of hospitalization, ICU admission, a need for mechanical ventilation, and mortality among people with sickle cell disease and COVID-19. Objectively, the hospitalization rate in this population ranged from 26 to 77.1%, the intubation rate was between 9 and 10%, and mortality varied from 3.2 to 8.4% (15, 16, 38, 39, 76, 83). Clift et al. (40) demonstrated a 2- to 4-fold increased risk of hospitalization for people with sickle cell disease and COVID-19 and an enhanced risk of death from the infection up to 2.6-fold in this population. Some reports have pointed out that the increased risks for poorer outcomes in this group remain even in the presence of novel variants of the virus, among vaccines, and among children, which are situations associated with less severe clinical presentations in the general public (95, 96, 118). In some cases, even individuals with sickle cell trait are considered to be at risk (40, 110, 112, 119). The immunosuppressive state, increased risk of sepsis, endothelial dysfunction, and cardiovascular impairment are some of the characteristics of sickle cell disease that may explain these outcomes (2, 51, 54, 61, 63, 66, 68). The fact that COVID-19 acts as a trigger for the occurrence of sickle cell complications, which are events that are associated with high mortality, may also contribute to this scenario, as will be discussed in the next section.
It has also been observed that COVID-19 may present atypically in this population, with hepatobiliary manifestations (29), hematological abnormalities (105, 111), and the absence of typical respiratory symptoms (33, 34, 64, 82). This picture could make it difficult to diagnose the infection and has led some authors to recommend testing individuals with sickle cell disease for COVID-19 even in the absence of classic symptoms (64, 68, 82). In the same spirit, some markers used to predict a worse prognosis in COVID-19, such as serum ferritin, which are often adopted for clinical evaluation in the general population, have a controversial application in this group. The frequent blood transfusions and the state of chronic inflammation lead to higher baseline levels of ferritin in individuals with sickle cell disease. Thus, this parameter does not appear to have good predictive value for identifying immune dysregulation associated with SARS-CoV-2 infection in these individuals, which should also be considered by health professionals in their routine (102).
Finally, some studies suggest that when it comes to COVID-19, individuals with sickle cell disease or sickle cell trait have similar rates of death, hospitalization, and ICU admission compared to people without sickle cell disease or sickle cell trait (31, 34, 42, 47, 49, 58, 70, 80, 85, 87, 108). These papers did not identify mechanisms related to sickle cell disease that act directly in the clinical course of COVID-19 but instead highlighted features also observed in the general population, such as the existence of other comorbidities, advanced age, and the presence of organ damage, as risk factors for unfavorable outcomes (57, 59).
4.2. COVID-19 as a trigger for sickle cell disease complications
Similar to what is observed for other viral infections, COVID-19 appears to be able to precipitate acute complications typical of sickle cell disease. These manifestations have been reported since the beginning of the pandemic with significant frequency, although the cause-effect correlation cannot always be clearly determined. There are points of disagreement about the biological impact of COVID-19 in individuals with sickle cell disease, but most authors seem to agree that SARS-CoV-2 can act as a trigger for vaso-occlusive crises and acute chest syndrome (14, 29, 30, 32, 34, 37, 39, 42, 43, 45, 46, 67, 71, 72, 74, 75, 77, 79, 82, 84, 86, 90, 92, 98, 104, 106, 109, 112, 118). Explanations for this are grounded in empirical data and well-established knowledge about the mechanisms by which infections trigger complications of sickle cell disease. During an infectious process, there is an exacerbation of the chronic inflammatory state inherent in sickle cell disease. The recruitment of leukocytes, the release of cytokines, and direct injury to the endothelium further increase the hypercoagulability phenomena, with amplification of vasoconstriction, platelet stimulation, and secretion of adhesion molecules, propitiating the occurrence of vaso-occlusion and associated symptoms (2, 3).
There is not much evidence on the real impact of these events on the morbidity and mortality of COVID-19 among individuals with sickle cell disease, but acute chest syndrome is one of the leading causes of death in this population (6). Therefore, there is a substantial potential for an unfavorable clinical course in these cases. In addition, sickle cell complications are associated with higher rates of hospitalization (72, 88) and, of course, with the expenditure of more therapeutic resources, such as oxygen supplementation, antibiotic therapy, and blood transfusions. In contrast, Alkindi et al. (31) show that the impact of COVID-19 on the morbidity and mortality of vaso-occlusive crises among individuals with sickle cell anemia was not significant. The occurrence of other sickle cell complications in the context of COVID-19, such as osteonecrosis, acute hemolytic crisis, post-transfusion hyperhemolysis syndrome, and splenic sequestration, has also been reported, although in a minor incidence (31, 65, 89, 97).
4.3. The influence of different genotypes
Some studies suggest that the clinical course of SARS-CoV-2 infection in sickle cell disease patients may vary according to their genotype. In certain samples, more severe cases of COVID-19 were seen in milder genotypes, especially the HbSC genotype, while among genotypes associated with more severe manifestations of sickle cell disease, such as HbSS and HbSβ-, COVID-19 was more commonly observed in its milder form (34, 35, 83, 88, 90, 114). At first glance, these observations are consistent with the hypotheses that chronic inflammation and hemolytic anemia could exert favorable effects on COVID-19 since these mechanisms would be more “active” in individuals with more severe genotypes. It is also worth noting that sickle cell individuals with severe genotypes are those who most often use hydroxyurea (59, 112), which could also have a favorable influence on the clinical course of COVID-19, as discussed earlier. In the Arlet et al. (114) cohort, the HbSC genotype was associated with a higher risk of mortality and development of thromboembolic events compared to the other groups (SS/Sβ-/Sβ+). According to these authors, this finding could be explained by SC hemoglobinopathy-specific endothelial dysfunctions; this would also explain higher mortality rates associated with this genetic profile in dengue cases, for example. There is, however, disagreement on the subject. Other studies, with similar levels of evidence, show more severe cases and higher hospitalization rates in individuals with HbSS and HbSSβ- genotypes (31, 36) or conclude that there is no relationship between sickle cell disease genotypes and the severity of COVID-19 (33, 59, 69).
