- 1Institute of Immunology and Immunotherapy, College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
- 2Advanced Medical and Dental Institute, Universiti Sains Malaysia, Kepala Batas, Penang, Malaysia
- 3Centre for Clinical Haematology, Queen Elizabeth Hospital, Birmingham, United Kingdom
Introduction: NK cells play an important role in suppression of viral replication and are critical for effective control of persistent infections such as herpesviruses. Cytomegalovirus infection is associated with expansion of ‘adaptive-memory’ NK cells with a characteristic CD56dimCD16bright NKG2C+ phenotype but the mechanisms by which this population is maintained remain uncertain.
Methods: We studied NK cell reconstitution in patients undergoing haemopoietic stem cell transplantation and related this to CMV reactivation.
Results: NK cells expanded in the early post-transplant period but then remained stable in the absence of viral reactivation. However, CMV reactivation led to a rapid and sustained 10-fold increase in NK cell number. The proportion of NKG2C-expressing cells increases on all NK subsets although the kinetics of expansion peaked at 6 months on immature CD56bright cells whilst continuing to rise on the mature CD56dim pool. Phenotypic maturation was observed by acquisition of CD57 expression. Effective control of viral reactivation was seen when the peripheral NK cell count reached 20,000/ml.
Discussion: These data show that short term CMV reactivation acts to reprogramme hemopoiesis to drive a sustained modulation and expansion of the NK cell pool and reveal further insight into long term regulation of the innate immune repertoire by infectious challenge.
1. Introduction
Natural killer (NK) cells have the capacity to mediate lysis of virally-infected and transformed cells through integration of signalling from activating and inhibitory receptors (1, 2) and play an important role in the control of herpesvirus infections (3). Cytomegalovirus (CMV) is not cleared after initial infection but establishes a persistent infection which acts to shape the subsequent peripheral NK cell repertoire (4). In particular, CMV-seropositive people develop expansion of a population of ‘adaptive NK cells’ with a predominant CD56dimCD16brightNKG2C+CD57+ phenotype (5, 6). This may be driven largely by engagement of NKG2C with viral peptides from the UL40 protein presented by HLA-E on virally infected cells (7) although such populations are also observed in people with an NKG2C-/- genotype (8). The NKG2 proteins are important regulators of NK activation and both NKG2A and NKG2C form a heterodimer with CD94 that binds to HLA-E (9, 10). However, whilst NKG2A acts as an inhibitory receptor and is predominantly a marker of immature NK cells, NKG2C is an activating receptor that is expressed on highly differentiated populations. The potential functional importance of this adaptive NK cell subset remains somewhat unclear although it has high capacity for antibody-dependent cellular cytotoxicity (ADCC).
Allogeneic haemopoietic stem cell transplantation (HSCT) is an important therapeutic modality within haemato-oncology and has the potential to cure patients with chemotherapy-resistant disease (11). Much of this curative effect is mediated through the activity of the donor immune system (12) and there is increasing interest in the potential role of NK cells in this regard. The number of NK cells within the donor graft correlates with protection from disease relapse after allo-HSCT (13) and early NK reconstitution can help to suppress GvHD whilst increasing the ‘graft versus leukaemia’ effect (14–16). Patients are highly immune suppressed in the early period after HSCT and reactivation of CMV is an important clinical complication that is associated with increased rates of morbidity and mortality (17, 18). However, despite the increased short term clinical risk mediated by CMV reactivation it has also been demonstrated that viral reactivation may reduce subsequent post-transplant leukaemia relapse (19–21). The mechanism behind this observation remains uncertain but may relate to the generation of high numbers of CMV-driven donor NKG2C+ NK cells that increase capacity for control of host tumour cells.
Although CMV reactivation after hempoietic or solid organ transplantation has been shown to boost the number of mature NKG2C+ NK cells (22, 23) relatively little is known regarding the kinetics of this response from the time of reactivation. Here we determined the profile peripheral NK cell repertoire in patients after an episode of CMV reactivation following HSCT. Importantly, samples were taken immediately after viral reactivation and then followed prospectively. We observe that CMV viral reactivation leads to a long term expansion of NKG2C+ NK cells that transitions across the NK differentiation repertoire over a period of at least 10 months. Transient viral reactivation is thus seen to reprogramme long term NK cell differentiation and reveals further insights into pathogen-driven regulation of lymphopoiesis.
2. Materials and methods
2.1. Patients and control subjects
41 patients who had undergone allo-HSCT in the Queen Elizabeth Hospital were recruited at the time of CMV reactivation following written informed consent under the BOOST ethics (RG 13-172) according to Declaration of Helsinki. 60ml of peripheral blood in sodium heparin (BD Vacutainer®, Cat#367876) was collected for the first four weeks following CMV reactivation and 36ml of heparinised and clotted blood was also available pre-transplant, pre-reactivation and for up to 10 months post-transplant. Samples were also collected from patients undergoing allo-HSCT but without CMV reactivation (n=25) at equivalent time points pre- and post-transplant for use as controls. This group of patients were also followed for up to 10 months post-transplant.
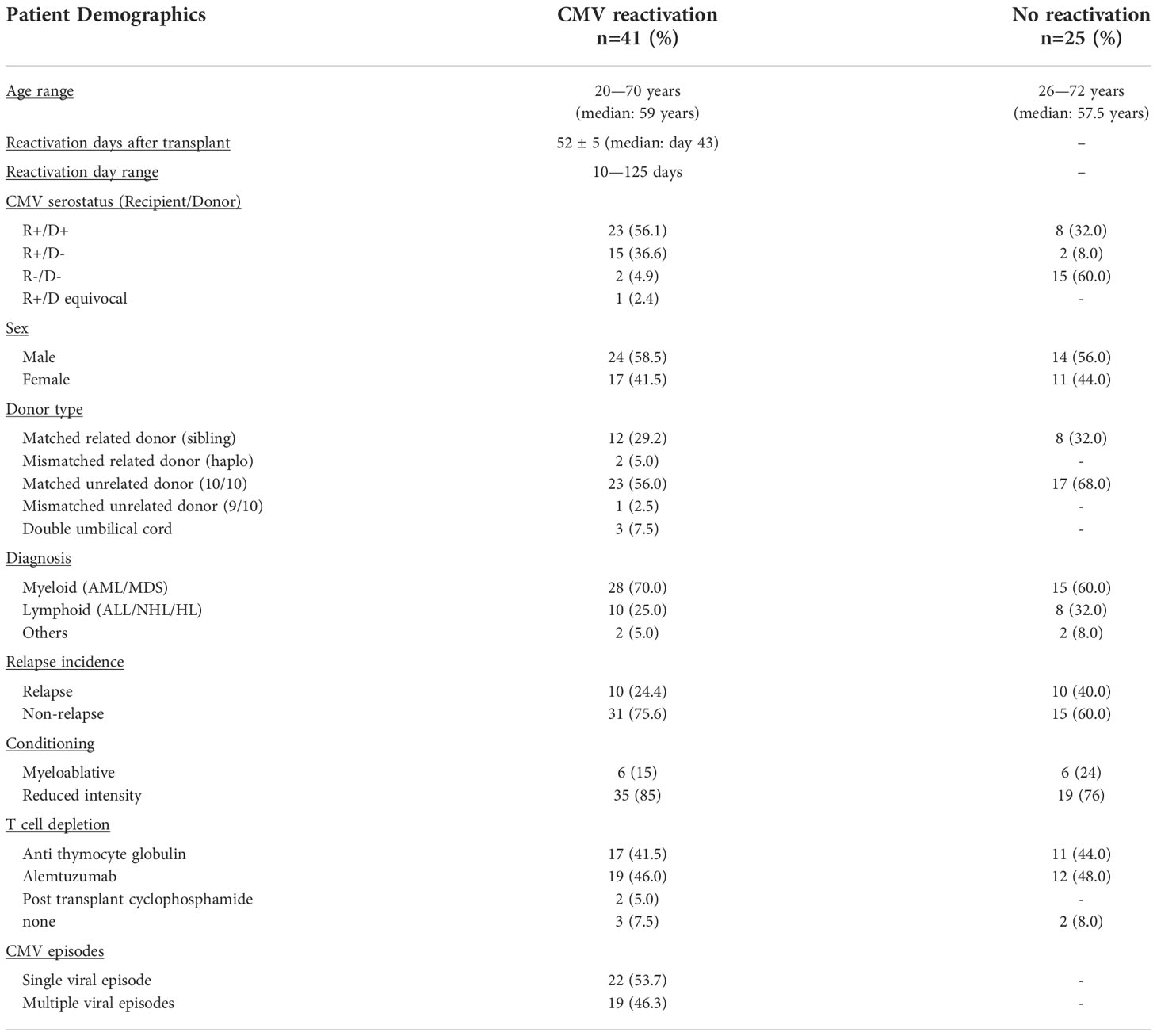
All 66 patients who underwent allo-HSCT with a 10/10 HLA-matched sibling or unrelated donor were recruited to this prospective study (Table 1) and PCR monitoring for CMV reactivation performed weekly. 12/66 (18%) patients received myeloablative transplants, 7 using myeloablative total body irradiation plus chemotherapy, and 5 chemotherapy alone. The remaining 82% (54/66) received reduced intensity chemotherapy conditioning. 61 patients (92%) received T cell depletion, with approximately half receiving ATG (n=28) or alemtuzumab (n=31), whilst 2 patients received post-transplant cyclophosphamide as part of a haploidentical transplant. All patients received ciclosporin based GvhD prophylaxis, with methotrexate added to myeloblative regimens, and mycophopheolate mofetil to all busulphan containing regimens. All patients received PBSC-mobilised stem cell grafts. Approximately one third of patients (n=20) had a matched related (sibling) donor, whilst two patients had a mismatched related haplo-identical donor. Almost two thirds of patients (n=40) had a matched (10/10) unrelated donor, and one had a 9/10 mismatched unrelated donor. The remaining 3 patients received double umbilical cord transplants. These baseline characteristics of patients are summarised in Table 1 and stratified according to the presence of subsequent CMV reactivation.
