Interactive Effects of meteorological Factors and Ambient air Pollutants on Mumps Incidences in Ningxia, China Between 2015 and 2019
- 1School of Public Health and Management, Ningxia Medical University, Yinchuan, China
- 2Key Laboratory of Environmental Factors and Chronic Disease Control, Yinchuan, China
- 3JC School of Public Health and Primary Care, Chinese University of Hong Kong, Hong Kong, China
- 4CUHK Shenzhen Research Institute, Shenzhen, China
- 5Department of Infectious Diseases, Ningxia Center for Disease Control and Prevention, Yinchuan, China
Background: Existing evidence suggests that mumps epidemics, a global public health issue, are associated with meteorological factors and air pollutants at the population scale. However, the interaction effect of meteorological factors and air pollutants on mumps remains underexplored.
Methods: Daily cases of mumps, meteorological factors, and air pollutants were collected in Ningxia, China, from 2015 to 2019. First, a distributed lag nonlinear model (DLNM) was employed to assess the confounding-adjusted relationship between meteorological factors, ambient air pollutants, and mumps incidences. According to the results of DLNM, stratification in both air pollutants and meteorological factors was adopted to further explore the interaction effect of particulate matter less than or equal to 2.5 μm in aerodynamic diameter (PM2.5) and ground-level ozone (O3) with temperature and relative humidity (RH).
Results: We reported significant individual associations between mumps incidences and environmental factors, including temperature, relative humidity, PM2.5, and O3. Evident multiplicate and additive interactions between meteorological factors and PM2.5 were found with interaction relative risk (IRR) of 1.14 (95%CI: 1.01, 1.29) and relative excess risk due to interaction (RERI) of 0.17 (95%CI: 0.02, 0.32) for a moderate level of temperature at 12°C, and IRR of 1.37 (95%CI: 1.14, 1.66), RERI of 0.36 (95%CI: 0.11, 0.60) for a high level of temperature at 20°C, respectively. These results indicated that PM2.5 and temperature have a significant synergistic effect on the cases of mumps, while no interaction between relative humidity and PM2.5 is observed. Regarding O3 and meteorological factors (temperature = 12°C, 20°C), IRR and RERI were 1.33 (95%CI: 1.17, 1.52) and 0.30 (95%CI: 0.16, 0.45), 1.91 (95%CI: 1.46, 2.49) and 0.69 (95%CI: 0.32, 1.07), respectively. And IRR of 1.17 (95%CI: 1.06, 1.29), RERI of 0.13 (95%CI: 0.04, 0.21) for a middle level of relative humidity at 48%.
Conclusion: Our findings indicated that meteorological factors and air pollutants imposed a significantly lagged and nonlinear effect on the incidence of mumps. The interaction between low temperature and O3 showed antagonistic effects, while temperature (medium and high) with PM2.5 and O3 presented synergistic effects. For relative humidity, the interaction with O3 is synergistic. These results provide scientific evidence to relevant health authorities for the precise disease control and prevention of mumps in arid and semi-arid areas.
1 Introduction
Mumps is an acute respiratory infection caused by the mumps virus (MuV), which occurs in children and adolescents characterized by swelling of the parotid or other salivary glands (Hviid et al., 2008). The onset of mumps presents a definite seasonal variation, with two peaks in April–July, and November–January (Hu et al., 2014; Su et al., 2016). The seasonality of mumps suggests that meteorological factors possibly affect the occurrence of the disease. Several studies have also indicated a strong association between mumps and meteorological factors (Hu et al., 2018; Yu et al., 2018; Wu et al., 2020; Zhou et al., 2020). For example, an investigation in Guangzhou in 2014 (Yang et al., 2014) applied DLNM to estimate the non-linear and lagged effects simultaneously to explore the influence of meteorological factors on the onset of mumps and found a non-linear relationship between meteorological factors and the occurrence of mumps, except for sunshine hours. A study in Taiwan discovered that there is an inverse V-shaped relationship between the incidence curve of mumps and temperature as a whole (Ho et al., 2015). Yu et al. (2018) found that temperature and wind speed exerts a significant impact on the incidence of mumps in Guangzhou. In addition, recent studies showed that oxidative stress and inflammation may be the mechanisms of air pollution-induced health effects on respiratory diseases. Oxidative stress can trigger redox-sensitive pathways that lead to different biological processes such as inflammation and cell death (Maura and Elisabetta, 2011). Some results found that the meteorological factors were significantly associated with the incidence of Mumps in Guangzhou (Lu et al., 2019), and the authors explained that for relative humidity, water in the droplets evaporates quickly if the relative humidity is low. The longer the droplet with mumps viruses remains airborne, the easier it is for the mumps infection. These findings demonstrated that the onset of mumps is heterogeneous across cities due to the differences in meteorological and demographic factors.
In recent years, air pollution and climate change were becoming major environmental issues that threaten the health of people throughout the world. Existing epidemiological studies have shown that meteorological factors or air pollution are associated with mumps epidemics. For instance, a study in Wuhan found that exposure to nitrogen dioxide (NO2) and sulfur dioxide (SO2) was significantly associated with a higher risk of developing mumps (Hao et al., 2019). A study of multiple provinces in China indicates that there is a positive relationship between particulate matter (PM) and the incidence of mumps (Zhang and Zhu, 2021). World Health Organization (WHO) reported that around seven million people have been influenced by air pollution during the year worldwide, and almost 99% of the people are breathing air with pollutant levels which exceed the upper limit of WHO standards (WHO (World Health Organization), 2022). Despite the remarkable achievements of Chinese air pollution prevention and control, there are still more than 40% of cities where ambient air quality exceeds the standard (Ministry of Ecology and Environment of China, 2021) and leading to a progressive increase in associated morbidity and mortality of respiratory system disease (Song et al., 2017). Therefore, it is urgent for public health to explore the health influence of air pollution and the interaction effect with other meteorological factors on mumps.
Despite growing literature on the exposure of ambient air pollutants or meteorological factors and their individual associations with mumps, fewer studies explored the interaction between meteorological factors and air pollutants as well as the impacts on mumps (Du et al., 2019; Mokoena et al., 2020). Moreover, it is worth to be mentioned here that the related studies were most from plains, coastal, and tropics (subtropics) areas, and more efforts are needed to assess the association in different geographical regions such as arid and semi-arid areas. In this study, we evaluate the individual and interactive associations between air pollutants and meteorological factors on the risk of mumps using the daily time series data in Ningxia, China, from 2015 to 2019. These results may provide epidemiological evidence for understanding the patterns and environmental-associated risks of mumps in arid and semi-arid areas and may inform health authorities about the disease control and prevention of mumps in similar settings.