The role of sickle cell trait in the clinical course of COVID-19 was also evaluated. Some researchers believed that the higher mortality observed among individuals from ethnic groups of African origin in the United Kingdom and the United States could be explained by differences in hemoglobin-producing genes, given the high prevalence of a sickle cell trait in this population (14, 41).
Resurreccion et al. (119) note that, even to a minor extent, carriers of the trait exhibit an increased mortality trend, as well as having a significantly higher cumulative risk if they have other associated comorbidities, such as diabetes. In addition, the study published by Verma et al. (110) reported that people with sickle cell trait are more likely to suffer from chronic kidney disease, diabetic kidney disease, hypertensive kidney disease, pulmonary embolisms, and cerebrovascular illnesses. Ultimately, this combination of factors appears to increase the risk of these individuals having worse outcomes in COVID-19, and independently, the infection itself seems to raise the risk for these individuals to develop acute kidney failure. Another paper reports a higher rate of intensive care unit admission in this population, as high as 36.4% (70). Furthermore, Clift et al. (40) reveal a 1.38 increased risk of hospitalization and a 1.51 increased risk for death among individuals with sickle cell trait and COVID-19.
At least two case reports describe individuals who discovered the status of sickle cell trait carrier at the onset of COVID-19, which triggered vaso-occlusive symptoms and endothelial dysfunction for the first time, making the diagnosis feasible. These situations also reveal a possible relationship of greater severity between the two clinical entities (45, 71).
The influence of the sickle cell trait on the evolution of COVID-19 remains controversial. Most papers refute the idea of increased risk, arguing that, after adjusting for the variables, sickle cell carriers have no significant differences in SARS-CoV-2 mortality compared with those without the trait. Socioeconomic vulnerabilities, from this point of view, appear to better explain the health disparities observed among the black population in the United Kingdom and the United States (15, 30, 49, 58, 69).
4.4. Therapeutic options
Blood transfusions, especially exchange transfusions, may benefit individuals with sickle cell disease and COVID-19, especially in the presence of significant anemia and acute chest syndrome (56, 57, 65, 74, 78, 81, 84, 90, 92, 106). However, there are disagreements regarding the early or prophylactic use of this measure. While some authors suggest that transfusion may be considered as early as possible (56, 65, 72, 78, 84, 90, 92), others believe that the criteria for use should be individualized and based on existing indication protocols (81). Likewise, there is no consensus when it comes to prophylactic anticoagulation. Many authors consider it plausible to intensify these regimens among sickle cell patients, given the potentially increased risk for coagulation disorders in this group (94, 103). Others, such as Singh et al. (108), facing the evidence that the risks are similar to those observed in the general population, suggest that anticoagulation should be carried out rationally, following the guidelines adopted in each institution.
A case report discusses the use of Voxelotor, an inhibitor of HbS polymerization that increases the affinity of hemoglobin for oxygen, as an alternative for sickle cell disease patients infected with SARS-CoV-2 to avoid transfusions (44). Approved by the Food and Drug Administration in 2019, this substance has been used in the treatment of sickle cell disease, usually in continuous schemes (93). The application in an acute situation, in an individual with pneumonia, falling hemoglobin levels, and a history of transfusion of two units of leukoreduced red blood cells without response, was quite satisfactory, leading to improvements in clinical and laboratory parameters that were observed after the second day of administration, without the need to resort to erythrocytapheresis (44).
The administration of tocilizumab, an anti-human IL-6 receptor monoclonal antibody that inhibits signal transduction by binding to sIL-6R and mIL-6R, has been described in some case reports of sickle cell individuals infected by the SARS-CoV-2, demonstrating successful results (74, 77, 79, 97). This resource, which has even been made available to the general population in some places, should be considered for patients at higher risk of developing a hyperinflammatory syndrome or sickle cell complications, for example (74, 120).
It was identified that four cases of extracorporeal membrane oxygenation (ECMO) had been performed in patients with sickle cell disease infected with SARS-CoV-2, all of which had relatively satisfactory outcomes (66, 72, 101). The use in patients with acute chest syndrome is particularly noteworthy, considering that ECMO has unfavorable repercussions and is not usually indicated in these situations. The successful application in these cases may indicate that the pathophysiology of this sickle cell complication in the setting of COVID-19 has particularities when contrasting with other triggering viral conditions (72, 101).
It should also be emphasized that oxygen support, antibiotic therapy, analgesia, and hydration—pillars in the management of acute episodes of sickle cell disease—must not be ignored or underestimated in COVID-19, even to the detriment of more modern therapeutic options. It is crucial to use these measures as soon as possible to ensure patient stabilization and reduce morbidity and mortality (72).
Vaccination, an essential tool for reducing mortality from infectious causes in this population, should also be encouraged in all age groups, as it has been for the general population (2, 47, 106). Studies show that there may be some hesitation among people with sickle cell disease regarding the safety profile of immunizers against SARS-CoV-2 and the occurrence of adverse effects (121). Therefore, professionals must clarify possible myths and highlight the proven benefits of vaccination. Studies, such as Friedman et al. (122), which show no association between vaccination and the occurrence of pain episodes in this population, can be used to corroborate the safety of the COVID-19 vaccines.
4.5. Study limitations
Despite the methodological rigor, this study has some limitations. One of them is temporal, as we included articles published up to October 2022. Although there is a downward trend in scientific production as the pandemic advances, it is possible that relevant studies published later were missed.
Another limitation is regarding the lower levels of evidence of most of the primary articles included in the review, which prevents us from postulating more robust generalizations and indicates the need to expand the research on the subject. In addition, considering that this study included articles from several countries, it is likely that varying treatment guidelines for COVID-19 across these regions and over the period considered in the search make it difficult to generalize the findings about this specific topic.