2.2. Assessment of CMV serostatus and CMV reactivation
Patients were routinely monitored for CMV reactivation by quantitative PCR and reactivation was diagnosed by value of >200 copies/ml of CMV DNA in whole blood. CMV viral load was monitored for each week following reactivation. Patients were classified according to their CMV serostatus pair; recipient positive and donor positive (R+/D+); recipient positive and donor negative (R+/D-); recipient negative and donor positive (R-/D+) and recipient negative and donor negative (R-/D-). Donors with ambiguous CMV serostatus are classified as equivocal (R+/Dequi).
All patients received anti-viral propylaxis with acyclovir. Patients with a matched unrelated donor received IV aciclovir 500mg/m2 tds until mucositis resolved and then 800mg qds orally until day +100. Those who received a stem cell graft from a sibling donor were given oral aciclovir 200mg qds until day +35. Following viral reactivation patients received valganciclovir when viral load was >10,000 copies/ml.
2.3. Healthy donors
40 healthy donors (HD) were used as controls following written informed consent (REC reference Number: 14/WM/1254). Up to 60 ml of peripheral blood was collected in sodium heparin tubes and CMV serostatus was determined.
2.4. Isolation of peripheral blood mononuclear cells
PBMCs were isolated by density gradient centrifugation over Lymphoprep™ (Stem cell Technologies, Cat #07861) within 24 hours of collection. Peripheral blood was diluted 1:1 with RPMI-1640 Medium (Sigma, Cat#R8758) with 1% Penicillin/Streptomycin (Gibco™ Cat#15070063), layered at a ratio of 2:1 and centrifuged at 2000 x g for 25 minutes (brake off). Buffy coats were harvested and resuspended in RPMI media and centrifuged at 500 x g for 10 minutes and the number of cells determined using a haemocytometer (Fast-Read 102®, Kova International, Cat #88010). Cells were washed and centrifuged at 500 x g for 10 minutes before being cryopreserved in freezing media (RPMI-1640 Medium [Sigma, Cat#R8758], 10% DMSO [Sigma, Cat #D2650]).
2.4.1. Surface flow cytometry analysis
Frozen cells were recovered by rapid thawing at 37°C in a water bath and centrifuging in pre-warmed growth media at 500 x g for 10 minutes. PBMCs were surface stained with series of antibodies (anti-human CD158 [KIR2DL1/S1/S3/S5]-FITC [BioLegend, Cat#339504], anti-human CD158b [KIR2DL2/L3, NKAT2]-FITC [BioLegend, Cat#312604], anti-human CD158e1 [KIR3DL1, NKB1]-FITC [BioLegend, Cat#312706], anti-human NKG2C/CD159c-PE [R&D Biosystems, Cat#FAB138P], anti-CD14-ECD [Beckman Coulter, Cat#IM2707U], anti-CD19-ECD [Beckman Coulter, Cat#A07770], anti-CD3-PerCP-Cy5.5 [Beckman Coulter, Cat#300328], anti-CD159a (NKG2A)-APC [Miltenyi Biotec; Cat#130-098-8123], anti-human CD56 (NCAM)-APC/Cy7 [BioLegend, Cat#318332], anti-human CD57-PB (BioLegend, Cat#322316], anti-human CD16-V500 [BD Biosciences, Cat#561314], anti-human CD69-PE-Cy7 [BioLegend, Cat#310190], anti-human CD279 (PD-1)-PE-Cy7 [BioLegend, Cat#329916], anti-KLRG1-APC-Vio770 [Miltenyi Biotec, Cat#322316], Live/Dead (PB) [Invitrogen, Cat#L34955]) were used. 5x105 to 1x106 cells were re-suspended in residual buffer and antibody panels added and incubated on ice for 20 to 30 minutes, then being washed in MACS buffer (1xPBS [Oxoid™/Thermo Scientific™ Cat#BR0014G], 0.5% BSA [Sigma, Cat#A7906] and 2mM EDTA [Sigma Cat#S8045] and centrifuged at 500 x g for 5 minutes. 1.5 µl of PI was also added and samples were run on the Gallios™ Flow Cytometer (Beckman Coulter, Inc).
2.5. Intracellular cytokines staining
one million PBMCs from CMV reactivation, without reactivation and healthy donors were co-cultured with K562 cells overnight (1:1 ratio) in incubator and suspended within 500 µl of growth media with of Brefeldin A (Sigma, Cat #B5936). The cells were spun down, washed next day. Surface markers were stained before the cells were fixed and permeabilized. At last anti-human TNF-α-AF488 [BioLegend, Cat#502917], anti-human IFN-γ-AF700 [BioLegend,Cat#502519] were added, incubated and washed. The data was collected from the Gallios™ and analysed using Kaluza® Flow Analysis software version 2.1a (Beckman Coulter Inc.).
2.5.1. Absolute NK cell count
The absolute NK cell count was calculated by applying the percentage of NK cells, according the flow cytometry staining (gated from the live and lymphocyte subsets, Supplementary Figure 1), to the total lymphocyte count (109/L) obtained from the clinical haematology laboratory.
2.6. Statistical analysis
Data were analysed by using Mann-Whitney test for comparison between patients’ groups and Wilcoxon sign rank test for different time-points within similar patients. Friedman test was used for comparison in more than two groups within similar group of patients. All sample sizes in the different time-points are small and treated as not normally distributed and analysed by using GraphPad Prism 8 and SPSS 20.
3. Results
3.1. CMV reactivation following HSCT drives rapid and long term expansion of NK cells
66 patients who underwent allo-HSCT with a 10/10 HLA-matched sibling or unrelated donor were recruited to this prospective study (Table 1) and PCR monitoring for CMV reactivation performed weekly. These baseline characteristics of patients are summarised in Table 1 and stratified according to the presence of subsequent CMV reactivation.
CMV reactivation was observed in 41 patients (62%) at an average time of 52 days post-transplant. Blood samples were then taken at the time of reactivation and at weeks 1, 2, 3, 4, and months 3, 6, 10, after CMV reactivation. Control post-transplant samples were also taken from patients without evidence of viral reactivation and were matched for equivalent timepoints of collection. Blood samples were also available pre-transplant and pre-reactivation from almost all donors.
In initial studies, the percentage of NK cells within peripheral blood was determined using flow cytometry (Figure 1). The proportion of NK cells was markedly higher in patients compared to healthy donors (HD) and reflects early and robust NK reconstitution in the early post-transplant setting. Indeed, NK cells comprised over 50% of PBMC within the first 4-weeks post-HSCT and prior to any episode of viral reactivation. This value remained stable following CMV reactivation before declining gradually after 4 weeks towards the normal range (Figure 1A). Moreover, the absolute number of NK cells also increased rapidly following CMV reactivation but then continued to rise further over the next 10 months. Indeed, values rose 11-fold from 3 cells/µl at the time of reactivation to 35 cells/µl at the final timepoint of assessment at 10 months (Figure 1C). In contrast, the NK cell number remained very stable in patients who did not experience CMV reactivation (Figure 1D). These observations reveal that short term CMV reactivation drives rapid and long term NK cell expansion.
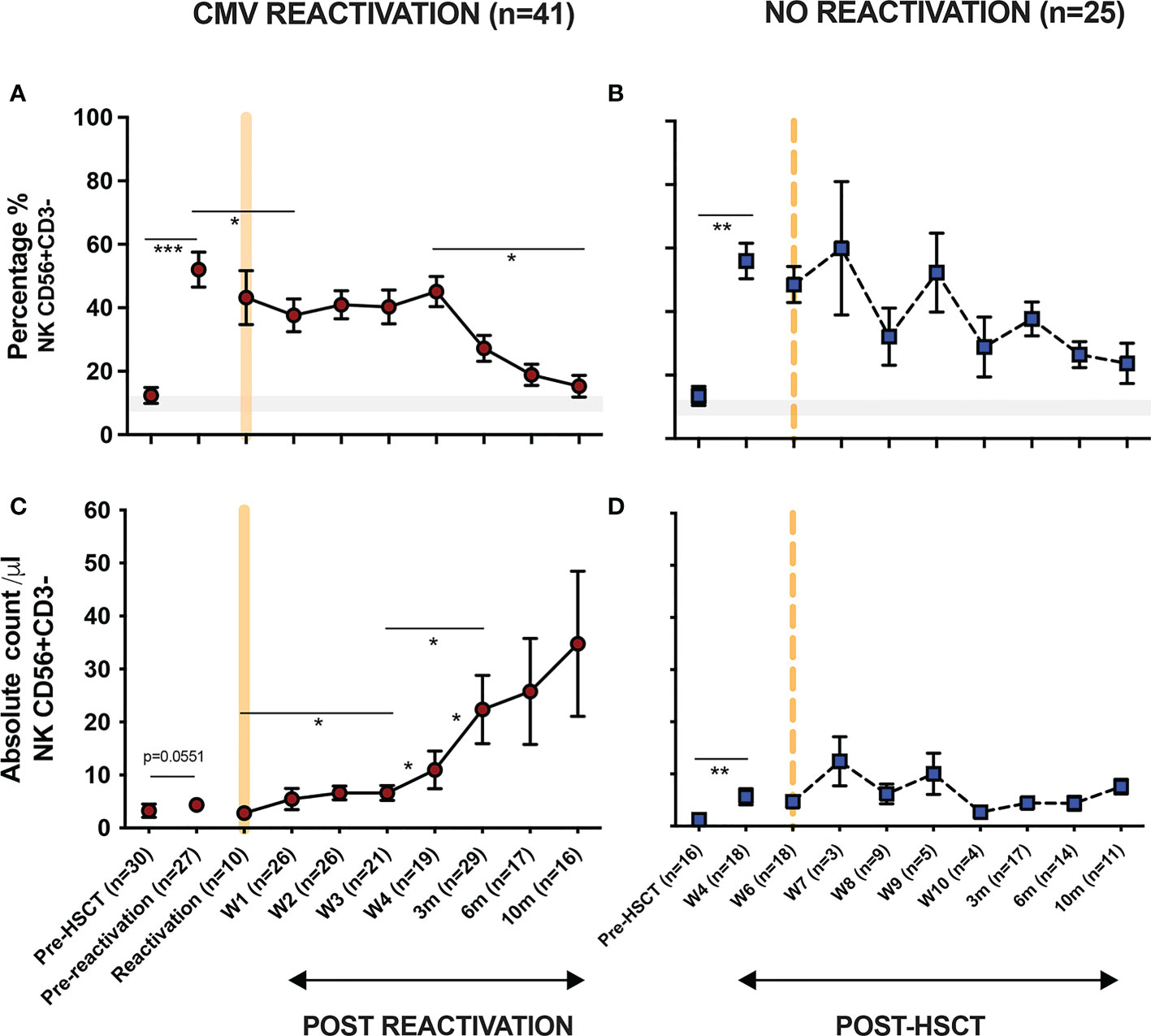
Figure 1 NK cells undergo long term expansion following short term CMV reactivation. The percentage and number of peripheral NK cells was measured at regular timepoints prior to, and following, an episode of CMV reactivation in patients after HSCT. Matched timepoint samples were obtained from patients without an episode of reactivation. Sample times are shown as week (W) or month (m). (A) Percentage of NK cells in patients with CMV reactivation. (B) Percentage of NK cells in patients without CMV reactivation. (C) Number of NK cells in patients with CMV reactivation. (D) Number of NK cells in patients without CMV reactivation. Patients were classified as undergoing an episode of CMV reactivation when viral load reached > 200 copies/ml. Grey line represents the percentage range of NK cells within healthy donors. (*p<0.05, **p<0.01, ***p<0.001; Wilcoxon sign rank test for matched time points).