2 Materials and Methods
2.1 Setting and Data
Ningxia is one of the provinces located in northwest China, with a resident population of 7.2 million as of 2020. In this study, surveillance data of mumps cases in Ningxia from 1 January 2015 to 31 December 2019 were collected from the information management system of infectious diseases reports in China. The province-level daily meteorological data during the same period were collected from the National Meteorological Information Center (http://data.cma.gov), including daily average temperature, daily air pressure, daily mean relative humidity, and daily wind speed. The daily average of the concentrations of sulfur dioxide (SO2), nitrogen dioxide (NO2), carbon monoxide (CO), ground-level ozone (O3), particulate matter less than or equal to 10 μm in aerodynamic diameter (PM10), and particulate matter less than or equal to 2.5 μm in aerodynamic diameter (PM2.5) in Ningxia from January 2015 to December 2019 were collected from the China Meteorological Science data sharing Service system (http://hz.hjhj-e.com/home). Meteorological and pollutant data were obtained from the average of four areas in Yinchuan, Shizuishan, Zhongwei, Wuzhong, and Guyuan cities, with missing rates of 3 and 1%, respectively, which were filled by using the average value of the same period, the spatial distribution of meteorological stations and pollutant monitoring stations were depicted in Supplementary Appendix Figure S1.
2.2 Statistical Analysis
2.2.1 Distributed Lag Nonlinear Model
As one of the widely adopted approaches in environmental epidemiology (Ge et al., 2018; Xu et al., 2019; Lu et al., 2020), DLNM is employed to assess the lagged and nonlinear association between environmental factors and the incidence of mumps by adjusting for the effects of known confounding variables, long-term trends, and seasonality. The Akaike information criteria (AIC) is used to choose the optimal degrees of freedom (df) (Gasparrini et al., 2010; Hu et al., 2019). The model is described as follows:
where
The model with the smallest AIC value was selected to establish the cumulative association of environmental parameters for mumps. The lags of meteorological factors and the lags of air pollutants (PM2.5 and O3) were both 21 days.
2.2.2 Interaction Analysis
Prior to fitting the Poisson regression, air pollutants (PM2.5, and O3) were dichotomized into binary variables from the DLNM model based on the turning points, which is lower than the turning point and higher than the turning point (Du et al., 2019; Mokoena et al., 2020; Pan et al., 2020). Consequently, PM2.5 and O3 were transformed as PM2.5 = 0 (if PM2.5<=turning point) and PM2.5 = 1 (if PM2.5 > turning point), O3 = 0 (if O3>turning point) and O3 = 1 (if O3<=turning point). Similarly, the meteorological factors including temperature (T), relative humidity (RH) were divided into binary variables according to quartiles (low quartile, Median, and upper quartile). The interaction model was constructed as follows:
According to Poisson regression, we calculated the relative risk from the regression coefficient estimates, which are denoted by RR01, RR10, and RR11 for the relative risk when T (or RH) = 0 and PM2.5 (or O3) = 1, the relative risk when T (or RH) = 1 and PM2.5 (or O3) = 0, and the relative risk when T (or RH) = 1 and PM2.5 (or O3) = 1, respectively. Then, the IRR (interaction relative risk) and RERI (relative excess risk due to interaction) were calculated based on the multiplicative and additive.
Model of interaction theory (Austin et al., 2013) as follows:
No interaction was observed when IRR = 1 or RERI = 0, synergistic interaction when IRR > 1 or RERI > 0, and antagonistic interaction when IRR < 1 or RERI < 0.
To further examine the interactive effect of the meteorological and pollution variables, the response surface methodology (RSM) was conducted to evaluate the combined effects of meteorological and air pollutants on the mumps cases based on the generalized additive model (GAM) (Myers et al., 2004; Du et al., 2019).
All statistical analyses were carried out using R software (version 4.0.4) (The R Foundation for Statistical Computing, Vienna, Austria) with packages of “ggpairs”, “splines”, “dlnm”, “glm”, “epiR”, and “mgcv”. All p-values were two-sided, and statistical significance was claimed when p < 0.05.
2.2.3 Subgroup Analysis
Studies have shown that people under age of 15 are at high risk of mumps, and schools and nurseries are the main places for mumps outbreaks, age was previously reported to be a risk factor for mumps (Leah et al., 2021). Thus, subgroup analysis by 0–4 years, 5–14 years and over 15 age of years was performed to examine the effect of age disparities on the interaction effect of meteorological factors and ambient air pollutants on mumps incidences.
2.3 Sensitivity Analysis
To check the sensitivity of DLNM statistics results, we performed the following sensitivity analysis respectively. First, we changed the degree of freedom for meteorological factors (relative humidity, temperature), air pollutants (PM2.5, O3), and time from 2 to 9.
3 Results
3.1 Descriptive Analysis
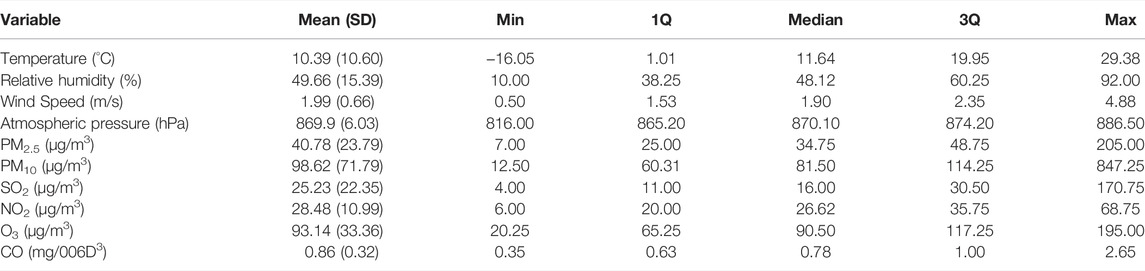
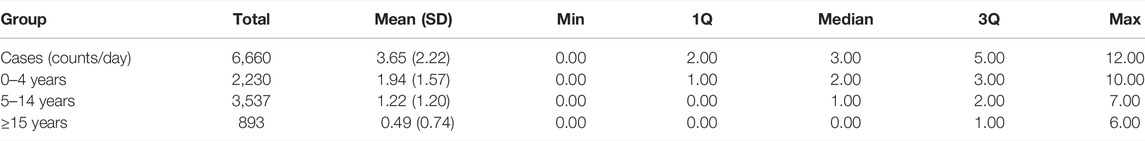
Tables, 1, 2 present the characteristics of environmental factors and mumps cases from January 2015 through December 2019. According to GB3095-2012 standards, the annual average concentrations of PM2.5 (40.78 μg/m3) and PM10 (98.62 μg/m3) exceeded China’s ambient air quality secondary standards (35 μg/m3, 75 μg/m3), while the other pollutants (SO2, NO2, O3, CO) are within the permissible limits (60 μg/m3, 40 μg/m3, 160 μg/m3 and 4 mg/m3). The daily average values of temperature, relative humidity, wind speed, air pressure, and a number of cases in the Ningxia area were 10.39 °C, 49.66%, 1.99 m/s, 869.90 hpa, and 3.63, respectively.