5. Conclusion
Data analysis available in the literature on the impact of COVID-19 in individuals with sickle cell disease reveals many divergences, especially about the role of molecular mechanisms associated with sickle cell pathogenesis, such as chronic inflammation, hypercoagulability, and hemolytic anemia; and factors of possible indirect influence, namely the use of hydroxyurea and access to medical care. The studies lead us to conclude, however, that SARS-CoV-2, similar to other viral agents, is capable of acting as a precipitator of typical sickle cell disease events, especially acute chest syndrome and vaso-occlusive crises, historically linked to increased morbidity and mortality. Moreover, COVID-19 has the potential to present clinically in an atypical form in this group, often with the absence of respiratory symptoms.
Thus, more than outlining individuals with sickle cell disease as part or not of a risk group, this information highlights the need to direct investments toward robust research that is able to broaden the understanding of the particularities of the clinical course of SARS-CoV-2 infection in the context of sickle cell disease, including the expansion of topics such as incidence of thromboembolic events and the role of different genotypes. Providing insight into these fields may also contribute to a better understanding of the underlying pathophysiology of sickle cell disease and COVID-19. In addition, the data draw attention to the importance of capacitating healthcare services and professionals regarding the management of SARS-CoV-2-infected sickle cell individuals. Specific guidelines and therapeutic protocols should include close monitoring, extensive testing, and the use of different therapeutic resources according to the severity of the clinical presentation. Public policies directed to sickle cell individuals must be considered.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
LP: conceptualization, data curation, formal analysis, interpretation, and drafting the original manuscript. MS: data curation, formal analysis, interpretation, and reviewing the manuscript. CG and IE: formal analysis, interpretation, and reviewing the manuscript. DM: conceptualization, data curation, formal analysis, interpretation, project management, and reviewing the manuscript. All authors participated in the final approval of the version submitted.
Funding
This work was supported by the São Paulo Research Foundation (Fundação de Amparo à Pesquisa do Estado de São Paulo) - FAPESP, grant 21/06191-9. The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
The authors would like to thank Daniel Souza da Silva for his assistance in updating the database searches. The authors would also like to thank FAPESP (21/06191-9) for the financial support of this project and for all the institutional actions to promote science in Brazil.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1144226/full#supplementary-material
References
1. Azar S, Wong TE. Sickle cell disease: a brief update. Med Clin North Am. (2017) 101:375–93. doi: 10.1016/j.mcna.2016.09.009
2. Kato GJ, Piel FB, Reid CD, Gaston MH, Ohene-Frempong K, Krishnamurti L, et al. Sickle cell disease. Nat Rev Dis Prim. (2018) 4:1–22. doi: 10.1038/nrdp.2018.10
3. Piel FB, Steinberg MH, Rees DC. Sickle cell disease. N Engl J Med. (2017) 376:1561–73. doi: 10.1056/NEJMra1510865
4. Stuart MJ, Nagel RL. Sickle-cell disease. Lancet. (2004) 364:1343–60. doi: 10.1016/S0140-6736(04)17192-4
5. Piel FB. The present and future global burden of the inherited disorders of hemoglobin. Hematol Oncol Clin North Am. (2016) 30:327–41. doi: 10.1016/j.hoc.2015.11.004
6. Vichinsky EP, Neumayr LD, Earles AN, Williams R, Lennette ET, Dean D, et al. Causes and outcomes of the acute chest syndrome in sickle cell disease. N Engl J Med. (2000) 342:1855–65. doi: 10.1056/NEJM200006223422502
7. Manci EA, Culberson DE, Yang YM, Gardner TM, Powell R, Haynes J, et al. Causes of death in sickle cell disease: an autopsy study. Br J Haematol. (2003) 123:359–65. doi: 10.1046/j.1365-2141.2003.04594.x
8. World Health Organization (WHO). WHO Coronavirus (COVID-19) Dashboard. (2020) https://covid19.who.int/ (accessed March 16, 2023).
9. Cevik M, Bamford CGG, Ho A. COVID-19 pandemic—a focused review for clinicians. Clin Microbiol Infect. (2020) 26:842–7. doi: 10.1016/j.cmi.2020.04.023
10. Kumar M, Al Khodor S. Pathophysiology and treatment strategies for COVID-19. J Transl Med. (2020) 18:353. doi: 10.1186/s12967-020-02520-8
11. Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA - J Am Med Assoc. (2020) 324:782–93. doi: 10.1001/jama.2020.12839
12. Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. (2021) 21: doi: 10.1186/s12879-021-06536-3
13. CDC. Science Brief: Evidence used to update the list of underlying medical conditions that increase a person's risk of severe illness from COVID-19. (2021) https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html#hemoglobin-disorders (accessed March 16, 2023).
14. Kehinde TA, Osundiji MA. Sickle cell trait and the potential risk of severe coronavirus disease 2019—A mini-review. Eur J Haematol. (2020) 105:519–23. doi: 10.1111/ejh.13478
15. Panepinto JA, Brandow A, Mucalo L, Yusuf F, Singh A, Taylor B, et al. Coronavirus disease among persons with sickle cell disease, United States, March 20–May 21, 2020. Emerg Infect Dis. (2020) 26:2473–76. doi: 10.3201/eid2610.202792
16. Singh A, Brandow AM, Panepinto JA. COVID-19 in individuals with sickle cell disease/trait compared with other Black individuals. Blood Adv. (2021) 5:1915–21. doi: 10.1182/bloodadvances.2020003741
17. Souza MT De, Silva MD da, Carvalho R De. Integrative review: what is it? How to do it? Einstein (São Paulo). (2010) 8:102–6. doi: 10.1590/s1679-45082010rw1134
18. Hopia H, Latvala E, Liimatainen L. Reviewing the methodology of an integrative review. Scand J Caring Sci. (2016) 30:662–9. doi: 10.1111/scs.12327
19. Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. (2005) 52:546–53. doi: 10.1111/j.1365-2648.2005.03621.x
20. Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. (2021) 372:n160. doi: 10.1136/bmj.n160
21. Moher D, Liberati A, Tetzlaff J, Altman D. Principais itens para relatar Revisões sistemáticas e Meta-análises: A recomendação PRISMA. Epidemiol e Serviços Saúde. (2015) 24:335–42. doi: 10.5123/S1679-49742015000200017
22. Stillwell SB, Fineout-Overholt E, Melnyk BM, Williamson KM. Evidence-Based Practice, Step by Step: Asking the Clinical Question. AJN, Am J Nurs. (2010) 110:58–61. doi: 10.1097/01.NAJ.0000368959.11129.79
23. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. (2016) 5:1–10. doi: 10.1186/s13643-016-0384-4
25. Melnyk B, Fineout- Overholt E. Evidence-Based Practice in Nursing and Healthcare: A Guide to Best Practice. 1st ed. Philadelphia, PA: Lippincott Williams and Wilkins (2005).