3.2. CD56dim CD16bright NK cells expressing NKG2C undergo a rapid and sustained expansion following CMV reactivation in patients after allo-HSCT
CD56dim CD16bright NK cells comprise the dominant peripheral population of NK cells and we next went on to assess the relative expression of NKG2C and NKG2A on this subset in relation to CMV reactivation (Figure 2A). Average expression of NKG2C in healthy CMV seronegative donors was 1.4% ( ± 0.2) compared to 11% (± 3.5%) in seropositive individuals (p<0.0001). Values for NKG2A+ were 50% ( ± 2.6%) and 40% ( ± 3.2%) respectively (p=0.0065) indicating that CMV-driven expansion of the NKG2C+ pool comes at the expense of a decrease in the NKG2A+ repertoire (Figure 2B).
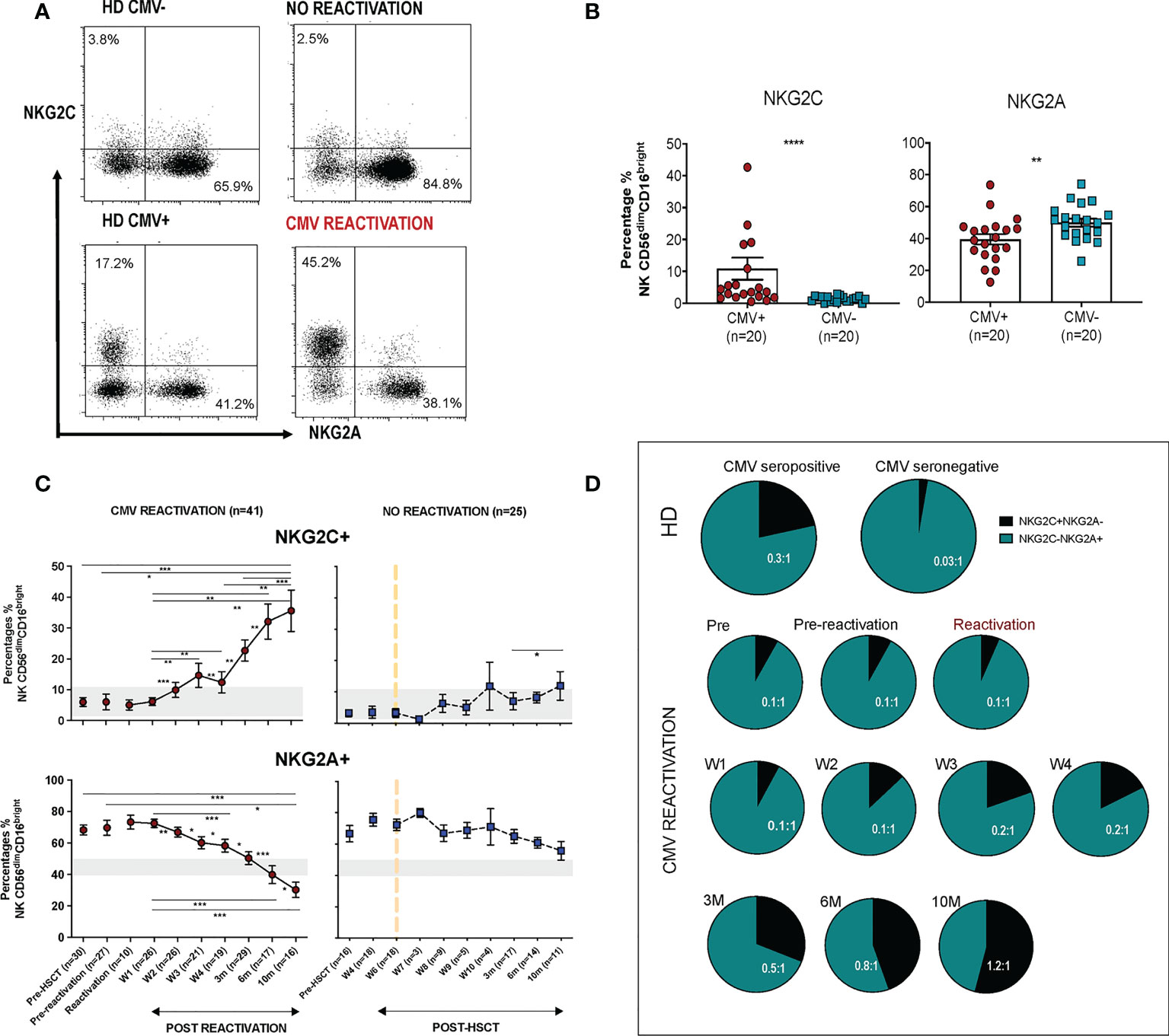
Figure 2 Rapid and long term expansion of the NKG2C+ NK cell subset following CMV reactivation in patients after allo-HSCT. (A) Gating examples to show NKG2C/NKG2A expression on CD56dimCD16bright NK subsets in CMV seropositive or seronegative healthy donors (HD) and allo-HSCT patients following CMV reactivation or no-reactivation. (B) Percentage of NKG2C+ and NKG2A+ NK cells within the CD56dimCD16bright subset in CMV seronegative and seropositive HDs. (**p<0.01, ****p<0.0001; Mann Whitney test). (C) Percentage of NKG2C+ (Top) and NKG2A+ (bottom) NK cells from CD56dimCD16bright population in patients following reactivation (left) and without reactivation patients (right). Grey lines represent the range of NKG2C+ and NKG2A+ NK cells in HDs. (*p<0.05, **p<0.01, ***p<0.001; Wilcoxon sign rank test for matched time points). (D) Ratio of NKG2C+ and NKG2A+ cells within CD56dimCD16bright population in HSCT patients with CMV reactivation and in healthy donors.
Within CMV-seropositive HSCT patients the percentage of NKG2C+ NK cells was comparable to that seen in CMV-seropositive controls prior to reactivation. However, a rapid expansion of CD56dimCD16bright NK cells expressing NKG2C was observed within the first 7 days after viral reactivation. Furthermore, this population continued to expand for a further 10 months following clearance of viral reactivation such that the NKG2C+ cell proportion represented up to 36% of the total NK cell pool, a value far higher than the normal range in CMV-seropositive healthy donors (Figure 2C). A much more modest increment was seen in patients who did not suffer an episode of CMV reactivation. The proportion of NKG2A+ cells within HSCT patients was initially higher than in healthy donors and is likely to reflect production of immature NKG2A+ NK cells during NK reconstitution. However, CMV reactivation accelerated NK cell maturation with an early decrease in the proportion of NKG2A+ cells after reactivation and a continuing fall to ~30% at month 10, a value below that seen in controls (Figure 2C).
The NKG2C:NKG2A ratio was next determined on the NK cell pool at different time points. Within healthy donors this was very low at 0.03:1 in CMV-seronegative people compared to 0.3:1 in the CMV-seropositive group (Figure 2D). Within HSCT patients the ratio was initially 0.1:1 but following viral reactivation it increased to reach 0.2-0.5:1 at 3 months, comparable to values seen in CMV-seropositive HD. Moreover, this increased further such that at 10 months the NKG2C+ cell percentage exceeded that of NKG2A+ with a ratio of 1.2:1. These data show that there is a rapid and long term expansion of the NKG2C+ NK cell subset following CMV reactivation in patients after allo-HSCT and that the relative proportion of this subset expands above that seen in healthy CMV seropositive people.