Supplementary Appendix Figure S2 shows the time series of daily cases of mumps, meteorological factors, and air pollutants from 1 January 2015 to 31 December 2019. We observed that mumps cases were distributed annually in each season, with a slightly higher incidence during summer than in winter. The concentrations of air pollutants had seasonality and were significantly higher in winter than that in summer, and presented a marked downward trend over time. Moreover, Supplementary Appendix Figure S3 presents the correlation coefficient matrix and scatter plot between mumps cases and part of the environmental variables of concern.
3.2 Distributed Lag Non-linear Models
As shown in Figure 1, the relationship between meteorological factors (temperature and relative humidity) and air pollutants (PM2.5 and O3) in relation to mumps cases. The association between risk of mumps and temperature has a gradual upward trend. Meanwhile, though not statistically significant, a U-shaped curve with a trough (50%) was observed for relative humidity. For PM2.5 and O3, approximate inverted shape S were observed, with the first minimum at 47µg/m3 and 86 μg/m3, respectively. Accordingly, we divided meteorological factors (temperature and relative humidity) and pollutants (PM2.5, O3) into binary variables based on quartiles or DLNM turning points as cutoff. One group is composed of three levels of temperature (low, moderate, high), which combined with two levels (low and high) for two air pollutants (PM2.5 and O3), generated 12 categories (3
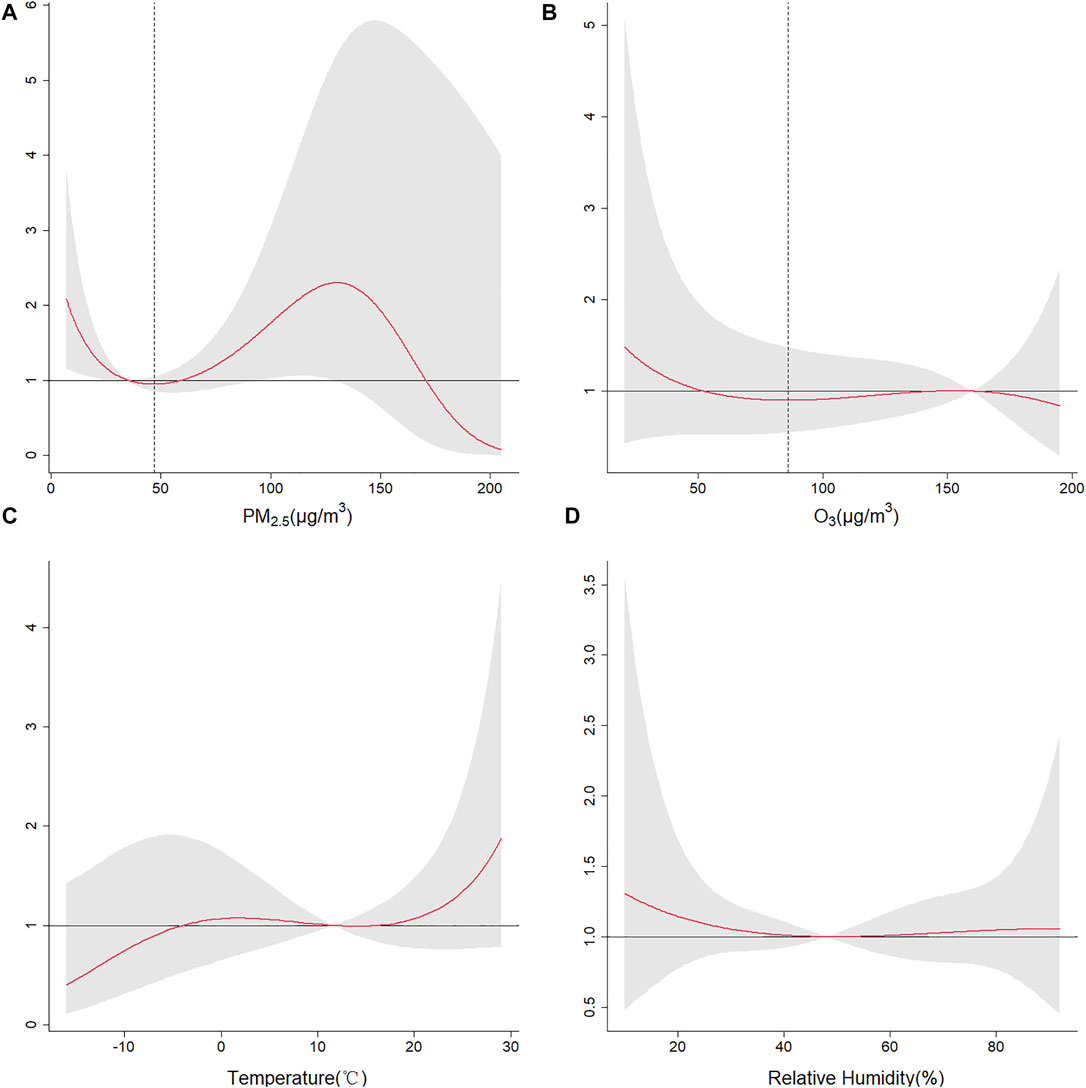
FIGURE 1. Plot of cumulative RR of mumps by environmental factors in Ningxia, 2015–2019. (A) For PM2.5; (B) for O3; (C) for temperature; and (D) for relative humidity.