26. Stillwell SB, Fineout-Overholt E, Melnyk BM, Williamson KM. Evidence-based practice, step by step: searching for the evidence. Am J Nurs. (2010) 110:41–7. doi: 10.1097/01.NAJ.0000372071.24134.7e
27. Kiger ME, Varpio L. Thematic analysis of qualitative data: AMEE Guide No. 131 Med Teach. (2020) 42:846–54. doi: 10.1080/0142159X.2020.1755030
28. Thomas DR, A. General Inductive Approach for Analyzing Qualitative Evaluation Data. Am J Eval. (2006) 27:237–46. doi: 10.1177/1098214005283748
29. Alghamdi BM, Kashari OF. Hepatobiliary manifistations of COVID-19 in sickle cell disease: a case report. Blood. (2020) 136:33–4. doi: 10.1182/blood-2020-142657
30. Al-Hebshi A, Zolaly M, Alshengeti A, Al Qurainees G, Yamani S, Hamdan N, et al. Saudi family with sickle cell disease presented with acute crises and COVID-19 infection. Pediatr Blood Cancer. (2020) 67:10–2. doi: 10.1002/pbc.28547
31. Alkindi S, Elsadek RA, Al-Madhani A, Al-Musalhi M, AlKindi SY, Al-Khadouri G, et al. Impact of COVID-19 on vasooclusive crisis in patients with sickle cell anaemia. Int J Infect Dis. (2021) 106:128–33. doi: 10.1016/j.ijid.2021.03.044
32. Al Yazidi LS, Al Hinai Z, Al Waili B, Al Hashami H, Al Reesi M, Al Othmani F, et al. Epidemiology, characteristics and outcome of children hospitalized with COVID-19 in Oman: a multicenter cohort study. Int J Infect Dis. (2021) 104:655–60. doi: 10.1016/j.ijid.2021.01.036
33. Anusim N, Gupta R, Ahaneku H, Franklin C, Balaraman S, Huben M, et al. Presentation, management, and outcomes of COVID-19 in patients with sickle cell disease. eJHaem. (2021) 2:121–4. doi: 10.1002/jha2.162
34. Arlet J-B, de Luna G, Khimoud D, Odièvre M-H, de Montalembert M, Joseph L, et al. Prognosis of patients with sickle cell disease and COVID-19: a French experience. Lancet Haematol. (2020) 7:e632–4. doi: 10.1016/S2352-3026(20)30204-0
35. Azerad M, Bayoudh F, Weber T, Minon J, Ketelslegers O, Hoyoux M, et al. Sickle cell disease and COVID-19: atypical presentations and favorable outcomes. eJHaem. (2020) 1:338–41. doi: 10.1002/jha2.74
36. Balanchivadze N, Kudirka AA, Askar S, Almadhoun K, Kuriakose P, Fadel R, et al. Impact of COVID-19 infection on 24 patients with sickle cell disease. One Center Urban Exp Hemoglobin. (2020) 44:284–9. doi: 10.1080/03630269.2020.1797775
37. Beerkens F, John M, Puliafito B, Corbett V, Edwards C, Tremblay D. COVID-19 pneumonia as a cause of acute chest syndrome in an adult sickle cell patient. Am J Hematol. (2020) 95:E154–6. doi: 10.1002/ajh.25809
38. Boga C, Asma S, Leblebisatan G, Sen N, Tombak A, Demiroglu YZ, et al. Comparison of the clinical course of COVID-19 infection in sickle cell disease patients with healthcare professionals. Ann Hematol. (2021) 100:2195–202. doi: 10.1007/s00277-021-04549-1
39. Chen-Goodspeed A, Idowu M. COVID-19 presentation in patients with sickle cell disease: a case series. Am J Case Rep. (2021) 22:1758. doi: 10.12659/AJCR.931758
40. Clift AK, Saatci D, Coupland CAC, Dambha-Miller H, Hippisley-Cox J. Sickle cell disorders and severe COVID-19 outcomes: a cohort study. Ann Intern Med. (2021) 174:1483–7. doi: 10.7326/M21-1375
41. Cook M. Potential factors linked to high COVID-19 death rates in British minority ethnic groups. Lancet Infect Dis. (2021) 21:e68. doi: 10.1016/S1473-3099(20)30583-1
42. De Luna G, Lemonier N, Aidan A, Bontemps L, Hautefaye M, Diakonoff H, et al. Pham Hung D'Alexandry D'Orengiani A-L, Bachir D, Driss F, et al. Drepadom - home care services and hospitalizations for sickle cell disease patients during the COVID-19 pandemic. Blood. (2020) 136:12–12. doi: 10.1182/blood-2020-142796
43. Español MG, Gardner R V, Alicea-Marrero MM, Marrero-Rivera G, Bradford T, LeBlanc DM, et al. Multisystem inflammatory syndrome in a pediatric patient with sickle cell disease and COVID-19: a case report. J Pediatr Hematol Oncol. (2022) 44:E134–7. doi: 10.1097/MPH.0000000000002191
44. Ershler WB, Holbrook ME. Sickle cell anemia and COVID-19: Use of voxelotor to avoid transfusion. Transfusion. (2020) 60:3066–7. doi: 10.1111/trf.16068
45. Freitas LAR, Carvalho LVS, Fontes JLM, Souza CS, Santos RB, Cardoso LT, et al. Vaso-occlusive crisis in a patient with sickle cell trait and COVID-19. J Cell Mol Med. (2021) 25:10318–20. doi: 10.1111/jcmm.16948
46. Fronza M, Bardaro F, Stirpe E. Acute lung failure due to COVID-19 in a patient with sickle cell anemia. Minerva Pneumol. (2020) 59:44–6. doi: 10.23736/S0026-4954.20.01880-5
47. Hall R, Meenan J, Mihalca D, Katumba A, Badle S, Osakonor D, et al. The real impact of COVID-19 on an East London Sickle cell population: results of a service-wide survey. Br J Haematol. (2021) 195:532–5. doi: 10.1111/bjh.17740