3.3. The proportion of NKG2C-expressing cells increases on all NK cells subsets following CMV reactivation and peaks earlier on immature populations
CMV-driven adaptive memory NK cells have been characterised previously only within the CD56dimCD16bright NK cell subset. The relative expression of CD16 and CD56 is a marker of NK cell differentation and, given the finding of increased NKG2C expression on the cytotoxic CD56dimCD16bright pool following CMV reactivation, we next went on to determine NKG2C and NKG2A expression on additional NK cell subsets (Figure 3A).
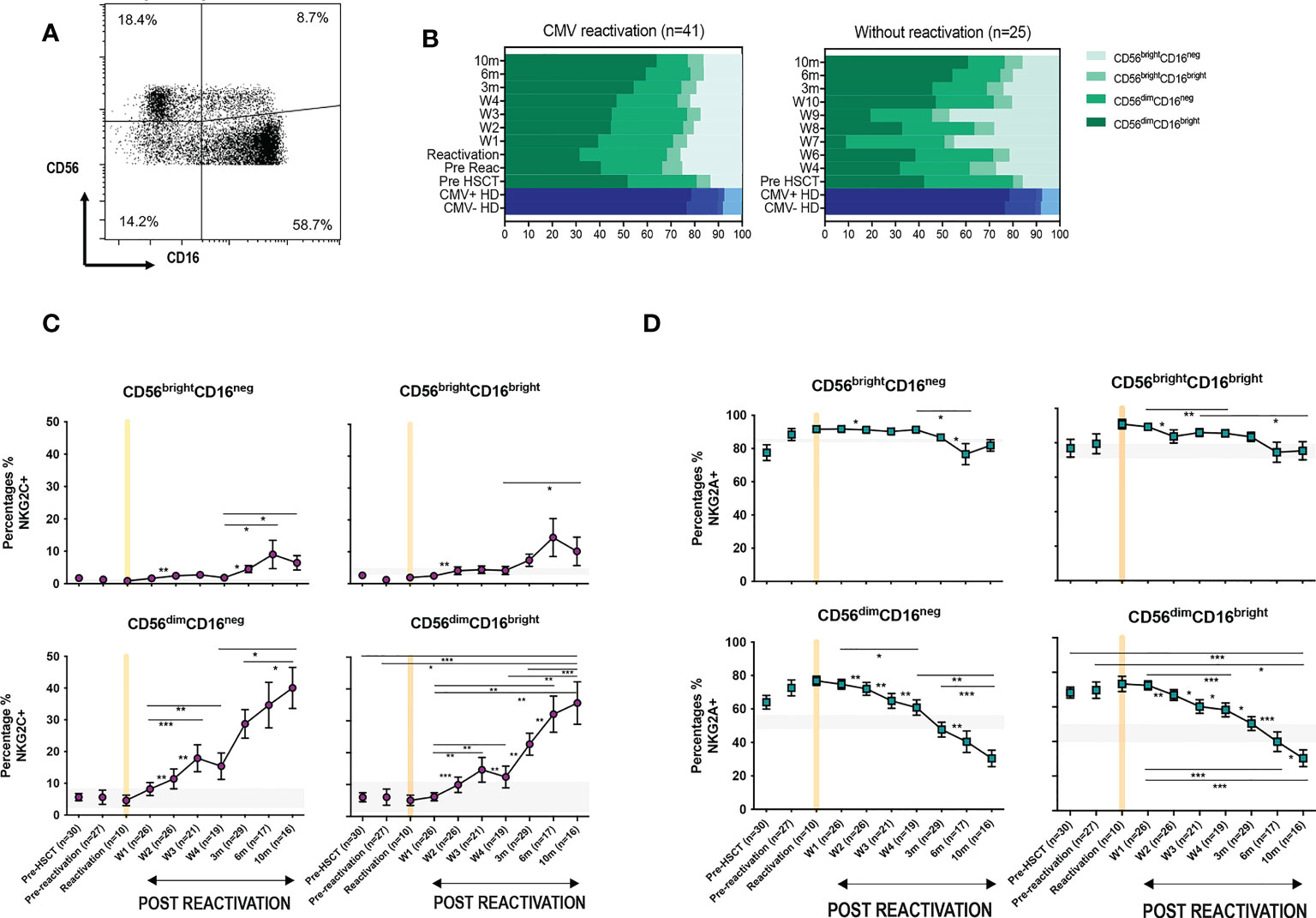
Figure 3 CMV reactivation leads to increased expression of NKG2C+ on all CD56dim and CD56bright subpopulations. (A) Gating to show separation of four NK subsets according to CD16 and CD56 expression. (B) Relative distribution of NK subsets in patients following CMV reactivation (left) and those without reactivation (right) Blue bars represent the NK subsets in CMV+ and CMV- HDs. (C) Relative NKG2C expression on NK subsets following CMV reactivation. (D) Relative NKG2A expression on NK subsets following CMV reactivation. Grey lines represent the range of NKG2C+ and NKG2A+ NK cells in HDs. (*p<0.05, **p<0.01, ***P<0.001; Wilcoxon sign rank test for matched time points).
The percentage of CD56bright cells was increased in HSCT patients compared with controls, irrespective of CMV reactivation, and reflects accumulation of immature NK cells during early post-transplant lymphoid reconstitution (Figure 3B). Interestingly, the proportion of NKG2C-expressing cells increases on all NK cells subsets and was associated with reciprocal loss of NKG2A+ (Figures 3C, D). NKG2C expression was 3-4 fold higher on mature cytotoxic CD56dim NK subsets compared to CD56bright cells. In addition, it was noteworthy that the kinetics of NKG2C expression differed between these two populations with NKG2C expression peaking at 6 months (representative examples are shown on Supplementary Figure 2) on CD56bright cells whilst continuing to increase to month 10 on CD56dim cells.
These data indicate that CMV-driven enhancement of NKG2C expression is imprinted at the immature stage of NK differentiation, peaking at 6-months, whilst continuing to accumulate on more mature subsets for a further 4 months.
3.4. Transplantation from CMV seropositive donors modulates the profile of viraemia following reactivation
We next went on to determine how the CMV-serostatus of the haemopoietic transplant donor (D) acted to influence the magnitude of viral reactivation and profile of NK maturation following CMV reactivation in the patient (‘recipient’; R). Transplantation using a CMV-seropositive donor will infuse CMV-specific immune memory populations within the stem cell graft whilst immune cells from a CMV-seronegative donor will need to develop a primary CMV-specific immune response to control reactivation. 54% of patients who suffered an episode of CMV reactivation patients had R+/D+ CMV-serostatus whilst 37% had an R+/D- profile.
The magnitude and kinetics of viral load at reactivation were influenced by donor CMV serostatus. Of note, the initial viral load at the time of CMV reactivation was higher in R+/D+ patients (2350 ± 810 copies/ml vs 897 ± 270 copies/ml in R+/D- patients; (p=0.05) (Figure 4A). However, the subsequent peak viral load was considerably higher in the R+/D- cohort, indicating a role for transferred CMV-specific immunity in accelerating control of viral replication. Two or more episodes of viraemia were seen in 79% R+/D- patients (11 out of 14) but only 26% of R+/D+ patients (6 out of 23). Second peaks of viraemia occurred most commonly between weeks 2 and 4 and were typically higher than seen at initial reactivation. Viral load became virtually undetectable when the absolute NK count rose above 20/μl suggesting that this may represent a potential biomarker for effective control of viraemia.
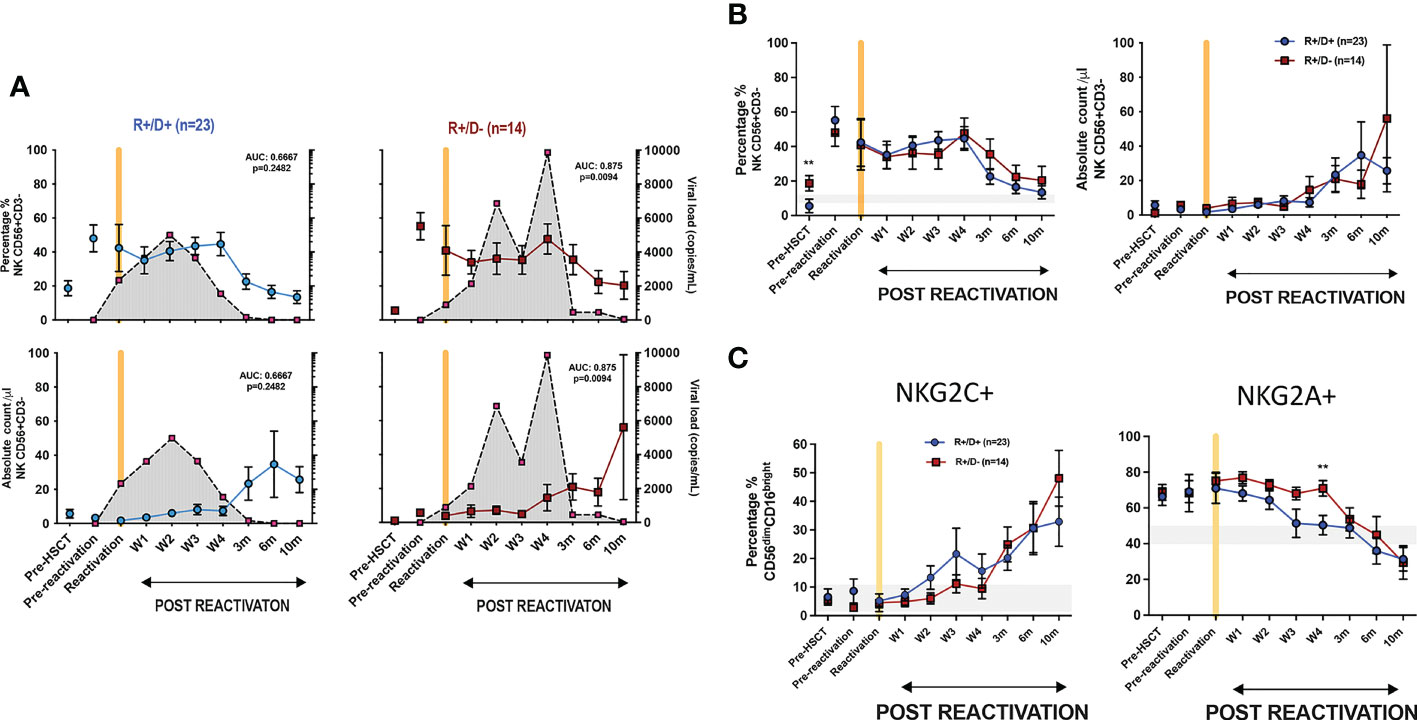
Figure 4 Influence of CMV serostatus of transplant donor on the kinetics of viral load at reactivation and subsequent profile of NK cells. (A) Viral load and NK cell percentage and number following CMV reactivation in relation to CMV serostatus of donor (positive; D+ or negative; D-). Grey shading represents aggregate profile of CMV viral load over time. (B) Comparison of percentage and number of NK cells following CMV reactivation in relation to donor serostatus (R+/D+ in blue line and R+/D- in purple line). (C) Percentage of NKG2C+ (left) and NKG2A+ (right) NK cells following CMV reactivation in relation to donor serostatus (R+/D+ in blue line and R+/D- in purple line). Grey lines represent the range of NKG2C+ and NKG2A+ NK cells in healthy donors. (*p<0.05, **p<0.01, ***P<0.001; Wilcoxon sign rank test for matched phenotypes).