3.3 Interaction Analysis
Table 3 shows the results of the interaction effect between air pollutants and meteorological factors on mumps. For PM2.5 and O3, the first minimum at 47µg/m3 and 86µg/m3 were taken as the turning points based on DLNM results. The multiplicative and additive interaction effects were generally consistent among for the same pair of meteorological factor and pollutant. Evident multiplicative and additive interactions between meteorological factors and PM2.5 were found with IRR of 1.14 (95%CI: 1.01, 1.29) and RERI of 0.17 (95%CI: 0.02, 0.32) for moderate level of temperature at 12°C, and IRR of 1.37 (95%CI: 1.14, 1.66), RERI of 0.36 (95%CI: 0.11, 0.60) for high level of temperature at 20°C, respectively. These results indicated that PM2.5 and temperature have a significant synergistic effect on the cases of mumps, while no interaction between relative humidity and PM2.5 is observed. Regarding O3 and meteorological factors (temperature = 12°C, 20°C), IRR and RERI were 1.33 (95%CI: 1.17, 1.52) and 0.30 (95%CI: 0.16, 0.45), 1.91 (95%CI: 1.46, 2.49) and 0.69 (95%CI: 0.32, 1.07), respectively. And IRR of 1.17 (95%CI: 1.06, 1.29), RERI of 0.13 (95%CI: 0.04, 0.21) for middle level of relative humidity at 48%. This demonstrated that temperature and relative humidity interact with O3 on the risk of mumps synergistically.
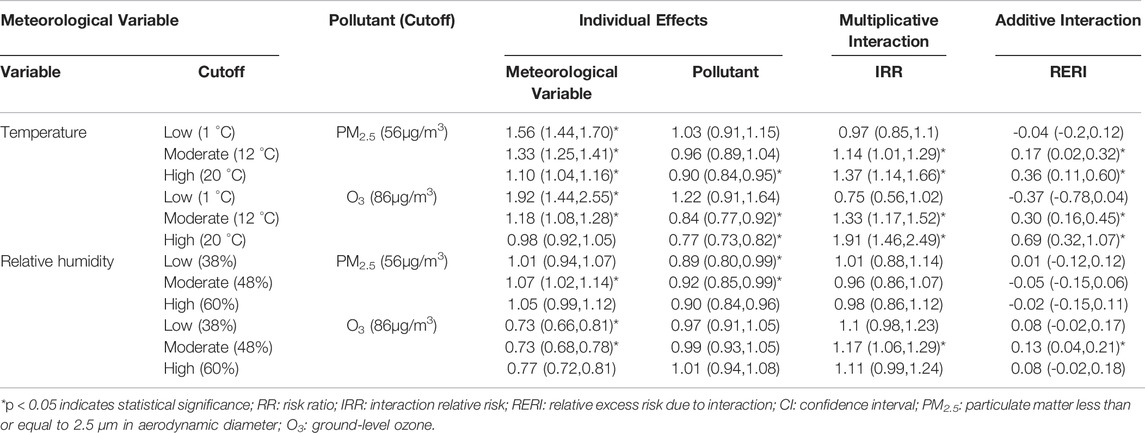
TABLE 3. Additive and multiplicative interactive analysis between meteorological variables and air pollutants on mumps.
In addition, as shown in Figure 2, the estimated number of mumps served as the response variable, bivariate response surface analysis appeared nonlinearly that was also verified that the interactive effect of air pollutants (PM2.5, O3) and meteorological factors (relative humidity, temperature) were non-linear and joint association with mumps.
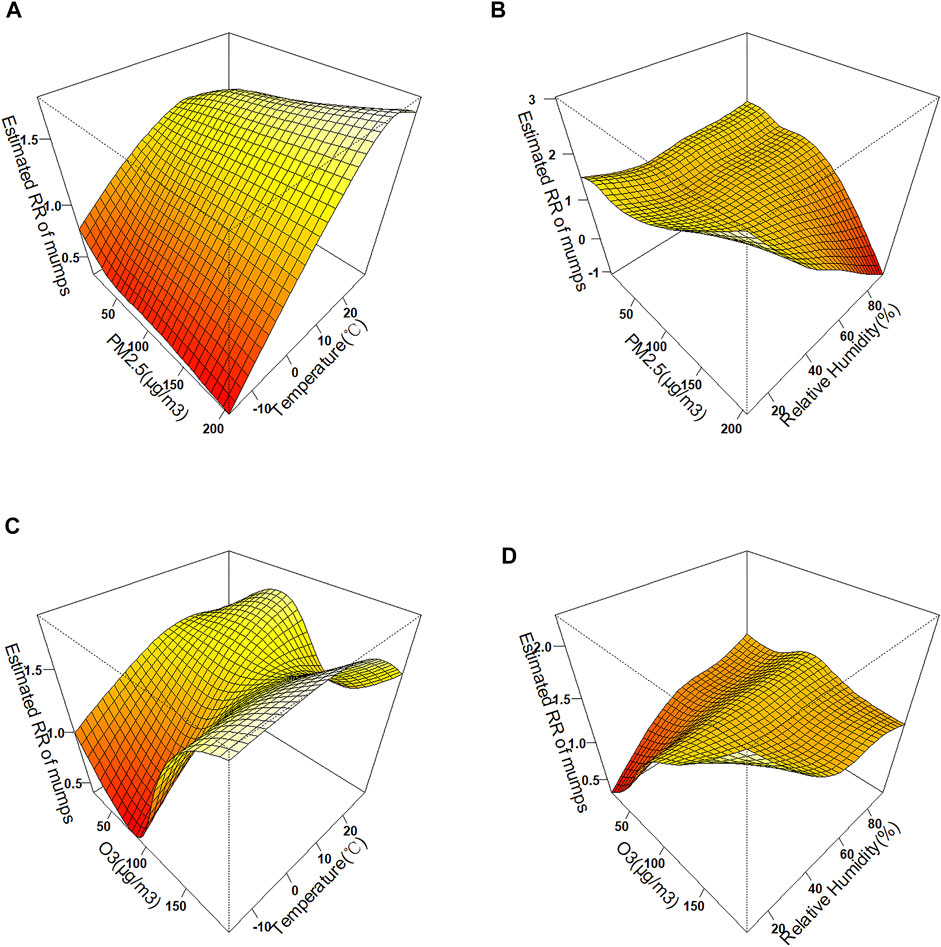
FIGURE 2. Bivariate response surfaces of meteorology and air pollutants in Ningxia, China, 2015–2019. (A) For temperature and PM2.5; (B) for relative humidity and PM2.5; (C) for temperature and O3; and (D) for relative humidity and O3.