48. Hippisley-Cox J, Coupland CAC, Mehta N, Keogh RH, Diaz-Ordaz K, Khunti K, et al. Risk prediction of covid-19 related death and hospital admission in adults after covid-19 vaccination: National prospective cohort study. BMJ. (2021) 374: 2244. doi: 10.1136/bmj.n2244
49. Hoogenboom WS, Fleysher R, Soby S, Mirhaji P, Mitchell WB, Morrone KA, et al. Individuals with sickle cell disease and sickle cell trait demonstrate no increase in mortality or critical illness from COVID-19 - a fifteen hospital observational study in the Bronx, New York. Haematologica. (2021) 106:3014–6. doi: 10.3324/haematol.2021.279222
50. Hussain FA, Njoku FU, Saraf SL, Molokie RE, Gordeuk VR, Han J. COVID-19 infection in patients with sickle cell disease. Br J Haematol. (2020) 189:851–2. doi: 10.1111/bjh.16734
51. John NA, John JE. Implications of COVID-19 infections in sickle cell disease. Pan Afr Med J. (2020) 36:81. doi: 10.11604/pamj.2020.36.158.24011
52. John NA, John J, Kamblec P, Singhal A, Daulatabad V, Vamshidhar IS. Patients with sticky platelet syndrome, sickle cell disease and glanzmann syndrome may promulgate severe thrombosis if infected with covid-19. Maedica. (2021) 16:268–73. doi: 10.26574/maedica.2020.16.2.268
53. Kasinathan S, Mohammad Ashraf H, Minkowitz S, Adeyinka A, Bailey-Correa K. COVID-19 infection and acute pulmonary embolism in an adolescent female with sickle cell disease. Cureus. (2020) 12:12348. doi: 10.7759/cureus.12348
54. Kingsley A, Betta EC, Edakabasi A, Ofonime E, Philemon BG. Successful management of sickle cell disease patient with covid-19 infection in a low resource setting: case study. J Pharm Res Int. (2021) 33:110–4. doi: 10.9734/jpri/2021/v33i26A31475
55. Madany E, Okwan-Duodu D, Balbuena-Merle R, Hendrickson JE, Gibb DR. Potential implications of a type 1 interferon gene signature on covid-19 severity and chronic inflammation in sickle cell disease. Front Med. (2021) 8:679030. doi: 10.3389/fmed.2021.679030
56. Mazloom A, Nimkar N, Paul S, Baptiste A. Clinical course and outcomes of sickle cell disease patients with COVID-19 at a new york hospital. Blood. (2020) 136:34–6. doi: 10.1182/blood-2020-143022
57. McCloskey KA, Meenan J, Hall R, Tsitsikas DA. COVID-19 infection and sickle cell disease: a UK centre experience. Br J Haematol. (2020) 190:E57–8. doi: 10.1111/bjh.16779
58. Merz LE, Mistry K, Neuberg D, Freedman R, Menard G, Dorfman DM, et al. Impact of sickle cell trait on morbidity and mortality from SARS-CoV-2 infection. Blood Adv. (2021) 5:3690–3. doi: 10.1182/bloodadvances.2021004977
59. Minniti CP, Zaidi AU, Nouraie M, Manwani D, Crouch GD, Crouch AS, et al. Clinical predictors of poor outcomes in patients with sickle cell disease and COVID-19 infection. Blood Adv. (2021) 5:207–15. doi: 10.1182/bloodadvances.2020003456
60. Mitchell WB, Davila JG, Keenan J, Jackson J, Tal A, Morrone KA. Children and young adults admitted to a NYC children's hospital had a similar rate of severe COVID-19 coagulopathy as that reported in older adults. Blood. (2020) 136:794. doi: 10.1182/blood-2020-138794
61. Mucalo L, Brandow AM, Dasgupta M, Mason SF, Simpson PM, Singh A, et al. Comorbidities are risk factors for hospitalization and serious COVID-19 illness in children and adults with sickle cell disease. Blood Adv. (2021) 5:2717–24. doi: 10.1182/bloodadvances.2021004288
62. Noisette L, Mandava M, Gregoski M, Bergmann S. Sickle cell disease related outcomes in patients evaluated for COVID-19 infections in south carolina. Blood. (2020) 136:38–9. doi: 10.1182/blood-2020-141359
63. Noun P, Ibrahim A, Hodroj MH, Bou-Fakhredin R, Taher AT. COVID-19 in benign hematology: emerging challenges and special considerations for healthcare professionals. Expert Rev Hematol. (2020) 13:1081–92. doi: 10.1080/17474086.2020.1819785
64. Nur E, Gaartman AE, van Tuijn CFJ, Tang MW, Biemond BJ. Vaso-occlusive crisis and acute chest syndrome in sickle cell disease due to 2019 novel coronavirus disease (COVID-19). Am J Hematol. (2020) 95:725–6. doi: 10.1002/ajh.25821
65. Okar L, Rezek M, Gameil A, Mulikandayhil Y, Yassin MA. Severe hemolysis and vaso-occlusive crisis due to COVID-19 infection in a sickle cell disease patient improved after red blood cell exchange. Clin Case Rep. (2021) 9:2117–21. doi: 10.1002/ccr3.3960
66. Parodi E, Voi V, Vania B, Lonardi P, Saracco P, Longobardo A, et al. Simultaneous diagnosis of severe SARS-CoV-2 infection and sickle cell disease in two infants. Blood Transfus. (2021) 19:120–3. doi: 10.2450/2021.0430-20
67. Sahu KK, George L, Jones N, Mangla A. COVID-19 in patients with sickle cell disease: a single center experience from Ohio, United States. J Med Virol. (2021) 93:2591–4. doi: 10.1002/jmv.26816