A trend towards a differential pattern of expression of NKG2C and NKG2A was observed in relation to donor serostatus (Figures 4B, C) but the number and percentage of NK cells were not altered and no difference was observed in extended NK cell phenotype (Supplementary Figures 3 and 4).
These data suggest that transfer of memory NKG2C+ NK cells from a CMV seropositive donor may contribute to control of viraemia although little impact is seen on NK cell phenotype or number after reactivation.
3.5. NK cells show a more activated phenotype and produce higher cytokine levels after HCMV reactivation in HSCT patients
The pattern of expression of the early activation marker CD69 and the differentiation-associated protein CD57 was then assessed on the cytotoxic CD56dimCD16bright NK subset. Of note, the percentage of CD69+ NK cells was much higher in HSCT patients compared to healthy donors at virtually all time points after transplant and is likely to reflect an influence of homeostatic proliferation (Figure 5A). The highest level of expression was seen at the time of CMV reactivation and then fell over the next few weeks whilst values were stable in the absence of reactivation. Interestingly, no significant difference in CD69 expression among four NK subsets (NKG2A-/NKG2C-, NKG2A+/NKG2C-, NKG2A-/NKG2C+, NKG2A+/NKG2C+) was seen at any time point (Supplementary Figure 6). The proportion of CD57+ NK cells decreased rapidly after CMV reactivation and remained low until week 4 before returning to the normal range at 3 months and increasing further thereafter (Figure 5A). In contrast, the proportion of CD57+ NK cells remained very stable in the absence of reactivation. An increase in the proportion of KIRs+ NK cells was also apparent after HCMV reactivation, most notably within the first 4 weeks, although no significant change was seen in relation to the pattern of PD-1 or KLRG1 expression (Supplementary Figure 5).
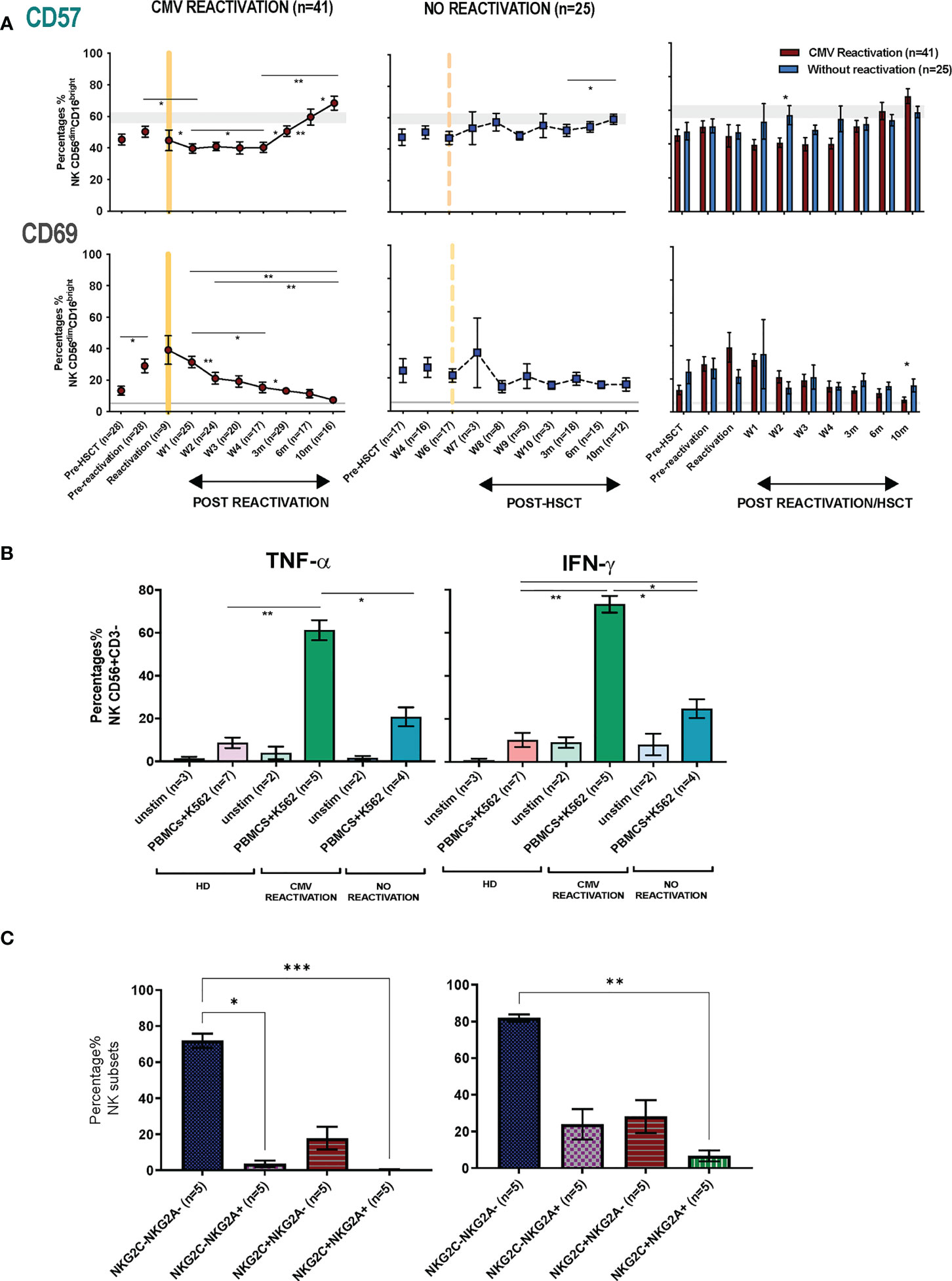
Figure 5 NK cells from HSCT patients who have undergone an episode of CMV reactivation demonstrate early proliferation with subsequent maturation and enhanced production of cytokines. (A) The percentage of CD57+ and CD69+ on NK cells from patients following CMV reactivation (purple line and bar) or without CMV reactivation (blue line and bar). Grey lines represent the range of CD57+ and CD69+ NK cells in healthy controls. (*p<0.05, **p<0.01, ***P<0.001; Wilcoxon sign rank test for matched phenotypes). (B) Enhanced TNF-α (left panel) and IFN-γ (right panel) production from NK cells of HSCT patients following prior CMV reactivation. Data are shown as percentage of cytokine-positive NK cells following K562 stimulation. (*p<0.05**p<0.01; Anova test). (C) TNF-α (left panel) and IFN-γ (right panel) production from four NK subsets (NKG2A-/NKG2C-, NKG2A+/NKG2C-, NKG2A-/NKG2C+, NKG2A+/NKG2C+) in patients following prior CMV reactivation. Data are shown as percentage of cytokine-positive NK subsets following K562 stimulation. (*p<0.05**p<0.01***p<0.001; Anova test).
The profile of TNF-α and IFN- γ production by NK cells was also determined in relation to prior history of viral reactivation. Due to limited sample availability, analysis was undertaken at 6-10 months post transplant and NK cells were co-cultured with K562 cells and assessed by intracellular flow cytometry. Higher baseline levels of cytokine production were seen post-transplant compared to controls and may reflect increased baseline proliferation as shown above (Figure 5B). However, activation-induced cytokine production was markedly increased in patients who had experienced an episode of CMV reactivation. In particular, TNF-α and IFN-γ production was observed in 61% and 73% of NK cells respectively compared to only 21% and 25% in patients without reactivation (Figure 5B). A higher level of cytokine production was seen from CD56dim NK cells compared with CD56bri NK cells (Supplementary Figure 7). Furthermore, the highest level of cytokines were seen within NKG2A-/NKG2C- NK cells followed by the NKG2A-/NKG2C+ subset, whilst very few NKG2A+/NKG2C+ NK cells were cytokine positive (Figure 5C). Cytotoxic responses against K562 were comparable between groups (data not shown).
These findings show that an episode of CMV reactivation serves to drive NK cell proliferation and differentiation and mediates a sustained increase in capacity for inflammatory cytokine production.