From the sensitivity analysis, our findings were consistent in similar scale and same sign, including the alternative degree of freedom of PM2.5 and O3 from 2 to 9 (see Supplementary Appendix Figure S4) and alternative degree of freedom of time variable (for long-term trend and seasonality) from 2 to 9 (see Supplementary Appendix Figure S5). The non-linear associations between PM2.5 (O3, temperature and relative humidity) and Mumps appeared consistent across a wide range of model assumptions, which implies the robustness of our main findings. In addition, these results were still clear and robust when change the time to character the long-time trend and seasonality.
4 Discussion
This study explored the effects of meteorological factors and air pollutants on mumps by constructing a DLNM model. The time-series plots indicated that meteorological factors and air pollutants showed evident seasonality, and the scatterplot matrix suggested mild but significant pairwise correlations between these variables. The results of the DLNM model showed a nonlinear relationship between all environmental factors and the cases of mumps, with some variability in the effect on the cumulative effect of mumps. We found that the exposure-response curves for temperature and mumps were approximately S-shaped, which was similar to previous studies (Yang et al., 2014). Compared with the low temperature, the risk of morbidity is higher at high temperatures, some epidemiological studies indicated that the participation of adolescents in physical activities decreases during cold periods and increases with warmer temperatures (Belanger et al., 2009), which increases the risk of mumps infection through more frequent contact among children and adolescents because of the appropriate temperature.
In terms of relative humidity, we found that lower relative humidity increased the risk of mumps, which differs from studies in Jining (Li et al., 2016) and Fujian (Hu et al., 2018). Some studies have shown that the survival of enveloped viruses is higher at low relative humidity. It may be attributed to the fact that viruses are more stable in dry conditions and can be easily preserved for a long time (Aguilera and Karel, 1997; Morgan et al., 2006).
In addition to meteorological factors, we included PM2.5 and O3 for exploring the potential impact of atmospheric pollutants on mumps and observed that the risk of morbidity was higher at high levels of PM2.5 while it decreased gradually with further increasing concentrations, whereas the risk of morbidity was found higher at lower O3 levels and declined progressively as concentration increased. Zhang et al.(Zhang and Zhu, 2021) found a positive association between PM2.5 and mumps cases. Pulmonary macrophages play an important role in binding and clearing of inhaled particulate matter (Arredouani et al., 2004; Arredouani et al., 2006), whereas exposure to PM2.5 decrease the antimicrobial activity of pulmonary macrophages (Migliaccio et al., 2013), which probably increased the body’s susceptibility for respiratory tract infections. Xie et al. (Xie et al., 2021) reported that Ozone exposure can increase the risk of mumps infection. A possible reason is that environmental pollutants can impair ciliary structure and function to impact mucociliary clearance, and can result in lower respiratory tract disease (Cao et al., 2020).
Regarding the interactive and subgroup analysis, we found significant interactions between PM2.5 and O3 with meteorological factors. Moderate and high temperatures increased the risk of mumps from high PM2.5. Regarding the lower level of O3, both moderate relative humidity and moderate and high temperatures increase the risk of mumps. The significant age disparities in the interaction effect of meteorological and air pollutants factors on mumps incidences were found in Table. 4, which was consistent with the result in Guangzhou (Lu et al., 2019). The 5–14 years age group is more susceptible to pollutants and meteorological factors than the other age groups. Thus, protective measures and health education for children and adolescents of 5–14 years may be an advantage to reduce the risks of Mumps. Some reasonable mechanisms may be responsible for this. On the one hand, high temperatures increase thermoregulatory as well as immune system stress (Garrett et al., 2009; Dittmar et al., 2014), which probably increases susceptibility to air pollution (Gordon, 2003). In contrast, the relative humidity could moderate the area of the air-liquid interface for virus accumulation, and the size and surface area of the aerosol is larger with increasing relative humidity, which might enhance the exposure of virus on the air-liquid interface area, in response to these mechanisms (surface tension, shear stress, and hydrophobically driven conformational rearrangements), the viruses partition on the surface of aerosols may be damaged (Casanova et al., 2010; Yang and Marr, 2012). On the other hand, the interaction of heat stress and air pollutants worsened respiratory distress (McCormack et al., 2016). Additionally, particulate matter and ozone can induce oxidative stress leading to apoptosis (Jaspers et al., 2005; Wang et al., 2010), and people with enhanced oxidative stress are more susceptible to virus infection (Ciencewicki et al., 2008). Nevertheless, it was argued that O3 could reduce the risk of respiratory infection that might be attributed to O3 exposure induced protective immunity of interleukin (IL)-33 against viral infection (Ali et al., 2018) while enveloped viruses probably lose infectivity after exposure to O3 by undergoing lipid peroxidation (Murray et al., 2008).