68. Sahu KK, Siddiqui AD, Cerny J. Managing sickle cell patients with COVID-19 infection: the need to pool our collective experience. Br J Haematol. (2020) 190:e86–9. doi: 10.1111/bjh.16880
69. Sayad B, Karimi M, Rahimi Z. Sickle cell disease and COVID-19: Susceptibility and severity. Pediatr Blood Cancer. (2021) 68:1–9. doi: 10.1002/pbc.29075
70. Sewaralthahab S, Smith H. Outcomes of sickle cell disorders in COVID-19 infection: an institutional experience. Blood. (2020) 136:30–1. doi: 10.1182/blood-2020-139365
71. Sheha D, El-Shayeb M, Eid Y, Amin M, Saeed A, Abdou D, et al. Unfolding of sickle cell trait by coronavirus disease 2019 (COVID-19) infection. Br J Haematol. (2020) 191:e38–40. doi: 10.1111/bjh.17089
72. Teulier M, Elabbadi A, Gerotziafas G, Lionnet F, Voiriot G, Fartoukh M. Severe COVID-19 with acute respiratory distress syndrome (ARDS) in a sickle cell disease adult patient: case report. BMC Pulm Med. (2021) 21:1–15. doi: 10.1186/s12890-021-01412-x
73. Dun C, Walsh CM, Bae S, Adalja A, Toner E, Lash TA, et al. A machine learning study of 534,023 medicare beneficiaries with COVID-19: implications for personalized risk prediction. medRxiv. (2020)1–17. doi: 10.1101/2020.10.27.20220970
74. De Luna G, Habibi A, Deux JF, Colard M, Pham Hung d'Alexandry d'Orengiani AL, Schlemmer F, et al. Rapid and severe Covid-19 pneumonia with severe acute chest syndrome in a sickle cell patient successfully treated with tocilizumab. Am J Hematol. (2020) 95:876–8. doi: 10.1002/ajh.25833
75. Subarna C, Giselle P-P, Fester I, Virginia T, Charlotte G, David R, Sara S-S. COVID-19 in patients with sickle cell disease - a case series from a UK Tertiary Hospital. Haematologica. (2020) 105:2691–3. doi: 10.3324/haematol.2020.254250
76. de Sanctis V, Canatan D, Corrons JLV, Karimi M, Daar S, Kattamis C, et al. Preliminary data on COVID-19 in patients with hemoglobinopathies: a multicentre ICET-A study. Mediterr J Hematol Infect Dis. (2020) 12:1–9. doi: 10.4084/mjhid.2020.046
77. Odièvre MH, de Marcellus C, Ducou Le Pointe H, Allali S, Romain AS, Youn J, et al. Dramatic improvement after tocilizumab of severe COVID-19 in a child with sickle cell disease and acute chest syndrome. Am J Hematol. (2020) 95:E192–4. doi: 10.1002/ajh.25855
78. Okar L, Aldeeb M, Yassin MA. The role of red blood cell exchange in sickle cell disease in patient with COVID-19 infection and pulmonary infiltrates. Clin Case Rep. (2021) 9:337–44. doi: 10.1002/ccr3.3526
79. Heilbronner C, Berteloot L, Tremolieres P, Dupic L, de Saint Blanquat L, Lesage F, et al. Patients with sickle cell disease and suspected COVID-19 in a paediatric intensive care unit. Br J Haematol. (2020) 190:e21–4. doi: 10.1111/bjh.16802
80. Hardy YO, Amenuke DAY, Abukari Y, Oti-Acheampong A, Hutton-Mensah K, Amoah-Dankwah J, et al. Clinical presentations and outcomes of COVID-19 infection in sickle cell disease patients: Case series from Komfo Anokye teaching hospital, Ghana. Clin Case Rep. (2021) 9:1018–23. doi: 10.1002/ccr3.3719
81. Morrone KA, Strumph K, Liszewski MJ, Jackson J, Rinke ML, Silver EJ, et al. Acute chest syndrome in the setting of SARS-CoV-2 infections—A case series at an urban medical center in the Bronx. Pediatr Blood Cancer. (2020) 67:2–7. doi: 10.1002/pbc.28579
82. Quaresima M, Quaresima V, Naldini MM, Cirillo DM, Ferrari A, Mazzi A, et al. Clinical management of a Nigerian patient affected by sickle cell disease with rare blood group and persistent SARS-CoV-2 positivity. eJHaem. (2020) 1:384–7. doi: 10.1002/jha2.53
83. Telfer P. De la Fuente J, Sohal M, Brown R, Eleftheriou P, Roy N, Piel FB, Chakravorty S, Gardner K, Velangi M, et al. Real-time national survey of COVID-19 in hemoglobinopathy and rare inherited anemia patients. Haematologica. (2020) 105:2651–4. doi: 10.3324/haematol.2020.259440
84. Appiah-Kubi A, Acharya S, Fein Levy C, Vlachos A, Ostovar G, Murphy K, et al. Varying presentations and favourable outcomes of COVID-19 infection in children and young adults with sickle cell disease: an additional case series with comparisons to published cases. Br J Haematol. (2020) 190:e221–4. doi: 10.1111/bjh.17013
85. Ramachandran P, Perisetti A, Kathirvelu B, Gajendran M, Ghanta S, Onukogu I, et al. Low morbidity and mortality with COVID-19 in sickle cell disease: a single center experience. eJHaem. (2020) 1:608–14. doi: 10.1002/jha2.87
86. Menapace LA, Thein SL. COVID-19 and sickle cell disease. Haematologica. (2020) 105:2501–4. doi: 10.3324/haematol.2020.255398
87. AbdulRahman A, AlAli S, Yaghi O, Shabaan M, Otoom S, Atkin SL, et al. COVID-19 and sickle cell disease in Bahrain. Int J Infect Dis. (2020) 101:14–6. doi: 10.1016/j.ijid.2020.09.1433