4. Discussion
CMV establishes a persistent infection that is controlled by immune surveillance and leads to imprinting of the peripheral lymphoid repertoire (4). We find that short term viral reactivation leads to rapid and sustained expansion of NK subsets over a period of many months. Our studies were undertaken in immune suppressed patients after allogeneic stem cell transplantation but the findings are likely to inform directly on the mechanisms that control CMV reactivation within healthy immune competent people. As such they provide insight into the immune control of CMV replication and further demonstration of how pathogens can modulate the long term profile of innate immunity.
NK cells are amongst the first lymphocyte subsets to reconstitute after HSCT and this was reflected in both the high percentage of NK cells and an increased proportion of immature subsets in the early post-transplant period (16). However, an episode of CMV reactivation was seen to have a profound impact on the subsequent profile of NK cell maturation and expansion. CMV reactivation occurred at a median of 52 days which is consistent with previous reports and reflects early reactivation of virus from host tissues (22). The number of NK cells in the early post-transplant period was low but was not predictive of reactivation risk. In patients who did not experience an episode of viral reactivation the percentage and number of NK cells remained broadly stable over the next 10 months. In contrast, viral reactivation led to a significant expansion of NK cells within 3-weeks which then continued such that NK cell number increased by 11-fold after 10 months. Interestingly, this increase was accompanied by a reduction in the NK cell percentage within the peripheral repertoire and reflects the profound impact of CMV reactivation on expansion of other lymphoid subsets, most notably T cells (24). The nature of HSCT transplant conditioning and donor choice is likely to impact substantially on the profile of NK reconstitution and similar findings have been seen after umbilical donor transplantion (22)although an increase in NK number was not seen in the setting of haploidential transplantation (25, 26). In the renal transplant setting a recent study has revealed a similar finding of increased number and frequency of NK cells after HCMV reactivation (27).
A particular focus was on the kinetics of the adaptive memory NKG2C+CD56dimCD16bright NK subset that is expanded in CMV seropositive donors. The NKG2C genotyping was not included in this study, but there are two CMV seronegative HD controls and one non CMV reactivation HSCT patient in this study do not have NKG2C+ NK cells at all. We took advantage of early sampling to show that this population increased within 2 weeks of reactivation and the proportion of NKG2C-expressing cells increased incrementally from 4% to 35% of the CD56dimCD16bright pool over 10 months. Expression NKG2C or NKG2A was largely mutually exclusive and a comparable fall in the percentage of the NKG2A population was therefore seen over this period. There is also increasing interest in the potential role of CD56negative NK cells and Hess and colleagues have demonstrated expansion of CD56negCD16bri NK cells in donors with CMV and EBV coinfection (28) although we were not able to study this subset within our analysis.
Previous studies have identified CMV-driven NKG2C+ adaptive memory cells only within the mature CD56dim NK population but here we also found this to develop on CD56bright populations. Indeed, a relative increase in proportion of NKG2C-expressing cells was seen on all four NK subsets as defined by CD56 and CD16 expression although the relative kinetics and magnitude were markedly different. The increment in NKG2C expression on the immature CD56bright subsets was much more modest than seen on CD56dim cells, with maximal values of 8% and 15% for the CD16neg and CD16bright subsets respectively. A particular finding of interest was that NKG2C+ expression on CD56bright cells peaked at 6 months whilst that on the CD56dim subset continued to increase at month 10. CD56bright cells are believed to be precursors of the CD56dim population (29) and as such these data indicate that NKG2C+ CD56dim cell expansion following CMV reactivation is at least partially supported by differentiation from NKG2C+ CD56bright NK cell precursors during the first 6-months (Figure 6). However, studies in patients with GATA2 mutation or PNH have indicated that adaptive cells may have self-renewing properties and as such the lineage derivation of this pool remains unclear (30, 31). In addition recent data from murine models has shown that an ILC1-like splenic-resident memory pool is induced following murine CMV infection (32) and the broad impact of viral reactivation on the repertoire of innate memory is therefore likely to have been underestimated (33).
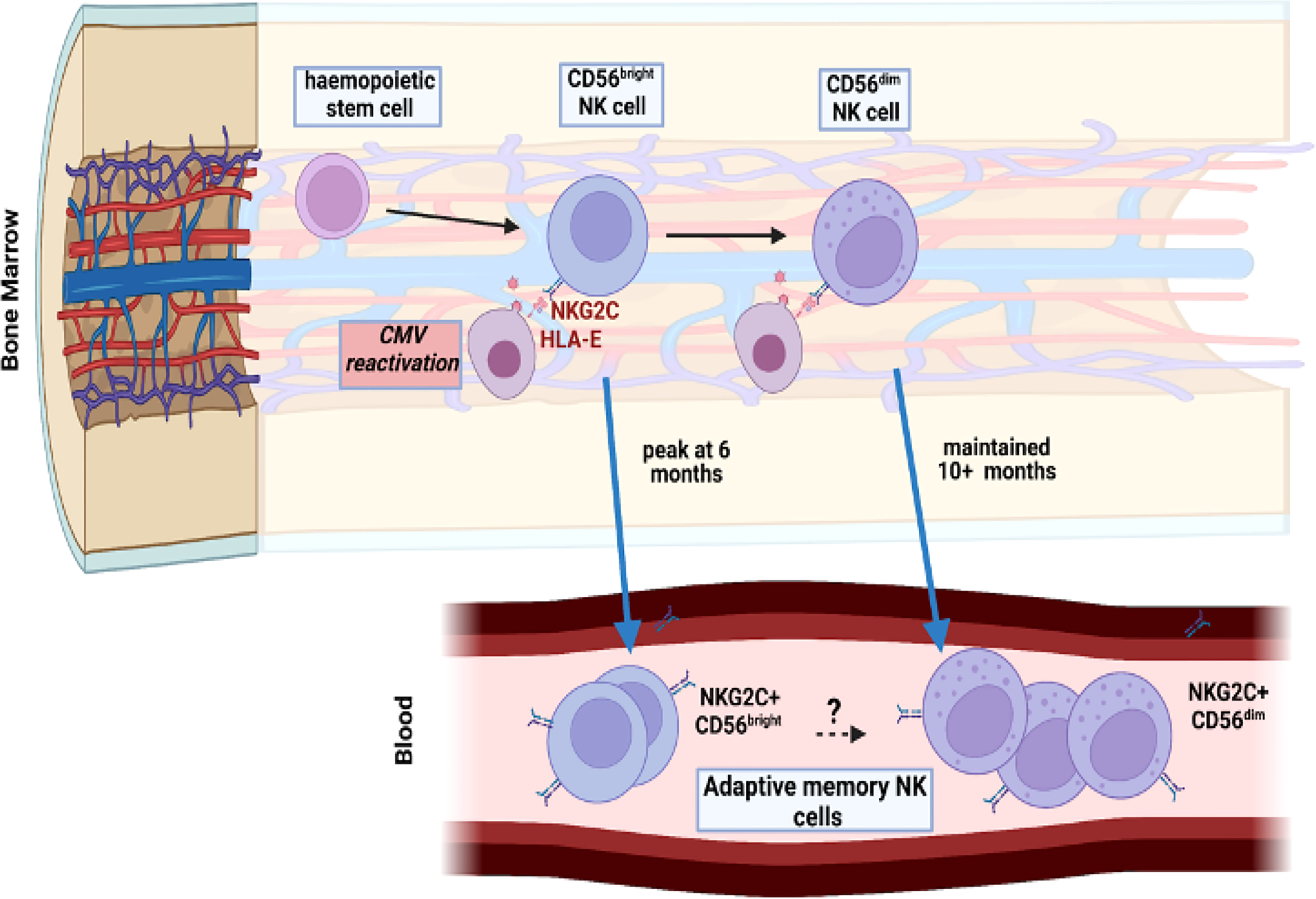
Figure 6 Model of potential maintenance of the adaptive memory NK cell pool through reactivation of CMV within bone marrow. CMV reactivation leads to a pattern of increased peripheral expression of NKG2C on both CD56dim mature NK cells and the more immature CD56bright subset. The peak of this expansion occurs earlier, at 6 months, in the immature population compared to 10 months in the mature subset. Viral reactivation may potentially engage both populations independently or CD56dim cells may differentiate from the more immature CD56bright subset.
The functional importance of transfer of ‘immune’ adaptive memory NK cells from the transplant donor was assessed by comparison of immune reconstitution between transplants with either a CMV-seropositive or seronegative donor. It was noteworthy that the initial viral load was elevated following transplantation from a CMV seropositive donor and this may reflect either viral replication from donor leucocytes or a consequence of donor CMV-specific immunity acting to transiently enhance short term viral load at reactivation (34). Despite this effect, peak viral load and longer term control of viremia were improved following transplantation from a CMV-seropositive donor. NK cells retain and transfer immune memory to facilitate control of viral reactivation (35) and a trend was seen towards more rapid NKG2C+ cell expansion within the first four weeks after reactivation within the R+/D+ group although NK cell number and phenotype were broadly comparable. Of note, prospective analysis allowed assessment of NK number in relation to control of viral reactivation and identified that viral load was controlled in all subjects when the peripheral NK cell count reached 20,000/ml (20/μl), comparable to values of 18/μl associated with higher overall survival at day 60 post transplant (36). The lymphocyte count in peripheral blood of healthy donors is ~106/ml and, with an NK cell percentage of 2-10%, this number is comparable to the value of 20-100,000 NK cells/ml in CMV-seropositive healthy donors. Sustained control of viral reactivation is likely to also require T cells and the role of adaptive memory cells in antigen presentation is of note in this regard (37).