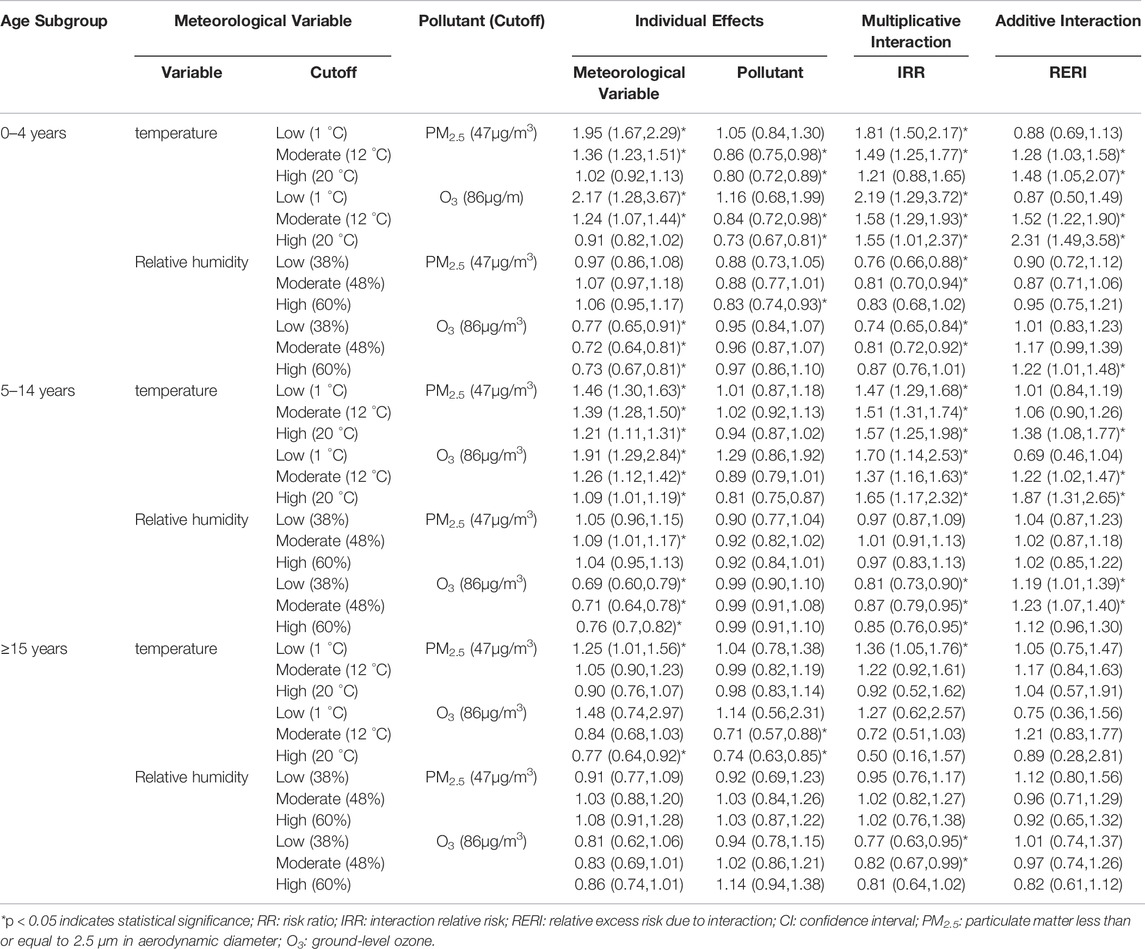
TABLE 4. Subgroup interactive analysis between meteorological variables and air pollutants on mumps.
Although we explored some new aspects of the relationship between mumps and ambient factors. The study also contained several limitations. First, we selected the specific pollutants (PM2.5 and O3) in this study, while similar effects of other pollutants may be explored in further investigations. Second, due to the insufficient number of daily cases in each city for modeling analysis, we pooled the number of daily cases by province-level to achieve sufficient statistical power. Third, the new index should be considered to evaluate the optimal model in environmental epidemiology (Zhou et al., 2021). Finally, environmental factors were used for our analysis, which inadequately represents the real exposure levels of individuals, resulting in ecological fallacies.
This study possesses notable strengths, with the exploration of the interaction between air pollution and meteorological factors with mumps cases. Furthermore, differing from previous studies, we targeted specific pollutants rather than AQI for analysis to explore the interaction of different concentrations of pollutants and meteorological factors as well as the impact on mumps. It is crucial for further understanding of the impact of meteorological factors and air pollution on human health.
Conclusion
Higher temperature and lower relative humidity were found associating with higher incidence rate of mumps as well as high concentration of PM2.5 and low concentration of O3. Our study brought insights into the interactive association of air pollution and meteorological factors in relation to the risk of mumps. Simultaneously, understanding the interaction of air pollution and meteorological factors on mumps is essential for implementing precise and effective public health intervention strategies to predict the impact of changes in environmental factors in arid and semi-arid areas.
Data Availability Statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Author Contributions
WL: formal analysis, writing the original draft. SZ: methodology, writing—review and editing. RG: project administration, resources, review editing. YZ: writing—review and editing. FD: validation, methodology. RW: writing—review and editing. XL: investigation, data curation. LZ: investigation, data curation. YZ: methodology, supervision, writing—review and editing.
Funding
This work was supported by the National Natural Science Foundation of China (12061058), Natural Science Foundation of Ningxia (2020AAC03186), and Ningxia Key Research and Development Project (2021BEG02026).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fenvs.2022.937450/full#supplementary-material
References
Aguilera, J. M., and Karel, M. (1997). Preservation of Biological Materials under Desiccation. Crit. Rev. Food Sci. Nutr. 37 (3), 287–309. doi:10.1080/10408399709527776
Ali, S. T., Wu, P., Cauchemez, S., He, D., Fang, V. J., Cowling, B. J., et al. (2018). Ambient Ozone and Influenza Transmissibility in Hong Kong. Eur. Respir. J. 51 (5), 1800369. doi:10.1183/13993003.00369-2018
Arredouani, M. S., Yang, Z., Imrich, A., Ning, Y., Qin, G., and Kobzik, L. (2006). The Macrophage Scavenger Receptor SR-AI/II and Lung Defense against Pneumococci and Particles. Am. J. Respir. Cell. Mol. Biol. 35 (4), 474–478. doi:10.1165/rcmb.2006-0128OC
Arredouani, M., Yang, Z., Ning, Y., Qin, G., Soininen, R., Tryggvason, K., et al. (2004). The Scavenger Receptor MARCO Is Required for Lung Defense against Pneumococcal Pneumonia and Inhaled Particles. J. Exp. Med. 200 (2), 267–272. doi:10.1084/jem.20040731
Austin, M. A., Beaty, T. H., and Dotson, W. D. (2013). Genetic Epidemiology: Methods and applicationsGenetic Epidemiology: Methods and Applications. Wallingford, United Kingdom: CABI.