88. Sivalingam T, Inusa B, Doyle P, Oteng-Ntim E. COVID-19 and the pulmonary complications of sickle cell disease. eJHaem. (2020) 1:545–7. doi: 10.1002/jha2.105
89. Jacob S, Dworkin A, Romanos-Sirakis E. A pediatric patient with sickle cell disease presenting with severe anemia and splenic sequestration in the setting of COVID-19. Pediatr Blood Cancer. (2020) 67:2–3. doi: 10.1002/pbc.28511
90. Elia GM, Angel A, Regacini R, Nais RP, Santos ARA. dos, Vieira PPMG, Braga JAP. Acute chest syndrome and COVID-19 in sickle cell disease pediatric patients. Hematol Transfus Cell Ther. (2021) 43:104–8. doi: 10.1016/j.htct.2020.11.005
91. Justino CC, Campanharo FF, Augusto MN, Morais SC de, Figueiredo MS. COVID-19 as a trigger of acute chest syndrome in a pregnant woman with sickle cell anemia. Hematol Transfus Cell Ther. (2020) 42:212–4. doi: 10.1016/j.htct.2020.06.003
92. Allison D, Campbell-Lee S, Crane J, Vidanovic V, Webb S, Fraidenburg D, et al. Red blood cell exchange to avoid intubating a COVID-19 positive patient with sickle cell disease? J Clin Apher. (2020) 35:378–81. doi: 10.1002/jca.21809
93. Ali MA, Ahmad A, Chaudry H, Aiman W, Aamir S, Anwar MY. Efficacy and safety of recently approved drugs for sickle cell disease: a review of clinical trials. Exp Hematol. (2020) 92:11–18. doi: 10.1016/j.exphem.2020.08.008
94. Attoh SA, Sarkodie E, Fatchu R, Kuma ABA, Asumanu E, McAddy M, et al. COVID-19 and sickle cell disease: autopsy findings of three deaths at the 37 Military Hospital, Accra, Ghana. Pan Afr Med J. (2022) 41:30035. doi: 10.11604/pamj.2022.41.332.30035
95. Campbell JI, Dubois MM, Savage TJ, Hood-Pishchany MI, Sharma TS, Petty CR, Lamb GS, Nakamura MM. Comorbidities associated with hospitalization and progression among adolescents with symptomatic coronavirus disease 2019. J Pediatr. (2022) 245:102–10. doi: 10.1016/j.jpeds.2022.02.048
96. Dejong J, Sainato R, Forouhar M, Robinson D, Kunz A. Multisystem inflammatory syndrome in a previously vaccinated adolescent female with sickle cell disease. Pediatr Infect Dis J. (2022) 41:E104–5. doi: 10.1097/INF.0000000000003444
97. Fuja C, Kothary V, Carll TC, Singh S, Mansfield P, Wool GD. Hyperhemolysis in a patient with sickle cell disease and recent SARS-CoV-2 infection, with complex auto- and alloantibody work-up, successfully treated with tocilizumab. Transfusion. (2022) 62:1446–51. doi: 10.1111/trf.16932
98. Gupta A, Marzook H, Ahmad F. Comorbidities and clinical complications associated with SARS-CoV-2 infection: an overview. Clin Exp Med. (2022) 1:1–19. doi: 10.1007/s10238-022-00821-4
99. De Jesus GKG, De Araújo LT, Silva MB da. Aumento dos fatores de risco e suscetibilidade para o desenvolvimento de eventos tromboembólicos em indivíduos portadores de doença falciforme infectados pela Covid-19: uma revisão integrativa. Rev Ciências Médicas e Biológicas. (2021) 20:125. doi: 10.9771/cmbio.v20i1.37720
100. Hippisley-Cox J, Khunti K, Sheikh A, Nguyen-Van-Tam J, Coupland C. QCovid 4 - Predicting risk of death or hospitalisation from COVID-19 in adults testing positive for SARS-CoV-2 infection during the Omicron wave in England. medRxiv. (2022). doi: 10.1101/2022.08.13.22278733
101. Koh W, Malik P, Whitehead J, Morales DLS, Hayes D. Successful use of veno-venous extracorporeal membrane oxygenation for acute chest syndrome in a child with sickle cell disease and SARS-CoV-2. Pediatr Pulmonol. (2022) 57:1096–9. doi: 10.1002/ppul.25843
102. Lee JX, Chieng WK, Abdul Jalal MI, Tan CE, Lau SCD. Role of serum ferritin in predicting outcomes of COVID-19 infection among sickle cell disease patients: a systematic review and meta-analysis. Front Med. (2022) 9:919159. doi: 10.3389/fmed.2022.919159
103. Lubala TK, Kayembe-Kitenge T, Makinko P, Kalenga L, Kachil H, Kayembe A, et al. Deep venous thrombosis and acute pericarditis associated with severe acute respiratory syndrome coronavirus 2 infection in a Congolese infant with sickle cell disease: a case report. J Med Case Rep. (2022) 16:1–4. doi: 10.1186/s13256-022-03459-8
104. Mawalla WF, Nasser A, Jingu JS, Joseph H, Mmbaga LG, Shija E, et al. Acute chest syndrome and COVID-19 in hydroxyurea naïve sickle cell disease patient in a low resource setting. eJHaem. (2022) 3:507–12. doi: 10.1002/jha2.397
105. Mitra A, Mitra AD, Patel G, Dwyre DM, Graff JP. Leukoerythroblastosis in a sickle cell patient with pregnancy: an interesting peripheral blood smear finding. J Hematol. (2022) 11:15–20. doi: 10.14740/jh921
106. Santos OF. dos, Espósito TS, Almeida RDM, Santos ACA dos, Lopes JAS, Gusmão A do C, Magalhães NNS, Rodrigues DOW. Aspectos da assistência em pacientes com Doença Falciforme no contexto da pandemia da COVID-19. Rev Médica Minas Gerais. (2022) 32:1–7. doi: 10.5935/2238-3182.2022e32204