Analysis of the kinetics of the extended phenotype of CD56dimCD16bright NK cells after viral reactivation focussed on CD57 and CD69. Expression of CD57, a marker of late differentiation, was somewhat lower in the first month post-reactivation but then increased continuously over subsequent months. As such, the classical expression of CD57 and KIR on adaptive memory NK cells is seen to develop late after reactivation (38) and supports evidence for coupling of differentiation and proliferation of NK cells over an extended period (26, 39, 40). It is not clear why expression was reduced during the first month after reactivation although this may reflect preferential recruitment of this subset into tissue. CD69 is upregulated upon NK cell activation (41) and expression was broadly increased within all patients which is likely to reflect in the impact of homeostatic proliferation and immune reconstitution. However, values were at their highest level at the time of viral reactivation and then gradually fell and there was no correlation between CD69 and NKG2C expression.
The relative functional capacity of NK cells was assessed by the profile of cytokine secretion and cytotoxic capacity following activation in vitro. Cytokine production was generally enhanced within NK cells from HSCT patients compared to healthy donors and may reflect the increased proliferative status in this setting. However, CMV reactivation further primed for the production of high levels of TNF-α and IFN-γ, as seen previously (22), and consistent with epigenetic modification of the IFNG locus (42). There is interest in the potential beneficial impact that may arise from CMV-driven enhancement of NK maturation (43) and reactivation has been associated with a reduction in the risk of leukaemia relapse in some studies although the underlying mechanisms remain unclear (44, 45).
Homeostatic expansion (46, 47) and the high level of viral reactivation are both likely to enhance NK cell expansion in the post-transplant period and likely to underlie the ‘supra-physiological’ expansion of the NKG2C+ NK cell subsets that was observed. However, the broad features relating to the kinetics and phenotypic profile of viral-induced NK expansion are likely to be applicable to immune competent populations (48). NKG2C+ cells remain elevated for decades following CMV infection and, as hemopoietic and myeloid precursors are reservoirs for CMV latency, these observations suggest that this may be maintained by intermittent viral reactivation acting to modulate NK cell differentiation within the bone marrow. The finding that NK cell expansion is sustained for at least 10 months might appear surprising given that innate responses are typically regarded as reactive and short term. Very low levels of subclinical viral reactivation in the post-transplant setting cannot be ruled out but were not detected by sensitive PCR. Moreover, the findings concur with observations that other innate cells, such as neutrophils and monocytes, also show long term peripheral changes after acute events and suggest that epigenetic regulation of stem cell precursors acts to establish long term adaptive memory (49, 50). Limitations of our study were that we were unable to determine NKG2C genotype in participants and the cessation of sampling at 10 months after reactivation.
In conclusion we show that CMV reactivation drives rapid and long term expansion of NKG2C+ NK cells over a period of at least 10 months. Indeed, this mechanism might underlie the maintenance of expanded NKG2C+ populations within CMV seropositive healthy donors but this was not addressed in this study (Figure 6). These findings are of potential importance for management of CMV reactivation after HSCT and suggest that NKG2C+ NK cell monitoring might be used to predict immune capacity to control reactivation. Furthermore, this profile of expansion following short-term viral reactivation extends insight into pathogen-driven haemopoietic programming of stem cell precursors to enhance innate cell memory.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by West Midlands - South Birmingham Research Ethics Committee ‘REC reference number: 15/WM/0194’. The patients/participants provided their written informed consent to participate in this study.
Author contributions
PM, NH, JZ wrote the manuscript. PM, JZ designed the study. FK, CC, RM recruited participants. NH, SE, CS, JZ performed the experiments. NH, JZ analysed the data. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by Blood Cancer UK (Grant Code: 12052), Medical Research Council and Ministry of Education Malaysia.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2022.935949/full#supplementary-material
References
1. Freud AG, Mundy-Bosse BL, Yu J, Caligiuri MA. The broad spectrum of human natural killer cell diversity. Immunity (2017) 47(5):820–33. doi: 10.1016/j.immuni.2017.10.008
2. Vitale M, Cantoni C, Della Chiesa M, Ferlazzo G, Carlomagno S, Pende D, et al. An historical overview: The discovery of how NK cells can kill enemies, recruit defense troops, and more. Front Immunol (2019) 10:1415. doi: 10.3389/fimmu.2019.01415
3. Orange JS. Natural killer cell deficiency. J Allergy Clin Immunol (2013) 132(3):515–25. doi: 10.1016/j.jaci.2013.07.020
4. Chidrawar S, Khan N, Wei W, McLarnon A, Smith N, Nayak L, et al. Cytomegalovirus-seropositivity has a profound influence on the magnitude of major lymphoid subsets within healthy individuals. Clin Exp Immunol (2009) 155(3):423–32. doi: 10.1111/j.1365-2249.2008.03785.x
5. Gumá MN, Angulo A, Vilches C, Gómez-Lozano N, Malats NR, López-Botet M. Imprint of human cytomegalovirus infection on the NK cell receptor repertoire. Blood (2004) 104(12):3664–71. doi: 10.1182/blood-2004-05-2058
6. Béziat V, Liu LL, Malmberg J-A, Ivarsson MA, Sohlberg E, Björklund AT, et al. NK cell responses to cytomegalovirus infection lead to stable imprints in the human KIR repertoire and involve activating KIRs. Blood (2013) 121(14):2678–88. doi: 10.1182/blood-2012-10-459545
7. Hammer Q, Rückert T, Borst EM, Dunst J, Haubner A, Durek P, et al. Peptide-specific recognition of human cytomegalovirus strains controls adaptive natural killer cells. Nat Immunol (2018) 19(5):453–63. doi: 10.1038/s41590-018-0082-6
8. Della Chiesa M, Falco M, Bertaina A, Muccio L, Alicata C, Frassoni F, et al. Human cytomegalovirus infection promotes rapid maturation of NK cells expressing activating killer ig-like receptor in patients transplanted with NKG2C-/- umbilical cord blood. J Immunol (2014) 192(4):1471–9. doi: 10.4049/jimmunol.1302053
9. Arlettaz L, Villard J, de Rham C, Degermann S, Chapuis B, Huard B, et al. Activating CD94:NKG2C and inhibitory CD94:NKG2A receptors are expressed by distinct subsets of committed CD8+ TCR αβ lymphocytes. Eur J Immunol (2004) 34(12):3456–64. doi: 10.1002/eji.200425210
10. Braud VM, Allan DS, O'Callaghan CA, Söderström K, D'Andrea A, Ogg GS, et al. HLA-e binds to natural killer cell receptors CD94/NKG2A, b and c. Nature (1998) 391(6669):795–9. doi: 10.1038/35869
11. Barrett J, Craddock C. Bone marrow transplantation in the united kingdom - past, present and future. Br J haematol (2020) 191(4):612–6. doi: 10.1111/bjh.17151
12. O'Neill AT, Chakraverty R. Graft versus leukemia: Current status and future perspectives. J Clin Oncol (2021) 39(5):361–72. doi: 10.1200/jco.20.01801
13. Maggs L, Kinsella F, Chan YLT, Eldershaw S, Murray D, Nunnick J, et al. The number of CD56(dim) NK cells in the graft has a major impact on risk of disease relapse following allo-HSCT. Blood Adv (2017) 1(19):1589–97. doi: 10.1182/bloodadvances.2017008631
14. Ullah MA, Hill GR, Tey S-K. Functional reconstitution of natural killer cells in allogeneic hematopoietic stem cell transplantation. Front Immunol (2016) 7:144. doi: 10.3389/fimmu.2016.00144
15. Minculescu L, Marquart HV, Friis LS, Petersen SL, Schiødt I, Ryder LP, et al. Early natural killer cell reconstitution predicts overall survival in T cell-replete allogeneic hematopoietic stem cell transplantation. Biol Blood marrow Transplant (2016) 22(12):2187–93. doi: 10.1016/j.bbmt.2016.09.006
16. Pical-Izard C, Crocchiolo R, Granjeaud S, Kochbati E, Just-Landi S, Chabannon C, et al. Reconstitution of natural killer cells in HLA-matched HSCT after reduced-intensity conditioning: impact on clinical outcome. Biol Blood Marrow Transplant (2015) 21(3):429–39. doi: 10.1016/j.bbmt.2014.11.681
17. Teira P, Battiwalla M, Ramanathan M, Barrett AJ, Ahn KW, Chen M, et al. Early cytomegalovirus reactivation remains associated with increased transplant-related mortality in the current era: a CIBMTR analysis. Blood (2016) 127(20):2427–38. doi: 10.1182/blood-2015-11-679639
18. Green ML, Leisenring W, Xie H, Mast TC, Cui Y, Sandmaier BM, et al. Cytomegalovirus viral load and mortality after haemopoietic stem cell transplantation in the era of pre-emptive therapy: a retrospective cohort study. Lancet Haematol (2016) 3(3):e119–27. doi: 10.1016/s2352-3026(15)00289-6
19. Elmaagacli AH, Steckel NK, Koldehoff M, Hegerfeldt Y, Trenschel R, Ditschkowski M, et al. Early human cytomegalovirus replication after transplantation is associated with a decreased relapse risk: evidence for a putative virus-versus-leukemia effect in acute myeloid leukemia patients. Blood (2011) 118(5):1402–12. doi: 10.1182/blood-2010-08-304121
20. Green ML, Leisenring WM, Xie H, Walter RB, Mielcarek M, Sandmaier BM, et al. CMV reactivation after allogeneic HCT and relapse risk: evidence for early protection in acute myeloid leukemia. Blood (2013) 122(7):1316–24. doi: 10.1182/blood-2013-02-487074
21. Takenaka K, Nishida T, Asano-Mori Y, Oshima K, Ohashi K, Mori T, et al. Cytomegalovirus reactivation after allogeneic hematopoietic stem cell transplantation is associated with a reduced risk of relapse in patients with acute myeloid leukemia who survived to day 100 after transplantation: The Japan society for hematopoietic cell transplantation transplantation-related complication working group. Biol Blood Marrow Transplant (2015) 21(11):2008–16. doi: 10.1016/j.bbmt.2015.07.019
22. Foley B, Cooley S, Verneris MR, Pitt M, Curtsinger J, Luo X, et al. Cytomegalovirus reactivation after allogeneic transplantation promotes a lasting increase in educated NKG2C+ natural killer cells with potent function. Blood (2012) 119(11):2665–74. doi: 10.1182/blood-2011-10-386995
23. Della Chiesa M, Falco M, Podestà M, Locatelli F, Moretta L, Frassoni F, et al. Phenotypic and functional heterogeneity of human NK cells developing after umbilical cord blood transplantation: a role for human cytomegalovirus? Blood (2012) 119(2):399–410. doi: 10.1182/blood-2011-08-372003
24. Würsch AM, Gratama JW, Middeldorp JM, Nissen C, Gratwohl A, Speck B, et al. The effect of cytomegalovirus infection on T lymphocytes after allogeneic bone marrow transplantation. Clin Exp Immunol (1985) 62(2):278–87.