Bélanger, M., Gray-Donald, K., O'Loughlin, J., Paradis, G., and Hanley, J. (2009). Influence of Weather Conditions and Season on Physical Activity in Adolescents. Ann. Epidemiol. 19 (3), 180–186. doi:10.1016/j.annepidem.2008.12.008
Cao, Y., Chen, M., Dong, D., Xie, S., and Liu, M. (2020). Environmental Pollutants Damage Airway Epithelial Cell Cilia: Implications for the Prevention of Obstructive Lung Diseases. Thorac. Cancer 11 (3), 505–510. doi:10.1111/1759-7714.13323
Casanova, L. M., Jeon, S., Rutala, W. A., Weber, D. J., and Sobsey, M. D. (2010). Effects of Air Temperature and Relative Humidity on Coronavirus Survival on Surfaces. Appl. Environ. Microbiol. 76 (9), 2712–2717. doi:10.1128/AEM.02291-09
Ciencewicki, J., Trivedi, S., and Kleeberger, S. R. (2008). Oxidants and the Pathogenesis of Lung Diseases. J. Allergy Clin. Immunol. 122 (3), 456–468. doi:10.1016/j.jaci.2008.08.004
Dittmar, J., Janssen, H., Kuske, A., Kurtz, J., and Scharsack, J. P. (2014). Heat and Immunity: an Experimental Heat Wave Alters Immune Functions in Three-Spined Sticklebacks (Gasterosteus aculeatus). J. Anim. Ecol. 83 (4), 744–757. doi:10.1111/1365-2656.12175
Du, Z., Lawrence, W. R., Zhang, W., Zhang, D., Yu, S., and Hao, Y. (2019). Interactions between Climate Factors and Air Pollution on Daily HFMD Cases: A Time Series Study in Guangdong, China. Sci. Total Environ. 656, 1358–1364. doi:10.1016/j.scitotenv.2018.11.391
Garrett, A. T., Goosens, N. G., Rehrer, N. G., Patterson, M. J., and Cotter, J. D. (2009). Induction and Decay of Short-Term Heat Acclimation. Eur. J. Appl. Physiol. 107 (6), 659–670. doi:10.1007/s00421-009-1182-7
Gasparrini, A., Armstrong, B., and Kenward, M. G. (2010). Distributed Lag Non-linear Models. Stat. Med. 29 (21), 2224–2234. doi:10.1002/sim.3940
Ge, E., Lai, K., Xiao, X., Luo, M., Fang, Z., Zeng, Y., et al. (2018). Differential Effects of Size-specific Particulate Matter on Emergency Department Visits for Respiratory and Cardiovascular Diseases in Guangzhou, China. Environ. Pollut. 243 (Pt A), 336–345. doi:10.1016/j.envpol.2018.08.068
Gordon, C. J. (2003). Role of Environmental Stress in the Physiological Response to Chemical Toxicants. Environ. Res. 92 (1), 1–7. doi:10.1016/s0013-9351(02)00008-7
Hao, J., Yang, Z., Huang, S., Yang, W., Zhu, Z., Tian, L., et al. (2019). The Association between Short-Term Exposure to Ambient Air Pollution and the Incidence of Mumps in Wuhan, China: A Time-Series Study. Environ. Res. 177, 108660. doi:10.1016/j.envres.2019.108660
Ho, Y.-C., Su, B.-H., Su, H.-J., Chang, H.-L., Lin, C.-Y., Chen, H., et al. (2015). The Association between the Incidence of Mumps and Meteorological Parameters in Taiwan. Hum. Vaccines Immunother. 11 (6), 1406–1412. doi:10.1080/21645515.2015.1029687
Hu, A., Hao, L. X., and Hq, W. (2014). Local Green Practice. China Vaccine Immun. 20 (2), 127–153. doi:10.1007/978-3-642-54962-5_6
Hu, W., Li, Y., Han, W., Xue, L., Zhang, W., Ma, W., et al. (2018). Meteorological Factors and the Incidence of Mumps in Fujian Province, China, 2005-2013: Non-linear Effects. Sci. Total Environ. 619-620, 1286–1298. doi:10.1016/j.scitotenv.2017.11.108
Hu, Z., Chen, X., Zhou, Q., Chen, D., and Li, J. (2019). DISO: A Rethink of Taylor Diagram. Int. J. Climatol. 39, 2825–2832. doi:10.1002/joc.5972
Hviid, A., Rubin, S., and Mühlemann, K. (2008). Mumps. Lancet 371 (9616), 932–944. doi:10.1016/S0140-6736(08)60419-5
Jaspers, I., Ciencewicki, J. M., Zhang, W., Brighton, L. E., Carson, J. L., Beck, M. A., et al. (2005). Diesel Exhaust Enhances Influenza Virus Infections in Respiratory Epithelial Cells. Toxicol. Sci. 85 (2), 990–1002. doi:10.1093/toxsci/kfi141
Li, R., Lin, H., Liang, Y., Zhang, T., Luo, C., Jiang, Z., et al. (2016). The Short-Term Association between Meteorological Factors and Mumps in Jining, China. Sci. Total Environ. 568, 1069–1075. doi:10.1016/j.scitotenv.2016.06.158
Lu, J., Yang, Z., Ma, X., Ma, M., and Zhang, Z. (2019). The Role of Meteorological Factors on Mumps Incidence Among Children in Guangzhou, Southern China. PLoS ONE 15 (4), e0232273. doi:10.1371/journal.pone.0232273
Lu, P., Xia, G., Zhao, Q., Xu, R., Li, S., and Guo, Y. (2020). Temporal Trends of the Association between Ambient Temperature and Hospitalisations for Cardiovascular Diseases in Queensland, Australia from 1995 to 2016: A Time-Stratified Case-Crossover Study. PLoS Med. 17 (7), e1003176. doi:10.1371/journal.pmed.1003176
Maura, L., and Elisabetta, B. (2011). Oxidative Stress and Air Pollution Exposure. J. Toxicol 2011, 487074. doi:10.1155/2011/487074
McCormack, M. C., Belli, A. J., Waugh, D., Matsui, E. C., Peng, R. D., Williams, D. A. L., et al. (2016). Respiratory Effects of Indoor Heat and the Interaction with Air Pollution in Chronic Obstructive Pulmonary Disease. Ann. ATS 13 (12), 2125–2131. doi:10.1513/AnnalsATS.201605-329OC
Migliaccio, C. T., Kobos, E., King, Q. O., Porter, V., Jessop, F., and Ward, T. (2013). Adverse Effects of Wood Smoke PM(2.5) exposure on Macrophage Functions. Inhal. Toxicol. 25 (2), 67–76. doi:10.3109/08958378.2012.756086
Ministry of Ecology and Environment of China, (2021). 2020 Bulletin on China’s Ecological Environment. Available at: https://www.mee.gov.cn/hjzl/sthjzk/zghjzkgb/202105/P020210526572756184785.pdf.