107. Silva-Pinto AC, Santos-Oliveira L, Santos FLS, Kashima Haddad S, De Santis GC, Do Tocantins Calado R. COVID-19 infection in sickle cell patients in a developing country: a case series. Acta Haematol. (2022) 145:1–4. doi: 10.1159/000519028
108. Singh A, Brandow AM, Wun T, Shet AS. COVID-19 and venous thromboembolism risk in patients with sickle cell disease. Blood Adv. (2022) 6:4408–12. doi: 10.1182/bloodadvances.2022007219
109. Tentolouris A, Stafylidis C, Siafarikas C, Dimopoulou MN, Makrodimitri S, Bousi S, et al. Favorable outcomes of patients with sickle cell disease hospitalized due to COVID-19: a report of three cases. Exp Ther Med. (2022) 23: 11268. doi: 10.3892/etm.2022.11268
110. Verma A, Huffman JE, Gao L, Minnier J, Wu WC, Cho K, et al. Association of kidney comorbidities and acute kidney failure with unfavorable outcomes after COVID-19 in individuals with the sickle cell trait. JAMA Intern Med. (2022) 182:796–804. doi: 10.1001/jamainternmed.2022.2141
111. Yurtsever N, Nandi V, Ziemba Y, Shi PA. Prognostic factors associated with COVID-19 related severity in sickle cell disease. Blood Cells, Mol Dis. (2021) 92:102627. doi: 10.1016/j.bcmd.2021.102627
112. Hoogenboom WS, Alamuri TT, McMahon DM, Balanchivadze N, Dabak V, Mitchell WB, et al. Clinical outcomes of COVID-19 in patients with sickle cell disease and sickle cell trait: a critical appraisal of the literature. Blood Rev. (2022) 53:100911. doi: 10.1016/j.blre.2021.100911
113. Waghmare R, Chaaithanya IK, Zala S, Deshmukh J, Uikey P, Wankhede S, et al. Outcomes of COVID-19 in pregnant women with sickle cell disease in India: a case series. Indian J Hematol Blood Transfus. (2022) 38:191–3. doi: 10.1007/s12288-021-01482-1
114. Arlet JB, Lionnet F, Khimoud D, Joseph L, de Montalembert M, Morisset S, et al. Risk factors for severe COVID-19 in hospitalized sickle cell disease patients: a study of 319 patients in France. Am J Hematol. (2022) 97:E86–91. doi: 10.1002/ajh.26432
115. Mulaku M, Opiyo N, Karumbi J, Kitonyi G, Thoithi G, English M. Evidence review of hydroxyurea for the prevention of sickle cell complications in low-income countries. Arch Dis Child. (2013) 98:908–14. doi: 10.1136/archdischild-2012-302387
116. Ben Moftah M, Eswayah A. Repurposing of hydroxyurea against COVID-19: a promising immunomodulatory role. Assay Drug Dev Technol. (2022) 20:55–62. doi: 10.1089/adt.2021.090
117. Abdelzaher MA, Ibrahim AES. Negm EM. Increasing fetal hemoglobin as a possible key for improvement of hypoxia and saving last breath in COVID-19 patient: “postulating a hypothesis” Egypt. J Bronchol. (2021) 15:33. doi: 10.1186/s43168-021-00078-7
118. Ali E, Hatim A, Yassin M. SARS-CoV-2 omicron variant may present with severe sickle cell painful crisis: a report of two cases. Clin Case Rep. (2022) 10:5934. doi: 10.1002/ccr3.5934
119. Resurreccion WK, Hulsizer J, Shi Z, Wei J, Wang CH, Na R, et al. Association of sickle cell trait with risk and mortality of COVID-19: results from the united kingdom biobank. Am J Trop Med Hyg. (2021) 105:368–71. doi: 10.4269/ajtmh.20-1657
120. Cortegiani A, Ippolito M, Greco M, Granone V, Protti A, Gregoretti C, et al. Rationale and evidence on the use of tocilizumab in COVID-19: a systematic review. Pulmonology. (2021) 27:52–66. doi: 10.1016/j.pulmoe.2020.07.003
121. Jan H, Waheeb A, AlAhwal H, Almohammadi A, Al-Marzouki A, Barefah A, et al. COVID-19 vaccine perception and hesitancy among patients with sickle cell disease in the western region of Saudi Arabia. Cureus J Med Sci. (2022) 14: 21026. doi: 10.7759/cureus.21026
Keywords: sickle cell disease, sickle cell trait, COVID-19, SARS-CoV-2 infection, acute chest syndrome, risk factors, hydroxyurea, disease management
Citation: Pereira LRG, da Silva MVG, Germano CMR, Estevao IF and Melo DG (2023) Impact of the SARS-CoV-2 infection in individuals with sickle cell disease: an integrative review. Front. Med. 10:1144226. doi: 10.3389/fmed.2023.1144226
Received: 14 January 2023; Accepted: 04 April 2023;
Published: 02 May 2023.
Edited by:
Wei Li, Marshall University, United StatesReviewed by:
Nitya Kumar, Royal College of Surgeons in Ireland – Medical University of Bahrain, BahrainJin Han, University of Illinois at Chicago, United States
Copyright © 2023 Pereira, da Silva, Germano, Estevao and Melo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Débora Gusmão Melo, dgmelo@ufscar.br
 Laura Resende Guimarães Pereira
Laura Resende Guimarães Pereira Maria Vitoria Gomes da Silva
Maria Vitoria Gomes da Silva Carla Maria Ramos Germano
Carla Maria Ramos Germano Isabeth F. Estevao
Isabeth F. Estevao Débora Gusmão Melo
Débora Gusmão Melo