25. Locatelli F, Pende D, Maccario R, Mingari MC, Moretta A, Moretta L. Haploidentical hemopoietic stem cell transplantation for the treatment of high-risk leukemias: How NK cells make the difference. Clin Immunol (2009) 133(2):171–8. doi: 10.1016/j.clim.2009.04.009
26. Zaghi E, Calvi M, Puccio S, Spata G, Terzoli S, Peano C, et al. Single-cell profiling identifies impaired adaptive NK cells expanded after HCMV reactivation in haploidentical HSCT. JCI Insight (2021) 6(12). doi: 10.1172/jci.insight.146973
27. Ishiyama K, Arakawa-Hoyt J, Aguilar OA, Damm I, Towfighi P, Sigdel T, et al. Mass cytometry reveals single-cell kinetics of cytotoxic lymphocyte evolution in CMV-infected renal transplant patients. Proc Natl Acad Sci (2022) 119(8):e2116588119. doi: 10.1073/pnas.2116588119
28. Müller-Durovic B, Grählert J, Devine OP, Akbar AN, Hess C. CD56-negative NK cells with impaired effector function expand in CMV and EBV co-infected healthy donors with age. Aging (2019) 11(2):724–40. doi: 10.18632/aging.101774
29. Caligiuri MA. Human natural killer cells. Blood (2008) 112(3):461–9. doi: 10.1182/blood-2007-09-077438
30. Schlums H, Jung M, Han H, Theorell J, Bigley V, Chiang SCC, et al. Adaptive NK cells can persist in patients with GATA2 mutation depleted of stem and progenitor cells. Blood (2017) 129(14):1927–39. doi: 10.1182/blood-2016-08-734236
31. Corat MAF, Schlums H, Wu C, Theorell J, Espinoza DA, Sellers SE, et al. Acquired somatic mutations in PNH reveal long-term maintenance of adaptive NK cells independent of HSPCs. Blood (2017) 129(14):1940–6. doi: 10.1182/blood-2016-08-734285
32. Flommersfeld S, Böttcher JP, Ersching J, Flossdorf M, Meiser P, Pachmayr LO, et al. Fate mapping of single NK cells identifies a type 1 innate lymphoid-like lineage that bridges innate and adaptive recognition of viral infection. Immunity (2021) 54(10):2288–304.e7. doi: 10.1016/j.immuni.2021.08.002
33. Wu C, Espinoza DA, Koelle SJ, Yang D, Truitt L, Schlums H, et al. Clonal expansion and compartmentalized maintenance of rhesus macaque NK cell subsets. Sci Immunol (2018) 3(29). doi: 10.1126/sciimmunol.aat9781
34. Barron M, Gao D, Springer K, Patterson J, Brunvand M, McSweeney P, et al. Relationship of reconstituted adaptive and innate cytomegalovirus (CMV)-specific immune responses with CMV viremia in hematopoietic stem cell transplant recipients. Clin Infect Dis (2009) 49:1777–83. doi: 10.1086/648423
35. Foley B, Cooley S, Verneris MR, Curtsinger J, Luo X, Waller EK, et al. Human cytomegalovirus (CMV)-induced memory-like NKG2C(+) NK cells are transplantable and expand in vivo in response to recipient CMV antigen. J Immunol (2012) 189(10):5082–8. doi: 10.4049/jimmunol.1201964
36. Erin MD, Mathew PB, Jeff BL, Jesse DS, Herwig-Ulf M-K, Vijay R. The relationship between circulating natural killer cells after reduced intensity conditioning hematopoietic stem cell transplantation and relapse-free survival and graft-versus-host disease. Haematologica (2008) 93(12):1852–8. doi: 10.3324/haematol.13033
37. Costa-García M, Ataya M, Moraru M, Vilches C, López-Botet M, Muntasell A. Human cytomegalovirus antigen presentation by HLA-DR+ NKG2C+ adaptive NK cells specifically activates polyfunctional effector memory CD4+ T lymphocytes. Front Immunol (2019) 10:687. doi: 10.3389/fimmu.2019.00687
38. Lopez-Vergès S, Milush JM, Schwartz BS, Pando MJ, Jarjoura J, York VA, et al. Expansion of a unique CD57+NKG2Chi natural killer cell subset during acute human cytomegalovirus infection. Proc Natl Acad Sci USA (2011) 108(36):14725–32. doi: 10.1073/pnas.1110900108
39. Grassmann S, Pachmayr LO, Leube J, Mihatsch L, Andrae I, Flommersfeld S, et al. Distinct surface expression of activating receptor Ly49H drives differential expansion of NK cell clones upon murine cytomegalovirus infection. Immunity (2019) 50(6):1391–400.e4. doi: 10.1016/j.immuni.2019.04.015
40. Muccio L, Falco M, Bertaina A, Locatelli F, Frassoni F, Sivori S, et al. Late development of FcϵRγneg adaptive natural killer cells upon human cytomegalovirus reactivation in umbilical cord blood transplantation recipients. Front Immunol (2018) 9:1050. doi: 10.3389/fimmu.2018.01050
41. Fogel LA, Sun MM, Geurs TL, Carayannopoulos LN, French AR. Markers of nonselective and specific NK cell activation. J Immunol (2013) 190(12):6269–76. doi: 10.4049/jimmunol.1202533
42. Schlums H, Cichocki F, Tesi B, Theorell J, Beziat V, Holmes TD, et al. Cytomegalovirus infection drives adaptive epigenetic diversification of NK cells with altered signaling and effector function. Immunity (2015) 42(3):443–56. doi: 10.1016/j.immuni.2015.02.008
43. Cichocki F, Taras E, Chiuppesi F, Wagner JE, Blazar BR, Brunstein C, et al. Adaptive NK cell reconstitution is associated with better clinical outcomes. JCI Insight (2019) 4(2). doi: 10.1172/jci.insight.125553
44. Ito S, Pophali P, Co W, Koklanaris EK, Superata J, Fahle GA, et al. CMV reactivation is associated with a lower incidence of relapse after allo-SCT for CML. Bone Marrow Transplant (2013) 48(10):1313–6. doi: 10.1038/bmt.2013.49
45. Cichocki F, Cooley S, Davis Z, DeFor TE, Schlums H, Zhang B, et al. CD56dimCD57+NKG2C+ NK cell expansion is associated with reduced leukemia relapse after reduced intensity HCT. Leukemia (2016) 30(2):456–63. doi: 10.1038/leu.2015.260
46. Prlic M, Blazar BR, Farrar MA, Jameson SC. In vivo survival and homeostatic proliferation of natural killer cells. J Exp Med (2003) 197(8):967–76. doi: 10.1084/jem.20021847
47. Sun JC, Beilke JN, Bezman NA, Lanier LL. Homeostatic proliferation generates long-lived natural killer cells that respond against viral infection. J Exp Med (2011) 208(2):357–68. doi: 10.1084/jem.20100479
48. Adams NM, Grassmann S, Sun JC. Clonal expansion of innate and adaptive lymphocytes. Nat Rev Immunol (2020) 20(11):694–707. doi: 10.1038/s41577-020-0307-4
49. Netea MG, Joosten LA, Latz E, Mills KH, Natoli G, Stunnenberg HG, et al. Trained immunity: A program of innate immune memory in health and disease. Sci (New York NY) (2016) 352(6284):aaf1098. doi: 10.1126/science.aaf1098
Keywords: adaptive NK cells, NKG2C+, CMV reactivation, human cytomegalovirus, allogeneic HSCT
Citation: Hassan N, Eldershaw S, Stephens C, Kinsella F, Craddock C, Malladi R, Zuo J and Moss P (2022) CMV reactivation initiates long-term expansion and differentiation of the NK cell repertoire. Front. Immunol. 13:935949. doi: 10.3389/fimmu.2022.935949
Received: 04 May 2022; Accepted: 04 November 2022;
Published: 01 December 2022.
Edited by:
Emilie Narni-Mancinelli, INSERM U1104 Centre d’immunologie de Marseille-Luminy, FranceReviewed by:
Daniela Pende, San Martino Hospital, Scientific Institute for Research, Hospitalization and Healthcare (IRCCS), ItalyColleen Lau, Cornell University, United States
Copyright © 2022 Hassan, Eldershaw, Stephens, Kinsella, Craddock, Malladi, Zuo and Moss. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paul Moss, p.moss@bham.ac.uk
†These authors have contributed equally to this work
 Norfarazieda Hassan
Norfarazieda Hassan Suzy Eldershaw1
Suzy Eldershaw1 Francesca Kinsella
Francesca Kinsella Jianmin Zuo
Jianmin Zuo Paul Moss
Paul Moss