Mokoena, K. K., Ethan, C. J., Yu, Y., and Quachie, A. T. (2020). Interaction Effects of Air Pollution and Climatic Factors on Circulatory and Respiratory Mortality in Xi'an, China between 2014 and 2016. Ijerph 17 (23), 9027. doi:10.3390/ijerph17239027
Morgan, C. A., Herman, N., White, P. A., and Vesey, G. (2006). Preservation of Micro-organisms by Drying; a Review. J. Microbiol. Methods 66 (2), 183–193. doi:10.1016/j.mimet.2006.02.017
Murray, B. K., Ohmine, S., Tomer, D. P., Jensen, K. J., Johnson, F. B., Kirsi, J. J., et al. (2008). Virion Disruption by Ozone-Mediated Reactive Oxygen Species. J. Virological Methods 153 (1), 74–77. doi:10.1016/j.jviromet.2008.06.004
Myers, R. H., Montgomery, D. C., Vining, G. G., Borror, C. M., and Kowalski, S. M. (2004). Response Surface Methodology: A Retrospective and Literature Survey. J. Qual. Technol. 36 (1), 53–77. doi:10.1080/00224065.2004.11980252
Pan, R., Wang, X., Yi, W., Wei, Q., Gao, J., Xu, Z., et al. (2020). Interactions between Climate Factors and Air Quality Index for Improved Childhood Asthma Self-Management. Sci. Total Environ. 723, 137804. doi:10.1016/j.scitotenv.2020.137804
Richardson, M., Elliman, D., Maguire, H., Simpson, J., and Nicoll, A. (2001). Evidence Base of Incubation Periods, Periods of Infectiousness and Exclusion Policies for the Control of Communicable Diseases in Schools and Preschools. Pediatr. Infect. Dis. J. 20 (4), 380–391. doi:10.1097/00006454-200104000-00004
Shepersky, L., Marin, M., Zhang, J., Pham, H., and Marlow, M. A. (2021). Mumps in Vaccinated Children and Adolescents: 2007-2019. Pediatrics 148 (6), e2021051873. doi:10.1542/peds.2021-051873
Song, C., Wu, L., Xie, Y., He, J., Chen, X., Wang, T., et al. (2017). Air Pollution in China: Status and Spatiotemporal Variations. Environ. Pollut. 227, 334–347. doi:10.1016/j.envpol.2017.04.075
Su, Q. R., Liu, J., Ma, C., Fan, C. X., Wen, N., and Hm, L. (2016). Analysis of Epidemiological Characteristics of Mumps in China from 2004-2013. Chin. J. Prev. Med. 50 (7), 611–614. doi:10.3760/cma.j.issn.0253-9624.2016.07.009
Wang, T., Chiang, E. T., Moreno-Vinasco, L., Lang, G. D., Pendyala, S., Samet, J. M., et al. (2010). Particulate Matter Disrupts Human Lung Endothelial Barrier Integrity via ROS- and P38 MAPK-dependent Pathways. Am. J. Respir. Cell. Mol. Biol. 42 (4), 442–449. doi:10.1165/rcmb.2008-0402OC
WHO (World Health Organization) (2022). Air Pollution. Available at: https://www.who.int/health-topics/air-pollution#tab=tab_1 (Accessed April 21, 2022).
Wu, H., You, E., Jiang, C., Yang, Y., Wang, L., Niu, Q., et al. (2020). Effects of Extreme Meteorological Factors on Daily Mumps Cases in Hefei, China, during 2011-2016. Environ. Sci. Pollut. Res. 27 (4), 4489–4501. doi:10.1007/s11356-019-07073-y
Xie, W., Zhao, H., Shu, C., Wang, B., Zeng, W., and Zhan, Y. (2021). Association between Ozone Exposure and Prevalence of Mumps: a Time-Series Study in a Megacity of Southwest China. Environ. Sci. Pollut. Res. 28 (45), 64848–64857. doi:10.1007/s11356-021-15473-2
Xu, D., Zhang, Y., Wang, B., Yang, H., Ban, J., Liu, F., et al. (2019). Acute Effects of Temperature Exposure on Blood Pressure: An Hourly Level Panel Study. Environ. Int. 124, 493–500. doi:10.1016/j.envint.2019.01.045
Yang, Q., Yang, Z., Ding, H., Zhang, X., Dong, Z., Hu, W., et al. (2014). The Relationship between Meteorological Factors and Mumps Incidence in Guangzhou, China, 2005-2012:. Hum. Vaccines Immunother. 10 (8), 2421–2432. doi:10.4161/hv.29286
Yang, W., and Marr, L. C. (2012). Mechanisms by Which Ambient Humidity May Affect Viruses in Aerosols. Appl. Environ. Microbiol. 78 (19), 6781–6788. doi:10.1128/AEM.01658-12
Yu, G., Yang, R., Yu, D., Cai, J., Tang, J., Zhai, W., et al. (2018). Impact of Meteorological Factors on Mumps and Potential Effect Modifiers: An Analysis of 10 Cities in Guangxi, Southern China. Environ. Res. 166, 577–587. doi:10.1016/j.envres.2018.06.047
Zhang, M., and Zhu, Y. (2021). Association between Particulate Matter Pollution and the Incidence of Mumps in 31 Provinces from China. Environ. Sci. Pollut. Res. 28 (37), 51210–51216. doi:10.1007/s11356-021-14287-6
Zhou, Q., Chen, D., Hu, Z., and Chen, X. (2021). Decompositions of Taylor Diagram and DISO Performance Criteria. Int. J. Climatol. 41, 5726–5732. doi:10.1002/joc.7149
Keywords: meteorological factors, pollutant, mumps, interactive effects, China
Citation: Liu W, Zhao S, Gong R, Zhang Y, Ding F, Zhang L, Li X, Wang R, Ma N and Zhao Y (2022) Interactive Effects of meteorological Factors and Ambient air Pollutants on Mumps Incidences in Ningxia, China Between 2015 and 2019. Front. Environ. Sci. 10:937450. doi: 10.3389/fenvs.2022.937450
Received: 06 May 2022; Accepted: 23 May 2022;
Published: 07 July 2022.
Edited by:
Zengyun Hu, Chinese Academy of Sciences (CAS), ChinaReviewed by:
Mingwang Shen, Xi’an Jiaotong University, ChinaZhaobin Sun, China Meteorological Administration, China
Copyright © 2022 Liu, Zhao, Gong, Zhang, Ding, Zhang, Li, Wang, Ma and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu Zhao, zhaoyu@nxmu.edu.cn
†These authors have contributed equally to this work
 Weichen Liu
Weichen Liu Shi Zhao
Shi Zhao Rui Gong5
Rui Gong5  Yu Zhao
Yu Zhao